Abstract
Background
Despite advances in resuscitation medicine, the burden of in‐hospital cardiac arrest (IHCA) remains substantial. The impact of these advances and changes in resuscitation guidelines on IHCA survival remains poorly defined. To better characterize evolving patient characteristics and temporal trends in the nature and outcomes of IHCA, we undertook a 20‐year analysis of a national database.
Methods and Results
We analyzed the National Inpatient Sample (1999–2018) using International Classification of Diseases, Ninth Revision and Tenth Revision, Clinical Modification (ICD‐9‐CM and ICD‐10‐CM) codes to identify all adult patients suffering IHCA. Subgroup analysis was performed based on the type of cardiac arrest (ie, ventricular tachycardia/ventricular fibrillation or pulseless electrical activity‐asystole). An age‐ and sex‐adjusted model and a multivariable risk‐adjusted model were used to adjust for potential confounders. Over the 20‐year study period, a steady increase in rates of IHCA was observed, predominantly driven by pulseless electrical activity‐asystole arrest. Overall, survival rates increased by over 10% after adjusting for risk factors. In recent years (2014–2018), a similar trend toward improved survival is noted, though this only achieved statistical significance in the pulseless electrical activity‐asystole cohort.
Conclusions
Though the ideal quality metric in IHCA is meaningful neurological recovery, survival is the first step toward this. As overall IHCA rates rise, overall survival rates are improving in tandem. However, in more recent years, these improvements have plateaued, especially in the realm of ventricular tachycardia/ventricular fibrillation‐related survival. Future work is needed to better identify characteristics of IHCA nonsurvivors to improve resource allocation and health care policy in this area.
Keywords: cardiac arrest, populational studies, resuscitation, survival, trends
Subject Categories: Cardiopulmonary Arrest, Quality and Outcomes, Cardiopulmonary Resuscitation and Emergency Cardiac Care
The annual incidence of in‐hospital cardiac arrest (IHCA) is estimated to be approximately 300 000 in the United States. 1 This ranges from 1.6 to 2.85 per 1000 hospital admissions based on data from the United Kingdom and United States, respectively. 2 , 3 Shockable rhythms (pulseless ventricular tachycardia/ventricular fibrillation [VT/VF]) account for 15.3% of these events, with the remaining composed of pulseless electrical activity (PEA)‐asystole arrest.
The past decade has witnessed significant improvements in rates of survival, which range from 18.4% to 25.6% in the United Kingdom and the United States registry, respectively. 4 However, population‐level data from recent years with regard to these trends remain limited. The American Heart Association resuscitation guidelines have witnessed many modifications over the past 2 decades along with substantial improvements in emergency and intensive‐care therapeutics such as early and standardized chest compression techniques, prompt use of capnography, mechanical ventilation, and target temperature management, as well as early revascularization when indicated. 5 However, the temporal impact of these interventions on IHCA survival remains poorly defined.
In an attempt to better understand the evolving patient characteristics as well as temporal trends in the nature and outcomes of IHCA, we undertook a long‐term, 20‐year analysis of a US national database. This population‐level analysis could provide insight into the implications of changes in clinical practice and guide future health policy.
Methods
The current trend analysis was conducted using the National Inpatient Sample (NIS) from 1999 to 2018. The NIS is the largest publicly available in‐hospital database in the United States, with data covering over 30 million hospitalizations. 6 Local institutional review board approval was waived in lieu of the deidentified nature of the data. The data that support the findings of this study are available from the corresponding author upon reasonable request.
