Abstract
Background
Objective markers of cardiac function are limited in the outpatient setting and may be beneficial for monitoring patients with chronic cardiac conditions. We assess the accuracy of a scale, with the ability to capture ballistocardiography, electrocardiography, and impedance plethysmography signals from a patient’s feet while standing on the scale, in measuring stroke volume and cardiac output compared with the gold‐standard direct Fick method.
Methods and Results
Thirty‐two patients with unexplained dyspnea undergoing level 3 invasive cardiopulmonary exercise test at a tertiary medical center were included in the final analysis. We obtained scale and direct Fick measurements of stroke volume and cardiac output before and immediately after invasive cardiopulmonary exercise test. Stroke volume and cardiac output from a cardiac scale and the direct Fick method correlated with r=0.81 and r=0.85, respectively (P<0.001 each). The mean absolute error of the scale estimated stroke volume was −1.58 mL, with a 95% limits of agreement of −21.97 to 18.81 mL. The mean error for the scale estimated cardiac output was −0.31 L/min, with a 95% limits of agreement of −2.62 to 2.00 L/min. The changes in stroke volume and cardiac output before and after exercise were 78.9% and 96.7% concordant, respectively, between the 2 measuring methods.
Conclusions
In a proof‐of‐concept study, this novel scale with cardiac monitoring abilities may allow for noninvasive, longitudinal measures of cardiac function. Using the widely accepted form factor of a bathroom scale, this method of monitoring can be easily integrated into a patient’s lifestyle.
Keywords: digital health, exercise testing, heart failure, hemodynamics, intelligence, machine learning and artificial
Subject Categories: Exercise Testing, Machine Learning
Nonstandard Abbreviations and Acronyms
- bpm
beats per minute
- iCPET
invasive cardiopulmonary exercise test
- IPG
impedance plethysmography
- LOA
limits of agreement
- PE
percentage error
Clinical Perspective
What Is New?
This study demonstrates the feasibility of a novel connected cardiac scale to approximate stroke volume and cardiac output compared with the direct Fick method.
What Are the Clinical Implications?
This technology has the potential to be deployed in the home setting to easily and longitudinally monitor hemodynamic status.
Cardiovascular disease, in particular heart failure, is a major health and economic problem worldwide, expected to increase in incidence and prevalence because of the aging population and an increase in comorbidities. 1 , 2 Novel approaches for easily monitoring cardiac function trends over time in the home environment may prove to be important in dealing with these conditions. Accelerated by the COVID‐19 pandemic, the field of medicine is increasingly shifting toward telemedicine and remote patient monitoring, welcoming innovation. 3 , 4 In this study, we investigate the accuracy of a connected cardiac scale with ballistocardiography, impedance plethysmography (IPG), and electrocardiography sensors in measuring stroke volume and cardiac output compared with the direct Fick method.
Ballistocardiography measures the effects of the cyclical hemodynamic forces transmitted from the heart with each cardiac systolic ejection. 5 The method for ballistocardiography was developed and popularized in the 1950s, but its use waned later in the century because of the impractical nature of the apparatus, limited reliability of the measurements in diseased states, and a focus on other measures of cardiovascular function, such as blood pressure recordings. 6 , 7 However, over the past decade, ballistocardiography has regained popularity as a result of the ability to obtain measurements from novel sensor platforms, such as bathroom scales, advances in data processing and machine learning algorithms, and the emergence of more rigorous studies demonstrating the utility of ballistocardiography recordings from patients with cardiac diseases. 8 , 9 , 10 IPG measures pulsatile blood flow via changes in electrical impedance. This measurement, along with electrocardiography, can identify important cardiac time intervals, such as valvular opening and closing, measures of contractility, such as left ventricular ejection time, and estimates for stroke volume and cardiac output. 11 The simultaneous extraction of electrocardiography, IPG, and ballistocardiography signals from a single scale measurement can enhance the amount of cardiovascular information obtained for any individual signal in isolation.
