Abstract
Background
Patients with atrial fibrillation commonly have complex clinical backgrounds of multimorbidity and polypharmacy. The Atrial Fibrillation Better Care (ABC) pathway has been developed to help deliver integrated and holistic care for patients with atrial fibrillation. In this ancillary analysis, we assessed the adherence to and the effectiveness of the ABC pathway at reducing adverse outcomes in Chinese patients with atrial fibrillation with a complex clinical background of multimorbidity or polypharmacy.
Methods and Results
The ChiOTEAF (Optimal Thromboprophylaxis in Elderly Chinese Patients With Atrial Fibrillation) registry is a prospective, multicenter, nationwide study conducted from October 2014 to December 2018. The primary outcomes of interest were the composite end point of all‐cause death and thromboembolic events, as well as individual end points of all‐cause death, thromboembolic events, and major bleeding. Multimorbidity was defined as the presence of ≥2 comorbidities, and polypharmacy was defined as the concomitant use of ≥5 medications. The eligible cohort included 4644 patients with multimorbidity, of whom 2610 (56.2%) had available data to assess the ABC pathway usage (mean age, 74.4±10.2; 42.8% women). Among patients with polypharmacy (n=2262; mean age, 74.6±10.1; 43.3% women), 1328 (58.7%) had available data to assess the use of the ABC pathway. Adherence to the ABC pathway was associated with a lower risk of the primary composite outcome among patients with multimorbidity (odds ratio, 0.48; 95% CI, 0.29–0.79) and in the polypharmacy group (odds ratio, 0.39; 95% CI, 0.19–0.78). Health‐related quality of life was lower in the non–ABC‐adherent group compared with the ABC‐treated patients.
Conclusions
This nationwide real‐world registry shows that adherence to the ABC pathway is associated with improved clinical outcomes and health‐related quality of life in clinically complex Chinese patients with atrial fibrillation with multimorbidity or polypharmacy.
Keywords: Asia, atrial fibrillation, multimorbidity, polypharmacy, registry
Subject Categories: Atrial Fibrillation, Ischemic Stroke, Aging, Risk Factors
Nonstandard Abbreviations and Acronyms
- ABC
Atrial Fibrillation Better Care
- ChiOTEAF
Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation
- OAC
oral anticoagulant
Clinical Perspective
What Is New?
Adherence to the Atrial Fibrillation Better Care pathway is associated with improved outcomes when managing clinically complex Chinese patients with multimorbidity or polypharmacy.
What Are the Clinical Implications?
Patients with multimorbidity or polypharmacy are considered challenging to manage when associated with atrial fibrillation.
Use of the Atrial Fibrillation Better Care pathway is feasible among these patients and improves clinical outcomes and health‐related quality of life.
This may lead to lower health care costs and mortality rates.
The importance and evident benefits of a well‐rounded holistic and integrated approach to evaluation, characterization, and management of atrial fibrillation (AF) have been emphasized in recent guidelines. 1 , 2 , 3 Standardizing holistic management through protocolization and implementation of framework models can lead to improved patient care. 4 , 5 The Atrial Fibrillation Better Care (ABC) pathway promotes such an integrated approach to AF management 6 : (A) avoid stroke; (B) better symptom control, with patient‐centered symptom‐guided decisions on rate or rhythm control; and (C) cardiovascular risk factor and comorbidity optimization, including lifestyle changes. 7 The ABC pathway offers a systematic approach to AF management that has been shown to be associated with improved clinical outcomes and significantly lower health‐related costs in retrospective and prospective cohorts as well as a prospective randomized trial (mAFA [Mobile Atrial Fibrillation Application]‐II), even in subgroups of clinically complex patients. 8 , 9 , 10 , 11 , 12
Patients with AF often have multiple comorbidities, 13 , 14 which consequently lead to polypharmacy, 15 , 16 , 17 frequent hospital admissions, 18 higher health care costs, 19 and higher mortality rates. 15 , 20 , 21 , 22 , 23 , 24 , 25 These patients are considered challenging to manage in both the community and hospital settings because of such a complex clinical background commonly being associated with AF.
In this ancillary analysis of the contemporary nationwide registry, we assessed the adherence to and the effectiveness of the ABC pathway at reducing the adverse outcomes in Chinese patients with AF with a complex clinical background of multimorbidity or polypharmacy.
Methods
Ethics Approval
This study was performed in line with the principles of the Declaration of Helsinki. Ethics approval was granted by the Central Medical Ethic Committee of Chinese PLA General Hospital (approval No. S2014‐065‐01).