International Classification of Diseases, Ninth and Tenth Revision, Clinical Modification (ICD‐9‐CM and ICD‐10‐CM) codes (Table S1) were used to identify all adult patients suffering an IHCA (9960, 9963; 5A12012). 3 , 7 , 8 Out‐of‐hospital cardiac arrests (4275; I46) were excluded before analysis. 8 This coding approach has yielded an 83.3% positive predictive value in the identification of IHCA based on prior studies. 9 VT/VF were identified using secondary diagnosis codes (427.4x, I472, I490), and the remainder of cases without these codes were considered to have PEA‐asystole cardiac arrest. 7 , 8 A General Equivalence Mapping tool published by the Centers for Medicare and Medicaid Services was used to assist the conversion of ICD‐9‐CM to ICD‐10‐CM codes. Demographics, including age, sex, race, income, insurance, and Charlson Combiditiy Index scores (Table S2), as well as hospital characteristics, were analyzed in four 5‐year groups to assess the temporal trends in event rates as well as outcomes. We used discharge trend weights files provided by the Agency for Healthcare Research and Quality to account for changes in the NIS over time. 6 A further separate trend analysis was performed from years 2014 to 2018 to better reflect recent trends and the impact of changes in societal guidelines. 5 The methodological standard of the Healthcare Cost and Utilization Project were adhered to throughout the analysis. 10
Statistical Analysis
The Wilcoxon rank sum test was used to evaluate temporal trends for categorical variables and linear regression for continuous variables. To better assess changes in survival characteristics over time, we further developed an age‐ and sex‐adjusted model as well as a multivariable risk‐adjusted model using generalized estimation equations for the overall cohort. 11 The multivariable risk‐adjusted model accounts for the age, sex, race, income, insurance, comorbidity burden, as well as hospital level variables including hospital bed size, geographical region, and teaching versus nonteaching status. Clustering effect was incorporated within the model using unique hospital identification numbers. Furthermore, the Zou method was used to directly estimate rate ratios instead of odds ratio by specifying a Poisson distribution and including a robust variance estimate. 11 Adjusted annual survival rates were calculated by multiplying each reference year with its respective adjusted rate ratio. All statistical analyses were conducted using Stata version 15.1 (StataCorp).
Results
Over a 20‐year study period from 1999 to 2018, a steady rise in IHCA as a proportion of all hospital admissions was observed (2.28–3.82 per 1000 hospitalization, P trend<0.001) (Figure [A]). This was predominantly composed of PEA‐asystole cardiac arrests, which accounted for 76.81% of IHCAs. A substantial 118% and 52% increase in VT/VF (from 0.50 to 1.09 per 1000 hospitalizations) and PEA‐asystole arrests (from 1.79 to 2.73 per 1000 hospitalizations), respectively, were observed during the study period.
Figure . Yearly trends of in‐hospital cardiac arrest (IHCA) incidence and survival from 1999 to 2018 in the United States.
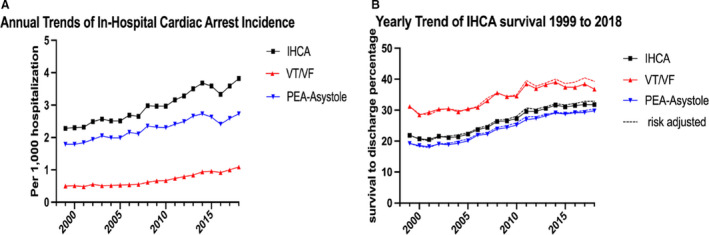
A, Annualized incidence of IHCA demonstrating a steady increase over 20 years in all cohorts of patients. B, Crude and risk‐adjusted annualized survival trends in IHCA patients demonstrating significant improvement in long‐term survival rates, primarily driven by improved PEA‐asystole survival. PEA indicates pulseless electrical activity; and VT/VF, ventricular tachycardia/ventricular fibrillation.
Trends in the characteristics of patients suffering cardiac arrests were analyzed on a 5‐year basis (Table 1). During this period, a significant decrease in mean age was observed (68.38 to 66.60 years, P trend<0.001), with a concomitant reduction in the proportion of White patients (68.7% to 62.1%, P trend<0.001). From a socioeconomic standpoint, a significant increase in patients in the lowest quartile of median income suffering IHCA was observed (12.6% to 34.3%, P trend<0.001), with relatively stable proportions of patients in different insurance groups over this period.
Table 1.
