Abstract
Background
To compare estimated 10‐year and 30‐year cardiovascular risk in primary care patients with and without serious mental illness (SMI; bipolar disorder, schizophrenia, or schizoaffective disorder).
Methods and Results
All patients aged 18 to 75 years with a primary care visit in January 2016 to September 2018 were included and were grouped into those with and without SMI using diagnosis codes. Ten‐year cardiovascular risk was estimated using atherosclerotic cardiovascular disease scores for patients aged 40 to 75 years without cardiovascular disease; 30‐year cardiovascular risk was estimated using Framingham risk scores for patients aged 18 to 59 years without cardiovascular disease. Demographic, vital sign, medication, diagnosis, and health insurance data were collected from the electronic health record by a clinical decision support system. Descriptive statistics examined unadjusted differences, while general linear models examined differences for continuous variables and logistic regression models for categorical variables. Models were then adjusted for age, sex, race, ethnicity, and insurance type. A total of 11 333 patients with SMI and 579 924 patients without SMI were included. After covariate adjustment, 10‐year cardiovascular risk was significantly higher in patients with SMI (mean, 9.44%; 95% CI, 9.29%–9.60%) compared with patients without SMI (mean, 7.99%; 95% CI, 7.97–8.02). Similarly, 30‐year cardiovascular risk was significantly higher in those with SMI (25% of patients with SMI in the highest‐risk group compared with 11% of patients without SMI; P<0.001). The individual cardiovascular risk factors contributing most to increased risk for those with SMI were elevated body mass index and smoking. Among SMI subtypes, patients with bipolar disorder had the highest 10‐year cardiovascular risk, while patients with schizoaffective disorder had the highest 30‐year cardiovascular risk.
Conclusions
The significantly increased cardiovascular risk associated with SMI is evident even in young adults. This suggests the importance of addressing uncontrolled major cardiovascular risk factors in those with SMI at as early an age as possible.
Registration
URL: https://www.clinicaltrials.gov; Unique identifier: NCT02451670.
Keywords: bipolar disorder, cardiovascular, risk factors, schizophrenia, serious mental illness
Subject Categories: Cardiovascular Disease, Mental Health, Primary Prevention, Risk Factors, Race and Ethnicity, Women
Nonstandard Abbreviations and Acronyms
- DBP
diastolic blood pressure
- NIMH
National Institute of Mental Health
- SBP
systolic blood pressure
- SMI
serious mental illness
Clinical Perspective
What Is New?
Adults of all ages with serious mental illness—bipolar disorder, schizophrenia, or schizoaffective disorder—had significantly increased cardiovascular risk compared with their peers.
What Are the Clinical Implications?
It is important to address uncontrolled major cardiovascular risk factors in those with serious mental illness at as early an age as possible to reduce morbidity and mortality in this population.
Cardiovascular disease is the leading cause of death for people with serious mental illness (SMI; bipolar disorder, schizophrenia, or schizoaffective disorder). 1 On average, people with SMI die 10 to 20 years earlier than the general population. 2 Cardiovascular risk prediction models such as the American College of Cardiology/American Heart Association cardiovascular disease (CVD) pooled 10‐year risk equations were developed for the general adult population aged 40 to 75 years on the basis of age, race, sex, blood pressure (BP), BP medication status, diabetes status, smoking status, and lipoprotein levels. For those aged 20 to 59 years, the Framingham 30‐year CVD risk equations can be used to estimate risk. Both of these equations predict likelihood of a nonfatal myocardial infarction or stroke or cardiovascular death. Although these equations are known to be imperfect, they provide a standardized metric that can be used to assess the contributions of major uncontrolled cardiovascular risk factors to overall cardiovascular risk in those with and without SMI.
A handful of studies have examined cardiovascular risk estimates in those with and without SMI, but most have used control populations from separate studies or general population estimates. 3 , 4 , 5 This approach is suboptimal, as there can be underlying and unaccounted‐for differences in such factors as race and ethnicity, socioeconomic status, or geographic representation between cohorts. As part of a cluster‐randomized trial aimed at reducing cardiovascular risk in patients with SMI, we collected baseline cardiovascular risk estimates for patients with and without SMI from the same clinic populations, allowing for adjustment for baseline differences in age, sex, race, ethnicity, and insurance coverage. 6 These analyses are the focus of this article.
Methods
The data that support the findings of this study are available from the corresponding author upon reasonable request. This study was approved by the HealthPartners Institutional Review Board, and a waiver of informed consent was granted.
Study Design and Settings
Two health care delivery organizations (HealthPartners and Park Nicollet) in Minnesota and Wisconsin participated in a larger trial of clinical decision support in primary care clinics to reduce cardiovascular risk in patients with SMI. 7 Study enrollment occurred between January 20, 2016, and September 19, 2018.
Enrollment and Eligibility
Encounter data were collected for every patient who made a visit to a randomized primary care clinic during the study enrollment period. To be included in this study, patients had to have an index visit, defined as the first visit at a randomized primary care clinic during the enrollment period for which patients met the following criteria at the time of the index visit: (1) age 18 to 75 years; (2) no evidence of pregnancy; (3) no active cancer diagnosis; and (4) not residing in a nursing home or receiving palliative care (see Figure for participant flow).
Figure . Study participant flow.
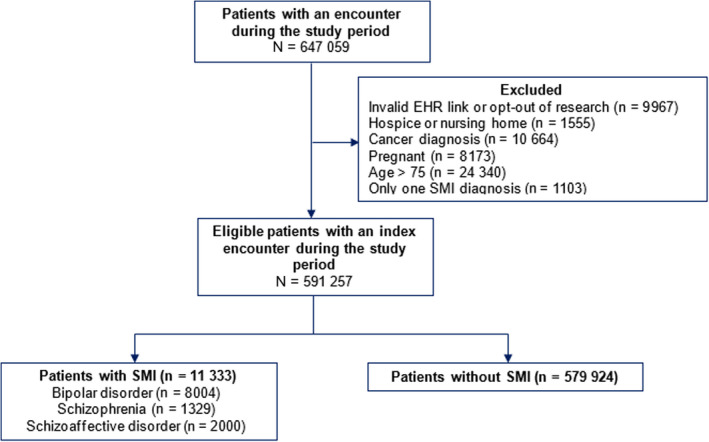
EHR indicates electronic health record; and SMI, serious mental illness.
To be included in the SMI group, patients had to have ≥2 outpatient diagnostic codes or ≥1 inpatient codes for SMI documented in the electronic health record (EHR) in the 2 years before the index date. SMI was defined as having bipolar disorder (International Classification of Diseases, Ninth Revision [ICD‐9] codes of 296.00–296.89, 301.11; International Classification of Diseases, Tenth Revision [ICD‐10] codes of F30.1–F31.9), schizophrenia (ICD‐9 codes of 295.0–295.6, 295.8–295.9, 297.1, 297.3, 298.8, 298.9, 301.22; ICD‐10 codes of F20.0–F24, F28–F29), or schizoaffective disorder (ICD‐9 code of 295.6; ICD‐10 codes of F25.0–F25.9). Patients with codes that crossed subcategories of SMI (schizophrenia+schizoaffective disorder, bipolar disorder+schizoaffective disorder, bipolar disorder+schizophrenia) were considered to have schizoaffective disorder. Patients who had only 1 outpatient SMI code were excluded from analyses. Patients who did not have any SMI codes were included in the non‐SMI group. Patients who requested to be excluded from research studies were omitted from analyses.
Measures
Cardiovascular Risk
Total cardiovascular risk was calculated using 2 different equations. For patients aged 40 to 75 years without CVD, 10‐year cardiovascular risk was estimated using the atherosclerotic cardiovascular disease (ASCVD) risk score. 6 This score theoretically ranges from 0 to 100 and corresponds to the percent likelihood of having a myocardial infarction, stroke, or cardiovascular death in the next 10 years. Patients with diagnosed ASCVD were excluded from analyses of total cardiovascular risk. For patients aged 18 to 59 without CVD, 30‐year (lifetime) risk was estimated using the Framingham risk score. 8 Patients were categorized into one of five 30‐year risk groups based on risk factors (BP, lipids, diabetes status, and smoking status): all optimal risk factors (BP <120/80 mm Hg, total cholesterol<180 mg/dL, nonsmoker, without diabetes), ≥1 not optimal risk factor (systolic BP [SBP] 120–139 mm Hg, diastolic BP [DBP] 80–89 mm Hg, total cholesterol 180–199 mg/dL, nonsmoker, without diabetes), ≥1 elevated risk factor (total cholesterol 200–239 mg/dL, SBP 140–159 mm Hg, DBP 90–99 mm Hg, nonsmoker, without diabetes), 1 major risk factor (total cholesterol ≥240 mg/dL, SBP ≥160 mm Hg, DBP ≥100 mm Hg, smoker, or with diabetes), or ≥2 major risk factors.
