Abstract
Introduction
Endovascular therapy (EVT) use increased following clinical trials publication in 2015, but limited data suggest there may be persistent race and ethnicity differences.
Methods and Results
We included all patients with acute ischemic stroke arriving within 6 hours of last known well and with National Institute of Health Stroke Scale (NIHSS) score ≥6 between April 2012 and June 2019 in the Get With The Guidelines‐Stroke database and evaluated the association between race and ethnicity and EVT use and outcomes, comparing the era before versus after 2015. Of 302 965 potentially eligible patients; 42 422 (14%) underwent EVT. Although EVT use increased over time in all racial and ethnic groups, Black patients had reduced odds of EVT use compared with non‐Hispanic White (NHW) patients (adjusted odds ratio [aOR] before 2015, 0.68 [0.58‒0.78]; aOR after 2015, 0.83 [0.76‒0.90]). In‐hospital mortality/discharge to hospice was less frequent in Black, Hispanic, and Asian patients compared with NHW. Conversely discharge home was more frequent in Hispanic (29.7%; aOR, 1.28 [1.16‒1.42]), Asian (28.2%; aOR, 1.23 [1.05‒1.44]), and Black (29.1%; aOR, 1.08 [1.00‒1.18]) patients compared with NHW (24%). However, at 3 months, functional independence (modified Rankin Scale, 0–2) occurred less frequently in Black (37.5%; aOR, 0.84 [0.75‒0.95]) and Asian (33%; aOR, 0.79 [0.65‒0.98]) patients compared with NHW patients (38.1%).
Conclusions
In a large cohort of patients treated with EVT, Black versus NHW patient disparities in EVT use have narrowed over time but still exist. Discharge related outcomes were slightly more favorable in racial and ethnic underrepresented groups; 3‐month functional outcomes were worse but improved across all groups with time.
Keywords: endovascular therapy, health equity, ischemic stroke, race and ethnicity
Subject Categories: Race and Ethnicity, Disparities, Health Equity, Ischemic Stroke, Cerebrovascular Disease/Stroke
Nonstandard Abbreviations and Acronyms
- EVT
endovascular therapy
- GWTG
Get With The Guidelines
- NHW
non‐Hispanic White
Clinical Perspective
What Is New?
Since the advent of endovascular therapy, some acute ischemic strokes secondary to large vessel occlusion are eligible for further treatment, leading to improved functional neurologic outcomes.
There are preexisting racial and ethnic disparities in stroke care which are also evident in the use of endovascular therapy for acute ischemic stroke. In this study, we demonstrate that these disparities have narrowed post publication of major endovascular therapy trials in 2015 but persist particularly for Black patients compared with Non‐Hispanic White patients.
What Are the Clinical Implications?
We also found that outcomes post‐endovascular therapy have similarly improved over time for all racial and ethnic groups, but long‐term outcomes seem to be worse in under‐represented racial and ethnic groups. Dedicated efforts to understand the underlying causes for these disparities and address them with focused educational and systemic health care interventions are urgently required.
Acute ischemic stroke is a significant public health problem with a higher incidence and mortality among certain racial and ethnic groups such as Black and Hispanic individuals. 1 There are prior reports of racial disparities for intravenous tissue plasminogen activator access and acute ischemic stroke outcomes 2 , 3 , 4 , 5 , 6 because of barriers such as poor stroke recognition and delayed arrival times. There are similar disparities in access to endovascular therapy (EVT). For example, Black and Native American patients had significantly lower rates of EVT than White, Hispanic, and Asian/Pacific Islander patients, 7 while in a large GWTG (Get With The Guidelines) study published in 2015, Black patients had lower odds of receiving EVT (odds ratio [OR], 0.70; 95% CI, 0.66–0.75) compared with Non‐Hispanic White (NHW) patients. 8
Given the publication in 2015 of several randomized controlled clinical trials as well as meta‐analyses showing benefit of EVT, we used the GWTG database to examine if clinical practices had changed the magnitude of race and ethnicity differences in the rates of mechanical thrombectomy during the pre‐ and post‐publication eras. The comprehensive GWTG database is uniquely suited to analyze factors related to the potential racial and ethnic disparities in the rates of EVT, and to further explore whether such factors contribute to differences in clinical outcome.
Methods
The authors declare that all supporting data are available within the article and its online supplementary files.
GWTG Program Design
GWTG–Stroke is a voluntary, continuous registry and performance improvement initiative. It was designed as an in‐hospital program for improving stroke care by promoting consistent adherence to the latest scientific treatment guidelines. Since its initiation in 2003, 3517 hospitals have entered >7 million patient records into the GWTG‒Stroke database. 9 Numerous published studies demonstrate the program's success in achieving measurable patient outcome improvements. A detailed description of this registry was published previously. 5 , 10 , 11 The nationwide representativeness of the GWTG registry for stroke in regards to patient demographics and clinic characteristics has also been well documented. 12 , 13
The eligibility of each acute stroke is confirmed at chart review before abstraction. This is followed by de‐identified patient data entry into the GWTG–Stroke database using a web‐based patient management tool (Outcome, A Quintiles Company; Cambridge, MA).
All participating institutions were required to comply with local regulatory and privacy guidelines and to secure institutional review board approval if necessary. The Duke Clinical Research Institute (Durham, NC) serves as the data analysis center, and its institutional review board approval was granted to analyze aggregate de‐identified data for research purposes.
Data were collected from patients admitted and discharged at GWTG participating hospitals between April 2012 and June 2019 with a final diagnosis of acute ischemic stroke (Figure 1). Sites had to have at least 30 patients and participate for >4 consecutive quarters. We included all patients potentially eligible for EVT, defined as those with ischemic stroke presenting <6 hours of last known well time and with admission NIHSS of at least 6 points. The NIHSS is a systematic assessment tool that provides a quantitative measure of stroke‐related neurologic deficit. We excluded patients with missing data for race and ethnicity or key time points, inpatient stroke onset, or receipt of EVT at an outside hospital. To be included as treated with EVT, patients needed to receive EVT within 8 hours of last known well. Informed consent was not required given data collected through GWTG registry in accordance with guidelines in the Journal’s “Instructions to Authors” section.
