Abstract
Background
Long scanning times impede cardiac magnetic resonance (CMR) clinical uptake. A “one‐size‐fits‐all” shortened, focused protocol (eg, only function and late‐gadolinium enhancement) reduces scanning time and costs, but provides less information. We developed 2 question‐driven CMR and stress‐CMR protocols, including tailored advanced tissue characterization, and tested their effectiveness in reducing scanning time while retaining the diagnostic performances of standard protocols.
Methods and Results
Eighty three consecutive patients with cardiomyopathy or ischemic heart disease underwent the tailored CMR. Each scan consisted of standard cines, late‐gadolinium enhancement imaging, native T1‐mapping, and extracellular volume. Fat/edema modules, right ventricle cine, and in‐line quantitative perfusion mapping were performed as clinically required. Workflow was optimized to avoid gaps. Time target was <30 minutes for a CMR and <35 minutes for a stress‐CMR. CMR was considered impactful when its results drove changes in diagnosis or management. Advanced tissue characterization was considered impactful when it changed the confidence level in the diagnosis. The quality of the images was assessed. A control group of 137 patients was identified among scans performed before February 2020. Compared with standard protocols, the average scan duration dropped by >30% (CMR: from 42±8 to 28±6 minutes; stress‐CMR: from 50±10 to 34±6 minutes, both P<0.0001). Independent on the protocol, CMR was impactful in ≈60% cases, and advanced tissue characterization was impactful in >45% of cases. Quality grading was similar between the 2 protocols. Tailored protocols did not require additional staff.
Conclusions
Tailored CMR and stress‐CMR protocols including advanced tissue characterization are accurate and time‐effective for cardiomyopathies and ischemic heart disease.
Keywords: cardiomyopathy, cardiovascular magnetic resonance, ischemic heart disease, rapid scanning, time‐effectiveness
Subject Categories: Magnetic Resonance Imaging (MRI), Cardiomyopathy, Chronic Ischemic Heart Disease
Cardiac magnetic resonance (CMR) is the reference technique for cardiac chamber geometry, systolic function assessment, and noninvasive myocardial tissue characterization. 1 First‐pass perfusion stress CMR (stress‐CMR) is also accurate and cost‐effective in detecting ischemia and guiding revascularization. 2 , 3 Despite the amount of information provided with a single scan, CMR uptake is limited globally by lengthy acquisition times that contribute to higher cost and negatively affects patient comfort and compliance. Indeed, the average CMR acquisition time can last up to 45 minutes, with additional 15 minutes in case of stress‐CMR.
Reducing scan duration is a significant CMR challenge. Main drives traditionally were economic sustainability, comfort and compliance of patients, and imaging resources optimization. The COVID‐19 pandemic has put additional pressure on the health care systems, because of the need to reschedule cancelled tests while at the same time carrying on with routine activity and ensuring additional safety measures, including social distancing and ad‐hoc equipment sanitation.
To reduce CMR duration, industry has contributed technological advances, including faster reconstruction, parallel imaging, compressed sensing, and automated workflows. These strategies are effective but limited by the need for costly hardware and software upgrades. On the other hand, protocol workflow optimization and image selection tailored to the clinical question effectively reduce acquisition times, while retaining diagnostic performance. Examples are a noncontrast, 6‐minute, 10‐breath hold CMR protocol for the assessment of cardiac and liver iron load, myocardial function, and extracardiac anatomy in patients with thalassemia, 4 , 5 a shortened cardiothoracic‐MR protocol to rule out myocardial inflammation, and pulmonary embolism in half of the time of a standard CMR, 6 and 2 stress‐CMR protocols for the evaluation of inducible ischemia in <30 minutes. 7 , 8 Although very time‐effective, the main limitation of these protocols is the lack of transferability to other cardiac conditions. 4 , 6
Finally, in the INCA‐Peru study, an 18‐minute CMR protocol for the evaluation of cardiomyopathies, consisting of left ventricle (LV) long‐ and short‐ axis cines, aortic valve cines, and late gadolinium enhancement imaging, was developed and tested. 9 The authors reported a CMR‐driven change in management in 56% of patients, consistent with that reported in international registries, 10 confirming the importance of late gadolinium enhancement within the imaging portfolio and improving both CMR feasibility and cost‐effectiveness in Low‐Middle Income Countries. 9 Menacho’s protocol is suitable for a wide range of indications, including all cardiomyopathies and viability assessment. Nevertheless, 1‐way scans were shortened was by the omission of more advanced tissue characterization such as mapping. However, these still have a role providing unique information with diagnostic and prognostic relevance for scenarios including the evaluation of LV hypertrophy, diffuse fibrosis, inflammatory heart conditions, infiltrative diseases, and myocardial infarction with nonobstructed coronary arteries, and thus should not be omitted. 11 , 12 , 13
Therefore, we explored the use of a more complete, but still abbreviated, tailored CMR and stress‐CMR strategy for key indications (focusing on cardiomyopathies and ischemic heart disease), with targeted advanced tissue characterization (T1 mapping and extracellular volume, fat, and edema modules) and additional cines (right ventricle [RV] module), 12 but with substantially shorter scan times, aiming for no more than 10 minutes longer than Menacho’s rapid CMR and at least 10 minutes shorter than conventional imaging.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request.
