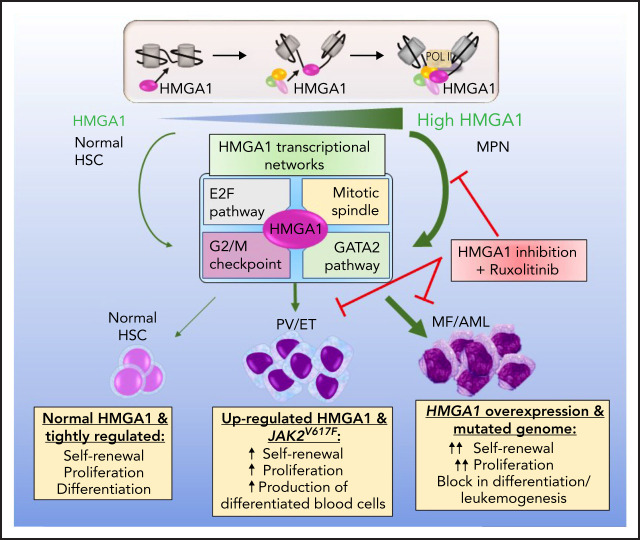
A major cause of mortality for patients with myeloproliferative neoplasms (MPN) is progression to myelofibrosis and acute leukemia. Li et al identified that High Mobility Group A1 (HMGA1) acts as an epigenetic switch during MPN progression and that HMGA1 deficiency prevents myelofibrosis and enhances sensitivity to ruxolitinib, prolonging survival in murine models of JAK2 mutant secondary acute myeloid leukemia. These data suggest HMGA1 is a therapeutic target to treat or prevent progression.
Key Points
HMGA1 is a novel epigenetic switch that induces aberrant transcriptional networks during MPN progression to MF and AML.
HMGA1 deficiency prevents MF and enhances sensitivity to ruxolitinib, prolonging survival in murine models of JAK2V617F AML.
Visual Abstract
Abstract
Myeloproliferative neoplasms (MPNs) transform to myelofibrosis (MF) and highly lethal acute myeloid leukemia (AML), although the actionable mechanisms driving progression remain elusive. Here, we elucidate the role of the high mobility group A1 (HMGA1) chromatin regulator as a novel driver of MPN progression. HMGA1 is upregulated in MPN, with highest levels after transformation to MF or AML. To define HMGA1 function, we disrupted gene expression via CRISPR/Cas9, short hairpin RNA, or genetic deletion in MPN models. HMGA1 depletion in JAK2V617F AML cell lines disrupts proliferation, clonogenicity, and leukemic engraftment. Surprisingly, loss of just a single Hmga1 allele prevents progression to MF in JAK2V617F mice, decreasing erythrocytosis, thrombocytosis, megakaryocyte hyperplasia, and expansion of stem and progenitors, while preventing splenomegaly and fibrosis within the spleen and BM. RNA-sequencing and chromatin immunoprecipitation sequencing revealed HMGA1 transcriptional networks and chromatin occupancy at genes that govern proliferation (E2F, G2M, mitotic spindle) and cell fate, including the GATA2 master regulatory gene. Silencing GATA2 recapitulates most phenotypes observed with HMGA1 depletion, whereas GATA2 re-expression partially rescues leukemogenesis. HMGA1 transactivates GATA2 through sequences near the developmental enhancer (+9.5), increasing chromatin accessibility and recruiting active histone marks. Further, HMGA1 transcriptional networks, including proliferation pathways and GATA2, are activated in human MF and MPN leukemic transformation. Importantly, HMGA1 depletion enhances responses to the JAK2 inhibitor, ruxolitinib, preventing MF and prolonging survival in murine models of JAK2V617F AML. These findings illuminate HMGA1 as a key epigenetic switch involved in MPN transformation and a promising therapeutic target to treat or prevent disease progression.
Introduction
Myeloproliferative neoplasms (MPNs) are clonal hematopoietic stem cell (HSC) disorders that are characterized by hyperactive JAK/STAT signaling and an increased risk for transformation to myelofibrosis (MF) and acute myeloid leukemia (AML).1-18 However, actionable mechanisms driving progression remain elusive, and therapies are ineffective after leukemic transformation. The most common driver mutation, JAK2V617F, enhances phosphorylation of STAT3/5 proteins, leading to overproduction of myeloid lineages.19-22 Most patients present with chronic indolent disease and elevations in platelets (essential thrombocythemia; ET) or red cells and platelets (polycythemia vera; PV), although a subset presents with primary MF that is characterized by bone marrow (BM) and splenic fibrosis, osteosclerosis, splenomegaly, pancytopenia, and shortened life spans.1-22 Although transformation to MF or AML is associated with acquisition of new mutations, therapies to prevent or treat transformation are lacking.2-26
Chromatin regulators maintain gene expression, conferring plasticity and other stem cell properties during development and oncogenic transformation.27 The HMGA1 chromatin regulator gene is highly expressed in embryonic and adult stem cells, with low or undetectable levels in most differentiated tissues.28-33 In diverse solid tumors, HMGA1 is aberrantly re-expressed; high levels are associated with adverse outcomes.28-30,33-44 Located on chromosome 6p21, HMGA1 encodes HMGA1a/HMGA1b protein isoforms that bind to AT-rich regions in DNA, displacing repressive histones that compact chromatin.28,29,34,45-52 After binding DNA and “opening” the minor groove, HMGA1 recruits transcriptional complexes to modulate gene expression.28,29,34,45-52 Transgenic mice overexpressing Hmga1 in lymphoid cells develop clonal expansion and leukemia.53-56 HMGA1 is also overexpressed in human lymphoid and myeloid malignancies.53-61 Intriguingly, a recent study found that germline lesions within the HMGA1 loci predispose individuals to MPN.62 However, the role of HMGA1 in MPN had not been elucidated.
Here, we report that HMGA1 is upregulated and activates specific transcriptional networks during MPN progression. HMGA1 deficiency enhances sensitivity to the JAK inhibitor ruxolitinib and delays leukemogenesis in murine models of JAK2V617 AML. Further, deletion of just a single Hmga1 allele prevents MF in JAK2V617F mice. Our findings demonstrate that HMGA1 is a key epigenetic switch in MPN, thus opening the door to novel therapeutic approaches to treat or prevent progression.
Methods
Murine models
Hmga1-deficient mice44,63 and JAK2V617F transgenic mice64,65 were crossed to obtain the desired genotypes. We generated leukemia xenografts (DAMI/SET-2 cells; 1-5 × 106) by tail vein injection into NOD Scid γ (NSG) mice. For transplantation studies, BM cells (4 × 106) from 16-week donors (JAK2V617F/V617F vs JAK2V617F/V617F with Hmga1 heterozygosity [Hmga1+/−]) were injected into lethally irradiated recipients (8 weeks; Ly5.1, 10 Gy).
Patient samples, cell lines, and in vitro studies
Patient samples, protein and RNA analyses, chromatin immunoprecipitation sequencing (ChIPseq), chromatin immunoprecipitation polymerase chain reaction (ChIP-PCR), assay for transposase-accessible chromatin-sequencing (ATACseq), flow cytometry, immunohistochemistry, and cell-based assays were performed as described.31-33,40-44,53-61,66-72 RNA sequencing (RNAseq)/ATACseq and ChIP-PCR in parental DAMI cells (with and without HMGA1 silencing) were performed in triplicate. DAMI (American Type Culture Collection),73,74 SET-2 (Leibniz Institute DSMZ),75 and UKE-1 (Coriell Institute)76 were cultured as recommended.
RNAseq analysis
RNAseq of JAK2V617F AML cells (DAMI/SET-2) was performed after transduction with control lentivirus or short hairpin RNA (shRNA) targeting HMGA1. Following data analyses, pathways were identified via MSig gene set enrichment analysis (GSEA).77,78 Data from RNAseq, Gene Expression Omnibus data sets (GSE103237,79 GSE122198,71 GSE14456870), and peripheral blood mononuclear cells (PBMCs) from matched patients with MF that transformed to AML were analyzed as described.26 Single-cell RNAseq (scRNAseq) was performed in BM-derived lineage−sca1+c-kit+ (LSK) cells from JAK2V617F/V617F mice with both Hmga1 alleles intact or with Hmga1 heterozygous deficiency (2 mice per condition) and analyzed as described.71,72
Statistical analysis
After ascertaining normal distributions (Ryan-Joyner, D’Agostino-Pearson tests), data were analyzed with a 2-tailed Student t test for 2 groups or 1-way analysis of variance (ANOVA), followed by Tukey’s multiple-comparison test; if not normal, we used the Mann-Whitney U test for 2 groups and the Kruskal-Wallis test, followed by Dunn’s test, for multiple comparisons. Cytotoxicity curves were analyzed by 2-way ANOVA. We compared survival using the Kaplan-Meier test, with the log-rank (Mantel-Cox) test and the Bonferroni method for multiple comparisons. Fisher’s exact test was used to compare differences in scRNAseq clusters across genotype. P < .05 was considered significant (GraphPad Prism 8.)
Additional details about methods and RNAseq analyses are provided in supplemental Methods (available on the Blood Web site).
Results
HMGA1 is overexpressed in MPN progression
To explore HMGA1 function in MPN, we first assessed gene expression in CD34+ cells from patients with MPN with acquired JAK2V617F mutations (Figure 1A). Compared with unaffected individuals, HMGA1 was upregulated in peripheral blood (PB) CD34+ cells, with the highest levels after leukemic transformation. In a separate cohort (GSE103237),79 HMGA1 was overexpressed in BM CD34+ cells from JAK2V617F ET and PV. Intriguingly, HMGA1 was not overexpressed in CALR-mutant ET. By scRNAseq of PB CD34+ cells (GSE122198),71 HMGA1 was also overexpressed in JAK2V617F mutant cells from MF compared with unmutated cells from the same patients or unaffected individuals. HMGA1 overexpression in CD34+ cells from patients with MF compared with age-matched healthy individuals was confirmed by scRNAseq in another cohort (GSE14456870). Together, these data demonstrate that HMGA1 is upregulated in JAK2V617 MPNs.
Figure 1.