Characteristics of IHCA
| Variable | 5‐year trends | Overall P trend value | |||
|---|---|---|---|---|---|
| 1999–2003, n=354 013 | 2004–2008, n=412 553 | 2009–2013, n=491 336 | 2014–2018, n=537 460 | ||
| Patient characteristics | |||||
| Age, y, mean±SD | 68.38±0.17 | 67.38±0.18 | 66.61±0.11 | 66.03±0.59 | 0.001 |
| Age <65 y, % | 34.39 | 38.54 | 41.24 | 42.11 | 0.001 |
| Age 65–75 y, % | 23.51 | 21.98 | 22.99 | 25.51 | 0.001 |
| Age >75–85 y, % | 28.57 | 26.20 | 22.93 | 21.23 | 0.001 |
| Age >85 y, % | 13.52 | 13.28 | 12.84 | 11.15 | 0.001 |
| Women, % | 46.28 | 45.54 | 44.40 | 42.70 | 0.001 |
| Race and ethnicity, % | |||||
| White | 68.71 | 65.50 | 63.00 | 62.13 | 0.001 |
| Black | 17.63 | 18.83 | 20.92 | 21.27 | 0.798 |
| Hispanic | 8.36 | 9.50 | 9.59 | 9.81 | 0.9 |
| Other* | 5.31 | 6.16 | 6.50 | 6.79 | 0.961 |
| Charlson Comorbidity Index score, mean±SD | 2.08±0.01 | 2.33±0.01 | 2.82±0.01 | 3.25±0.01 | 0.001 |
| 0, % | 16.78 | 15.93 | 13.27 | 10.18 | 0.001 |
| 1, % | 27.27 | 23.67 | 18.82 | 15.95 | 0.001 |
| ≥2, % | 55.95 | 60.41 | 67.91 | 73.87 | 0.001 |
| Median income, % | |||||
| First quartile | 12.59 | 25.99 | 26.53 | 34.31 | 0.001 |
| Second quartile | 30.59 | 26.00 | 23.00 | 20.44 | 0.001 |
| Third quartile | 32.17 | 25.23 | 23.59 | 18.99 | 0.001 |
| Fourth quartile | 34.30 | 25.59 | 22.10 | 17.99 | 0.001 |
| Insurance details, % | |||||
| Medicaid, Medicare | 75.13 | 74.10 | 74.66 | 75.81 | 0.001 |
| Private | 18.69 | 18.51 | 17.30 | 17.36 | 0.001 |
| Self‐pay, other | 5.93 | 7.27 | 7.85 | 6.71 | 0.001 |
| Hospital region, % | |||||
| Northeast | 20.61 | 19.56 | 18.77 | 15.81 | 0.001 |
| Midwest | 20.37 | 18.66 | 19.72 | 21.54 | 0.001 |
| South | 33.55 | 36.54 | 38.97 | 41.44 | 0.001 |
| West | 25.47 | 25.24 | 22.55 | 21.21 | 0.001 |
| Hospital size, no. of beds, % | |||||
| Small, 1–99 | 9.29 | 9.38 | 9.38 | 15.27 | 0.001 |
| Medium, 100–200 | 25.62 | 25.75 | 25.33 | 29.54 | 0.001 |
| Large, >200 | 65.09 | 64.86 | 65.29 | 55.19 | 0.001 |
| Urban hospital, % | 88.75 | 90.66 | 91.67 | 94.29 | 0.001 |
| Teaching hospital, % | 40.90 | 42.62 | 48.98 | 69.89 | 0.001 |
| Admission diagnosis, % | |||||
| Sepsis | 12.20 | 16.65 | 21.43 | 24.55 | 0.001 |
| AMI | 13.98 | 10.20 | 9.84 | 10.99 | 0.001 |
| Respiratory failure | 6.05 | 10.06 | 9.42 | 8.12 | 0.001 |
| Heart failure | 6.46 | 5.86 | 4.67 | 4.81 | 0.001 |
| Length of stay, d | 8.22±0.13 | 8.68±0.12 | 8.60±0.08 | 8.51±0.05 | 0.061 |
| VT/VF arrest, % | 21.27 | 20.61 | 23.26 | 27.33 | 0.001 |
| Intervention, % | |||||