Figure 1. Flow diagram for inclusion/exclusion of study subjects.
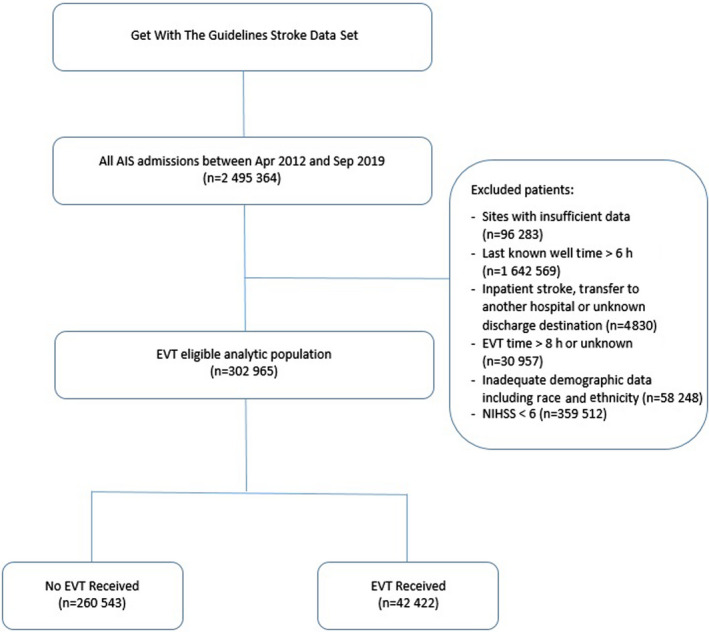
The National Institutes of Health Stroke Scale (NIHSS) is a systematic assessment tool that provides a quantitative measure of stroke‐related neurologic deficit. AIS indicates acute ischemic stroke; EVT, endovascular therapy.
Race and ethnicity were determined from the relevant fields in the medical record entered into GWTG. Racial and ethnic groups were defined as NHW, non‐Hispanic Black, Hispanic, Asian, and other. “Other” refers to people including but not limited to Alaskan, Native American, Native Hawaiian, and Pacific Islanders. 14 Our outcomes of interest were receipt of EVT and short‐term functional outcome, as measured at discharge by destination and ambulatory status. We also report modified Rankin Scale (mRS) 0 to 2 at discharge and 90 days, as well in‐hospital death/hospice, and symptomatic intracranial hemorrhage.
Statistical Analysis
Pearson χ 2 tests were used to compare differences in categorical variables (presented as frequencies and percentages) across the 2 groups, and Wilcoxon rank‐sum tests were used to compare continuous variables (presented as medians and interquartile ranges) across the 2 groups. The temporal trends of EVT use were examined using Cochran‐Armitage trend test by calendar quarters and the overall EVT eligible population stratified by racial and ethnic groups. The exposure of interest was race and ethnicity, and the outcomes of interest included the utilization of EVT, short term and long‐term outcomes including in‐hospital mortality/discharge to hospice and other discharge dispositions (home or rehabilitation). Unadjusted and adjusted associations of race and ethnicity and end points were analyzed using generalized logistic regression models for the entire data set and for strokes pre‐ and post‐2015. The adjusted model controlled for baseline patient characteristics and hospital‐level factors that are expected to be predictive of outcome and have been used in prior GWTG‐Stroke analyses. 8 , 15 , 16 , 17 Analysis adjusting for sex and race and ethnicity only was also performed. Generalized estimating equations were used to account for patients clustered within the same hospital site. Odds ratios (OR) for each race and ethnicity group comparing with the reference group NHW are reported. The adjusted models adjusted for demographics (age, sex, insurance type), medical history (atrial fibrillation/flutter, prosthetic heart valve, previous stroke/TIA, coronary artery disease (CAD)/prior myocardial infarction, heart failure, carotid stenosis, peripheral vascular disease, hypertension, dyslipidemia, diabetes, smoker, prior antithrombotic or anticoagulant use), clinical variables (stroke location in chronic health care facility versus other), ambulatory status before current event and at admission, arrival mode, on‐hours arrival, initial NIHSS, initial exam findings of weakness, level of consciousness and aphasia, treated with tissue plasminogen activator (in this hospital or at an outside hospital), stroke year and quarter, and hospital characteristics (rural location, region, Comprehensive/Primary Stroke Center status, teaching status, bed size, stroke volume, intravenous tissue plasminogen activator volume, EVT volume). Pre‐ and post‐2015 associations were analyzed by 2‐way interaction terms between race and ethnicity and time (ie, before 2015 versus after).
All statistical analyses were performed using SAS version 9.4 statistical software (SAS Institute Inc., Cary, North Carolina). All P values are 2‐sided, with P<0.05 considered statistically significant.
Results
Demographics
Of the 302 965 patients meeting inclusion criteria for potential EVT eligibility, 42 422 (14%) received EVT. Figure 1 (flow diagram) outlines patients who were excluded at different stages. The median age was 75 (interquartile range, 63–85) and 54.1% were women. Of the overall patient population, 69.8% were NHW, 16.0% non‐Hispanic Black, 7.1% Hispanic, 2.8% Asian, and 4.3% other or “unable to determine.” Of the patients who received EVT, 69.4% were NHW, 14.6% were non‐Hispanic Black, 6.8% were Hispanic, and 3.2% were Asian (Table 1). Other demographic and medical comorbidity variables are included in Table S1.
Table 1.
Patient Demographics in Stroke Patients Eligible for EVT
| Variable | Overall | EVT | No EVT | P value |
|---|---|---|---|---|
| Patient demographics | N=302 965 | n=42 422 | n=260 543 | |
| Age,y) | 75 (63–85) | 72 (61–81) | 76 (63–85) | <0.0001 |
| Women | 163 951 (54.1) | 21 634 (51.0) | 142 317 (54.6) | <0.0001 |
| Race or ethnicity | <0.0001 | |||
| White | 211 349 (69.8) | 29 429 (69.4) | 181 920 (69.8) | |
| Black | 48 532 (16.0) | 6214 (14.6) | 42 318 (16.2) | |
| Hispanic (any race) | 21 503 (7.1) | 2887 (6.8) | 18 616 (7.1) | |
| Asian | 8631 (2.8) | 1342 (3.2) | 7289 (2.8) |
EVT indicates endovascular therapy.
