Abstract
Background
Exposure to inhaled smoke, pollutants, volatile organic compounds, and polycyclic aromatic hydrocarbons in the firefighting environment has been associated with detrimental respiratory and cardiovascular effects, making firefighters a unique population with both personal and occupational risk factors for cardiovascular disease. Some of these exposures are also associated with development of atrial fibrillation. We aimed to study the association of atrial fibrillation and occupational exposure in firefighters.
Methods and Results
A cross‐sectional survey was conducted between October 2018 and December 2019. Data were gathered electronically and stored in a secure REDCap database through Louisiana State University Health Shreveport. Firefighters who were members of at least 1 of 5 preselected professional organizations were surveyed via electronic links distributed by the organizations. The survey queried the number of fires fought per year as a measure of occupational exposure, as well as self‐reported cardiovascular disease. A total of 10 860 active firefighters completed the survey, of whom 93.5% were men and 95.5% were aged ≤60 years. Firefighters who fought a higher number of fires per year had a significantly higher prevalence of atrial fibrillation (0–5 fires per year 2%, 6–10 fires per year 2.3%, 11–20 fires per year 2.7%, 21–30 fires per year 3%, 31 or more fires per year 4.5%; P<0.001). Multivariable logistic regression showed that a higher number of fires fought per year was associated with an increased risk of atrial fibrillation (odds ratio 1.14 [95% CI, 1.04–1.25]; P=0.006).
Conclusions
Firefighters may have an increased risk of atrial fibrillation associated with the number of fires they fight per year. Further clinical and translational studies are needed to explore causation and mechanisms.
Keywords: atrial fibrillation, cardiovascular disease, firefighter, risk factors, smoke
Subject Categories: Atrial Fibrillation, Risk Factors, Cerebrovascular Disease/Stroke, Epidemiology
Nonstandard Abbreviations and Acronyms
- FF
fire fighters
- MCP‐1
monocyte chemoattractant protein‐1
- PAI‐1
plasminogen activator inhibitor
- PM
particulate matter
Clinical Perspective
What Is New?
In this survey‐based study of 10 860 firefighters, an increased prevalence of atrial fibrillation was observed among firefighters with increased fire exposure as measured by fires fought per year (0–5 fires per year 2%, 6–10 fires per year 2.3%, 11–20 fires per year 2.7%, 21–30 fires per year 3%, 31 or more fires per year 4.5%; P<0.001).
In a multivariable analysis, fires fought per year was a risk factor for atrial fibrillation (odds ratio 1.14 [95% CI, 1.04–1.25]; P= 0.006).
What Are the Clinical Implications?
The association between atrial fibrillation and fire exposure is cause for concern.
Further studies to elucidate the mechanisms are essential.
Firefighters (FF) are a unique subsection of the population exposed to occupational risk factors for cardiovascular disease (CVD). 1 , 2 , 3 According to the National Fire Protection Association, in 2018 there were 29 705 fire departments with ≈1.1 million FF in the United States who were predominantly men (92%) and primarily composed of volunteer FF (67%) versus career FF (33%). 4 Over 50% of American FF fall in the 30‐ to 49‐year‐old age range. Despite being a younger population, CVD is associated with the greatest proportion of duty‐related fatalities among FF. 5 , 6 The cause of CVD in FF is multifactorial, with obesity, excessive stress, inhalational exposures, and altered circadian rhythms being just a few of the proposed factors. 2 , 3 , 5 , 7 , 8 , 9 , 10
Atrial fibrillation (AF), the most common clinical arrhythmia, affects over 2.2 million Americans and up to 37.5 million people worldwide, increasing their risk of stroke, congestive heart failure, and other cardiac complications. 11 Risk factors for AF, including hypertension, diabetes, coronary artery disease, and alcohol use, are common among FF. 5 , 12 , 13 In addition to these risk factors, FF are exposed to inhaled smoke, particulate matter (PM), polycyclic aromatic hydrocarbons, and volatile organic compounds in the firefighting environment. These exposures have been associated with proinflammatory cytokine release, oxidative stress, endothelial dysfunction, and impairment of autonomic function. 14 , 15 , 16 , 17 , 18 This may serve as a trigger for AF, either directly by causing a proarrhythmic substrate in the atria, or indirectly by contributing to atrial remodeling secondary to other structural heart disease. A prospective study performed by Link et al showed increased odds of AF following PM exposure within the prior 24 hours. 19
Stroke and transient ischemic attack (TIA) are known major complications of AF. CHA2DS2VASc score is used in clinical practice to quantify stroke risk in the setting of an AF diagnosis, and subsequently to guide the discussion of using anticoagulation in these patients. 20 The score ranges from 0 to 9, with 2 or higher denoting moderate–high risk of stroke. This risk stratification tool incorporates the patient’s other risk modifiers such as age, sex, congestive heart failure, diabetes, hypertension, stroke/TIA/thromboembolism, and vascular disease.
The objective of this study was to investigate the association of occupational exposures with AF, stroke/TIA, and other comorbidities in FF. We hypothesized that there would be a positive correlation between prevalence of AF among FF and number of fires fought per year.
