Abstract
Background
Evaluating premature (<65 years of age) mortality because of acute myocardial infarction (AMI) by demographic and regional characteristics may inform public health interventions.
Methods and Results
We used the Centers for Disease Control and Prevention’s WONDER (Wide‐Ranging Online Data for Epidemiologic Research) death certificate database to examine premature (<65 years of age) age‐adjusted AMI mortality rates per 100 000 and average annual percentage change from 1999 to 2019. Overall, the age‐adjusted AMI mortality rate was 13.4 (95% CI, 13.3–13.5). Middle‐aged adults, men, non‐Hispanic Black adults, and rural counties had higher mortality than young adults, women, NH White adults, and urban counties, respectively. Between 1999 and 2019, the age‐adjusted AMI mortality rate decreased at an average annual percentage change of −3.4 per year (95% CI, −3.6 to −3.3), with the average annual percentage change showing higher decline in age‐adjusted AMI mortality rates among large (−4.2 per year [95% CI, −4.4 to −4.0]), and medium/small metros (−3.3 per year [95% CI, −3.5 to −3.1]) than rural counties (−2.4 per year [95% CI, −2.8 to −1.9]). Age‐adjusted AMI mortality rates >90th percentile were distributed in the Southern states, and those with mortality <10th percentile were clustered in the Western and Northeastern states. After an initial decline between 1999 and 2011 (−4.3 per year [95% CI, −4.6 to −4.1]), the average annual percentage change showed deceleration in mortality since 2011 (−2.1 per year [95% CI, −2.4 to −1.8]). These trends were consistent across both sexes, all ethnicities and races, and urban/rural counties.
Conclusions
During the past 20 years, decline in premature AMI mortality has slowed down in the United States since 2011, with considerable heterogeneity across demographic groups, states, and urbanicity. Systemic efforts are mandated to address cardiovascular health disparities and outcomes among nonelderly adults.
Keywords: acute myocardial infarction, epidemiology, mortality
Subject Categories: Cardiovascular Disease, Epidemiology
Nonstandard Abbreviations and Acronyms
- AAPC
average annual percent change
- NH
non‐Hispanic
- WONDER
Wide‐Ranging Online Data for Epidemiologic Research
Clinical Perspective
What Is New?
Between 1999 and 2019, the decline in premature acute myocardial infarction mortality has decelerated since 2011, with considerable demographic and regional variability in age‐adjusted mortality rates.
The premature acute myocardial infarction mortality decline was slower in the rural counties compared with urban counties.
What Are the Clinical Implications?
The deceleration in premature mortality because of acute myocardial infarction may reflect the growing burden of cardiovascular disease among the nonelderly population.
Implementing evidence‐based strategies to treat premature cardiovascular disease and public health interventions targeting high‐risk groups may reduce the demographic and regional disparities.
Cardiovascular disease (CVD) is the leading cause of mortality and morbidity in the United States. 1 , 2 Although therapeutic advances have led to a decline in CVD mortality, 3 , 4 the initial decrease in CVD mortality observed in the United States at the turn of the century has plateaued since 2011. 5 , 6 These concerning trends are mainly driven by the slowing of CVD mortality among elderly adults (≥65 years of age). In contrast, the decline in CVD mortality has stalled among nonelderly individuals (≤65 years of age). 6 Acute myocardial infarction (AMI) is the major contributor to CVD mortality. Studies have illustrated age‐based disparities regarding revascularization strategies, with higher use of revascularization limited to older adults (≥65 years of age). 7 Furthermore, the comorbidity profile of nonelderly adults experiencing AMI has become complex over the years. 7 , 8 The age‐based differences might be further heightened by sex, ethnic and racial, and regional disparities. Therefore, examining premature mortality because of AMI may serve as an essential foundation for shaping health care policy and curb the growing burden of premature CVD. Consequently, we studied the US death certificate database to examine premature mortality (<65 years of age) from AMI, stratified by demographic groups, states, and counties.
Methods
Data Availability Statement
The Centers for Disease Control and Prevention’s WONDER (Wide‐Ranging OnLine Data for Epidemiologic Research) 9 data sets used in this project are publicly available. Therefore, the results of this study are easily replicable from the methods described in the article.
