Abstract
Background
Magnesium supplements may have beneficial effects on arterial stiffness. Yet, to our knowledge, no head‐to‐head comparison between various magnesium formulations in terms of effects on arterial stiffness has been performed. We assessed the effects of magnesium citrate supplementation on arterial stiffness and blood pressure and explored whether other formulations of magnesium have similar effects.
Methods and Results
In this randomized trial, subjects who were overweight and slightly obese received either magnesium citrate, magnesium oxide, magnesium sulfate, or placebo for 24 weeks. The total daily dose of magnesium was 450 mg/d. The primary outcome was carotid‐to‐femoral pulse wave velocity, which is the gold standard method for measuring arterial stiffness. Secondary outcomes included blood pressure and plasma and urine magnesium. Overall, 164 participants (mean±SD age, 63.2±6.8 years; 104 [63.4%] women) were included. In the intention‐to‐treat analysis, neither magnesium citrate nor the other formulations had an effect on carotid‐to‐femoral pulse wave velocity or blood pressure at 24 weeks compared with placebo. Magnesium citrate increased plasma (+0.04 mmol/L; 95% CI, +0.02 to +0.06 mmol/L) and urine magnesium (+3.12 mmol/24 h; 95% CI, +2.23 to +4.01 mmol/24 h) compared with placebo. Effects on plasma magnesium were similar among the magnesium supplementation groups, but magnesium citrate led to a more pronounced increase in 24‐hour urinary magnesium excretion than magnesium oxide or magnesium sulfate. One serious adverse event was reported, which was considered unrelated to the study treatment.
Conclusions
Oral magnesium citrate supplementation for 24 weeks did not significantly change arterial stiffness or blood pressure. Magnesium oxide and magnesium sulfate had similar nonsignificant effects.
Registration
URL: https://www.clinicaltrials.gov; Unique identifier: NCT03632590.
Keywords: arterial stiffness, blood pressure, intervention study, magnesium, pulse wave velocity, supplementation
Subject Categories: Cardiovascular Disease, Obesity, Diet and Nutrition, Treatment
Nonstandard Abbreviations and Acronyms
- c‐fPWV
carotid‐to‐femoral pulse wave velocity
- PHQ‐15
Patient Health Questionnaire‐15
Clinical Perspective
What Is New?
We performed a randomized controlled trial to address whether a relatively high dose of magnesium supplementation (450 mg/d) has beneficial effects on arterial stiffness and blood pressure.
To our knowledge, this is the first head‐to‐head comparison between various organic and inorganic magnesium supplements and their potential effects on vascular function markers and blood pressure.
Magnesium citrate did not change arterial stiffness and blood pressure. Other inorganic formulations had similar nonsignificant effects.
What Are the Clinical Implications?
Magnesium supplements may not have beneficial effects on arterial stiffness, at least not in subjects with normal arterial stiffness values.
Future studies should investigate whether oral magnesium supplementation is effective in patients with increased arterial stiffness at baseline, such as patients with chronic kidney disease.
Arterial stiffness is an independent predictor of coronary heart disease and stroke. 1 Although arterial stiffness increases with age, lifestyle changes such as weight loss and lowering dietary salt and alcohol intake have been shown to reduce arterial stiffening. 2 , 3 , 4 In addition, increasing dietary magnesium intake may improve arterial stiffness. 5 Magnesium acts as a natural calcium channel blocker and has been suggested to modulate vasomotor tone and peripheral blood flow. 6 , 7 Preclinical studies demonstrated a protective role of magnesium on vascular calcification, 8 , 9 which may in turn lead to reduced arterial stiffening.
We previously investigated the effect of long‐term oral magnesium supplementation on vascular function markers and blood pressure. 10 We observed a significant improvement of arterial stiffness after 24 weeks of magnesium citrate supplementation compared with placebo. Yet it is unknown whether the effect was induced by magnesium itself or by the counterbalancing anion citrate, as the study was based on a single comparison between magnesium citrate and placebo. Citrate binds calcium and may therefore be able to inhibit the growth of calcium crystals and inhibit vascular calcification, 11 , 12 which may have contributed to the observed effect on arterial stiffness. Furthermore, in our previous study we found no effect on blood pressure, while blood pressure is a major determinant of arterial stiffness. One explanation could be that the total daily dose of magnesium was too low to exert an effect on blood pressure, as suggested by 2 meta‐analyses. 13 , 14
To date, no study has performed a head‐to‐head comparison between various magnesium formulations and their potential effects on vascular function markers and blood pressure. Differences between organic and inorganic formulations might be of interest as bioavailability may vary between formulations. 15 Several studies have shown that magnesium citrate has a higher bioavailability. 16 , 17 On the other hand, a meta‐analysis has shown that inorganic formulations, such as magnesium oxide, exhibited a greater increase in circulating magnesium levels than organic formulations. 18
The main objective of this randomized, double‐blind, placebo‐controlled intervention trial was to demonstrate the effect of magnesium citrate supplementation, in a higher dose than in our previous study, on carotid‐to‐femoral pulse wave velocity (c‐fPWV). 10 To further explore whether the previously observed effect was induced by magnesium itself or by the counterbalancing anion citrate, we studied whether 2 inorganic formulations of magnesium, magnesium oxide and magnesium sulfate, are noninferior to magnesium citrate. Finally, we addressed the effects of a relatively high dose of various magnesium supplements on blood pressure, plasma magnesium, and 24‐hour urinary magnesium excretion as secondary outcomes.
Methods
Study Population
We recruited participants who were overweight and slightly obese via posters in the hospital and advertisements in local newspapers. Furthermore, we approached volunteers who participated in an earlier study in the University Medical Center Groningen. Details of the inclusion and exclusion criteria have been described previously. 15 In brief, subjects were 45‐ to 75‐year‐old nonsmokers, with a stable body weight (weight gain or loss ≤3 kg in the past 3 months) and a body mass index (BMI) between 25 and 35 kg/m2. We included subjects who were overweight and slightly obese, because they were expected to have increased arterial stiffness and blood pressure at baseline, allowing for improvement by the intervention. 10 , 19 Furthermore, we excluded premenopausal women to reduce possible variations in the study outcomes attributable to hormonal effects (<2 years after last menstruation). Individuals with a high dietary magnesium intake (urinary magnesium excretion ≥7.0 mmol/24 h for men and ≥5.9 mmol/24 h for women) or high fasting levels of plasma glucose (≥7.0 mmol/L), total cholesterol (≥8.0 mmol/L), and triglycerides (≥2.2 mmol/L) were also not eligible for the study. Participants were instructed to continue any preexisting medication without alterations throughout the study.
All subjects provided written informed consent before the screening visit. The study was conducted according to the Declaration of Helsinki, and ethics committee approval was obtained from the University Medical Center Groningen, The Netherlands (METc2017/220). The study was registered at clinicaltrials.gov as NCT03632590. The procedures followed were in accordance with the University Medical Center Groningen guidelines. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Study Design
In this randomized, double‐blind, placebo‐controlled, parallel‐group trial, 164 study participants were randomly assigned to receive either a magnesium citrate supplement, a magnesium oxide supplement, a magnesium sulfate supplement, or placebo, all in capsules with identical appearance, smell, and taste. The capsules were provided by Laboratorium Medisan (Heerenveen, The Netherlands), which also conducted the randomization procedure. For this, a categorical list in logical order was created. The list included 1 intervention for each participant. Based on a computer‐generated list of random numbers, subjects were randomly assigned into 1 of the groups. 15 Participants took 2 capsules thrice daily for 24 weeks. On the test days (at baseline, at 2 weeks, 12 weeks, and 24 weeks), the first 2 capsules were taken after all measurements were completed. Each magnesium supplement provided 75 mg of magnesium (magnesium citrate complex [Mg 15.5%], magnesium oxide complex [Mg 60.3%], magnesium sulfate complex [Mg 17.4%]). Thus, the total daily dose of magnesium was 450 mg, which is higher than in our previous study (350 mg/d). 10 The placebo capsules contained starch (amylum solani). The total treatment duration was based on the previous study. 10
Dietary Intake
Subjects were instructed not to change their food intake pattern or alcohol use during the entire study. To address potential changes in the food intake pattern and use of alcohol, participants completed a 3‐day food diary at baseline and at the end of the study using standard supply units. All diaries were checked for completeness by the investigator and were calculated by a research dietitian using the software program EvryDietist, version 7.3.5.0 (Evry BV). This software uses the Dutch Food Composition Database 2016 to calculate energy and nutrient intake.
Blood and Urine Collection
Participants collected 24‐hour urine samples before each test day. They were instructed to discard the first morning urine sample and to collect all urine for the following 24 hours, including the next morning urine. Furthermore, participants were requested to not consume any foods or drinks (except for water) 8 hours before the study visit. Fasting blood samples were drawn at each test day from the forearm vein by venipuncture. Plasma and urine concentrations of magnesium, calcium, potassium, sodium, and creatinine were determined photometrically on a Cobas 8000 platform (Roche, Mannheim, Germany). Sodium and potassium concentrations were measured with indirect ion‐selective electrode method, magnesium with the xylidyl blue colorimetric assay, and creatinine with an enzymatic assay. Plasma glucose concentrations were measured on a Cobas 8000 platform (Roche, Mannheim, Germany) using a hexokinase ultraviolet test and hemoglobin A1c concentrations were measured on a Tosoh G8 (high‐performance liquid chromatography; Sysmex Corporation, Norderstedt, Germany). Plasma calcium was adjusted for albumin concentration using the following formula: Calciumadj=plasma calcium (mmol/L)+0.02×(40–plasma albumin [g/L]). 20 Total and high‐density lipoprotein cholesterol and triglycerides were measured on a Cobas 8000 platform. Dyslipidemia was defined as high low‐density lipoprotein cholesterol concentrations (≥4.8 mmol/L), or high triglyceride concentrations (≥2.0 mmol/L) or low high‐density lipoprotein cholesterol concentrations (≤1.0 mmol/L in men or ≤1.30 mmol/L in women) or the use of lipid‐lowering drugs. 21
Anthropometrics and Body Composition
All clinical measurements were performed by the same investigator as much as possible and were carried out in a fasting state. Height was measured during the screening visit using a wall‐mounted stadiometer (Seca 222; Seca GMBH, Hamburg, Germany). Body weight was measured using a calibrated digital measuring scale without shoes and heavy clothing (Seca 877; Seca GMBH). Body composition was measured using a Bio‐Electrical Impedance Analysis device (Bodystat Quadscan 4000; Quadscan, Douglas, Isle of Man, UK).