| TTM | 0.02 | 0.12 | 1.35 | 1.50 | 0.001 |
| Coronary angiography | 5.33 | 6.17 | 7.93 | 11.60 | 0.001 |
| PCI | 3.09 | 3.80 | 5.16 | 7.66 | 0.001 |
| ECMO | 0.03 | 0.05 | 0.27 | 0.31 | 0.001 |
| Disposition, % of all IHCA | |||||
| Home | 7.46 | 6.95 | 7.62 | 8.60 | 0.001 |
| SAR | 3.99 | 3.08 | 3.31 | 3.83 | 0.111 |
| SNF | 7.00 | 8.93 | 11.61 | 13.97 | 0.001 |
| HHC | 2.53 | 3.06 | 3.80 | 4.74 | 0.001 |
| Hospital cost, $, adjusted for inflation to 2018 | 70 150±1806 | 95 572±2183 | 125 877±2270 | 166 235±1425 | 0.001 |
AMI indicates acute myocardial infarction; ECMO, extracorporeal membrane oxygenation; HHC, home health care; IHCA, in‐hospital cardiac arrest; PCI, percutaneous coronary intervention; SAR, subacute rehab; SNF, skilled nursing facility; TTM, targeted temperature management; and VT/VF, ventricular tachycardia/ventricular fibrillation.
Other: Asian or Pacific Islander, Native American and other unclassified racial and ethnic groups.
A substantial increase in the comorbidity burdens of patients suffering cardiac arrests was observed, as reflected by an increase in mean Charlson Comorbidity Index scores (2.08 to 3.25, P trend<0.001). Geographically, we observed an increase in the incidence of cardiac arrests in the South, whereas rates in the Northeast region declined significantly. In terms of types of hospitals, a steady rise in urban and teaching hospitals was noted, along with a significant increase in patients admitted to small and medium‐sized hospitals, with a decline in those admitted to large hospitals. Sepsis was the most commonly encountered admitting diagnosis, with a significant increase (12.2% to 24.6%, P trend<0.001) during the study period, followed by respiratory failure. Interestingly, rates of heart failure as the admitting diagnosis saw a significant decline, from 6.5% to 4.8% (P trend<0.001) over the study period.
In terms of survival, unadjusted, age‐ and sex‐adjusted as well as a risk‐adjusted analysis was performed (Table 2 and Figure [B]). Between 1999 and 2018, a significant improvement in IHCA‐related survival rates was noted overall, exceeding 10% after risk adjustment (21.3% to 32.7%, P trend<0.001). This was largely driven by improvements in PEA‐asystole survival (from 18.9% to 30.2%, P trend<0.001) and to a lesser extent by VT/VF survival (from 29.8% to 39.7%, P trend<0.001) (Table 2). In more recent years (2014–2018), a relative plateauing of IHCA survival rates was observed, except for PEA‐asystole–related survival (29.1% to 30.2%, P trend<0.001) (Table 2).
Table 2.