In this study, Bodyport Inc, a company based in San Francisco, CA, and the Brigham and Women’s Hospital collaborated to assess the accuracy of the Bodyport Cardiac Scale in noninvasively measuring stroke volume and cardiac output. The cardiac scale has the form of a bathroom scale and has a multisensor system that can capture single lead electrocardiography, IPG, and ballistocardiography signals when a patient stands on the scale (Figure 1). This study investigates the accuracy of this scale in measuring stroke volume and cardiac output compared with the gold‐standard direct Fick method from pulmonary arterial catheters.
Figure 1.
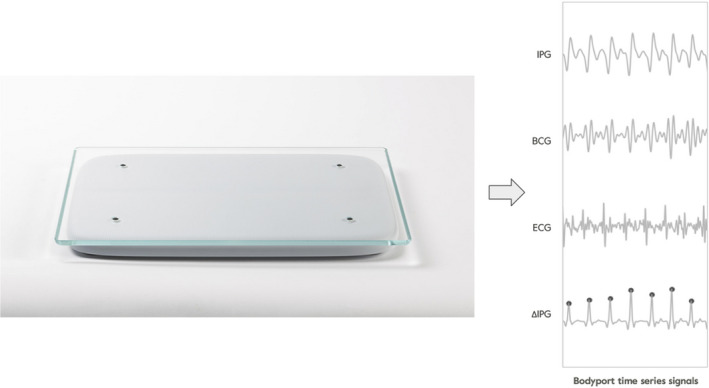
Image of the Bodyport Cardiac Scale (left) and example of scale‐derived signals for the impedance plethysmograph (IPG), ballistocardiograph (BCG), electrocardiograph (ECG), and derivative of the IPG (ΔIPG) (right).
METHODS
Subject Population
The data that support the findings of this study are available from the corresponding author on reasonable request. This research study was approved by the institutional review board at Brigham and Women’s Hospital. Fifty‐six subjects undergoing a level 3 invasive cardiopulmonary exercise test (iCPET) at the Shapiro Cardiovascular Center at Brigham and Women’s Hospital were recruited and consented between July 2018 and January 2019. The patients were each undergoing the iCPET to evaluate unexplained dyspnea. These patients had an array of underlying comorbidities, including heart failure, pulmonary artery hypertension, peripheral vasomotor abnormalities, valvular pathological conditions, and pulmonary diseases. The study was not designed to discriminate the accuracy of the cardiac output measurements dependent on the patient’s underlying medical condition. Of the 56 subjects enrolled in the study, 32 (9 men, 23 women) were included in the final analysis. Twenty‐four subjects were excluded from the final analysis. Among the 24 patients excluded, 11 experienced light‐headedness at the completion of the iCPET, making it unsafe for them to stand on the scale. Six subjects had missing or incorrect reference data because of instrumentation‐related issues (ie, patient pulled face mask off before Fick measurement completed). Seven patients had poor balance during the postexercise recovery measurement, requiring assistance from the clinical staff, which caused excessive motion artifacts, requiring exclusion of the data. The age range for participants was 26 to 78 years (mean, 51.7 years; SD, 14.5 years). Among the excluded participants, there were 8 men and 16 women, and the age range was 31 to 75 years (mean, 53.6 years; SD, 12.9 years).
Study Protocol
We obtained scale measurements before and immediately after the iCPET. Ultrasound‐guided pulmonary artery catheters were placed before patient arrival in the iCPET laboratory. Once in the iCPET laboratory, patients were asked to stand, and a baseline pulmonary artery measurement was obtained, followed immediately by a 2‐minute baseline measurement on the cardiac scale. Patients then mounted an upright cycle ergometer to perform the exercise portion of the test. The exercise workload was gradually increased in a ramped protocol until the patient reached exhaustion or developed objective evidence of hemodynamic instability or myocardial ischemia. After the exercise limit was reached, patients dismounted from the bicycle as quickly as possible to obtain a recovery pulmonary artery catheter measurement. This was immediately followed by a 2‐minute recovery cardiac scale measurement.
Direct Fick Measurements
The measurements obtained from the metabolic cart and radial and pulmonary artery catheters before and immediately after the iCPET study include ventilation, pulmonary gas exchange, venous and arterial blood gases, a 12‐lead electrocardiogram, heart rate, pulmonary artery pressure, and blood pressure from a radial artery catheter. Cardiac output was calculated using the direct Fick method as the current gold standard. Stroke volume was derived from its relationship with the measured cardiac output and heart rate.