Temporal Trend in EVT According to Race and Ethnicity
EVT use among patients who are eligible (ie, those presenting within 6 hours and with an NIHSS ≥6) has steadily increased since publication of the positive thrombectomy trials in 2015 with no plateau reached yet. This holds true across all racial and ethnic groups. Figure 2. However, when adjusted odds ratios (OR) were calculated, Black patients had a lower odds of EVT use as compared with NHW ones. Notably, the OR for the comparison of the 2 groups after 2015 was closer to 1 (OR before=0.68, OR after=0.83, interaction‐P=0.0187), indicating a significant reduction in the racial gap in EVT treatment rate between the 2 groups post‐2015. Patients in “Other” racial group were significantly more likely to receive EVT compared with NHW patients after 2015 (OR, 1.25; P<0.0001). Please refer to Table 2. Of note, analysis adjusting for sex and race and ethnicity only is outlined in Table S2 and baseline characteristics by race and ethnicity in Table S3.
Figure 2. Endovascular therapy use stratified by race and ethnicity.
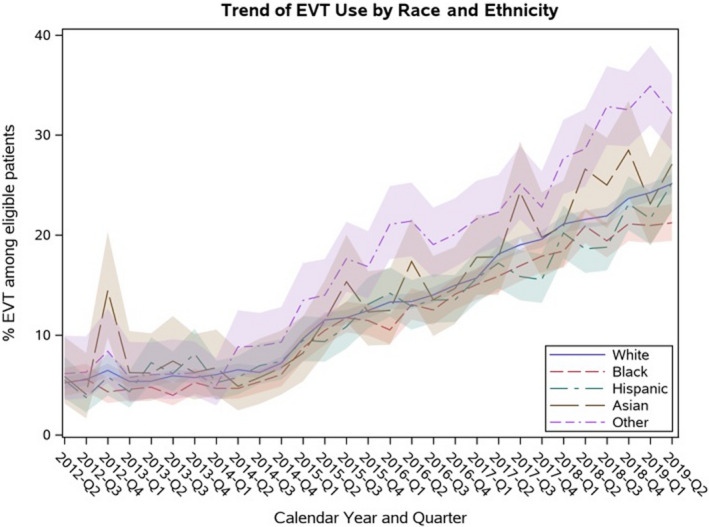
“Other” refers to people including but not limited to Alaskan, Native American, Native Hawaiian, and Pacific Islanders. EVT indicates endovascular therapy.
Table 2.
Adjusted Associations of Race and Ethnicity With EVT Use Before and After 2015 (n=302 965)
| Before 2015 | During/After 2015 | P value for interaction | |||
|---|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | ||
| Race or ethnicity | |||||
| Black | 0.68 (0.58‒0.78) | <0.0001 | 0.83 (0.76‒0.90) | <0.0001 | 0.0187 |
| Hispanic | 1.06 (0.79‒1.43) | 0.6957 | 1.01 (0.89‒1.13) | 0.9273 | |
| Asian | 1.04 (0.80‒1.33) | 0.7835 | 0.96 (0.83‒1.11) | 0.5517 | |
| Other* | 0.99 (0.78‒1.24) | 0.9025 | 1.25 (1.15‒1.36) | <0.0001 | |
| White | Reference | Reference | |||
“After 2015” includes the year of 2015. EVT indicates endovascular therapy; and OR, odds ratio.
“Other” refers to people including but not limited to Alaskan, Native American, Native Hawaiian, and Pacific Islanders.
Temporal Trend (pre‐ and post‐2015) in Outcomes According to Race and Ethnicity
There was an overall improvement in the proportion of patients discharged home, independent ambulation at discharge, and having good functional outcome at discharge (mRS 0–2) and at 90‐day mRS when comparing the era before and post‐2015. Please refer to Table 3. Yet there were differences across the racial and ethnic groups as outlined below.
Table 3.
Outcomes Before and After 2015, Overall and By Race and Ethnicity
| Variable | Overall | Before 2015 | After 2015 | P value |
|---|---|---|---|---|
| N=42 422 | n=5422 | n=37 000 | ||
| Overall | ||||
| Discharged home | 10 813 (25.5) | 1254 (23.1) | 9559 (25.8) | <0.0001 |
| Independent ambulation at discharge (discharged alive only) | 12 365 (36.0) | 1326 (31.7) | 11 039 (36.6) | <0.0001 |
| Race or ethnicity: White | ||||
| Discharged home | 7073 (24.0) | 845 (21.4) | 6228 (24.4) | <0.0001 |
| Independent ambulation at discharge (discharged alive only) | 8406 (35.3) | 932 (30.6) | 7474 (36.0) | <0.0001 |
| Race or ethnicity: Black | ||||
| Discharged home | 1806 (29.1) | 180 (26.3) | 1626 (29.4) | 0.089 |
| Independent ambulation at discharge (discharged alive only) | 2034 (38.9) | 201 (35.3) | 1833 (39.3) | 0.07 |
| Race or ethnicity: Hispanic (any race) | ||||
| Discharged home | 857 (29.7) | 112 (29.1) | 745 (29.8) | 0.78 |
| Independent ambulation at discharge (discharged alive only) | 782 (34.5) | 90 (30.9) | 692 (35.0) | 0.17 |
| Race or ethnicity: Asian | ||||
| Discharged home | 378 (28.2) | 48 (29.4) | 330 (28.0) | 0.70 |
| Independent ambulation at discharge (discharged alive only) | 381 (36.0) | 38 (32.8) | 343 (36.5) | 0.43 |
NHW Patients
Among NHW patients, comparing the era prior 2015 to the era post, there was an improvement in discharge home (21.4% – 24.4%, P<0.0001), independent ambulation at discharge (30.6% – 36%, P<0.0001), mRS at discharge (0‐–2) (17.9% – 21.8%, P<0.0001) and 90‐day mRS 0 to 2 (29.0% – 38.3%, P=0.0017). When comparing other race and ethnicity groups to the outcomes for NHW patients, the latter did worse for discharge home (OR >1), in‐hospital mortality/discharge to hospice (OR <1), but non‐Hispanic Black and Asian patients had lower mRS 0 to 2 at 90 days compared with NHW (OR <1). Please refer to Table 4. In addition, mRS at discharge and independent ambulation at discharge was not different comparing the different racial and ethnic groups.