Consent to Participate
Written informed consent was obtained from all individual participants included in the study. Consent for publication was not applicable. Authors are responsible for correctness of the statements provided in the article.
Data Availability Statement
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.
The ChiOTEAF (Optimal Thromboprophylaxis in Elderly Chinese Patients With Atrial Fibrillation) is a prospective cohort study. The protocol of the ChioTEAF registry, the method of implementation of the ABC pathway, and the characteristics of patients with multimorbidity and polypharmacy have been previously described. 26 , 27 , 28 The study was conducted between October 2014 and December 2018 at 44 sites in 20 Chinese provinces. The study enrolled consecutive patients with AF (with a documented AF episode within 12 months before enrollment) presenting to cardiology, neurology, or surgical services. Follow‐up visits were performed at 6 and 12 months and thereafter annually for the next 2 years. Data were gathered by the local investigators at the point of enrollment and during follow‐up visits (face‐to‐face follow‐up and/or telephone follow‐up and/or chart review).
Multimorbidity was defined as the presence of ≥2 comorbidities (in addition to AF) at enrollment. 29 , 30 Polypharmacy was defined as the concomitant use of ≥5 medications (regardless of the reasons and utility) at enrollment. 31
The participants were assessed against the ABC pathway criteria according to its original definition: patients qualified for the “A” criterion if they were treated with oral anticoagulants (OACs) according to their thromboembolic risk; the “B” criterion if they demonstrated optimal symptom control defined as European Heart Rhythm Association score of I (no symptoms) or II (mild symptoms) at baseline; “C” criterion if they received disease‑specific treatment(s) according to current guidelines at baseline. Patients were considered as ABC adherent if they fulfilled all 3 criteria (A+B+C).
Other variables were defined in line with the EORP‐AF (EURObservational Research Programme Atrial Fibrillation) long‐term general registry 32 protocol. The CHA2DS2‐VASc score 33 and the HAS‐BLED bleeding score 34 were used to assess the thromboembolic and bleeding risks. Bleeding events (intracranial and extracranial haemorrhages) were categorized on the basis of the International Society on Thrombosis and Haemostasis definition. 35 The EuroQol 5 dimensions questionnaire (EQ‐5D‐5L) 36 was used to assess the patient‐reported quality of life.
Objectives
The primary objective of the present analysis was to evaluate the impact of ABC pathway adherence on the clinical outcomes among patients with multimorbidity and patients with polypharmacy at 1 year of follow‐up. The primary outcomes of interest were the composite end point of all‐cause death and thromboembolic events (ischemic stroke, transient ischemic attack, or peripheral embolism), as well as individual end points of all‐cause death, thromboembolic events, and major bleeding. The secondary objectives included (1) identifying the potential predictors of the compliance with the ABC pathway among multimorbid patients with AF; (2) evaluating the impact of the ABC pathway on clinical outcomes among the subgroup of patients with concomitant multimorbidity and polypharmacy; and (3) evaluating the impact of the ABC pathway on clinical outcomes among the overall multimorbidity and polypharmacy cohorts, that is, comparing ABC‐adherent patients with multimorbidity or polypharmacy with all other patients with multimorbidity or polypharmacy, respectively, regardless of the availability of the ABC pathway usage data.
Statistical Analysis
Continuous variables were reported as mean± SD; between‐group comparisons were made using Student’s t test or the Mann‐Whitney U test (based on distribution). Categorical variables were reported as counts and percentages; between‐group comparisons were made by the χ2 test. The quality of life was assessed on the basis of the EuroQol summary index (range, 0–1; a score of 1 indicating the best health state) estimated from the EuroQol 5 dimensions questionnaire value set for China. 37 Logistic regression analysis was performed to assess the age‐adjusted associations between the ABC compliance and clinical outcomes (composite outcome of all‐cause death/any thromboembolic, all‐cause death, thromboembolic events, and major bleeding) among patients with AF with (1) multimorbidity and (2) polypharmacy. For the secondary objectives, a logistic univariate regression analysis was used to identify the predictors of ABC compliance in the multimorbidity group. All the significant variables were included in a multivariate regression model. Finally, sensitivity analysis was performed for (1) patients with AF with both multimorbidity and polypharmacy, (2) the overall multimorbidity cohort, and (3) the overall polypharmacy cohort. Results were expressed as odds ratio (OR) with 95% CI. In all analyses, a P value <0.05 was considered statistically significant. Statistical analysis was performed using SPSS version 24 (IBM Corp., Armonk, NY).