We applied the new CMR protocols to the patients referred for either a CMR or a stress‐CMR to our Institution from June 1 to July 29, 2020 (tailored CMR group). A control group consisted of a sample of standard CMR and stress‐CMR scans performed from February 1, 2019 to January 30, 2020 (standard CMR group). Patients of the standard CMR group were similar to patients of the tailored CMR group in terms of age, sex, proportion of first diagnostic scan versus follow‐up scans, and presence of arrhythmias. Both groups included outpatients referred by Auxologico staff cardiologists and external physicians, as well as Auxologico inpatients. The study was retrospective, approved by the local Ethics Committee, and conducted in accordance with the Helsinki Declaration. All patients signed an informed consent for “general” research purposes, at the time of CMR.
Protocoling
All patients were required to bring a copy of their previous cardiology records on the CMR day, including reports of ECGs, echocardiography, exercise tests, Holter ECG, and clinical letters. While the patient underwent cannulation, an experienced cardiologist (C.T. or S.C.) reviewed the documents and protocoled the scan, depending on the clinical indication, and accordingly to current guidelines 12 (Figure 1; Table S1).
Figure 1. Tailored protocols schematics and different indications.
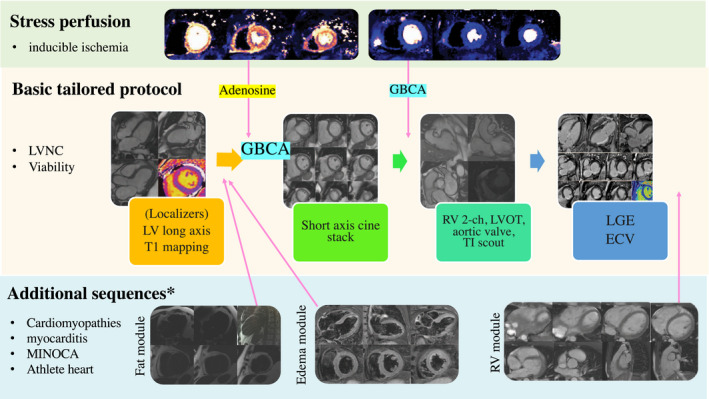
The “basic tailored protocol,” adapted from Menacho et al, 9 consists of localizers, left ventricular long‐axis cines, short‐axis cines, 2‐chamber right ventricle, LV outflow tract and aortic valve cines, late gadolinium enhancement imaging, 1 midventricular short‐axis native T1 mapping slice and corresponding extracellular volume (ECV) assessment, and lasts ≈20 minutes. Adding LVOT, aortic valve and 2‐chambers cine views and advanced tissue characterization (either edema module or fat module plus right ventricle focused cine), the whole protocol can be completed in <30 minutes. Adding both perfusion and advanced tissue characterization, the protocol lasts <35 minutes. *Different additional images were added depending on clinical need as illustrated in Table S1. Cine, balanced steady‐state free precession cine sequences; ECV, extracellular volume; GBCA indicates gadolinium‐based contrast agent; LGE, late gadolinium enhancement; LV, left ventricle; LVNC, left ventricular non‐compaction; LVOT, LV outflow tract; MINOCA, myocardial infarction with nonobstructed coronary arteries; RV, right ventricle; and TI, inversion time.