HMGA1 is upregulated during MPN progression and required for leukemia engraftment. (Ai) Relative HMGA1 expression (mean ± standard deviation [SD]) performed in triplicate (quantitative polymerase chain reaction) in CD34+ cells from patients with MPN with acquired JAK2V617F mutations (PV, n = 8; MF, n = 5; AML, n = 6) or control subjects (Normal; n = 2). RPLP0 was used to control for loading. *P < .05, 1-way ANOVA, followed by Tukey’s multiple-comparison test. (Aii) HMGA1 expression in CD34+ cells from BM of patients with MPN with JAK2V617F ET (n = 17), JAK2V617F PV (n = 26), or CALR-mutant ET (n = 7) or from unaffected individuals (n = 15) by microarray. Each point represents a single patient. *P < .05, **P <. 01, ***P < .001, 1-way ANOVA, followed by Tukey’s multiple-comparison test. (Aiii) HMGA1 expression in JAK2-mutant CD34+ PB cells from patients with MF compared with unmutated CD34+ cells from the same patient with MF (n = 8) and unaffected individuals (n = 2) by scRNAseq; each point represents the expression level for a single cell. **P < .01, ***P < .001, 1-way ANOVA, followed by Tukey’s multiple-comparison test. (Aiv) HMGA1 expression in lineage− CD34+ PB from patients with MF and age-matched healthy donors. HMGA1 was detected in 81.1% of cells (30 786/37 941) from healthy donors and in 89.7% of cells (34 038/37 941) from patients with MF. White dots on the violin plot indicate the mean level of expression; black points represent expression values for each single cell. ***P ≤ .001, Wilcoxon rank-sum test. (B) Western blot analysis of HMGA1, β-actin, and GAPDH (loading control) protein levels from DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing. Western blots were performed 3 times; a representative blot is shown. Size markers (kDa) are indicated. (C) Proliferation (mean ± SD) estimated by MTS [3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium; Promega)] in DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2; mean ± SD, at the indicated time points. ***P < .001, 2-tailed Student t test. (D) Colony-forming units (CFU; mean ± SD) in DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2), performed in triplicate from 2 independent experiments (upper panels). Representative images of colonies are shown (lower panels). Scale bars, 200 μm. ***P < .001; 2-tailed Student t test. (E) Edu (5-ethynyl-2′-deoxyuridine) cell cycle analysis (mean ± SD) by flow cytometry assessed in DAMI, SET-2 and UKE-1 cells, with or without HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2), performed in triplicate from 2 independent experiments; *P < .05, **P < .01, ***P < .001; 2-tailed Student t test. (F) Annexin V apoptosis by flow cytometry assessed in DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2), performed in triplicate from 2 independent experiments, ***P < .001; 2-tailed Student t test. Representative density plots from each group are also shown. (G) Representative images of spleens and graphical comparisons of relative spleen weight (spleen/body weight %; mean ± SD); leukemia cell engraftment by flow cytometry (mean ± SD) in spleen from NSG mice injected with DAMI cells and SET-2 cells, with or without HMGA1 silencing (control vs HMGA1-sh1; n = 4 or 5 per group). *P < .05, **P < .01, ***P < .001; 2-tailed Student t test. (H) Leukemia cell engraftment (mean ± SD) assessed by flow cytometry in BM from NSG mice injected with DAMI cells (left panel) or SET-2 cells (middle panel), with or without HMGA1 silencing (control vs HMGA1-sh1; n = 4 or 5 per group). Representative flow cytometry plots from each group and hematoxylin and eosin-stained BM from DAMI cells (right panels). Scale bar, 200 μm. ***P < .001; 2-tailed Student t test. (I) Survival analysis by Kaplan-Meier estimate in NSG mice injected with DAMI cells, with or without HMGA1 silencing (Control: median survival, 24 days vs HMGA1-sh1: median survival, 38 days; n = 6 per group). ***P < .001, log-rank (Mantel-Cox) test. mRNA, messenger RNA; ns, not significant.
HMGA1 is required for proliferation, clonogenicity, and leukemic engraftment
Next, we disrupted gene expression via shRNA targeting 2 HMGA1 sequences or by CRISPR/Cas9 in JAK2V617F AML cell lines (DAMI, SET-2, UKE-1).73-76 Strikingly, depleting HMGA1 in all cell lines disrupts proliferation and clonogenicity, decreasing colony number and size (Figure 1B-D; supplemental Figure 1A-F). HMGA1 depletion also decreases the percentage of cells in S phase while increasing apoptosis (Figure 1E-F). Notably, HMGA2, a related HMGA family member, did not change with HMGA1 silencing (supplemental Figure 1A). Next, we compared leukemic engraftment following tail vein injection of AML cells into NSG mice. HMGA1 depletion in DAMI or SET-2 cells decreases spleen size, circulating blasts, and leukemic engraftment in BM and spleen 23 days following injection (Figure 1G-H; supplemental Figure 2A). BM architecture was generally normal in recipients of HMGA1-depleted cells, whereas architecture was effaced by leukemic blasts in recipients of AML cells lacking HMGA1 depletion. Survival was also prolonged in recipients of AML cells with HMGA1 silencing (Figure 1I; supplemental Figure 2A). Intriguingly, the small percentage of engrafted blasts from the pool of AML cells with HMGA1 silencing express higher HMGA1 than do the injected cells, suggesting that escape from gene silencing allows these cells to engraft (supplemental Figure 2B-C). Our findings indicate that HMGA1 is required for salient AML phenotypes, including proliferation, clonogenicity, and leukemic engraftment.
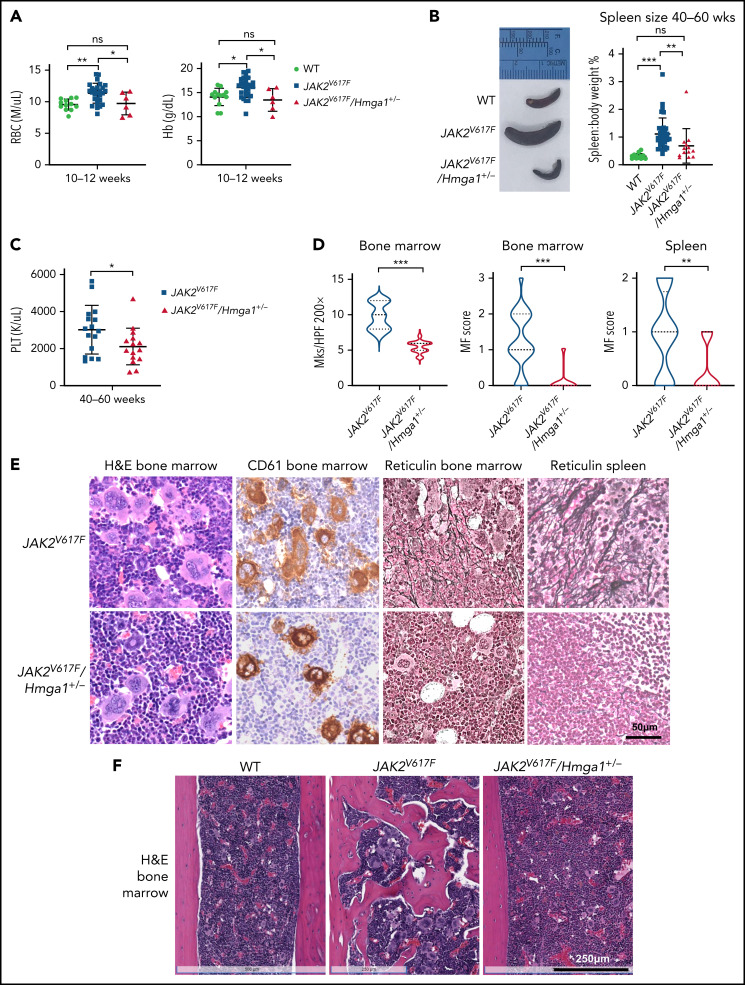
Hmga1 haploinsufficiency prevents progression to MF
To investigate HMGA1 in models of chronic MPN, we crossed a well-characterized JAK2V617F transgenic model64,65 onto a background with global heterozygous Hmga1 deficiency.44,63 JAK2V617F mice express 13 copies of the transgene and recapitulate features of chronic MPN with erythrocytosis and thrombocytosis by 12 weeks and progression to MF by 40 weeks, with osteosclerosis, splenomegaly, and fibrosis involving the spleen and BM (Figure 2; supplemental Figure 3A). Importantly, Hmga1 heterozygous mice have normal life spans and unperturbed hematopoiesis, based on steady-state blood counts, for up to 60 weeks (supplemental Figure 3B). Strikingly, loss of a single Hmga1 allele in JAK2V617F mice prevents progression to MF, decreasing erythrocytosis by 12 weeks, and thrombocytosis, megakaryocyte hyperplasia, splenomegaly, fibrosis (spleen, BM) and osteosclerosis after 40 weeks (Figure 2).
Figure 2.
Hmga1 is required for progression of chronic MPN to MF in JAKV617F-mutant mice. (A) Red blood cell (RBC) count and hemoglobin (Hb) (mean ± standard deviation [SD]) in PB from 10- to 12-week-old WT, JAK2V617F, and JAK2V617F/Hmga1+/− mice. (B) Representative spleens (left panel) and graph showing relative spleen sizes (right panel; mean ± SD) in WT, JAK2V617F, and JAK2V617F/Hmga1+/− mice. (C) Platelet (PLT) count from 40- to 60-week-old JAK2V617F and JAK2V617F/Hmga1+/− mice. (D) Megakaryocytes per high-power field (Mks/HPF) in BM from JAK2V617F and JAK2V617F/Hmga1+/− mice (left panel). MF scores in BM (middle panel) and spleen (right panel) from JAK2V617F and JAK2V617F/Hmga1+/− mice. (E) Representative images from mouse models stained with hematoxylin and eosin (H&E of BM from femurs; left panels), CD61 by immunohistochemistry (BM from femurs; left middle panels), fibrosis (BM reticulin stain; right middle panels) and splenic fibrosis (reticulin; right panels)). Scale bar, 50 μm. (F) Representative images of BM from the femurs of WT, JAK2V617F, and JAK2V617F/Hmga1+/− mice (H&E stain). Scale bars, 250 μm. Data in (A-D) are mean ± standard deviation. *P < .05, **P < .01, ***P < .001, 1-way ANOVA, followed by Tukey’s multiple-comparison test (A [right panel]), Kruskal-Wallis test, followed by Dunn’s multiple-comparison test (A [left panel], B), Mann-Whitney U test (C), 2-tailed Student t test (D). ns, not significant.
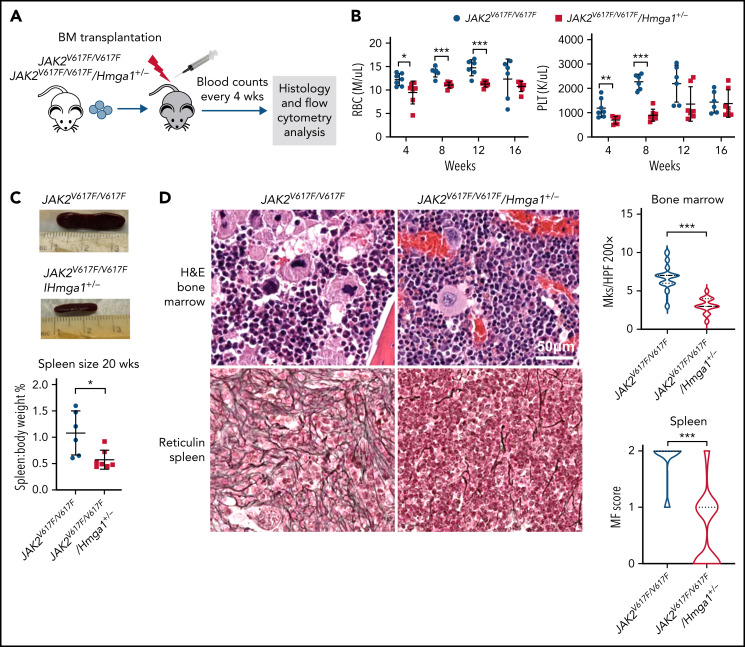
To determine whether these effects depend on Hmga1 within the hematopoietic compartment, we transplanted BM from mice biallelic for the JAK2V617F transgene (26 copies; denoted JAK2V617F/V617F) with Hmga1 heterozygosity or both alleles intact into lethally irradiated recipients. As before, Hmga1 deficiency decreased erythrocytosis, thrombocytosis, megakaryocyte hyperplasia, splenomegaly, and fibrosis (spleen, BM) (Figure 3A-D), demonstrating that Hmga1 haploinsufficiency within hematopoietic cells is responsible for abrogating MF.