Methods
The data supporting the findings of this study are available by emailed request to the corresponding author. Subjects were selected for participation in this study based on their affiliation with one of the following organizations that represent career and/or volunteer FF: International Association of Fire Fighters, National Volunteer Fire Council, National Fallen Firefighter Foundation, International Association of Fire Chiefs, and Secret List. With the help of these organizations, the survey link was distributed to members electronically in an email or on the webpage of the organization. The recipients were provided with information about the study aims and details of participation before completing the survey. Any FF affiliated with the organizations listed above who were aged ≥18 years, active members of the fire service, and completed the survey were included in the study. Institutional review board approval was obtained for the study (LSU Health Shreveport Institutional Review Board, number 00001031), and implied consent was given by the FF based on their acceptance of the information provided to them and their subsequent completion of the survey.
Study participants completed a survey with demographic information, occupational history, cardiac history, and other health history (Figure 1). Attempts were made to recruit non‐FF family members or friends as a control group by asking the FF participants to forward the survey link to them. Despite multiple reminders and an extension of the study period, we were unable to collect enough data from non‐FF to constitute a reasonable control group. Therefore, according to a preplanned protocol, the data collected from FF were stratified by level of exposure to fires for data analysis.
Figure 1. Survey distribution and data collection.
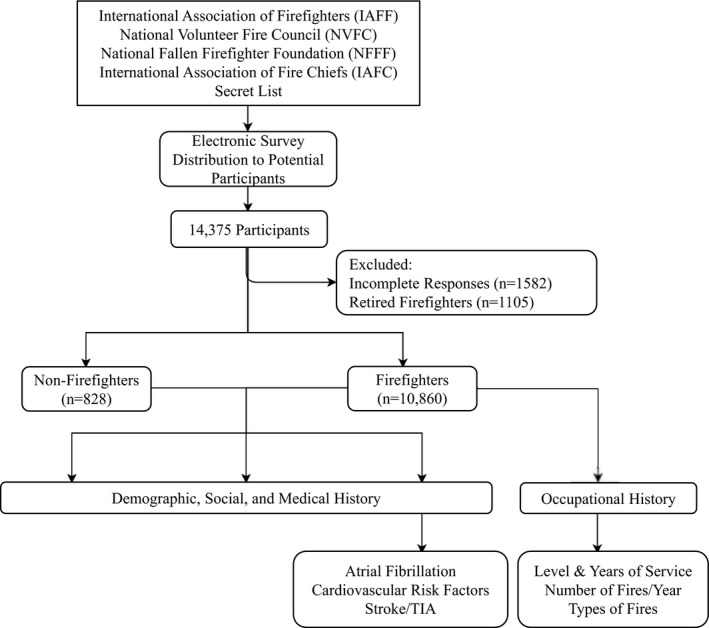
An electronic survey was distributed to firefighter members of 5 professional organizations. There were 14 735 survey responses collected via secure REDCap database. Demographic, social, medical, and occupational history was obtained. Incomplete responses (n=1582) and responses from retired firefighters (n=1105) were excluded. A total of 10 860 responses were included in the statistical analysis. TIA indicates transient ischemic attack.
Statistical Analysis
χ2 test and Fisher exact test were used where appropriate to assess the association between participant characteristics and the presence of AF diagnosis. Multivariable logistic regression was performed to assess the odds of having AF. Covariates included in the AF regression model included known risk factors for AF, specifically: age ≥61 years, male sex, White race, alcohol use, current or prior smoking, secondhand smoke exposure, diabetes mellitus, obstructive sleep apnea, and hypertension. Covariates in the stroke/TIA regression model included: age ≥61 years, male sex, Black race, AF, diabetes mellitus, hypertension, and absence of anticoagulation use. CHA2DS2VASc score was defined by aggregating age, sex, hypertension, diabetes, heart failure, stroke/TIA, and vascular disease history as reported by study respondents. P values <0.05 were considered statistically significant.
Results
Characteristics of Responding Firefighters
A total of 14 375 respondents attempted the questionnaire; 10860 responses were from active (not retired) FF aged >18 years (Figure 1). The remaining responses were from retired FF, non‐FF subjects, or were incomplete responses, and were thus excluded. Among FF, the participants were predominantly men (93.5%), aged ≤60 years (95.5%), and primarily of White, American Indian, or Alaskan Native race (92.2%), as shown in Table S1. Among these, 15.4% of FF had prior military experience. The majority of FF (77.3%) served at the local level, whereas others served at the county (18.2%), state (3.3%), or federal (1.2%) levels of the fire service. The respondents were predominantly career FF (89%). Career firefighters are employed by a city, municipality, or fire district and are paid for their work. They typically work more hours than a volunteer firefighter would, but schedules vary by location. The comorbidities observed and other participant characteristics are listed in Table S1. Self‐reported CVD among FF included AF (2.7%), myocardial infarction (1.7%), coronary artery disease (4.2%), peripheral artery disease (0.5%), and stroke/TIA (0.8%).
AF in Firefighters
Among FF, 2.9% of men and 0.9% women reported diagnoses of AF (P=0.005). Prevalence of AF increased with age. FF aged ≥61 years had a significant increase in AF compared with FF who were aged ≤60 years (8.2% versus 2.5%; P<0.001). The governmental level at which the FF were employed (federal, state, county, or local), the type of employment (career, volunteer, or paid per call), and presence of prior military service had no effect on the prevalence of AF (Table S2).