Cardiac Scale Measurements
The Bodyport Cardiac Scale is a physical platform on which the patient stands with bare feet. Using embedded sensors, the scale measures 3 cardiovascular biosignals that are used to extract various cardiac biomarkers. The ballistocardiography, electrocardiography, and IPG signals are analyzed by Bodyport’s software and proprietary algorithms to extract characteristic features in each waveform that are used to estimate parameters, including heart rate, heart rate variability, cardiac time intervals, and signal morphological features used to derive estimates of stroke volume and cardiac output.
Signal Processing
The scale signals (ballistocardiography, electrocardiography, and IPG) were filtered and interpolated before feature extraction and model validation. Signal regions containing motion artifacts or excessive noise were objectively identified and removed. Motion artifacts and other sources of signal interference were detected through adaptive thresholding and monitoring of the patient’s center of pressure during the measurement. Linear phase and digital low‐pass and high‐pass filters were applied to the signals to prevent distortion. Cutoff frequencies were established for each signal (ballistocardiography, electrocardiography, and IPG) and ranged from 0.5 to 50 Hz. All 3 signals were simultaneously sampled at 250 Hz. Ensemble averaged waveforms were constructed from the real‐time signals. Signal processing calibration is not required on a per‐patient basis. The signal processing algorithms are fixed for all measurements.
Feature Identification, Extraction, and Selection
Feature identification and extraction methods were designed, developed, and validated on data collected from prior internal studies. These customized feature extraction methods were tailored for each feature of interest. The candidate feature set included time intervals and amplitudes obtained from time aligned ensemble averaged signals. Certain features were chosen on the basis of existing equations used in impedance cardiography and ballistocardiography, including those of Kubicek et al. The ballistocardiography J‐wave amplitude, which correlates with pulse pressure, along with additional proprietary electromechanical parameters from the ballistocardiography, electrocardiography, and IPG signals, specifically preejection period and left ventricular ejection time, were ultimately included in the final feature set. 5 Heart rate was used as a correction factor applied to time interval features. Additional noncardiovascular parameters collected directly from the scale, such as body weight and basal impedance, were also incorporated into the model to remove the need for calibration and compensate for individual anthropomorphic variability.
From the candidate features, the final stroke volume model features were selected using light gradient boosting machine. Light gradient boosting machine is a supervised tree‐based model that uses candidate features as inputs and the Fick derived stroke volume as the model output. It measures the relative importance of each candidate feature and removes the features of lower importance to arrive at the final feature set. 13
Stroke Volume Model Development and Training
Regression model training for stroke volume was accomplished using a tree‐based pipeline optimization tool. 14 This tool evaluates the performance of individual regression models, while optimizing hyperparameters. The following models were preselected to be used by tree‐based pipeline optimization tool: linear regression, lasso, elastic net, ridge, random forest, support vector regression, and multilayer perceptron. Feature preprocessors were also predefined to be included as part of the tree‐based pipeline optimization tool process. Tree‐based pipeline optimization tool iterates over combinations of models and preprocessors, as well as the hyperparameter space. Each trained model in this stage used 3‐fold cross‐validation, and the mean absolute error of the model was calculated. The final model was selected on the basis of the lowest mean absolute error of each evaluated model. The final model was an ensemble regression pipeline consisting of a random forest and gradient boosting regression.
Stroke Volume Model Validation and Cardiac Output Calculation
The accuracy of the selected multivariable regression model was evaluated using leave one out cross‐validation. This cross‐validation technique fits the model on all but one measurement, which is then used as the test measurement. Each measurement was held out once, and the final accuracy was determined on the basis of the performance of all held out test measurements. Bodyport‐derived heart rate and stroke volume were used to calculate an estimate of cardiac output using the relationship: cardiac output equals the product of heart rate and stroke volume.
