Abstract
Background
A minority of acute coronary syndrome (ACS) cases are associated with ventricular arrhythmias (VA) and/or cardiac arrest (CA). We investigated the effect of VA/CA at the time of ACS on long‐term outcomes.
Methods and Results
We analyzed routine clinical data from 5 National Health Service trusts in the United Kingdom, collected between 2010 and 2017 by the National Institute for Health Research Health Informatics Collaborative. A total of 13 444 patients with ACS, 376 (2.8%) of whom had concurrent VA, survived to hospital discharge and were followed up for a median of 3.42 years. Patients with VA or CA at index presentation had significantly increased risks of subsequent VA during follow‐up (VA group: adjusted hazard ratio [HR], 4.15 [95% CI, 2.42–7.09]; CA group: adjusted HR, 2.60 [95% CI, 1.23–5.48]). Patients who suffered a CA in the context of ACS and survived to discharge also had a 36% increase in long‐term mortality (adjusted HR, 1.36 [95% CI, 1.04–1.78]), although the concurrent diagnosis of VA alone during ACS did not affect all‐cause mortality (adjusted HR, 1.03 [95% CI, 0.80–1.33]).
Conclusions
Patients who develop VA or CA during ACS who survive to discharge have increased risks of subsequent VA, whereas those who have CA during ACS also have an increase in long‐term mortality. These individuals may represent a subgroup at greater risk of subsequent arrhythmic events as a result of intrinsically lower thresholds for developing VA.
Keywords: acute coronary syndrome, cardiac arrest, ventricular arrhythmia
Subject Categories: Myocardial Infarction
Nonstandard Abbreviations and Acronyms
- CA
cardiac arrest
- NIHR
National Institute for Health Research
- VA
ventricular arrhythmia
Clinical Perspective
What Is New?
Patients who develop ventricular arrhythmia during acute coronary syndrome who survive to discharge have increased risks of subsequent ventricular arrhythmia.
Cardiac arrest in the context of acute coronary syndrome is associated with an increased incidence of subsequent ventricular arrhythmia and long‐term mortality.
What Are the Clinical Implications?
Individuals who develop ventricular arrhythmia and/or cardiac arrest during acute coronary syndrome may represent a subgroup of patients who have intrinsically lower thresholds to developing ventricular arrhythmia.
A minority of acute coronary syndrome (ACS) patients who survive to hospital admission are associated with ventricular arrhythmia (VA), a subset of which cause cardiac arrest (CA). 1 Acute myocardial ischemia leads to a series of progressive electrophysiological changes at the cellular level that predispose to VA, 2 although it remains unclear why only a minority of patients with ACS develop VA, whereas the vast majority do not. 3
There are data to suggest that patients who present with VA during ACS may represent a subgroup of patients with greater intrinsic risks of subsequent arrhythmic events. A family history of sudden cardiac death increases the likelihood of occurrence of ventricular fibrillation (VF) during ACS, 4 and genome‐wide association studies have demonstrated that the propensity to VF during ACS is in part genetically mediated. 5 However, although clinical guidelines recommend implantable cardioverter defibrillators (ICDs) for secondary prevention in patients who develop VA causing hemodynamic instability or CA, individuals who develop VA or CA specifically in the context ACS do not qualify as ACS is considered a reversible cause. 6 , 7 , 8
The current prognostic significance of VA during ACS is unclear, and it is specifically unknown if VA during ACS predicts future VA occurrence. Although patients with ST‐segment–elevation myocardial infarction (STEMI) have been more broadly studied, 9 , 10 , 11 , 12 long‐term follow‐up data of patients with VA in the context of non–ST‐segment–elevation ACS are sparse, with recent studies being significantly smaller with relatively short‐term follow‐up or studying specific subgroups. 13 , 14 , 15 , 16 , 17 , 18
Using a large database of >250 000 patients with troponin measurements, we sought to describe the long‐term prognosis of patients presenting with ACS, with or without VA, who survive to hospital discharge. A secondary objective was to study the impact of VA on in‐hospital mortality. We hypothesized that patients who present with VA or CA at the time of ACS are at greater risk of subsequent VA and have increased long‐term mortality.
METHODS
Data Sharing
The data sets generated or analyzed or both during this study are not publicly available owing to ethical restrictions.
Ethical Approval
The study database was approved by the London‐South East Research Ethics Committee (reference number 16/HRA/3327). The requirement for individual patient consent was waived. This analysis was approved by the National Institute for Health Research (NIHR) Health Informatics Collaborative steering committee.
The NIHR Health Informatics Collaborative database consists of routinely collected data, currently from 10 collaborating National Health Service Trusts. For this study, data were collected from 5 NHS trusts (Imperial College Healthcare, University College Hospital, Oxford University Hospital, King’s College Hospital, and Guy’s and St Thomas’ Hospital), all tertiary centers with emergency departments. As previously described, the cohort inclusion criterion was any patient who had their troponin level measured for any reason (n=257 948) at each of the 5 academic centers between 2010 (2008 for University College Hospital) and 2017. 19 , 20 , 21 For patients with >1 hospital episode, only the first episode in which troponin was measured was eligible. There were no other exclusion criteria. Patients meeting inclusion criteria were followed up using routinely collected data until death or censoring on April 1, 2017. Life status was ascertained using routinely collected data on the National Health Service Personal Demographics Service, which incorporates national death registry information and local notifications. For the readmissions outcome, only readmissions to the same hospital as the initial presentation were available.
Diagnoses were assigned on the basis of International Classification of Diseases, Tenth Revision (ICD‐10) codes. We classified patients as having had an ACS or CA on the basis of the ICD‐10 codes listed in the supplemental material (Tables S1–S3). ACS included the diagnoses of STEMI, non–ST‐segment–elevation myocardial infarction, and unstable angina. 22 , 23 A patient was classified as having had VA if they had the ICD‐10 codes for reentry VA, ventricular tachycardia (VT) or VF, and flutter. Comorbidities, risk factors, and implantation of a device was also determined using ICD‐10 codes. For adjusted analyses, peak troponin was used. As the troponin assay used differed between study sites, a normalized value of peak troponin as a multiple of the assay upper limit of normal was used. If patients had both VT and VF, they were assigned to the VF group for subgroup analysis.
A small proportion of cases had missing data for covariates of interest. These data were expected to be missing at random, and given the small proportion (1%), these were handled with listwise deletion for the adjusted analysis. To avoid introducing unnecessary bias, the unadjusted analyses included all cases, including those with missing data in the covariate fields.