AF was more prevalent in FF with multiple different medical comorbidities including chronic obstructive pulmonary disease, myocardial infarction, peripheral or carotid artery disease, congestive heart failure, valvular heart disease, diabetes, obstructive sleep apnea, and hypertension (Table 1). Exposure to secondhand smoke was significantly associated with AF compared with FF without secondhand smoke exposure (3.5% versus 2.3%; P<0.001; Table S2).
Table 1.
Prevalence of AF in Firefighters Based on Comorbidities (n=10860)
| Prevalence of AF with comorbidity (%) | Prevalence of AF without comorbidity (%) | P value* | |
|---|---|---|---|
| Risk factors | |||
| Cancer | 55/891 (6.2) | 242/9897 (2.4) | <0.001 |
| Carotid artery disease | 7/35 (20) | 289/10 813 (2.7) | <0.001 |
| Chronic obstructive pulmonary disease | 7/94 (7.4) | 290/10 746 (2.7) | 0.015 |
| Congestive heart failure | 16/50 (32) | 280/10 801 (2.6) | <0.001 |
| Coronary artery disease | 62/456 (13.6) | 233/10 363 (2.2) | <0.001 |
| Diabetes | 20/470 (4.3) | 275/10 367 (2.7) | 0.042 |
| Hypertension | 150/2551 (5.9) | 146/8245 (1.8) | <0.001 |
| Myocardial infarction | 18/189 (9.5) | 277/10 655 (2.6) | <0.001 |
| Obstructive sleep apnea | 93/1660 (5.6) | 196/9024 (2.2) | <0.001 |
| Open heart surgery | 19/102 (18.6) | 279/10 756 (2.6) | <0.001 |
| Peripheral artery disease | 12/58 (20.7) | 283/10 776 (2.6) | <0.001 |
| Stroke/transient ischemic attack | 13/83 (15.7) | 285/10 765 (2.6) | <0.001 |
| Valvular disease | 20/288 (6.9) | 276/10 515 (2.6) | <0.001 |
AF indicates atrial fibrillation.
χ2 test. P<0.05 is considered significant.
Risk of AF and Number of Fires Fought
As shown in Figure 2, the prevalence of AF increased significantly with the increase in the number of fires fought per year (2.01% in FF fighting 0–5 fires per year, 2.28% in FF fighting 6–10 fires per year, 2.75% in FF fighting 11–20 fires per year, 3.01% in FF fighting 21–30 fires per year, and 4.55% in FF fighting ≥31 fires per year; P<0.001). We performed a multivariable analysis to identify risk factors for AF among survey respondents (Table 2). We investigated the occupational risks associated with increased exposure to the firefighting environment by analyzing fires per year by logistic regression. Age, male sex, obstructive sleep apnea, and hypertension were all associated with increased risk of AF (Table 2). Alcohol use in this population, however, was inversely associated with AF risk. An increased number of fires fought per year was associated with an increased risk of AF (odds ratio, 1.14 [95% CI, 1.04–1.25]; P=0.006). The Hosmer‐Lemeshow test was performed for goodness of fit (P=0.365).
Figure 2. Prevalence of atrial fibrillation (AF) and stroke/transient ischemic attack (TIA) in firefighters based on fires fought per year.
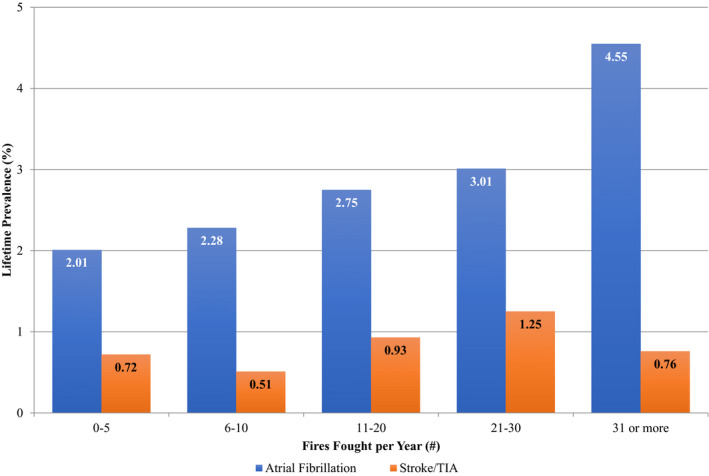
This graph depicts self‐reported prevalence data for AF and stroke/TIA collected from firefighters in the electronic survey. Atrial fibrillation prevalence increases with fires fought per year, whereas stroke/TIA prevalence does not.
Table 2.
