Abstract
Malignant hypertension is a hypertensive emergency, with rapid disease progression and poor prognosis. Although recognized as a separate entity more than a century ago, significant knowledge gaps remain about its pathogenesis and treatment. This narrative review summarizes current viewpoints, research gaps, and challenges with a view to pooling future efforts at improving treatment and prognosis.
Keywords: basic science, clinical research, hypertensive emergency, malignant hypertension
Subject Categories: Hypertension, Basic Science Research, Clinical Studies
About 0.5% to 3% of all emergency department visits concern individuals who present with a suspected hypertensive emergency. One quarter of them have a hypertensive emergency that requires urgent treatment to lower blood pressure (BP) to safe levels. 1 Hypertensive emergencies are potentially life‐threatening manifestations of hypertension, associated with acute impairment of ≥1 organs including the large arteries, heart, kidney, and brain. 2 The Studying the Treatment of Acute Hypertension registry reported 6.9% hospital mortality and a 37% readmission rate 90 days after discharge for a hypertensive emergency in 25 US institutions, between January 2007 and April 2008. 3 Of the different types of hypertensive emergencies, malignant hypertension (MHT) is characterized by extreme BP elevations and acute microvascular damage affecting various organs, in particular the retina, brain, and kidney (Table). 2 , 4 , 5 , 6 , 7 Data on prevalence and incidence of MHT are sparse. In large multi‐ethnic urban communities in Birmingham (United Kingdom) and Amsterdam (Netherlands), overall incident rates of MHT have been 2 new cases per 100 000 individuals per year, with up to 4‐fold higher rates (7.3 per 100 000 per year) reported for self‐reported Black‐African/Afro‐Caribbean ethnicity. 8 While survival after MHT has considerably improved, it is still associated with significant morbidity and mortality. Amraoui et al reported an all‐cause mortality of 10% at 5 years in patients with a mean age of 44 years, 9 while 20% needed a kidney replacement. Yet MHT has received little attention from the medical and scientific community, and diagnostic and therapeutic guidelines are mainly based on consensus rather than robust data, while definitions are not uniform (Table). 2
Table 1.
Agreement and Disagreement About Malignant Hypertension Definition in Latest Hypertension Guidelines/Consensus
| Guidelines/DOI | Definition | Agreement and disagreement |
|---|---|---|
| ISH 2020 4 |
Severe blood pressure elevation (commonly >200/120 mm Hg) associated with advanced bilateral retinopathy (hemorrhages, cotton wool spots, papilledema) |
Need for severe rise in blood pressure is commonly accepted, but no specific threshold has been validated to date. In this context, presence of severe hypertensive retinopathy triggers diagnosis of malignant hypertension. This is a consensus. Whether it is mandatory in presence of heart, kidney, brain damage, and/or thrombotic microangiopathy is debated, as is need for bilateral retinal involvement or presence of papilledema. Isolated dry exudates, cotton wool spots, and hemorrhages may also evoke severe hypertensive retinopathy |
| NICE 2019 5 | Severe increase in blood pressure to 180/120 mm Hg or higher (and often >220/120 mm Hg) with signs of retinal hemorrhage and/or papilledema (swelling of optic nerve). Usually associated with new or progressive target organ damage | Committee agreed that further research is needed in this area. No relevant clinical studies or published evidence were identified during review process |
| ESC/ESH 2018 6 | Malignant hypertension is a hypertensive emergency characterized by presence of severe BP elevation (usually >200/120 mm Hg) and advanced retinopathy, defined as bilateral presence of flame‐shaped hemorrhages, cotton wool spots, or papilledema | Authors stated that rate and magnitude of BP increase may be at least as important as absolute BP level in determining magnitude of organ injury |
| European Consensus 2018 2 | Coexistence of high BP values (often >200/120 mm Hg) with advanced retinopathy (defined as bilateral presence of flame‐shaped hemorrhages, cotton wool spots, or papilledema), acute renal failure, and/or thrombotic microangiopathy. Because systemic microcirculatory damage is a pathological hallmark of malignant hypertension, and retinal lesions can be absent in patients with acute microvascular damage to kidney and brain, acute hypertensive microangiopathy could be an alternative term | Plea for broader definition, considering gaps in evidence and pathophysiology of disease, because retinal lesions may be absent in patients with acute microvascular damage to kidney, heart, and brain |
| AHA 2017 7 | Not mentioned | Malignant hypertension not mentioned in section on hypertensive emergencies, reflecting oversight of this form by medical community |
BP indicates blood pressure.
In this review, we summarize current viewpoints on MHT, highlight ongoing challenges in its management, and propose future investigations to improve patient care.