Statistical Analysis
Descriptive statistics are displayed as medians (interquartile ranges) for continuous variables and numbers (percentages) for categorical variables. Kaplan–Meier plots were used to display cumulative mortality. The log‐rank test was used to compare survival curves. In the Kaplan–Meier analyses, pairwise comparisons between groups were performed with the Benjamini and Hochberg correction for multiple testing (Figure 4). 24 Cox proportional hazards regression modeling was used to estimate mortality hazard ratios (HRs) in patients with and without VA/CA. To model nonlinear relationships, we used restricted cubic splines for Cox regression. Preliminary investigation suggested that 4 knots should be used to model troponin level in the restricted cubic spline analyses. Log transformation was applied to peak troponin because of the positive skew of troponin values. We performed multivariable analyses adjusting for sex, ethnicity, hemoglobin level, white cell count, platelet count, sodium level, potassium level, creatinine level, peak troponin (multiple of the assay upper limit of normal), family history of cardiovascular disease, current smoker, diabetes, hypertension, hypercholesterolemia, heart failure, previous ischemic heart disease, previous myocardial infarction, atrial fibrillation, aortic stenosis, chronic kidney disease, malignancy, obstructive lung disease, type of ACS, percutaneous coronary intervention (PCI), coronary artery bypass graft, and implantation of device. The proportional hazards assumption was tested using Schoenfeld residuals. There was a nonsignificant relationship between the Schoenfeld residuals and time for all of the univariate analyses. There was evidence of nonproportionality for some covariates in the multivariable analyses (Table S4). Recent work suggests that virtually all real‐world clinical data sets will violate the proportional hazards assumptions if sufficiently powered and that statistical tests for the proportional hazards assumption may be unnecessary. 25 In line with these recommendations, the HR from our Cox models should be interpreted as a weighted average of the true HRs during the follow‐up period. Negative binomial regression was performed to compare number of episodes of VA during follow‐up. Patients with any missing characteristic data were excluded from analysis of adjusted Cox proportional hazards models. Statistical analyses were performed with R 4.0.0 statistical package (R Core Team, Vienna, Austria).
Figure 4. Kaplan–Meier survival curves according to presence or absence of VA stratified by type of ACS diagnosis.
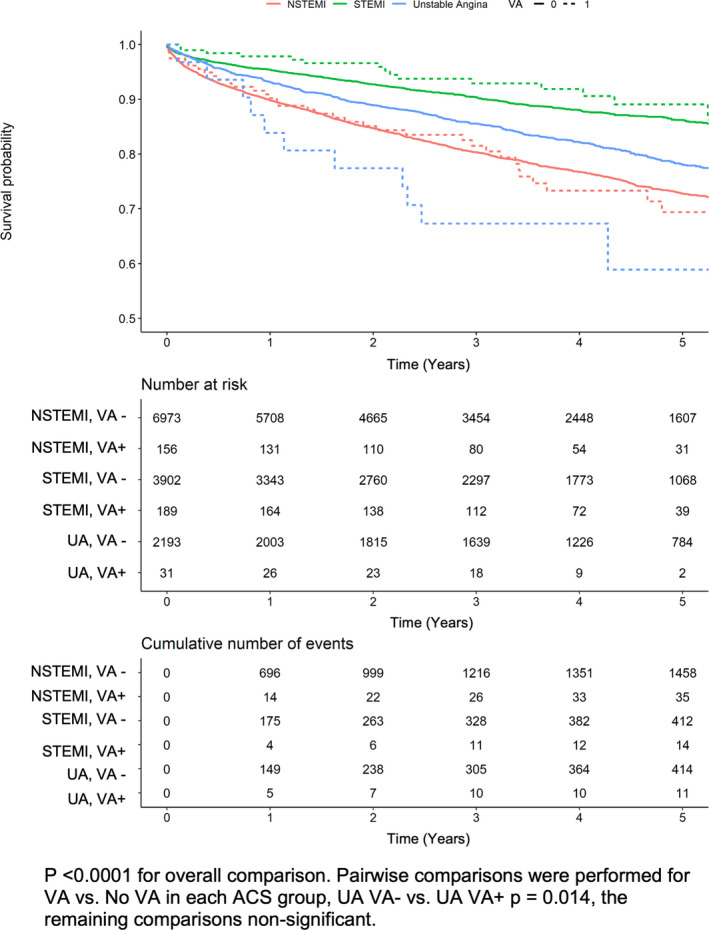
Data presented are for a landmark analysis of patients with ACS who survive to discharge. VA in the context of UA is associated with increased long‐term mortality. Curves compared using log‐rank statistic. ACS indicates acute coronary syndrome; NSTEMI, non–ST‐segment–elevation myocardial infarction; STEMI, ST‐segment–elevation myocardial infarction; UA, unstable angina; and VA, ventricular arrhythmia.
The NIHR Health Informatics Collaborative data set was registered with ClinicalTrials.gov, NCT03507309.
RESULTS
Patient Characteristics
A total of 14 468 patients had a diagnosis of ACS, 13 444 of whom survived to hospital discharge (Figure 1). Of the 14468 patients with ACS, 461 (3.2%) also had a diagnosis of a VA, whereas 508 (3.5%) suffered a CA. Of those surviving to discharge, 376 (2.8%) had a concurrent diagnosis of a VA, whereas 280 (2.1%) had a CA. The baseline characteristics grouped by presence or absence of VA are displayed in Table 1 and by type of ACS in Table S5. At a median follow‐up of 3.42 years (interquartile range, 1.69–5.10 years), there were 2480 (18.4%) deaths. In the subgroup of patients with STEMI (n=4091), 3448 (84%) underwent PCI. Of those who underwent PCI, 3066 (89%) underwent PCI on the same day as the first troponin measurement.
Figure 1. Flow of study cohort: 257 948 patients were eligible for inclusion based on the first troponin measurement during study period.
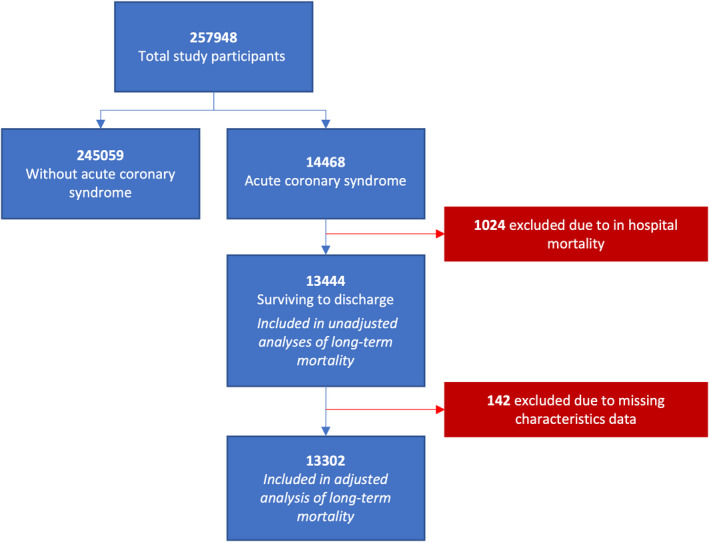
Table 1.