Figure 3.
Hmga1 deficiency prevents MPN phenotypes and expansion of long-term HSC and myeloid progenitors from JAKV617F/V617F mice in a transplantation model. (A) Experimental design to determine Hmga1 function in transplantation model. (B) Red blood cell (RBC) and platelet (PLT) counts from PB of age-matched recipients transplanted with JAK2V617F/V617F or JAK2V617F/V617F/Hmga1+/− BM cells (n = 6 or 7 per group). (C) Representative spleens and relative spleen size (mean ± standard deviation [SD]) in recipient mice transplanted with JAK2V617F/V617F or JAK2V617F/V617F/Hmga1+/− BM cells. (D) Representative BM (humerus; hematoxylin and eosin [H&E] stain) and spleen fibrosis (reticulin staining). Scale bar, 50 μm (left and middle panels). Megakaryocyte numbers per high-power field (Mks/HPF) in BM (humerus; mean ± SD) and splenic fibrosis scores (mean ± SD) from recipient mice transplanted with JAK2V617F/V617F or JAK2V617F/V617F/Hmga1+/− BM cells (n = 6 or 7 per group). (E) Representative flow cytometry plots of BM HSPC. Flow cytometric analysis (mean ± SD) assessed in BM or spleen from recipient mice transplanted with JAK2V617F/V617F or JAK2V617F/V617F/Hmga1+/− BM cells (n = 6 or 7 per group). (F) t-SNE plot of LSK transcriptomes from scRNAseq colored by clusters. The 2 genotypes (JAK2V617F/V617F and JAK2V617F/V617F/Hmga1+/−) are superimposed (left panel). t-SNE plot from JAK2V617F/V617F (middle panel) and JAK2V617F/V617F/Hmga1+/− (right panel) are shown separately to highlight the variation in distribution among the clusters. Hmga1 heterozygous deficiency decreases clusters with markers of HSC (cluster 7), megakaryocyte-biased progenitors (cluster 8), and megakaryocyte/erythroid-biased progenitors (clusters 5-6), while increasing clusters with lymphoid-biased progenitors (clusters 0 and 1). The clusters with the greatest differences across genotype are outlined. The table shows the fraction of LSK cells in clusters grouped by genotype (JAK2V617F/V617F vs JAK2V617F/V617F/Hmga1+/−); P values show differences between genotypes in clusters grouped by cell identity. *P < .05, **P < .01, ***P < .001, Mann–Whitney U test (B-C,E), 2-tailed Student t test (D).
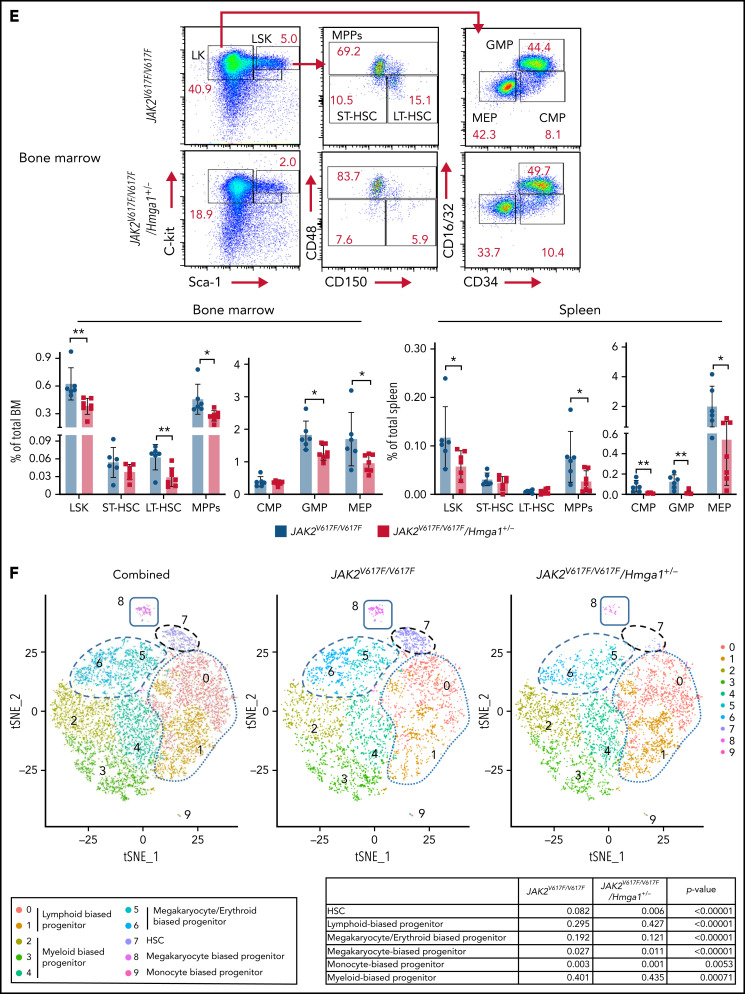
Hmga1 haploinsufficiency dampens expansion of JAKV617F/V617F HSCs and progenitors
To determine how Hmga1 prevents MF, we assessed the frequency and function of hematopoietic stem cells (HSCs) and hematopoietic stem and progenitor cells (HSPCs). Long-term HSCs, LSK cells, and myeloid progenitors, including multipotent progenitors, granulocyte-monocyte progenitors (GMPs), and megakaryocyte-erythrocyte progenitors (MEPs) all decrease in BM from JAKV617F/V617F transplants with Hmga1 haploinsufficiency. LSK cells, multipotent progenitors, common myeloid progenitors, GMPs, and MEPs decrease in spleen (Figure 3E), although there was no difference in common lymphoid progenitors (CLPs) in marrow or spleen (supplemental Figure 4). Hmga1 heterozygosity also dampens the clonogenic potential of JAK2V617F/V617F BM and spleen cells, decreasing total colony-forming units, granulocyte-monocyte colony-forming units, and burst-forming unit-erythroid (supplemental Figure 5). These data demonstrate that Hmga1 haploinsufficiency within JAKV617F/V617F HSCs dampens clonogenicity and expansion in HSCs and distinct progenitors.
To further characterize HSPCs regulated by Hmga1, we compared scRNAseq in BM-derived LSK cells from JAK2V617F/V617F mice and JAK2V617F/JAKV617F mice with Hmga1 heterozygous deficiency. Cell identify was assigned to clusters using published results.72,80-83 Similar to our flow cytometry results, the cluster(s) enriched for markers of HSCs (cluster 7), megakaryocyte-biased progenitors (cluster 8), and megakaryocyte/erythroid-biased progenitors (clusters 5-6) all decreased in JAK2V617F mice with Hmga1 heterozygous deficiency, whereas those with lymphoid-biased progenitor markers (clusters 0-1) increased (Figure 3F). These findings parallel our flow cytometry results, demonstrating that Hmga1 deficiency mitigates expansion in HSCs and distinct progenitors involved in MPN.
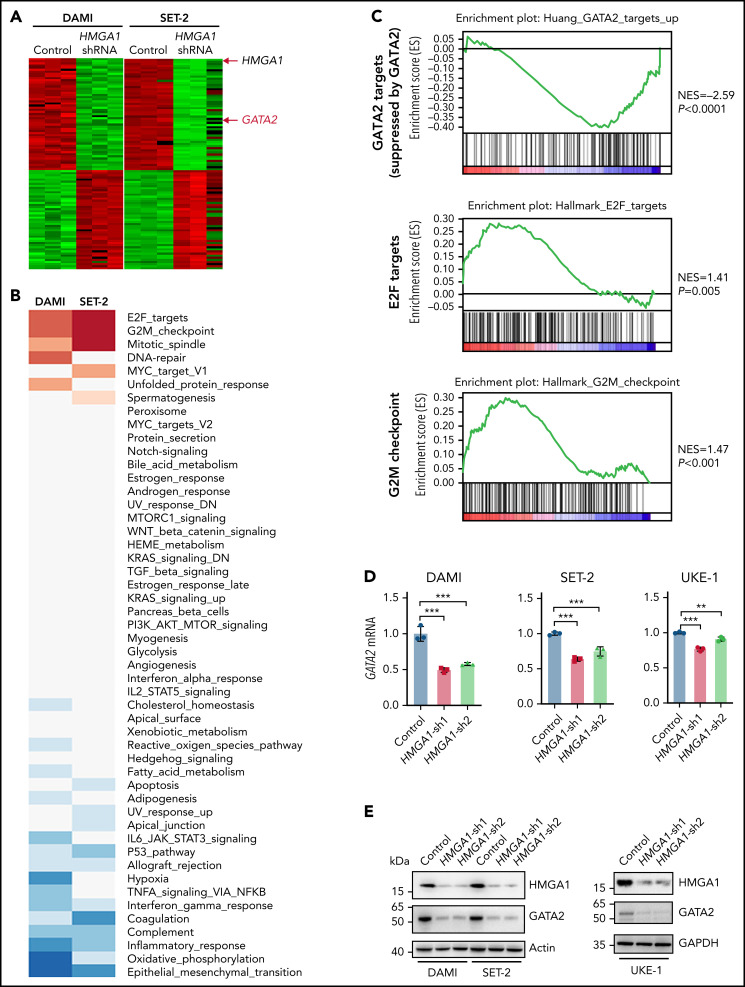
HMGA1 activates transcriptional networks involved in proliferation and cell fate
To further elucidate the molecular underpinnings of HMGA1, we performed RNAseq in DAMI and SET-2 cells and ChIPseq/ATACseq in DAMI cells. GSEA from RNAseq revealed an HMGA1 signature of genes involved in cell cycle progression (E2F targets, G2M checkpoint, mitotic spindle, MYC targets) and cell fate decisions (GATA2 transcriptional networks; Figure 4A-C). Ingenuity Pathway Analysis showed similar networks, in addition to those governing cell-cell signaling, inflammation, and fibrosis. To determine which genes could be direct targets of HMGA1, we integrated RNAseq with ChIPseq to detect differentially regulated genes with HMGA1 occupancy in potential gene-regulatory regions, which identified E2F targets, mitotic spindle, G2M checkpoint, and GATA2 networks (supplemental Table 1). ATACseq showed differentially enhanced chromatin accessibility in DAMI control cells compared with cells with HMGA1 depletion in promoters for genes regulating cell growth and signal transduction. Integrating RNAseq/ATACseq (by Enrichr; supplemental Table 2) revealed enrichment for GATA genes, KRAS signaling, and active histone marks H3 lysine 4 monomethylation (H3K4me1) or H3 lysine 4 trimethylation (H3K4me3). We focused on GATA2, given its robust regulation by HMGA1 in JAK2V617F AML cells, role in HSC fate, and association with poor outcomes in myeloid malignancies.84-87 HMGA1-dependent expression of GATA2 was validated (messenger RNA, protein) in DAMI, SET-2, and UKE-1 cells with HMGA1 deficiency via HMGA1 shRNA or CRISPR/Cas9 (Figure 4D-E; supplemental Figure 6A-B). Conversely, HMGA1 overexpression via CRISPR activation (HMGA1-CRISPRa) upregulates GATA2 (supplemental Figure 6C).
Figure 4.