Table 4.
Association of Race and Ethnicity With Outcomes
| Variable | Sex and race adjusted | Fully adjusted | ||
|---|---|---|---|---|
| OR (95% CI) | P value | OR (95% CI) | P value | |
| Discharged home (n=42 422) | ||||
| Women vs Men | 0.81 (0.77‒0.84) | <0.0001 | 1.04 (0.99‒1.09) | 0.11 |
| Black vs White | 1.29 (1.19‒1.41) | <0.0001 | 1.08 (1.00‒1.18) | 0.05 |
| Hispanic vs White | 1.33 (1.21‒1.46) | <0.0001 | 1.28 (1.16‒1.42) | <0.0001 |
| Asian vs White | 1.24 (1.08‒1.43) | 0.002 | 1.23 (1.05‒1.44) | 0.01 |
| Other* vs White | 1.19 (1.08‒1.32) | 0.0005 | 1.15 (1.03‒1.28) | 0.01 |
| Ambulate independently at discharge (n=34 375) | ||||
| Women vs Men | 0.77 (0.74‒0.80) | <0.0001 | 0.94 (0.90‒0.99) | 0.01 |
| Black vs White | 1.16 (1.07‒1.27) | 0.0006 | 1.03 (0.94‒1.13) | 0.47 |
| Hispanic vs White | 0.96 (0.85‒1.08) | 0.46 | 0.92 (0.81‒1.05) | 0.22 |
| Asian vs White | 1.04 (0.87‒1.24) | 0.69 | 1.00 (0.83‒1.21) | 0.99 |
| Other* vs White | 1.13 (1.02‒1.25) | 0.02 | 1.05 (0.94‒1.17) | 0.41 |
| In‐hospital‐mortality/discharged to hospice (n=42 422) | ||||
| Women vs Men | 1.17 (1.12‒1.22) | <0.0001 | 0.94 (0.89‒0.99) | 0.02 |
| Black vs White | 0.57 (0.52‒0.62) | <0.0001 | 0.61 (0.55‒0.67) | <0.0001 |
| Hispanic vs White | 0.85 (0.75‒0.95) | 0.0055 | 0.77 (0.68‒0.87) | <0.0001 |
| Asian vs White | 0.85 (0.75‒0.97) | 0.01 | 0.78 (0.68‒0.90) | 0.0006 |
| Other* vs White | 1.02 (0.91‒1.14) | 0.78 | 1.06 (0.94‒1.20) | 0.35 |
| mRS at discharge (0–2) (n=31 443) | ||||
| Women vs Men | 0.78 (0.74‒0.82) | <0.0001 | 0.96 (0.90‒1.01) | 0.10 |
| Black vs White | 1.24 (1.10‒1.39) | 0.0003 | 1.02 (0.90‒1.14) | 0.80 |
| Hispanic vs White | 0.91 (0.80‒1.03) | 0.15 | 0.89 (0.76‒1.03) | 0.12 |
| Asian vs White | 1.07 (0.90‒1.29) | 0.43 | 1.16 (0.95‒1.42) | 0.15 |
| Other* vs White | 1.13 (0.99‒1.28) | 0.07 | 1.10 (0.97‒1.26) | 0.13 |
| 90‐d mRS post‐discharge (0–2) (n=16 068) | ||||
| Women vs Men | 0.75 (0.71‒0.80) | <0.0001 | 0.92 (0.87‒0.99) | 0.02 |
| Black vs White | 0.97 (0.87‒1.09) | 0.65 | 0.84 (0.75‒0.95) | 0.006 |
| Hispanic vs White | 0.94 (0.81‒1.08) | 0.38 | 0.94 (0.81‒1.10) | 0.43 |
| Asian vs White | 0.81 (0.67‒0.98) | 0.03 | 0.79 (0.65‒0.98) | 0.03 |
| Other* vs White | 0.92 (0.80‒1.05) | 0.22 | 0.90 (0.77‒1.05) | 0.18 |
OR indicates odds ratio.
“Other” refers to people including but not limited to Alaskan, Native American, Native Hawaiian and Pacific Islanders.
Non‐Hispanic Black Patients
Comparing pre‐ and post‐2015 there was a trend towards higher discharge home (26.3% – 29.4%, P=0.089) and higher independent ambulation at discharge (35.3% – 39.3%, P=0.065). There was also a statistically significant improvement in the mRS 0 to 2 at discharge over time (21.3% – 25.5%, P=0.0437) and median mRS at 90 days improved from 4 to 3 (P=0.0455). After adjustment, short‐term outcomes were slightly better in non‐Hispanic Black patients compared with NHW ones (adjusted odds ratio [aOR] for discharge home 1.08, [1.00‒1.18]; aOR for in‐hospital mortality/discharge to hospice was 0.61 [0.55‒0.67]); but the rate of good functional outcome, ie, mRS 0 to 2 at 90 days was worse in non‐Hispanic Black patients (aOR 0.84 (0.75 – 0.95)). Please refer to Table 4. Baseline characteristics for missing rates and imputation details are outlined in Table S4.
Symptomatic intracranial hemorrhage was lower in non‐Hispanic Black patients compared with NHW ones (OR, 0.86; P = 0.038) after 2015 but not in the overall adjusted analysis.
Hispanic Patients
There was no significant change in discharge and short‐term outcomes comparing pre‐ and post‐2015 however there was an improvement in 90‐day mRS from median of 6 to 3 (P=0.001) and a trend towards improvement in the 90‐day good functional outcomes (mRS 0–2). Like other under‐represented racial and ethnic groups, Hispanic patients had some better short‐term outcomes compared with NHW ones such as higher discharge home (OR, 1.28; 1.16‒1.42) and lower in‐hospital mortality/discharge to hospice (OR, 0.77; 0.68‒0.87). However independent ambulation at discharge, mRS at discharge, and 90‐day mRS was no different compared with NHW patients. Please refer to Table 4.