Odds of Atrial Fibrillation and Stroke/Transient Ischemic Attack in Firefighters
| Unadjusted, OR (95% CI)* | P value † |
Adjusted OR (95% CI)* |
P value † | |
|---|---|---|---|---|
| Atrial fibrillation | ||||
| Age, y, ≤60 vs ≥61) | 0.28 (0.20–0.40) | <0.001 | 0.50 (0.34–0.73) | <0.001 |
| Sex, men vs women | 3.45 (1.53–7.77) | 0.003 | 2.98 (1.22–7.25) | 0.017 |
| Race, Black § vs White ‡ | 0.78 (0.34–1.79) | 0.555 | 0.68 (0.30–1.57) | 0.858 |
| Race, Asian ‖ vs White ‡ | 0.48 (0.24–0.98) | 0.044 | 0.55 (0.27–1.12) | 0.323 |
| Military service | 0.90 (0.64–1.26) | 0.541 | 0.88 (0.63–1.23) | 0.457 |
| Level of service, county vs state | 1.18 (0.56–2.50) | 0.664 | 1.09 (0.51–2.35) | 0.860 |
| Level of service, federal vs state | 2.04 (0.70–5.88) | 0.189 | 1.35 (0.42–4.31) | 0.619 |
| Level of service, local vs state | 1.23 (0.61–2.50) | 0.555 | 1.09 (0.53–2.26) | 0.852 |
| Alcohol use, yes vs no | 0.60 (0.47–0.77) | <0.001 | 0.68 (0.52–0.89) | 0.004 |
| Smoking, never smoker vs current | 0.76 (0.36–1.64) | 0.495 | 1.03 (0.47–2.25) | 0.646 |
| Smoking, quit vs current | 0.82 (0.37–1.82) | 0.628 | 0.86 (0.38–1.95) | 0.502 |
| Secondhand smoke exposure | 1.56 (1.24–1.96) | <0.001 | 1.23 (0.96–1.57) | 0.095 |
| Diabetes | 1.63 (1.03–2.59) | 0.039 | 0.72 (0.45–1.18) | 0.196 |
| Obstructive sleep apnea | 2.67 (2.08–3.44) | <0.001 | 1.89 (1.44–2.48) | <0.001 |
| Hypertension | 3.47 (2.75–4.37) | <0.001 | 2.75 (2.13–3.53) | <0.001 |
| Fires per year ¶ | 1.14 (1.04–1.25) | 0.006 | ||
| Stroke/transient ischemic attack | ||||
| Age, y, ≤60 vs ≥61 | 0.19 (0.11–0.34) | <0.001 | 0.42 (0.22–0.78) | 0.006 |
| Sex, men vs women) | 1.39 (0.51–3.81) | 0.519 | 1.04 (0.37–2.92) | 0.939 |
| Race, Black § vs White ‡ | 0.47 (0.06–3.33) | 0.449 | 0.46 (0.06–3.34) | 0.577 |
| Race, Asian ‖ vs White ‡ | 0.65 (0.21–2.08) | 0.472 | 0.68 (0.21–2.23) | 0.996 |
| Atrial fibrillation | 4.95 (3.15–7.76) | <0.001 | 3.40 (1.62–7.14) | 0.001 |
| Diabetes | 5.36 (3.08–9.31) | <0.001 | 3.14 (1.72–5.75) | <0.001 |
| Hypertension | 3.69 (2.40–5.70) | <0.001 | 2.33 (1.44–3.76) | 0.001 |
| Anticoagulation use | 9.98 (4.49–22.18) | <0.001 | 2.78 (1.03–7.52) | 0.043 |
| Fires per year ¶ | 1.01 (0.85–1.2) | 0.898 | ||
OR indicates odds ratio.
OR with 95% CI.
P<0.05 is considered significant.
Race includes White/American Indian/Alaskan Native.
Race includes Black/African American.
Race includes Asian/Native Hawaiian/Pacific Islander/Other.
No unadjusted analysis for this variable because it was incorporated as a continuous variable via logistic regression. See Figure 2 for atrial fibrillation and stroke/transient ischemic attack prevalence by fires per year.
Risk of Stroke/TIA and CHA2DS2VASc Score
Only 83 out of 10 860 respondents reported a history of stroke/TIA. Stroke/TIA prevalence did not exhibit a linear relationship with fires fought per year, as shown in Figure 2. In the adjusted multivariable model shown in Table 2, AF, diabetes, hypertension, and anticoagulation use were associated with a statistically significant increased risk of stroke/TIA. Age ≤60 years was associated with decreased risk of stroke/TIA. Fires fought per year did not have a statistically significant impact on risk of stroke/TIA. The Hosmer‐Lemeshow test was performed for goodness of fit (P=0.861). CHA2DS2VASc score for FF with AF exhibited the following breakdown: 36.6% (104/284) with a score of 0, 40.5% (115/284) with a score of 1, 13.0% (37/284) with a score of 2, 4.6% (13/284) with a score of 3, 3.9% (11/284) with a score of 4, and 1.4% (4/284) with a score of 5 or higher.