Statistical Analysis
The P value for the correlation coefficients was calculated using the Wald test with t‐distribution of the test statistic. The Bland‐Altman limits of agreement analysis for the combined preexercise and postexercise data set accounted for the multiple measurements from the same subject using the method described by Bland and Altman. 15 We measured the degree of agreement between the cardiac scale and direct Fick methods after exercise by calculating their concordance. Concordance rate was calculated using each paired measurement for all subjects. A concordant pair is determined if the change in stroke volume or cardiac output (postexercise minus preexercise) for each of the measured value and the reference value was positive or negative. The number of subjects who are concordant divided by the total number of subjects was the final concordance rate. To reduce statistical noise from the analysis, we excluded data points (13 for stroke volume and 2 for cardiac output) where the change in stroke volume or cardiac output was <15% of the mean value in the study. 16
RESULTS
The multivariable regression model demonstrated a strong relationship between the scale and Fick‐derived estimates for stroke volume and cardiac output (Figure 2). The stroke volume in the preexercise analysis correlated with the Fick‐derived stroke volume with a coefficient of r=0.77 (P<0.001), mean error (bias) of −2.08 mL, SD of 10.65 mL, 95% limits of agreement (LOA) for the mean error of −22.95 to 18.79 mL, and percentage error (PE), defined as the 95% LOA divided by the average Fick‐derived stroke volume, of 39.14% (Table). In the postexercise analysis, the model had a correlation coefficient of r=0.84 (P<0.001), mean error of −1.09 mL, SD of 9.92 mL, 95% LOA of −20.53 to 18.35 mL, and PE of 33.66%. The combined preexercise and postexercise data set had a correlation coefficient of r=0.81 (P<0.001), mean error of −1.58 mL, SD of 10.30 mL, 95% LOA of −21.97 to 18.81 mL, and PE of 36.73%.
Figure 2. Left, Scatterplot with regression line for stroke volume (SV), measured by the scale and direct Fick method (64 data pairs; r=0.81); Right, Bland‐Altman analysis with mean error (bias) of −1.58 mL, 95% limits of agreement (LOA) of −21.97 to 18.81 mL, and percentage error (PE) of 36.73%.
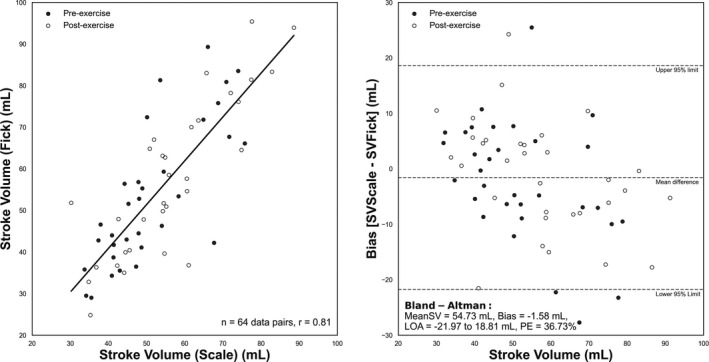
Preexercise data denoted with a black circle, and postexercise data denoted with a white circle. MeanSV indicates mean SV for combined scale and Fick measurements.
Table 1.
Summary Statistics and Accuracy Metrics for Scale Estimates of Stroke Volume and Cardiac Output Compared With the Direct Fick Method
| Variable | Scale measure, mean (range) | Fick measure, mean (range) | Correlation coefficient, r | Mean error (95% LOA) | % Error |
|---|---|---|---|---|---|
| Stroke volume, mL | |||||
| Preexercise | 51.23 (33.72 to 75.77) | 53.31 (29.0 to 89.3) | 0.77 | −2.08 (−22.95 to 18.79) | 39.14 |
| Postexercise | 56.65 (30.25 to 88.62) | 57.74 (24.8 to 95.4) | 0.84 | −1.09 (−20.53 to 18.35) | 33.66 |
| Combined | 53.94 (30.25 to 88.63) | 55.52 (24.8 to 95.4) | 0.81 | −1.58 (−21.97 to 18.81) | 36.73 |
| Cardiac output, L/min | |||||
| Preexercise | 4.39 (3.07 to 6.74) | 4.56 (2.77 to 8.13) | 0.70 | −0.17 (−1.97 to 1.63) | 39.52 |
| Postexercise | 6.20 (4.20 to 9.86) | 6.65 (3.45 to 13.07) | 0.83 | −0.45 (−3.11 to 2.20) | 39.89 |
| Combined | 5.29 (3.07 to 9.85) | 5.61 (2.77 to 13.07) | 0.85 | −0.31 (−2.62 to 2.00) | 41.18 |
Scale cardiac output is calculated from the product of scale‐derived heart rate and stroke volume, cardiac output=heart rate×stroke volume. Direct Fick stroke volume is calculated from the division of Fick‐derived cardiac output and heart rate, stroke volume=cardiac output/heart rate. LOA indicates limits of agreement.