Asian Patients
No significant changes pre‐ and post‐2015 era were observed. When compared with NHW patients, Asian patients had slightly better short‐term outcomes (OR of 1.23 for being discharged home [CI, 1.05‒1.44], OR of 0.78 for discharge to hospice and in‐patient mortality [CI, 0.68‒0.90]). Good functional outcomes were worse however compared with NHW patients; OR for mRS 0 to 2 at 90 days was 0.79 (0.65‒0.98). Please refer to Table 4.
Discussion
In this large cohort of “real world” patients eligible for EVT from the GWTG registry, we demonstrate that despite overall increase in EVT use across all racial and ethnic groups and narrowing of the disparity gap especially in the era post‐2015, there continues to be significant racial and ethnic differences in the use of this therapy. Non‐Hispanic Black patients had a significantly lower likelihood of receiving EVT compared with NHW ones. In addition, although some short‐term outcomes were better in under‐represented racial and ethnic groups, they did worse compared with NHW patients in regards to long‐term outcomes.
Various factors have been proposed for disparities in EVT use including a lack of awareness of stroke signs and symptoms, 18 lack of knowledge on need for urgent care among under‐represented racial and ethnic groups with delays in arriving to emergency rooms, lower socioeconomic status, and lack of insurance coverage. The higher incidence of intracranial atherosclerosis among Black, Asian, and Hispanic individuals compared with NHW ones needs to be considered in the lower rates of EVT in these populations despite comparable arrival times. 19 Conversely, the concept of allostatic load burden as a contributor to higher incidence of chronic disease and worse outcomes among under‐represented racial and ethnic groups should not be ignored by the medical community. 20 There is also mistrust of the health care system likely because of historic inequalities and injustices exacerbated by fewer health care providers from under‐represented race and ethnic groups. 21 The presence of bias, whether on a provider or system‐wide level in the health care delivery system is the most difficult to evaluate for and systemic racism has become an increasingly identified problem of public health significance in more recent years 22 , 23 ; this is also reflected in unequal participation in clinical trials including stroke research of under‐represented race and ethnic groups. 2
Importantly, our study demonstrated that these inter‐racial differences have narrowed over time comparing the era pre‐ and post‐publication (in 2015). This improvement may in part reflect the effects of prior multiethnic educational campaigns (particularly from a young age) 24 , 25 and improved awareness among the society including health care providers post publication of positive stroke trials. It is important to note that despite an overall sharp increase in use of EVT after January 2015 as demonstrated in a large GWTG study, there is also a persistent geographic variation. 15
Multiple previous observational studies have documented the presence of disparities in stroke incidence, care, and outcomes according to racial and ethnic groups beginning with the NOMAS (Northern Manhattan Study). 1 , 19 A study of a large cohort of patients admitted to GWTG hospitals between 2003 and 2008 documented a differential quality of care post‐acute ischemic stroke among Black patients compared with Hispanic and NHW patients in regards to implementation of evidence‐based treatments. 5 There are few studies looking at EVT and differences according to race andethnicity. 7 , 8 , 26 In a large nationwide database for admissions for acute ischemic stroke to endovascular centers, the overall use of EVT was reported to be 8.4% which is lower than the 14% documented in our cohort. They did find lower use of EVT in Black and Hispanic patients. Another GWTG study also demonstrated a higher rate of transfer of NHW patients compared with under‐represented racial and ethnic groups to EVT capable centers. 27
In our cohort, under‐represented racial and ethnic groups compared with NHW had certain better short‐term outcomes including a lower in‐hospital mortality/discharge to hospice and higher discharge to home however with no significant difference in good functional outcomes (mRS 0–2) and independent ambulation at discharge. These results corroborate similar findings in recent studies showing lower in‐hospital mortality and higher discharge to home among Black and Hispanic patients and are in contrast with earlier studies which demonstrated higher in‐hospital mortality among under‐represented racial and ethnic groups. 5 , 28 , 29 , 30 , 31 The differences in end of life decisions may be, in part, explained by different attitudes towards end of life care among NHW patients compared with under‐represented racial and ethnic groups, with the former more likely to opt for Do Not Resuscitate status, withdrawal of care, and hospice. 32 , 33 Availability of palliative care services also tends to be better in hospitals serving NHW majorities. 34 Notably, our study did demonstrate a lower likelihood of symptomatic intracranial hemorrhage in Black patients which was statistically significant after 2015 compared with NHW but did not achieve significance in the overall adjusted analysis.
Our 3‐month analysis however revealed lower rates of good functional outcomes (mRS 0–2) in under‐represented racial and ethnic groups compared with NHW patients. Of note, loss to follow‐up at 90 days was slightly higher among Asian patients (27.3%) compared with NHW patients (25.4%) however this was not statistically significant (P=0.44 across all racial and ethnic groups, P=0.19 comparing NHW and Asian patients). There is evidence from a Veterans Affairs study that post‐hospital environment differences negatively affect recovery from stroke for poor Black patients compared with poor NHW patients and patients of higher incomes. 35 Another study in the general population revealed higher rates of rehabilitation admission and discharge functional status ratings among NHW patients compared with under‐represented racial and ethnic groups. 36 This may provide an explanation for the discordant discharge compared with 90‐day outcome findings from our study and raise the possibility that discharge to home is a multifaceted outcome variable which may not always be representative of functional status at discharge since there are socioeconomic and cultural factors that may influence willingness of patients and their families to continue rehabilitation at home versus in an institution.
Outcomes by race andethnicity were similar in models adjusted for age and sex only (Table 4), with the exception that the association of Black race with better discharge outcomes after age and sex adjustment was attenuated after additionally adjusting for stroke severity, clinical variables, risk factors, and hospital characteristics (Table 4). This may reflect race‐related differences in mechanism of the preventing stroke, as Black patients were less likely to have atrial fibrillation and more likely to have hypertension and diabetes (Table S2). Black race was not associated with odds of good outcome at 90 days in analyses adjusted for age and sex only, but after additionally adjusting for stroke severity, risk factors, and hospital characteristics it was associated with lower odds of good outcome (defined as mRS 0–2). This suggests that there are disparities in longer term stroke recovery in Black patients compared with NHW patients that cannot be explained by their medical history or features of their acute stroke.