Characteristics of Patients According to Whether VAs Were Diagnosed at Index Presentation in a Landmark Analysis of Patients With ACS Who Survive to Discharge
| No VAs (n=13 068) | VAs (n=376) | P value | Missing (n) | |
|---|---|---|---|---|
| Demographics | ||||
| Age, y | 69 (59–80) | 67 (55–76) | <0.001 | 0 |
| Male sex, n (%) | 9149 (70) | 300 (79.8) | <0.001 | 0 |
| Ethnicity, n (%) | 0.729 | 0 | ||
| Caucasian | 7828 (59.9) | 222 (59) | ||
| South Asian | 955 (7.3) | 31 (8.2) | ||
| Black | 535 (4.1) | 12 (3.2) | ||
| Other | 3750 (28.7) | 111 (29.5) | ||
| Hematology and biochemistry | ||||
| Hemoglobin (g/dL) | 13.5 (12.0–14.7) | 13.8 (12.3–15) | 0.009 | 87 |
| White cell count (×109/L) | 9.6 (7.5–12.4) | 12 (9.5–15.8) | <0.001 | 87 |
| Platelet count (×109/L) | 228 (188–273) | 236.5 (187–287) | 0.156 | 89 |
| Sodium (mmol/L) | 138 (136–140) | 138.5 (136–140) | 0.017 | 75 |
| Potassium (mmol/L) | 4.2 (3.9–4.5) | 4.2 (3.8–4.6) | 0.634 | 108 |
| Creatinine (μmol/L) | 82.00 (70–101) | 88.5 (74–109) | <0.001 | 72 |
| Peak troponin (×ULN) | 64.67 (5.6–437.38) | 308.4 (55.1–1184.8) | <0.001 | 0 |
| Comorbidities/cardiovascular risk factors, n (%) | ||||
| Hypertension | 5127 (39.2) | 128 (34.0) | 0.048 | 0 |
| Family history of CAD | 1802 (13.8) | 44 (11.7) | 0.279 | 0 |
| Previous MI | 759 (5.8) | 26 (6.9) | 0.429 | 0 |
| Diabetes | 3035 (23.2) | 59 (15.7) | 0.001 | 0 |
| Hypercholesterolemia | 4983 (38.1) | 117 (31.1) | 0.007 | 0 |
| Heart failure | 1858 (14.2) | 108 (28.7) | <0.001 | 0 |
| Atrial fibrillation | 1104 (8.4) | 40 (10.6) | 0.159 | 0 |
| Aortic stenosis | 322 (2.5) | 2 (0.5) | 0.025 | 0 |
| Chronic kidney disease | 691 (5.3) | 22 (5.9) | 0.716 | 0 |
| Malignancy | 742 (5.7) | 10 (2.7) | 0.017 | 0 |
| Obstructive lung disease | 98 (0.7) | 1 (0.3) | 0.438 | 0 |
| Smoker | 3046 (23.3) | 106 (28.2) | 0.032 | 0 |
| Ischemic heart disease | 8710 (66.7) | 283 (75.3) | 0.001 | 0 |
| ACS type, n (%) | <0.001 | 0 | ||
| STEMI | 3902 (29.9) | 189 (50.3) | ||
| NSTEMI | 6973 (53.4) | 156 (41.5) | ||
| Unstable angina | 2193 (16.8) | 31 (8.2) | ||
| Treatment, n (%) | 0 | |||
| CABG | 1253 (9.6) | 22 (5.9) | 0.019 | |
| PCI | 7797 (59.7) | 281 (74.7) | <0.001 | |
| Implantation of device | 72 (0.6) | 4 (1.1) | 0.338 | |
| Results | ||||
| Follow‐up, y | 3.45 (1.70–5.13) | 3.36 (1.86–4.71) | 0.194 | |
| Hospital admission duration, d | 3 (2–8) | 6 (3–13) | <0.001 | |
| Mortality, n (%) | 2419 (18.5) | 61 (16.2) | 0.289 | |
| Recurrent VA, n (%) | 122 (0.9) | 18 (4.8) | <0.001 | |
Values are provided as median (interquartile range) unless otherwise stated. ACS indicates acute coronary syndrome; CABG, coronary artery bypass graft; CAD, coronary artery disease; MI, myocardial infarction; NSTEMI, non–ST‐segment–elevation myocardial infarction; PCI, percutaneous coronary intervention; STEMI, ST‐segment–elevation myocardial infarction; ×ULN, multiple of the assay upper limit of normal; and VA, ventricular arrhythmia.
VA During ACS Is Associated With Increased In‐Hospital Mortality But Not With Long‐Term Mortality
Considering all patients with ACS, concurrent VA was associated with a significant increase in in‐hospital mortality (unadjusted HR, 1.96 [95% CI, 1.56–2.45]; adjusted HR, 1.89 [95% CI, 1.49–2.40]; Figure 2; Table 2). However, in patients who survived to hospital discharge, concurrent VA had no effect on all‐cause mortality overall (unadjusted HR, 0.9 [95% CI, 0.7–1.16]; adjusted HR, 1.03 [95% CI, 0.80–1.33]; Figure 3A), nor when stratified by age groups (Figure S1) or in the subgroups of non–ST‐segment–elevation myocardial infarction and STEMI (Figure 4).
Figure 2. VA at time of acute coronary syndrome is associated with increased 30‐day mortality: Kaplan–Meier curves of 30‐day survival according to presence or absence of VAs at index admission in all patients with acute coronary syndrome.