Cardiac output was estimated using the scale‐derived stroke volume and heart rate. In the preexercise set, the correlation coefficient was r=0.70 (P<0.001) (Figure 3), mean error of −0.17 L/min, SD of 0.92 L/min, 95% LOA of −1.97 to 1.63 L/min, and PE of 39.52%. The postexercise set correlation coefficient was r=0.83 (P<0.001), mean error of −0.45 L/min, SD of 1.36 L/min, 95% LOA of −3.11 to 2.2 L/min, and PE of 39.89%. Combining the 2 sets yielded a correlation coefficient of r=0.85 (P<0.001), mean error of −0.31 L/min, SD of 0.98 L/min, 95% LOA of −2.62 to 2.00 L/min, and PE of 41.18%.
Figure 3. Left, Scatterplot with regression line for cardiac output (CO), measured by the scale and direct Fick method (64 data pairs; r=0.85); Right, Bland‐Altman analysis with mean error (bias) of −0.31 mL, 95% limits of agreement (LOA) of −2.62 to 2.00 L/min, and percentage error (PE) of 41.18%.
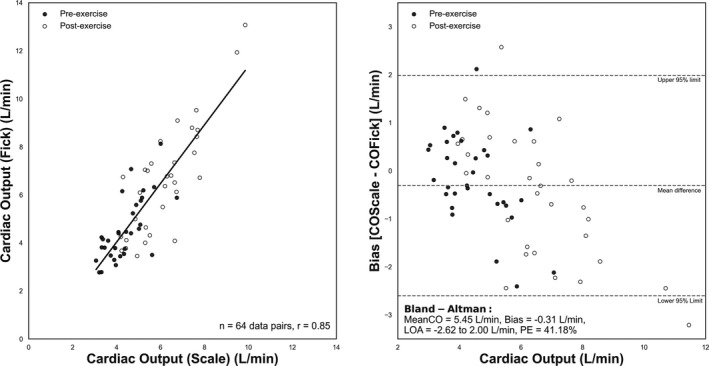
Preexercise data denoted with a black circle, and postexercise data denoted with a white circle. MeanCO indicates mean CO for combined scale and Fick measurements.
The change in stroke volume and cardiac output was evaluated preexercise and postexercise test for both the scale‐derived and Fick methods, to assess if the scale can trend directional changes in these perfusion markers. We measured the degree of agreement between these 2 methods by calculating their concordance: the fraction of patients for which the changes in stroke volume or cardiac output (postexercise minus preexercise) were either both positive or negative using both modalities. The concordances for stroke volume and cardiac output were 78.9% and 96.7%, respectively (P<0.001, each, derived from the concordance correlation) (Figure 4). To reduce statistical noise from the analysis, we excluded data points (13 for stroke volume and 2 for cardiac output) where the change in stroke volume or cardiac output was <15% of the mean value in the study. 16
Figure 4. Concordance plot.
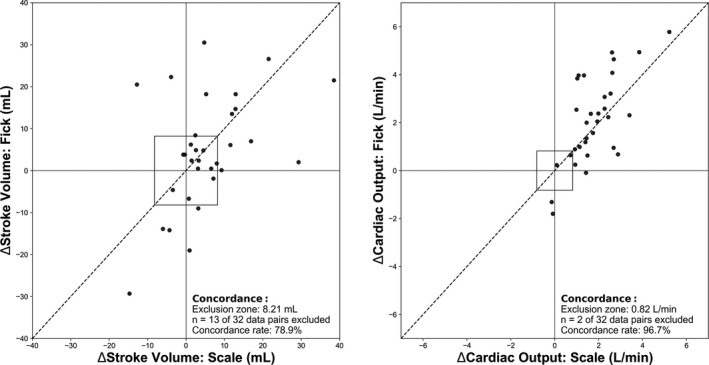
Left: Change in stroke volume postexercise minus preexercise from the scale vs the direct Fick method. Right: Similar plot for cardiac output. A central exclusion zone (square) represents the data within 15% of the mean stroke volume or cardiac output in the study, as they contain a high level of random variation compared with changes in the cardiac output. The line of identity y=x is shown.