Six major modifiable cardiovascular risk factors (in addition to age, race, and sex) were captured by the clinical decision support system: blood pressure (SBP and DBP), lipids (total cholesterol, low‐density lipoprotein, high‐density lipoprotein, triglycerides, and statin use), glycemic control as measured by glycosylated hemoglobin, weight (body mass index as kg/m2 [BMI]), smoking status, and aspirin use. For glycosylated hemoglobin and lipids, the most recent test in the past 5 years was used for analyses. Appropriateness of aspirin use was considered for patients with coronary heart disease according to US Preventive Services Task Force recommendations. 9 Treatment with an antihypertensive medication was also used in the 10‐year American College of Cardiology/American Heart Association CVD risk equations.
Diagnoses
Diagnoses for coronary heart disease, CVD, hypertension, and diabetes were defined as having ≥2 outpatient diagnostic codes or ≥1 inpatient codes documented in the EHR in the 2 years before the index date. Coronary heart disease was identified with ICD‐9 codes of 410 to 414.9 and 429.2, and ICD‐10 codes of I20‐I25.9. ASCVD was identified using ICD‐9 codes of 430 to 432.9, 433 to 434.91, 435, 435.8 to 435.9, 436, 440 to 440.4, and 445 to 445.89, and ICD‐10 codes of I63.02 to I63.9, I65 to I67.82, I70.0 to I70.92, and I74 to I74.9. Hypertension was identified via ICD‐9 codes of 401 to 405.9 and ICD‐10 codes of I10 to 15.9. Diabetes was identified using ICD‐9 codes of 250 to 250.93, 357.2, 362.01 to 362.07, and 366.41, and ICD‐10 codes of E10 to E11.9.
Data Sources
Much of the data collection was done by the clinical decision support tool itself, which harvested EHR data for each web service call, including vitals, medications, diagnoses, and orders. Data not routinely collected by the clinical decision support, such as race and ethnicity or insurance status, were harvested from the EHR data repository.
Statistical Analysis
Descriptive statistics were calculated to examine unadjusted differences in demographic characteristics (age, sex, race, ethnicity, health insurance coverage) and cardiovascular risk factors between patients with and without diagnosed SMI and among patients with different SMI diagnoses (bipolar disorder, schizophrenia disorder, and schizoaffective disorder). General linear models were used to examine differences among the groups for continuous variables (eg, 10‐year cardiovascular risk), and χ 2 analyses were used to examine differences among categorical variables (eg, smoking status). Because of significant differences among groups in demographic characteristics, models were then adjusted for age, sex, race, ethnicity, and insurance coverage to predict differences in overall and individual cardiovascular risk factors. General linear models were used for continuous dependent variables (eg, 10‐year ASCVD risk, BMI, SBP, DBP, and lipids). For categorical dependent variables, 3 types of logistic regression were used: (1) binary (for dichotomous outcomes, such as presence or absence of a diagnosis; (2) ordinal (for ranked categorical outcomes, such as 30‐year lifetime risk or categorized versions of 10‐year ASCVD risk, glycosylated hemoglobin, and BMI); and (3) multinomial (for categorical outcomes in the absence of an ordered list, including smoking status). In sensitivity analyses, we stratified models by age to determine the pattern of age differences between patients with and without SMI on 10‐year and 30‐year cardiovascular risk.
Results
A total of 647 059 patients had primary care visits at a randomized primary care clinic during the study period (January 20, 2016, to September 19, 2018; Table 1, Figure). After applying study eligibility criteria, 591 257 patients were retained for analyses. Of note, 1103 patients were excluded from analyses because they had only 1 outpatient diagnosis of SMI. In the final sample, 11 333 patients (1.9%) were included in the SMI group. The majority of patients with SMI were diagnosed with bipolar disorder (n=8004; 70.6% of those with SMI), followed by schizoaffective disorder (n=2000; 17.6%) and schizophrenia (n=1329; 11.7%). On average, patients with SMI were younger and more likely to be women; to self‐identify as Black, Native American/Alaskan Native, or of multiple races; and to be insured by Medicaid or Medicare than their counterparts.
Table 1.
Patients With and Without SMI: Demographics, Total Cardiovascular Risk, and Individual Modifiable Cardiovascular Risk Factors
| Patient characteristic |
Patients With SMI n=11 333 |
Patients Without SMI n=579 924 |
P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean | SD | n | % | Mean | SD | ||
| Age, y | 44.8 | 14.1 | 45.3 | 15.7 | <0.0001 | ||||
| Age, y, categorical | <0.0001 | ||||||||
| 18–34 | 3177 | 28.0 | 173 939 | 30.0 | |||||
| 35–49 | 3639 | 32.1 | 155 391 | 26.8 | |||||
| 50–64 | 3482 | 30.7 | 175 061 | 30.2 | |||||
| 65+ | 1035 | 9.1 | 75 533 | 13.0 | |||||
| Sex, female | 6550 | 57.8 | 313 345 | 54.0 | <0.0001 | ||||
| Race | <0.0001 | ||||||||
| White | 8808 | 77.7 | 446 603 | 77.0 | |||||
| Black | 1543 | 13.6 | 53 735 | 9.3 | |||||
| Asian | 335 | 3.0 | 32 621 | 5.6 | |||||
| Native American/Alaska Native | 91 | 0.8 | 1753 | 0.3 | |||||
| Native Hawaiian/Pacific Islander | 16 | 0.1 | 745 | 0.1 | |||||
| Multiple | 101 | 0.9 | 2342 | 0.4 | |||||
| Other | 89 | 0.8 | 7721 | 1.3 | |||||
| Unknown | 350 | 3.1 | 34 404 | 5.9 | |||||
| Ethnicity | <0.0001 | ||||||||
| Hispanic | 309 | 2.7 | 18400 | 3.2 | |||||
| Non‐Hispanic | 9689 | 85.5 | 437 042 | 75.4 | |||||
| Unknown | 1335 | 11.8 | 124 481 | 21.5 | |||||
| Insurance type | <0.0001 | ||||||||
| Self‐pay/uninsured | 215 | 1.9 | 13 307 | 2.3 | |||||
| Medicare only | 1209 | 10.7 | 49 154 | 8.5 | |||||
| Medicaid only | 3027 | 26.7 | 68 594 | 11.8 | |||||
| Commercial only | 2552 | 22.5 | 348 319 | 60.1 | |||||
| Other only | 78 | 0.7 | 5924 | 1.0 | |||||
| Medicare+Medicaid | 1970 | 17.4 | 6593 | 1.1 | |||||
| Medicare+Commercial | 345 | 3.0 | 17 774 | 3.1 | |||||
| ≥2 insurances | 1937 | 17.1 | 70 259 | 12.1 | |||||
| 10‐year ASCVD risk* | 8.0 | 8.4 | 7.9 | 8.4 | 0.58 | ||||
| 10‐year ASCVD risk, categorical* | <0.0001 | ||||||||
| <5% | 2503 | 48.0 | 120 890 | 49.8 | |||||
| 5%–9.9% | 1292 | 24.8 | 53 506 | 22.1 | |||||
| 10%–14.9% | 647 | 12.4 | 29 253 | 12.1 | |||||
| 15%–19.9% | 322 | 6.2 | 17 040 | 7.0 | |||||
| ≥20% | 454 | 8.7 | 22 002 | 9.1 | |||||
| 30‐year lifetime risk † | <0.0001 | ||||||||
| All optimal risk factors | 612 | 9.8 | 30 840 | 14.2 | |||||
| ≥1 not optimal risk factors | 894 | 14.4 | 54 465 | 25.1 | |||||
| ≥1 elevated risk factors | 231 | 3.7 | 19 393 | 8.9 | |||||
| 1 major risk factor | 2844 | 45.8 | 85 887 | 39.6 | |||||
| ≥2 major risk factors | 1636 | 26.3 | 26 536 | 12.2 | |||||
| CHD | 337 | 3.0 | 15 114 | 2.6 | 0.0152 | ||||
| CVD | 520 | 4.6 | 21 164 | 3.7 | <0.0001 | ||||
| BP | |||||||||
| Hypertension | 1684 | 14.9 | 76 314 | 13.2 | <0.0001 | ||||
| High BP at visit (≥140/90 mm Hg) | 1889 | 16.7 | 101 489 | 17.5 | 0.0213 | ||||
| SBP | 121.4 | 16.4 | 123.6 | 16.7 | <0.0001 | ||||
| DBP | 77.1 | 11.5 | 76.7 | 11.3 | 0.0017 | ||||
| Cholesterol | |||||||||
| Total cholesterol | 183.0 | 42.1 | 188.1 | 39.1 | <0.0001 | ||||
| LDL (statin only) | 94.2 | 36.7 | 98.9 | 35.0 | <0.0001 | ||||
| LDL (nonstatin only) | 109.5 | 32.4 | 115.6 | 31.6 | <0.0001 | ||||
| HDL | 48.3 | 15.8 | 52.3 | 16.5 | <0.0001 | ||||
| Triglycerides | 153.3 | 118.2 | 128.0 | 93.2 | <0.0001 | ||||
| Statin use | 2478 | 21.9 | 91 532 | 15.8 | <0.0001 | ||||
| Glucose | |||||||||
| Diabetes | 1553 | 13.7 | 37805 | 6.5 | <0.0001 | ||||
| A1c (Diabetes only)c | 7.3 | 1.8 | 7.4 | 1.6 | 0.0019 | ||||
| A1c (non DM only) § | 5.6 | 0.8 | 5.7 | 0.7 | 0.0022 | ||||
| A1c (DM only), categorical ‡ | <0.0001 | ||||||||
| <7.0 | 803 | 54.6 | 17 325 | 47.9 | |||||
| 7.0–7.9 | 319 | 21.7 | 9379 | 30.0 | |||||
| 8.0–8.9 | 126 | 8.6 | 4125 | 11.4 | |||||
| ≥9 | 222 | 15.1 | 5031 | 13.9 | |||||
| Weight | |||||||||
| BMI | 31.1 | 7.8 | 28.8 | 6.7 | <0.0001 | ||||
| BMI, categorical | <0.0001 | ||||||||
| <18.5, underweight | 117 | 1.2 | 6354 | 1.3 | |||||
| 18.5–24.9, normal | 2075 | 21.1 | 146 034 | 30.0 | |||||
| 25–29.9, overweight | 2779 | 28.2 | 161 544 | 33.2 | |||||
| 30–34.9, obese I | 2282 | 23.2 | 96479 | 19.8 | |||||
| 35–39.9, obese II | 1378 | 14.0 | 45 042 | 9.3 | |||||
| ≥40, obese III | 1227 | 12.5 | 31 720 | 6.5 | |||||
| Smoking status | <0.0001 | ||||||||
| Current smoker | 4099 | 36.2 | 70 375 | 12.1 | |||||
| Former smoker | 3065 | 27.0 | 123 316 | 21.3 | |||||
| Nonsmoker | 4169 | 36.8 | 386 174 | 66.6 | |||||
| Appropriate aspirin use || | 295 | 87.5 | 13 699 | 90.6 | 0.05 | ||||
A1c indicates glycosylated hemoglobin; ASCVD, 10‐year atherosclerotic cardiovascular disease risk; BMI, body mass index; BP, blood pressure; CHD, coronary heart disease; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; SMI, serious mental illness; and SBP, systolic blood pressure.