Data Source
We analyzed the Underlying Cause of Death Public Use Record from the National Center for Health Statistics database, which provides state‐ and county‐level mortality data for all US populations based on death certificates from the Centers for Disease Control and Prevention’s WONDER database. 9 , 10 Underlying cause of death is selected from the conditions entered by the physician or other individuals besides physicians, such as the local coroner in certain out‐of‐hospital deaths, on the cause of death section of the death certificate. In case of more than one cause or condition, the underlying cause is determined by the sequence of conditions on the certificate leading to death, the International Classification of Diseases, Tenth Revision (ICD‐10) provisions, and associated selection rules and modifications. The population estimates are Census Bureau estimates of US national, state, and county resident populations. 9
We selected natural deaths attributed to AMI identified using ICD‐10 codes I21‐I22. 9 , 10 , 11 The funeral director reports ethnicity and race information as provided by the surviving next of kin or based on observation, in the case of the informant’s absence. We determined ethnicity and race using the death certificates, reporting race and Hispanic origin separately following the standards put forth by the Office of Management and Budget. 12 We abstracted population estimates using the Census Bureau estimates of US national, state, and county resident populations. 13 Race and ethnicity information from the census is based on self‐description.
This study did not require institutional review board approval because the analysis used government‐issued public‐use data without individually identifiable information.
Data Extraction
We abstracted the number of deaths attributable to AMI and the population size from 1999 to 2019. We abstracted the data on age, sex, ethnicity and race, states, and counties, further stratified by urbanicity. We selected decedents <65 years of age and grouped them into young (18–44 years of age) and middle‐aged (45–64 years of age) adults to focus on premature mortality. We identified race and ethnicity on death certificates as non‐Hispanic (NH) White adults, NH Black adults, and Hispanic adults. For ethnicity and race, we classified the study population into NH White adults, NH Black adults, and Hispanic adults. We did not include NH American Indian or Alaska Native and Asian/Pacific Islander populations in the study because the mortality estimates were small among these demographic subgroups. Finally, we classified counties using the National Center for Health Statistics 2013 Urban‐Rural Classification Scheme and divided them into large and medium metro, small metro, and rural counties (micropolitan and noncore).
Statistical Analysis
We calculated the individual‐year crude death rates by dividing the number of AMI deaths by the corresponding population. Then, using the 2000 US standard population, we directly adjusted the mortality rates per 100 000 US adults. 14 We considered statistically significant differences for age‐adjusted mortality rates between 2 independent populations when their 95% CIs did not overlap. Temporal trends were analyzed by fitting log‐linear regression models using the Joinpoint Regression Program version 4.7.0.0 (National Cancer Institute). 15 We applied the grid search method (2, 2, 0), 0 to 3 joinpoints, permutation test, and parametric method to estimate average annual percent change (AAPC) and 95% CIs. We calculated AAPC with 95% CIs in age‐adjusted mortality rates for all analyses from 1999 to 2019, further stratified into 1999 to 2011 and 2011 to 2019, weighted to account for differences among inflection points. 6 , 16 We used 2011 as the inflection point in mortality trends following the national mortality data reporting CVD mortality trends. 16 , 17 Slopes were perceived as increasing or decreasing if the estimated slope differed significantly from 0. 18 , 19 For all analyses, statistical significance was set at 5%.
Results
Between 1999 and 2019, a total of 615 848 premature deaths occurred in adults (3 964 352 768 person‐years) corresponding to an age‐adjusted AMI mortality rate of 13.4 (95% CI, 13.3–13.5) per 100 000 (Table S1). Overall, the age‐adjusted AMI mortality rate decreased from 20.4 (95% CI, 20.2–20.7) per 100 000 in 1999 to 9.9 (95% CI, 9.8–10.6) per 100 000 in 2019, with an AAPC of −3.4 per year (95% CI, −3.6 to −3.3). Between 1999 and 2011, the AAPC in age‐adjusted AMI mortality rate was −4.3 per year (95% CI, −4.6 to −4.1), which slowed down between 2011 and 2019 (−2.1 per year [95% CI, −2.4 to −1.8]) (Figure 1).
Figure 1.
