Abstract
Background
Heart‐healthy lifestyles promote lifelong cardiovascular health. However, patients with hypertrophic cardiomyopathy are often advised to avoid strenuous exercise because of the risk of sudden cardiac death. Given these restrictions, this study explored youth and parent perceptions of a heart‐healthy lifestyle and the barriers and facilitators to this lifestyle.
Methods and Results
Youth and parents were purposefully recruited at 2 Canadian hospitals for this photovoice project. Participants were given cameras and took pictures of everyday heart‐healthy or heart‐unhealthy choices. Photos were discussed during one‐on‐one qualitative interviews with youth and parents separately to understand the photos’ meaning and significance. Inductive descriptive thematic analysis was employed. A total of 16 youth (median age, 14.4 years [range, 10.5–17.7 years]; 63% boys) and 16 parents (100% women) participated. A total of 15 youth were activity restricted. Data analysis revealed 7 categories organized into perceptions of healthy living (health is holistic and individualized) and factors influencing engagement in healthy living (self‐awareness, ownership and autonomy, feeling restricted and peer pressure, support from parents, and support from the cardiologist). Participants had a complex understanding of health and discussed the importance of physical, mental, and social well‐being. Youth used self‐awareness and taking responsibility as facilitators of healthy living. Healthy living was shaped by peers, parent role‐modeling, and cardiologist recommendations.
Conclusions
This study depicts the realities for youth with hypertrophic cardiomyopathy and can be used to inform the development of responsive interventions. Holistic, patient‐specific interventions may be more successful, and strategies such as shared decision making may be important to promote self‐awareness and autonomy.
Keywords: congenital heart disease, health promotion, hypertrophic cardiomyopathy, pediatric cardiology, qualitative research
Subject Categories: Pediatrics, Diet and Nutrition, Exercise, Lifestyle, Primary Prevention
Nonstandard Abbreviations and Acronyms
- HCM
hypertrophic cardiomyopathy
- NYHA
New York Heart Association
Clinical Perspective
What Is New?
This is the first study to use photovoice, a novel qualitative data–generating strategy, to explore youth and parent perspectives on living with hypertrophic cardiomyopathy.
Youth and parents perceived health as holistic and individualized, which aligns with the World Health Organization’s definition of health.
Youth described their actions as central to healthy living and shared how their health behaviors were shaped by peers, parents, and cardiologists.
What Are the Clinical Implications?
Healthy living programs for youth with hypertrophic cardiomyopathy should be patient specific and promote physical, mental, and social well‐being.
Share decision making, which has been highlighted by the American Heart Association and the European Society of Cardiology, should be incorporated into these programs because youth are more likely to engage in healthy living when they are in control of their choices.
To address patients’ holistic needs, interventions should include multidisciplinary teams.
Hypertrophic cardiomyopathy (HCM) is an inherited cardiomyopathy with the hallmark feature of left ventricular hypertrophy. It is the most common inherited cardiomyopathy with a prevalence of 1 in 500 in the general population. 1 , 2 Common features of HCM include outflow obstruction and risk of arrhythmias and sudden cardiac death. 3 Emerging evidence suggests that risk factors for cardiovascular disease, including being overweight/obesity, are high among children and adolescents with HCM. 4 This is concerning as the development of these risk factors early in life has been shown to increase the risk of developing cardiovascular disease in adulthood. 5 Indeed, a cross‐sectional survey demonstrated that adults with HCM are less physically active with higher body mass indexes compared with the general population. 6 These data suggest that primary prevention and early intervention strategies are needed to promote cardiovascular health among children and youth with HCM.
It is widely acknowledged that lifestyle behaviors such as physical activity, diet, weight management, never smoking, and alcohol consumption reduction are important for promoting cardiovascular health in pediatric and adult populations. 7 , 8 Until recently, guidelines advised patients with HCM to avoid intense physical activity and competitive sports because of the risk of sudden cardiac death. 9 Qualitative studies indicate that these physical activity restrictions significantly impact daily routines of children and limit physical activity participation. 10 , 11 Recently, the American College of Cardiology/American Heart Association have transitioned away from providing blanket physical activity restriction recommendations toward a shared decision‐making model. 12 Although these guidelines clearly identify the benefits of healthy living, 12 it remains unclear how these guidelines will be implemented in pediatrics. In addition, more research is needed to understand what factors promote or hinder youth and their family’s ability to engage in healthy living.
To address this gap, qualitative methods have been used to understand the barriers and facilitators that underlie individual health behaviors. 13 In particular, photovoice, a qualitative data–generation strategy in which participants take photos to record their lives, has been used to elicit young people’s voice and perspectives. 14 , 15 Participants then engage in an interview to explore the meaning and significance of their photos. This strategy prioritizes participants’ voices and facilitates a deeper understanding of participants’ lived experience by depicting their everyday realities. These insights are valuable and can be used to inform the development of interventions that are responsive to the needs of the patient population. 13 This is especially important in pediatrics, as childhood is a window of opportunity to intervene and establish healthy behaviors. 8 Furthermore, given the integral role parents play in supporting their child as they manage their chronic health condition, it is important to include parent perceptions as well. 16 As such, this study used photovoice to explore youth with HCM and parent perceptions of (1) a heart‐healthy lifestyle and (2) the barriers and facilitators to a heart‐healthy lifestyle. Understanding youth and parent perceptions of health and the factors that influence their engagement in healthy living is important to inform the development of tailored and responsive healthy living programs.
Methods
Interpretive description, which has its roots in applied health sciences, was used as the qualitative method to study participant perceptions of cardiovascular health. 17 Interpretive description allows researchers to generate new understandings of participants’ subjective experiences to inform decision making. Another strength of interpretive description is that it encourages clinician researchers to act reflexively, applying clinical reasoning to guide interpretation, and thus inform clinical decision making. The data that support the findings of this study are available from the corresponding author upon reasonable request.