ASCVD risk is calculated only for patients aged 40–75 years without known CVD (n=247 909).
Thirty‐year lifetime risk of CVD is calculated only for patients aged 18–59 years without known CVD (n=233 308).
Calculated for patients with diabetes who have available A1c tests within the past 5 years (n=37 600).
Calculated for patients without diabetes who have available A1c tests within the past 5 years (n=33 055).
Aspirin use was calculated only for individuals with known CHD (n=15 451).
Differences in Baseline Cardiovascular Risk Between Patients With and Without SMI
Unadjusted estimates suggested overall 10‐year cardiovascular risk was not significantly different between patients with (mean, 8.0; SD, 8.4) and without SMI (mean, 7.9; SD, 8.4; Table 1). However, 30‐year cardiovascular risk was significantly higher for patients with SMI in unadjusted estimates, with a greater proportion of patients with SMI having ≥1 major uncontrolled cardiovascular risk factor than patients without SMI. A greater proportion of patients with SMI were diagnosed with CVD (4.6% versus 3.7%; P<0.0001), coronary heart disease (3.0% versus 2.6%; P=0.015) or hypertension (14.9% versus 13.2%; P<0.0001). Patients with SMI were twice as likely to be diagnosed with diabetes, yet they were more likely to have a glycosylated hemoglobin <7.0% than patients without SMI. Patients with SMI generally had lower BP and cholesterol than patients without SMI, but these differences were small. Patients with SMI had significantly higher triglycerides and statin use than patients without SMI. There were no differences in appropriate aspirin use.
Patients with SMI had rates of elevated BMI and smoking. BMI was significantly higher in patients with SMI (mean, 31.1; SD, 7.8) compared with patients without SMI (mean, 28.8; SD, 6.7). Further, compared with patients without SMI, patients with SMI were more likely to have BMIs ≥30 (49.7% versus 35.6%; P<0.0001) and nearly twice the rate of obesity class III (BMI ≥40 kg/m2). Patients with SMI were 3 times more likely to be current smokers (36.2%) than those without SMI (12.1%).
After adjusting for age, race, ethnicity, sex, and insurance coverage, many of the differences between patients with and without SMI remained the same or increased (Table 2, Table S1). Notably, estimated 10‐year cardiovascular risk in those aged 40 to 75 years was significantly higher in patients with SMI than those without SMI (mean, 7.92; 95% CI, 7.90–7.95; P<0.0001) Similarly, for those aged 18 to 59 years, having a diagnosis of SMI was associated with 1.92 greater odds (95% CI, 1.82–2.01; P<0.0001) of being in a higher‐risk group compared with patients without SMI.
Table 2.
Patients With and Without SMI: Adjusted Estimates of Total Cardiovascular Risk and Individual Modifiable Cardiovascular Risk Factors
| Cardiovascular risk |
Patients With SMI n=11 333 |
Patients Without SMI n=579 924 |
P value | ||||||
|---|---|---|---|---|---|---|---|---|---|
| Mean | PP | 95% CI | Mean | PP | 95% CI | ||||
| LL | UL | LL | UL | ||||||
| 10‐year ASCVD risk* | 8.31 | 8.15 | 8.46 | 7.92 | 7.90 | 7.95 | <0.0001 | ||
| 10‐year ASCVD risk*, categorical | <0.0001 | ||||||||
| <5% | 39.6 | 38.1 | 41.1 | 49.3 | 49.0 | 49.6 | |||
| 5%–9.9% | 45.9 | 44.4 | 47.4 | 40.5 | 40.2 | 40.8 | |||
| 10%–14.9% | 10.8 | 10.0 | 11.6 | 7.7 | 7.6 | 7.9 | |||
| 15%–19.9% | 2.5 | 2.3 | 2.8 | 1.7 | 1.7 | 1.8 | |||
| ≥20% | 1.2 | 1.1 | 1.3 | 0.8 | 0.8 | 0.8 | |||
| 30‐year lifetime risk † | <0.0001 | ||||||||
| All optimal risk factors | 6.9 | 6.6 | 7.2 | 12.4 | 12.3 | 12.6 | |||
| ≥1 not optimal risk factors | 17.7 | 17.3 | 18.0 | 26.0 | 25.8 | 26.1 | |||
| ≥ 1 elevated risk factors | 8.0 | 7.1 | 8.9 | 9.7 | 9.4 | 9.9 | |||
| 1 major risk factor | 48.6 | 47.6 | 49.7 | 41.2 | 41.0 | 41.4 | |||
| ≥2 major risk factors | 18.8 | 18.1 | 19.6 | 10.8 | 10.7 | 10.9 | |||
| CHD | 0.8 | 0.7 | 0.9 | 0.7 | 0.6 | 0.7 | 0.004 | ||
| CVD | 1.4 | 1.2 | 1.6 | 1.2 | 1.1 | 1.2 | <0.0001 | ||
| Blood pressure | |||||||||
| Hypertension | 10.0 | 9.4 | 10.4 | 8.1 | 8.0 | 8.1 | <0.0001 | ||
| High BP at visit (≥140/90 mm Hg) | 16.1 | 15.4 | 16.8 | 16.0 | 15.9 | 16.1 | 0.73 | ||
| SBP | 122.2 | 121.9 | 122.5 | 123.6 | 123.6 | 123.6 | <0.0001 | ||
| DBP | 77.8 | 77.6 | 78.0 | 76.7 | 76.7 | 76.7 | <0.0001 | ||
| Cholesterol | |||||||||
| Total cholesterol | 188.8 | 188.0 | 189.7 | 188.8 | 188.7 | 189.0 | 0.98 | ||
| LDL (statin only) | 92.3 | 90.9 | 93.8 | 99.0 | 98.7 | 99.2 | <0.0001 | ||
| LDL (nonstatin only) | 114.7 | 113.9 | 115.5 | 115.8 | 115.7 | 116.0 | 0.007 | ||
| HDL | 49.5 | 49.1 | 49.8 | 52.0 | 51.9 | 52.0 | <0.0001 | ||
| Triglycerides | 151.8 | 149.7 | 153.9 | 129.0 | 128.7 | 129.4 | <0.0001 | ||
| Statin use | 12.8 | 12.3 | 13.5 | 7.4 | 7.3 | 7.5 | <0.0001 | ||
| Glucose | |||||||||
| Diabetes | 7.6% | 7.2% | 8.0% | 3.7% | 3.6% | 3.7% | <0.0001 | ||
| A1c (diabetes only) ‡ | 7.14 | 7.05 | 7.22 | 7.41 | 7.39 | 7.42 | <0.0001 | ||
| A1c (non‐diabetes only) § | 5.52 | 5.50 | 5.55 | 5.58 | 5.57 | 5.58 | <0.0001 | ||
| A1c (diabetes only), categorical ‡ | <0.0001 | ||||||||
| <7.0 | 55.4 | 52.9 | 57.9 | 48.3 | 47.8 | 48.8 | |||
| 7.0–7.9 | 24.3 | 21.8 | 26.8 | 26.4 | 25.9 | 26.9 | |||
| 8.0–8.9 | 9.6 | 7.9 | 11.2 | 11.5 | 11.1 | 12.0 | |||
| ≥9 | 10.7 | 9.7 | 11.7 | 13.8 | 13.4 | 14.1 | |||
| Weight | |||||||||
| BMI | 30.8 | 30.6 | 30.9 | 28.8 | 28.8 | 28.9 | <0.0001 | ||
| BMI, categorical | <0.0001 | ||||||||
| <18.5, underweight | 0.7 | 0.6 | 0.7 | 1.2 | 1.2 | 1.2 | |||
| 18.5–24.9, normal | 19.3 | 19.2 | 19.3 | 29.8 | 29.6 | 29.9 | |||
| 25–29.9, overweight | 31.4 | 30.8 | 31.9 | 34.5 | 34.4 | 34.7 | |||
| 30–34.9, obese I | 24.8 | 23.9 | 25.6 | 19.6 | 19.5 | 19.8 | |||
| 35–39.9, obese II | 13.5 | 12.8 | 14.1 | 8.8 | 8.7 | 8.9 | |||
| ≥40, obese III | 10.5 | 10.1 | 10.8 | 6.1 | 6.0 | 6.2 | |||
| Smoking status | <0.0001 | ||||||||
| Current smoker | 27.6 | 26.8 | 28.4 | 11.6 | 11.6 | 11.7 | |||
| Former smoker | 27.9 | 27.0 | 28.8 | 19.7 | 19.6 | 19.8 | |||
| Nonsmoker | 44.5 | 43.5 | 45.5 | 68.7 | 68.5 | 68.8 | |||
| Appropriate aspirin use || | 90.4 | 87.2 | 93.0 | 91.1 | 90.6 | 91.5 | 0.69 | ||
Models adjusted for age, sex, race, ethnicity, and insurance coverage. A1c indicates glycosylated hemoglobin; ASCVD, 10‐year atherosclerotic cardiovascular disease risk; BMI, body mass index; CHD, coronary heart disease; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDL, high density lipoprotein; LDL, low density lipoprotein; LL, lower 95% confidence limit; PP, predicted probability (proportion); SBP, systolic blood pressure; SMI, serious mental illness; and UL, upper 95% confidence limit.