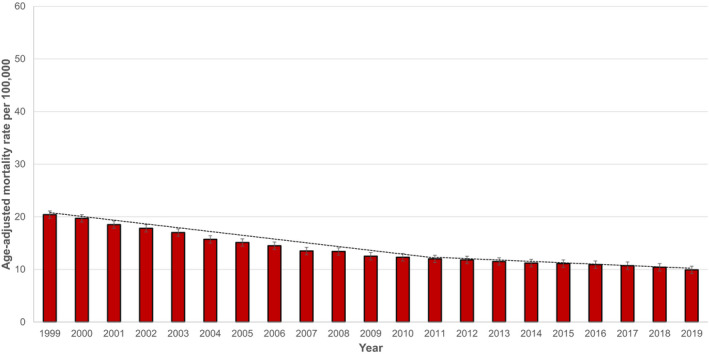
Trends in age‐adjusted acute myocardial infarction mortality rates per 100 000 among adults <65 years of age in the United States, 1999 to 2019.
Trends in AMI Mortality by Age
The age‐adjusted AMI mortality rates were higher for middle‐aged (34.9 [95% CI, 34.8–35.0]) adults than young adults (2.5 [95% CI, 2.4–2.6]). Table S2 reports age‐adjusted AMI mortality rates among young and middle‐aged adults, stratified by sex, ethnicity and race, and US states. Between 1999 and 2019, the AAPCs in age‐adjusted AMI mortality rates were −2.7 per year (95% CI, −3.1 to −2.5) in young adults, and −2.1 per year (95% CI, −2.4 to −1.7) in middle‐aged adults. The AAPC in age‐adjusted AMI mortality rates in young adults did not vary over the study period (Figure 2A ; Table S1). However, for middle‐aged adults, after initial decline in age‐adjusted AMI mortality rates between 1999 and 2011 (AAPC, −3.6 per year [95% CI, −4.0 to −3.2]), mortality decreased at an accelerated pace between 2011 and 2019 (AAPC, −4.6 per year [95% CI, −5.2 to −4.0]).
Figure 2.
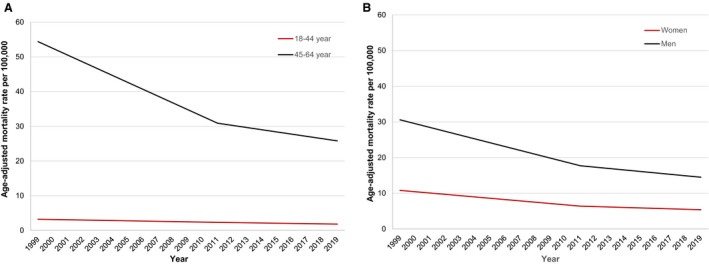
Trends in age‐adjusted acute myocardial infarction mortality rates per 100 000 among adults <65 years of age stratified by (A) age, and (B) sex in the United States, 1999 to 2019.
Trends in AMI Mortality by Sex
Overall, age‐adjusted AMI mortality rates were higher in men (20.0 [95% CI, 19.9–20.1]) than women (7.3 [95% CI, 7.2–7.4]). Table S3 reports age‐adjusted AMI mortality rates by sex, stratified by the US states. Between 1999 and 2019, the AAPCs in age‐adjusted AMI mortality rates were −3.3 per year (95% CI, −3.6 to −3.1) in women and −3.5 per year (95% CI, −3.7 to −3.4) in men. In both sexes, after an initial decrease, AAPCs showed that age‐adjusted AMI mortality decline has slowed down between 2011 and 2019 (Figure 2B; Table S1).
Trends in AMI Mortality by Ethnicity and Race
Overall, age‐adjusted AMI mortality rates were higher in NH Black adults (17.5 [95% CI, 17.4–17.6]) than NH White adults (13.7 [95% CI, 13.6–13.8]). Table S3 reports age‐adjusted AMI mortality rates by ethnicity and race, stratified by the US states. Between 1999 and 2019, the AAPCs in age‐adjusted AMI mortality rates were −3.9 per year (95% CI, −4.3 to −3.6) in NH Black adults, −3.3 per year (95% CI, −3.5 to −3.1) in NH White adults, and −3.5 per year (95% CI, −4.1 to −3.0) in Hispanic adults. Between 1999 and 2011, AAPCs showed a reduction in age‐adjusted AMI mortality rates for all ethnicities and races. However, AAPCs showed a significant deceleration in age‐adjusted AMI mortality rates between 2011 and 2019 among all ethnicities and races (Figure 3; Table S1).