After exercise, the average cardiac output increased by 1.81 L/min when measured by the scale (4.39 L/min preexercise to 6.20 L/min postexercise), and by 2.09 L/min (from 4.56 to 6.65 L/min) when measured by the Fick method. The heart rate increased by an average of 24 beats per minute (bpm) (88 bpm preexercise to 112 bpm postexercise) on the scale, and 40 bpm (76 bpm preexercise to 116 bpm postexercise) for the Fick measurement. The stroke volume increased by an average of 5.24 mL (51.23 mL preexercise to 56.65 mL postexercise) on the scale and 4.43 mL (53.31 mL preexercise to 57.74 mL postexercise) using the Fick method.
DISCUSSION
Principal Findings
The results demonstrate a strong relationship between the cardiac scale and direct Fick estimates for stroke volume and cardiac output. The correlation persisted through a dynamic range of stroke volumes (30–90 mL) and cardiac outputs preexercise and postexercise (3–10 L/min). A recent meta‐analysis comparing noninvasive measures of cardiac output, including pulse wave transit time, noninvasive pulse contour analysis, thoracic bioimpedance, and CO2 rebreathing with bolus thermodilution, reported a pooled mean error of −0.13 L/min, 95% LOA of ±2.23 L/min, and PE of 47%, which compares similarly to our findings of a mean error of −0.31 L/min, 95% LOA of ±2.31 L/min, and PE of 42% 17 , 18 One of the potential advantages of the scale is to provide longitudinal measures of cardiac output in the home setting, not to entirely replace the “gold‐standard” catheterization laboratory measurement. The ability to track longitudinal measurements needs to be evaluated in future studies.
The stroke volume and cardiac output concordances before and immediately after exercise were 78.9% and 96.7%, respectively. Current advice for trending ability in cardiac output studies is a concordance >92%, which is achieved in this cardiac output analysis but not the stroke volume. 19 The increased concordance for the cardiac output is likely a result of an increased heart rate postexercise, compared with the more variable response seen in the stroke volume. Because exercise is incorporated in the iCPET, cardiac output is expected to increase. This is why most of the data points fall in the upper right corner of the cardiac output concordance plot (Figure 4). Another experimental design is necessary to better detect reductions in cardiac output.
Having all sensors integrated in one device is imperative for the future adoption of such a technology, because applying multiple sensor technologies simultaneously is cumbersome and would likely yield low patient adherence. The analysis of these orthogonal sensor signals is further enhanced by ongoing advancements in signal processing and machine learning techniques. Using the form factor of a bathroom scale will also enhance patient adherence, because taking scale measurements is a behavior already adapted by many patients, especially those with cardiac conditions, such as heart failure.
A noninvasive, scalable, and inexpensive method for assessing cardiac function could have widespread applications in medicine. Robust estimates of stroke volume and cardiac output may help monitor the cardiac performance of patients with chronic conditions, such as heart failure, and facilitate early detection of decompensation and the virtual titration of goal‐directed medical therapy. Given the simplicity of use and existing user behaviors for self‐weighing on a scale, longitudinal data can be obtained and trended in large populations to identify novel biomarkers of cardiovascular health.
Limitations
This proof‐of‐concept study was not designed or powered to measure changes in cardiac output in relation to the patients’ underlying medical conditions. The 95% LOA in cardiac output during the postexercise phase was up to 3 L/min. This is partially accounted for by the 2‐minute time delay between the Fick and scale measurements, allowing interval cardiac recovery. There was a decrease in postexercise heart rate by an average of 16 bpm between the Fick and scale measurements, whereas the stroke volume only decreased by an average of 1.09 mL. With an average stroke volume of 57.74 mL in the postexercise Fick subgroup, a decrease in heart rate by 16 bpm would reduce the cardiac output by 0.92 L, supporting a postexercise cardiac output 95% LOA closer to 2 L/min, similar to that seen in the preexercise analysis. Additional sources of error include patient balance post exertion, the study’s limited sample size, and intrinsic errors of both the direct Fick measurement and scale technology.