ASCVD risk is calculated only for patients aged 40–75 years without known CVD (n=247 909).
Thirty‐year lifetime risk of CVD is calculated only for patients aged 18–59 without known CVD (n=233 308).
Calculated for patients with DM who have available A1c tests within the past 5 years (n=37 600).
Calculated for patients without DM who have available A1c tests within the past 5 years (n=33 055).
Aspirin use was calculated only for individuals with known CHD (n=15 451).
Differences in Baseline Cardiovascular Risk Among Patients With Different SMI Diagnoses
Patients within the SMI group were then compared by specific SMI diagnosis: bipolar disorder, schizophrenia disorder, or schizoaffective disorder (see Table 3 for unadjusted estimates and Table 4 and Table S2 for adjusted estimates). Patients with bipolar disorder were younger and more likely to be women and White compared with patients with schizophrenia or schizoaffective disorder. In unadjusted estimates, patients with schizophrenia had the highest 10‐year cardiovascular risk, and patients with bipolar disorder had the lowest risk. However, after adjusting for demographics, patients aged 40 to 75 years with bipolar disorder had significantly greater 10‐year cardiovascular risk than patients with schizophrenia or schizoaffective disorder. In contrast, after adjusting for demographics, patients aged 18 to 59 years with schizoaffective disorder had 30‐year cardiovascular risk that was significantly higher than in patients with schizophrenia or bipolar disorder.
Table 3.
Patients With SMI: Demographics, Total Cardiovascular Risk and Individual Modifiable Cardiovascular Risk Factors
| Patient characteristic |
Patients with bipolar disorder n=8004 |
Patients with schizophrenia disorder n=1329 |
Patients with schizoaffective disorder n=2000 |
P value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| n | % | Mean | SD | n | % | Mean | SD | n | % | Mean | SD | ||
| Age, y | 43.7* , † | 14.1 | 47.8 | 14.5 | 47.1 | 13.5 | <0.0001 | ||||||
| Age, y, categorical | |||||||||||||
| 18–34 | 2439* , † | 30.5 | 308 † | 23.2 | 430 | 21.5 | <0.0001 | ||||||
| 35–49 | 2673 | 33.4 | 346 | 26.0 | 620 | 31.0 | |||||||
| 50–64 | 2212 | 27.6 | 506 | 38.1 | 764 | 38.2 | |||||||
| 65+ | 680 | 8.5 | 1169 | 12.7 | 186 | 9.3 | |||||||
| Sex, female | 5091* , † | 63.6 | 450 † | 33.9 | 1009 | 50.5 | <0.0001 | ||||||
| Race | <0.0001 | ||||||||||||
| White | 6585* , † | 82.3 | 830 † | 62.5 | 1393 | 69.7 | |||||||
| Black | 827 | 10.3 | 317 | 23.9 | 399 | 20.0 | |||||||
| Asian | 139 | 1.7 | 107 | 8.1 | 89 | 4.5 | |||||||
| Native American/Alaska Native | 65 | 0.8 | 11 | 0.8 | 15 | 0.8 | |||||||
| Native Hawaiian/Pacific Islander | 10 | 0.1 | 3 | 0.2 | 3 | 0.2 | |||||||
| Multiple | 72 | 0.9 | 6 | 0.5 | 23 | 1.2 | |||||||
| Other | 58 | 0.7 | 11 | 0.8 | 20 | 1.0 | |||||||
| Unknown | 248 | 3.1 | 44 | 3.3 | 58 | 2.9 | |||||||
| Ethnicity | <0.0001 | ||||||||||||
| Hispanic | 216* , † | 2.7 | 26 † | 2.0 | 67 | 3.4 | |||||||
| Non‐Hispanic | 6852 | 85.6 | 1097 | 82.5 | 1740 | 87.0 | |||||||
| Unknown | 936 | 11.7 | 206 | 15.5 | 193 | 9.6 | |||||||
| Insurance type | <0.0001 | ||||||||||||
| Self‐pay/uninsured | 167* , † | 2.1 | 22 | 1.7 | 26 | 1.3 | |||||||
| Medicare only | 779 | 9.7 | 176 | 13.2 | 254 | 12.7 | |||||||
| Medicaid only | 2150 | 26.9 | 354 | 26.7 | 523 | 26.2 | |||||||
| Commercial only | 2297 | 28.7 | 97 | 7.3 | 158 | 7.9 | |||||||
| Other only | 61 | 0.8 | 8 | 0.6 | 9 | 0.5 | |||||||
| Medicare+Medicaid | 845 | 10.6 | 477 | 35.9 | 648 | 32.4 | |||||||
| Medicare+Commercial | 249 | 3.1 | 31 | 2.3 | 65 | 3.3 | |||||||
| 2 or more insurances | 1456 | 18.2 | 164 | 12.3 | 317 | 15.9 | |||||||
| 10‐year ASCVD risk ‡ | 7.4* , † | 8.4 | 10.1 † | 9.0 | 8.5 | 7.9 | <0.0001 | ||||||
| 10‐year ASCVD risk ‡ , categorical | <0.0001 | ||||||||||||
| <5% | 1793* , † | 52.6 | 244 † | 34.4 | 466 | 42.4 | |||||||
| 5%–9.9% | 788 | 23.1 | 202 | 28.5 | 302 | 27.5 | |||||||
| 10%–14.9% | 377 | 11.1 | 112 | 15.8 | 158 | 14.4 | |||||||
| 15%–19.9% | 181 | 5.3 | 66 | 9.3 | 75 | 6.8 | |||||||
| ≥20% | 271 | 8.0 | 85 | 12.0 | 98 | 8.9 | |||||||
| 30‐year lifetime risk § | <0.0001 | ||||||||||||
| All optimal risk factors | 448* , † | 10.5 | 77 † | 10.7 | 87 | 7.1 | |||||||
| ≥ 1 not optimal risk factors | 674 | 15.8 | 86 | 11.9 | 134 | 11.0 | |||||||
| ≥ 1 elevated risk factors | 149 | 3.5% | 35 | 4.8% | 47 | 3.9% | |||||||
| 1 major risk factor | 1989 | 46.5 | 320 | 44.3 | 535 | 43.9 | |||||||
| ≥ 2 major risk factors | 1014 | 23.7 | 205 | 28.4 | 417 | 34.2 | |||||||
| CHD | 224 | 2.8 | 38 | 2.9 | 75 | 3.8 | 0.08 | ||||||
| CVD | 342 † | 4.3 | 64 | 4.8 | 114 | 5.7 | 0.02 | ||||||
| Blood pressure (BP) | |||||||||||||
| Hypertension | 1117* , † | 14.0 | 233 | 17.5 | 334 | 16.7 | 0.0001 | ||||||
| High BP at visit (≥140/90 mm Hg ) | 1369 | 17.1 | 221 | 16.6 | 299 | 15.0 | 0.07 | ||||||
| SBP | 118.3 | 14.2 | 118.6 | 13.8 | 118.1 | 13.6 | 0.84 | ||||||
| DBP | 76.4 | 11.0 | 75.6 | 10.7 | 76.9 | 11.1 | 0.19 | ||||||
| Cholesterol | |||||||||||||
| Total cholesterol | 178.2 | 37.1 | 175.2 | 38.1 | 177.4 | 39.3 | 0.45 | ||||||
| LDL (statin only) | 97.8* , † | 38.0 | 88.4 | 33.6 | 89.5 | 34.6 | <0.0001 | ||||||
| LDL (nonstatin only) | 110.4* , † | 32.1 | 106.1 | 33.4 | 107.9 | 33.1 | 0.0014 | ||||||
| HDL | 48.1* , † | 15.7 | 41.8 | 11.9 | 44.0 | 13.6 | <0.0001 | ||||||
| Triglycerides | 143.0 † | 128.9 | 149.1 | 100.5 | 161.6 | 145.2 | .02 | ||||||
| Statin use | 1486* , † | 18.6 | 395 | 29.7 | 597 | 29.9 | <0.0001 | ||||||
| Glucose | |||||||||||||
| Diabetes | 892* , † | 11.1 | 239 † | 18.0 | 422 | 21.1 | <0.0001 | ||||||
| A1c (DM only) || | 7.4 | 1.8 | 7.1 | 1.7 | 7.2 | 1.7 | 0.08 | ||||||
| A1c (non‐diabetes only) # | 5.6 | 0.9 | 5.6 | 0.7 | 5.6 | 0.8 | 0.75 | ||||||
| A1c (diabetes only), categorical || | 0.14 | ||||||||||||
| <7.0 | 437 | 52.2 | 141 | 59.8 | 225 | 56.7 | |||||||
| 7.0–7.9 | 185 | 22.1 | 52 | 22.0 | 82 | 20.7 | |||||||
| 8.0–8.9 | 78 | 9.3 | 20 | 8.5 | 28 | 7.1 | |||||||