Blood Pressure
Blood pressure was measured 4 times (1 minute apart) after an acclimatization period of at least 10 minutes in a supine position using a continuous blood pressure monitoring device (Criticare 506 N3; Criticare Systems Inc., Waukesha, WI). The first measurement was discarded, and the mean of the last 3 measurements was reported. Hypertension was defined as a systolic blood pressure of ≥120 mm Hg, a diastolic blood pressure of ≥90 mm Hg, or the use of antihypertensive drugs.
Arterial Stiffness
A direct marker of arterial stiffness is c‐fPWV, which is the gold standard method for the quantification of arterial stiffness. An indirect measure of arterial stiffness is the augmentation index adjusted for heart rate, of which the central arterial waveform can be indirectly estimated from a transfer function from radial artery tonometry. After measuring blood pressure, c‐fPWV and augmentation index adjusted for heart rate measurements were recorded in duplicate using a validated device (SphygmoCor v9; AtCor Medical, West Ryde, Australia). For the c‐fPWV measurement, the distance from the suprasternal notch to the femoral recording site (via umbilicus) was measured, and subsequently the distance from the suprasternal notch to the carotid recording site (right) was subtracted. A detailed description of the vascular function measurements was previously published in our study protocol. 15 Arterial stiffness measurements were performed in accordance with the expert consensus document on arterial stiffness by the European Network for Non‐invasive Investigation of Large Arteries. 22
Somatic and Gastrointestinal Symptom Severity
Participants completed a Patient Health Questionnaire (PHQ‐15) before the baseline, 12‐week, and 24‐week visits. Severity was rated for the past 4 weeks (baseline), or since the last visit (follow‐up) as 1 (“not bothered at all”), 2 (“slightly bothered”), or 3 (“remarkably bothered”). The item “menstrual cramps” was removed, as only postmenopausal women participated in the current study. The somatic symptom severity score was calculated by taking the mean score of the 14 somatic symptoms of the PHQ‐15. The PHQ‐15 includes 3 gastrointestinal items: (1) stomach pain; (2) constipation, loose bowels, or diarrhea; and (3) nausea, gas, or indigestion. Scores for the 3 items were added up in a composite gastrointestinal score, with scores ranging from 1 to 6.
Statistical Analysis
Given our 2 main research questions, we evaluated whether magnesium citrate is superior to placebo to improve c‐fPWV (primary confirmatory objective) and explored whether magnesium oxide and magnesium sulfate are noninferior to magnesium citrate to improve c‐fPWV (secondary objectives). Because the primary objective was confirmation of a previous finding, sample size calculation was based on a 2‐sided type I error of 0.05 and a power of at least 95%. Using the standard deviation of change in c‐fPWV over time of the primary study of 0.9 m/s, it was calculated that 24 participants were required for both the magnesium citrate and the placebo group to allow for detection of a treatment effect of at least 1.0 m/s in c‐fPWV. To account for potential dropout by 10%, group sizes were increased to 26 participants. For the exploratory secondary objective sample size calculation was based on a 1‐sided type I error of 0.05 and a power of 80% and a noninferiority design. Using the SD of change in c‐fPWV over time of the primary study of 0.9 m/s, it was calculated that 41 participants were required for the comparison of magnesium oxide with magnesium citrate and the comparison of magnesium sulfate with magnesium citrate with a noninferiority margin of 0.5 m/s in c‐fPWV. To account for potential dropout by 10%, group sizes were increased to 46 participants. Because we included 46 participants in the magnesium citrate group to provide power for the secondary analyses, the power for the primary analysis consisting of comparison of magnesium citrate with placebo treatment became 99%. All main analyses were performed according to the intention‐to‐treat principle. Additional per‐protocol analyses were performed to examine whether exclusion of noncompliant subjects influenced the results.
Normally distributed variables are presented as mean±SD and nonnormally distributed variables as median (interquartile range). Data on somatic and gastrointestinal symptom severity (PHQ‐15) are presented as mean±SEM. Longitudinal effects of magnesium supplementation were quantified, with linear mixed‐effect models specifying time, intervention, and the interaction between time and intervention as fixed effects. The models were adjusted for age, sex, and the baseline value of the outcome of interest. Our primary outcome was c‐fPWV. First, we determined effects of magnesium citrate, magnesium oxide, and magnesium sulfate versus placebo treatment by means of a 95% CI derived from a linear mixed‐effect model. Second, for the noninferiority testing of magnesium oxide versus magnesium citrate and of magnesium sulfate versus magnesium citrate, a 90% CI was reported and a Δ of 0.5 m/s was used to determine noninferiority. 10 For the primary objective, the 4 groups were analyzed in 1 linear mixed‐effect model. Similar models were analyzed for the secondary objectives but without the placebo group. Secondary outcomes, including blood pressure, plasma magnesium, and 24‐hour urinary magnesium excretion, other plasma and urinary minerals, and body composition were assessed using linear mixed‐effect models specifying the same linear predictor. Because data on somatic and gastrointestinal symptom severity were nonnormally distributed, we performed Mann‐Whitney U tests to compare between‐group differences at baseline, 12 weeks, and 24 weeks.
Findings from a recent meta‐analysis prompted us to explore effects of magnesium citrate, magnesium oxide, and magnesium sulfate supplementation (versus placebo) on c‐fPWV in several subgroups, based on their mean baseline values. 23 These subgroups included age (<63 years and ≥63 years), sex (m/f), BMI (<28 kg/m2 and ≥28 kg/m2), waist circumference (men, <102 and ≥102 cm; women, <92 and ≥92 cm), diuretic use (y/n), dyslipidemia (y/n), hypertension (y/n), and c‐fPWV (<9 and ≥9 m/s). Subgroup analyses were also performed based on clinically relevant cutoff points (age <60 years and ≥60 years), BMI (<30 kg/m2 and ≥30 kg/m2), waist circumference (men, <102 cm and ≥102 cm; women, <88 cm and ≥88 cm). and c‐fPWV (<10 m/s and ≥10 m/s), as recommended in the Expert Consensus document of 2012. 22 Effect modification was investigated by adding interaction terms (intervention [0/1]×subgroup [0/1] ). Subgroup analyses were assessed at 24 weeks.
Statistical analyses were performed using SPSS 23.0 software for Windows (SPSS Incorporated, Chicago, IL) and Rstudio version 1.1.383 (R Foundation for Statistical Computing, Vienna, Austria).
Results
Study Subjects
A Consolidated Standards of Reporting Trials flow diagram is shown in Figure 1. After screening, 164 individuals were eligible to participate in the study. The first participant was enrolled on March 27, 2018, and the last visit was performed on June 4, 2020. In total, 7 (4.3%) participants discontinued the study treatment. The main reasons for discontinuation were gastrointestinal complaints. In addition, 3 participants were lost to follow‐up because of COVID‐19 infection. Details are depicted in Table S1.
Figure 1. Consolidated Standards of Reporting Trials flow diagram of participants throughout the study.
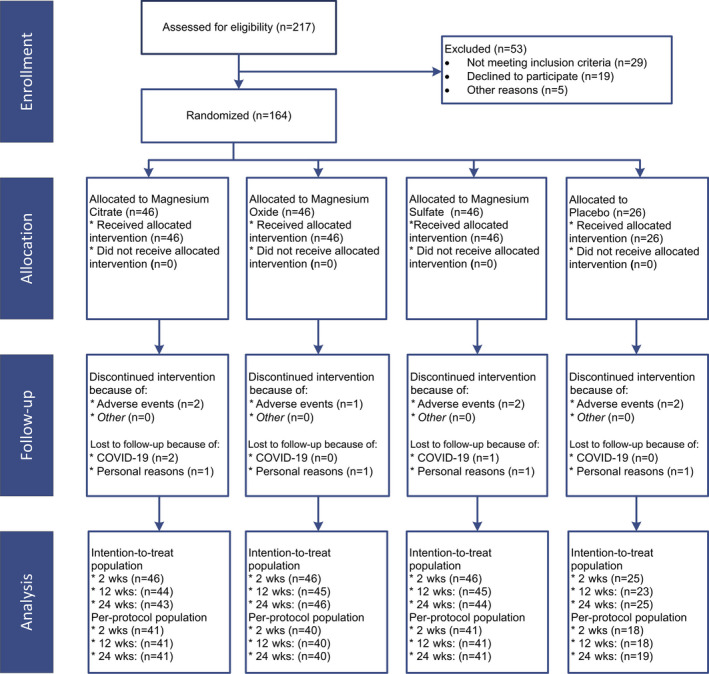
Baseline characteristics of the participants are shown in Table 1. Mean age of the study participants was 63.2±6.8 years, 104 (63.4%) were women, and mean BMI was 28.1±2.8 kg/m2. In total, 25 (15.2%) participants used antihypertensive drugs, of whom 11 (6.7%) used diuretics. In addition, 10 (6.1%) used lipid‐lowering drugs. Baseline characteristics were comparable between the groups.