Figure 3.
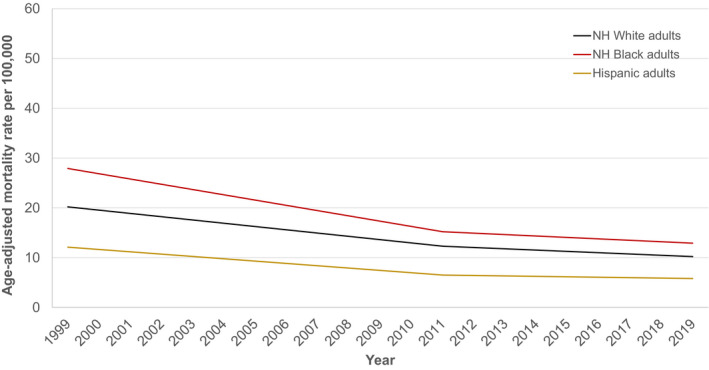
Trends in age‐adjusted acute myocardial infarction mortality rates per 100 000 among adults <65 years of age stratified by ethnicity and race in the United States, 1999 to 2019.
Trends in AMI Mortality by the US States
Table S1 documents trends in age‐adjusted AMI mortality rates across the US states. Figure 4 illustrates the distribution of age‐adjusted AMI mortality rates across the US states. States with age‐adjusted AMI mortality rates >90th percentile were distributed in the South (Arkansas, Mississippi, Kentucky, Louisiana, and Tennessee), and those with age‐adjusted AMI mortality rates <10th percentile were clustered in the West and Northeast (Colorado, Utah, Vermont, Connecticut, and Alaska). We noted marked state‐level variations in AMI mortality trends. For instance, in New Mexico, age‐adjusted AMI mortality rates decreased at an AAPC of −4.2 per year (95% CI, −4.9 to −3.4) between 1999 and 2011, followed by an increase at an AAPC of 3.5 per year (95% CI, 0.3–6.8) between 2011 and 2019. However, after an initial decrease in mortality, AAPCs showed that age‐adjusted AMI mortality decline had stalled between 2011 and 2019 in the US states clustered in the West (Arizona, Idaho, Montana, and Nevada), the South (Arkansas and Mississippi), and in the Midwest (Nebraska and South Dakota).
Figure 4.
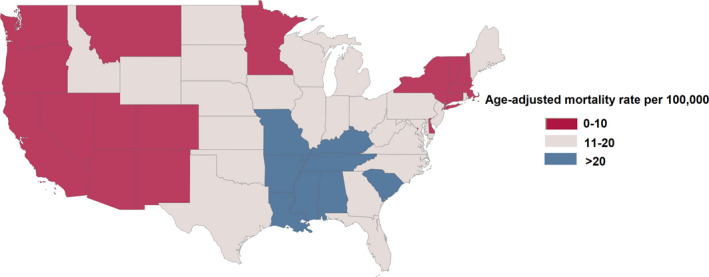
Age‐adjusted acute myocardial infarction mortality rates per 100 000 across the United States, 1999 to 2019.
Trends in AMI Mortality by Urbanicity
Age‐adjusted AMI mortality rates were significantly higher in the rural versus urban counties (Table S1). Between 1999 and 2019, AAPCs showed higher decline in age‐adjusted AMI mortality rates among large (−4.2 per year [95% CI, −4.4 to −4.0]), and medium/small metros (−3.3 per year [95% CI, −3.5 to −3.1]) than rural counties (−2.4 per year [95% CI, −2.8 to −1.9]). Between 1999 and 2011, AAPCs showed a substantial decline in age‐adjusted AMI mortality rates, followed by deceleration between 2011 and 2019.
Discussion
During the past 20 years, we found considerable demographic and geographic variations in premature AMI mortality in the United States. Overall, premature AMI mortality rates were higher in men versus women, NH Black adults versus NH White adults, and rural versus urban counties. Although premature AMI mortality has declined by nearly 52% during the past 2 decades, the initial gains in cardiovascular survival achieved by an accelerated decline in premature AMI mortality have been attenuated by the deceleration in mortality decline since 2011. These trends were consistent across demographic subgroups and by urbanicity.