| ≥9 | 137 | 16.4 | 23 | 9.8 | 62 | 15.6 | |||||||
| Weight | |||||||||||||
| BMI | 30.7* , † | 8.2 | 30.0 † | 7.4 | 32.3 | 8.3 | <0.0001 | ||||||
| BMI, categorical | <0.0001 | ||||||||||||
| <18.5, underweight | 81 † | 1.2 | 18 † | 1.6 | 18 | 1.0 | |||||||
| 18.5–24.9, normal | 1536 | 22.1 | 250 | 21.8 | 289 | 16.5 | |||||||
| 25–29.9, overweight | 1977 | 28.4 | 361 | 31.4 | 441 | 25.1 | |||||||
| 30–34.9, obese I | 1569 | 22.6 | 260 | 22.6 | 453 | 25.8 | |||||||
| 35–39.9, obese II | 944 | 13.6 | 145 | 12.6 | 289 | 16.5 | |||||||
| ≥40, obese III | 847 | 12.2 | 115 | 10.0 | 265 | 15.1 | |||||||
| Smoking status | <0.0001 | ||||||||||||
| Current smoker | 2702* , † | 33.8 | 549 † | 41.3 | 848 | 42.4 | |||||||
| Former smoker | 2272 | 28.4 | 292 | 22.0 | 501 | 25.1 | |||||||
| Nonsmoker | 3030 | 37.9 | 488 | 36.7 | 651 | 32.6 | |||||||
| Appropriate aspirin use** | 190 | 84.8 | 70 | 93.3 | 35 | 92.1 | 0.10 | ||||||
A1c indicates glycosylated hemoglobin; ASCVD,10‐year atherosclerotic cardiovascular disease risk; BMI, body mass index; CHD, coronary heart disease; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; SBP, systolic blood pressure; and SMI, serious mental illness.
Significantly different from schizophrenia (P<0.05).
Significantly different from schizoaffective disorder (P<0.05).
ASCVD risk is calculated only for patients aged 40–75 years without CVD (n=5218).
Thirty‐year lifetime risk of CVD is calculated only for patients aged 18–59 years without CVD (n=6217).
Calculated for patients with diabetes who have available A1c tests within the past 5 years (n=1470).
Calculated for patients without diabetes who have available A1c tests within the past 5 years (n=812).
Aspirin use was calculated only for individuals with known CHD (n=337).
Table 4.
Patients With SMI at Baseline: Adjusted Estimates of Total Cardiovascular Risk and Individual Modifiable Cardiovascular Risk Factors
| Cardiovascular risk |
Patients with bipolar disorder n=8004 |
Patients With schizophrenia disorder n=1329 |
Patients with schizoaffective disorder N=2000 |
P value | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| M | PP | LL | UL | M | PP | LL | UL | M | PP | LL | UL | ||
| 10‐year ASCVD risk ‡ | 8.24* , † | 8.03 | 8.47 | 7.22 | 6.28 | 7.71 | 7.76 | 7.37 | 8.14 | 0.0008 | |||
| 10‐year ASCVD risk, ‡ categorical | 0.0008 | ||||||||||||
| <5% | 45.7* | 43.6 | 47.8 | 53.6 † | 49.5 | 57.5 | 45.2 | 42.0 | 48.5 | ||||
| 5%–9.9% | 38.9 | 36.8 | 41.0 | 34.7 | 30.7 | 38.7 | 39.1 | 35.9 | 42.4 | ||||
| 10%–14.9% | 10.3 | 9.0 | 11.6 | 7.9 | 6.2 | 9.7 | 10.5 | 8.6 | |||||
| 15%–19.9% | 2.9 | 2.3 | 3.5 | 2.2 | 1.5 | 2.8 | 3.0 | 2.2 | 3.7 | ||||
| ≥20% | 2.2 | 1.9 | 2.5 | 1.6 | 1.3 | 2.0 | 2.2 | 1.9 | 2.7 | ||||
| 30‐year lifetime risk § | 0.0002 | ||||||||||||
| All optimal risk factors | 8.5* , † | 7.8 | 9.3 | 10.3 † | 9.0 | 11.9 | 7.4 | 6.6 | 8.4 | ||||
| ≥1 not optimal risk factors | 14.0 | 13.2 | 14.7 | 16.1 | 14.6 | 17.6 | 12.6 | 11.6 | 13.5 | ||||
| ≥1 elevated risk factors | 3.8 | 2.6 | 5.0 | 4.2 | 1.4 | 7.1 | 3.5 | 1.7 | 5.4 | ||||
| 1 major risk factor | 49.1 | 47.8 | 50.4 | 48.5 | 45.4 | 51.6 | 49.0 | 47.0 | 51.1 | ||||
| ≥2 major risk factors | 24.6 | 23.4 | 25.9 | 20.8 | 18.5 | 23.4 | 27.5 | 25.3 | 29.8 | ||||
| CHD | 1.4* | 1.2 | 1.8 | 0.8 † | 0.6 | 1.2 | 1.4 | 1.0 | 1.9 | 0.018 | |||
| CVD | 2.4* | 2.1 | 2.9 | 1.6 † | 1.2 | 2.2 | 2.3 | 1.8 | 2.9 | 0.027 | |||
| BP | |||||||||||||
| Hypertension | 11.9 | 11.0 | 12.8 | 10.3 | 8.9 | 12.0 | 10.9 | 9.6 | 12.3 | 0.14 | |||
| High BP at visit (≥140/90 mm Hg) | 17.1* , † | 16.1 | 18.2 | 13.2 | 11.4 | 15.1 | 13.1 | 11.6 | 14.7 | <0.0001 | |||
| SBP | 122.1* , † | 121.8 | 122.5 | 118.8 † | 117.9 | 119.7 | 120.1 | 119.3 | 120.7 | <0.0001 | |||
| DBP | 77.5* , † | 77.3 | 77.7 | 75.2 † | 74.6 | 75.9 | 76.4 | 75.9 | 77.0 | <0.0001 | |||
| Cholesterol | |||||||||||||
| Total cholesterol | 185.0* , † | 183.9 | 186.2 | 177.7 | 175.0 | 180.3 | 180.1 | 178.0 | 182.2 | <0.0001 | |||
| LDL (statin only) | 97.3* , † | 95.9 | 99.3 | 90.3 | 86.4 | 94.1 | 89.7 | 86.7 | 92.8 | <0.0001 | |||
| LDL (nonstatin only) | 110.0 | 109.0 | 111.1 | 106.8 | 104.2 | 109.4 | 108.7 | 106.7 | 110.7 | 0.071 | |||
| HDL | 49.2* , † | 48.8 | 49.6 | 47.2 | 46.2 | 48.1 | 46.1 | 45.4 | 46.9 | <0.0001 | |||
| Triglycerides | 152.4 † | 149.1 | 155.6 | 144.1 † | 136.5 | 151.8 | 159.3 | 153.4 | 165.3 | 0.006 | |||
| Statin use | 14.5 † | 13.5 | 15.5 | 15.8 † | 13.9 | 17.9 | 19.0 | 17.2 | 20.9 | <0.0001 | |||
| Glucose | |||||||||||||
| Diabetes | 9.5 † | 8.8 | 10.3 | 9.6 † | 8.2 | 11.2 | 13.4 | 12.0 | 15.1 | <0.0001 | |||
| A1c (diabetes only) || | 7.32 | 7.20 | 7.44 | 7.17 | 6.94 | 7.41 | 7.20 | 7.02 | 7.38 | 0.40 | |||
| A1c (non‐diabetes only) # | 5.51 | 5.48 | 5.54 | 5.45 | 5.39 | 5.52 | 5.49 | 5.44 | 5.55 | 0.36 | |||
| A1c (diabetes only), categorical || | 0.166 | ||||||||||||
| <7.0 | 52.3 | 48.9 | 55.8 | 59.1 | 52.4 | 65.4 | 55.9 | 51.1 | 60.7 | ||||
| 7.0–7.9 | 23.1 | 19.6 | 26.5 | 21.0 | 14.5 | 27.6 | 22.1 | 17.2 | 26.9 | ||||
| 8.0–8.9 | 9.2 | 6.4 | 12.0 | 7.7 | 3.3 | 12.1 | 8.4 | 4.8 | 12.0 | ||||
| ≥9 | 15.4 | 13.4 | 17.8 | 12.2 | 9.4 | 15.6 | 13.6 | 11.2 | 16.5 | ||||
| Weight | |||||||||||||
| BMI | 31.0* , † | 30.9 | 31.2 | 30.3 † | 29.8 | 30.8 | 32.0 | 31.6 | 32.4 | <0.0001 | |||
| BMI, categorical | <0.0001 | ||||||||||||
| <18.5, underweight | 1.2* , † | 1.0 | 1.4 | 1.4 † | 1.1 | 1.7 | 0.9 | 0.8 | 1.1 | ||||
| 18.5–24.9, normal | 21.1 | 20.2 | 22.0 | 23.6 | 23.3 | 23.9 | 17.3 | 17.1 | 17.5 | ||||
| 25–29.9, overweight | 28.7 | 27.8 | 29.7 | 29.7 | 27.6 | 31.8 | 26.5 | 25.1 | 27.9 | ||||
| 30–34.9, obese I | 23.4 | 22.2 | 24.6 | 22.4 | 19.7 | 25.1 | 24.6 | 22.4 | 26.7 | ||||
| 35–39.9, obese II | 13.7 | 12.8 | 14.7 | 12.5 | 10.5 | 14.5 | 15.9 | 14.0 | 17.8 | ||||
| ≥40, obese III | 11.9 | 11.2 | 12.6 | 10.4 | 9.3 | 11.6 | 14.8 | 13.6 | 16.0 | ||||
| Smoking status | <0.0001 | ||||||||||||
| Current smoker | 34.3* , † | 33.0 | 35.6 | 36.3 † | 33.4 | 39.1 | 38.6 | 36.2 | 40.9 | ||||