Table 1.
Baseline Characteristics of the Study Participants
|
All participants (n=164) |
Magnesium citrate (n=46) | Magnesium oxide (n=46) | Magnesium sulphate (n=46) |
Placebo (n=26) |
|
|---|---|---|---|---|---|
| Demographics | |||||
| Age, y | 63.2±6.8 | 64.1±6.1 | 63.2±6.7 | 62.0±6.9 | 63.8±7.8 |
| Women | 104 (63.4) | 31 (67.4) | 29 (63.0) | 30 (65.2) | 14 (53.8) |
| Caucasians | 162 (98.8) | 45 (97.8) | 46 (100) | 45 (97.8) | 25 (100) |
| Body composition | |||||
| Weight, kg | 85.0±12.0 | 85.6±13.0 | 82.8±12.1 | 86.2±11.8 | 85.6±10.3 |
| BMI, kg/m2 | 28.1±2.8 | 28.7±3.4 | 27.5±2.1 | 28.4±2.9 | 27.8±2.4 |
| Waist circumference, cm | 95±9 | 97±10 | 94±10 | 96±9 | 96±8 |
| Men, cm | 102±8 | 104±9 | 101±9 | 101±9 | 101±7 |
| Women, cm | 92±8 | 93±8 | 89±8 | 93±9 | 92±7 |
| Hip circumference, cm | 107±7 | 110±8 | 106±6 | 107±7 | 107±5 |
| Total body fat, % | 35.3±7.6 | 37.0±8.0 | 34.2±6.7 | 35.7±8.3 | 33.8±7.1 |
| Men, cm | 27.0±3.9 | 27.7±4.6 | 26.9±4.0 | 26.0±3.2 | 27.8±3.9 |
| Women, cm | 40.3±4.2 | 41.7±4.5 | 38.7±3.0 | 41.0±4.3 | 39.3±4.4 |
| Medication usage | |||||
| Antihypertensive treatment | 25 (15.2) | 8 (17.4) | 4 (8.7) | 7 (15.2) | 6 (23.1) |
| Beta blockers | 9 (5.5) | 4 (8.7) | 0 (0) | 4 (8.7) | 1 (3.8) |
| Calcium channel blockers | 4 (2.4) | 2 (4.3) | 0 (0) | 1 (2.2) | 1 (3.8) |
| ACE inhibitors | 9 (5.5) | 3 (6.5) | 2 (4.3) | 1 (2.2) | 3 (11.5) |
| ARBs | 5 (3.0) | 1 (2.2) | 2 (4.3) | 2 (4.3) | 0 (0) |
| Diuretics | 11 (6.7) | 2 (4.3) | 2 (4.3) | 3 (6.5) | 3 (11.5) |
| Lipid‐lowering treatment | 10 (6.1) | 2 (4.3) | 3 (6.5) | 3 (6.5) | 2 (7.7) |
| Hypertension | 61 (37.2) | 19 (41.3) | 14 (30.4) | 17 (37.0) | 11 (42.3) |
| Dyslipidemia | 47 (28.7) | 11 (23.9) | 12 (26.1) | 16 (34.8) | 8 (30.8) |
| Total cholesterol, mmol/L | 5.20±0.82 | 5.23±0.90 | 5.32±0.84 | 5.08±0.72 | 5.16±0.79 |
| HDL cholesterol, mmol/L | 1.47±0.37 | 1.45±0.33 | 1,52±0.36 | 1.45±0.37 | 1.45±0.44 |
| Triglycerides, mmol/L | 1.02 (0.78–1.50) | 1.02 (0.77–1.61) | 1.06 (0.72–1.56) | 1.02 (0.78–1.54) | 0.99 (0.83–1.37) |
| Vascular function markers | |||||
| c‐fPWV, m/s | 8.6±1.6 | 9.0±1.7 | 8.2±1.6 | 8.6±1.6 | 8.4±1.5 |
| AI@HR75, % | 24.7±8.6 | 26.9±8.8 | 23.0±8.8 | 24.6±8.2 | 24.0±8.2 |
| Blood pressure | |||||
| Systolic blood pressure , mm Hg | 130±15 | 133±15 | 127±15 | 130±15 | 130±14 |
| Diastolic blood pressure , mm Hg | 79±9 | 79±9 | 77±9 | 79±9 | 80±8 |
| Mean arterial pressure, mm Hg | 96±10 | 97±10 | 93±11 | 96±11 | 97±10 |
| Pulse pressure, mm Hg | 51±9 | 54±9 | 50±10 | 51±9 | 50±9 |
| Heart rate, bpm | 60±8 | 61±9 | 60±6 | 60±8 | 61±8 |
| Plasma minerals | |||||
| Magnesium, mmol/L | 0.85±0.06 | 0.86±0.06 | 0.84±0.04 | 0.85±0.09 | 0.87±0.06 |
| Calcium, mmol/L | 2.34±0.08 | 2.33±0.08 | 2.34±0.09 | 2.35±0.07 | 2.35±0.09 |
| Potassium, mmol/L | 4.1±0.3 | 4.1±0.3 | 4.2±0.3 | 4.1±0.3 | 4.1±0.3 |
| Sodium, mmol/L | 140±2 | 140±2 | 140±2 | 140±2 | 141±1 |
| Phosphate, mmol/L | 1.00±0.14 | 1.00±0.12 | 1.00±0.16 | 0.98±0.15 | 1.01±0.13 |
| Creatinine, µmol/L | 73.0 (65.0–85.0) | 73.0 (67.0–84.3) | 76.0 (63.5–88.3) | 71.0 (64.0–84.0) | 71.0 (63.5–92.8) |
| Albumin | 44.1±3.3 | 44.8±4.9 | 44.3±2.2 | 43.5±2.5 | 43.7±2.6 |
| Urinary minerals | |||||
| Magnesium, mmol/24‐h | 5.06±1.72 | 4.94±1.47 | 5.13±1.65 | 4.89±2.0 | 5.46±1.67 |
| Calcium, mmol/24‐h | 4.88±2.25 | 4.59±1.95 | 5.29±2.49 | 4.96±2.39 | 4.54±2.06 |
| Potassium, mmol/24‐h | 87.6±25.4 | 81.0±20.3 | 93.4±23.7 | 86.9±26.2 | 90.2±32.9 |
Values are mean±SD, median (interquartile range), or number (percentage).
ACE indicates angiotensin‐converting enzyme; AI@HR75, augmentation index adjusted for heart rate; ARBs, angiotensin II receptor blockers; BMI, body mass index; and c‐fPWV, carotid‐to‐femoral pulse wave velocity.
Magnesium Versus Placebo
Treatment with magnesium citrate did not have a significant effect on c‐fPWV and augmentation index adjusted for heart rate at any time point during the trial, compared with placebo (Table 2). There were also no significant effects of magnesium citrate supplementation on blood pressure or heart rate (Table 3). Magnesium citrate treatment significantly increased plasma and 24‐hour urinary concentrations of magnesium compared with placebo at all time points (Table 4). In addition, participants in the magnesium citrate group showed higher plasma phosphate and higher 24‐hour urinary excretions of potassium and calcium; no effects on body composition were found (Table S2 through S4). Dietary and alcohol intake according to the food diaries did not change during the study period (Table S5). Excluding noncompliant subjects as well as subjects on antihypertensive or lipid‐lowering drugs did not materially change the results (data not shown). When compared with placebo, effects of treatment with magnesium oxide and magnesium sulfate on c‐fPWV, augmentation index adjusted for heart rate, and blood pressure were also nonsignificant (Table 2, 3, 4). Participants in the magnesium oxide and magnesium sulfate groups showed, similar to participants in the magnesium citrate group, higher 24‐hour urinary calcium, potassium, and sodium during the treatment period when compared with placebo (Table S3).
Table 2.
Effects of Magnesium Citrate, Magnesium Oxide, and Magnesium Sulfate (Versus Placebo) on Vascular Function Markers
|
Magnesium citrate (n=46) |
Magnesium oxide (n=46) |
Magnesium sulfate (n=46) |
Placebo (n=26) |
|
|---|---|---|---|---|
| c‐fPWV | ||||
| 2‐wk | ||||
| Mean, m/s | 9.1±1.9 | 8.5±1.4 | 8.4±1.4 | 8.4±1.9 |
| Difference vs placebo | 0.2 (−0.5 to 0.8) | 0.2 (−0.4 to 0.9) | −0.2 (−0.9 to 0.4) | … |
| 12‐wk | ||||
| Mean, m/s | 9.0±1.9 | 8.5±1.2 | 8.7±1.7 | 8.5±1.5 |
| Difference vs placebo | 0.0 (−0.6 to 0.7) | −0.0 (−0.7 to 0.6) | −0.0 (−0.7 to 0.6) | … |
| 24‐wk | ||||
| Mean, m/s | 9.0±1.6 | 8.4±1.6 | 8.3±1.4 | 8.5±2.3 |
| Difference vs placebo | −0.0 (−0.7 to 0.6) | −0.0 (−0.6 to 0.6) | −0.3 (−1.0 to 0.3) | … |
| AI@HR75 | ||||
| 2‐wk | ||||
| Mean, % | 25.0±8.5 | 21.7±8.6 | 23.4±8.5 | 22.9±10.8 |
| Difference vs placebo | −1.1 (−3.4 to 1.2) | −0.6 (−3.0 to 1.8) | −0.3 (−0.6 to 2.0) | … |
| 12‐wk | ||||
| Mean, % | 25.3±8.4 | 20.8±9.0 | 23.3±9.1 | 21.5±10.0 |
| Difference vs placebo | 0.7 (−1.7 to 3.0) | 0.1 (−2.2 to 2.5) | 0.7 (−1.6 to 3.0) | … |
| 24‐wk | ||||
| Mean, % | 24.7±8.9 | 21.3±8.3 | 23.9±9.1 | 22.4±10.4 |
| Difference vs placebo | −1.0 (−3.3 to 1.4) | −0.1 (−2.5 to 2.2) | 0.5 (−1.8 to 2.8) | … |
Values are mean±SD. Adjusted mean differences (95% CIs) were obtained from linear mixed‐effect models with age, sex, baseline value of the outcome of interest, time, intervention, and the interaction time×intervention as fixed effects. AI@HR75 indicates augmentation index adjusted for heart rate; and c‐fPWV; carotid‐to‐femoral pulse wave velocity.