Despite seeming gains in EVT use among all racial and ethnic groups, the ongoing COVID‐19 pandemic is threatening to undo these gains with alarming declines in EVT performed among Black patients. 37 The pandemic along with the changing sociopolitical climate has resulted in systemic racism once again coming under scrutiny as evidenced by the recently published American Heart Association/American Stroke Association presidential advisory. 23 Thus, recognizing disparities in stroke care and designing effective and sustainable interventions has become a priority.
There are a number of limitations to this study. First, certain racial and ethnic groups were not individually reported such as people of Native American, Alaskan, and other under‐represented race and ethnic heritage groups—these groups were classified as “other.” Second, participation in GWTG database is voluntary and the design of our study is observational. Third, EVT eligibility was determined clinically (NIHSS ≥6 and LSW<6 hours) and no CT angiography or angiographic confirmation was available. The incidence of LVO in patients presenting with NIHSS ≥6 presenting under 6 hours may differ according to race andethnicity as evidenced in a UK‐based study. 38 While the lack of angiographic confirmation is an important limitation, these findings have not been consistently replicated across other larger studies some of which have demonstrated all ischemic stroke subtypes are more prevalent in Black patients compared with NHW patients. 39 Fourth, the statistical approach of using all covariates without tests of significance in univariate testing may lead the study to underestimate the true size of the disparities as experienced from a patient perspective. Our study has significant strengths. First and foremost is the large sample size which provides sufficient number of patients for most ethnic under—represented racial and ethnic groups allowing meaningful associations and inferences. Of note, there was no significant racial difference in 90‐day mRS missingness across racial and ethnic groups; P=0.44. In addition, the overall representative cohort provides high quality granular data enabling a proper understanding of the “real world” situation in US hospitals in regard to EVT use and subsequent outcomes. 12
Conclusions
We demonstrated in this large GWTG cohort that despite overall improvement in EVT use across racial and ethnic groups post‐2015 likely corresponding to publication of groundbreaking trials and subsequent guidelines, differences still exist according to race andethnicity with Non‐ Hispanic Black patients having lower rates of EVT use than NHW patients. These differences have narrowed over time. Despite slightly better short‐term outcomes among under‐represented racial and ethnic groups including Black, Hispanic, and Asian compared with NHW patients, these improvements were not sustained at 3 months. Intensification of preexistingefforts to eradicate systemic racism and convert “observations (of racial and ethnic disparities) to actions” are necessary in uniformly increasing access to life‐saving therapies such as EVT and subsequent outcomes among all racial and ethnic groups. 23 , 40
GWTG‒Stroke Funding Statement
The Get With The Guidelines–Stroke program is provided by the American Heart Association/American Stroke Association. It is sponsored, in part, by Novartis, Boehringer Ingelheim and Eli Lilly Diabetes Alliance, Novo Nordisk, Sanofi, AstraZeneca, Bayer, and Portola Pharmaceuticals.
Disclosures
F.S., H.X., A.M., V.G., A.V., R.M., Y.X., M.R., E.S., G.R., and S.C. have no relevant disclosures.
Dr Saver is an employee of the University of California. The University of California has patent rights in retrieval devices for stroke. The University of California Regents received payments on the basis of clinical trial contracts for the number of subjects enrolled in multicenter clinical trials sponsored by Medtronic, Stryker, and Cerenovus, BrainsGate, and Boehringer Ingelheim (prevention only); Dr Saver served as an unpaid site investigator under these contracts. Dr Saver serves as an unpaid consultant to Genentech advising on the design and conduct of the PRISMS trial; neither the University of California nor Dr Saver received any payments for this voluntary service. Dr Saver paid for his own travel. Dr Saver has received contracted hourly payments and travel reimbursement for services as a scientific consultant advising on rigorous trial design and conduct to Medtronic, Stryker, Cerenovus, BrainsGate, Boehringer Ingelheim (prevention only), Diffusion Medical, BrainQ, and Abbott. Dr Saver has received contracted stock options for services as a scientific consultant advising on rigorous trial design and conduct to Rapid Medical.”
Dr Fonarow reports research funding from the Patient Centered Outcome Research Institute, being a member of the GWTG Steering Committee, and an employee of University of California which has a patent on an endovascular device.
Dr Schwamm serves as a scientific consultant on trial design and conduct to Genentech (late window thrombolysis) and Member of steering committee (TIMELESS NCT03785678); consultant on user interface design and usability to LifeImage; stroke systems of care consultant to the Massachusetts Department of Public Health; member of a Data Safety Monitoring Boards (DSMB) for Penumbra (MIND NCT03342664) and for Diffusion Pharma (PHAST‐TSC NCT03763929); Serving as National PI for Medtronic (Stroke AF NCT02700945); Site PI, StrokeNet Network NINDS (New England Regional Coordinating Center U24NS107243).
Supporting information
Table S1–S3
For Disclosures, see page 9.