Setting
This research was undertaken at the Stollery Children’s Hospital in Edmonton, Alberta, Canada, and the Hospital for Sick Children in Toronto, Ontario, Canada. The research project was housed within the Pediatric Cardiomyopathy and Heart Function service at both centers. These teams offer inpatient and outpatient support including multidisciplinary care for children and youth with primary heart muscles diseases.
Participant Recruitment
Youth and their parents were purposefully recruited through outpatient clinics at 2 sites. 18 Child–parent dyads were eligible to participate if the child was aged between 10 and 19 years and met diagnostic criteria for primary HCM, adjudicated by a cardiomyopathy‐experienced cardiologist. The final sample size of 16 youth and 16 parents is consistent with recommendations of 30 to 60 participants 19 and aligns with previous research using photovoice with children and youth. 20 , 21 , 22 However, sample size was ultimately determined when data saturation was achieved, meaning no new ideas or categories emerged despite continued interviewing. 23 Saturated data are “comprehensive and convincing” and the resulting findings “make sense.” 23 To determine when saturation was achieved, data generation and analysis occurred concurrently. Parents and mature youth (aged 15–18 years) provided written and verbal informed consent. Parents provided written consent for youth aged <15 years, and youth provided verbal assent before starting the interview. This project obtained ethical approval from the Health Research Ethics Board at the University of Alberta and the University of Toronto. The procedures followed were in accordance with institutional guidelines.
Data Generation
Based on an established protocol for photovoice, 20 youth and their parents were each given a 24‐exposure disposable camera with a “mission” to each take at least 12 photos depicting choices in their everyday lives that were either healthy or not healthy for their heart. Each participant then took part in a one‐on‐one qualitative interview to understand the meaning and significance of their photos using a modified version of the SHOWed mnemonic (See Data S1). 14 , 24 This involved asking participants to select and contextualize their photos. First, participants were asked to select 5 to 6 photos that best represent choices in their everyday lives that were either healthy or not healthy for their heart. Participants were then asked to describe what was happening in each photo and how it related to heart‐healthy or heart‐unhealthy choices. To better understand participant perceptions and the barriers and facilitators to healthy living, probing questions such as (1) “What does it mean to live a heart‐healthy or unhealthy lifestyle?” and (2) “Is it ever hard to make healthy choices for your heart? Why or why not?” were also asked. Interviews were semistructured, allowing a structured exploration of the phenomenon of interest while remaining open to related phenomena. 18 This approach was also used for feasibility reasons because it allowed multiple interviewers trained in qualitative methods to be involved. Youth and parents were interviewed separately. All in‐person interviews (n=26) occurred in a quiet part of the hospital or research building to promote a meaningful conversation around participant perceptions of a heart‐healthy lifestyle. A total of 6 interviews were conducted virtually using the Personal Health Information Protection Act–compliant version of Microsoft Teams because of restrictions resulting from COVID‐19. 25 Int minutes (median, 42 minutes) and were audio recorded. Data generation and analysis occurred concurrently. 18 Throughout the data generation process, interviewers met to discuss emerging findings. Based on these discussions, the interview guide was modified to probe for emerging findings.
Age, sex, and activity restriction recommendations were extracted from the patient’s medical chart. Weight and height were measured at a clinic visit by the research coordinator. Body mass index for age was used to screen for overweight (85th–95th percentile) or obesity (>97th percentile). 26 Participant‐reported cardiac symptoms were also collected and categorized using the New York Heart Association (NYHA) classification of heart failure. 27
Data Analysis
Interviews were transcribed verbatim and uploaded to ATLAS.ti 8 to assist with data management. Data were analyzed using inductive descriptive thematic analysis. 28 This involved reading transcripts to identify broad‐based codes that brought together segments of information that were thematically linked. Segments of information that described similar ideas were assigned the same code. A list of codes was produced and grouped into categories. The final step involved identifying patterns and relationships within the data. 17 The analysis was completed by a research assistant familiar with this technique and trained in qualitative methods. To affirm participant perceptions, photos and supportive quotes were incorporated into the manuscript. However, because of poor photo quality, an artist was commissioned to recreate participant photos (see Figures S1 through S6 for copies of the original photos).
Methodological Rigor
To establish trustworthiness, specific strategies were employed. Strategies to promote credibility included in depth interviewing with youth and parents to develop a comprehensive understanding of the phenomenon, collecting and analyzing data concurrently, and debriefing with peers. 18 Specifically, the research assistant involved in the data analysis engaged in regular discussions with members of the multidisciplinary research team to reflect on and refine research findings. Transferability, or the ability to apply learnings to understand similar problems, was enhanced by identifying participants who could provide the best information about the phenomenon of interest as well as represented a range of experiences. 18 , 29 In this study, purposeful sampling was used to select participants who could provide in‐depth descriptions of their perceptions of healthy living and the barriers and facilitators to this lifestyle. Our sample also included participants with a range of experiences of living with HCM from asymptomatic to symptomatic at rest. These descriptions were then analyzed to develop a “comprehensive, complete, and saturated” understanding of the phenomenon. 29 This is important because it makes the findings more useful to others interested in developing healthy living interventions for pediatric patients with HCM. Dependability and confirmability were achieved by documenting the research process. 13 Collectively, these strategies were used to unpack the phenomena of interest and ensure that the findings represent participants’ perceptions. 18
Results
In all, 16 youth and parent dyads participated in the study. The median age of pediatric study participants was 14.4 years (range, 10.5–17.7 years). Youth were predominately boys (n=10), and the parents were all women. A total of 8 male youth participants (8/10) were classified as overweight/obese (overweight, 1; obese, 7), and 3 female youth participants (3/6) were classified as overweight/obese (overweight, 2; obese, 1). Most youth had activity restriction recommendations (n=15). Using the NYHA classification of heart failure, 27 6 youth reported no limitation of physical activity (NYHA I), 9 reported symptoms with moderate exertion (NYHA II), and one reported symptoms at rest (NYHA IV). A total of 10 youth reported symptom limitations including shortness of breath (n=5), edema (n=2), exercise intolerance (n=6), chest pain (n=4), dizziness (n=4), palpitations (n=6), and headaches behind the eyes (n=1).