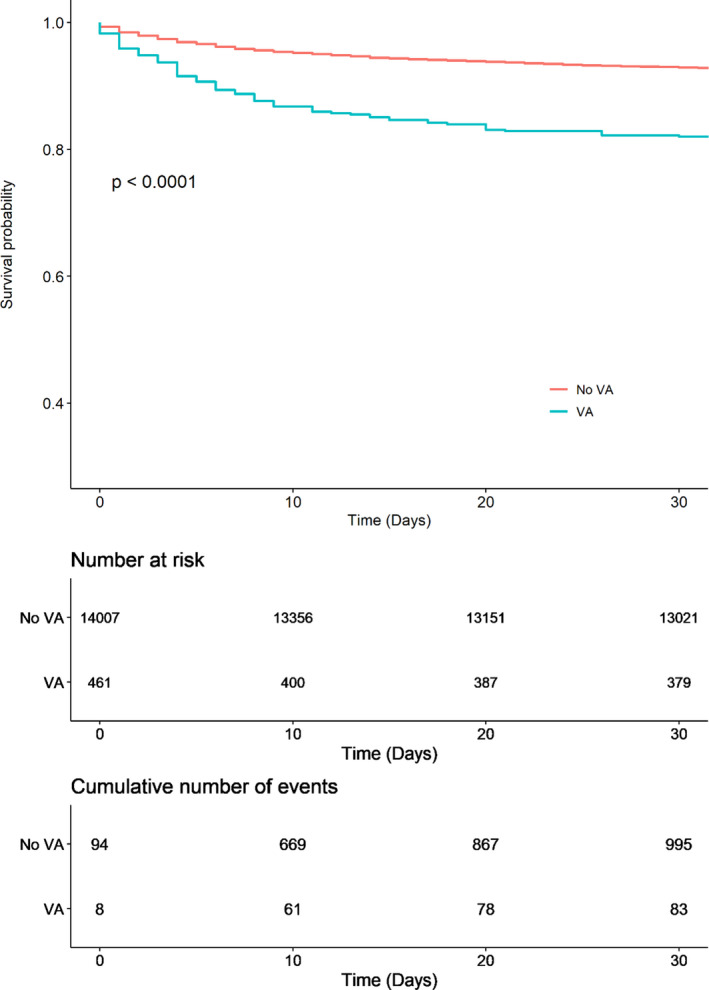
Curves compared using log‐rank statistic. VA indicates ventricular arrhythmia.
Table 2.
Summary Table of Main Cox Proportional Hazards Analyses
| Analysis | Unadjusted | Adjusted* | ||||
|---|---|---|---|---|---|---|
| HR | 95% CI | P value | HR | 95% CI | P value | |
| VA vs no VA | ||||||
| In‐hospital mortality | 1.96 | 1.56–2.45 | <0.0001 | 1.89 | 1.49–2.40 | <0.0001 |
| Long‐term mortality in patients surviving to discharge | 0.90 | 0.70–1.16 | 0.43 | 1.03 | 0.80–1.33 | 0.82 |
| Recurrent VA in patients surviving to discharge | 5.38 | 3.30–8.80 | <0.0001 | 4.15 | 2.42–7.09 | <0.0001 |
| Composite end point of death, VA, or CA in patients surviving to discharge | 1.11 | 0.90–1.40 | 0.355 | 1.24 | 0.98–1.57 | 0.07 |
| CA vs no CA | ||||||
| Long‐term mortality in patients surviving to discharge | 1.31 | 1.01–1.70 | 0.04 | 1.36 | 1.04–1.78 | 0.02 |
| Recurrent VA in patients surviving to discharge | 3.35 | 1.64–6.84 | <0.001 | 2.60 | 1.23–5.48 | 0.01 |
CA indicates cardiac arrest; HR, hazard ratio; and VA, ventricular arrhythmia.
Adjusted for sex, ethnicity, hemoglobin level, white cell count, platelet count, sodium level, potassium level, creatinine level, peak troponin (× upper limit of normal), family history of cardiovascular disease, current smoker, diabetes, hypertension, hypercholesterolemia, heart failure, previous ischemic heart disease, previous myocardial infarction, atrial fibrillation, aortic stenosis, chronic kidney disease, malignancy, obstructive lung disease, type of acute coronary syndrome, percutaneous coronary intervention, coronary artery bypass graft, and implantation of device.
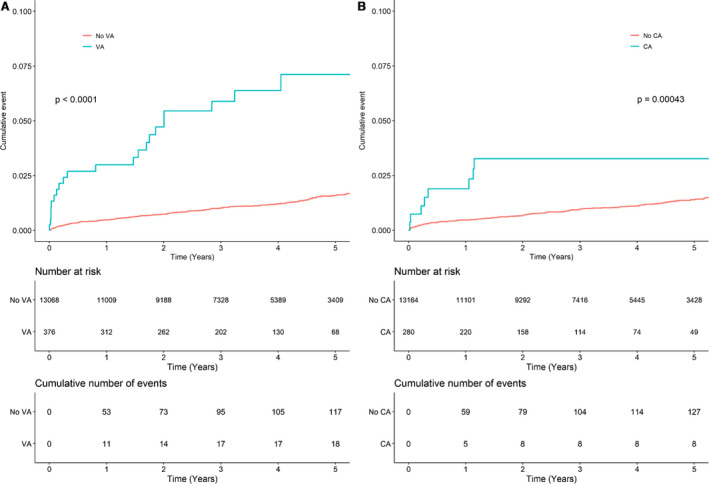
Figure 3. CA at time of acute coronary syndrome is associated with increased long‐term mortality: Kaplan–Meier survival curves in patients with acute coronary syndrome who survive to discharge according to presence or absence of (A) VA or (B) CA at index admission.
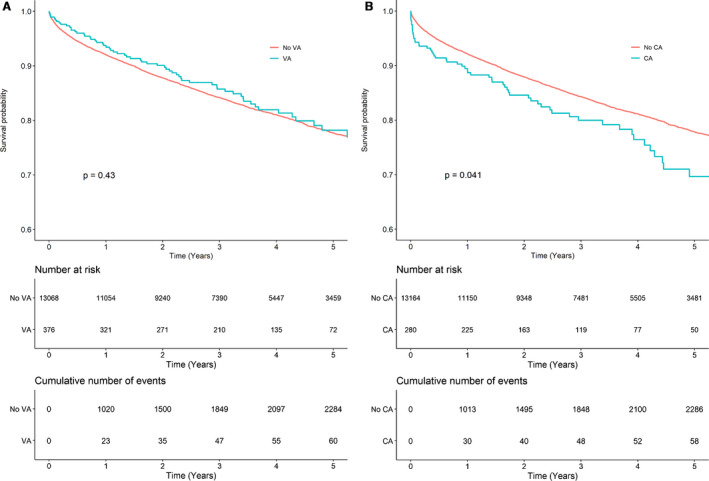
Curves compared using log‐rank statistic. CA indicates cardiac arrest; and VA, ventricular arrhythmia.