EPIDEMIOLOGICAL CHALLENGES
While progress in the treatment and control of hypertension in the population at large has resulted in a decline in the number of MHT cases, it still exists. Recent evidence from the Birmingham, Bordeaux 10 and Amsterdam MHT registries suggests that the number of cases is rising, 2 , 8 in particular among ethnic minority groups. In the Bordeaux cohort, mean inclusions increased from 3 to 5 patients per year between 2001 and 2006 to >15 after 2016. In line with this observation, the number of patients on hemodialysis owing to MHT has also increased in hemodialysis registries in the Netherlands and elsewhere in Europe. MHT is probably underdiagnosed, being classified as hypertensive emergency or being missed for several reasons: (1) BP may not be taken initially because patients often present with atypical symptoms, including headache, visual disturbances, or gastrointestinal complaints; (2) differentiating between severe uncontrolled hypertension and malignant hypertension maybe challenging if target organs are not systematically screened 11 ; (3) the clinical presentation is heterogeneous with cardiac, renal, or neurological forms sometimes predominating and involving several disciplines. 10
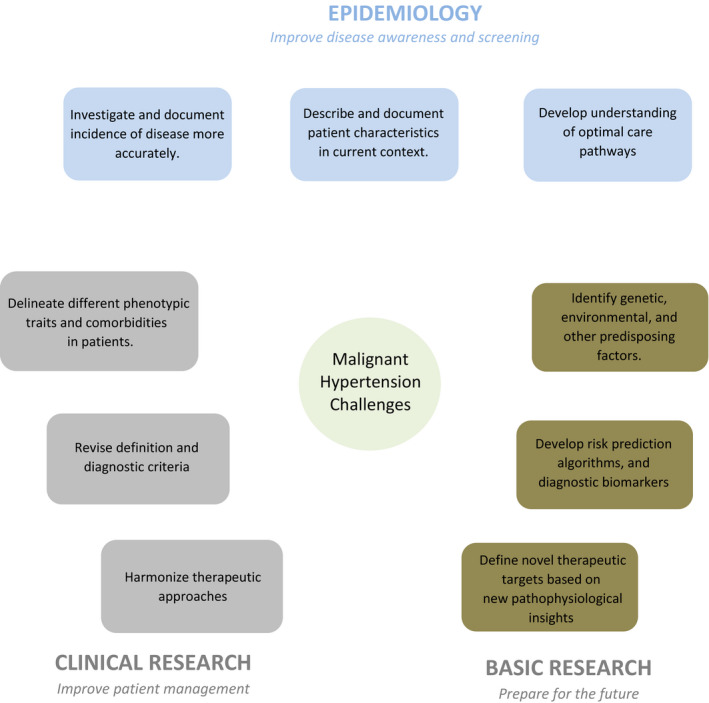
In summary, the main challenge from the clinical epidemiology point of view is to define the current incidence and prevalence of malignant hypertension in developing countries and to specify the characteristics of patients and different care pathways involved ( Figure ). This may help increase awareness about the disease among physicians managing MHT. A prospective international registry should be set up to answer these questions.
Figure 1. Challenges in malignant hypertension research and management.
CLINICAL RESEARCH CHALLENGES
To improve the management of patients with MHT, clinical research must be strengthened. Currently, diagnostic criteria and treatment proposals can only be based on consensus, as no solid scientific evidence is available in this area.
Clinical Diagnosis
There is debate whether the traditional definition fully captures the extent of the microvascular damage associated with MHT and whether a more extensive definition should be used to better identify patients with acute microvascular damage. This is also reflected in current definitions which, to various degrees, tend to go beyond the original definition (see Table). A recent proposal is based on the presence of multiorgan damage to define MHT, even if the fundus is normal or data are not available. 12 This definition assumes the availability of modern diagnostic methods to explore target organ damage resulting from microcirculatory damage, including blood and urine samples for the evaluation of thrombotic microangiopathy and acute kidney injury, respectively, and cerebral and cardiac magnetic resonance imaging. 12 Future research is needed to establish whether patients with the classical or the new definition share the same prognosis and clinical and paraclinical features.
Challenges With Heterogeneous Presentations and Associated Factors
It is widely considered that any condition that results in a significant BP increase (such as associated kidney disease or renal artery stenosis, use of pressor or toxic agent, poor adherence) may further worsen BP control in those who are untreated or uncontrolled despite medication and present them with signs and symptoms consistent with MHT. 2 Pregnancy is another known precipitating factors.