This study uncovered demographic and regional heterogeneities in premature AMI mortality, which could have been masked in aggregate CVD mortality. Previous data showed that CVD mortality rates in nonelderly adults (25–64 years of age) had no appreciable change since 2011, despite a 70% decline in the preceding 4 decades (1968–2011). 20 However, in a subgroup of adults 55 to 64 years of age, a slight 4% increase in CVD mortality was observed between 2011 and 2017. In contrast, the rates were stable for adults 25 to 54 years of age. 20 Shah and colleagues reported a modest 3% decline in young and a ~2% increase in cardiac mortality in middle‐aged adults between 2011 and 2018. 6 The rise in cardiac mortality in the middle‐age group was driven by increased mortality because of heart failure, hypertensive heart disease, valvular heart disease, arrhythmia, pulmonary heart disease, and other causes. 6 Another report mentioned that over 20% of cardiometabolic deaths (heart disease, stroke, and diabetes) occurred in adults <65 years of age. 20 We focused explicitly on premature mortality attributable to AMI to understand the influence of this fundamental determinant of CVD mortality.
In our study, mortality rates were higher for middle‐aged versus younger adults. The absolute difference in AAPC between middle‐aged and young adults during the past 2 decades was −0.7 per year, suggesting that the rate of decline was slower in the middle‐aged adults than in the younger population. The observed heterogeneity may be explained by the higher prevalence of traditional cardiovascular risk factors in the middle‐aged than young adults, making protective secular trends less effective in this age group. For instance, during 2015 to 2016, hypertension prevalence was 33.2% in individuals 40 to 59 years of age, compared with 7.5% in the 18 to 39 years of age group. 21 Furthermore, a higher prevalence of cardiometabolic diseases in the middle aged, such as hypertensive heart disease or diabetes, might explain this variation. 20 , 22 , 23
We reported higher AMI mortality rates for men than women and a comparable reduction in mortality across both sexes over time. We also noted higher AMI morality for NH Black than NH White adults. Previous observations demonstrated that NH Black adults have a higher prevalence of diabetes and hypertension than NH White adults. 24 , 25 Additionally, low socioeconomic status, higher uninsured rates, and limited access to health care among NH Black minorities widen the health gap between both races. 26 , 27 NH Black patients had fewer resources for procedural access, low procedural success, higher recurrence of AMI, hospitalizations, and death after AMI than their counterparts, even after adjustment for baseline characteristics or treatment approach. 28 This scenario gets further complicated because of the underuse of revascularization and guideline‐recommended medical therapy after AMI in NH Black individuals versus NH White adults. 28 The recent AMI mortality trends underscore health care disparities faced by ethnic and racial minorities. 29
We noted higher AMI mortality in the Southern states than other regions and rural versus urban counties. Southern states have a higher age‐adjusted obesity prevalence (Mississippi 40.7%, Arkansas 37.6%, Kentucky 36.2%, Louisiana 35.9%, and Tennessee 36.3%), 30 and lower self‐reported amount of physical activity (Kentucky 16.1%, Mississippi 16.2%, Arkansas 9.4%, Louisiana 19.8%, and Tennessee 22.1%). 30 Similarly, smoking, hypertension, and hypercholesterolemia were also highly prevalent in states in the South. 30 Moreover, social gradients in education, employment, immigration, and demographic behavior patterns are essential factors shaping these mortality trends. 31 For instance, besides Kentucky, none of the other states with higher AMI mortality were early adopters of the Patient Protection and Affordable Care Act, the largest Medicaid coverage expansion since the inception of the program, 32 which may influence the survival of nonelderly adults by limiting access to health care. 32 In this regard, the rural–urban CVD mortality gap doubled during the past 2 decades, predominantly because of the same disproportionate distribution of socioeconomic and health indicators between rural and urban counties. 33