A negative trend in the bias with larger stroke volumes and cardiac outputs is observed in Figures 2 and 3. The trend in bias for cardiac output is partially accounted for by a larger postexercise decrease in heart rate in patients with higher cardiac outputs. However, this does not account for the negative trend in the stroke volume bias. Additional data from future studies and continued development of the mathematical model may potentially help correct for this trend in bias.
The exclusion of patients in this study was largely because of unstable hemodynamics (hypotension), symptomatic factors during testing (dizziness and poor balance), and incomplete reference measurements. The application of this scale in its normal use, a stable, nonstress setting, such as the patient’s home, would mitigate these factors.
CONCLUSIONS
This study highlights how enhancements in technology have allowed for the integration of ballistocardiography, electrocardiography, and IPG sensors into form factors (eg, a weight scale creating novel methods for assessing cardiac function). We observed strong correlations between scale‐derived and Fick‐derived estimates of stroke volume and cardiac output, with r=0.81 and 0.85, respectively. The mean errors of the scale estimates for stroke volume and cardiac output were relatively accurate at −1.58 mL (range, −21.97 to 18.81 mL) and −0.31 L/min (range, −2.62 to 2.00 L/min), respectively. The scale and direct Fick estimates for cardiac output were strongly concordant preexercise and postexercise at 96.7%, demonstrating the ability for scale to trend increases in cardiac output. Future studies will gather additional data to improve the model and will also assess longitudinal scale measurements from individuals in clinical settings to better understand how these biomarkers, when integrated, can be used to assess relevant changes in a range of disorders.
Sources of Funding
None.
Disclosures
Dr Yazdi and S. Patel are employees at Bodyport Inc. S. Smith and C. Centen are founders of Bodyport Inc. Dr MacRae is an advisor for Bodyport Inc. The remaining authors have no disclosures to report.
Acknowledgments
We would like to thank the staff of the Brigham and Women’s Hospital cardiopulmonary exercise laboratory for helping collect the data. Scales were provided by Bodyport Inc.
For Sources of Funding and Disclosures, see page 8.
REFERENCES
- 1. Ambrosy AP, Fonarow GC, Butler J, Chioncel O, Greene SJ, Vaduganathan M, Nodari S, Lam CSP, Sato N, Shah AN, et al. The global health and economic burden of hospitalizations for heart failure: lessons learned from hospitalized heart failure registries. J Am Coll Cardiol. 2014;63:1123–1133. doi: 10.1016/j.jacc.2013.11.053 [DOI] [PubMed] [Google Scholar]
- 2. Conrad N, Judge A, Tran J, Mohseni H, Hedgecott D, Crespillo AP, Allison M, Hemingway H, Cleland JG, McMurray JJV, et al. Temporal trends and patterns in heart failure incidence: a population‐based study of 4 million individuals. Lancet. 2018;391:572–580. doi: 10.1016/S0140-6736(17)32520-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Shachar C, Engel J, Elwyn G. Implications for telehealth in a postpandemic future: regulatory and privacy issues. JAMA. 2020;323:2375–2376. doi: 10.1001/jama.2020.7943 [DOI] [PubMed] [Google Scholar]
- 4. Kelly SA, Schesing KB, Thibodeau JT, Ayers CR, Drazner MH. Feasibility of remote video assessment of jugular venous pressure and implications for telehealth. JAMA Cardiol. 2020;5:1194–1195. doi: 10.1001/jamacardio.2020.2339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Kim C‐S, Ober SL, McMurtry MS, Finegan BA, Inan OT, Mukkamala R, Hahn J‐O. Ballistocardiogram: mechanism and potential for unobtrusive cardiovascular health monitoring. Sci Rep. 2016;6:31297. doi: 10.1038/srep31297 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Eddleman EE Jr, Harrison WK, Jackson DH, Taylor HL. A critical appraisal of ballistocardiography. Am J Cardiol. 1972;29:120–122. doi: 10.1016/0002-9149(72)90427-4 [DOI] [PubMed] [Google Scholar]