HMGA1 transcriptional networks are involved in cell fate and cell cycle progression. (A) Heat map showssubsets of differentially expressed genes that are upregulated or downregulated by HMGA1 in DAMI and SET-2 JAK2V617F AML cell lines. (B) HMGA1 transcriptional networks are enriched for gene sets involved in cell cycle progression (E2F targets, mitotic spindle, G2M checkpoint, MYC targets) and cell fate decisions (GATA2 networks and GATA2). The left column was derived from DAMI and the right column from SET-2 . (C) GSEA performed from transcriptomes from DAMI and SET-2 , with or without HMGA1 silencing (control vs HMGA1-sh1). Adjusted P values and normalized enrichment scores (NES) are shown. (D) Relative GATA2 expression (mean ± standard deviation [SD]) assessed from 2 independent experiments performed in triplicate (quantitative polymerase chain reaction) in DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2). GAPDH was used to control for loading. (E) Western blots for HMGA1, GATA2, and β-actin (loading control) protein levels from DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2). Western blots were performed 3 times with similar results; a representative blot is shown. Size markers (kDa) are indicated. (F) Integrative Genomics Viewer browser view of HMGA1 ChIPseq (top, red), H3 ChIPseq (middle, blue), and overlay (bottom) across the GATA2 locus from DAMI WT cells. (G) Schematic representation of the human GATA2 region with 6 regions (red) that include in silico–predicted HMGA1 DNA binding motifs (upper part of panel). GATA2-1S and GATA2-1G promoters are shown with black arrows to indicate the transcriptional start sites (TSS). The black box represents the untranslated region, and the orange boxes are coding exons. Numbers indicate the nucleotide positions relative to the GATA2-IS TSS. Schematic representation of region with 4 putative HMGA1 binding motifs within a 230-bp fragment of the GATA2 +9.5 enhancer area (lower part of panel). The 4 predicted HMGA1 binding motifs (A-D) are marked with red arrowheads. The +9.5 enhancer (yellow) with 3 DNA binding motifs (E-box, green; GATA, pink; and erythroblast transformation specific [ETS], gray) are also shown. (H) HMGA1 enrichment at the +9.5 enhancer and +9.7 regions within the GATA2 locus by ChIP-PCR in DAMI cells, with or without HMGA1 silencing, performed in triplicate from 3 independent experiments. Results (mean ± SD) are the percentage recovered from the total input DNA (% input). GAPDH promoter (left lane) was used as a negative control for HMGA1 occupancy. (I, left) HMGA1 ChIP-PCR assays comparing occupancy at +9, +9.5, and +9.7 regions using DAMI cells, with or without HMGA1 silencing (control vs HMGA1-sh1). Results (mean ± SD) are presented as the percentage recovered from the total input DNA (% input) performed in triplicate in 3 independent experiments. (I, center and right) HMGA1 recruits active histone marks at +9, +9.5, and +9.7 regions with enrichment for H3K4me1 (Middle) and H3K4me3 (Right), by ChIP-PCR in control DAMI cells with abundant HMGA1; active marks are depleted with HMGA1 silencing (control vs HMGA1-sh1). ChIP-PCR was performed in triplicate in 3 independent experiments. (J) HMGA1 DNA binding activity to probe sequences from 4 putative binding sites near the +9.5 enhancer by electrophoretic mobility shift assay. HMGA1-DNA complexes from 3 independent experiments (mean ± SD) were compared quantitatively in the bar graph. A GC-rich probe was used as a negative control. (K) HMGA1 induces GATA2 enhancer sequences linked to a luciferase reporter gene in control DAMI cells, with decreased reporter gene activation with HMGA1 silencing (control vs HMGA1-sh1 or HMGA1-sh2). Constructs include GATA2-1S promoter, GATA2-1S promoter plus HMGA1 binding motif A, and GATA2-1S promoter plus HMGA1 binding motifs A and B. Results (mean ± SD) represent 2 experiments performed with 4 replicates. *P < .05, **P < .01,***P < .001, ****P < .0001, 2-tailed Student t test (D,I), 1-way ANOVA, followed by Tukey’s multiple-comparison test (H,J-K).
HMGA1 and GATA2 are coexpressed in HSPCs
Next, we determined whether HMGA1 and GATA2 are coexpressed in wild-type (WT) or JAK2V617F-mutant HSPCs. In unaffected human and murine HSPCs, HMGA1/Hmga1 and GATA2/Gata2 are positively correlated (supplemental Figure 6D-G). In JAK2V617F murine HSPCs, Hmga1 and Gata2 are coexpressed and positively correlated, but only in LSK cells and MEPs (no correlation in common myeloid progenitors or GMPs; supplemental Figure 6H-I). Notably, LSK cell and MEP populations constitute MPN progenitors in JAK2V617F models.88 These findings demonstrate coexpression of HMGA1 and GATA2 in HSPCs and MPN progenitors in JAK2V617F mice.
HMGA1 induces GATA2 by binding to the developmental enhancer, increasing chromatin accessibility, and recruiting active histone marks
To determine whether HMGA1 directly activates GATA2, we identified 42 putative DNA binding sites throughout GATA2 regulatory regions using in silico algorithms, including 6 regions with ≥2 sites within 500 bp. HMGA1 chromatin occupancy at these 6 regions by ChIP-PCR and ChIPseq show the greatest enrichment around an established +9.5 GATA2 enhancer (Figure 4F-H) that is critical for HSC and MEP development during embryonic hematopoiesis.84-86 Further, HMGA1 occupancy (ChIP-PCR) was depleted by HMGA1 silencing (Figure 4F-I). This +9.5 enhancer partially overlaps with a 224-bp sequence with 4 predicted HMGA1 binding sites (A, B, C, D). ChIP-PCR, used to compare occupancy around these sites, showed the greatest enrichment at sites A and B; recombinant HMGA1 binding by gel shift analysis was also most robust with probes within site A or B (Figure 4H-J; supplemental Figure 7A-E). Because HMGA1 induces GATA2 and associates with regions with active histone marks by ATACseq (H3K4me1, H3K4me3), we compared these marks by ChIP-PCR, which revealed enrichment at the +9.5 enhancer; both decreased upon HMGA1 depletion (Figure 4H-I). Conversely, there was no change in H3K27Ac or control histone H3 binding, suggesting that HMGA1 recruits H3K4me1/H3K4me3 in JAK2V617F AML DAMI cells (supplemental Figure 7F-G).
To determine whether HMGA1 transactivates the GATA2 developmental enhancer, we assessed luciferase reporter gene activation of the +9.5 enhancer region upstream of the GATA2 minimal promoter (GATA2-1S). GATA2-1S showed low activity, which remained unchanged by HMGA1 silencing, whereas reporter activity increased more than three-fold when the +9.5 enhancer site A was present and more than four-fold when sites A and B were included; accordingly, +9.5 reporter activity decreased upon HMGA1 silencing (Figure 4K). Together, these results indicate that HMGA1 binds directly to sites near the GATA2 +9.5 enhancer, increasing chromatin accessibility and recruiting active histone marks (H3K4me1/H3K4me3) to induce GATA2.
GATA2 silencing phenocopies HMGA1 deficiency, and GATA2 restoration partially rescues antileukemogenic effects of HMGA1 depletion
To determine whether GATA2 is required for HMGA1 function, we depleted GATA2 in JAK2V617F AML cell lines (DAMI, SET-2, and UKE-1) via shRNA targeting of 2 different sequences. Silencing GATA2 decreases proliferation, clonogenicity, and the frequency of cells in S phase while increasing apoptosis, recapitulating phenotypes observed with HMGA1 depletion (Figure 5A-F; supplemental Figure 8). GATA2 deficiency also disrupts the leukemogenic potential of DAMI cells, decreasing splenomegaly and leukemic engraftment (BM, spleen); moreover, survival was prolonged in recipients of DAMI cells with GATA2 silencing (Figure 5G-I). Similar to our results with HMGA1, engrafted leukemic cells from the pool of cells with GATA2 silencing express higher GATA2 compared with the injected cells, suggesting that a critical level of GATA2 is required for engraftment (supplemental Figure 9). Collectively, our results indicate that GATA2 is an important mediator of HMGA1 in these JAK2V617F AML models.
Figure 5.
GATA2 silencing phenocopies HMGA1 silencing in preclinical models of JAK2V617F MPN AML. (A) Relative GATA2 expression (mean ± standard deviation [SD]) from 2 experiments performed in triplicate (quantitative polymerase chain reaction) in DAMI, SET-2, and UKE-1 cells, with or without HMGA1 silencing (control vs GATA2-sh1 or GATA2-sh2). GAPDH was used as a loading control. (B) Western blots of GATA2, β-actin, and GAPDH (loading control) protein levels from DAMI, SET-2, and UKE-1 cells, with or without GATA2 silencing (control vs GATA2-sh1 or GATA2-sh2). Western blots were performed 3 times with similar results; a representative blot is shown. Size markers (kDa) are indicated. (C) Proliferation (mean ± SD) by MTS [3-(4,5-dimethylthiazol-2-yl)-5-(3-carboxymethoxyphenyl)-2-(4-sulfophenyl)-2H-tetrazolium; Promega)] assay in DAMI, SET-2 and UKE-1 cells, with or without GATA2 silencing (control vs GATA2-sh1 or GATA2-sh2), at the indicated time points. (D) Colony-forming units (CFU; mean ± SD) in DAMI, SET-2, and UKE-1 cells, with or without GATA2 silencing (control vs GATA2-sh1 or GATA2-sh2), in 2 experiments performed in triplicate. Representative images of colony formation after silencing GATA2 by delivery of a lentiviral vector expressing shRNA targeting GATA2 (control vs GATA2-sh1 or GATA2-sh2) are shown. Scale bars, 200 μm. (E) Edu (5-ethynyl-2′-deoxyuridine) cell cycle (mean ± SD) by flow cytometry assessed in DAMI, SET-2, and UKE-1 cells, with or without GATA2 silencing (control vs GATA2-sh1 or GATA2-sh2), in 2 experiments performed in triplicate. (F) Annexin V apoptosis by flow cytometry assessed in DAMI, SET-2, and UKE-1 cells, with or without GATA2 silencing (control vs GATA2-sh1 or GATA2-sh2) in 2 experiments. (G) Representative images of spleens and relative spleen size (mean ± SD); leukemia cell engraftment (mean ± SD) assessed by flow cytometry in spleen from NSG mice injected with DAMI cells with or without GATA2 silencing (control vs GATA2-sh1; n = 4 per group). (H) Leukemia cell engraftment assessed by flow cytometry (mean ± SD) in BM from NSG mice injected with DAMI cells, with or without GATA2 silencing (control vs GATA2-sh1; n = 4 per group). Representative flow cytometry plots from each group and hematoxylin and eosin–stained BM are shown. Scale bar, 200 μm. (I) Survival analysis by Kaplan-Meier estimate assessed in NSG mice injected with DAMI cells transduced with lentivirus (control: median survival, 24 days vs GATA2-sh1: median survival, 38.5 days; n = 6 per group). *P < .05, **P < .01, ***P < .001, ***P <.001, 2-tailed Student t test (A,C-H), log-rank (Mantel-Cox) test (I).