The same physician reviewed images before contrast administration and at the end of the scan for quality and to evaluate whether additional images were needed, and issued the clinical report (Figure S1).
CMR Technique
Images were acquired on a 1.5‐T scanner (Avanto Fit; Siemens Healthineers, Erlangen, Germany) using dedicated cardiac software, phase‐array surface receiver coil, and ECG triggering. A standardized protocol was carried out in all patients (Figure 1), including (1) localizers, bright‐blood and half‐Fourier acquisition single‐shot turbo spin echo transversal stack; (2) long‐axis cines (2‐, 3‐, and 4‐chamber); (3) a native short‐axis midventricular T1 map; (4) bolus of gadolinium‐based contrast agent (Gadovist; Bayer Healthcare, Switzerland) of 0.1 mmol/kg; (5) stack of short‐axis cines, a second LV outflow tract cine, aortic valve short‐axis cine, and RV 2‐chambers cine; (6) late gadolinium enhancement images (3 LV long‐axis and a short‐axis stack); and (7) a postcontrast short‐axis midventricular T1 map and extracellular volume map.
Stress‐CMR scan protocol also included in‐line quantitative perfusion mapping 14 acquired during stress (at peak adenosine infusion 12 ) and at rest, with an iv gadolinium‐based contrast agent bolus (0.05 mmol/kg during stress and rest acquisition, respectively). Rest perfusion images were acquired >5 minutes after stress. During this time, short‐axis stack cines were acquired. LV outflow tract, aortic valve, and RV 2‐chamber cine views were acquired after rest perfusion.
Cines used a breath‐hold steady‐state free‐precession sequence. T1 maps used Modified Look‐Lockers Inversion recovery images (MOLLI, Siemens WIP1041). Late gadolinium enhancement images were acquired >5 minutes after contrast administration by motion‐corrected segmented inversion‐recovery and phase‐sensitive‐inversion‐recovery gradient‐echo sequence. 15 Inversion‐time to null normal myocardium was optimized on Look‐Locker images. Postcontrast T1 maps were acquired >10 minutes postcontrast.
Additional sequences, acquired on the basis of the clinical need, included (1) edema module (black blood Short Tau Inversion‐Recovery, 3‐long and 3‐short‐axis views, precontrast; (2) fat module (multi‐echo Dixon fat‐water separated images 16 ), 3‐short and 3‐long‐axis views, precontrast; and (3) RV cine outflow tract view, inflow–outflow tract view, transverse stack. 12
Image Analysis and Quality Grading
Images were analyzed with a dedicated software (Argus, Siemens Healthineers). Image quality was graded as: (1) poor (inadequate to answer the clinical question); (2) moderate (presence of artifact not significantly affecting diagnostic performance); and (3) good (optimal image quality). Scan duration was calculated from the timestamp of the first to the last images.
Impact of CMR
Follow‐up was performed at 6 to 12 months reviewing available clinical records and contacting the referring physicians. CMR was considered to have a clinical impact when it resulted in (1) diagnostic consequences (ie, either a confirmation of a previously suspected diagnosis, such as a diagnosis of hypertrophic cardiomyopathy in patients referred for differential diagnosis of LV hypertrophy) or changing the current diagnosis (eg, diagnosis of active cardiac sarcoidosis in patient referred for ventricular arrhythmias); (2) therapeutic consequences, evaluated at a 6‐ to 12‐month follow‐up, ie, (1) change in medication; (2) ordering an invasive procedure; (3) hospital admission/discharge; or (4) ordering new testing because of the CMR findings. 10
Impact of Advanced Tissue Characterization
To assess the impact of advanced tissue characterization, the scans were processed as follows (Figure 2).
Figure 2. Assessment of advanced tissue characterization value.