| Former smoker | 28.6% | 27.3% | 30.0% | 22.6% | 20.1% | 25.1% | 25.4% | 23.3% | 27.5% | ||||
| Nonsmoker | 37.2 | 35.9 | 38.4 | 41.1 | 38.2 | 44.1 | 36.0 | 33.8 | 38.3 | ||||
| Appropriate aspirin use** , †† | 91.2 † | 0.1 | 100 | 95.3 | 0.2 | 100 | 97.7 | 0.5 | 100 | 0.048 | |||
Models adjusted for age, sex, race, and ethnicity. A1c indicates glycosylated hemoglobin; ASCVD, 10‐year atherosclerotic cardiovascular disease risk; BMI, body mass index; CHD, coronary heart disease; CVD, cardiovascular disease; DBP, diastolic blood pressure; HDL, high‐density lipoprotein; LDL, low‐density lipoprotein; PP, predicted probability (percent); SBP, ystolic blood pressure; and SMI, serious mental illness.
Significantly different from schizophrenia (P<0.05).
Significantly different from schizoaffective disorder (P<0.05).
ASCVD risk is calculated only for patients aged 40–75 years without CVD (n=5218).
Thirty‐year lifetime risk of CVD is calculated only for patients aged 18–59 years without CVD (n=6217).
Calculated for patients with diabetes who have available A1c tests within the past 5 years (n=1470).
Calculated for patients without diabetes who have available A1c tests within the past 5 years (n=812).
Aspirin use was only calculated for individuals with known CHD (n=337).
Separation occurred with this model, which inflated the confidence limits.
Sensitivity Analyses
To determine which covariate(s) contributed the most to cardiovascular risk differences between groups, models predicting differences for patients with and without SMI on 10‐year cardiovascular risk and 30‐year cardiovascular risk were run separately for each covariate. For both models, adjusting for sex or race and ethnicity alone had little impact on estimates. For example, for 10‐year cardiovascular risk, adjusting for race and ethnicity slightly decreased cardiovascular risk estimates and adjusting for sex slightly increased cardiovascular risk estimates for patients with SMI. In contrast, adjusting for age greatly increased estimated 10‐year cardiovascular risk (predicted mean, 9.30; 95% CI, 9.13–9.48) and adjusting for insurance type greatly decreased estimated 10‐year cardiovascular risk (predicted mean, 6.11; 95% CI, 5.9–6.3).
To further understand the impact of age on cardiovascular risk, models predicting differences in 10‐year cardiovascular risk and 30‐year cardiovascular risk for patients with and without SMI were stratified by age (Table 5). For both the 10‐year and 30‐year cardiovascular risk measures, the differences in cardiovascular risk were greatest at younger ages, suggesting a clinically significant increased cardiovascular risk in young adult patients with SMI compared with young adult patients without SMI. The differences in 10‐year cardiovascular risk between SMI and non‐SMI patients were attenuated at older ages.
Table 5.
Cardiovascular Risk for Patients With SMI and Without SMI, Stratified by Age
| Cardiovascular risk | β | LL | UL | P value |
|---|---|---|---|---|
| 10‐year ASCVD risk* | ||||
| Age 40–49 y, n=64 240 | 1.46 | 1.30 | 1.62 | <0.0001 |
| Age 50–59 y, n=86 425 | 1.70 | 1.46 | 1.93 | <0.0001 |
| Age 60–69 y, n=74 355 | 0.76 | 0.31 | 1.20 | 0.0008 |
| Age 70–75 y, n=22 889 | −0.04 | −1.26 | 1.18 | 0.95 |
| OR | LL | UL | P value | |
|---|---|---|---|---|
| 30‐year lifetime risk* | ||||
| Age 18–29 y, n=24 960 | 2.98 | 2.64 | 3.37 | <0.0001 |
| Age 30–39 y, n=46 559 | 3.20 | 2.92 | 3.52 | <0.0001 |
| Age 40–49 y, n=65 281 | 2.89 | 2.62 | 3.13 | <0.0001 |
| Age 50–59 y, n=86 508 | 0.45 | 0.41 | 0.48 | <0.0001 |
β indicates unstandardized regression coefficient; LL, 95% lower confidence limit; OR, odds ratio; SMI, serious mental illness; and UL; 95% upper confidence limit.
10‐year ASCVD risk and 30‐year lifetime risk are calculated only for patients without CVD.
Discussion
In this cross‐sectional study of 11 333 people with SMI, patients with SMI had greater cardiovascular risk at younger ages than those without SMI. Patients with SMI who were aged 40 to 75 years without known CVD had a significantly elevated mean 10‐year cardiovascular risk of 8.31, compared with 7.95 in those without SMI, after adjustment for age, sex, race, ethnicity, and insurance type. This difference in risk diminished with age. This observation might be related to increased treatment and control of cardiovascular risk factors in older patients with SMI. Alternatively, it may reflect survival bias, with patients with SMI dying at younger ages than those without SMI. For 30‐year risk, calculated for those aged 18 to 59 years without known CVD, significantly more patients with SMI were in the highest tier of risk (≥ 2 major risk factors) compared with those without SMI (18.8% versus 10.8%; P<0.0001). This elevated 30‐year risk in patients with SMI may be related to elevated rates of smoking and obesity in young adults with SMI, as well as delayed recognition or management of elevated cardiovascular risk factors in this population. Regardless, these data support the growing body of evidence that early identification and management of major cardiovascular risk factors in young adults with SMI is indicated and could have a substantive impact on subsequent adverse cardiovascular outcomes in this group of young adults. 10
Estimated 10‐year cardiovascular risk in unadjusted models was highest for patients with schizophrenia, followed by schizoaffective disorder and bipolar disorder. However, because patients with bipolar disorder were younger, more likely to be women, and more likely to be White, adjustment for age, sex, race, and ethnicity resulted in 10‐year cardiovascular risk estimates that were more similar across SMI subgroups. The adjusted mean estimated 10‐year cardiovascular risk for patients with SMI of 8.31 is similar to those reported in previous studies. 3 , 11 , 12 , 13 Of note, inclusion of patients with mental health diagnoses other than SMI in the “patients without SMI” group may make our estimates of elevated cardiovascular risk for “patients with SMI” conservative.