Thematic analysis revealed 7 categories that were organized into the following: perceptions of healthy living (health is holistic and individualized) and factors influencing engagement in healthy living (self‐awareness, ownership and autonomy, feeling restricted and peer pressure, support from parents, and support from the cardiologist). See Figure 1 for a summary of the study findings. Overall, interviews indicated that participants had a complex understanding of health. Youths ability to engage in healthy living was impacted by various individual and interpersonal factors. A detailed description of each category, including supporting quotes, is outlined in the following sections.
Figure 1. Key findings from the qualitative analysis.
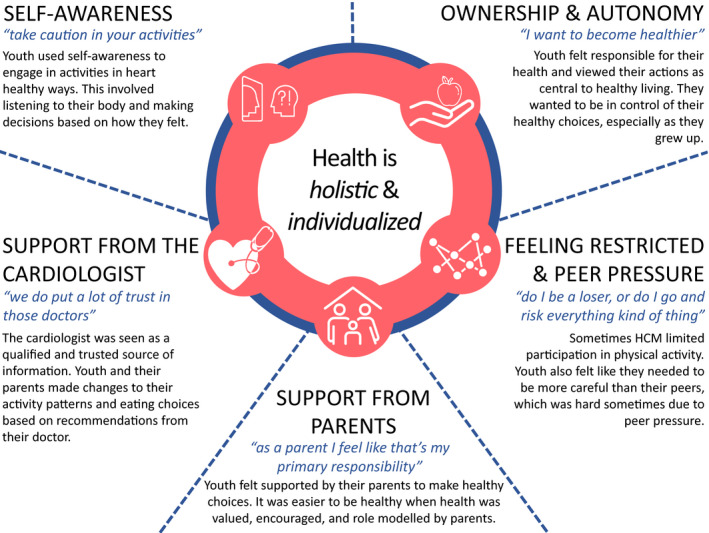
A summary of participant perceptions of healthy living (health is holistic and individualized) and factors influencing engagement in healthy living (self‐awareness, ownership and autonomy, feeling restricted and peer pressure, support from parents, and support from the cardiologist). HCM indicates hypertrophic cardiomyopathy.
Health Is Holistic—“the Heart … Is Just One Part of Our Bodies”
Youth and their parents perceived health as multidimensional. One parent explained it as: “So it’s like everything, it’s like a whole holistic approach, right. It’s not just one thing, it’s like everything together” (01_04 parent). Although physical and mental health were identified most often, participants also described the importance of social health for well‐being. To represent their holistic perceptions of health, participants took more photos of choices in their everyday lives that were either healthy or not healthy in general as opposed to specifically healthy or not healthy for their hearts. Participants explained that their hearts are just one part of who they are and that it is important to take care of yourself as a whole person. This was exemplified by one parent when they shared:
So to me the heart and that physical piece of it, is just one part of our bodies … but all the other aspects of [their] well‐being I think needs to be included as well … like [their] spirit, [their] mind, that needs to be healthy as well in order for [their] heart to be healthy. (01_06 parent)
Participants described how a healthy lifestyle includes engaging in health‐promoting behaviors such as engaging in physical activity, eating healthy, managing stress, connecting with family and friends, maintaining a healthy weight, going to the doctor, and getting enough sleep. In contrast, non–health‐promoting behaviors included unhealthy eating, a sedentary lifestyle, technology use, excess alcohol use, and tobacco and drug use. Health‐promoting behaviors were described as supporting physical, mental, and social health.
Participants also described the importance of balance. In the context of these findings, balance was described as picking the healthy choice most of the time. Similarly, participants described limiting unhealthy choices. For example, one youth took a photo to represent a typical meal and explained (Figure 2):
That’s on a daily basis, pretty much what we eat for dinner. Except for like Fridays and Saturdays um, Friday night’s always pizza. And then Saturday is just kind of whatever. But generally, throughout the week I eat pretty healthy. (01_06 youth)
Figure 2. A balanced meal.
A youth took a photo of their dinner plate, which represents the theme of health is holistic.
Participants described letting themselves or their family make unhealthy choices because it made them happy and promoted social and emotional well‐being. Importantly, it seemed as though their decision to engage in non–health‐promoting behaviors fulfilled other needs. Participants explained that they are not only considering their heart health but also trying to balance their physical, mental, and social well‐being when making choices.
Health Is Individualized—“Do What’s Good for You … Based on Your Situation”
Youth and their parents perceived health as individualized and described tailoring their health behaviors considering their preferences and heart health. One youth described being healthy as “mak[ing] sure you do what’s good for you … based on your situation” (02_03 youth). This was echoed by a parent when they shared their perception of healthy living. They stated, “I think it really just means that you’re taking care of yourself, you’re addressing like your unique concerns as a person …” (01_02 parent).