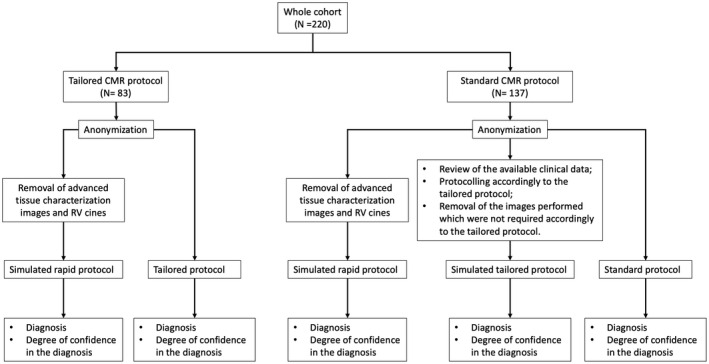
Scans in the tailored CMR group had been anonymized and reported twice (ie, with and without advanced tissue characterization). Scans in the control group (standard CMR protocol) had been anonymized and reported 3 times: (1) without any advanced tissue characterization image or RV cine images, simulating the rapid protocol of the INCA Peru Study 9 ; (2) with advanced tissue characterization and cine images accordingly to the tailored CMR approach; and (3) with all the original images. Each time, the reporting physician expressed a diagnosis and a degree of confidence in that diagnosis (poor, moderate, strong). CMR indicates cardiac magnetic resonance; and RV, right ventricle.
The tailored CMR scans were anonymized and reported twice, once in their original form and once excluding all advanced tissue characterization images and RV cines, according to the rapid scanning approach. The control group scans were anonymized and reported 3 times: (1) with all the sequences originally acquired as per the standard protocol; (2) with a set of sequence simulating the tailored CMR approach; and (3) excluding all advanced tissue characterization images and RV cines, simulating the rapid scanning approach.
C.T./S.C. and F.C. (2 cardiologists and a radiologist, all with >5 years CMR experience) acquired and read all the scans for clinical purposes. V.V./S.F. performed all the “research” reads. Neither V.V. nor S.F. took part in images acquisition/report for clinical purposes, because they did not work at Auxologico at the time of scanning. Scans were not randomized but at least 1 month passed between 1 read and the other. The order was as follows: (1) simulated rapid CMR (from both standard and tailored CMR); (2) tailored CMR (full set of images) and standard CMR (full set of images); and (3) simulated tailored CMR (from standard CMR). Simulated tailored CMR (from standard CMR) was read last because it was an additional read required during a revision. Between read 2 and 3, >3 months passed. V.V. and S.F. were blinded to the original acquisition (ie, if the scan was protocoled and acquired as a standard CMR or a tailored CMR) in all cases. They were made aware of the referral question and asked to make a diagnosis and express a degree of confidence in it (expressed as “poor,” “moderate,” and “strong”). Then, concordance in the diagnosis between the “clinical” and the “research” reports was assessed, along with changes in confidence related to the different protocols.
Statistical Analysis
Continuous variables are shown as means and SD or median and interquartile range for non‐normally distributed data, and categorical ones as absolute and relative frequencies. Comparisons of group‐specific means (medians) were performed by the t test (Wilcoxon test), whereas comparisons of group‐specific proportions were performed using the χ 2 or the Fisher test. Statistical significance was set at the 0.05 level. All P values were 2‐sided. All analyses were performed using the Statistical Analysis System Software (version 9.4; SAS Institute, Cary, NC).
Results
The study consisted of 222 patients, 85 in the tailored CMR group and 137 in the standard CMR group. Of the tailored CMR group, 2 were excluded because of scanner malfunction, leaving 83 patients.
Forty‐four patients (20%) were lost at follow‐up: 32 (23%) in the standard CMR group and 12 (14%) in the tailored CMR group.
Clinical indications for CMR were (1) suspected cardiomyopathy, myocarditis, and myocardial infarction with nonobstructed coronary arteries (n=128; 58%); (2) assessment of inducible ischemia and/or viability (n=43; 20%); (3) research scans in patients with Brugada syndrome and heart failure with preserved ejection fraction (n=30; 14%); (4) suspected athlete’s heart (n=9; 4%); and (5) other, including cardiac mass, iron overload, and family history of sudden cardiac death (n=10; 5%).
No statistically significant difference in the prevalence of each indication among the groups was observed (Table 1).
Table 1.