Table 3.
Effects of Magnesium Citrate, Magnesium Oxide, and Magnesium Sulfate (Versus Placebo) on Blood Pressure
| Magnesium citrate (n=46) | Magnesium oxide (n=46) | Magnesium sulfate (n=46) |
Placebo (n=26) |
|
|---|---|---|---|---|
| Systolic blood pressure | ||||
| 2‐wk | ||||
| Mean, mm Hg | 131±14 | 127±15 | 130±15 | 130±15 |
| Difference vs placebo | −1 (−5 to 2) | −0 (−4 to 3) | 0 (−4 to 4) | … |
| 12‐wk | ||||
| Mean, mm Hg | 132±15 | 125±14 | 129±13 | 127±13 |
| Difference vs placebo | 2 (−2 to 6) | 1 (−3 to 5) | 2 (−2 to 5) | … |
| 24‐wk | ||||
| Mean, mm Hg | 133±16 | 127±15 | 131±16 | 129±13 |
| Difference vs placebo | 1 (−2 to 5) | 1 (−2 to 5) | 2 (−2 to 6) | … |
| Diastolic blood pressure | ||||
| 2‐wk | ||||
| Mean, mm Hg | 78±8 | 77±8 | 79±8 | 80±8 |
| Difference vs placebo | −1 (−3 to 1) | −1 (−3 to 1) | −1 (−2 to 1) | … |
| 12‐wk | ||||
| Mean, mm Hg | 78±9 | 75±8 | 79±8 | 80±9 |
| Difference vs placebo | −1 (−3 to 2) | −1 (−4 to 1) | −1 (−3 to 2) | … |
| 24‐wk | ||||
| Mean, mm Hg | 79±9 | 76±9 | 79±9 | 80±9 |
| Difference vs placebo | 0 (−2 to 2) | −0 (−2 to 2) | −0 (−2 to 2) | … |
| Mean arterial pressure | ||||
| 2‐wk | ||||
| Mean, mm Hg | 96±10 | 93±10 | 96±10 | 97±10 |
| Difference vs placebo | −1 (−3 to 1) | 0 (−2 to 2) | −0 (−3 to 2) | … |
| 12‐wk | ||||
| Mean, mm Hg | 96±11 | 92±9 | 95±9 | 96±10 |
| Difference vs placebo | 0 (−2 to 3) | −0 (−3 to 2) | 0 (−2 to 3) | … |
| 24‐wk | ||||
| Mean, mm Hg | 97±11 | 93±10 | 96±11 | 96±10 |
| Difference vs placebo | 0 (−2 to 3) | 1 (−2 to 3) | 1 (−2 to 3) | … |
| Pulse pressure | ||||
| 2‐wk | ||||
| Mean, mm Hg | 53±9 | 50±10 | 51±10 | 50±8 |
| Difference vs placebo | −0 (−3 to 3) | 0 (−3 to 3) | 1 (−2 to 4) | … |
| 12‐wk | ||||
| Mean, mm Hg | 53±10 | 49±9 | 51±9 | 48±6 |
| Difference vs placebo | 3 (−0 to 6) | 2 (−1 to 5) | 2 (−1 to 5) | … |
| 24‐wk | ||||
| Mean, mm Hg | 54±10 | 51±11 | 52±10 | 49±6 |
| Difference vs placebo | 2 (−1 to 5) | 2 (−1 to 5) | 3 (−0 to 6) | … |
| Heart rate | ||||
| 2‐wk | ||||
| Mean, bpm | 61±8 | 59±8 | 59±7 | 62±7 |
| Difference vs placebo | −0 (−3 to 2) | −1 (−4 to 1) | −1 (−3 to 2) | … |
| 12‐wk | ||||
| Mean, bpm | 61±8 | 59±7 | 60±6 | 61±8 |
| Difference vs placebo | −0 (−3 to 2) | −2 (−4 to 1) | −1 (−3 to 2) | … |
| 24‐wk | ||||
| Mean, bpm | 62±8 | 59±7 | 59±6 | 62±7 |
| Difference vs placebo | 0 (−2 to 3) | −3 (−5 to −0)* | −1 (−4 to 1) | … |
Values are mean±SD. Adjusted mean differences (95% CIs) were obtained from linear mixed‐effect models with age, sex, baseline value of the outcome of interest, time, intervention, and the interaction time×intervention as fixed effects.
P<0.05 (two‐sided P values).
Table 4.
Effects of Magnesium Citrate, Magnesium Oxide, and Magnesium Sulfate (Versus Placebo) on Magnesium Parameters
|
Magnesium citrate (n=46) |
Magnesium oxide (n=46) |
Magnesium sulfate (n=46) |
Placebo (n=26) |
|
|---|---|---|---|---|
| Plasma magnesium | ||||
| 2‐wk | ||||
| Mean, mmol/L | 0.88±0.06 | 0.86±0.05 | 0.86±0.08 | 0.85±0.07 |
| Difference vs placebo | 0.03 (0.01–0.05)** | 0.03 (0.01–0.05)* | 0.02 (0.00–0.04) | … |
| 12‐wk | ||||
| Mean, mmol/L | 0.87±0.05 | 0.86±0.04 | 0.86±0.10 | 0.85±0.06 |
| Difference vs placebo | 0.03 (0.01–0.05)* | 0.04 (0.02–0.06)** | 0.03 (0.01–0.05)* | … |
| 24‐wk | ||||
| Mean, mmol/L | 0.88±0.06 | 0.86±0.05 | 0.85±0.08 | 0.85±0.06 |
| Difference vs placebo | 0.04 (0.02–0.06)** | 0.03 (0.01–0.05)** | 0.02 (0.00–0.04) | … |
| Urinary magnesium | ||||
| 2‐wk | ||||
| Mean, mmol/24‐h | 7.24±2.11 | 7.06±1.86 | 6.80±2.12 | 5.41±1.97 |
| Difference vs placebo | 2.29 (1.41–3.17)*** | 1.93 (1.05–2.80)*** | 1.82 (0.95–2.70)*** | … |
| 12‐wk | ||||
| Mean, mmol/24‐h | 7.60±1.91 | 7.03±2.01 | 6.61±2.35 | 5.32±2.11 |
| Difference vs placebo | 2.71 (1.83–3.59)*** | 2.14 (1.26–3.02)*** | 1.75 (0.87–2.63)*** | … |
| 24‐wk | ||||
| Mean, mmol/24‐h | 7.79±1.92 | 7.07±1.88 | 6.62±2.23 | 5.11±1.83 |
| Difference vs placebo | 3.12 (2.23–4.01)*** | 2.38 (1.50–3.26)*** | 2.07 (1.19–2.96)*** | … |
Values are mean±SD. Adjusted mean differences (95% CIs) were obtained from linear mixed‐effect models with age, sex, baseline value of the outcome of interest, time, intervention, and the interaction time×intervention as fixed effects.
P<0.05.
P<0.01.
P<0.001 (2‐sided P values).
Magnesium Oxide Versus Magnesium Citrate
During the treatment period, vascular function markers (Table 5) and blood pressure (Table 6) were not different between the magnesium oxide and magnesium citrate groups. Heart rate was significantly lower in the magnesium oxide group by 3 bpm at 24 weeks (90% CI, 1–5 bpm). Plasma magnesium was similar among the 2 magnesium groups, whereas 24‐hour urinary magnesium excretion was slightly lower in the magnesium oxide group compared with the magnesium citrate group (Table 7). Plasma albumin was significantly higher in the magnesium oxide group at 2 weeks and 24 weeks (Table S6). No differences were observed between magnesium oxide and magnesium citrate in terms of 24‐hour urinary excretions of calcium, potassium, sodium, and creatinine during the treatment period (Table S7). Participants in the magnesium oxide group had a lower waist circumference after 24 weeks (−2.0 cm; 90% CI, −3.2 to −0.7 cm) compared with participants in the magnesium citrate group (Table S8). Dietary and alcohol intake according to the food diaries did not change during the study period (Table S9). Excluding noncompliant subjects as well as subjects on antihypertensive or lipid‐lowering drugs did not materially change the results (data not shown).
Table 5.