This study has several limitations. Vital statistics and census data rely on death certificates. Therefore, accurate ascertainment of demographic information and cause of death based on ICD‐10 codes, which are subject to misclassification, can bias the results. 34 The Framingham Heart Study showed that death certificates might overestimate coronary heart disease (CHD) as the cause of death up to 24% compared with physician‐adjudicated CHD mortality. 34 , 35 These observations were consistent across other studies comparing death certificates with nosologists’ coding of death certificates, 35 or with data gathered through informant interviews, physician, or coroner questionnaires. 36 However, in the Framingham Heart Study, overestimation of CHD mortality was more prominent among older adults, showing a 109% difference between death certificates and physician‐ascertained CHD mortality. Whereas, after excluding deaths from unknown causes, death certificates were shown to slightly underestimate CHD mortality compared with physician‐adjudicated mortality among nonelderly adults (<65 years of age, −2.2%). 34 Therefore, these trivial differences among the nonelderly population are unlikely to influence mortality trends over 2 decades. 20 Since the Centers for Disease Control and Prevention’s WONDER database does not specify certain groups in each bridged‐race category, reliable disaggregated data on NH American Indian/Alaska Native decedents and NH Asian/Pacific Islander individuals were unavailable. 20 The database also lacks information on clinical and social determinants of health. Thus, the apparent disparities in demographic and census region variations cannot be directly ascribed to clinical variables or social determinants of health. Although reporting of deaths may vary across states or deaths within the population, the vital statistics records deaths to the state of residence at the time of death and does not account for migration between states. 37
In conclusion, premature mortality attributable to AMI declined in the United States during the past 20 years. However, this decline was more prominent in the first decade but diminished since 2011. The rate of decline varied across demographic groups, states, and urban/rural counties. Future studies are warranted to define key drivers and the best interventions to ameliorate premature mortality attributable to AMI. These findings have sizeable public health implications regarding identifying clinical differences and social vulnerabilities in critical demographic subgroups and geographic hotspots.
Sources of Funding
None.
Disclosures
S.S.V. has received research support from the Department of Veterans Affairs, World Heart Federation, Tahir, and Jooma Family Honorarium. He is Associate Editor for the American College of Cardiology (innovations, https://www.acc.org/). M.D.S. is on advisory activities with Amgen, Alexion, Esperion, and Novartis. K.N. serves as a consultant for Amgen, Novartis, and Novo Nordisk. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S3.
Supplemental Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.021682
For Sources of Funding and Disclosures, see page 7.
References
- 1. Vos T, Lim SS, Abbafati C, Abbas KM, Abbasi M, Abbasifard M, Abbasi‐Kangevari M, Abbastabar H, Abd‐Allah F, Abdelalim A, et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet. 2020;396:1204–1222. doi: 10.1016/S0140-6736(20)30925-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Virani Salim S, Alonso A, Benjamin Emelia J, Bittencourt Marcio S, Callaway Clifton W, Carson April P, Chamberlain Alanna M, Chang Alexander R, Cheng S, Delling Francesca N, et al. Heart disease and stroke statistics—2020 update: a report from the American heart association. Circulation. 2020;141:e139–e596. doi: 10.1161/CIR.0000000000000757 [DOI] [PubMed] [Google Scholar]
- 3. Wilmot KA, O’Flaherty M, Capewell S, Ford ES, Vaccarino V. Coronary heart disease mortality declines in the united states from 1979 through 2011. Circulation. 2015;132:997–1002. doi: 10.1161/CIRCULATIONAHA.115.015293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Ma J, Ward EM, Siegel RL, Jemal A. Temporal trends in mortality in the United States, 1969–2013. JAMA. 2015;314:1731. doi: 10.1001/jama.2015.12319 [DOI] [PubMed] [Google Scholar]
- 5. Sidney S, Quesenberry CP, Jaffe MG, Sorel M, Nguyen‐Huynh MN, Kushi LH, Go AS, Rana JS. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiology. 2016;1:594. doi: 10.1001/jamacardio.2016.1326 [DOI] [PubMed] [Google Scholar]