To determine whether restoring GATA2 rescues anti-leukemogenic phenotypes mediated by HMGA1 silencing, we engineered DAMI, SET-2, and UKE-1 cells with HMGA1 silencing and concurrent expression of GATA2, such that GATA2 levels (messenger RNA, protein) approximate those of parental cells. GATA2 partially rescues phenotypes associated with HMGA1 depletion, increasing, but not restoring, clonogenicity in JAK2V617F AML cell lines (Figure 6A-C; supplemental Figure 10A). GATA2 rescues the frequency of apoptotic cells to baseline levels, although proliferation and cell cycle progression were unchanged (Figure 6D; supplemental 10B-C). GATA2 restoration also partially rescues the antileukemogenic effects of HMGA1 silencing (Figure 6E-F). As before, disease latency was shortest in recipients of DAMI cells with endogenous expression of HMGA1 and GATA2 (median survival, 24 days) and was longest in recipients of cells with HMGA1 depletion (median survival, 38 days). The recipients of leukemic cells with HMGA1 silencing and GATA2 overexpression had intermediate survival (32.5 days; P < .01). GATA2 restoration increases the frequency of BM-engrafted DAMI cells more than two-fold compared with those with HMGA1 depletion, although splenic engraftment was unchanged (Figure 6F; supplemental Figure 10D). These results demonstrate that GATA2 partially mediates HMGA1 function in models of JAK2V617F AML.
Figure 6.
GATA2 restoration partially rescues antileukemogenic effects of HMGA1 silencing; GATA2 and HMGA1 are coexpressed in primary MPN and HMGA1 networks and are activated in leukemic blasts from patients with MPN. (A) Relative HMGA1 and GATA2 expression (mean ± standard deviation [SD]) from 2 experiments performed in triplicate (quantitative polymerase chain reaction) in DAMI, SET-2, and UKE-1 cells (control vs HMGA1-sh1 vs HMGA1-sh1 + GATA2 overexpression [OE]). GAPDH was used to control for loading. (B) Western blots of HMGA1, GATA2, β-actin, and GAPDH (loading control) protein levels from DAMI, SET-2, and UKE-1 cells transduced with lentivirus (control vs HMGA1-sh1 vs HMGA1-sh1 + GATA2 OE). Western blots were performed 3 times with similar results; a representative blot is shown. Size markers (kDa) are indicated. (C) Colony-forming units (CFU; mean ± SD) from DAMI, SET-2, and UKE-1 cells (control vs HMGA1-sh1 vs HMGA1-sh1 + GATA2 OE) in 2 experiments. Representative images of colonies are shown. Scale bars, 200 μm. (D) Annexin V apoptosis by flow cytometry in DAMI, SET-2, and UKE-1 cells (control vs HMGA1-sh1 vs HMGA1-sh1 + GATA2 OE) in 2 experiments. (E) Survival curve (Kaplan-Meier plots) in NSG mice injected with DAMI cells (control vs HMGA1-sh1 vs HMGA1-sh1 + GATA2 OE; n = 6). (F) Leukemia cell engraftment assessed by flow cytometry (mean ± SD) in BM from NSG mice injected with DAMI cells transduced with lentivirus (control vs HMGA1-sh1 vs HMGA1-sh1 + GATA2 OE; n = 4 per group). Representative BM histology (hematoxylin and eosin stain) from each group are shown. Scale bar, 200 μm. (Gi) HMGA1 and GATA2 expression (RNAseq) from PBMCs from a cohort of matched patient samples with MF that progressed to AML (n = 11 per group). (Gii) HMGA1 and GATA2 are positively correlated (P < .001); Pearson correlation coefficient. (Giii) HMGA1 and GATA2 are positively correlated (P < .01) in JAK2-mutant CD34+ BM cells from patients with ET or PV and unaffected individuals (GSE103237); Pearson correlation coefficient. (Giv) HMGA1 and GATA2 in JAK2-mutant CD34+ PB cells from patients with MF compared with unmutated CD34+ cells from the same patients (n = 8) or unaffected individuals (n = 2) by scRNAseq (GSE122198). Each dot represents the expression value for each single cell (P < .0010); Pearson correlation coefficient. (H) Transcriptional networks activated in MPN PBMCs after leukemic transformation correlate positively with HMGA1 expression levels (P < .05; Spearman correlation > 0.6) and overlap with the top HMGA1 networks (red) identified in JAKV617F MPN cell lines (DAMI, SET-2). *P < .05, **P < .01, ***P <. 001; 1-way ANOVA, followed by Tukey’s multiple-comparison test (A-D,F), log-rank (Mantel-Cox) test, followed by Bonferroni correction (E).
HMGA1 networks are activated with leukemic transformation in human MPN
To determine the significance of the HMGA1-GATA2 network in human MPN progression, we compared the expression of HMGA1 and GATA2 in primary human MPN. Strikingly, GATA2 and HMGA1 are coexpressed and positively correlated via RNAseq from PBMCs from a cohort of matched patients with MF that transformed to AML (n = 11) (Figure 6Gi-ii).26 Further, this relationship was validated in independent studies (Figure 6Giii-iv; supplemental Figure 11): (1) HMGA1 and GATA2 are coexpressed and upregulated in BM CD34+ cells with progression from PV or ET to MF (GSE103237),79 (2) HMGA1 and GATA2 are upregulated in PB CD34+ cells from MF compared with age-matched healthy controls by scRNAseq (GSE144568),71 and, (3) in another scRNAseq cohort with greater sequencing depth, HMGA1 and GATA2 are coexpressed and upregulated in JAK2-mutated PB CD34+ cells from MF compared with unmutated CD34+ cells from the same patients or CD34+ cells from unaffected individuals (GSE122198).70
Next, we identified the pathways that are activated in human MPN. In the matched cohort of MF to AML, most leukemic samples show activation of pathways distinct from those in MF, and there was a striking overlap with pathways activated in leukemia and HMGA1 networks identified in our cell-based models. Specifically, networks driving cell cycle progression pathways are activated after transformation to AML, including the most significant HMGA1 pathways (G2M, mitotic spindle, E2F; Figure 6H). Pathways repressed in the leukemic samples overlap with those repressed by HMGA in JAK2V617F AML cell-based models, including interferon-γ (data not shown). Furthermore, HMGA1 transcript levels correlate with HMGA1 pathway activation in the primary MPN AML cells (Figure 6H). Similarly, the scRNAseq cohorts show activation of HMGA1 networks (E2F targets, G2M checkpoint, DNA repair), including GATA2 with progression to MF.70,71 Together, these results implicate HMGA1 as a driver of transcriptional networks required in human MPN progression.
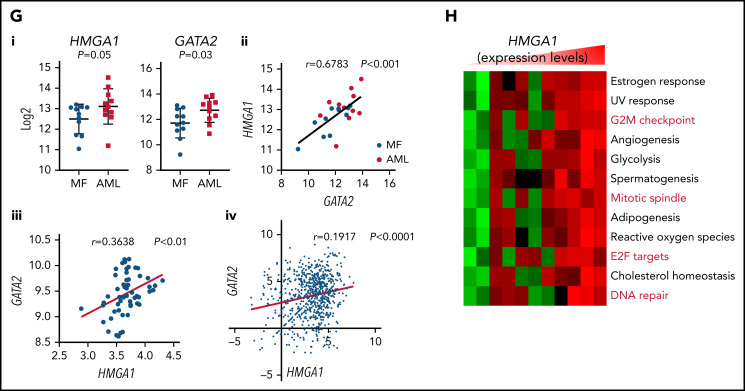
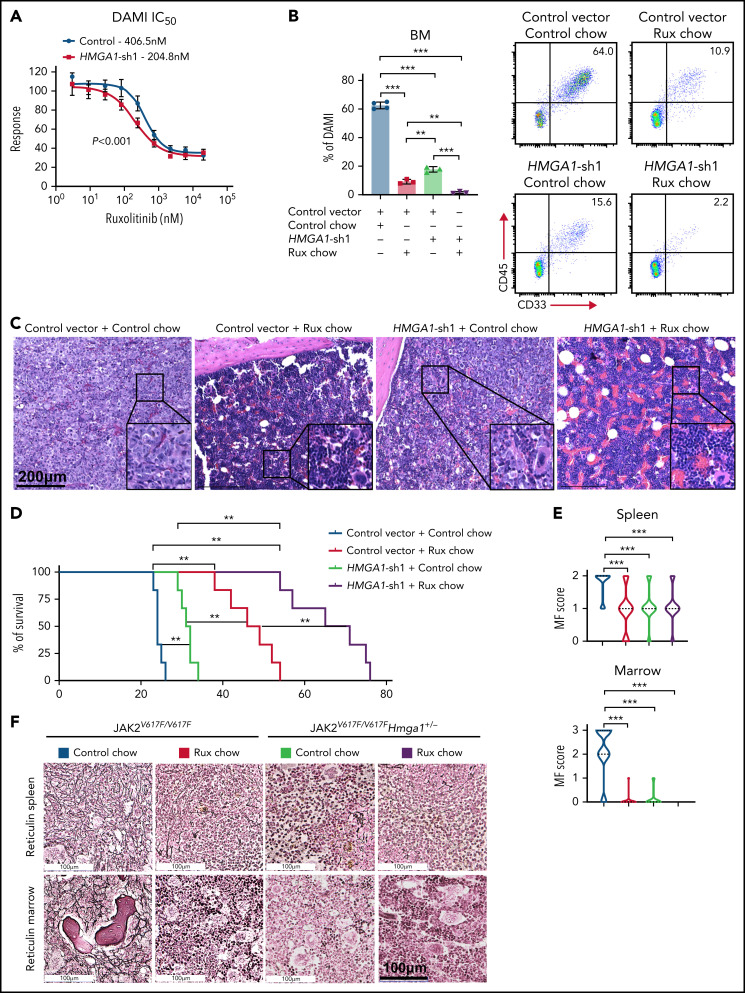
HMGA1 depletion enhances responses to the JAK/STAT inhibitor ruxolitinib
Next, we determined whether HMGA1 deficiency enhances sensitivity to the JAK/STAT inhibitor ruxolitinib in JAK2V617F AML. First, we found that the concentration at which 50% of DAMI cells stop proliferating with ruxolitinib treatment decreases upon HMGA1 depletion (406.5 nM vs 204.8 nM; P < .001) (Figure 7A). Second, we tested the effects of ruxolitinib with HMGA1 silencing on leukemogenesis in vivo. Therapy was delivered via chow supplemented with ruxolitinib (2000 mg INCB01842 per kilogram diet) to provide doses shown to reach therapeutic levels in mice89,90; control chow was identical except it lacked ruxolitinib. We included 4 groups: (1) DAMI control, control chow, (2) DAMI control, ruxolitinib chow, (3) DAMI with HMGA1 depletion, control chow, and (4) DAMI with HMGA1 depletion, ruxolitinib chow. After 24 days of therapy, we assessed leukemic engraftment. Mice injected with control DAMI cells and placed on control chow had the highest leukemic burdens in spleen and BM, whereas recipients of DAMI cells with HMGA1 silencing and ruxolitinib treatment showed the lowest engraftment and spleen sizes, followed by recipients of DAMI cells with HMGA1 silencing and control chow (Figure 7B-C; supplemental Figure 12). Moreover, survival is prolonged in recipients of AML cells with HMGA1 silencing and ruxolitinib therapy (Figure 7D).
Figure 7.