Effects of Magnesium Oxide and Magnesium Sulfate (Versus Magnesium Citrate) on Vascular Function Markers
|
Magnesium oxide (n=46) |
Magnesium sulfate (n=46) |
Magnesium citrate (n=46) |
|
|---|---|---|---|
| c‐fPWV | |||
| 2‐wk | |||
| Mean, m/s | 8.5±1.4 | 8.4±1.4 | 9.1±1.9 |
| Difference vs magnesium citrate | 0.0 (−0.4 to 0.5) | −0.4 (−0.9 to 0.0) | … |
| 12‐wk | |||
| Mean, m/s | 8.5±1.2 | 8.7±1.7 | 9.0±1.9 |
| Difference vs magnesium citrate | −0.0 (−0.5 to 0.4) | −0.1 (−0.5 to 0.4) | … |
| 24‐wk | |||
| Mean, m/s | 8.4±1.6 | 8.3±1.4 | 9.0±1.6 |
| Difference vs magnesium citrate | 0.1 (−0.5 to 0.5) | −0.4 (−0.8 to 0.1) | … |
| AI@HR75 | |||
| 2‐wk | |||
| Mean, % | 21.7±8.6 | 23.4±8.5 | 25.0±8.5 |
| Difference vs magnesium citrate | 0.4 (−1.2 to 2.0) | 0.8 (−0.8 to 2.3) | … |
| 12‐wk | |||
| Mean, % | 20.8±9.0 | 23.3±9.1 | 25.3±8.4 |
| Difference vs magnesium citrate | −0.4 (−2.0 to 1.2) | 0.1 (−1.5 to 1.7) | … |
| 24‐wk | |||
| Mean, % | 21.3±8.3 | 23.9±9.1 | 24.7±8.9 |
| Difference vs magnesium citrate | 0.8 (−0.9 to 2.4) | 1.5 (−0.1 to 3.1) | … |
Values are mean±SD. Adjusted mean differences (90% CIs) were obtained from linear mixed‐effect models with age, sex, baseline value of the outcome of interest, time, intervention, and the interaction time×intervention as fixed effects. AI@HR75 indicates augmentation index adjusted for heart rate; and c‐fPWV; carotid‐to‐femoral pulse wave velocity.
Table 6.
Effects of Magnesium Oxide and Magnesium Sulfate (Versus Magnesium Citrate) on Blood Pressure
|
Magnesium oxide (n=46) |
Magnesium sulfate (n=46) |
Magnesium citrate (n=46) |
|
|---|---|---|---|
| Systolic blood pressure | |||
| 2‐wk | |||
| Mean, mm Hg | 127±15 | 130±15 | 131±14 |
| Difference vs magnesium citrate | 1 (−2 to 3) | 1 (−1 to 4) | … |
| 12‐wk | |||
| Mean, mm Hg | 125±14 | 129±13 | 132±15 |
| Difference vs magnesium citrate | −1 (−4 to 1) | −0 (−3 to 2) | … |
| 24‐wk | |||
| Mean, mm Hg | 127±15 | 131±16 | 133±16 |
| Difference vs magnesium citrate | −0 (−3 to 3) | 1 (−2 to 4) | … |
| Diastolic blood pressure | |||
| 2‐wk | |||
| Mean, mm Hg | 77±8 | 79±8 | 78±8 |
| Difference vs magnesium citrate | 0 (−1 to 2) | 0 (−1 to 2) | … |
| 12‐wk | |||
| Mean, mm Hg | 75±8 | 79±8 | 78±9 |
| Difference vs magnesium citrate | −1 (−2 to 1) | 0 (−1 to 2) | … |
| 24‐wk | |||
| Mean, mm Hg | 76±9 | 79±9 | 79±9 |
| Difference vs magnesium citrate | −0 (−2 to 1) | −1 (−2 to 1) | … |
| Mean arterial pressure | |||
| 2‐wk | |||
| Mean, mm Hg | 93±10 | 96±10 | 96±10 |
| Difference vs magnesium citrate | 1 (−1 to 3) | 1 (−1 to 2) | … |
| 12‐wk | |||
| Mean, mm Hg | 92±9 | 95±9 | 96±11 |
| Difference vs magnesium citrate | −0 (−2 to 1) | 0 (−2 to 2) | … |
| 24‐wk | |||
| Mean, mm Hg | 93±10 | 96±11 | 97±11 |
| Difference vs magnesium citrate | 0 (−1 to 2) | 0 (−2 to 2) | … |
| Pulse pressure | |||
| 2‐wk | |||
| Mean, mm Hg | 50±10 | 51±10 | 53±9 |
| Difference vs magnesium citrate | 1 (−2 to 3) | 1 (−1 to 3) | … |
| 12‐wk | |||
| Mean, mm Hg | 49±9 | 51±9 | 53±10 |
| Difference vs magnesium citrate | 1 (−3 to 2) | −1 (−3 to 2) | … |
| 24‐wk | |||
| Mean, mm Hg | 51±11 | 52±10 | 54±10 |
| Difference vs magnesium citrate | 0 (−2 to 2) | 1 (−1 to 3) | … |
| Heart rate | |||
| 2‐wk | |||
| Mean, bpm | 59±8 | 59±7 | 61±8 |
| Difference vs magnesium citrate | −1 (−3 to 1) | −0 (−2 to 1) | … |
| 12‐wk | |||
| Mean, bpm | 59±7 | 60±6 | 61±8 |
| Difference vs magnesium citrate | −1 (−3 to 0) | −0 (−2 to 1) | … |
| 24‐wk | |||
| Mean, bpm | 59±7 | 59±6 | 62±8 |
| Difference vs magnesium citrate | −3 (−5 to −1)* | −2 (−3 to −0) | … |
Values are mean±SD. Adjusted mean differences (90% CIs) were obtained from linear mixed‐effect models with age, sex, baseline value of the outcome of interest, time, intervention, and the interaction time×intervention as fixed effects.
P<0.01 (one‐sided P values).
Table 7.
Effects of Magnesium Oxide and Magnesium Sulfate (Versus Magnesium Citrate) on Magnesium Parameters
|
Magnesium oxide (n=46) |
Magnesium sulfate (n=46) |
Magnesium citrate (n=46) |
|
|---|---|---|---|
| Plasma magnesium | |||
| 2‐wk | |||
| Mean, mmol/L | 0.86±0.05 | 0.86±0.08 | 0.88±0.06 |
| Difference vs magnesium citrate | −0.00 (−0.02 to 0.01) | −0.01 (−0.03 to 0.00) | … |
| 12‐wk | |||
| Mean, mmol/L | 0.86±0.04 | 0.86±0.10 | 0.87±0.05 |
| Difference vs magnesium citrate | 0.01 (−0.01 to 0.03) | −0.00 (−0.02 to 0.01) | … |
| 24‐wk | |||
| Mean, mmol/L | 0.86±0.05 | 0.85±0.08 | 0.88±0.06 |
| Difference vs magnesium citrate | −0.01 (−0.02 to 0.01) | −0.02 (−0.04 to −0.00) | … |
| Urinary magnesium | |||
| 2‐wk | |||
| Mean, mmol/24‐h | 7.06±1.86 | 6.80±2.12 | 7.24±2.11 |
| Difference vs magnesium citrate | −0.35 (−1.00 to 0.29) | −0.47 (−1.10 to 0.17) | … |
| 12‐wk | |||
| Mean, mmol/24‐h | 7.03±2.01 | 6.61±2.35 | 7.60±1.91 |
| Difference vs magnesium citrate | −0.56 (−1.21 to 0.08) | −0.96 (−1.61 to −0.32)* | … |
| 24‐wk | |||
| Mean, mmol/24‐h | 7.07±1.88 | 6.62±2.23 | 7.79±1.92 |
| Difference vs magnesium citrate | −0.74 (−1.39 to −0.10)* | −1.05 (−1.69 to −0.41)** | … |
Values are mean±SD. Adjusted mean differences (90% CIs) were obtained from linear mixed‐effect models with age, sex, baseline value of the outcome of interest, time, intervention, and the interaction time×intervention as fixed effects.
P<0.05.
P<0.01 (one‐sided P values).
Magnesium Sulfate Versus Magnesium Citrate
No significant differences in vascular function markers (Table 5), blood pressure (Table 6), or plasma magnesium (Table 7) were observed between magnesium sulfate and magnesium citrate treatment. Urinary magnesium excretion was significantly lower at 12 weeks and at 24 weeks in the magnesium sulfate group (−0.96 mmol/24 h; 90% CI, −1.61 to −0.32 mmol/24 h and −1.05 mmol/24 h; 90% CI, −1.69 to −0.41 mmol/24 h, respectively). Plasma albumin was significantly higher in the magnesium sulfate group at 24 weeks (Table S6). No differences were observed between magnesium sulfate and magnesium citrate in terms of 24‐hour urinary excretions of calcium, potassium, sodium, and creatinine during the treatment period (Table S7). Body weight and BMI were significantly higher after 24 weeks of magnesium sulfate (0.8 kg; 90% CI, 0.2–1.3 kg and 0.2 kg/m2; 90% CI, 0.1–0.4 kg/m2) compared with magnesium citrate supplementation (Table S8). Dietary and alcohol intake according to the food diaries did not change during the study period (Table S9). Excluding noncompliant subjects as well as subjects on antihypertensive or lipid‐lowering drugs did not materially change the results (data not shown).