- 6. Shah NS, Molsberry R, Rana JS, Sidney S, Capewell S, O'Flaherty M, Carnethon M, Lloyd‐Jones DM, Khan SS. Heterogeneous trends in burden of heart disease mortality by subtypes in the United States, 1999–2018: observational analysis of vital statistics. BMJ. 2020;370:m2688. doi: 10.1136/bmj.m2688 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Alkhouli M, Alqahtani F, Kalra A, Gafoor S, Alhajji M, Alreshidan M, Holmes DR, Lerman A. Trends in characteristics and outcomes of hospital in patients undergoing coronary revascularization in the United States, 2003–2016. JAMA Network Open. 2020;3:e1921326. doi: 10.1001/jamanetworkopen.2019.21326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Dani SS, Minhas AMK, Arshad A, Krupica T, Goel SS, Virani SS, Sharma G, Blankstein R, Blaha MJ, Al‐Kindi SG, et al. Trends in characteristics and outcomes of hospitalized young patients undergoing coronary artery bypass grafting in the United States, 2004 to 2018. J Am Heart Assoc. 2021;10:e021361. doi: 10.1161/JAHA.121.021361 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. The Centers for Disease Control and Prevention (CDC) National Center for Health Statistics . About underlying cause of death 1999–2018. (https://wonder.cdc.gov/wonder/help/ucd.html). Accessed on 02/10/2020
- 10. Friede A, Reid JA, Ory HW. CDC WONDER: a comprehensive on‐line public health information system of the Centers for Disease Control and Prevention. Am J Public Health. 1993;83:1289–1294. doi: 10.2105/AJPH.83.9.1289 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Khan SU, Bashir ZS, Khan MZ, Khan MS, Gulati M, Blankstein R, Blumenthal RS, Michos ED. Trends in cardiovascular deaths among young adults in the United States, 1999 to 2018. The American Journal of Cardiology. 2020;128:216–217. doi: 10.1016/j.amjcard.2020.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Burhansstipanov L, Satter DE. Office of management and budget racial categories and implications for American Indians and Alaska Natives. Am J Public Health. 2000;90:1720. doi: 10.2105/ajph.90.11.1720 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. The United States Census Bureau . Population and Housing Unit Estimates. (https://www.census.gov/programs‐surveys/popest.html). Accessed on 12/25/2020
- 14. Hoyert DL, Anderson RN. Age‐adjusted death rates: trend data based on the year 2000 standard population. National Vital Statistics Reports: from the Centers for Disease Control and Prevention, National Center for Health Statistics, National Vital Statistics System. 2001;49:1–6. [PubMed] [Google Scholar]
- 15. Clegg LX, Hankey BF, Tiwari R, Feuer EJ, Edwards BK. Estimating average annual per cent change in trend analysis. Stat Med. 2009;28:3670–3682. doi: 10.1002/sim.3733 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Woolf SH, Schoomaker H. Life expectancy and mortality rates in the United States, 1959–2017. JAMA. 2019;322:1996–2016. doi: 10.1001/jama.2019.16932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Khan SU, Bashir ZS, Khan MZ, Khan MS, Gulati M, Blankstein R, Blumenthal RS, Michos ED. Trends in cardiovascular deaths among young adults in the United States, 1999 to 2018. Am J Cardiol. 2020;128:216–217. doi: 10.1016/j.amjcard.2020.05.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Sidney S, Quesenberry CP Jr, Jaffe MG, Sorel M, Nguyen‐Huynh MN, Kushi LH, Go AS, Rana JS. Recent trends in cardiovascular mortality in the United States and public health goals. JAMA Cardiol. 2016;1:594–599. doi: 10.1001/jamacardio.2016.1326 [DOI] [PubMed] [Google Scholar]
- 19. Ritchey MD, Wall HK, George MG, Wright JS. US trends in premature heart disease mortality over the past 50 years: where do we go from here? Trends Cardiovasc Med. 2020;30:364–374. doi: 10.1016/j.tcm.2019.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Shah NS, Lloyd‐Jones DM, Kandula NR, Huffman MD, Capewell S, O’Flaherty M, Kershaw KN, Carnethon MR, Khan SS. Adverse trends in premature cardiometabolic mortality in the United States, 1999 to 2018. JAHA. 2020;9:e018213. doi: 10.1161/JAHA.120.018213 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fryar CD, Ostchega Y, Hales CM, Zhang G, Kruszon‐Moran D. Hypertension prevalence and control among adults: United States, 2015‐2016. NCHS Data Brief. 2017:1–8. [PubMed] [Google Scholar]