In the subgroup of patients with unstable angina (n=2224), VA at index presentation was associated with increased long‐term all‐cause mortality (unadjusted HR, 2.18 [95% CI, 1.20–3.96]; adjusted HR, 2.11 [95% CI, 1.11–3.99]), although the number of patients were small, with only 31 patients in this group having VA at the index presentation (Figure 4). In this unstable angina subgroup, 1011 (45%) patients without VA had PCI or a coronary artery bypass graft, whereas in the VA group the number was 20 (64.5%). This was significantly lower than in the myocardial infarction subgroup where 8039 (73.9%) had PCI in the group without VA and 283 (82%) had PCI in the VA group (P<0.0001 and P<0.02, respectively).
CA During ACS Is Associated With Increased Long‐Term Mortality
In patients who had a diagnosis of ACS who survived to hospital discharge, there remained a 36% increase in long‐term mortality (unadjusted HR, 1.31 [95% CI, 1.01–1.70]; adjusted HR, 1.36 [95% CI, 1.04–1.78]; Figure 3B).
VA or CA During ACS Is Associated With an Increased Risk of Subsequent VA
VA at index presentation significantly increased the risk of VA at follow‐up (unadjusted HR, 5.38 [95% CI, 3.3–8.8]; adjusted HR, 4.15 [95% CI, 2.42–7.09]; adjusted incident rate ratio, 5.54 [95% CI, 2.76–11.13]; Figure 5A) but did not affect the composite end point of death, VA, or CA (unadjusted HR, 1.12 [95% CI, 0.90–1.4]; adjusted HR, 1.24 [95% CI, 0.98–1.57]). Of patients with VA during ACS, 4.8% had subsequent VA during follow‐up, whereas 0.9% of patients who did not have VA during the index ACS admission had subsequent VA. Only a small minority of subsequent VA were in the context of an ACS (3.3% in VA group and 7.6% in the no VA group). CA at index presentation also significantly increased the risk of VA at follow‐up (unadjusted HR, 3.35 [95% CI, 1.64–6.84]; adjusted HR, 2.60 [95% CI, 1.23–5.48]; adjusted incident rate ratio, 1.98 [95% CI, 0.73–5.35]; Figure 5B).
Figure 5. VA or CA at time of acute coronary syndrome are both associated with increased subsequent risks of VA: Kaplan–Meier curves of cumulative time to first VA after discharge in patients with acute coronary syndrome who survive to discharge according to presence or absence of (A) VAs or (B) CA at index admission.
Curves compared using log‐rank statistic. CA indicates cardiac arrest; and VA, ventricular arrhythmia.
Type of VA Does Not Affect Long‐Term Mortality
In an unadjusted subgroup analysis of VA type, patients with VF at the time of ACS had reduced all‐cause mortality compared with patients with VT or no VA (Figure S2); however, after adjusting for confounding factors, this association was no longer seen (unadjusted HR, 0.60 [95% CI, 0.4–0.9]; adjusted HR, 0.82 [95% CI, 0.54–1.24]).
DISCUSSION
We report the largest and most contemporaneous study of the prognostic significance of VA and CA in the context of ACS. Our key findings are (1) VA in the context of ACS is associated with increased in‐hospital mortality and long‐term recurrence of VA but does not increase long‐term mortality and (2) CA in the context of ACS is associated with increased in‐hospital mortality, long‐term recurrence of VA, and long‐term mortality.
VA in the Context of ACS Is Associated With Greater In‐Hospital Mortality and Recurrent VA
In 14 468 patients with ACS, concurrent VA was associated with increased in‐hospital mortality. Patients surviving to discharge had increased risks of recurrent VA. This finding is in agreement with a previous study of 2033 patients, where VT in the context of ACS was associated with increased recurrent VTs. 15 The individuals who develop VA in the context of ACS may represent a subgroup of patients who have intrinsically lower thresholds to developing VA in response to any extrinsic triggers such as ACS and are therefore more likely to have subsequent episodes of VA. Genetic factors in particular may make patients more susceptible to VA. 4 , 5 A genome‐wide association study has identified a locus, rs2824292 at 21q21, that is associated with VF in the context of myocardial infarction. 5 In addition, acquired factors such as burden and distribution of myocardial scarring may predispose certain individuals to recurrent VA. 26
VA in the Context of ACS Is Not Associated With Adverse Long‐Term Prognosis
In the 13 444 patients with an ACS who survived to discharge, VA was not associated with adverse long‐term prognosis. This finding is broadly in agreement with previous data 9 , 10 , 12 , 13 , 16 , 17 but provides data from a cohort that is both more recent and larger in size. In contrast, in a study of patients with non–ST‐segment–elevation myocardial infarction, part of the early glycoprotein IIb/IIIa inhibition in non–ST‐segment elevation acute coronary syndrome (EARLY ACS) trial, VA was found to be associated with both increased 30‐day and 1‐year mortality. 27 The difference in findings may be attributed to differences in the definitions of VA. The EARLY ACS study included VF or VT that was sustained for >30 seconds and/or causing hemodynamic compromise, whereas nonsustained VT could also have been included in our study. In addition, EARLY ACS used a 48‐hour landmark period, whereas our study primarily analyzed patients who survived to discharge. Other possible factors include the time period studied (enrollment for their study was between 2004 and 2008) or the high‐risk population enrolled in EARLY ACS (2 or more criteria out of age ≥60, elevated creatine kinase MB or troponin, ST‐segment depression, or transient elevation) versus the “all‐comers” population in our study. Hai et al found that monomorphic VT was an independent predictor of all‐cause mortality in patients with ACS who survived to discharge, but nonmonomorphic VT was not. 15 In adjusted analyses, we found no difference between VT versus VF; however, in our study we were unable to differentiate between polymorphic and monomorphic VT.
We hypothesize that competing causes of death in a relatively high‐risk population may explain the increase in recurrent VA without increase in mortality in the group of patients with VA during the index admission. Unfortunately, we were unable to test this hypothesis as we were unable to ascertain the causes of death in this data set. The trials of early ICD after myocardial infarction with high‐risk features for VA show a similar phenomenon. Both trials demonstrated a significant reduction in arrhythmic death in the ICD group but did not show an overall reduction in all‐cause mortality attributed to more nonarrhythmic deaths in the ICD arms. 28 , 29
CA in the Context of ACS Is Associated With an Increased Recurrence of VA and Both In‐Hospital and Long‐Term Mortality
Because of the limitations of ICD‐10 coding, we were unable to accurately differentiate shockable (VT or VF) versus nonshockable (bradyarrhythmia or pulseless electrical activity) rhythms during CA. However, previous data from a similar cohort suggested that 89.6% of patients who have out‐of‐hospital CA in the context of ACS have VT or VF as the presenting rhythm, 1 which provide the basis for our assumption that the vast majority of CAs at the time of ACS in our study are attributed to VAs.