References
- 1. Northern Manhattan Stroke Study C , Sacco RL, Boden‐Albala B, Gan R, Chen X, Kargman DE, Shea S, Paik MC, Hauser WA, et al. Stroke incidence among white, black, and Hispanic residents of an urban community: the Northern Manhattan Stroke study. Am J Epidemiol. 1998;147:259–268. doi: 10.1093/oxfordjournals.aje.a009445 [DOI] [PubMed] [Google Scholar]
- 2. Cruz‐Flores S, Rabinstein A, Biller J, Elkind MSV, Griffith P, Gorelick PB, Howard G, Leira EC, Morgenstern LB, Ovbiagele B, et al. Racial‐ethnic disparities in stroke care: the American experience. Stroke. 2011;42:2091–2116. doi: 10.1161/STR.0b013e3182213e24 [DOI] [PubMed] [Google Scholar]
- 3. Fang MC, Cutler DM, Rosen AB. Trends in thrombolytic use for ischemic stroke in the United States. J Hosp Med. 2010;5:406–409. doi: 10.1002/jhm.689 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Nasr DM, Brinjikji W, Cloft HJ, Rabinstein AA. Racial and ethnic disparities in the use of intravenous recombinant tissue plasminogen activator and outcomes for acute ischemic stroke. J Stroke Cerebrovasc Dis. 2013;22:154–160. doi: 10.1016/j.jstrokecerebrovasdis.2011.07.003 [DOI] [PubMed] [Google Scholar]
- 5. Schwamm LH, Reeves MJ, Pan W, Smith EE, Frankel MR, Olson DW, Zhao X, Peterson E, Fonarow GC, et al. Race/ethnicity, quality of care, and outcomes in ischemic stroke. Circulation. 2010;121:1492–1501. doi: 10.1161/CIRCULATIONAHA.109.881490 [DOI] [PubMed] [Google Scholar]
- 6. Reddy S, Wu T‐C, Zhang J, Rahbar MH, Ankrom C, Zha A, Cossey TC, Aertker B, Vahidy F, Parsha K, et al. Lack of racial, ethnic, and sex disparities in ischemic stroke care metrics within a tele‐stroke network. J Stroke Cerebrovasc Dis. 2021;30:105418. doi: 10.1016/j.jstrokecerebrovasdis.2020.105418 [DOI] [PubMed] [Google Scholar]
- 7. Attenello FJ, Adamczyk P, Wen GE, He S, Zhang K, Russin JJ, Sanossian N, Amar AP, Mack WJ, et al. Racial and socioeconomic disparities in access to mechanical revascularization procedures for acute ischemic stroke. J Stroke Cerebrovasc Dis. 2014;23:327–334. doi: 10.1016/j.jstrokecerebrovasdis.2013.03.036 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Menon BK, Saver JL, Goyal M, Nogueira R, Prabhakaran S, Liang LI, Xian Y, Hernandez AF, Fonarow GC, Schwamm L, et al. Trends in endovascular therapy and clinical outcomes within the nationwide get with the Guidelines‐Stroke Registry. Stroke. 2015;46:989–995. doi: 10.1161/STROKEAHA.114.007542 [DOI] [PubMed] [Google Scholar]
- 9. https://heart.irp.iqvia.com/portalPage.html. In.
- 10. Fonarow Gregg C, Reeves Mathew J, Smith Eric E, Saver Jeffrey L, Zhao X, Olson Dai W, et al. Characteristics, performance measures, and in‐hospital outcomes of the first one million stroke and transient ischemic attack admissions in Get With The Guidelines‐Stroke. Circ Cardiovasc Qual Outcomes. 2010;3:291–302. doi: 10.1161/CIRCOUTCOMES.109.921858 [DOI] [PubMed] [Google Scholar]
- 11. Schwamm LH, Fonarow GC, Reeves MJ, Pan W, Frankel MR, Smith EE, Ellrodt G, Cannon CP, Liang LI, Peterson E, et al. Get With the Guidelines‐Stroke is associated with sustained improvement in care for patients hospitalized with acute stroke or transient ischemic attack. Circulation. 2009;119:107–115. doi: 10.1161/CIRCULATIONAHA.108.783688 [DOI] [PubMed] [Google Scholar]
- 12. Reeves MJ, Fonarow GC, Smith EE, Pan W, Olson DaiWai, Hernandez AF, Peterson ED, Schwamm LH, et al. Representativeness of the Get With The Guidelines‐Stroke Registry. Stroke. 2012;43:44–49. doi: 10.1161/STROKEAHA.111.626978 [DOI] [PubMed] [Google Scholar]
- 13. Ziaeian B, Xu H, Matsouaka RA, Xian Y, Khan Y, Schwamm LS, Smith EE, Fonarow GC, et al. National surveillance of stroke quality of care and outcomes by applying post‐stratification survey weights on the Get With The Guidelines‐Stroke patient registry. BMC Med Res Methodol. 2021;21:23. doi: 10.1186/s12874-021-01214-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. https://grants.nih.gov/grants/guide/notice‐files/not‐od‐15‐089.html. In.
- 15. Smith EE, Saver JL, Cox M, Liang LI, Matsouaka R, Xian Y, Bhatt DL, Fonarow GC, Schwamm LH, et al. Increase in endovascular therapy in get with the guidelines‐stroke after the publication of pivotal trials. Circulation. 2017;136:2303–2310. doi: 10.1161/CIRCULATIONAHA.117.031097 [DOI] [PubMed] [Google Scholar]
- 16. Jahan R, Saver JL, Schwamm LH, Fonarow GC, Liang LI, Matsouaka RA, Xian Y, Holmes DN, Peterson ED, Yavagal D, et al. Association between time to treatment with endovascular reperfusion therapy and outcomes in patients with acute ischemic stroke treated in clinical practice. JAMA. 2019;322:252–263. doi: 10.1001/jama.2019.8286 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Menon BK, Xu H, Cox M, Saver JL, Goyal M, Peterson E, Xian Y, Matsuoka R, Jehan R, Yavagal D, et al. Components and trends in door to treatment times for endovascular therapy in get with the guidelines‐stroke hospitals. Circulation. 2019;139:169–179. doi: 10.1161/CIRCULATIONAHA.118.036701 [DOI] [PubMed] [Google Scholar]
- 18. Willey JZ, Williams O, Boden‐Albala B. Stroke literacy in Central Harlem: a high‐risk stroke population. Neurology. 2009;73:1950–1956. doi: 10.1212/WNL.0b013e3181c51a7d [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Sacco RL, Kargman DE, Gu Q, Zamanillo MC. Race‐ethnicity and determinants of intracranial atherosclerotic cerebral infarction: the Northern Manhattan Stroke Study. Stroke. 1995;26:14–20. doi: 10.1161/01.STR.26.1.14 [DOI] [PubMed] [Google Scholar]