Youth participants’ approach to healthy living was shaped in part by their illness. For example, some youth participants described tailoring their food choices and water intake to help manage their blood pressure. Others described needing to find the right activity. The right activity was described as something they enjoyed but was not too strenuous. One youth included a photo of them playing goalie to represent the right activity. They described (Figure 3):
And it’s—it’s just moving side to side and that, so it’s like you’re getting some physical activity, but like not enough to push your heart. And like you know have an episode or something or have a cardiac arrest. (02_08 youth)
Figure 3. The right activity—enjoyable, but not too strenuous.
A youth took a photo of a hockey rink, which represents the theme of health is individualized.
Indeed, participants engaged in a wide variety of activities including biking, playing with friends, and playing noncompetitive sports because what was considered appropriate for one youth was not appropriate for another. Taken together, these examples demonstrate how youth participants’ health behaviors were shaped by their preferences and heart health. Their lifestyle needed to be adaptable as each person is unique and their experience of living with HCM is different.
Self‐Awareness—“Take Caution in Your Activities”
Participants identified self‐awareness as an important influencer of healthy living. This was the most prominent finding to emerge from the study. Within the context of these findings, self‐awareness was described as listening to body cues and making decisions based on how you feel. One youth explained that “your body pretty much knows what it wants if you take the time to listen to it, I guess and figure out what it needs” (01_ 07 youth). Youth seemed to be in tune with their bodies and made decisions that made them feel healthy.
In the context of physical activity, self‐awareness involved self‐limiting. This included limiting participation based on symptoms. Youth stated that they listened to how they felt and stopped doing an activity if they experienced chest pain, palpitations, or shortness of breath. For example, one youth explained that when they feel chest pain while exercising, “I would just stop. And take a break” (01_03 youth). Importantly, youth described needing to know their limits to avoid getting to the point where they felt symptoms. This strategy was illustrated by one youth when they took a photo of a caution sign and explained (Figure 4): “I chose that photo because to maintain a healthy heart you have to take caution in your activities. … You can’t push yourself too hard and you can’t—you have to know when to take caution and take a break ...” (02_04 youth).
Figure 4. Taking caution when doing activity.

A youth took a photo of a caution sign, which represents the theme of self‐awareness.
Parents supported this strategy as a way to encourage their child to be active in heart‐healthy ways. Parents trusted that their child would take breaks as needed, especially as they grew up and developed an understanding of “their heart.” One parent stated, “[They’ve] lived with [their heart] almost [their] whole life, so [they] know when [they] feel tired, to stop … but [they] can participate. If [they] feel well enough” (02_04 parent). Parents explained how this strategy meant that their child did not have to completely stop playing but could continue to participate within their limits, which were often discussed and developed with their cardiologist.
Ownership and Autonomy—“I Want to Become Healthier”
Youth described taking responsibility for their health and felt that their actions were central to healthy living. One youth described taking on more responsibility by doing meal planning and grocery shopping. They explained that “sometimes me and my brother will go do [the grocery shopping] ourselves, so. Yeah there’s definitely that responsibility in like trust they put in us to go do that…” (01_06 youth).
Closely tied to ownership was autonomy. Similar to many youth interviewed, one participant wanted autonomy to make healthy choices, especially as they grew up. They chose to take a photo of a car to represent (Figure 5) “having freedom because you can drive anywhere,” which related to a heart‐healthy lifestyle because it meant that “I can choose what I do” (01_03 youth). Indeed, some youth expressed frustration when they did not feel in control or felt like they were being told what to do. For example, one youth stated, “[My doctor] essentially [told] me what I can and cannot do, which sucks” (01_05 youth).
Figure 5. Having freedom.

A youth took a photo of their car, which represents the theme of ownership and autonomy.
Parents echoed the importance of letting their child be in control of their healthy choices. Parents described how as their child grew up, they were engaging in activities more independently. This meant that their child needed to take on more responsibility for their health. One parent conveyed:
Like when you send them to school, I’m not there with you. You know you have to be able to, to do this and eventually you know, you will be an adult. And—and you have to take care of your body. (01_10 parent)
Feeling Restricted and Peer Pressure—“Do I Be a Loser, or Do I Go and Risk Everything Kind of Thing”
In general, youth were accepting of lifestyle changes and restrictions because of their heart condition. One youth summarized it as: “you’re sort of the same as [your peers], but you just need to take more breaks and be more healthy” (02_11 youth). However, participants described how HCM limited their participation in certain health‐promoting behaviors, notably physical activity. For example, youth and their parents explained that they were advised to avoid strenuous physical activity. This was identified by some as a barrier to healthy living. One parent listed approved activities as “golf, bowling, and swimming” and later went on to say: “well just that we were so limited” (01_01 parent). These restrictions made youth upset when they felt limited or held back from being like their peers. One youth took a photo of their dog to explain how (Figure 6):
[Being active and playing with my dog] helps sometimes, but sometimes it makes it worse, like it’s hard for me to re‐catch my breath. … And it also kind of sucks because sometimes um, when I’m playing with him, I’ll have to stop really soon. (01_05 patient)
Figure 6. Needing to catch my breath.

A youth took a photo of their dog, which represents the theme of feeling restricted and peer pressure.
Beyond physical activity, some youth described feeling restricted because they needed to be more careful than their peers. They described avoiding alcohol, cigarettes, roller coasters, and certain unhealthy foods because it was seen as unhealthy for their hearts. One youth shared how they cannot consume alcohol like their peers because of the medication they are taking. Peer pressure sometimes made it harder for youth to make the healthy choice. They had to decide: “do I be a loser, or do I go and risk everything kind of thing…” (01_08 youth).