Annualized Trends in Survival Rates
| Annual rates | Adjusted rate ratio per year (95% CI) | Overall P trend value | P trend value since 2014 | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1999–2000* | 2001–2002 | 2003– 2004 | 2005– 2006 | 2007–2008 | 2009–2010 | 2011–2012 | 2013–2014 | 2015–2016 | 2017–2018 | ||||
| Overall survival | |||||||||||||
| Unadjusted | 21.28 † | 21.05 | 21.28 | 23.05 | 25.46 | 26.93 | 29.64 | 31.12 | 31.26 | 31.80 | N/A | 0.001 | 0.43 |
| Age/sex adjusted | 21.28 | 21.10 | 21.48 | 23.06 | 25.45 | 26.78 | 29.21 | 30.23 | 30.36 | 30.83 | 1.04 (1.04–1.05) | 0.001 | 0.45 |
| Risk adjusted | 21.28 | 20.93 | 21.60 | 23.74 | 26.02 | 27.44 | 30.41 | 31.52 | 31.72 | 32.70 | 1.05 (1.05–1.06) | 0.001 | 0.049 ‡ |
| Ventricular tachycardia/fibrillation | |||||||||||||
| Unadjusted | 29.79 | 29.86 | 29.94 | 30.67 | 34.41 | 34.46 | 37.69 | 38.61 | 37.43 | 37.57 | N/A | 0.001 | 0.12 |
| Age/sex adjusted | 29.79 | 29.50 | 29.73 | 29.77 | 33.78 | 33.56 | 36.53 | 37.23 | 36.14 | 36.12 | 1.01 (1.01–1.01) | 0.001 | 0.07 |
| Risk adjusted | 29.79 | 29.17 | 30.01 | 30.59 | 34.66 | 34.55 | 38.49 | 39.34 | 38.71 | 39.73 | 1.03 (1.03–1.04) | 0.001 | 0.9 |
| PEA‐asystole | |||||||||||||
| Unadjusted | 18.89 | 18.65 | 19.07 | 21.10 | 23.11 | 24.76 | 27.12 | 28.64 | 28.96 | 29.53 | N/A | 0.001 | 0.21 |
| Age/sex adjusted | 18.89 | 18.91 | 19.46 | 21.43 | 23.37 | 24.96 | 26.95 | 27.93 | 28.17 | 28.70 | 1.02 (1.02–1.03) | 0.001 | 0.001 ‡ |
| Risk adjusted | 18.89 | 18.78 | 19.54 | 22.07 | 23.87 | 25.58 | 28.02 | 29.09 | 29.23 | 30.16 | 1.03 (1.03–1.03) | 0.001 | 0.001 ‡ |
N/A indicates not applicable; and PEA, pulseless electrical activity.
Year 1999 to 2000 is used as reference year for risk adjustment.
Each cell reflects the average value of 2 years.
P‐value is less than 0.05.
In accordance with the American Heart Association resuscitation guideline, use of target temperature management, coronary angiography, percutaneous coronary intervention, and extracorporeal membrane oxygenation has increased significantly in the setting of IHCA (Table 1). A significant increase in hospitalization costs was observed during the study period, even after adjustment for inflation ($70 150±$1806–$166 235±$1425, P trend<0.001). With regard to disposition following hospital discharge, a significant increase in patients discharged home with health care and to skilled nursing facilities was observed. However, rates of discharge to subacute rehabilitation facilities have remained steady over the past 20 years.
Discussion
Tremendous advances in resuscitative as well as post–cardiac arrest care have been made over the past 2 decades, which is reflected by this analysis. The current study of a nationally representative population reflects a gradual shift in IHCA toward a younger albeit sicker population. This increase has been most marked in patients in the lowest quartile of median income. A clear transition in proportions of IHCA cases from larger‐sized, rural hospitals toward smaller and medium‐sized urban teaching hospitals is noted. Furthermore, we also observed an increased burden of comorbidities among patients with IHCA, which is consistent with recent data from the Get With The Guidelines registry. 12 Interestingly, the proportion of IHCAs associated with noncardiac admissions, such as sepsis, have increased substantially, whereas cardiac disorders such as acute myocardial infarction and heart failure have gradually declined. This is perhaps a consequence of advances in medical management of acute myocardial infarction and heart failure over the past 2 decades. 4
IHCA‐related survival rates, especially in the setting of PEA‐asystole, have increased significantly over the past 2 decades, in alignment with reports by Thompson et al 13 and recent data from a Swedish registry. 14 VT/VF‐related survival has plateaued in recent years after rapid initial improvements in outcomes at the turn of the century. These survival rates correlate well with data from the Get With The Guidelines registry, 4 , 11 , 12 , 13 prior NIS‐based studies, 3 , 7 , 8 and data from a Swedish registry, 14 but were lower compared with the UK National Cardiac Arrest Audit Database between 2011 and 2013 (reported survival after shockable rhythm of 49%). 2 The improved IHCA survival may have been a result of improvements in resuscitation techniques, the increasing use of guideline‐directed intervention such as target temperature management, and early revascularization where indicated. Furthermore, the use of specialized code teams and a more protocolized approach to resuscitative care has likely contributed as well. 5