Discussion
Firefighters represent a unique population with occupational exposure to smoke and other inhaled matter in the firefighting environment, which are known to have a negative impact on pulmonary and cardiovascular health. 1 , 3 , 5 , 7 , 10 , 21 , 22 , 23 , 24 , 25 There are many potential mechanisms by which fire suppression could be associated with increased prevalence of atrial fibrillation. During firefighting, firefighters are exposed to polycyclic aromatic hydrocarbons, PM, benzene, and hydrogen cyanide along with many other compounds. 26 , 27 , 28 , 29 Although respiratory protection is intended to limit exposure to these compounds, firefighters do not always wear respiratory protection before entering a structure, even when smoke levels in the air are high. Furthermore, firefighters may remove their self‐contained breathing apparatus during the overhaul/cleanup phase of firefighting because of the weight and increased heat. 27 , 28 , 29 Dermal absorption is also of concern, because polycyclic aromatic hydrocarbons breakthrough the personal protective clothing, deposit on the skin, and may be absorbed into the body. 26 Research has begun to investigate the magnitude of exposure based on type of fire and fuel load, protective equipment design, and mitigation strategies, but more research is necessary to fully understand the exposure risk of firefighters responding to different types of fires (ie, cars, residential homes with different building construction, industrial) and performing different roles or wearing different personal protective equipment.
Our study shows that there is a statistically significant correlation between increased exposure (based on the number of fires fought per year) and increased prevalence of AF as well as several other cardiac and medical diagnoses. The mechanism for this correlation is almost certainly multifactorial, with stress response, long work hours, inhaled exposure to products of combustion, smoke inhalation, and strong activation of the sympathetic nervous system all playing a role.
Prior studies have demonstrated an increased risk of CVD among FF. CVD has been documented at autopsy in a large fraction of duty‐related deaths in FF, which has been attributed to personal risk factors as well as job‐related factors including exposure to products of combustion, strenuous work, and the sympathetic nervous system activation associated with responding to emergencies. 1 , 3 , 5 , 25 Occupational stress has also been correlated with the development of CVD and sleep disorders in FF in particular. 3 A study of FF with greater exposure to the World Trade Center fires in New York after the September 11, 2001 terrorist attacks demonstrated that they had a 44% increased risk for the primary outcome of the study, which was composed of myocardial infarction, stroke, unstable angina, revascularization, or cardiovascular death. 30 Our findings build on this established knowledge of the clustering of CVD and its risk factors in FF.
This study shows, for the first time, a dose‐dependent relationship between AF and occupational exposure in FF. The prevalence of AF increased incrementally by approximately a half or full percentage point with every additional 5 to 10 fires fought per year. Given the fact that the age of an FF may be directly related to his or her experience and the number of fires fought per year, our multivariable analysis of AF was risk adjusted for age in addition to other common risk factors for AF.
AF risk in FF can be attributed to several proposed mechanisms. Firefighting and exposure to PM have been linked to reduced heart rate variability. 7 , 15 Agarwal et al reported in 2017 that low overall heart rate variability and increased sympathetic‐to‐parasympathetic dominance were independently associated with higher AF risk. 31 Low heart rate variability, coupled with the prominent sympathetic tone found in FF, could increase the prevalence of AF in FF. 21 Systemic inflammation, a finding connected to AF risk, has also been seen in connection with firefighting. FF have been found to have increased monocytes and inflammatory cytokines such as IL‐6 (interleukin‐6), IL‐8 (interleukin‐8), and MCP‐1 (monocyte chemoattractant protein‐1) in their blood after firefighting activities. 9 , 32 Multiple studies have also shown that PM exposure is associated with increased odds of new‐onset AF and AF‐related admissions to the hospital. 19 , 33 , 34 A 2019 study revealed increased ventricular arrhythmias and ST segment changes on electrocardiograms taken within a period of time immediately after firefighting compared with a control period. 35 Exposure to PM can cause mitochondrial dysfunction by increasing mitochondrial permeability transition pore opening and altering calcium regulation, resulting in a favorable atrial substrate for arrhythmias. 36 These direct effects of firefighting and exposure to inhaled matter in the firefighting environment may interact with the personal susceptibilities of individual FF because of background CVD risk factors, which are also increased by some of the same mechanisms, and play a major role in increasing AF risk.
Firefighting has also been associated with an increased risk of thrombogenesis. Firefighting activities increase platelet numbers, platelet activity, coagulation factor VIII, and tissue factor, leading to a net reduction in activated partial thromboplastin time. 37 Moreover, PAI‐1 (plasminogen activator inhibitor‐1), a protein that has been implicated in thrombogenesis, is elevated after FF activities and exposure to PM. 37 , 38 , 39 , 40 Exposure to extreme heat and physical exertion during firefighting is associated with increased platelet monocyte binding and altered endothelial function as illustrated by attenuated flow mediated dilatation. 6 Therefore, we speculated that FF may have a higher prevalence of stroke/TIA, with or without AF. Our analysis of association between fires fought per year and stroke/TIA risk did not reveal a statistically significant correlation, but the hypothesis requires further investigation.
By design, this study is not able to elucidate any causal relationships, but the association between firefighting and AF is striking and merits deeper research. Our findings with regard to AF are consequential particularly because FF are at increased occupational risk of physical injury, making anticoagulation, a cornerstone of medical AF management, more dangerous. Further investigation into the cause of increased AF prevalence in FF is certainly indicated, but these results alone may be a reasonable basis to offer firefighters screening electrocardiograms or other monitoring to identify AF and pursue treatment earlier. Such an intervention may greatly prevent the high‐morbidity sequelae associated with AF, including tachycardia‐ or arrhythmia‐induced cardiomyopathy and TIA or stroke.