Support From Parents—“As a Parent I Feel Like That’s My Primary Responsibility”
Parents were described as strong influencers of healthy living. Youth felt supported by their parents to make healthy choices. Similarly, parents felt like it was their responsibility to promote healthy living. One parent stated, “I mean obviously as a parent I feel like that’s my primary responsibility to be having those conversations [about healthy living] all the time” (01_02 parent).
Although youth cited their own research, teachers, and the cardiologist as important sources of information, parents seemed to be the most influential. Parents taught and encouraged healthy behaviors and created healthy home environments. For example, youth described eating healthy or being active because they learned from their parents that it is good for you. In addition, it was easier to be healthy when healthy living was valued, encouraged, role modeled, and done together. One youth explained how their parent was an important influencer of healthy living: “I’ve always done healthy things. I’ve always been told to like go outside, run around, play basketball” (02_03 youth). Another parent took a photo of their salad to represent how they started making salads for themselves and then their child joined in (Figure 7): “I think that’s more about it, right, cause again I can’t tell [them] what [they] should or shouldn’t be doing Um, I, its—it’s truly modeling, I think” (01_06 parent). Finally, it was easier to be healthy when the home environment facilitated healthy living; healthy foods were available, foods were prepared in healthy ways, space/opportunities to be active were provided, and use of electronics was monitored/limited.
Figure 7. Role modeling healthy living.

A parent took a photo of their open fridge, which represents the theme of support from parents.
Support From the Cardiologist—“We Do Put a Lot of Trust in Those Doctors”
Support from the cardiologist to manage their heart condition was identified as a facilitator of healthy living. Participants explained how their cardiologist promoted heart‐healthy lifestyles by providing education and recommendations about physical activity, healthy eating, screen time, vaping, and drugs. Furthermore, the cardiologist was seen as a qualified and trusted source of information as exemplified by one parent when they stated that “ we do put a lot of trust in those doctors” (parent 02_07). Therefore, youth and their parents made changes based on recommendations from their cardiologists.
Often the cardiologist was connected to a multidisciplinary team of dieticians, exercise physiologists, and counselors who were also available to support youth and their parents to engage in healthy living. One parent shared how important this team of health care professionals was:
I was more—more stressed than [child] was when we got diagnosed but when [they] got on a program, [they] work with a psychologist, [they] work with the exercise specialist; [they] work with nutritionist, and all the specialists. I think I got um, more comfortable [with child] doing more stuff. (01_08 parent)
Some youth also participated in healthy lifestyle programming focused on health education.
Discussion
This study used photovoice to explore how youth with HCM and their parents conceptualize a heart‐healthy lifestyle, and the barriers and facilitators to a heart‐healthy lifestyle. This is the first study to explore pediatric patient and parent experiences of living with HCM using photovoice. Our results demonstrated that participants perceived health to be holistic and individualized. Therefore, participants described engaging in health‐promoting behaviors to support their physical, mental, and social well‐being. Participants emphasized the importance of tailoring their behaviors considering their preferences and heart health. This study also revealed how ownership and autonomy, self‐awareness, feeling restricted and peer pressure, support from parents, and support from the cardiologist impact youths ability to engage in healthy living.
Health Is Holistic and Individualized
Participants’ perceptions of health aligned with the World Health Organization’s definition of health, which emphasizes physical, mental, and social well‐being. 30 They demonstrated their commitment to health by engaging in a diversity of healthy behaviors, most notably engaging in physical activity, eating healthy, managing stress, and connecting with others. By elucidating participant perceptions of healthy living, we learned how families make choices about engaging in healthy and unhealthy behaviors. For them, it was important to achieve balance, which sometimes meant doing things that were seen as unhealthy for their heart because it promoted other dimensions of well‐being. We also learned that participants envisioned health as individualized, fluid, and tailored to their unique context. Taken together, it seems as though a successful intervention would balance youth’s physical, mental, and social well‐being while considering their unique needs, notably their cardiovascular health.
Promoting Self‐Awareness, Ownership, and Autonomy
Youth in this study used self‐awareness as one strategy to determine the appropriateness of their activity’s intensity. This included modifying their activity to avoid experiencing symptoms or stopping activity if symptoms arose. This is consistent with another study that looked at the impact of HCM on daily life; pediatric participants described engaging in activity “on their level.” 10 Although no information is available about the safety of this strategy, it may be an important component within a model of shared decision making. Shared decision making is identified in the most recent guidelines from the American College of Cardiology/American Heart Association and the European Society of Cardiology. 12 , 31 These guidelines recommend considering participation in competitive sports on an individual basis in adults. Using shared decision making, patients and providers discuss the patient’s risk profile and their activity needs and interests to determine the appropriateness of competitive sports/vigorous intensity activity. Coupled with risk stratification, patients could use self‐awareness as an additional strategy to monitor their intensity level and safety. This approach requires further study in light of the recent work done to better understand the risk profile of children with HCM. 32 , 33
A shared decision‐making model also aligns with our findings that youth wanted ownership and autonomy over their health behaviors. Our study demonstrated that although physicians and parents can influence healthy living, it is the youth’s responsibility to enact those behaviors. Therefore, it is important for healthy living programs to empower youth to take control over their health, especially as they transition into adulthood where health care services/resources may decrease. 34 Indeed, parents in our study supported their children to take on more responsibility for their health. For this to be successful, youth need the confidence and competence (knowledge and skills) to know how to manage their disease. 35 Strategies to address this could include providing age‐appropriate educational packages that families could use to teach their children.