Subgroup Analyses
As secondary post hoc analyses, we assessed whether the effect of magnesium citrate, magnesium oxide and magnesium sulfate versus placebo on c‐fPWV was modified by age, sex, BMI, waist circumference, use of diuretics, dyslipidemia, hypertension, or baseline c‐fPWV (Figure 2). We found that the effect on c‐fPWV of magnesium citrate versus placebo and of magnesium oxide versus placebo was significantly modified by age; the effect of magnesium oxide versus placebo was significantly modified by BMI; the effect of magnesium citrate versus placebo was significantly modified by dyslipidemia; and the effect of magnesium citrate versus placebo and of magnesium sulfate versus placebo was significantly modified by baseline c‐fPWV. In younger participants receiving magnesium oxide supplements, c‐fPWV was significantly increased by treatment (1.1 m/s; 95% CI, 0.2–1.6 m/s), while in older participants c‐fPWV tended to decrease in all magnesium groups, although effects were not significantly different from placebo. In participants with a BMI of ≥28 kg/m2, c‐fPWV was reduced by magnesium supplementation, with the strongest effect observed in the magnesium oxide group, albeit without reaching statistical significance compared with placebo treatment. In participants with dyslipidemia, there was a significant increase in c‐fPWV in response to magnesium citrate supplementation (1.6 m/s; 95% CI, 0.2–3.0 m/s). Finally, in participants with a higher prevalent c‐fPWV (≥9.0 m/s), magnesium sulfate supplementation resulted in a significant decrease in c‐fPWV (−1.4 m/s; 95% CI, −2.7 to −0.1 m/s). Per‐protocol analyses did not materially change the results. Results of the subgroup analyses based on clinically relevant cutoff points are shown in Figure S1. Participants in the magnesium groups with a baseline arterial stiffness value of ≥10 m/s showed a stronger decrease in arterial stiffness compared with participants in the magnesium groups with baseline arterial stiffness of ≥9.0 m/s.
Figure 2. Treatment effects of magnesium citrate, magnesium oxide and magnesium sulfate supplementation (Versus placebo) on c‐fPWV by subgroups of age, sex, BMI, waist circumference, diuretic use, dyslipidemia, hypertension and c‐fPWV.
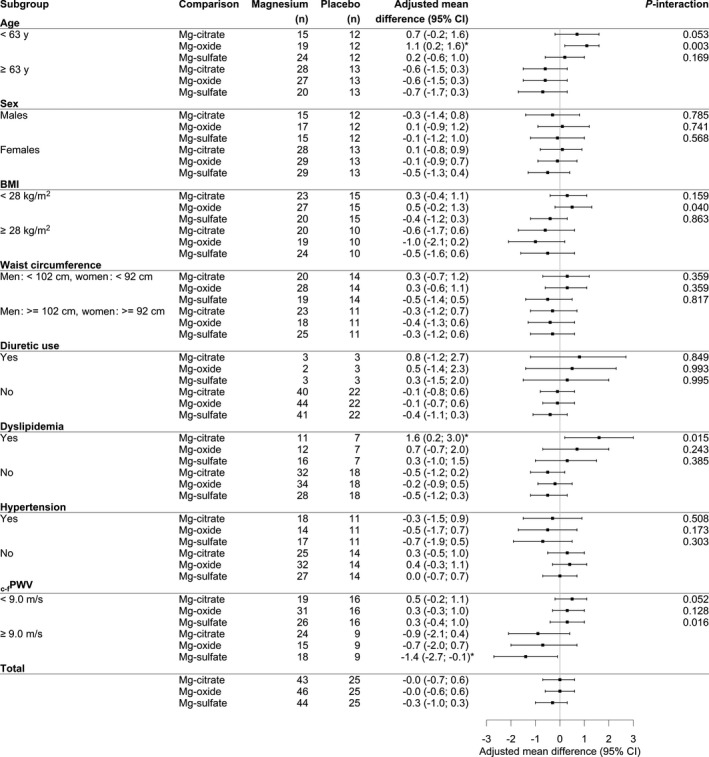
Effects of magnesium supplementation on c‐fPWV were quantified with linear mixed‐effect models specifying intervention and the baseline value of c‐fPWV as fixed effects. BMI indicates body mass index; and c‐fPWV; carotid‐to‐femoral pulse wave velocity.
Magnesium Versus Placebo on Gastrointestinal and Somatic Symptom Severity
Effects of oral magnesium supplementation on gastrointestinal and somatic symptom severity are depicted in Figure 3. Baseline symptom scores were similar between the groups. No differences were found in gastrointestinal symptom severity between the magnesium citrate and placebo group (Figure 3A). However, participants in the magnesium citrate group reported slightly more somatic symptoms at 12 weeks (P=0.036) compared with the placebo group, although scores were similar between the groups at 24 weeks (Figure 3B). Participants receiving magnesium oxide supplements reported fewer gastrointestinal symptoms at 12 weeks (versus=0.013) and 24 weeks (P=0.008; Figure 3A) and fewer somatic symptoms at 12 weeks (P=0.008) and 24 weeks (P=0.012; Figure 3B) compared with participants in the magnesium citrate group. Compared with placebo, participants in the magnesium sulfate group reported more gastrointestinal complaints at 24 weeks (P=0.021) and more somatic symptoms at 12 weeks (P=0.015) (Figure 3A and 3B, respectively). No significant differences were found in terms of gastrointestinal and somatic symptom severity between the magnesium sulfate and the magnesium citrate group.
Figure 3. Gastrointestinal symptom scores (A) and somatic symptom scores (B).
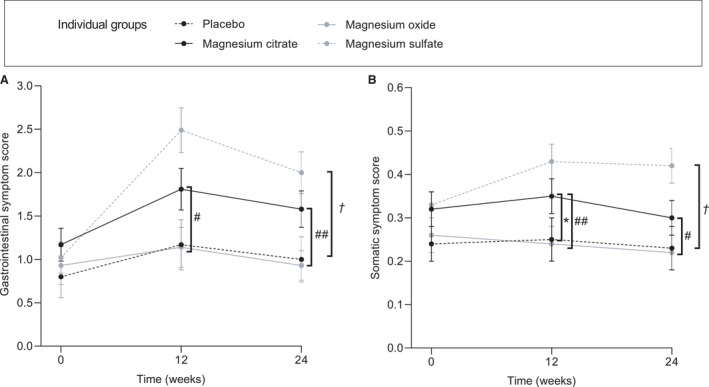
Scores represent mean±SEM. For the somatic symptom score, the mean of the 14 items was calculated. For the composite gastrointestinal score, the items “Stomach pain”, “constipation, loose bowels, or diarrhea,” and “nausea, gas, or indigestion” were summed up. Between‐group differences were calculated with the Mann‐Whitney U test. *P<0.05 magnesium citrate vs placebo, † P<0.05 magnesium sulfate vs placebo, # P<0.05 magnesium oxide vs magnesium citrate, ## P<0.01 magnesium vs magnesium citrate.
Compliance and Adverse Events
Urinary magnesium excretion was consistently increased in all magnesium groups throughout the study, indicating good overall adherence. This was confirmed by a mean compliance ≥90% based on number of returned capsules in all groups (Table S1). In total, 9 subjects were noncompliant according to capsule count (<80%). Adverse events reported by the study participants are shown in Table S1. Frequently reported adverse events included flatulence (n=10), stomach pain (n=13), and mild diarrhea (n=13). One female in the magnesium sulfate group experienced a stroke during week 3 of the study. This serious adverse event was considered unrelated to the study treatment, and the participant was able to continue the study.
Discussion
The primary aim of this study was to assess the effects of a relatively high dose of magnesium supplementation on arterial stiffness and blood pressure. A total daily dose of 450 mg/d was based on previous randomized controlled trials (RCTs) that suggested a greater blood pressure–lowering effect with a higher total daily dose of magnesium. 13 , 14 Furthermore, no prior study previously compared the efficacy of different magnesium formulations to pinpoint whether vascular effects may be driven by magnesium or the accompanying anion. Therefore, the main novel aspects of this trial are the higher magnesium dose and the head‐to‐head comparison among various types of magnesium supplements.
In contrast with our hypothesis, magnesium citrate supplementation of 450 mg/d for 24 weeks did not change arterial stiffness or blood pressure. Furthermore, compared with magnesium citrate treatment, magnesium oxide and magnesium sulfate did not significantly change c‐fPWV. In a secondary analysis, magnesium sulfate supplementation significantly improved c‐fPWV at 24 weeks in a subgroup with higher arterial stiffness at baseline. Effects of magnesium citrate and oxide supplementation on c‐fPWV at 24 weeks were in a similar direction, although not significantly different from placebo in these instances. Although these subgroup analyses should be interpreted with caution as it was not prespecified in the study protocol, this result suggests that oral magnesium supplementation is indeed effective to improve arterial stiffness in individuals with prevalent increased arterial stiffness. The current trial was mainly designed to confirm the previously observed effect of magnesium citrate supplementation on arterial stiffness, now with a slightly higher dose. In the previous study, we found a significant effect on c‐fPWV by 1.0 m/s after 24 weeks. 10 Interestingly, the effect size that we observed in individuals with prevalent increased arterial stiffness in the current study is similar to what we previously found.
To our knowledge, this is the first study that performed a head‐to‐head comparison between various magnesium formulations in terms of effects on arterial stiffness and blood pressure. Previous studies that addressed the effects of oral magnesium supplementation on vascular function markers deliberately chose a magnesium formulation based on their proposed bioavailability, whereas evidence regarding the bioavailability of magnesium formulations is still scarce. A higher bioavailability may yield greater effects, as more magnesium is absorbed and enters the circulation. Organic formulations, such as magnesium citrate or magnesium gluconate, are generally preferred over inorganic formulations, such as magnesium oxide and magnesium sulfate. 16 , 24 However, a recent meta‐analysis showed that the inorganic formulations exhibited a greater increase in serum magnesium compared with organic formulations. 18 This prompted us to compare the effects of organic with inorganic formulations, as bioavailability may differ between different formulations. The present study showed that the organic formulation magnesium citrate has a slightly higher bioavailability, assessed by 24‐hour urinary magnesium excretion, compared with the inorganic magnesium oxide and magnesium sulfate. However, the increase in plasma magnesium levels in the magnesium oxide and magnesium sulfate group was not significantly different from the increase in the magnesium citrate group during intervention. These findings are in line with the study of Coudray et al 17 showing that organic formulations were better absorbable than inorganic formulations, while no differences in terms of plasma magnesium were observed. Two studies reported higher 24‐hour urinary magnesium excretions as well as higher levels of serum and erythrocyte magnesium after magnesium citrate supplementation compared with magnesium oxide supplementation. 16 , 25 The intestinal solubility likely plays an important role in bioavailability of magnesium.