Limitations
This study is inherently limited based on the fact that the data on the medical conditions of the subjects are self‐reported, which could introduce reporting bias. Because we do not have access to the subjects’ health records, we are unable to verify the reported diagnoses. Study subjects were recruited by representative organizations, which may have biased the data set toward certain responders. This study design does not account for study subjects who have undiagnosed or asymptomatic AF, but this limitation related to formal diagnosis would be equally present across the entire study group. It is also possible that some study respondents may have retired from active FF duty because of AF or sequelae, which would not have been incorporated into this analysis because retired FF were excluded.
The lack of a robust non‐FF control group may prevent comparison to a wider population; however, this impediment in data collection was anticipated and addressed with a prespecified analysis to using internal comparison of FF based on the number of fires fought. This led to better matching of the unknown or uncollected confounders we could not have adjusted for in the analysis. The small size of the respondents with stroke/TIA history was a limiting factor for that subgroup analysis. A distinction between ischemic and hemorrhagic strokes was not made in the survey, because this detail in a self‐reported survey can be unreliable. In addition, we also did not adjust the stroke risk for CHA2DS2VASc score, because the scoring system includes stroke/TIA, and the cross‐sectional survey model does not provide the ability to ascertain current versus previous stroke.
We believe that the high number of responses from study participants balances the weaknesses of the study design. Furthermore, well‐established risk factors for AF and stroke/TIA were significantly associated in the multivariable analysis, providing internal validation for the quality of data obtained with this study.
Conclusions
Through survey‐based collection of data from over 10 000 respondents, this study has shown that increased prevalence of AF in FF is associated with increased exposure to the firefighting environment. Further research into causal relationships, underlying mechanisms, and risk mitigation strategies is crucial and will lead to a better understanding of cardiovascular risk factors in FF and the ability to protect and care for FF in the line of duty.
Sources of Funding
This publication was supported by an Institutional Development Award from the National Institutes of General Medical Sciences of the National Institutes of Health under grant number P20GM121307 to C. G. Kevil.
Disclosures
None.
Supporting information
Tables S1–S2
Acknowledgments
The authors sincerely thank the International Association of Fire Fighters, National Volunteer Fire Council, National Fallen Firefighter Foundation, International Association of Fire Chiefs, and the Secret List for distributing our electronic survey to their members. We would like to thank M. S. Bass, career firefighter for Bossier City Fire Department in Louisiana, for triggering our interest to study atrial fibrillation in firefighters. We would like to thank Dr. Smith and her associates at Skidmore College for their contributions to the firefighting community and to this study, in particular. We appreciate Dr. Ihsan’s assistance in obtaining institutional review board approval and organizing study team meetings. The authors also thank A. Timboe, who shared his valuable first‐hand experience to help refine the survey content and wording. The authors thank G. Morgan for her assistance in editing this article. Lastly, the authors thank all members of the fire service for their participation in this study and, more importantly, for their magnanimous service to their communities.
Author contributions: C.V. and R.T. were equal contributors to both development and completion of the study and interpretation of the study findings. C.V. jointly conceived the study with D.S. and P. Dominic. P. Dominic served as the principal investigator. A.B. acquired institutional review board approval. C.V. developed the survey in conjunction with D.S., P. Dherange, A.H., and P. Dominic. R.S. and R.T. performed statistical data analysis. All authors contributed to interpretation of the results. C.V., R.T., R.S., and P. Dominic wrote the article with input from all authors. Critical revision of the article for important intellectual content was provided by R.G., B.O., and D.L.S.
This article was sent to N.A. Mark Estes III, MD, Guest Editor, for review by expert referees, editorial decision, and final disposition.
A poster presentation of this work was featured at the American Heart Association Scientific Sessions, November 13–17, 2020.
For Sources of Funding and Disclosures, see page 8.