Fostering a Supportive Environment
In the present study, youth sometimes felt restricted because they needed to be more careful than their peers. This study adds to the literature by demonstrating that youth with HCM experience restrictions beyond physical activity, including, for example, the need to avoid alcohol, caffeine, and roller coasters. As in other reviews, 36 , 37 these restrictions made youth feel upset when it held them back from being like their peers. Peers have been identified as both positive and negative influencers of healthy living. Although our study demonstrated that peer pressure may act as a barrier to healthy living, others have suggested that youth may be more likely to engage in healthy living if their peers are engaging with them. 37 Collectively, these findings suggest that it would be useful to engage youth in conversations about peer‐to‐peer interactions as they seem to be an important contributor to healthy living.
Participants also reported support from parents and the cardiologist as facilitators of healthy living. Support from parents and health care professionals has been previously shown to predict patient compliance to care plans among adolescents living with a chronic disease. 38 Specifically, parents play an integral role by providing emotional and disease‐specific support. 39 This study unpacks the latter by describing the parent’s role in modeling healthy living and creating healthy home environments. Research supports the use of parent role modeling of and support for healthy living to promote fruit and vegetable consumption and engagement in physical activity. 40 , 41 , 42 With respect to the health care team, we learned that cardiologists are seen as trusted sources of information; youth and their parents described making changes based on their recommendations. Participants also described the importance of multidisciplinary care teams. Looking to interventions aimed at reducing overweight and obesity in pediatrics, it seems that more intensive interventions that involved multidisciplinary care teams were more effective compared with interventions that relied on motivational interviewing alone. 43 Using multidisciplinary care teams involving nurses, dietitians, exercise physiologists, and social workers may be more effective as they can leverage the skills of multiple disciplines and enable care to be holistically addressed, which aligns with youth and parent perceptions of health from this study. These interventions also seem well positioned to provide youth with the knowledge and skills to manage their disease.
Strengths and Limitations
There are a few limitations to this study. First, some issues arose around photo taking, including many photos not being developed or not visible because they were too dark. Despite this, interviewers were able to capture in‐depth understanding of participants’ perceptions by asking questions, such as “What would you have liked to take a photo of?” In addition, participant photos were recreated to improve the photo quality. Second, there is potential for recall error in part caused by the long interval between photo taking and the interview for some participants. Third, this study only interviewed female‐identifying parents. Given that male‐identifying parents are underrepresented in clinical research, 44 , 45 more research is needed to understand experiences and perspectives of male‐identifying parents as it represents a significant gap in our current knowledge. Lastly, part of this study was conducted during the COVID‐19 pandemic, so it needed to be transitioned to an online format part way through data generation. Despite this obstacle, the research team was able to adapt, and the use of virtual interviewing enabled us to capture data that otherwise would not have been collected. Other strengths of the study included the use of photovoice. Based on our experience, photovoice enabled participants to lead the discussion by choosing and describing photos that were most important to them. Similar to another study conducted with youth with sickle cell disease, 15 photovoice gave us a comprehensive picture of participant perceptions. Finally, this study has a relatively large sample size and inclusion of participants in 2 provinces from both urban and rural locations, which enhances the generalizability of our findings.
Conclusions
In conclusion, our results provide insight on the perceptions of youth living with HCM and their parents regarding a heart‐healthy lifestyle. The results suggest that youth and parents have a complex understanding of health, which aligns with the World Health Organization. Furthermore, youth described their central role in health promotion by using self‐awareness and taking responsibility and ownership for their health. Finally, this study elucidated how health‐promoting behaviors are shaped by peers, parent role‐modeling, and cardiologist recommendations.
These findings can be applied by clinicians to develop healthy living interventions that are responsive to the needs of pediatric patients with HCM. It is recommended that future interventions aim to promote children and youth’s physical, mental, and social well‐being while tailoring recommendations to their unique needs. For this to be successful, interventions would likely need to involve a multidisciplinary team. In addition, we recommend strategies such as shared decision making, which has been highlighted by the American Heart Association and the European Society of Cardiology, to promote self‐awareness and patient autonomy.
Sources of Funding
This project was supported by the Children’s Cardiomyopathy Foundation, the Labatt Family Heart Centre, and the generous support of the Stollery Children’s Hospital Foundation through the Women and Children’s Health Research Institute.
Disclosures
None.
Supporting information
Data S1
Figures S1–S6
Acknowledgments
We acknowledge Charlotte Greville for their artistic recreation of participant photos.
Supplemental Material for this article are available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.023572
For Sources of Funding and Disclosures, see page 11.