HMGA1 silencing enhances responses to the JAK/STAT inhibitor ruxolitinib (Rux), delaying leukemia engraftment and prolonging survival. (A) Dose response curve with 50% inhibitory concentration in DAMI cells, with or without HMGA1 silencing. (B) Leukemia cell engraftment by flow cytometry (mean ± standard deviation [SD]) in BM from NSG mice injected with DAMI cells, including DAMI controls with control chow, DAMI controls with Rux chow, DAMI cells with HMGA1 silencing and control chow, and DAMI cells with HMGA1 silencing and Rux chow (n = 3 or 4 per group). Representative flow cytometry plots from each group are shown. (C) BM (hematoxylin and eosin stain) from each group described above. Scale bar, 200 μm. (D) Survival curves (Kaplan-Meier plots) of NSG mice injected with DAMI cells and treated as follows: DAMI controls with control chow (median survival, 24 days), DAMI controls with Rux chow (median survival, 47.5 days), DAMI cells with HMGA1 silencing and control chow (median survival, 31.5 days), and DAMI cells with HMGA1 silencing and Rux chow (median survival 68 days; n = 6 per group). (E) MF scores based on reticulin staining (mean ± SD) in spleen (scale 0-2) and BM (scale 0-3) from JAK2V617F/V617F mice with control chow or rux chow and JAK2V617F/V617F/Hmga1+/− mice with control chow or rux chow mice were assessed. (F) Representative images of spleen (upper panels) and BM (lower panels) from femurs of JAK2V617F/V617F mice with control or rux chow and JAK2V617F/V617F/Hmga1+/− mice with control or rux chow (reticulin stain). Scale bar, 100 μm. *P < .01, **P < .01, ***P < .001, 1-way ANOVA, followed by Tukey’s multiple-comparison test (B,E), log-rank (Mantel-Cox) test, followed by Bonferroni correction (D), 2-way ANOVA (F).
We also tested ruxolitinib in the JAKV617F/V617F chronic MPN model with therapy beginning at 16 to 20 weeks of age when erythrocytosis and splenomegaly are well established (supplemental Figure 13A). Ruxolitinib decreased splenomegaly and fibrosis in JAKV617F/V617F mice (Figure 7E-F). In the JAKV617F/V617F model, Hmga1 heterozygosity decreases splenomegaly and prevents fibrosis (supplemental Figure 13B). Spleen sizes decrease further with ruxolitinib in JAKV617F/V617F mice with Hmga1 heterozygosity (supplemental Figure 13). There were decreases in leukocytosis with modest changes in erythrocytosis in both models (supplemental Figure 13A). Together, these results indicate that HMGA1 silencing or Hmga1 haploinsufficiency enhances sensitivity to ruxolitinib in preclinical MPN models and strongly support HMGA1 as a rational therapeutic target.
Discussion
We discovered a novel role for HMGA1 as an epigenetic switch involved in JAK2V617F MPN progression. Using shRNA-mediated or CRISPR/Cas9-mediated gene silencing in JAK2V617F models, we found that HMGA1 deficiency: 1) decreases proliferation, clonogenicity, and leukemic engraftment; 2) represses transcriptional networks involved in cell cycle progression, proliferation, and GATA2 function; and, 3) most importantly, enhances sensitivity to the JAK inhibitor ruxolitinib in disrupting leukemic engraftment and prolonging survival. We validated the significance of HMGA1 in human MPN because HMGA1 and downstream pathways, including GATA2, are upregulated during progression in independent cohorts. Moreover, HMGA1 transcriptional pathways are activated in JAK2V617F CD34+ cells compared with those lacking mutant JAK, and in matched MF samples after transformation to leukemia, further illuminating HMGA1 as a promising therapeutic target. The enhanced response to ruxolitinib by HMGA1 depletion is particularly striking in AML because ruxolitinib is not effective in patients with MPN after leukemic transformation.
Surprisingly, Hmga1 haploinsufficiency prevents MF in chronic MPN models, reducing erythrocytosis, megakaryocyte hyperplasia, splenomegaly, and fibrosis, while dampening expansion of JAK2V617F mutant stem and progenitor cells. This was unexpected for 2 reasons; first, although HMGA1 is a potent oncogene and driver of progression in aggressive solid tumor modes, its role in clonal hematopoiesis and more indolent neoplasia had not been demonstrated. Second, most studies focusing on HMGA1 in tumor cells rely on gene silencing to low levels. Thus, we did not anticipate that reducing levels by only 50% would so profoundly impact progression. Moreover, the normal steady-state hematopoiesis in Hmga1 heterozygous mice suggests that pharmacologic modulation of HMGA1 to this degree is a plausible therapeutic end point, although specific inhibitors of HMGA1 are not yet available.
To uncover actionable mechanisms mediated by HMGA1, we investigated downstream transcriptomic and epigenetic changes, which identified HMGA1-dependent transcriptional networks governing cell cycle progression and cell fate, including E2F and GATA2 targets. Intriguingly, a recent study using mutant MPLW515L murine models identified E2F networks in MPN progression that were targeted by inhibiting PRMT5, a protein arginine methyltransferase,25 although it remains to be shown whether similar approaches disrupt HMGA1 networks. Instead, we focused on the GATA2 master regulator, given its association with HSC function and poor outcomes in AML.84-87
HMGA1 aberrantly induces GATA2 in human JAKV617F AML cell lines and murine models. Moreover, this pathway is activated in human MPN progression. HMGA1-mediated induction of GATA2 could preclude normal GATA1 function in HSPCs and megakaryocytes, thereby mimicking the GATA1-low phenotype that causes MF in mice.91-93 Low GATA1 protein levels were observed in megakaryocytes from patients with MF.92,93 We did not test the effects of Gata2 loss in our JAKV617F mice because Gata2 deficiency disrupts hematopoiesis. Modulating HMGA1 provides a more attractive therapeutic approach. Notably, repressing GATA2 recapitulates many phenotypes observed with HMGA1 silencing, and restoring GATA2 only partially rescues anti-leukemic effects of HMGA1 depletion, demonstrating that GATA2 is only one HMGA1 effector in MPN. Indeed, RNAseq, ChIPseq and ATACseq revealed other networks that are involved in proliferation; thus, pharmacologically targeting these pathways may be beneficial.
The role of HMGA1 in orchestrating the assembly of specific histone marks had not been studied in detail. We found that HMGA1 enhances chromatin accessibility and recruits histone marks associated with gene activation, including H3K3me3 (for active promoters) and H3K4me1 (active enhancers). Previous studies focused on HMGA1 occupancy upstream of minimal promoters,28,29 although we discovered HMGA1 occupancy at the GATA2 +9.5 distal enhancer, suggesting that HMGA1 activates or “rewires” enhancer function when overexpressed during MPN progression.
In JAK2V617F mice, Hmga1 haploinsufficiency mitigates expansion of HSCs, specific myeloid progenitors (MEPs, GMPs), and megakaryocytes, without affecting CLPs. scRNAseq corroborated these results, indicating that Hmga1 haploinsufficiency decreased clusters with HS and megakaryocyte/erythroid-biased markers while expanding those with lymphoid-biased markers. HSCs and MEPs represent key progenitors in diverse MPN models of MF, including mice expressing JAK2V617F or mutant thrombopoietin receptor MPLW515L.23,94 HMGA1 is also a master regulator in other adult stem cell populations, including intestinal stem cells,28,33 which rely on many transcription factors that are active in HSCs. Further, intestinal epithelium and hematopoiesis require highly regenerative stem cell pools to replace mature progeny, and HMGA1 is re-expressed in hematologic and intestinal malignancies where it amplifies stem-like networks.28,33,54 These data suggest that tightly regulated HMGA1 is critical for stem cell function under homeostatic conditions, whereas mutated genomes, together with HMGA1 overexpression, foster aberrant proliferation, differentiation, and transformation.
Intriguingly, HMGA1 was upregulated in early-stage MPN with JAK2 mutations, but not in CALR-mutated early-stage disease. In our Johns Hopkins University cohort, CD34+ AML blasts with the highest HMGA1 expression also harbor mutant EZH2 and ASXL1, suggesting that other clonal hematopoiesis lesions may induce HMGA1. Given the prevalence of clonal hematopoiesis with aging, further studies to investigate HMGA1 in this setting are warranted. Although HMGA2 has been studied in myeloid malignancy and clonal hematopoiesis,95-98 RNAseq revealed barely detectable HMGA2 transcripts in human DAMI and SET-2 cell lines and very low levels in most primary human MPN samples. Moreover, Hmga2 deficiency did not impact progression in the JAK2V617F model when crossed to mice with homozygous or heterozygous deficiency of Hmga2. Together, our studies implicate HMGA1, rather than HMGA2, as a primary driver of JAK2V617F MPN progression.
In summary, we report a novel role for HMGA1 in JAK2V617F AML and MPN progression using diverse models and orthogonal approaches. Mechanistically, HMGA1 induces transcriptional networks that are involved in cell cycle progression and aberrant differentiation, the latter of which includes direct transactivation of GATA2. Together, our findings reveal HMGA1 as a new therapeutic target in MPN and open the door to novel therapeutic approaches to prevent disease progression. Because HMGA1 and GATA2 are also overexpressed in de novo AML, this pathway may be relevant, more broadly, in myeloid malignancies.
Supplementary Material
The online version of this article contains a data supplement.
Acknowledgments
The authors thank the Mutation Generation and Detection Core at the University of Utah (National Institute of Diabetes and Digestive and Kidney Diseases Cooperative Hematology Specialized Core Center Grant U54DK110858), the Yale Cooperative Centers of Excellence in Hematology (National Institute of Diabetes and Digestive and Kidney Diseases Grant U54DK106857), and the Johns Hopkins University Ross Flow Core (National Institutes of Health Shared Instrument Grants S10OD026859 for Cytek Aurora Full Spectrum Flow Cytometric Analyzer).
This work was supported by National Institutes of Health National Heart, Lung, and Blood Institute grants R01HL145780 (L.M.S.R., A.R.M.) and R01HL143818 (L.M.S.R.), National Institutes of Health National Cancer Institute grant CA232741 (L.M.S.R.), National Institutes of Health National Institute of Diabetes and Digestive and Kidney Diseases grant DK102943 (L.M.S.R.), the MPN Research Foundation (L.R., A.R.M.), the Children’s Cancer Research Fund (L.M.S.R.), Alex’s Lemonade Stand Foundation (L.M.S.R.), the Allegheny Health Network (L.M.S.R.), and the Maryland Stem Cell Research Fund (2021-MSCRFD-5697 and 2020-MSCRFD-5372) (L.M.S.R.).
Footnotes
DAMI and SET-2 Bulk RNAseq: GSE183374; DAMI ATACseq: GSE189568; DAMI ChIP-seq: GSE 189569; and scRNAseq: GSE197942.
Data sharing requests should be sent to Linda M. S. Resar (lresar@jhmi.edu).
The online version of this article contains a data supplement.
There is a Blood Commentary on this article in this issue.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 USC section 1734.
Authorship
Contribution: L.L. and J.-H.K. designed experiments, performed research, interpreted data, and wrote portions of the manuscript; W.L., D.M.W., and J.K. performed experiments and interpreted data; L.C. performed biostatistical analyses and wrote portions of the manuscript; R.K.R. and R.P.K. provided critical reagents and data; L.X. and L.Z.L. performed experiments; M.V. performed Ingenuity Pathway Analysis analyses; D.R.M. provided the GATA2 antibody and helped to edit the manuscript; Z.J.Z. provided JAK-mutant mice; O.R. performed experiments; M.C.S. provided ruxolitinib chow; K.R. provided guidance with ATACseq and chromatin immunoprecipitation experiments; A.-R.R. and B.P. performed scRNAseq analysis of patient samples; J.L.S. provided expertise and reagents and guidance for experiments and helped to write the manuscript; A.R.M. provided expertise and reagents, designed and performed experiments, and helped to write the manuscript; L.M.S.R. conceived the study, designed experiments, reviewed all data, and wrote the manuscript; and all authors reviewed the final manuscript and agreed to be coauthors.