To what extent genotype and pathophysiological background differ between such patients remains elusive, and whether understanding of these differences would improve their management or lead to new therapeutic pathways is still a matter of conjecture. In the Bordeaux cohort, most common reasons for hospital admission were visual impairment (25%), stroke (21%), and heart failure (10%), while the remaining patients were admitted for high BP (20%) and less specific symptoms including headaches, dizziness, anorexia, and asthenia (17%). 10 Although the original article in 1928 described the cardiac, neurological, and renal forms of the disease, 13 it is still unclear why these organs are particularly affected, even though autopsy studies reported generalized microvascular damage. 14
Limited Therapeutic Options
The optimal treatment for MHT remains to be established. Traditional intravenous therapy reducing mean BP of 25% in the first hours is being challenged in uncomplicated MHT. Inappropriate management may cause microvascular damage and result in irreversible tissue injury, while vigorous BP‐lowering treatment has resulted in ischemic stroke and death. Research has shown that cerebral autoregulation is impaired in patients with MHT, making them prone to cerebral hypoperfusion when BP is lowered. Whether intravenous therapy is always necessary is a matter of debate given recent reports that oral medication can also result in the controlled reduction of BP. 2 , 15 To date, no specific study has been conducted to answer these questions.
In summary, the main clinical challenges are as follows: (1) to better understand the different phenotypic presentations of MHT, and how their identification could improve patient management; (2) to update the definition and diagnostic criteria of MHT and to improve our therapeutic knowledge of it; and (3) to standardize and simplify the guidelines in terms of administration route, drug type, and BP targets ( Figure ).
BASIC SCIENCE CHALLENGES
The reason why some patients progress to MHT and others do not remains an enigma. In historical cohorts of patients with untreated hypertension, only 6% to 8% progress to MHT. 16 Progression to MHT likely results from a complex interaction of genetic and environmental factors. Past evidence points to the key role of the renal and renin‐angiotensin system in both animal models and in humans. 17 , 18 However, polymorphisms in the complement system may also predispose patients to thrombotic microangiopathy and MHT, 19 while the involvement of other relevant pathways involving the profibrotic and antiangiogenic systems remains unexplored.
In summary, the basic science challenges are to identify new pathophysiological pathways that could help define specific biomarkers for the risk assessment, diagnosis, and monitoring of MHT. This could lead to targeted prevention strategies involving personalized medicine and new therapeutic approaches based on specific pathophysiological data ( Figure ).
CONCLUSIONS
The management of MHT is mainly based on consensus gleaned from clinical expertise and evidence of inadequate quality. Accumulating good‐quality data through multicenter registries, comparative trials, and centralized biobanks could help improve the assessment and management of these patients. In this perspective, the Hypertension Arterielle MAligne (HAMA) project (NCT03755726) aims to become an international prospective database that would create a powerful platform for collaborative research on MHT.
Sources of Funding
None.
Disclosures
None.
This manuscript was sent to Alexandros Briasoulis, MD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
For Sources of Funding and Disclosures, see page 4.
REFERENCES
- 1. Paini A, Aggiusti C, Bertacchini F, Rosei CA, Maruelli G, Arnoldi C, Cappellini S, Muiesan ML, Salvetti M. Definitions and epidemiological aspects of hypertensive urgencies and emergencies. High Blood Press Cardiovasc Prev. 2018;25:241–244. doi: 10.1007/s40292-018-0263-2 [DOI] [PubMed] [Google Scholar]
- 2. Van den Born B‐J, Lip GYH, Brguljan‐Hitij J, Cremer A, Segura J, Morales E, Mahfoud F, Amraoui F, Persu A, Kahan T, et al. ESC Council on hypertension position document on the management of hypertensive emergencies. Eur Heart J Cardiovasc Pharmacother. 2019;5:37–46. doi: 10.1093/ehjcvp/pvy032 [DOI] [PubMed] [Google Scholar]
- 3. Katz JN, Gore JM, Amin A, Anderson FA, Dasta JF, Ferguson JJ, Kleinschmidt K, Mayer SA, Multz AS, Peacock WF, et al. Practice patterns, outcomes, and end‐organ dysfunction for patients with acute severe hypertension: the Studying the Treatment of Acute hyperTension (STAT) Registry. Am Heart J. 2009;158:599–606. doi: 10.1016/j.ahj.2009.07.020 [DOI] [PubMed] [Google Scholar]
- 4. Unger T, Borghi C, Charchar F, Khan NA, Poulter NR, Prabhakaran D, Ramirez A, Schlaich M, Stergiou GS, Tomaszewski M, et al. 2020 International Society of Hypertension Global Hypertension practice guidelines. Hypertension. 2020;75:1334–1357. doi: 10.1161/HYPERTENSIONAHA.120.15026 [DOI] [PubMed] [Google Scholar]
- 5. National Guideline Centre (UK) . Hypertension in adults: diagnosis and management. In: NBK547161. 2019.