We acknowledge that the ideal quality metric in IHCA is meaningful neurological recovery and long‐term survival; however, survival to hospitalization is the first step toward this. In an updated analysis of the Get With The Guidelines‐Resuscitation registry in 2017, among patients surviving to discharge, a majority had a favorable neurological profile (85% with cerebral performance category of 1 and 2). 4
Limitations
The findings of this study should be interpreted in the context of certain limitations. First, the NIS database uses administrative codes and not patient‐level data and is therefore subject to issues related to variability in reporting and coding errors. The ICD‐9‐CM codes for IHCA have been well validated in several prior studies. However, the ICD‐10‐CM codes for the same, though used widely in several recent articles, have not been formally validated. This could potentially lead to some coding‐related inaccuracies. The transition of coding practices from ICD‐9‐CM to ICD‐10‐CM in 2015 might have impacted IHCA incidence and survival results as reflected by a slight decline in rates in 2015. Furthermore, no specifics of resuscitative care or measures of meaningful neurological recovery could be made. We are unable to determine how our analyses could be affected by the differences in admission code status and its impact on in‐hospital survival. Although our study demonstrates increased risk‐adjusted survival after IHCA and increased use of interventions such as target temperature management and percutaneous coronary intervention, our data do not permit a more granular analysis of resuscitation specifics and rates of adherence to the guidelines.
Another limitation involves rhythm identification using ICD‐9‐CM and ICD‐10‐CM diagnosis codes. Prior studies have validated the positive predictive value of ICD‐9‐CM and ICD‐10‐CM codes in VT/VF identification at between 77% and 100%. 15 However, the identification of nonshockable rhythms has been challenging, because specific codes and results pertaining to them must be interpreted with caution.
Conclusions
During the past 2 decades, significant improvements in IHCA survival have been witnessed, both with shockable and nonshockable rhythms. Future work is needed to identify trends in the characteristics of survivors that could better guide resource allocation and health policy.
Sources of Funding
None.
Disclosures
None.
Supporting information
Tables S1–S2
Supplementary Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.021572
For Sources of Funding and Disclosures, see pages 6 and 7.
References
- 1. Andersen LW, Holmberg MJ, Berg KM, Donnino MW, Granfeldt A. In‐hospital cardiac arrest: a review. JAMA. 2019;321:1200–1210. doi: 10.1001/jama.2019.1696 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Nolan JP, Soar J, Smith GB, Gwinnutt C, Parrott F, Power S, Harrison DA, Nixon E, Rowan K; National Cardiac Arrest Audit . Incidence and outcome of in‐hospital cardiac arrest in the United Kingdom National Cardiac Arrest Audit. Resuscitation. 2014;85:987–992. doi: 10.1016/j.resuscitation.2014.04.002 [DOI] [PubMed] [Google Scholar]
- 3. Kolte D, Khera S, Aronow WS, Palaniswamy C, Mujib M, Ahn C, Iwai S, Jain D, Sule S, Ahmed A, et al. Regional variation in the incidence and outcomes of in‐hospital cardiac arrest in the United States. Circulation. 2015;131:1415–1425. doi: 10.1161/CIRCULATIONAHA.114.014542 [DOI] [PubMed] [Google Scholar]
- 4. Benjamin EJ, Muntner P, Alonso A, Bittencourt MS, Callaway CW, Carson AP, Chamberlain AM, Chang AR, Cheng S, Das SR, et al.; American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee . Heart disease and stroke statistics‐2019 update: a report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659 [DOI] [PubMed] [Google Scholar]
- 5. Neumar RW, Shuster M, Callaway CW, Gent LM, Atkins DL, Bhanji F, Brooks SC, de Caen AR, Donnino MW, Ferrer JME, et al. Part 1: executive summary: 2015 American Heart Association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation. 2015;132:S315–S367. doi: 10.1161/CIR.0000000000000252 [DOI] [PubMed] [Google Scholar]
- 6. Overview of the National (Nationwide) Inpatient Sample (NIS) . Available at: https://www.hcupus.ahrq.gov/nisoverview.jsp. Accessed January 15, 2017.