In our study, CA in the context of ACS was associated with adverse in‐hospital and long‐term prognosis, with increased recurrence of VA after discharge and increased long‐term mortality. Previous studies have primarily studied VF in the context of ACS and found increased in‐hospital mortality but no increase in long‐term mortality. 10 , 13 , 16 In contrast, our study, which did find an increase in long‐term mortality, also included CA attributed to VT, and potentially a small proportion of nonshockable rhythms causing CA. This group of patients with CA during ACS do not currently meet criteria for ICD implantation under primary or secondary prevention indications if fully revascularized. Although we do not have data on the left ventricular ejection fraction of the patients in our study, we did adjust for ICD‐10 codes of heart failure to reduce the effect of this confounding factor.
Our findings may have significant implications for this subgroup of patients with ACS. Given the increase in recurrent VA and long‐term mortality in this group, ICD implantation may be of benefit. However, this concept requires further systematic study as, because of the competing causes of death, there is the possibility that an ICD may reduce arrhythmic death without reducing all‐cause mortality, by converting the mode of death from arrhythmic death to nonarrhythmic death.
VA in the Context of Unstable Angina Is Associated With an Adverse Long‐Term Prognosis
In the subgroup of patients with unstable angina who survived to discharge, concurrent VA during the unstable angina episode was associated with adverse long‐term prognosis. In the era of high‐sensitivity troponin, VA in the context of unstable angina is a rare occurrence and therefore it may not be well suited to a cohort study design, and the very small sample in this study may therefore not be adequately represented in this study to make definitive conclusions.
However, in agreement with our findings, a previous study of 543 patients with unstable angina did reveal an association between VA in the context of unstable angina and in‐hospital and 6‐month all‐cause mortality. 30 It is possible that the adverse prognosis relates to the reduced rate of PCI in the unstable angina subgroup. Without treatment of the lesion responsible for the ACS, the “reversible” cause to which the VA is attributed to has not been truly reversed, thus predisposing to further VA and mortality. It is possible that a portion of this subgroup suffered VA caused by coronary vasospasm, which unlike STEMI and non–ST‐segment–elevation myocardial infarction, is not amenable to PCI and can be poorly treated, leaving these patients susceptible to recurrent episodes and future VA. 31
Limitations
This study benefits from data collected from a large number of patients from multiple UK hospitals. There are, however, some limitations. These real‐world data are likely to be representative of the UK population, and our findings may not be generalizable to other populations and health care systems. There can be difficulty in accounting for potential confounding factors because of the incomplete nature of, or inaccuracies in, the data. In particular, there were insufficient data on left ventricular ejection fraction, coronary anatomy, and results of revascularization to include in our models. Where an ICD was implanted, we do not have data regarding the indication, timing of implant, or therapies from the device. We included ICD‐10 codes for heart failure to adjust for this important confounder. We were also unable to accurately determine which patients underwent primary PCI. However, a large percentage of patients with STEMI had PCI on the same day as the first troponin measurement, which is likely to indicate primary PCI. We were also unable to distinguish polymorphic from monomorphic VT, accurately account for the type of CA (shockable versus nonshockable) at index presentation or follow‐up, determine the timing of arrhythmic events (eg, whether occurring only in the first 48 hours after the index event or not), or establish whether VT was sustained or nonsustained, and these factors all may have prognostic implications. It is possible that some patients with ACS were not coded as also having VAs; however, our VT/VF incidence is comparable with trials and prospective registries (3.2% in our study versus 1.5‐5.8% in others 3 , 11 , 27 , 32 ). Given that only readmissions to the same hospital are included in this data set, we may be underestimating the incidence of secondary outcomes; however, the most important end point, all‐cause mortality, is free from this limitation. Unfortunately, we were unable to determine the cause of death in this cohort. Patients with VAs are likely to have had different medications given during the hospital admission and on discharge, and the data on medications were not available. Lastly, the ICD‐10 code we used for device implantation is not specific to the type of device; therefore, it is unknown if the device was an ICD, pacemaker, or other device.
CONCLUSIONS
Patients who develop VA during ACS who survive to discharge have increased risks of subsequent VA, although this did not translate into an increase in all‐cause mortality. CA in the context of ACS is associated with an increased incidence of subsequent VA and long‐term mortality. These individuals who develop VA and/or CA during ACS may represent a subgroup of patients who have intrinsically lower thresholds to developing VA and are more likely to have subsequent episodes of VA. Future studies are warranted to determine how the risk of recurrent VA in this cohort may be reduced and whether an ICD should be considered for patients who present with CA in the context of ACS and survive to hospital discharge.
Sources of Funding
Dr Sau is supported by an NIHR Academic Clinical Fellowship (ACF‐2019‐21‐001). Dr Ng and Dr Peters are supported by the British Heart Foundation (BHF; RG/16/3/32175 and PG/16/17/32069). Dr Kaura is funded by a BHF clinical research training fellowship (FS/20/18/34972). Dr Elliott and H. Hemingway received Health Data Research funding. Dr R.S. Patel is funded by a BHF intermediate fellowship (FS/14/76/30933). Dr A.D. Shah is funded by a THIS Institute postdoctoral fellowship. Dr A.M. Shah is funded by a BHF Professorship (CH/1999001/11735). Dr Mayet is supported by the BHF Imperial Centre for Research Excellence (RE/18/4/34215).
Disclosures
None.
Supporting information
Tables S1‐S5
Figures S1‐S2
Acknowledgments
This article reports independent research led and funded by the National Institute for Health Research (NIHR) Imperial Biomedical Research Centre (BRC), as part of the NIHR Health Informatics Collaborative with the NIHR Oxford BRC, the NIHR University College London Hospitals BRC, the NIHR Guy’s & St Thomas’ BRC and the NIHR Cambridge BRC. The views expressed in this publication are those of the authors and not necessarily those of the National Health Service, the NIHR or the Department of Health. This research was enabled by the Imperial Clinical Analytics Research and Evaluation (iCARE) environment and used the iCARE team and data resources (https://imperialbrc.nihr.ac.uk/facilities/icare/).
For Sources of Funding and Disclosures, see page 11.