References
- 1. Soteriades ES, Smith DL, Tsismenakis AJ, Baur DM, Kales SN. Cardiovascular disease in US firefighters. Cardiol Rev. 2011;19: doi: 10.1097/CRD.0b013e318215c105 [DOI] [PubMed] [Google Scholar]
- 2. Karter MJ, Stein GP. US Fire Department Profile. 2013;1–36. [Google Scholar]
- 3. Yook YS. Firefighters’ occupational stress and its correlations with cardiorespiratory fitness, arterial stiffness, heart rate variability, and sleep quality. PLoS One. 2019;14:1–9. doi: 10.1371/journal.pone.0226739 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Evarts B, Stein GP. US Fire Department Profile 2018. NFPA Res. 2020;6. [Google Scholar]
- 5. Smith DL. Firefighter fitness: improving performance and preventing injuries and fatalities. Curr Sports Med Rep. 2011;10:167–172. doi: 10.1249/JSR.0b013e31821a9fec [DOI] [PubMed] [Google Scholar]
- 6. Hunter AL, Shah ASV, Langrish JP, Raftis JB, Lucking AJ, Brittan M, Venkatasubramanian S, Stables CL, Stelzle D, Marshall J, et al. Fire simulation and cardiovascular health in firefighters. Circulation. 2017;135:1284–1295. doi: 10.1161/CIRCULATIONAHA.116.025711 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Andersen MHG, Saber AT, Pedersen PB, Loft S, Hansen ÅM, Koponen IK, Pedersen JE, Ebbehøj N, Nørskov E‐C, Clausen PA, et al. Cardiovascular health effects following exposure of human volunteers during fire extinction exercises. Environ Heal A Glob Access Sci Source. 2017;16. doi: 10.1186/s12940-017-0303-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Rodrigues S, Paiva JS, Dias D, Cunha JPS. Stress among on‐duty firefighters: an ambulatory assessment study. PeerJ. 2018;2018:1–19. doi: 10.7717/peerj.5967 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Dorman SC, Ritz SA. Smoke exposure has transient pulmonary and systemic effects in wildland firefighters. J Respir Med. 2014;2014:1–9. doi: 10.1155/2014/943219 [DOI] [Google Scholar]
- 10. Jahnke SA, Poston WSC, Jitnarin N, Keith Haddock C. Health concerns of the U.S. fire service: perspectives from the firehouse. Am J Heal Promot. 2012;27:111–118. doi: 10.4278/ajhp.110311-QUAL-109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Lippi G, Sanchis‐Gomer F, Cervellin G. Global epidemiology of atrial fibrillation: an increasing epidemic and public health challenge. J Am Coll Cardiol. 2020;1–5. doi: 10.1177/1747493019897870 [DOI] [PubMed] [Google Scholar]
- 12. Khaja SU, Mathias KC, Bode ED, Stewart DF, Jack K, Moffatt SM, Smith DL. Hypertension in the United States fire service. Int J Environ Res Public Health. 2021;18:5432. doi: 10.3390/ijerph18105432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Moffatt SM, Stewart DF, Jack K, Dudar MD, Bode ED, Mathias KC, Smith DL. Cardiometabolic health among United States firefighters by age. Prev Med Rep. 2021;23:101492. doi: 10.1016/j.pmedr.2021.101492. PMID: 34354906; PMCID: PMC8322457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Brook RD, Rajagopalan S, Pope CA, Brook JR, Bhatnagar A, Diez‐Roux AV, Holguin F, Hong Y, Luepker RV, Mittleman MA, et al. Particulate matter air pollution and cardiovascular disease: an update to the scientific statement from the American Heart Association. Circulation. 2010;121:2331–2378. doi: 10.1161/CIR.0b013e3181dbece1 [DOI] [PubMed] [Google Scholar]
- 15. Pope CA, Burnett RT, Thurston GD, Thun MJ, Calle EE, Krewski D, Godleski JJ. Cardiovascular mortality and long‐term exposure to particulate air pollution: epidemiological evidence of general pathophysiological pathways of disease. Circulation. 2004;109:71–77. doi: 10.1161/01.CIR.0000108927.80044.7F [DOI] [PubMed] [Google Scholar]
- 16. Du Y, Xu X, Chu M, Guo Y, Wang J. Air particulate matter and cardiovascular disease: the epidemiological, biomedical and clinical evidence. J Thorac Dis. 2016;8:E8–E19. doi: 10.3978/j.issn.2072-1439.2015.11.37 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Lee BJ, Kim B, Lee K. Air pollution exposure and cardiovascular disease. Toxicol Res. 2014;30:71–75. doi: 10.5487/TR.2014.30.2.071 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Meo SA, Suraya F. Effect of environmental air pollution on cardiovascular diseases. Eur Rev Med Pharmacol Sci. 2015;19:4890–4897. [PubMed] [Google Scholar]
- 19. Link MS, Luttmann‐Gibson H, Schwartz J, Mittleman MA, Wessler B, Gold DR, Dockery DW, Laden F, et al. Acute exposure to air pollution triggers atrial fibrillation. J Am Coll Cardiol. 2013;62:816–825. doi: 10.1016/j.jacc.2013.05.043 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Lip GY, Nieuwlaat R, Pisters R, Lane DA, Crijns HJ. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor‐based approach: the euro heart survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584. Epub 2009 Sep 17 PMID: 19762550 [DOI] [PubMed] [Google Scholar]