To our knowledge, this is the first study examining estimated 30‐year (lifetime) cardiovascular risk in a large outpatient sample of patients with SMI, and the differences in 30‐year risk between patients with and without SMI are striking, with considerably higher 30‐year risk for patients with SMI in both unadjusted and adjusted models. As noted above, in adjusted models, 18.8% of those with SMI were at the highest level of 30‐year risk (ie, ≥2 major risk factors) compared with only 10.8% of those without SMI. Among those with SMI, nearly 3 times as many patients with schizoaffective disorder were at the highest level of 30‐year risk compared with those without SMI (27.5%; 95% CI, 25.3%–29.8%), while the rates of patients with bipolar disorder (24.6%; 95% CI, 23.4%–25.9%) and schizophrenia (20.8%; 95% CI, 18.5%–23.4%) with this highest level of risk were about twice that of patients without SMI. Given evidence that people with SMI die significantly earlier than their peers, 2 increased time spent in better midlife cardiovascular health has significant benefits for cardiovascular outcomes later in life for the general population, 14 and interventions to address cardiovascular risk for patients with SMI are maximally beneficial when initiated at younger ages, 10 we strongly encourage health care systems and clinicians to use 30‐year/lifetime estimated cardiovascular risk to identify at‐risk patients with SMI who are aged <40 years for early intervention. The more widely used 10‐year cardiovascular risk equations are not valid until age 40 years, and delayed clinical recognition and control of cardiovascular risk factors for many years may be a major factor driving excess mortality in those with SMI. Of note, Osborn and colleagues have developed and tested 10‐year cardiovascular risk prediction models meant to be specific to people with SMI, and we look forward to studies validating and implementing these models. 15 However, we think our findings stress the importance of also using 30‐year risk models in this highly at‐risk SMI population.
Many previous studies of cardiovascular risk for people with SMI have included only inpatients with SMI, cohorts that tend to have more severe SMI and more medical comorbidities than outpatients with SMI, or included patients with major depression in their definition of SMI. 16 This study, in contrast, includes a large sample of community‐dwelling US outpatients with SMI (defined as having bipolar disorder, schizophrenia, or schizoaffective disorder but not unipolar depression). Accordingly, our findings are likely more representative of cardiovascular risk in community populations with bipolar disorder or psychosis. These estimates of cardiovascular risk are still significantly higher than the general population.
Additionally, there are few studies that estimate cardiovascular risk in people both with and without SMI in the same study sample. Several studies, for example, compare cardiovascular risk in people with SMI in their sample to a National Health and Nutrition Examination study sample. 3 , 4 , 5 Such comparisons are potentially more fraught with volunteer and other bias and challenges in adjustment for sample characteristics; our study sample includes people with and without SMI cared for in the same outpatient care setting. However, despite inclusion of a large sample of people with SMI and without SMI insured by Medicaid or Medicare in additional to commercial insurance, we acknowledge that the patients receiving care in an integrated health care system may be relatively healthier than those seeking care in other settings, such as safety net clinics. The likely effect of this would be to make our estimates of cardiovascular risk associated with SMI more conservative.
By examination of the absolute differences in proportions of people with and without SMI not at goal for individual cardiovascular risk factors, the risk factors contributing most to increased cardiovascular risk for those with SMI were elevated BMI and smoking. In unadjusted estimates, nearly 80% of patients with SMI had a BMI >24.9 compared with 69% of patients without SMI, with 50% of patients with SMI meeting criteria for obesity (BMI ≥30) compared with 36% of patients without SMI (Table 1). This prevalence of obesity in patients with SMI is in line with other studies 17 , 18 , 19 , 20 that have reported rates generally ranging from 40% to 55%. Patients with schizoaffective disorder in our study had the highest mean BMI, at 32.3, and the highest percentage of patients with a BMI ≥40 at 15%. Of patients with SMI, 36% were current smokers compared with 12% of patients without SMI. Of note, this smoking prevalence for patients with SMI is lower than most previously reported rates (ranging from 49% to 68%) 15 , 19 , 20 and may reflect increasing access to smoking cessation strategies for those with SMI in our study population. 21 , 22 This is admittedly speculation, however, as we did not collect data on smoking cessation medication use in this study.
Regarding other individual cardiovascular risk factors, patients with SMI had double the rate of diagnosed diabetes than did patients without SMI (13.7% versus 6.5%; P<0.0001). These rates are similar to those reported in other studies 19 , 23 , 24 but lower than found in a large outpatient primary care sample in England, where 18.9% of patients with schizophrenia and 13.5% of patients with bipolar disorder were reported to have diabetes. 19 , 20 Patients with SMI had statistically but not clinically meaningfully lower total cholesterol compared with those without SMI, but clinically meaningful higher triglyceride levels (151.8 versus 129.0; P<0.0001), which would be consistent with metabolic changes associated with increased rates of obesity and diabetes. Notably, patients with SMI were more likely to be prescribed a statin than were those without SMI (12.8% versus 7.4%; P<0.0001). Overall, 10% of patients with SMI were diagnosed with hypertension. Estimates of hypertension for people with SMI have varied widely in other studies, with reported prevalence ranging from 19% to 61%. 16 , 19 , 20
This study focuses on the contribution of conventional major cardiovascular risk factors to overall cardiovascular risk for people with SMI. Our data are consistent with previous studies that found inferior preventative cardiovascular care and decreased or delayed treatment when cardiovascular risk is identified in those with SMI. 25 , 26 , 27 , 28 However, it is widely recognized that a number of other factors, including increased alcohol use, lower physical activity, poorer socioeconomic status, and suboptimal diet, also contribute to the observed excess burden of CVD in SMI patients. 29 Additionally, there is evidence of overlap between genetic risk for SMI and risk for hypertension, cardiac dysrhythmia, nonrheumatic heart disease, and type 1 diabetes. 30 Moreover, many medications used to treat SMI may increase cardiovascular risk, largely through cardiometabolic side effects. 31
We have already mentioned that a potential limitation of this study is its conduct in an integrated health care system, which may limit its generalizability to other settings. Other potential limitations include those inherent in observational studies, including possible classification bias related to SMI status when using EHR data and measured and unmeasured confounders that may affect findings. Additionally, we did not have data on some social determinants of health, such as relationship status, exercise, institutionalization, income, or education, all of which are significant predictors of cardiovascular health. We also did not take use of medications into account. Nonetheless, we submit that the benefits of understanding baseline cardiovascular risk in a large outpatient sample of patients with and without SMI using rich and reasonably complete EHR data outweigh these potential limitations.
In conclusion, patients with SMI have elevated 10‐year and 30‐year CV risk compared with patients without SMI. Given the shortened life span of people with SMI, and the considerable contribution of CV disease to earlier mortality, the data support more thorough screening and effective management of major cardiovascular risk factors for patients with SMI starting at a younger age, especially in those aged <40 years. Use of 30‐year cardiovascular risk estimates to help guide decisions about cardiovascular risk factor management and prevention in young adults with SMI may be important to decreasing rates of cardiovascular morbidity and mortality.
Sources of Funding
This work was supported by a Cooperative Agreement with the National Institute of Mental Health (NIMH) grant U19MH092201.
Disclosures
All authors declare no research grants beyond the support from NIMH listed above and no other research support, honoraria, expert witness fees, or ownership interest.
Supporting information
Tables S1–S2
Supplemental Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.021444
For Sources of Funding and Disclosures, see page 16.