Conflict-of-interest disclosure: M.C.S. is employed by Incyte Research Institute and holds individual shares in this privately held company. R.K.R has received consulting fees from Stemline Therapeutics, Celgene Corporation, Agios Pharmaceuticals, Apex Oncology, Beyond Spring, Partner Therapeutics, and Jazz Pharmaceuticals and has received research funding from Constellation Pharmaceuticals, Incyte Corporation, and Stemline Therapeutics. The remaining authors declare no competing financial interests.
Correspondence: Linda M. S. Resar, The Johns Hopkins University School of Medicine, Ross Research Building, Room 1025, 720 Rutland Ave, Baltimore, MD 21205; e-mail: lresar@jhmi.edu.
REFERENCES
- 1.Dameshek W. Some speculations on the myeloproliferative syndromes. Blood. 1951;6(4):372-375. [PubMed] [Google Scholar]
- 2.Pardanani A, Fridley BL, Lasho TL, Gilliland DG, Tefferi A. Host genetic variation contributes to phenotypic diversity in myeloproliferative disorders. Blood. 2008;111(5):2785-2789. [DOI] [PubMed] [Google Scholar]
- 3.Tam CS, Nussenzveig RM, Popat U, et al. The natural history and treatment outcome of blast phase BCR-ABL- myeloproliferative neoplasms. Blood. 2008;112(5):1628-1637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skoda RC. Hereditary myeloproliferative disorders. Haematologica. 2010;95(1):6-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lundberg P, Karow A, Nienhold R, et al. Clonal evolution and clinical correlates of somatic mutations in myeloproliferative neoplasms. Blood. 2014;123(14):2220-2228. [DOI] [PubMed] [Google Scholar]
- 6.Tefferi A, Guglielmelli P, Larson DR, et al. Long-term survival and blast transformation in molecularly annotated essential thrombocythemia, polycythemia vera, and myelofibrosis. Blood. 2014;124(16):2507-2513, quiz 2615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Spivak JL, Considine M, Williams DM, et al. Two clinical phenotypes in polycythemia vera. N Engl J Med. 2014;371(9):808-817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Spivak JL. Myeloproliferative neoplasms. N Engl J Med. 2017;376(22):2168-2181. [DOI] [PubMed] [Google Scholar]
- 9.Grinfeld J, Nangalia J, Green AR. Molecular determinants of pathogenesis and clinical phenotype in myeloproliferative neoplasms. Haematologica. 2017;102(1):7-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Tefferi A, Vannucchi AM. Genetic risk assessment in myeloproliferative neoplasms. Mayo Clin Proc. 2017;92(8):1283-1290. [DOI] [PubMed] [Google Scholar]
- 11.Marcellino BK, Hoffman R, Tripodi J, et al. Advanced forms of MPNs are accompanied by chromosomal abnormalities that lead to dysregulation of TP53. Blood Adv. 2018; 2(24):3581-3589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schieber M, Crispino JD, Stein B. Myelofibrosis in 2019: moving beyond JAK2 inhibition. Blood Cancer J. 2019;9(9):74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Karantanos T, Chaturvedi S, Braunstein EM, et al. Sex determines the presentation and outcomes in MPN and is related to sex-specific differences in the mutational burden. Blood Adv. 2020;4(12):2567-2576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mascarenhas JO, Rampal RK, Kosiorek HE, et al. Phase 2 study of ruxolitinib and decitabine in patients with myeloproliferative neoplasm in accelerated and blast phase. Blood Adv. 2020;4(20):5246-5256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moliterno AR, Kaizer H. Applied genomics in MPN presentation. Hematology Am Soc Hematol Educ Program. 2020;2020(1): 434-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Moliterno AR, Ginzburg YZ, Hoffman R. Clinical insights into the origins of thrombosis in myeloproliferative neoplasms. Blood. 2021;137(9):1145-1153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Grinfeld J, Nangalia J, Baxter EJ, et al. Classification and personalized prognosis in myeloproliferative neoplasms. N Engl J Med. 2018;379(15):1416-1430. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Van Egeren D, Escabi J, Nguyen M, et al. Reconstructing the lineage histories and differentiation trajectories of individual cancer cells in myeloproliferative neoplasms. Cell Stem Cell. 2021;28(3):514-523.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Baxter EJ, Scott LM, Campbell PJ, et al. ; Cancer Genome Project . Acquired mutation of the tyrosine kinase JAK2 in human myeloproliferative disorders. Lancet. 2005;365(9464):1054-1061. [DOI] [PubMed] [Google Scholar]
- 20.James C, Ugo V, Le Couédic JP, et al. A unique clonal JAK2 mutation leading to constitutive signalling causes polycythaemia vera. Nature. 2005;434(7037):1144-1148. [DOI] [PubMed] [Google Scholar]
- 21.Kralovics R, Passamonti F, Buser AS, et al. A gain-of-function mutation of JAK2 in myeloproliferative disorders. N Engl J Med. 2005;352(17):1779-1790. [DOI] [PubMed] [Google Scholar]
- 22.Levine RL, Wadleigh M, Cools J, et al. Activating mutation in the tyrosine kinase JAK2 in polycythemia vera, essential thrombocythemia, and myeloid metaplasia with myelofibrosis. Cancer Cell. 2005;7(4):387-397. [DOI] [PubMed] [Google Scholar]
- 23.Nielsen C, Bojesen SE, Nordestgaard BG, Kofoed KF, Birgens HS. JAK2V617F somatic mutation in the general population: myeloproliferative neoplasm development and progression rate. Haematologica. 2014;99(9):1448-1455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Jaiswal S, Ebert BL. Clonal hematopoiesis in human aging and disease. Science. 2019;366(6465):eaan4673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Pastore F, Bhagwat N, Pastore A, et al. PRMT5 inhibition modulates E2F1 methylation and gene-regulatory networks leading to therapeutic efficacy in JAK2V617F-mutant MPN. Cancer Discov. 2020;10(11):1742-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Marinaccio C, Suraneni P, Celik H, et al. LKB1/STK11 is a tumor suppressor in the progression of myeloproliferative neoplasms. Cancer Discov. 2021;11(6):1398-1410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Reddy KL, Feinberg AP. Higher order chromatin organization in cancer. Semin Cancer Biol. 2013;23(2):109-115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Resar L, Chia L, Xian L. Lessons from the crypt: HMGA1-amping up Wnt for stem cells and tumor progression. Cancer Res. 2018;78(8):1890-1897. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Resar LM. The high mobility group A1 gene: transforming inflammatory signals into cancer? Cancer Res. 2010;70(2):436-439. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ben-Porath I, Thomson MW, Carey VJ, et al. An embryonic stem cell-like gene expression signature in poorly differentiated aggressive human tumors. Nat Genet. 2008;40(5): 499-507. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Shah SN, Kerr C, Cope L, et al. HMGA1 reprograms somatic cells into pluripotent stem cells by inducing stem cell transcriptional networks. PLoS One. 2012; 7(11):e48533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Chou BK, Mali P, Huang X, et al. Efficient human iPS cell derivation by a non-integrating plasmid from blood cells with unique epigenetic and gene expression signatures. Cell Res. 2011;21(3):518-529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Xian L, Georgess D, Huso T, et al. HMGA1 amplifies Wnt signalling and expands the intestinal stem cell compartment and Paneth cell niche. Nat Commun. 2017;8(1):15008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reeves R, Beckerbauer L. HMGI/Y proteins: flexible regulators of transcription and chromatin structure. Biochim Biophys Acta. 2001;1519(1-2):13-29. [DOI] [PubMed] [Google Scholar]
- 35.Pomeroy SL, Tamayo P, Gaasenbeek M, et al. Prediction of central nervous system embryonal tumour outcome based on gene expression. Nature. 2002;415(6870):436-442. [DOI] [PubMed] [Google Scholar]
- 36.Sarhadi VK, Wikman H, Salmenkivi K, et al. Increased expression of high mobility group A proteins in lung cancer. J Pathol. 2006;209(2):206-212. [DOI] [PubMed] [Google Scholar]
- 37.Tesfaye A, Di Cello F, Hillion J, et al. The high-mobility group A1 gene up-regulates cyclooxygenase 2 expression in uterine tumorigenesis. Cancer Res. 2007;67(9):3998-4004. [DOI] [PubMed] [Google Scholar]
- 38.Hillion J, Wood LJ, Mukherjee M, et al. Upregulation of MMP-2 by HMGA1 promotes transformation in undifferentiated, large-cell lung cancer. Mol Cancer Res. 2009;7(11):1803-1812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Hristov AC, Cope L, Di Cello F, et al. HMGA1 correlates with advanced tumor grade and decreased survival in pancreatic ductal adenocarcinoma. Mod Pathol. 2010;23(1):98-104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Hillion J, Smail SS, Di Cello F, et al. The HMGA1-COX-2 axis: a key molecular pathway and potential target in pancreatic adenocarcinoma. Pancreatology. 2012;12(4):372-379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Shah SN, Cope L, Poh W, et al. HMGA1: a master regulator of tumor progression in triple-negative breast cancer cells. PLoS One. 2013;8(5):e63419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Belton A, Gabrovsky A, Bae YK, et al. HMGA1 induces intestinal polyposis in transgenic mice and drives tumor progression and stem cell properties in colon cancer cells. PLoS One. 2012;7(1):e30034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Hillion J, Roy S, Heydarian M, et al. The high mobility group A1 (HMGA1) gene is highly overexpressed in human uterine serous carcinomas and carcinosarcomas and drives matrix metalloproteinase-2 (MMP-2) in a subset of tumors. Gynecol Oncol. 2016;141(3):580-587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Gorbounov M, Carleton NM, Asch-Kendrick RJ, et al. High mobility group A1 (HMGA1) protein and gene expression correlate with ER-negativity and poor outcomes in breast cancer. Breast Cancer Res Treat. 2020; 179(1):25-35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Thanos D, Maniatis T. The high mobility group protein HMG I(Y) is required for NF-kappa B-dependent virus induction of the human IFN-beta gene. Cell. 1992;71(5):777-789. [DOI] [PubMed] [Google Scholar]
- 46.Zhao K, Käs E, Gonzalez E, Laemmli UK. SAR-dependent mobilization of histone H1 by HMG-I/Y in vitro: HMG-I/Y is enriched in H1-depleted chromatin. EMBO J. 1993; 12(8):3237-3247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Saitoh Y, Laemmli UK. Metaphase chromosome structure: bands arise from a differential folding path of the highly AT-rich scaffold. Cell. 1994;76(4):609-622. [DOI] [PubMed] [Google Scholar]
- 48.Geierstanger BH, Volkman BF, Kremer W, Wemmer DE. Short peptide fragments derived from HMG-I/Y proteins bind specifically to the minor groove of DNA. Biochemistry. 1994;33(17):5347-5355. [DOI] [PubMed] [Google Scholar]
- 49.Thanos D, Maniatis T. Virus induction of human IFN beta gene expression requires the assembly of an enhanceosome. Cell. 1995;83(7):1091-1100. [DOI] [PubMed] [Google Scholar]
- 50.Falvo JV, Thanos D, Maniatis T. Reversal of intrinsic DNA bends in the IFN beta gene enhancer by transcription factors and the architectural protein HMG I(Y). Cell. 1995; 83(7):1101-1111. [DOI] [PubMed] [Google Scholar]