We previously observed that, during a 24‐week period, arterial stiffness was significantly improved following oral magnesium citrate supplementation, while the effect was not present at 3 months. 10 In the current RCT, no effect of 24‐week oral magnesium supplementation on arterial stiffness was found. Similarly, Cunha et al 26 recently reported no effect on arterial stiffness after 6 months of oral magnesium chelate supplementation administered at a dosage of 600 mg/d, which is 25% higher than the dose that was administered in our current study. Subgroup analyses of a recently published meta‐analysis showed an effect of oral magnesium supplementation on endothelial function, which is another vascular function marker, was present only in RCTs with a study duration of at least 6 months. 23 Thus, it is possible that a 24‐week treatment period is too short to find an effect of magnesium supplementation on arterial stiffness and that RCTs with longer treatment periods are required to provide evidence for an effect of oral magnesium supplementation on arterial stiffness.
Although c‐fPWV values were comparable with the previous observed values, 10 in the present study we included more women, and mean BMI and total cholesterol levels were lower at baseline, suggesting that the study population might have been slightly healthier than our previously selected study population. The meta‐analysis of Marques et al 23 showed that magnesium was effective in RCTs including older and more overweight subjects. Indeed, in our subgroup analyses, the effect of oral magnesium supplementation on arterial stiffness was modified by age and BMI, in such a way that the effect was more pronounced in participants who were older and more overweight. However, the effects in these subgroups were not statistically significant. On the other hand, in participants with dyslipidemia, c‐fPWV was significantly increased after a 24‐week treatment with magnesium citrate supplements. The subgroup analyses also showed that oral magnesium supplementation was more effective in participants with increased arterial stiffness at baseline. Notably, the effect size in this group was comparable with the effect size that we found in our previous study. The interaction by age might be partly explained by the fact that aging induces functional and structural changes in large elastic arteries, suggesting that the subgroup of older participants had prevalent increased arterial stiffness as well. Thus, our subgroup analyses might indicate that future trials should investigate effects of magnesium supplementation in study populations with more severe arterial stiffness, such as patients with chronic kidney disease. 27
Gastrointestinal adverse events induced by magnesium supplements are frequently reported. Particularly, osmotic diarrhea is often a result of high dosages of magnesium from dietary supplements. Therefore, the European Food Safety Authority has set the upper level for magnesium supplements at 350 mg/d. 28 Magnesium oxide is often used for the treatment of constipation because of its laxative properties. Magnesium sulfate, on the other hand, is often intravenously administered for treating and prevention of eclamptic seizures. 29 As a consequence, trials using oral magnesium sulfate are scarce. To the best of our knowledge, this is the first study that assessed somatic and gastrointestinal symptom severity of various magnesium formulations. Both scores were derived from the PHQ‐15. In general, gastrointestinal complaints are frequently reported by RCTs that administered magnesium supplements 30 , 31 ; however, these adverse events are often derived from patients’ diaries or nonvalidated questionnaires, without a formal quantification. In the current study, administering 450 mg/d of magnesium citrate yielded slightly more gastrointestinal complaints at 12 weeks compared with a placebo. However, this effect was not observed at the end of the trial. Furthermore, participants in the magnesium oxide group reported significantly fewer somatic and gastrointestinal complaints at 12 weeks and 24 weeks compared with participants in the magnesium citrate group. Our findings may indicate that magnesium oxide supplements are better tolerated than magnesium citrate supplements and are likely better tolerated than magnesium sulfate supplements. This is further substantiated by the fact that none of the participants from the magnesium oxide group discontinued the study treatment because of gastrointestinal complaints, whereas 2 (4.3%) participants from the magnesium citrate group and 2 (4.3%) participants from the magnesium sulfate group reported gastrointestinal complaints as the main reason for discontinuation.
Strengths and Limitations
We performed a relatively large multiple‐arm, randomized, double‐blind, placebo‐controlled trial, allowing comparison of different magnesium formulations. Previous trials mainly administered only a single magnesium formulation, while the varying formulations between studies introduces significant heterogeneity. 23 Furthermore, the compliance of the treatment groups was excellent, as shown by both increased 24‐hour urinary magnesium excretion and the low rate of returned capsules. Another strength is that we measured c‐fPWV, currently the gold standard for the quantification of arterial stiffness. 32 Finally, our data showed that dietary intake according to food diaries did not change during the study. This strongly suggests that our findings were not influenced by changes in eating habits, since the participants maintained their usual diet.
Some limitations need to be addressed. First, the current study was not sufficiently powered to perform subgroup analyses, since the subgroup analyses were not included in our main analyses, on which the sample size calculation was based. Therefore, these analyses are exploratory and hypothesis generating and must be confirmed by further RCTs. Second, we did not measure 24‐hour ambulatory blood pressure, which is generally a more accurate method to measure the blood pressure. Instead, we measured office blood pressure 4 times according to a strict protocol. 33 Furthermore, it is well known that magnesium is the second most abundant intracellular cation. However, we did not study intracellular magnesium concentrations. It would therefore have been very interesting if we had measured the intracellular concentration of magnesium. Unfortunately, this was not included in the study protocol, and we did not collect samples to allow for measurement of the intracellular magnesium concentration. It would be interesting if future studies could include such measurements. Another limitation is that we did not record the direct carotid‐femoral distance, as recommended by the European Network for Non‐invasive Investigation of Large Arteries, 22 but rather the distance suprasternal notch and the umbilicus as required for calculation of c‐fPWV by the SphygmoCor software that we used. It should, however, be noted that a strong correlation of 0.97 between c‐fPWV calculated on the basis of 80% of the direct carotid‐femoral distance and c‐fPWV calculated on the basis of the suprasternal notch distance and the umbilicus has been reported. 34 Finally, the clinical measurements in the current study were performed by 3 investigators, of which 1 investigator performed the vast majority of the measurements and the other 2 were appointed as co‐operators. Although all the co‐operators were well trained by the main operator for several weeks, it may have introduced interoperator variability. However, intrasubject variability was minimized by using the same operator for each single participant as much as possible.
Conclusions
In this RCT conducted in 164 individuals who were overweight or slightly obese, administering 450 mg of magnesium per day in an organic form (magnesium citrate) for 24 weeks did not change arterial stiffness or blood pressure. Furthermore, the inorganic formulations magnesium oxide and magnesium sulfate had similar nonsignificant effects on arterial stiffness and blood pressure. This indicates that magnesium supplements may not have beneficial effects on arterial stiffness, at least not in subjects with normal arterial stiffness values. It should be further elucidated whether long‐term oral magnesium supplementation is effective in individuals with increased arterial stiffness, such as patients with chronic kidney disease.
Sources of Funding
This study was supported by funding from the Nedmag Industries Mining and Manufacturing BV and the NIGRAM2+ collaboration project, financed by the PPP Allowance, made available by Top Sector Life Sciences & Health to the Dutch Kidney Foundation to stimulate public‐private partnerships. Nedmag Industries Mining and Manufacturing BV and the NIGRAM2+ collaboration project had no input in the study design, data collection, analyses, or writing and submission of the article.
Disclosures
F. Goorman and R.M. Danel are employees of Nedmag Industries Mining and Manufacturing BV and Magnesium Health Institute, respectively. The remaining authors have no disclosures to report.
Supporting information
Tables S1–S9
Figure S1
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.021783
For Sources of Funding and Disclosures, see page 16.