General Characteristics of the Experimental and Control Group
| Whole cohort (N=220) |
Standard CMR (N=137) |
Tailored CMR (N=83) |
P value | |
|---|---|---|---|---|
| Age, y median [IQR] | 57 [43–70] | 57 [44–68] | 56 [43–73] | 0.987* |
| Male N (%) | 138 (63%) | 89 (65%) | 49 (59%) | 0.378 † , ‡ |
| Scan type N (%): | ||||
| CMR | 151 (69%) | 100 (73%) | 51 (61%) | 0.074 † , ‡ |
| Stress‐CMR | 69 (31%) | 37 (27%) | 32 (39%) | |
| First scan | 212 (96%) | 132 (96%) | 80 (96%) | 1.000 § |
| Follow up scan | 8 (4%) | 5 (4%) | 3 (4%) | |
| Arrhythmia N (13%) | 29 (13%) | 21 (15%) | 8 (10%) | 0.227 † , ‡ |
|
Duration, min, median [IQR] |
39 [31–47] | 45 [39–50] | 30 [27–34] | <0.0001* |
|
CMR, min |
38 [30–46] N=151 |
43 [38–49] N=100 |
28 [24–30] N=51 |
<0.0001* |
|
Stress‐CMR, min |
41 [34–48] N=69 |
48 [42–56] N=37 |
33 [30–36] N=32 |
<0.0001* |
| Quality N (%) | ||||
| Poor | 2 (1%) | 1 (0.73%) | 1 (1%) | 0.842 § |
| Moderate | 53 (24%) | 35 (26%) | 18 (22%) | |
| Good | 164 (75%) | 101 (74%) | 63 (77%) | |
| Primary indication N (%) | ||||
| Cardiomyopathy/myocarditis | 128 (58%) | 86 (63%) | 42 (51%) | 0.169 § |
| Inducible ischemia | 31 (14%) | 17 (12%) | 14 (17%) | |
| Myocardial viability | 12 (5%) | 8 (6%) | 4 (5%) | |
| Research scans | 30 (14%) | 14 (10%) | 16 (19%) | |
| Athlete’s heart | 9 (4%) | 4 (3%) | 5 (6%) | |
| Other | 10 (5%) | 8 (6%) | 2 (2%) | |
| Impact of CMR ‖ N(%) | ||||
| Total (lost to FU) | 190 (44) | 123 (32) | 67 (12) | |
| No. | 146 | 91 | 55 | |
| New diagnosis | 36 (25%) | 20 (22%) | 16 (29%) | |
| New unexpected diagnosis | 1 (<1%) | 0 | 1 (2%) | |
| Therapeutic consequences | ||||
| Change in medication | 20 (14%) | 16 (18%) | 4 (7%) | |
| Invasive procedure/surgery | 27 (18%) | 16 (18%) | 11 (20%) | |
| Ordering of new tests | 3 (2%) | 1 (1%) | 2 (4%) | |
| CMR impact N (%) | 87 (60%) | 53 (58%) | 34 (62%) | |
| Impact of advanced tissue characterization ¶ N (%) |
N=160 (73%) |
N=104 (76%) |
N=56 (67%) |
|
| Increased diagnosis confidence | 73 (45%) | 47 (45%) | 25 (45%) | |
| Unchanged diagnosis confidence | 87 (55%) | 57 (55%) | 31 (55%) | |
Scan duration was calculated from first to last image timestamp. Quality grading: poor (inadequate to answer the clinical question); moderate (presence of artifact not significantly affecting diagnostic performance); good (optimal). Data are expressed as [IQR], N (%), Mean (SD). CMR indicates Cardiac Magnetic Resonance; IQR, Interquartile range; n.s., non‐significant; SD, Standard Deviation; and Stress‐CMR, first‐pass stress perfusion CMR.
Wilcoxon test.
Chi‐square test.
T test.
Fisher test.
Excluding research scans.
Impact of advanced tissue characterization refers to the increase in diagnosis confidence between scans with and without advanced tissue characterization.
Quality Grading
Among the 220 scans included in the study, 218 (99%) were of diagnostic quality, with 164 graded as of good quality (75%). Arrhythmias and poor breath‐holding accounted for most of the 53 moderate quality scans (n=27: arrhythmic patients; n=14: poor breath‐holding).