- 20. Duru OK, Harawa NT, Kermah D, Norris KC. Allostatic load burden and racial disparities in mortality. J Natl Med Assoc. 2012;104:89–95. doi: 10.1016/S0027-9684(15)30120-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Armstrong K, Ravenell KL, McMurphy S, Putt M. Racial/ethnic differences in physician distrust in the United States. Am J Public Health. 2007;97:1283–1289. doi: 10.2105/AJPH.2005.080762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Bailey ZD, Feldman JM, Bassett MT. How structural racism works — racist policies as a root cause of U.S. racial health inequities. N Engl J Med. 2021;384:768–773. doi: 10.1056/NEJMms2025396 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Churchwell K, Elkind MSV, Benjamin RM, Carson AP, Chang EK, Lawrence W, Mills A, Odom TM, Rodriguez CJ, Rodriguez F, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020;142(24). doi: 10.1161/CIR.0000000000000936 [DOI] [PubMed] [Google Scholar]
- 24. Mullen Conley K, Juhl Majersik J, Gonzales NR, Maddox KE, Pary JK, Brown DL, Moyé LA, Espinosa N, Grotta JC, Morgenstern LB, et al. Kids Identifying and Defeating Stroke (KIDS): development and implementation of a multiethnic health education intervention to increase stroke awareness among middle school students and their parents. Health Promot Pract. 2010;11:95–103. doi: 10.1177/1524839907309867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Morgenstern LB, Gonzales NR, Maddox KE, Brown DL, Karim AP, Espinosa N, Moyé LA, Pary JK, Grotta JC, Lisabeth LD, et al. A randomized, controlled trial to teach middle school children to recognize stroke and call 911. Stroke. 2007;38:2972–2978. doi: 10.1161/STROKEAHA.107.490078 [DOI] [PubMed] [Google Scholar]
- 26. Rinaldo L, Rabinstein Alejandro A, Cloft H, Knudsen John M, Castilla Leonardo R, Brinjikji W. Racial and ethnic disparities in the utilization of thrombectomy for acute stroke. Stroke. 2019;50:2428–2432. doi: 10.1161/STROKEAHA.118.024651 [DOI] [PubMed] [Google Scholar]
- 27. Shah S, Xian Y, Sheng S, Zachrison KS, Saver JL, Sheth KN, Fonarow GC, Schwamm LH, Smith EE, et al. Use, temporal trends, and outcomes of endovascular therapy after interhospital transfer in the United States. Circulation. 2019;139:1568–1577. doi: 10.1161/CIRCULATIONAHA.118.036509 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Wolfe CDA, Smeeton NC, Coshall C, Tilling K, Rudd AG. Survival differences after stroke in a multiethnic population: follow‐up study with the south London stroke register. BMJ. 2005;331:431. doi: 10.1136/bmj.38510.458218.8F [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Gilesa WH, Crofta JB, Caspera ML, Millerb JK. Stroke incidence, comorbid conditions, health care utilization, and poststroke mortality in black and white medicare beneficiaries. Stroke in Blacks: A Guide to Management and Prevention. 1999:106. [Google Scholar]
- 30. Ayala C, Greenlund KJ, Croft JB, Keenan NL, Donehoo RS, Giles WH, et al. Racial/ethnic disparities in mortality by stroke subtype in the United States, 1995–1998. Am J Epidemiol. 2001;154:1057–1063. doi: 10.1093/aje/154.11.1057 [DOI] [PubMed] [Google Scholar]
- 31. Stansbury JP, Jia H, Williams LS, Vogel WB, Duncan PW. Ethnic disparities in stroke: epidemiology, acute care, and postacute outcomes. Stroke. 2005;36:374–386. doi: 10.1161/01.STR.0000153065.39325.fd [DOI] [PubMed] [Google Scholar]
- 32. Mayer SA, Kossoff SB. Withdrawal of life support in the neurological intensive care unit. Neurology. 1999;52(8):1602. doi: 10.1212/WNL.52.8.1602 [DOI] [PubMed] [Google Scholar]
- 33. Johnson RW, Newby LK, Granger CB, Cook WA, Peterson ED, Echols M, Bride W, Granger BB, et al. Differences in level of care at the end of life according to race. Am J Crit Care. 2010;19:335–343. doi: 10.4037/ajcc2010161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Faigle R, Ziai WC, Urrutia VC, Cooper LA, Gottesman RF. Racial Differences in palliative care use after stroke in majority‐white, minority‐serving, and racially integrated U.S. Hospitals. Crit Care Med. 2017;45:2046–2054. doi: 10.1097/CCM.0000000000002762 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Horner Ronnie D, Swanson Jeffrey W, Bosworth Hayden B, Matchar DB. Effects of race and poverty on the process and outcome of inpatient rehabilitation services among stroke patients. Stroke. 2003;34:1027–1031. doi: 10.1161/01.STR.0000060028.60365.5D [DOI] [PubMed] [Google Scholar]
- 36. Ottenbacher KJ, Campbell J, Kuo Y‐F, Deutsch A, Ostir GV, Granger CV. Racial and ethnic differences in postacute rehabilitation outcomes after stroke in the United States. Stroke. 2008;39:1514–1519. doi: 10.1161/STROKEAHA.107.501254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Al Kasab S, Almallouhi E, Alawieh A, Jabbour P, Sweid A, Starke RM, Saini V, Wolfe SQ, Fargen KM, Arthur AS, et al. Alarming downtrend in mechanical thrombectomy rates in African American patients during the COVID‐19 pandemic‐Insights from STAR. J NeuroIntervent Surg. 2021;13:304–307. doi: 10.1136/neurintsurg-2020-016946 [DOI] [PubMed] [Google Scholar]
- 38. Gulli G, Rutten‐Jacobs LCA, Kalra L, Rudd AG, Wolfe CDA, Markus HS. Differences in the distribution of stroke subtypes in a UK black stroke population—final results from the South London Ethnicity and Stroke Study. BMC Med. 2016;14:77. doi: 10.1186/s12916-016-0618-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. White H, Boden‐Albala B, Wang C, Elkind MSV, Rundek T, Wright CB, Sacco RL, et al. Ischemic stroke subtype incidence among whites, blacks, and Hispanics. Circulation. 2005;111:1327–1331. doi: 10.1161/01.CIR.0000157736.19739.D0 [DOI] [PubMed] [Google Scholar]
- 40. Sacco RL. Stroke disparities: from observations to actions. Stroke. 2020;51:3392–3405. doi: 10.1161/STROKEAHA.120.030428 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table S1–S3