- 51.Maher JF, Nathans D. Multivalent DNA-binding properties of the HMG-1 proteins. Proc Natl Acad Sci USA. 1996;93(13): 6716-6720. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Huth JR, Bewley CA, Nissen MS, et al. The solution structure of an HMG-I(Y)-DNA complex defines a new architectural minor groove binding motif. Nat Struct Biol. 1997;4(8):657-665. [DOI] [PubMed] [Google Scholar]
- 53.Hillion J, Dhara S, Sumter TF, et al. The high-mobility group A1a/signal transducer and activator of transcription-3 axis: an Achilles heel for hematopoietic malignancies? Cancer Res. 2008;68(24):10121-10127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Schuldenfrei A, Belton A, Kowalski J, et al. HMGA1 drives stem cell, inflammatory pathway, and cell cycle progression genes during lymphoid tumorigenesis. BMC Genomics. 2011;12(1):549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Xu Y, Sumter TF, Bhattacharya R, et al. The HMG-I oncogene causes highly penetrant, aggressive lymphoid malignancy in transgenic mice and is overexpressed in human leukemia. Cancer Res. 2004;64(10): 3371-3375. [DOI] [PubMed] [Google Scholar]
- 56.Di Cello F, Dhara S, Hristov AC, et al. Inactivation of the Cdkn2a locus cooperates with HMGA1 to drive T-cell leukemogenesis. Leuk Lymphoma. 2013;54(8):1762-1768. [DOI] [PubMed] [Google Scholar]
- 57.Roy S, Di Cello F, Kowalski J, et al. HMGA1 overexpression correlates with relapse in childhood B-lineage acute lymphoblastic leukemia. Leuk Lymphoma. 2013;54(11):2565-2567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wood LJ, Mukherjee M, Dolde CE, et al. HMG-I/Y, a new c-Myc target gene and potential oncogene. Mol Cell Biol. 2000; 20(15):5490-5502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Wood LJ, Maher JF, Bunton TE, Resar LM. The oncogenic properties of the HMG-I gene family. Cancer Res. 2000;60(15): 4256-4261. [PubMed] [Google Scholar]
- 60.Nelson DM, Joseph B, Hillion J, Segal J, Karp JE, Resar LM. Flavopiridol induces BCL-2 expression and represses oncogenic transcription factors in leukemic blasts from adults with refractory acute myeloid leukemia. Leuk Lymphoma. 2011;52(10): 1999-2006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Karp JE, Smith BD, Resar LS, et al. Phase 1 and pharmacokinetic study of bolus-infusion flavopiridol followed by cytosine arabinoside and mitoxantrone for acute leukemias. Blood. 2011;117(12):3302-3310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Bao EL, Nandakumar SK, Liao X, et al. ; 23andMe Research Team . Inherited myeloproliferative neoplasm risk affects haematopoietic stem cells. Nature. 2020;586(7831):769-775. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Skarnes WC, Rosen B, West AP, et al. A conditional knockout resource for the genome-wide study of mouse gene function. Nature. 2011;474(7351):337-342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xing S, Wanting TH, Zhao W, et al. Transgenic expression of JAK2V617F causes myeloproliferative disorders in mice. Blood. 2008;111(10):5109-5117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Spivak JL, Merchant A, Williams DM, et al. Thrombopoietin is required for full phenotype expression in a JAK2V617F transgenic mouse model of polycythemia vera. PLoS One. 2020;15(6):e0232801. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Mayle A, Luo M, Jeong M, Goodell MA. Flow cytometry analysis of murine hematopoietic stem cells. Cytometry A. 2013;83(1):27-37. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Freitas C, Wittner M, Nguyen J, et al. Lymphoid differentiation of hematopoietic stem cells requires efficient Cxcr4 desensitization. J Exp Med. 2017;214(7):2023-2040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Gudmundsson KO, Nguyen N, Oakley K, et al. Prdm16 is a critical regulator of adult long-term hematopoietic stem cell quiescence. Proc Natl Acad Sci USA. 2020;117(50):31945-31953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Buenrostro JD, Giresi PG, Zaba LC, Chang HY, Greenleaf WJ. Transposition of native chromatin for fast and sensitive epigenomic profiling of open chromatin, DNA-binding proteins and nucleosome position. Nat Methods. 2013;10(12):1213-1218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Psaila B, Wang G, Rodriguez-Meira A, et al. ; NIH Intramural Sequencing Center . Single-cell analyses reveal megakaryocyte-biased hematopoiesis in myelofibrosis and identify mutant clone-specific targets. Mol Cell. 2020;78(3):477-492.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Rodriguez-Meira A, Buck G, Clark SA, et al. Unravelling intratumoral heterogeneity through high-sensitivity single-cell mutational analysis and parallel RNA sequencing. Mol Cell. 2019;73(6):1292-1305.e8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Dingler FA, Wang M, Mu A, et al. Two aldehyde clearance systems are essential to prevent lethal formaldehyde accumulation in mice and humans. Mol Cell. 2020;80(6): 996-1012.e9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Greenberg SM, Rosenthal DS, Greeley TA, Tantravahi R, Handin RI. Characterization of a new megakaryocytic cell line: the Dami cell. Blood. 1988;72(6):1968-1977. [PubMed] [Google Scholar]
- 74.MacLeod RA, Dirks WG, Reid YA, Hay RJ, Drexler HG. Identity of original and late passage Dami megakaryocytes with HEL erythroleukemia cells shown by combined cytogenetics and DNA fingerprinting. Leukemia. 1997;11(12):2032-2038. [DOI] [PubMed] [Google Scholar]
- 75.Quentmeier H, MacLeod RA, Zaborski M, Drexler HG. JAK2 V617F tyrosine kinase mutation in cell lines derived from myeloproliferative disorders. Leukemia. 2006;20(3):471-476. [DOI] [PubMed] [Google Scholar]
- 76.Fiedler W, Henke RP, Ergün S, et al. Derivation of a new hematopoietic cell line with endothelial features from a patient with transformed myeloproliferative syndrome: a case report. Cancer. 2000;88(2):344-351. [DOI] [PubMed] [Google Scholar]
- 77.Subramanian A, Tamayo P, Mootha VK, et al. Gene set enrichment analysis: a knowledge-based approach for interpreting genome-wide expression profiles. Proc Natl Acad Sci USA. 2005;102(43):15545-15550. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Liberzon A, Birger C, Thorvaldsdóttir H, Ghandi M, Mesirov JP, Tamayo P. The Molecular Signatures Database (MSigDB) hallmark gene set collection. Cell Syst. 2015;1(6):417-425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Zini R, Guglielmelli P, Pietra D, et al. ; AGIMM (AIRC Gruppo Italiano Malattie Mieloproliferative) investigators . CALR mutational status identifies different disease subtypes of essential thrombocythemia showing distinct expression profiles. Blood Cancer J. 2017;7(12):638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Paul F, Arkin Y, Giladi A, et al. Transcriptional heterogeneity and lineage commitment in myeloid progenitors [published correction appears in Cell. 2016;164(1-2):325]. Cell. 2015;163(7): 1663-1677. [DOI] [PubMed] [Google Scholar]
- 81.Giladi A, Paul F, Herzog Y, et al. Single-cell characterization of haematopoietic progenitors and their trajectories in homeostasis and perturbed haematopoiesis. Nat Cell Biol. 2018;20(7):836-846. [DOI] [PubMed] [Google Scholar]
- 82.Nam AS, Kim KT, Chaligne R, et al. Somatic mutations and cell identity linked by genotyping of transcriptomes. Nature. 2019;571(7765):355-360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Izzo F, Lee SC, Poran A, et al. DNA methylation disruption reshapes the hematopoietic differentiation landscape. Nat Genet. 2020;52(4):378-387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Tsai FY, Keller G, Kuo FC, et al. An early haematopoietic defect in mice lacking the transcription factor GATA-2. Nature. 1994;371(6494):221-226. [DOI] [PubMed] [Google Scholar]
- 85.Bresnick EH, Jung MM, Katsumura KR. Human GATA2 mutations and hematologic disease: how many paths to pathogenesis? Blood Adv. 2020;4(18):4584-4592. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Huang Z, Dore LC, Li Z, et al. GATA-2 reinforces megakaryocyte development in the absence of GATA-1. Mol Cell Biol. 2009;29(18):5168-5180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Menendez-Gonzalez JB, Sinnadurai S, Gibbs A, et al. Inhibition of GATA2 restrains cell proliferation and enhances apoptosis and chemotherapy mediated apoptosis in human GATA2 overexpressing AML cells. Sci Rep. 2019;9(1):12212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Akada H, Yan D, Zou H, Fiering S, Hutchison RE, Mohi MG. Conditional expression of heterozygous or homozygous Jak2V617F from its endogenous promoter induces a polycythemia vera-like disease. Blood. 2010;115(17):3589-3597. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Iacobucci I, Li Y, Roberts KG, et al. Truncating erythropoietin receptor rearrangements in acute lymphoblastic leukemia. Cancer Cell. 2016;29(2):186-200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.Maude SL, Tasian SK, Vincent T, et al. Targeting JAK1/2 and mTOR in murine xenograft models of Ph-like acute lymphoblastic leukemia. Blood. 2012;120(17): 3510-3518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Gilles L, Arslan AD, Marinaccio C, et al. Downregulation of GATA1 drives impaired hematopoiesis in primary myelofibrosis. J Clin Invest. 2017;127(4):1316-1320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Zingariello M, Sancillo L, Martelli F, et al. The thrombopoietin/MPL axis is activated in the Gata1low mouse model of myelofibrosis and is associated with a defective RPS14 signature. Blood Cancer J. 2017;7(6):e572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Vannucchi AM, Pancrazzi A, Guglielmelli P, et al. Abnormalities of GATA-1 in megakaryocytes from patients with idiopathic myelofibrosis. Am J Pathol. 2005;167(3):849-858. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Kleppe M, Koche R, Zou L, et al. Dual targeting of oncogenic activation and inflammatory signaling increases therapeutic efficacy in myeloproliferative neoplasms [published correction appears in Cancer Cell. 2018;33(4):785–787]. Cancer Cell. 2018;33(1):29-43.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Ikeda K, Mason PJ, Bessler M. 3′UTR-truncated Hmga2 cDNA causes MPN-like hematopoiesis by conferring a clonal growth advantage at the level of HSC in mice. Blood. 2011;117(22):5860-5869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Dutta A, Hutchison RE, Mohi G. Hmga2 promotes the development of myelofibrosis in Jak2V617F knockin mice by enhancing TGF-β1 and Cxcl12 pathways. Blood. 2017;130(7):920-932. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Ueda K, Ikeda K, Ikezoe T, et al. Hmga2 collaborates with JAK2V617F in the development of myeloproliferative neoplasms. Blood Adv. 2017;1(15): 1001-1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Marquis M, Beaubois C, Lavallée VP, et al. High expression of HMGA2 independently predicts poor clinical outcomes in acute myeloid leukemia [published correction appears in Blood Cancer J. 2019;9(3):28]. Blood Cancer J. 2018;8(8):68. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.