REFERENCES
- 1. Couper K, Kimani PK, Gale CP, Quinn T, Squire IB, Marshall A, Black JJ, Cooke MW, Ewings B, Long J, et al. Variation in outcome of hospitalised patients with out‐of‐hospital cardiac arrest from acute coronary syndrome: a cohort study. Health Serv. Deliv. Res. 2018;6:1–116. [PubMed] [Google Scholar]
- 2. Akar JG, Akar FG. Regulation of ion channels and arrhythmias in the ischemic heart. J Electrocardiol. 2007;40:S37–S41. doi: 10.1016/j.jelectrocard.2007.05.020 [DOI] [PubMed] [Google Scholar]
- 3. Al‐Khatib SM, Granger CB, Huang Y, Lee KL, Califf RM, Simoons ML, Armstrong PW, Van de Werf F, White HD, Simes RJ, et al. Sustained ventricular arrhythmias among patients with acute coronary syndromes with no ST‐segment elevation: incidence, predictors, and outcomes. Circulation. 2002;106:309–312. doi: 10.1161/01.CIR.0000022692.49934.E3 [DOI] [PubMed] [Google Scholar]
- 4. Dekker LRC, Bezzina CR, Henriques JPS, Tanck MW, Koch KT, Alings MW, Arnold AER, de Boer M‐J, Gorgels APM, Michels HR, et al. Familial sudden death is an important risk factor for primary ventricular fibrillation: a case‐control study in acute myocardial infarction patients. Circulation. 2006;114:1140–1145. doi: 10.1161/CIRCULATIONAHA.105.606145 [DOI] [PubMed] [Google Scholar]
- 5. Bezzina CR, Pazoki R, Bardai A, Marsman RF, de Jong JSSG, Blom MT, Scicluna BP, Jukema JW, Bindraban NR, Lichtner P, et al. Genome‐wide association study identifies a susceptibility locus at 21q21 for ventricular fibrillation in acute myocardial infarction. Nat Genet. 2010;42:688–691. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Al‐Khatib SM, Stevenson WG, Ackerman MJ, Bryant WJ, Callans DJ, Curtis AB, Deal BJ, Dickfeld T, Field ME, Fonarow GC, et al. 2017 AHA/ACC/HRS guideline for management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: A Report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice Guidelines and the Heart Rhythm Society. Circulation [internet]. 2018;138:e272–e391. 10.1161/CIR.0000000000000549 [DOI] [PubMed] [Google Scholar]
- 7. Kalarus Z, Svendsen JH, Capodanno D, Dan G‐A, De Maria E, Gorenek B, Jędrzejczyk‐Patej E, Mazurek M, Podolecki T, Sticherling C, et al. Cardiac arrhythmias in the emergency settings of acute coronary syndrome and revascularization: an European Heart Rhythm Association (EHRA) consensus document, endorsed by the European Association of Percutaneous Cardiovascular Interventions (EAPCI), and European Acute Cardiovascular Care Association (ACCA). EP Eur. 2019;21:1603–1604. doi: 10.1093/europace/euz163 [DOI] [PubMed] [Google Scholar]
- 8. Priori SG, Blomström‐Lundqvist C, Mazzanti A, Blom N, Borggrefe M, Camm J, Elliott PM, Fitzsimons D, Hatala R, Hindricks G, et al. 2015 ESC Guidelines for the management of patients with ventricular arrhythmias and the prevention of sudden cardiac death: The Task Force for the Management of Patients with Ventricular Arrhythmias and the Prevention of Sudden Cardiac Death of the European Society of Cardiology (ESC)Endorsed by: Association for European Paediatric and Congenital Cardiology (AEPC). Eur Heart J. 2015;36:2793–2867. doi: 10.1093/eurheartj/ehv316 [DOI] [PubMed] [Google Scholar]
- 9. Mehta RH, Yu J, Piccini JP, Tcheng JE, Farkouh ME, Reiffel J, Fahy M, Mehran R, Stone GW. Prognostic Significance of Postprocedural Sustained Ventricular Tachycardia or Fibrillation in Patients Undergoing Primary Percutaneous Coronary Intervention (from the HORIZONS‐AMI Trial). Am J Cardiol. 2012;109:805–812. doi: 10.1016/j.amjcard.2011.10.043 [DOI] [PubMed] [Google Scholar]
- 10. Bougouin W, Marijon E, Puymirat E, Defaye P, Celermajer DS, Le Heuzey J‐Y, Boveda S, Kacet S, Mabo P, Barnay C, et al. Incidence of sudden cardiac death after ventricular fibrillation complicating acute myocardial infarction: a 5‐year cause‐of‐death analysis of the FAST‐MI 2005 registry. Eur Heart J. 2014;35:116–122. doi: 10.1093/eurheartj/eht453 [DOI] [PubMed] [Google Scholar]
- 11. Mehta RH, Starr AZ, Lopes RD, Hochman JS, Widimsky P, Pieper KS, Armstrong PW, Granger CB. Incidence of and outcomes associated with ventricular tachycardia or fibrillation in patients undergoing primary percutaneous coronary intervention. JAMA. 2009;301:1779–1789. doi: 10.1001/jama.2009.600 [DOI] [PubMed] [Google Scholar]
- 12. Demidova MM, Smith JG, Höijer C‐J, Holmqvist F, Erlinge D, Platonov PG. Prognostic impact of early ventricular fibrillation in patients with ST‐elevation myocardial infarction treated with primary PCI. Eur. Heart J. Acute Cardiovasc. Care. 2012;1:302–311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Álvarez‐Álvarez B, Bouzas‐Cruz N, Abu‐Assi E, Raposeiras‐Roubin S, López‐López A, González Cambeiro MC, Peña‐Gil C, García‐Acuña JM, González‐Juanatey JR. Impact of acute coronary syndrome complicated by ventricular fibrillation on long‐term incidence of sudden cardiac death. Rev. Esp. Cardiol. Engl. Ed. 2015;68:878–884. [DOI] [PubMed] [Google Scholar]
- 14. García‐García C, Oliveras T, Rueda F, Pérez‐Fernández S, Ferrer M, Serra J, Labata C, Vila J, Carrillo X, Rodríguez‐Leor O, et al. Primary ventricular fibrillation in the primary percutaneous coronary intervention ST‐Segment Elevation Myocardial Infarction Era (from the “Codi IAM” Multicenter Registry). Am J Cardiol. 2018;122:529–536. doi: 10.1016/j.amjcard.2018.04.054 [DOI] [PubMed] [Google Scholar]
- 15. Hai J‐J, Un K‐C, Wong C‐K, Wong K‐L, Zhang Z‐Y, Chan P‐H, Lau C‐P, Siu C‐W, Tse H‐F. Prognostic implications of early monomorphic and non–monomorphic tachyarrhythmias in patients discharged with acute coronary syndrome. Heart Rhythm. 2018;15:822–829. doi: 10.1016/j.hrthm.2018.02.016 [DOI] [PubMed] [Google Scholar]