- 6. Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, Burnier M, Clement DL, Coca A, de Simone G, Dominiczak A, et al. 2018 ESC/ESH guidelines for the management of arterial hypertension. Eur Heart J. 2018;33:3021–3104. doi: 10.1093/eurheartj/ehy339 [DOI] [PubMed] [Google Scholar]
- 7. Whelton PK, Carey RM, Aronow WS, Casey DE, Collins KJ, Himmelfarb CD, Depalma SM, Gidding S, Jamerson KA, Jones D, et al. 2017 ACC/AHA/AAPA/ABC/ACPM/AGS/APhA/ASH/ASPC/NMA/PCNA guideline for the prevention, detection, evaluation, and management of high blood pressure in adults: a report of the American College of Cardiology/American Heart Association Task Force on Clinical Practice guidelines. J Am Coll Cardio. 2018;71:127–248. doi: 10.1016/j.jacc.2017.11.006. [DOI] [PubMed] [Google Scholar]
- 8. Shantsila A, Lip GYH. Malignant hypertension revisited—does this still exist? Am J Hypertens. 2017;30:543–549. doi: 10.1093/ajh/hpx008 [DOI] [PubMed] [Google Scholar]
- 9. Amraoui F, Van Der Hoeven NV, Van Valkengoed IGM, Vogt L, Van Den Born B‐J. Mortality and cardiovascular risk in patients with a history of malignant hypertension: a case‐control study. J Clin Hypertens (Greenwich). 2014;16:122–126. doi: 10.1111/jch.12243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Rubin S, Cremer A, Boulestreau R, Rigothier C, Kuntz S, Gosse P. Malignant hypertension: diagnosis, treatment and prognosis with experience from the Bordeaux cohort. J Hypertens. 2018;36:1–9. doi: 10.1097/HJH.0000000000001913 [DOI] [PubMed] [Google Scholar]
- 11. Nijskens CM, Veldkamp SR, Van Der Werf DJ, Boonstra AH, Ten Wolde M. Funduscopy: yes or no? Hypertensive emergencies and retinopathy in the emergency care setting; a retrospective cohort study. J Clin Hypertens. 2020;00:1–6. doi: 10.1111/jch.14064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cremer A, Amraoui F, Lip GYH, Morales E, Rubin S, Segura J, Van den Born BJ, Gosse P. From malignant hypertension to hypertension‐MOD: a modern definition for an old but still dangerous emergency. J Hum Hypertens. 2016;30:463–466. doi: 10.1038/jhh.2015.112 [DOI] [PubMed] [Google Scholar]
- 13. Kernohan JW, Keith NM, Wagener HP. The syndrome of malignant hypertension. Arch Intern Med. 1928;230:141–188. [Google Scholar]
- 14. Keith N. Classification of hypertension and clinical differentitation of the malignant type. Am Heart J. 1927;11:597–608. doi: 10.1016/S0002-8703(27)90207-5 [DOI] [Google Scholar]
- 15. Gosse P, Boulestreau R, Brockers C, Puel C, Rubin S, Cremer A. The pharmacological management of malignant hypertension. J Hypertens. 2020;38:2325–2330. doi: 10.1097/HJH.0000000000002547 [DOI] [PubMed] [Google Scholar]
- 16. Dranov J, Skyler JS, Gunnels JC. Malignant hypertension. Arch Intern Med. 1974;133:791–801. doi: 10.1001/archinte.1974.00320170073006 [DOI] [PubMed] [Google Scholar]
- 17. van den Born BJH, Koopmans RP, van Montfrans GA. The renin‐angiotensin system in malignant hypertension revisited: plasma renin activity, microangiopathic hemolysis, and renal failure in malignant hypertension. Am J Hypertens. 2007;20:900–906. doi: 10.1016/j.amjhyper.2007.02.018 [DOI] [PubMed] [Google Scholar]
- 18. Lohmeier TE, Cowley AW. Hypertensive and renal effects of chronic low level intrarenal angiotensin infusion in the dog. Circ Res. 1979;44:154–160. doi: 10.1161/01.RES.44.2.154 [DOI] [PubMed] [Google Scholar]
- 19. Timmermans SAMEG, Wérion A, Damoiseaux JGMC, Morelle J, Reutelingsperger CP, Paassen VP. Diagnostic and risk factors for complement defects in hypertensive emergency and thrombotic microangiopathy. Hypertension. 2020;75:422–430. doi: 10.1161/HYPERTENSIONAHA.119.13714 [DOI] [PubMed] [Google Scholar]