There were no statistically significant differences between the tailored and the standard CMR scan groups in term of images quality (Table 1).
CMR Duration
The median scan time duration in the tailored CMR group was 28 (24–30) minutes for CMR (minimum and maximum duration: 18 and 43 minutes) and 33 (30–36) minutes for stress‐CMR (minimum and maximum duration: 26 and 48 minutes). The median scan time duration in the standard CMR group was 43 (38–49) minutes for CMR (minimum and maximum duration: 15 and 64 minutes) and 48 (42–56) minutes for stress‐CMR (minimum and maximum duration: 37 and 85 minutes). Compared with the standard CMR group, statistically significant reductions in the average scan duration of 34% in CMR and 33% in stress‐CMR were observed (Table 1).
Impact of CMR
Considering only patients for whom follow‐up data were available, CMR results changed patient management in 62/105 (59%) patients undergoing standard CMR and 38/71 (54%) patients undergoing tailored CMR: new clinical diagnosis in 21/105 (20%) patients undergoing standard CMR and 17/71 (24%) patients undergoing tailored CMR; therapeutic implication in 43/105 (40%) patients undergoing standard CMR and 22/71 (31%) patients undergoing tailored CMR (Table S2).
Considering only patients for whom follow‐up data were available, and excluding research scan, CMR results changed patient management in 53/91 (58%) patients undergoing standard CMR and 34/55 (62%) patients undergoing tailored CMR: new clinical diagnosis in 20/91 (22%) patients undergoing standard CMR and 17/55 (31%) patients undergoing tailored CMR; therapeutic implication in 33/91 (37%) patients undergoing standard CMR and 17/55 (31%) patients undergoing tailored CMR (Table 1). The extent of the clinical impact of CMR was similar in patients who underwent the tailored and the standard CMR scan protocol.
Impact of Advanced Tissue Characterization
Native T1 maps and extracellular volume were acquired in all patients. Additional advanced tissue characterization and cine were performed globally in 160 patients (70%): 104 patients (76%) in the standard CMR group and 56 (67%) in the tailored CMR group, respectively (P=0.20). There was consensus on all diagnoses reached. Advanced tissue characterization increased the confidence degree in the diagnosis in 45% of cases. This percentage was similar both as reported by the operators who issued the clinical reports and those who performed the second read (Table 1). Also, we noted no statistically significant differences in confidence in diagnosis between the simulated tailored CMR and the standard CMR (Table S3).
Discussion
This study is a proof‐of‐concept exploring the feasibility and accuracy of a question‐driven CMR scan protocol, comprehensive of advanced tissue characterization, to evaluate adult cardiomyopathies or viability in <30 minutes, and the presence of inducible ischemia in <35 minutes.
Reducing scan times is a priority for the CMR community. Rapid CMR protocols have been pioneered in low‐middle income countries where the main issue is CMR sustainability for health care systems. In high resource settings, where the needs are similar but less explicit, and may focus on accessibility, cost, and patient comfort in decision making between competing modalities, rapid CMR diffusion is still limited. Indeed, available abbreviated protocols are either designed to assess a single disease with focused, dedicated sequences, and thus lack transferability to other cardiac conditions, or are designed to assess a broad range of diseases using a minimal set of sequences, and thus may miss information. 4 , 6 , 7 , 9
With our study, we demonstrated that careful sequence selections based on clinical need, rather than a “one‐size‐fits‐all” approach, allows performance of guideline‐compliant advanced tissue characterization 12 in a workflow‐optimized protocol, reducing scanning time by >30% compared with standard scanning time.
We also demonstrated that advanced tissue characterization, as targeted here, strengthened the confidence in diagnosis in >45% of cases, and thus is worth performing. Finally, the data show that CMR impact in our cohort, defined as CMR‐driven changes in diagnosis and management, was similar to that reported in international registries. 10 Compared with previous experiences in the Low‐Middle Income Countries, 9 we observed a lower number of unexpected diagnosis and a higher number of invasive procedures/heart surgery led by the CMR results. These differences are likely because of the different health care accessibility in Italy versus Low‐Middle Income Countries.