References
- 1. Osborn DP, Levy G, Nazareth I, Petersen I, Islam A, King MB. Relative risk of cardiovascular and cancer mortality in people with severe mental illness from the United Kingdom's General Practice Research Database. Arch Gen Psychiatry. 2007;64:242–249. doi: 10.1001/archpsyc.64.2.242 [DOI] [PubMed] [Google Scholar]
- 2. Walker ER, McGee RE, Druss BG. Mortality in mental disorders and global disease burden implications: a systematic review and meta‐analysis. JAMA Psychiatry. 2015;72:334–341. doi: 10.1001/jamapsychiatry.2014.2502 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Goff DC, Sullivan LM, McEvoy JP, Meyer JM, Nasrallah HA, Daumit GL, Lamberti S, D'Agostino RB, Stroup TS, Davis S, et al. A comparison of ten‐year cardiac risk estimates in schizophrenia patients from the CATIE study and matched controls. Schizophr Res. 2005;80:45–53. doi: 10.1016/j.schres.2005.08.010 [DOI] [PubMed] [Google Scholar]
- 4. Ratliff JC, Palmese LB, Reutenauer EL, Srihari VH, Tek C. Obese schizophrenia spectrum patients have significantly higher 10‐year general cardiovascular risk and vascular ages than obese individuals without severe mental illness. Psychosomatics. 2013;54:67–73. doi: 10.1016/j.psym.2012.03.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Keenan TE, Yu A, Cooper LA, Appel LJ, Guallar E, Gennusa JV, Dickerson FB, Crum RM, Anderson CA, Campbell LM, et al. Racial patterns of cardiovascular disease risk factors in serious mental illness and the overall U.S. population. Schizophr Res. 2013;150:211–216. doi: 10.1016/j.schres.2013.07.022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Goff DC, Lloyd‐Jones DM, Bennett G, Coady S, D’Agostino RB, Gibbons R, Greenland P, Lackland DT, Levy D, O’Donnell CJ, et al. 2013 ACC/AHA guideline on the assessment of cardiovascular risk: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation. 2014;129:S49–S73. doi: 10.1161/01.cir.0000437741.48606.98 [DOI] [PubMed] [Google Scholar]
- 7. Rossom RC, O'Connor PJ, Crain AL, Waring S, Ohnsorg K, Taran A, Kopski K, Sperl‐Hillen JM. Pragmatic trial design of an intervention to reduce cardiovascular risk in people with serious mental illness. Contemp Clin Trials. 2020;91:105964. doi: 10.1016/j.cct.2020.105964 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Pencina MJ, D'Agostino RB Sr, Larson MG, Massaro JM, Vasan RS. Predicting the 30‐year risk of cardiovascular disease: the Framingham Heart Study. Circulation. 2009;119:3078–3084. doi: 10.1161/circulationaha.108.816694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Bibbins‐Domingo K. Aspirin use for the primary prevention of cardiovascular disease and colorectal cancer: U.S. Preventive Services Task Force recommendation statement. Ann Intern Med. 2016;164:836–845. doi: 10.7326/m16-0577 [DOI] [PubMed] [Google Scholar]
- 10. Hoang U, Goldacre MJ, Stewart R. Avoidable mortality in people with schizophrenia or bipolar disorder in England. Acta Psychiatr Scand. 2013;127:195–201. doi: 10.1111/acps.12045 [DOI] [PubMed] [Google Scholar]
- 11. Cohn T, Prud'homme D, Streiner D, Kameh H, Remington G. Characterizing coronary heart disease risk in chronic schizophrenia: high prevalence of the metabolic syndrome. Can J Psychiatry. 2004;49:753–760. doi: 10.1177/070674370404901106 [DOI] [PubMed] [Google Scholar]
- 12. Garcia‐Portilla MP, Saiz PA, Bascaran MT, Martínez AS, Benabarre A, Sierra P, Torres P, Montes JM, Bousoño M, Bobes J. Cardiovascular risk in patients with bipolar disorder. J Affect Disord. 2009;115:302–308. doi: 10.1016/j.jad.2008.09.008 [DOI] [PubMed] [Google Scholar]
- 13. Daumit GL, Dalcin AT, Dickerson FB, Miller ER, Evins AE, Cather C, Jerome GJ, Young DR, Charleston JB, Gennusa JV, et al. Effect of a comprehensive cardiovascular risk reduction intervention in persons with serious mental illness: a randomized clinical trial. JAMA Netw Open. 2020;3:e207247. doi: 10.1001/jamanetworkopen.2020.7247 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Corlin L, Short MI, Vasan RS, Xanthakis V. Association of the duration of ideal cardiovascular health through adulthood with cardiometabolic outcomes and mortality in the Framingham Offspring Study. JAMA Cardiol. 2020;5:549–556. doi: 10.1001/jamacardio.2020.0109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Osborn DPJ, Hardoon S, Omar RZ, Holt RIG, King M, Larsen J, Marston L, Morris RW, Nazareth I, Walters K, et al. Cardiovascular risk prediction models for people with severe mental illness: results from the Prediction and Management of Cardiovascular Risk in People With Severe Mental Illnesses (PRIMROSE) research program. JAMA Psychiatry. 2015;72:143–151. doi: 10.1001/jamapsychiatry.2014.2133 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Correll CU, Solmi M, Veronese N, Bortolato B, Rosson S, Santonastaso P, Thapa‐Chhetri N, Fornaro M, Gallicchio D, Collantoni E, et al. Prevalence, incidence and mortality from cardiovascular disease in patients with pooled and specific severe mental illness: a large‐scale meta‐analysis of 3,211,768 patients and 113,383,368 controls. World Psychiatry. 2017;16:163–180. doi: 10.1002/wps.20420 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Gardner‐Sood P, Lally J, Smith S, Atakan Z, Ismail K, Greenwood KE, Keen A, O'Brien C, Onagbesan O, Fung C, et al. Cardiovascular risk factors and metabolic syndrome in people with established psychotic illnesses: baseline data from the IMPaCT randomized controlled trial. Psychol Med. 2015;45:2619–2629. doi: 10.1017/s0033291715000562 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Correll CU, Druss BG, Lombardo I, O'Gorman C, Harnett JP, Sanders KN, Alvir JM, Cuffel BJ. Findings of a U.S. national cardiometabolic screening program among 10,084 psychiatric outpatients. Psychiatr Serv. 2010;61:892–898. doi: 10.1176/ps.2010.61.9.892 [DOI] [PubMed] [Google Scholar]
- 19. De Hert M, Dekker JM, Wood D, Kahl KG, Holt RI, Möller HJ. Cardiovascular disease and diabetes in people with severe mental illness position statement from the European Psychiatric Association (EPA), supported by the European Association for the Study of Diabetes (EASD) and the European Society of Cardiology (ESC). Eur Psychiatry. 2009;24:412–424. doi: 10.1016/j.eurpsy.2009.01.005 [DOI] [PubMed] [Google Scholar]
- 20. Pérez‐Piñar M, Mathur R, Foguet Q, Ayis S, Robson J, Ayerbe L. Cardiovascular risk factors among patients with schizophrenia, bipolar, depressive, anxiety, and personality disorders. Eur Psychiatry. 2016;35:8–15. doi: 10.1016/j.eurpsy.2016.02.004 [DOI] [PubMed] [Google Scholar]
- 21. Siskind DJ, Wu BT, Wong TT, Firth J, Kisely S. Pharmacological interventions for smoking cessation among people with schizophrenia spectrum disorders: a systematic review, meta‐analysis, and network meta‐analysis. Lancet Psychiatry. 2020;7:762–774. doi: 10.1016/s2215-0366(20)30261-3 [DOI] [PubMed] [Google Scholar]
- 22. Peckham E, Brabyn S, Cook L, Tew G, Gilbody S. Smoking cessation in severe mental ill health: what works? An updated systematic review and meta‐analysis. BMC Psychiatry. 2017;17:252. doi: 10.1186/s12888-017-1419-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Olsson E, Westman J, Sudic Hukic D, Eriksson SV, Edman G, Bodén R, Jedenius E, Reutfors J, Berntsson A, Hilding A, et al. Diabetes and glucose disturbances in patients with psychosis in Sweden. BMJ Open Diabetes Res Care. 2015;3:e000120. doi: 10.1136/bmjdrc-2015-000120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Vancampfort D, Correll CU, Galling B, Probst M, De Hert M, Ward PB, Rosenbaum S, Gaughran F, Lally J, Stubbs B. Diabetes mellitus in people with schizophrenia, bipolar disorder and major depressive disorder: a systematic review and large scale meta‐analysis. World Psychiatry. 2016;15:166–174. doi: 10.1002/wps.20309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Ayerbe L, Forgnone I, Addo J, Siguero A, Gelati S, Ayis S. Hypertension risk and clinical care in patients with bipolar disorder or schizophrenia; a systematic review and meta‐analysis. J Affect Disord. 2018;225:665–670. doi: 10.1016/j.jad.2017.09.002 [DOI] [PubMed] [Google Scholar]
- 26. Mitchell AJ, Lord O. Do deficits in cardiac care influence high mortality rates in schizophrenia? A systematic review and pooled analysis. J Psychopharmacol. 2010;24:69–80. doi: 10.1177/1359786810382056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Skrede S, Tvete IF, Tanum L, Steen VM, Bramness JG. Incident users of antipsychotic agents and future use of cholesterol‐lowering drugs: an observational, pharmacoepidemiologic study. J Clin Psychiatry. 2015;76:e111–e116. doi: 10.4088/JCP.14m08996 [DOI] [PubMed] [Google Scholar]
- 28. Heiberg IH, Jacobsen BK, Balteskard L, Bramness JG, Naess Ø, Ystrom E, Reichborn‐Kjennerud T, Hultman CM, Nesvåg R, Høye A. Undiagnosed cardiovascular disease prior to cardiovascular death in individuals with severe mental illness. Acta Psychiatr Scand. 2019;139:558–571. doi: 10.1111/acps.13017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. von Hausswolff‐Juhlin Y, Bjartveit M, Lindström E, Jones P. Schizophrenia and physical health problems. Acta Psychiatr Scand Suppl. 2009;119:15–21. doi: 10.1111/j.1600-0447.2008.01309.x [DOI] [PubMed] [Google Scholar]
- 30. Wang K, Gaitsch H, Poon H, Cox NJ, Rzhetsky A. Classification of common human diseases derived from shared genetic and environmental determinants. Nat Genet. 2017;49:1319–1325. doi: 10.1038/ng.3931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Tek C, Kucukgoncu S, Guloksuz S, Woods SW, Srihari VH, Annamalai A. Antipsychotic‐induced weight gain in first‐episode psychosis patients: a meta‐analysis of differential effects of antipsychotic medications. Early Interv Psychiatry. 2016;10:193–202. doi: 10.1111/eip.12251 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