- 21. Smith DL, Barr DA, Kales SN. Extreme sacrifice: sudden cardiac death in the US fire service. Extrem Physiol Med. 2013;2:6. doi: 10.1186/2046-7648-2-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Smith DL, Graham E, Stewart D, Mathias KC. Decreased pulmonary function over 5 years in US firefighters. J Occup Environ Med. 2020;62:816–819. doi: 10.1097/JOM.0000000000001944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Fernhall B, Fahs CA, Horn G, Rowland T, Smith D. Acute effects of firefighting on cardiac performance. Eur J Appl Physiol. 2012;112:735–741. doi: 10.1007/s00421-011-2033-x [DOI] [PubMed] [Google Scholar]
- 24. Fahs CA, Yan H, Ranadive S, Rossow LM, Agiovlasitis S, Echols G, Smith D, Horn GP, Rowland T, Lane A, et al. Acute effects of firefighting on arterial stiffness and blood flow. Vasc Med. 2011;16:113–118. doi: 10.1177/1358863X11404940 [DOI] [PubMed] [Google Scholar]
- 25. Smith DL, Haller JM, Korre M, Sampani K, Porto LGG, Fehling PC, Christophi CA, Kales KN. The relation of emergency duties to cardiac death among US firefighters. Am J Cardiol. 2019;123:736–741. doi: 10.1016/j.amjcard.2018.11.049 [DOI] [PubMed] [Google Scholar]
- 26. Mayer AC, Fent KW, Chen IC, Sammons D, Toennis C, Robertson S, Kerber S, Horn GP, Smith DL, Calafat AM, et al. Characterizing exposures to flame retardants, dioxins, and furans among firefighters responding to controlled residential fires. Int J Hyg Environ Health. 2021;236: doi: 10.1016/j.ijheh.2021.113782. PMID: 34119852; PMCID: PMC8325627 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Horn GP, Kerber S, Fent KW, Smith DL. Management of firefighters’ chemical & cardiovascular exposure risks on the fireground. Int Fire Ser J Leadersh Manag. 2020;14:7–16. [PMC free article] [PubMed] [Google Scholar]
- 28. Fent KW, LaGuardia M, Luellen D, McCormick S, Mayer A, Chen IC, Kerber S, Smith D, Horn GP. Flame retardants, dioxins, and furans in air and on firefighters' protective ensembles during controlled residential firefighting. Environ Int. 2020;140: doi: 10.1016/j.envint.2020.105756. PMID: 32388249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haskell WE III. NFPA 1971: Standard on Protective Ensembles for Structural Fire Fighting and Proximity Fire Fighting. 2018.
- 30. Cohen HW, Zeig‐Owens R, Joe C, Hall CB, Webber MP, Weiden MD, Cleven KL, Jaber N, Skerker M, Yip J, et al. Long‐term cardiovascular disease risk among firefighters after the world trade center disaster. JAMA Netw Open. 2019;2:e199775. doi: 10.1001/jamanetworkopen.2019.9775 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Agarwal SK, Norby FL, Whitsel EA, Soliman EZ, Chen LY, Loehr LR, Fuster V, Heiss G, Coresh J, Alonso A, et al. Cardiac autonomic dysfunction and incidence of atrial fibrillation in a large population‐based cohort. J Am Coll Cardiol. 2017;69:291–299. doi: 10.1016/j.jacc.2016.10.059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Swiston JR, Davidson W, Attridge S, Li GT, Brauer M, van Eeden SF. Wood smoke exposure induces a pulmonary and systemic inflammatory response in firefighters. Eur Respir J. 2008;32:129–138. doi: 10.1183/09031936.00097707 [DOI] [PubMed] [Google Scholar]
- 33. Lee HH, Pan SC, Chen BY, Lo SH, Guo YL. Atrial fibrillation hospitalization is associated with exposure to fine particulate air pollutants. Environ Heal A Glob Access Sci Source. 2019;18. doi: 10.1186/s12940-019-0554-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Liu X, Kong D, Liu Y, Fu J, Gao P, Chen T, Fang Q, Cheng K, Fan Z, et al. Effects of the short‐term exposure to ambient air pollution on atrial fibrillation. Pacing Clin Electrophysiol. 2018;41:1441–1446. doi: 10.1111/pace.13500 [DOI] [PubMed] [Google Scholar]
- 35. Smith DL, Horn GP, Fernhall B, Kesler RM, Fent KW, Kerber S, Rowland TW. Electrocardiographic responses following live‐fire firefighting drills. J Occup Environ Med. 2019;61:1030–1035. doi: 10.1097/JOM.0000000000001730 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Xia T, Korge P, Weiss JN, Li N, Venkatesen MR, Sioutas C, Nel A. Quinones and aromatic chemical compounds in particulate matter induce mitochondrial dysfunction: implications for ultrafine particle toxicity. Environ Health Perspect. 2004;112:1347–1358. doi: 10.1289/ehp.7167 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smith DL, Horn GP, Petruzzello SJ, Fahey G, Woods J, Fernhall B. Clotting and fibrinolytic changes after firefighting activities. Med Sci Sports Exerc. 2014;46:448–454. doi: 10.1249/MSS.0b013e3182a76dd2 [DOI] [PubMed] [Google Scholar]
- 38. Cozzi E, Wingard CJ, Cascio WE, Devlin RB, Miles JJ, Bofferding AR, Lust RM, Scott MRV, Henriksen RA. Effect of ambient particulate matter exposure on hemostasis. Transl Res. 2007;149:324–332. doi: 10.1016/j.trsl.2006.12.009 [DOI] [PubMed] [Google Scholar]
- 39. Franchini M, Mannucci PO. Thrombogenicity and cardiovascular effects of ambient air pollution. Blood. 2011;118:2405–2412. doi: 10.1182/blood-2011-04-343111 [DOI] [PubMed] [Google Scholar]
- 40. Shah ASV, Lee KK, McAllister DA, Hunter A, Nair H, Whiteley W, Langrish JP, Newby DE, Miles NL. Short term exposure to air pollution and stroke: systematic review and meta‐analysis. BMJ. 2015. doi: 10.1136/BMJ.h1295 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Tables S1–S2