REFERENCES
- 1. Semsarian C, Ingles J, Maron MS, Maron BJ. New perspectives on the prevalence of hypertrophic cardiomyopathy. J Am Coll Cardiol. 2015;65:1249–1254. doi: 10.1016/j.jacc.2015.01.019 [DOI] [PubMed] [Google Scholar]
- 2. Maron BJ, Gardin JM, Flack JM, Gidding SS, Kurosaki TT, Bild DE. Prevalence of hypertrophic cardiomyopathy in a general population of young adults: echocardiographic analysis of 4111 subjects in the CARDIA study. Circulation. 1995;92:785–789. doi: 10.1161/01.CIR.92.4.785 [DOI] [PubMed] [Google Scholar]
- 3. Maron BJ, Ommen SR, Semsarian C, Spirito P, Olivotto I, Maron MS. Hypertrophic cardiomyopathy: present and future, with translation into contemporary cardiovascular medicine. J Am Coll Cardiol. 2014;64:83–99. doi: 10.1016/j.jacc.2014.05.003 [DOI] [PubMed] [Google Scholar]
- 4. Christian S, Somerville M, Giuffre M, Atallah J. Physical activity restriction for children and adolescents diagnosed with an inherited arrhythmia or cardiomyopathy and its impact on body mass index. J Cardiovasc Electrophysiol. 2018;29:1648–1653. doi: 10.1111/jce.13713 [DOI] [PubMed] [Google Scholar]
- 5. Umer A, Kelley GA, Cottrell LE, Giacobbi P, Innes KE, Lilly CL. Childhood obesity and adult cardiovascular disease risk factors: a systematic review with meta‐analysis. BMC Public Health. 2017;17:683. doi: 10.1186/s12889-017-4691-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Reineck E, Rolston B, Bragg‐Gresham JL, Salberg L, Baty L, Kumar S, Wheeler MT, Ashley E, Saberi S, Day SM. Physical activity and other health behaviors in adults with hypertrophic cardiomyopathy. Am J Cardiol. 2013;111:1034–1039. doi: 10.1016/j.amjcard.2012.12.018 [DOI] [PubMed] [Google Scholar]
- 7. Arnett DK, Blumenthal RS, Albert MA, Buroker AB, Goldberger ZD, Hahn EJ, Himmelfarb CD, Khera A, Lloyd‐Jones D, McEvoy JW, et al. 2019 ACC/AHA guideline on the primary prevention of cardiovascular disease: a report of the American College of Cardiology/American Heart Association task force on clinical practice guidelines. Circulation. 2019;140:e596–e646. doi: 10.1161/CIR.0000000000000678 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Kavey RE, Daniels SR, Lauer RM, Atkins DL, Hayman LL, Taubert K. American Heart Association guidelines for primary prevention of atherosclerotic cardiovascular disease beginning in childhood. Circulation. 2003;107:1562–1566. doi: 10.1161/01.CIR.0000061521.15730.6E [DOI] [PubMed] [Google Scholar]
- 9. Gersh BJ, Maron BJ, Bonow RO, Dearani JA, Fifer MA, Link MS, Naidu SS, Nishimura RA, Ommen SR, Rakowski H, et al. 2011 ACCF/AHA guideline for the diagnosis and treatment of hypertrophic cardiomyopathy: a report of the American College of Cardiology Foundation/American Heart Association Task Force on practice guidelines. Circulation. 2011;124:2761–2796. doi: 10.1161/CIR.0b013e318223e230 [DOI] [PubMed] [Google Scholar]
- 10. Bratt EL, Sparud‐Lundin C, Ostman‐Smith I, Axelsson AB. The experience of being diagnosed with hypertrophic cardiomyopathy through family screening in childhood and adolescence. Cardiol Young. 2012;22:528–535. doi: 10.1017/S1047951111002101 [DOI] [PubMed] [Google Scholar]
- 11. Bratt EL, Ostman‐Smith I, Sparud‐Lundin C, Axelsson BA. Parents' experiences of having an asymptomatic child diagnosed with hypertrophic cardiomyopathy through family screening. Cardiol Young. 2011;21:8–14. doi: 10.1017/S1047951110001290 [DOI] [PubMed] [Google Scholar]
- 12. Ommen SR, Mital S, Burke MA, Day SM, Deswal A, Elliott P, Evanovich LL, Hung J, Joglar JA, Kantor P, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy. Circulation. 2020;142:e558–e631. doi: 10.1161/CIR.0000000000000937 [DOI] [PubMed] [Google Scholar]
- 13. McIlvennan CK, Morris MA, Guetterman TC, Matlock DD, Curry L. Qualitative methodology in cardiovascular outcomes research. Circ Cardiovasc Qual Outcomces. 2019;12:e005828. doi: 10.1161/CIRCOUTCOMES.119.005828 [DOI] [PubMed] [Google Scholar]
- 14. Wang C, Burris MA. Photovoice: concept, methodology, and use for participatory needs assessment. Health Educ Behav. 1997;24:369–387. doi: 10.1177/109019819702400309 [DOI] [PubMed] [Google Scholar]
- 15. Valenzuela JM, Vaughn LM, Crosby LE, Strong H, Kissling A, Mitchell MJ. Understanding the experiences of youth living with sickle cell disease: a photovoice pilot. Fam Community Health. 2013;36:97–108. doi: 10.1097/FCH.0b013e318282b2f2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Heath G, Farre A, Shaw K. Parenting a child with chronic illness as they transition into adulthood: a systematic review and thematic synthesis of parents' experiences. Patient Educ Couns. 2017;100:76–92. doi: 10.1016/j.pec.2016.08.011 [DOI] [PubMed] [Google Scholar]
- 17. Thorne SE. Interpretive Description. Walnut Creek, CA: Left Coast Press; 2008. [Google Scholar]
- 18. Mayan MJ. Essentials of Qualitative Inquiry. New York, NY: Routledge; 2016. [Google Scholar]
- 19. Morse JM. Qualitative tokenism. Qual Health Res. 2002;12:729–730. doi: 10.1177/104973230201200601 [DOI] [PubMed] [Google Scholar]
- 20. McKernan C, Montemurro G, Chahal H, Veugelers PJ, Gleddie D, Storey KE. Translation of school‐learned health behaviours into the home: student insights through photovoice. Can J Public Health. 2019;110:821–830. doi: 10.17269/s41997-019-00232-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Jennings D, Lowe J. Photovoice: giving voice to Indigenous youth. Pimatisiwin. 2013;11:521–537. [Google Scholar]
- 22. Genuis SK, Willows N, Alexander First Nation , Jardine C. Through the lens of our cameras: children's lived experience with food security in a Canadian Indigenous community. Child Care Health Dev. 2015;41:600–610. doi: 10.1111/cch.12182 [DOI] [PubMed] [Google Scholar]
- 23. Morse JM. The significance of saturation. Qual Health Res. 1995;5:147–149. doi: 10.1177/104973239500500201 [DOI] [Google Scholar]
- 24. Wang CC. Youth participation in photovoice as a strategy for community change. J Community Prac. 2006;14:147–161. doi: 10.1300/j125v14n01_09 [DOI] [Google Scholar]
- 25. Personal Health Protection Act. SO 2004, c3, Sch A. 2004. Available at: https://canlii.ca/t/552kj. Accessed February 15, 2022.