The results, both in terms of added value of advanced tissue characterization and impact of CMR, are similar in the standard CMR group and in the tailored CMR group, suggesting that, in patients with cardiomyopathies and in those undergoing stress‐CMR, the accuracy was unaffected by the sequences selection (ie, the reduction in scan times comes at no cost in terms of diagnostic performance).
Following the data collection, the routine application of these tailored protocols has significantly impacted our practice. We have been able to increase the scans volume by 10% (with another 10% increase planned with the ease of pandemic‐related safety measures), and to dedicate an average of 5 minutes/patient to research images acquisition. Indeed, the time needed to review patients’ medical records and to select additional images does not significantly affect the workflow: protocoling only requires a few minutes (although we did not quantify it), and all activities are carried out by the usual medical staff and clinical reports signed within the day.
Study limitations include that we used state‐of‐the‐art pulse sequences made available by the National Institutes of Health and Siemens Healthineers through research agreements. These were used primarily to increase image diagnostic performance rather than save time, although they will have reduced the need for repeat sequences in some cases. 15 We also acknowledge that our protocol requires significant expertise in clinical cardiology to identify the minimal effective sequences set. Since our study is monocentric, and the pandemic prevented us from acquiring concurrent controls, future research should include tailored CMR testing in other centers. Also, there was a high dropout rate, especially in the control group scans. Finally, the sample size was inadequate to assess the individual contribution of different advanced tissue characterization sequences.
Conclusions
There was a need for higher throughput, which was driven by COVID‐19 service pressures. By means of workflow optimization and selective sequence choices, we show that tailored CMR including stress and full tissue characterization as needed can fully answer clinical questions yet reduce average scan duration >30% for the key referral indications of cardiomyopathy and ischemic heart disease. This has wide potential benefits for global CMR delivery.
Sources of Funding
None.
Disclosures
None.
Supporting information
Tables S1–S3
Figure S1
For Sources of Funding and Disclosures, see page 7.
References
- 1. Leiner T, Bogaert J, Friedrich MG, Mohiaddin R, Muthurangu V, Myerson S, Powell AJ, Raman SV, Pennell DJ. SCMR Position Paper (2020) on clinical indications for cardiovascular magnetic resonance. J Cardiovasc Magn Reson. 2020;2020:22. doi: 10.1186/s12968-020-00682-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nagel E, Greenwood JP, McCann GP, Bettencourt N, Shah AM, Hussain ST, Perera D, Plein S, Bucciarelli‐Ducci C, Paul M, et al. Magnetic resonance perfusion or fractional flow reserve in coronary disease. N Engl J Med. 2019;380:2418–2428. doi: 10.1056/NEJMoa1716734 [DOI] [PubMed] [Google Scholar]
- 3. Schwitter J, Wacker CM, Wilke N, Al‐Saadi N, Sauer E, Huettle K, Schönberg SO, Luchner A, Strohm O, Ahlstrom H, et al. MR‐IMPACT II: Magnetic Resonance Imaging for Myocardial Perfusion Assessment in Coronary artery disease Trial: perfusion‐cardiac magnetic resonance vs. single‐photon emission computed tomography for the detection of coronary artery disease: a comparative multicentre, multivendor trial. Eur Heart J. 2013;34:775–781. doi: 10.1093/eurheartj/ehs022 [DOI] [PubMed] [Google Scholar]