- 16. Jabbari R, Risgaard B, Fosbøl EL, Scheike T, Philbert BT, Winkel BG, Albert CM, Glinge C, Ahtarovski KA, Haunsø S, et al. Factors associated with and outcomes after ventricular fibrillation before and during primary angioplasty in patients with ST‐segment elevation myocardial infarction. Am J Cardiol. 2015;116:678–685. doi: 10.1016/j.amjcard.2015.05.037 [DOI] [PubMed] [Google Scholar]
- 17. Liang JJ, Fender EA, Cha Y‐M, Lennon RJ, Prasad A, Barsness GW. Long‐term outcomes in survivors of early ventricular arrhythmias after acute ST‐elevation and non–ST‐elevation myocardial infarction treated with percutaneous coronary intervention. Am J Cardiol. 2016;117:709–713. doi: 10.1016/j.amjcard.2015.12.002 [DOI] [PubMed] [Google Scholar]
- 18. Podolecki T, Lenarczyk R, Kowalczyk J, Jedrzejczyk‐Patej E, Chodor P, Mazurek M, Francuz P, Streb W, Mitrega K, Kalarus Z. Prognostic significance of complex ventricular arrhythmias complicating ST‐segment elevation myocardial infarction. Am J Cardiol. 2018;121:805–809. doi: 10.1016/j.amjcard.2017.12.036 [DOI] [PubMed] [Google Scholar]
- 19. Kaura A, Panoulas V, Glampson B, Davies J, Mulla A, Woods K, Omigie J, Shah AD, Channon KM, Weber JN, et al. Association of troponin level and age with mortality in 250 000 patients: cohort study across five UK acute care centres. BMJ. 2019;367:l6055. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Kaura A, Arnold AD, Panoulas V, Glampson B, Davies J, Mulla A, Woods K, Omigie J, Shah AD, Channon KM, et al. Prognostic significance of troponin level in 3121 patients presenting with atrial fibrillation (The NIHR Health Informatics Collaborative TROP‐AF study). J Am Heart Assoc. 2020;9:e013684. doi: 10.1161/JAHA.119.013684 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Kaura A, Sterne JAC, Trickey A, Abbott S, Mulla A, Glampson B, Panoulas V, Davies J, Woods K, Omigie J, et al. Invasive versus non‐invasive management of older patients with non‐ST elevation myocardial infarction (SENIOR‐NSTEMI): a cohort study based on routine clinical data. Lancet Lond. Engl. 2020;396:623–634. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Collet J‐P, Thiele H, Barbato E, Barthélémy O, Bauersachs J, Bhatt DL, Dendale P, Dorobantu M, Edvardsen T, Folliguet T, et al. 2020 ESC Guidelines for the management of acute coronary syndromes in patients presenting without persistent ST‐segment elevation. Russian Journal of Cardiology. 2021;26(3):4418. 10.15829/1560-4071-2021-4418. doi: 10.15829/1560-4071-2021-4418 [DOI] [PubMed] [Google Scholar]
- 23. Ibanez B, James S, Agewall S, Antunes MJ, Bucciarelli‐Ducci C, Bueno H, Caforio ALP, Crea F, Goudevenos JA, Halvorsen S, et al. 2017 ESC Guidelines for the management of acute myocardial infarction in patients presenting with ST‐segment elevation: The Task Force for the management of acute myocardial infarction in patients presenting with ST‐segment elevation of the European Society of Cardiology (ESC). Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393 [DOI] [PubMed] [Google Scholar]
- 24. Benjamini Y, Hochberg Y. Controlling the false discovery rate: a practical and powerful approach to multiple testing. J. R. Stat. Soc. Ser. B Methodol. 1995;57:289–300. [Google Scholar]
- 25. Stensrud MJ, Hernán MA. Why test for proportional hazards? JAMA. 2020;323:1401. doi: 10.1001/jama.2020.1267 [DOI] [PubMed] [Google Scholar]
- 26. Schmidt André, Azevedo CF, Cheng A, Gupta SN, Bluemke DA, Foo TK, Gerstenblith G, Weiss RG, Marbán E, Tomaselli GF, et al. Infarct tissue heterogeneity by magnetic resonance imaging identifies enhanced cardiac arrhythmia susceptibility in patients with left ventricular dysfunction. Circulation. 2007;115:2006–2014. doi: 10.1161/CIRCULATIONAHA.106.653568 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Piccini JP, White JA, Mehta RH, Lokhnygina Y, Al‐Khatib SM, Tricoci P, Pollack CV, Montalescot G, Van de Werf F, Gibson CM, et al. Sustained ventricular tachycardia and ventricular fibrillation complicating Non–ST‐segment–elevation acute coronary syndromes. Circulation. 2012;126:41–49. doi: 10.1161/CIRCULATIONAHA.111.071860 [DOI] [PubMed] [Google Scholar]
- 28. Gerhard S, Dietrich A, Karlheinz S, Johannes B, Ellen H, Dariusz W, Zdzisława K‐J, Beata S, Géza L, Franz H, et al. Defibrillator implantation early after myocardial infarction. N Engl J Med. 2009;361:1427–1436. [DOI] [PubMed] [Google Scholar]
- 29. Hohnloser SH, Kuck KH, Dorian P, Roberts RS, Hampton JR, Hatala R, Fain E, Gent M, Connolly SJ. Prophylactic use of an implantable cardioverter‐defibrillator after acute myocardial infarction. N Engl J Med. 2004;8. doi: 10.1056/NEJMoa041489 [DOI] [PubMed] [Google Scholar]
- 30. Lanza GA. Prognostic value of ventricular arrhythmias and heart rate variability in patients with unstable angina. Heart. 2006;92:1055–1063. doi: 10.1136/hrt.2005.070714 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Matsue Y, Suzuki M, Nishizaki M, Hojo R, Hashimoto Y, Sakurada H. Clinical implications of an implantable cardioverter‐defibrillator in patients with vasospastic angina and lethal ventricular arrhythmia. J Am Coll Cardiol. 2012;60:908–913. [DOI] [PubMed] [Google Scholar]
- 32. Avezum Á, Piegas LS, Goldberg RJ, Brieger D, Stiles MK, Paolini R, Huang W, Gore JM. Magnitude and prognosis associated with ventricular arrhythmias in patients hospitalized with acute coronary syndromes (from the GRACE Registry). Am J Cardiol. 2008;102:1577–1582. doi: 10.1016/j.amjcard.2008.08.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1‐S5
Figures S1‐S2