- 7. Starr I. Essay on the ballistocardiogram. J Am Med Assoc. 1954;155:1413–1425. doi: 10.1001/jama.1954.73690340011009 [DOI] [PubMed] [Google Scholar]
- 8. Inan OT, Migeotte P‐F, Park K‐S, Etemadi M, Tavakolian K, Casanella R, Zanetti J, Tank J, Funtova I, Prisk GK, et al. Ballistocardiography and seismocardiography: a review of recent advances. IEEE J Biomed Health Inform. 2015;19:1414–1427. doi: 10.1109/JBHI.2014.2361732 [DOI] [PubMed] [Google Scholar]
- 9. Giovangrandi L, Inan OT, Banerjee D, Kovacs GTA. Preliminary results from BCG and ECG measurements in the heart failure clinic. Conf Proc IEEE Eng Med Biol Soc. 2012;2012:3780–3783. [DOI] [PubMed] [Google Scholar]
- 10. Inan OT, Etemadi M, Paloma A, Giovangrandi L, Kovacs GTA. Non‐invasive cardiac output trending during exercise recovery on a bathroom‐scale‐based ballistocardiograph. Physiol Meas. 2009;30:261–274. doi: 10.1088/0967-3334/30/3/003 [DOI] [PubMed] [Google Scholar]
- 11. Strobeck JE, Silver MA. Beyond the four quadrants: the critical and emerging role of impedance cardiography in heart failure. Congest Heart Fail. 2004;10:1–6. doi: 10.1111/j.1527-5299.2004.03405.x [DOI] [PubMed] [Google Scholar]
- 12. Kubicek WG, Kottke J, Ramos MU, Patterson RP, Witsoe DA, Labree JW, Remole W, Layman TE, Schoening H, Garamela JT. The Minnesota impedance cardiograph‐ theory and applications. Biomed Eng. 1974;9:410–416. [PubMed] [Google Scholar]
- 13. Al DE. Comparison between XGBoost, LightGBM and CatBoost using a home credit dataset. Int J Comput Inf Eng. 2019;13:6–10. [Google Scholar]
- 14. Le TT, Fu W, Moore JH. Scaling tree‐based automated machine learning to biomedical big data with a feature set selector. Bioinformatics. 2020;36:250–256. doi: 10.1093/bioinformatics/btz470 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Bland JM, Altman DG. Agreement between methods of measurement with multiple observations per individual. J Biopharm Stat. 2007;17:571–582. doi: 10.1080/10543400701329422 [DOI] [PubMed] [Google Scholar]
- 16. Perrino AC Jr, O’Connor T, Luther M. Transtracheal Doppler cardiac output monitoring: comparison to thermodilution during noncardiac surgery. Anesth Analg. 1994;78:1060–1066. doi: 10.1213/00000539-199406000-00005 [DOI] [PubMed] [Google Scholar]
- 17. Joosten A, Desebbe O, Suehiro K, Murphy L‐L, Essiet M, Alexander B, Fischer M‐O, Barvais L, Van Obbergh L, Maucort‐Boulch D, et al. Accuracy and precision of non‐invasive cardiac output monitoring devices in perioperative medicine: a systematic review and meta‐analysis†. Br J Anaesth. 2017;118:298–310. doi: 10.1093/bja/aew461 [DOI] [PubMed] [Google Scholar]
- 18. Opotowsky AR, Hess E, Maron BA, Brittain EL, Barón AE, Maddox TM, Alshawabkeh LI, Wertheim BM, Xu M, Assad TR, et al. Thermodilution vs estimated Fick cardiac output measurement in clinical practice: an analysis of mortality from the Veterans Affairs Clinical Assessment, Reporting, and Tracking (VA CART) Program and Vanderbilt University. JAMA Cardiol. 2017;2:1090–1099. doi: 10.1001/jamacardio.2017.2945 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Critchley LA, Lee A, Ho AM‐H. A critical review of the ability of continuous cardiac output monitors to measure trends in cardiac output. Anesth Analg. 2010;111:1180–1192. doi: 10.1213/ANE.0b013e3181f08a5b [DOI] [PubMed] [Google Scholar]