- 22. Gupta A, Wang Y, Spertus JA, Geda M, Lorenze N, Nkonde‐Price C, D'Onofrio G, Lichtman JH, Krumholz HM. Trends in acute myocardial infarction in young patients and differences by sex and race, 2001 to 2010. JACC. 2014;64:337–345. doi: 10.1016/j.jacc.2014.04.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Vikulova DN, Grubisic M, Zhao Y, Lynch K, Humphries KH, Pimstone SN, Brunham LR. Premature atherosclerotic cardiovascular disease: trends in incidence, risk factors, and sex related differences, 2000 to 2016. J Am Heart Assoc. 2019;8:e012178. doi: 10.1161/JAHA.119.012178 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Graham GN, Jones PG, Chan PS, Arnold SV, Krumholz HM, Spertus JA. Racial disparities in patient characteristics and survival after acute myocardial infarction. JAMA Network Open. 2018;1:e184240. doi: 10.1001/jamanetworkopen.2018.4240 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Rodríguez JE, Campbell KM. Racial and ethnic disparities in prevalence and care of patients with type 2 diabetes. Clin Diabetes. 2017;35:66–70. doi: 10.2337/cd15-0048 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Noonan AS, Velasco‐Mondragon HE, Wagner FA. Improving the health of African Americans in the USA: an overdue opportunity for social justice. Public Health Rev. 2016;37:12. doi: 10.1186/s40985-016-0025-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Mays VM, Cochran SD, Barnes NW. Race, race‐based discrimination, and health outcomes among African Americans. Annu Rev Psychol. 2007;58:201–225. doi: 10.1146/annurev.psych.57.102904.190212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sabatine MS, Blake GJ, Drazner MH, Morrow DA, Scirica BM, Murphy SA, Mccabe CH, Weintraub WS, Gibson CM, Cannon CP. Influence of race on death and ischemic complications in patients with non–ST‐elevation acute coronary syndromes despite modern, protocol‐guided treatment. Circulation. 2005;111:1217–1224. doi: 10.1161/01.CIR.0000157733.50479.B9 [DOI] [PubMed] [Google Scholar]
- 29. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American heart association. Circulation. 2020;142:e454–e468. doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 30. The Centers for Disease Control and Prevention . The Behavioral Risk Factor Surveillance System (BRFSS). (https://www.cdc.gov/brfss/brfssprevalence/index.html). Prevalence and Trends Data. Accessed on 11/18/2020
- 31. Silverstein M, Hsu HE, Bell A. Addressing social determinants to improve population health: the balance between clinical care and public health. JAMA. 2019;322(24):2379– 10.1001/jama.2019.18055. doi: 10.1001/jama.2019.18055 [DOI] [PubMed] [Google Scholar]
- 32. Khatana SAM, Bhatla A, Nathan AS, Giri J, Shen C, Kazi DS, Yeh RW, Groeneveld PW. Association of Medicaid expansion with cardiovascular mortality. JAMA Cardiology. 2019;4:671. doi: 10.1001/jamacardio.2019.1651 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Cross SH, Mehra MR, Bhatt DL, Nasir K, O'Donnell CJ, Califf RM, Warraich HJ. Rural‐urban differences in cardiovascular mortality in the US, 1999–2017. JAMA. 2020;323:1852–1854. doi: 10.1001/jama.2020.2047 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Lloyd‐Jones DM. Accuracy of death certificates for coding coronary heart disease as the cause of death. Ann Intern Med. 1998;129:1020. doi: 10.7326/0003-4819-129-12-199812150-00005 [DOI] [PubMed] [Google Scholar]
- 35. Ives DG, Samuel P, Psaty BM, Kuller LH. Agreement between nosologist and cardiovascular health study review of deaths: implications of coding differences. J Am Geriatr Soc. 2009;57:133–139. doi: 10.1111/j.1532-5415.2008.02056.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Coady SA, Sorlie PD, Cooper LS, Folsom AR, Rosamond WD, Conwill DE. Validation of death certificate diagnosis for coronary heart disease: the Atherosclerosis Risk in Communities (ARIC) Study. J Clin Epidemiol. 2001;54:40–50. doi: 10.1016/S0895-4356(00)00272-9 [DOI] [PubMed] [Google Scholar]
- 37. Roth GA, Dwyer‐Lindgren L, Bertozzi‐Villa A, Stubbs RW, Morozoff C, Naghavi M, Mokdad AH, Murray CJL. Trends and patterns of geographic variation in cardiovascular mortality among US counties, 1980–2014. JAMA. 2017;317:1976. doi: 10.1001/jama.2017.4150 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3.
Data Availability Statement
The Centers for Disease Control and Prevention’s WONDER (Wide‐Ranging OnLine Data for Epidemiologic Research) 9 data sets used in this project are publicly available. Therefore, the results of this study are easily replicable from the methods described in the article.