- 4. Abdel‐Gadir A, Vorasettakarnkij Y, Ngamkasem H, Nordin S, Ako EA, Tumkosit M, Sucharitchan P, Uaprasert N, Kellman P, Piechnik SK, et al. Ultrafast magnetic resonance imaging for iron quantification in thalassemia participants in the developing world: the TIC‐TOC Study (Thailand and UK International Collaboration in Thalassaemia Optimising Ultrafast CMR). Circulation. 2016;134:432–434. doi: 10.1161/CIRCULATIONAHA.116.022803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Fernandes JL, Siqueira MHA, Nobrega de Oliveira KT, Avila LF, Gottlieb I, Lopes MU, Fernandes AM, Strecker R, Greiser A. Use of an accelerated protocol for rapid analysis of iron overload in the heart and liver: the All Iron Detected (AID) Multicenter Study. J Cardiovasc Magn Reson. 2015;17:O62. doi: 10.1186/1532-429X-17-S1-O62 [DOI] [Google Scholar]
- 6. Galea N, Catapano F, Marchitelli L, Cundari G, Maestrini V, Panebianco V, Mancone M, Fedele F, Catalano C, Francone M. How to perform a cardio‐thoracic magnetic resonance imaging in COVID‐19: comprehensive assessment of heart, pulmonary arteries, and lung parenchyma. Eur Heart J ‐ Cardiovasc Imaging. 2020;22:728–731. doi: 10.1093/ehjci/jeaa335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Hendel RC, Friedrich MG, Schulz‐Menger J, Zemmrich C, Bengel F, Berman DS, Camici PG, Flamm SD, Le Guludec D, Kim R, et al. CMR first‐pass perfusion for suspected inducible myocardial ischemia. JACC Cardiovasc Imaging. 2016;9:1338–1348. doi: 10.1016/j.jcmg.2016.09.010 [DOI] [PubMed] [Google Scholar]
- 8. Foley JRJ, Richmond C, Fent GJ, Bissell M, Levelt E, Dall’armellina E, Swoboda PP, Plein S, Greenwood JP. Rapid Cardiovascular Magnetic Resonance for Ischemic Heart Disease Investigation (RAPID‐IHD). JACC Cardiovasc Imaging. 2020;13:1632–1634. doi: 10.1016/j.jcmg.2020.01.029 [DOI] [PubMed] [Google Scholar]
- 9. Menacho K, Ramirez S, Segura P, Nordin S, Abdel‐Gadir A, Illatopa V, Bhuva A, Benedetti G, Boubertakh R, Abad P, et al. INCA (Peru) Study: impact of non‐invasive cardiac magnetic resonance assessment in the developing world. J Am Heart Assoc. 2018;7:e008981. doi: 10.1161/JAHA.118.008981 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Bruder O, Wagner A, Lombardi M, Schwitter J, van Rossum A, Pilz G, Nothnagel D, Steen H, Petersen S, Nagel E, et al. European Cardiovascular Magnetic Resonance (EuroCMR) registry–multinational results from 57 centers in 15 countries. J Cardiovasc Magn Reson. 2013;15:9. doi: 10.1186/1532-429X-15-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Kramer CM. Potential for rapid and cost‐effective cardiac magnetic resonance in the developing (and Developed) World. J Am Heart Assoc. 2018;7:e010435. doi: 10.1161/JAHA.118.010435 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Kramer CM, Barkhausen J, Bucciarelli‐Ducci C, Flamm SD, Kim RJ, Nagel E. Standardized cardiovascular magnetic resonance imaging (CMR) protocols: 2020 update. J Cardiovasc Magn Reson. 2020;2020:22. doi: 10.1186/s12968-020-00607-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Tamis‐Holland JE, Jneid H, Reynolds HR, Agewall S, Brilakis ES, Brown TM, Lerman A, Cushman M, Kumbhani DJ, Arslanian‐Engoren C, et al. Contemporary diagnosis and management of patients with myocardial infarction in the absence of obstructive coronary artery disease: a scientific statement from the American Heart Association. Circulation. 2019;139:e891–e908. doi: 10.1161/CIR.0000000000000670 [DOI] [PubMed] [Google Scholar]
- 14. Kellman P, Hansen MS, Nielles‐Vallespin S, Nickander J, Themudo R, Ugander M, Xue H. Myocardial perfusion cardiovascular magnetic resonance: optimized dual sequence and reconstruction for quantification. J Cardiovasc Magn Reson. 2017;19:43. doi: 10.1186/s12968-017-0355-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Captur G, Lobascio I, Ye Y, Culotta V, Boubertakh R, Xue H, Kellman P, Moon JC. Motion‐corrected free‐breathing LGE delivers high quality imaging and reduces scan time by half: an independent validation study. Int J Cardiovasc Imaging. 2019;35:1893–1901. doi: 10.1007/s10554-019-01620-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kellman P, Hernando D, Shah S, Zuehlsdorff S, Jerecic R, Mancini C, Liang Z‐P, Arai AE. Multiecho dixon fat and water separation method for detecting fibrofatty infiltration in the myocardium. Magn Reson Med. 2009;61:215–221. doi: 10.1002/mrm.21657 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S3
Figure S1