References
- 1. Mattace‐Raso FUS, van der Cammen TJM, Hofman A, van Popele NM, Bos ML, Schalekamp MADH, Asmar R, Reneman RS, Hoeks APG, Breteler MMB, et al. Arterial stiffness and risk of coronary heart disease and stroke. Circulation. 2006;113:657–663. doi: 10.1161/CIRCULATIONAHA.105.555235 [DOI] [PubMed] [Google Scholar]
- 2. Zieman SJ, Melenovsky V, Kass DA. Mechanisms, pathophysiology, and therapy of arterial stiffness. Arterioscler Thromb Vasc Biol. 2005;25:932–943. doi: 10.1161/01.ATV.0000160548.78317.29 [DOI] [PubMed] [Google Scholar]
- 3. Dengo AL, Dennis EA, Orr JS, Marinik EL, Ehrlich E, Davy BM, Davy KP. Arterial destiffening with weight loss in overweight and obese middle‐aged and older adults. Hypertension. 2010;55:855–861. doi: 10.1161/HYPERTENSIONAHA.109.147850 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nordstrand N, Gjevestad E, Hertel JK, Johnson LK, Saltvedt E, Røislien J, Hjelmesæth J. Arterial stiffness, lifestyle intervention and a low‐calorie diet in morbidly obese patients—a nonrandomized clinical trial. Obesity. 2013;21:690–697. doi: 10.1002/oby.20099 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Del Gobbo LC, Imamura F, Wu JHY, de Oliveira Otto MC, Chiuve SE, Mozaffarian D. Circulating and dietary magnesium and risk of cardiovascular disease: a systematic review and meta‐analysis of prospective studies. Am J Clin Nutr. 2013;98:160–173. doi: 10.3945/ajcn.112.053132 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. de Baaij JHF, Hoenderop JGJ, Bindels RJM. Magnesium in man: implications for health and disease. Physiol Rev. 2015;95:1–46. doi: 10.1152/physrev.00012.2014 [DOI] [PubMed] [Google Scholar]
- 7. Schutten JC, Joosten MM, de Borst MH, Bakker SJL. Magnesium and blood pressure: a physiology‐based approach. Adv Chronic Kidney Dis. 2018;25:244–250. doi: 10.1053/j.ackd.2017.12.003 [DOI] [PubMed] [Google Scholar]
- 8. ter Braake AD, Tinnemans PT, Shanahan CM, Hoenderop JGJ, de Baaij JHF. Magnesium prevents vascular calcification in vitro by inhibition of hydroxyapatite crystal formation. Sci Rep. 2018;8:2069. doi: 10.1038/s41598-018-20241-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bai Y, Zhang J, Xu J, Cui L, Zhang H, Zhang S, Feng X. Magnesium prevents β‐glycerophosphate‐induced calcification in rat aortic vascular smooth muscle cells. Biomed Reports. 2015;3:593–597. doi: 10.3892/br.2015.473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Joris PJ, Plat J, Bakker SJ, Mensink RP. Long‐term magnesium supplementation improves arterial stiffness in overweight and obese adults: results of a randomized, double‐blind, placebo‐controlled intervention trial. Am J Clin Nutr. 2016;103:1260–1266. doi: 10.3945/ajcn.116.131466 [DOI] [PubMed] [Google Scholar]
- 11. Schlieper G, Westenfeld R, Brandenburg V, Ketteler M. Vascular calcification in patients with kidney disease: inhibitors of calcification in blood and urine. Semin Dial. 2007;20:113–121. doi: 10.1111/j.1525-139X.2007.00257.x [DOI] [PubMed] [Google Scholar]
- 12. Yao Z, Xu Y, Ma W, Sun X‐Y, Jia S, Zheng Y, Liu X, Fan Y, Wang C. Magnesium citrate protects against vascular calcification in an adenine‐induced chronic renal failure rat model. J Cardiovasc Pharmacol. 2018;72:270–276. doi: 10.1097/FJC.0000000000000590 [DOI] [PubMed] [Google Scholar]
- 13. Zhang X, Li Y, Del Gobbo LC, Rosanoff A, Wang J, Zhang W, Song Y. Effects of magnesium supplementation on blood pressure: a meta‐analysis of randomized double‐blind placebo‐controlled trials. Hypertens. 2016;68:324–333. doi: 10.1161/HYPERTENSIONAHA.116.07664 [DOI] [PubMed] [Google Scholar]
- 14. Kass L, Weekes J, Carpenter L. Effect of magnesium supplementation on blood pressure: a meta‐analysis. Eur J Clin Nutr. 2012;66:411–418. doi: 10.1038/ejcn.2012.4 [DOI] [PubMed] [Google Scholar]
- 15. Schutten JC, Joris PJ, Mensink RP, Danel RM, Goorman F, Heiner‐Fokkema MR, Weersma RK, Keyzer CA, de Borst MH, Bakker SJL. Effects of magnesium citrate, magnesium oxide and magnesium sulfate supplementation on arterial stiffness in healthy overweight individuals: a study protocol for a randomized controlled trial. Trials. 2019;20:295. doi: 10.1186/s13063-019-3414-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kappeler D, Heimbeck I, Herpich C, Naue N, Höfler J, Timmer W, Michalke B. Higher bioavailability of magnesium citrate as compared to magnesium oxide shown by evaluation of urinary excretion and serum levels after single‐dose administration in a randomized cross‐over study. BMC Nutr. 2017;3:7. doi: 10.1186/s40795-016-0121-3 [DOI] [Google Scholar]
- 17. Coudray C, Rambeau M, Feillet‐Coudray C, Gueux E, Tressol JC, Mazur A, Rayssiguier Y. Study of magnesium bioavailability from ten organic and inorganic Mg salts in Mg‐depleted rats using a stable isotope approach. Magnes Res. 2005;18:215–223. [PubMed] [Google Scholar]
- 18. Zhang X, Del Gobbo LC, Hruby A, Rosanoff A, He K, Dai Q, Costello RB, Zhang W, Song Y. The circulating concentration and 24‐h urine excretion of magnesium dose‐ and time‐dependently respond to oral magnesium supplementation in a meta‐analysis of randomized controlled trials. J Nutr. 2016;146:595–602. doi: 10.3945/jn.115.223453 [DOI] [PubMed] [Google Scholar]
- 19. Wildman RP, Mackey RH, Bostom A, Thompson T, Sutton‐Tyrrell K. Measures of obesity are associated with vascular stiffness in young and older adults. Hypertension. 2003;42:468–473. doi: 10.1161/01.HYP.0000090360.78539.CD [DOI] [PubMed] [Google Scholar]
- 20. Phillips P, Pain R. Correcting the calcium. BMJ. 1977;1:598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Grundy SM, Stone NJ, Bailey AL, Beam C, Birtcher KK, Blumenthal RS, Braun LT, de Ferranti S, Faiella‐Tommasino J, Forman DE, et al. 2018 AHA/ACC/AACVPR/AAPA/ABC/ACPM/ADA/AGS/APhA/ASPC/NLA/PCNA guideline on the management of blood cholesterol: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines. Circulation. 2019;139:e1082–e1143. doi: 10.1161/CIR.0000000000000625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Van Bortel LM, Laurent S, Boutouyrie P, Chowienczyk P, Cruickshank JK, De Backer T, Filipovsky J, Huybrechts S, Mattace‐Raso FUS, Protogerou AD, et al. Expert consensus document on the measurement of aortic stiffness in daily practice using carotid‐femoral pulse wave velocity. J Hypertens. 2012;30:445–448. doi: 10.1097/HJH.0b013e32834fa8b0 [DOI] [PubMed] [Google Scholar]
- 23. Marques BCAA, Klein MRST, da Cunha MR, de Souza MS, de Paula NL, de Paula T, Corrêa FM, Oigman W, Neves MF. Effects of oral magnesium supplementation on vascular function: a systematic review and meta‐analysis of randomized controlled trials. High Blood Press Cardiovasc Prev. 2020;27:19–28. doi: 10.1007/s40292-019-00355-z [DOI] [PubMed] [Google Scholar]
- 24. Walker AF, Marakis G, Christie S, Byng M. Mg citrate found more bioavailable than other Mg preparations in a randomised, double‐blind study. Magnes Res. 2003;16:183–191. [PubMed] [Google Scholar]
- 25. Lindberg JS, Zobitz MM, Poindexter JR, Pak CYC. Magnesium bioavailability from magnesium citrate and magnesium oxide. J Am Coll Nutr. 1990;9:48–55. doi: 10.1080/07315724.1990.10720349 [DOI] [PubMed] [Google Scholar]
- 26. Cunha AR, D’El‐Rei J, Medeiros F, Umbelino B, Oigman W, Touyz RM, Neves MF. Oral magnesium supplementation improves endothelial function and attenuates subclinical atherosclerosis in thiazide‐treated hypertensive women. J Hypertens. 2017;35:89–97. doi: 10.1097/HJH.0000000000001129 [DOI] [PubMed] [Google Scholar]
- 27. Toussaint ND, Lau KK, Strauss BJ, Polkinghorne KR, Kerr PG. Associations between vascular calcification, arterial stiffness and bone mineral density in chronic kidney disease. Nephrol Dial Transplant. 2007;23:586–593. doi: 10.1093/ndt/gfm660 [DOI] [PubMed] [Google Scholar]
- 28. Food and Nutrition Board I of M . Dietary Reference Intakes for Calcium, Phosphorus, Magnesium, Vitamin D, and Fluoride. Washington (DC): National Academies Press (US); 1997:190–249. [PubMed] [Google Scholar]
- 29. Euser AG, Cipolla MJ. Magnesium sulfate for the treatment of eclampsia. Stroke. 2009;40:1169–1175. doi: 10.1161/STROKEAHA.108.527788 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Lutsey P, Chen L, Eaton A, Jaeb M, Rudser K, Neaton J, Alonso A. A pilot randomized trial of oral magnesium supplementation on supraventricular arrhythmias. Nutrients. 2018;10:884. doi: 10.3390/nu10070884 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Roguin Maor N, Alperin M, Shturman E, Khairaldeen H, Friedman M, Karkabi K, Milman U. Effect of magnesium oxide supplementation on nocturnal leg cramps. JAMA Intern Med. 2017;177:617. doi: 10.1001/jamainternmed.2016.9261 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Laurent S, Cockcroft J, Van Bortel L, Boutouyrie P, Giannattasio C, Hayoz D, Pannier B, Vlachopoulos C, Wilkinson I, Struijker‐Boudier H. Expert consensus document on arterial stiffness: methodological issues and clinical applications. Eur Heart J. 2006;27:2588–2605. doi: 10.1093/eurheartj/ehl254 [DOI] [PubMed] [Google Scholar]
- 33. Burkard T, Mayr M, Winterhalder C, Leonardi L, Eckstein J, Vischer AS. Reliability of single office blood pressure measurements. Heart. 2018;104:1173–1179. doi: 10.1136/heartjnl-2017-312523 [DOI] [PubMed] [Google Scholar]
- 34. Sugawara J, Hayashi K, Yokoi T, Tanaka H. Carotid–femoral pulse wave velocity: impact of different arterial path length measurements. Artery Res. 2009;4:27. doi: 10.1016/j.artres.2009.11.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S9
Figure S1