- 7. Khan MZ, Syed M, Agrawal P, Osman M, Khan MU, Alharbi A, Benjamin MM, Khan SU, Balla S, Munir MB. Baseline characteristics and outcomes of end‐stage renal disease patients after in‐hospital sudden cardiac arrest: a national perspective. J Interv Card Electrophysiol. 2021.[e‐pub ahead of print]. doi: 10.1007/s10840-021-00977-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Patel N, Patel NJ, Macon CJ, Thakkar B, Desai M, Rengifo‐Moreno P, Alfonso CE, Myerburg RJ, Bhatt DL, Cohen MG. Trends and outcomes of coronary angiography and percutaneous coronary intervention after out‐of‐hospital cardiac arrest associated with ventricular fibrillation or pulseless ventricular tachycardia. JAMA Cardiol. 2016;1:890–899. doi: 10.1001/jamacardio.2016.2860 [DOI] [PubMed] [Google Scholar]
- 9. DeZorzi C, Boyle B, Qazi A, Luthra K, Khera R, Chan PS, Girotra S. Administrative billing codes for identifying patients with cardiac arrest. J Am Coll Cardiol. 2019;73:1598–1600. doi: 10.1016/j.jacc.2019.01.030 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Khera R, Angraal S, Couch T, Welsh JW, Nallamothu BK, Girotra S, Chan PS, Krumholz HM. Adherence to methodological standards in research using the national inpatient sample. JAMA. 2017;318:2011–2018. doi: 10.1001/jama.2017.17653 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Girotra S, Nallamothu BK, Spertus JA, Li Y, Krumholz HM, Chan PS; American Heart Association Get with the Guidelines‐Resuscitation Investigators . Trends in survival after in‐hospital cardiac arrest. N Engl J Med. 2012;367:1912–1920. doi: 10.1056/NEJMoa1109148 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Holmberg MJ, Granfeldt A, Girotra S, Donnino MW, Andersen LW; American Heart Association’s Get With The Guidelines®‐Resuscitation Investigators . Trends in survival and introduction of the 2010 and 2015 guidelines for adult in‐hospital cardiac arrest. Resuscitation. 2020;157:112–120. doi: 10.1016/j.resuscitation.2020.10.022 [DOI] [PubMed] [Google Scholar]
- 13. Thompson LE, Chan PS, Tang F, Nallamothu BK, Girotra S, Perman SM, Bose S, Daugherty SL, Bradley SM; American Heart Association’s Get With the Guidelines‐Resuscitation Investigators . Long‐term survival trends of medicare patients after in‐hospital cardiac arrest: insights from get with the guidelines‐resuscitation® . Resuscitation. 2018;123:58–64. doi: 10.1016/j.resuscitation.2017.10.023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Adielsson A, Djärv T, Rawshani A, Lundin S, Herlitz J. Changes over time in 30‐day survival and the incidence of shockable rhythms after in‐hospital cardiac arrest—a population‐based registry study of nearly 24,000 cases. Resuscitation. 2020;157:135–140. doi: 10.1016/j.resuscitation.2020.10.015 [DOI] [PubMed] [Google Scholar]
- 15. De Bruin ML, van Hemel NM, Leufkens HG, Hoes AW. Hospital discharge diagnoses of ventricular arrhythmias and cardiac arrest were useful for epidemiologic research. J Clin Epidemiol. 2005;58:1325–1329. doi: 10.1016/j.jclinepi.2005.04.009 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