- 26. Dietitians of Canada, Canadian Paediatric Society, The College of Family Physicians of Canada, Community Health Nurses of Canada . Promoting optimal monitoring of child growth in Canada: using the new WHO growth charts. Can J Diet Pract Res. 2010;71:e1–e3. doi: 10.3148/71.1.2010.54 [DOI] [PubMed] [Google Scholar]
- 27. White PD, Myers MM. The classification of cardiac diagnosis. JAMA. 1921;77:1414–1415. doi: 10.1001/jama.1921.02630440034013 [DOI] [Google Scholar]
- 28. Maykut PS, Morehouse RE. Beginning qualitative research: a philosophic and practical guide. London; Washington, DC: Falmer Press; 1994. [Google Scholar]
- 29. Morse JM. Qualitative generalizability. Qual Health Res. 1999;9:5–6. doi: 10.1177/104973299129121622 [DOI] [Google Scholar]
- 30. International Health Conference . Constitution of the World Health Organization. 1946. Bull World Health Organ. 2002;80:983–984. [PMC free article] [PubMed] [Google Scholar]
- 31. Pelliccia A, Sharma S, Gati S, Bäck M, Börjesson M, Caselli S, Collet J‐P, Corrado D, Drezner JA, Halle M, et al. 2020 ESC guidelines on sports cardiology and exercise in patients with cardiovascular disease. Eur Heart J. 2021;42:17–96. doi: 10.1093/eurheartj/ehaa605 [DOI] [PubMed] [Google Scholar]
- 32. Norrish G, Ding T, Field E, Ziólkowska L, Olivotto I, Limongelli G, Anastasakis A, Weintraub R, Biagini E, Ragni L, et al. Development of a novel risk prediction model for sudden cardiac death in childhood hypertrophic cardiomyopathy (HCM Risk‐Kids). JAMA Cardiol. 2019;4:918–927. doi: 10.1001/jamacardio.2019.2861 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Miron A, Lafreniere‐Roula M, Steve Fan C‐P, Armstrong KR, Dragulescu A, Papaz T, Manlhiot C, Kaufman B, Butts RJ, Gardin L, et al. A validated model for sudden cardiac death risk prediction in pediatric hypertrophic cardiomyopathy. Circulation. 2020;142:217–229. doi: 10.1161/CIRCULATIONAHA.120.047235 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Olsen R, Sutton J. More hassle, more alone: adolescents with diabetes and the role of formal and informal support. Child Care Health Dev. 1998;24:31–39. doi: 10.1046/j.1365-2214.1998.00060.x [DOI] [PubMed] [Google Scholar]
- 35. Miller VA. Parent‐child collaborative decision making for the management of chronic illness: a qualitative analysis. Fam Syst Health. 2009;27:249–266. doi: 10.1037/a0017308 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Shorey S, Ng ED. The lived experiences of children and adolescents with non‐communicable disease: a systematic review of qualitative studies. J Pediatr Nurs. 2020;51:75–84. doi: 10.1016/j.pedn.2019.12.013 [DOI] [PubMed] [Google Scholar]
- 37. La Greca AM, Bearman KJ, Moore H. Peer relations of youth with pediatric conditions and health risks: promoting social support and healthy lifestyles. J Dev Behav Pediatr. 2002;23:271–280. doi: 10.1097/00004703-200208000-00013 [DOI] [PubMed] [Google Scholar]
- 38. Kyngas H, Rissanen M. Support as a crucial predictor of good compliance of adolescents with a chronic disease. J Clin Nurs. 2001;10:767–774. doi: 10.1046/j.1365-2702.2001.00538.x [DOI] [PubMed] [Google Scholar]
- 39. Pate T. Families of children with chronic illness and the relational family model. Pers Chall. 2016;6:57–65. doi: 10.15633/pch.1892 [DOI] [Google Scholar]
- 40. Pearson N, Biddle SJH, Gorely T. Family correlates of fruit and vegetable consumption in children and adolescents: a systematic review. Public Health Nutr. 2009;12:267–283. doi: 10.1017/S1368980008002589 [DOI] [PubMed] [Google Scholar]
- 41. Pearson N, Timperio A, Salmon J, Crawford D, Biddle SJH. Family influences on children's physical activity and fruit and vegetable consumption. In J Behav Nutr Phys. 2009;6:34. doi: 10.1186/1479-5868-6-34 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Sallis JF, Prochaska JJ, Taylor WC. A review of correlates of physical activity of children and adolescents. Med Sci Sports Exerc. 2000;32:963–975. doi: 10.1097/00005768-200005000-00014 [DOI] [PubMed] [Google Scholar]
- 43. Foster BA, Farragher J, Parker P, Sosa ET. Treatment interventions for early childhood obesity: a systematic review. Aad Pediatr. 2015;15:353–361. doi: 10.1016/j.acap.2015.04.037 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Keys EM, Norris JM, Cameron EE, Bright KS, Tomfohr‐Madsen LM, Benzies KM. Recruitment and retention of fathers with young children in early childhood health intervention research: a systematic review and meta‐analysis protocol. Syst Rev. 2019;8:300. doi: 10.1186/s13643-019-1215-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Phares V, Lopez E, Fields S, Kamboukos D, Duhig AM. Are fathers involved in pediatric psychology research and treatment? J Pediatr Psychol. 2005;30:631–643. doi: 10.1093/jpepsy/jsi050 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data S1
Figures S1–S6