Results
The ChiOTEAF registry enrolled 7077 patients, of whom 657 (9.3%) were lost to follow‐up at 1 year (Figure 1). Among patients with multimorbidity (n=4644), 2610 (56.2%) had available data to assess ABC pathway usage (mean age, 74.4±10.2; 42.8% women). Among patients with polypharmacy (n=2262), 1328 (58.7%) had available data to assess the use of the ABC pathway (mean age, 74.6±10.1; 43.3% women).
Figure 1. Flowchart of patient inclusion.
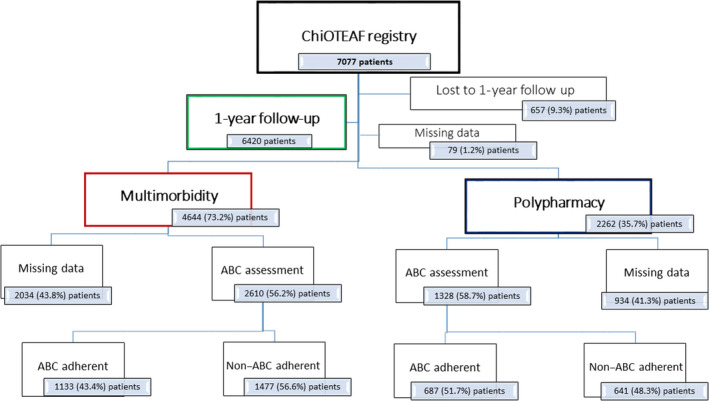
ABC indicates Atrial Fibrillation Better Care; and ChiOTEAF, Optimal Thromboprophylaxis in Elderly Chinese Patients With Atrial Fibrillation.
Multimorbidity Subgroup
Of the multimorbidity cohort, 1133 of 2610 (43.4%) patients were managed in accordance with the ABC pathway. Multimorbid patients with AF treated according to the ABC pathway were younger (mean age, 72.8±10.1 versus 75.7±10.1; P<0.001), with a lower proportion of patients with a first diagnosis of AF (13.7% versus 19.8%; P<0.001), coronary artery disease (54.9% versus 67.6%; P<0.001), and heart failure (39.6% versus 44.4%; P=0.014), compared with the non‐ABC group. Antiplatelet agents were used in 63.8% and OACs in 11.6% of patients in the non‐ABC group. Health‐related quality of life was lower in the non–ABC‐adherent group (mean EuroQol, 0.81±0.19 versus 0.84±0.17; P<0.001) compared with the ABC‐managed patients. Baseline characteristics are reported in Table 1.
Table 1.
Baseline Characteristics of the Study Cohort
|
Total multimorbidity n=2610 n (%) |
ABC group n=1133 n (%) |
Non‐ABC group n=1477 n (%) |
P value |
Total polypharmacy n=1328 n (%) |
ABC group n=687 n (%) |
Non‐ABC group n=641 n (%) |
P value | |
|---|---|---|---|---|---|---|---|---|
| Age, y* | 74.4±10.2 | 72.8±10.1 | 75.7±10.1 | <0.001 | 74.6±10.1 | 72.9±10.1 | 76.5±9.7 | <0.001 |
| Female sex | 1116 (42.8) | 497 (43.9) | 619 (41.9) | 0.317 | 575 (43.3) | 305 (44.4) | 270 (42.1) | 0.403 |
| BMI, kg/m2 * | 24.4±3.7 | 24.6±3.8 | 24.2±3.6 | 0.005 | 24.7±3.5 | 24.8±3.5 | 24.5±3.6 | 0.109 |
| First diagnosed AF | 433 (17.1) | 150 (13.7) | 283 (19.8) | <0.001 | 247 (19.1) | 102 (15.2) | 145 (23.3) | <0.001 |
| Medical history | ||||||||
| Diabetes | 879 (33.7) | 386 (34.1) | 493 (33.4) | 0.711 | 530 (39.2) | 267 (38.9) | 253 (39.5) | 0.821 |
| Hypertension | 1951 (74.8) | 901 (79.5) | 1050 (71.1) | <0.001 | 1022 (77.0) | 544 (79.2) | 478 (74.6) | 0.046 |
| Heart failure | 1105 (42.3) | 449 (39.6) | 656 (44.4) | 0.014 | 606 (45.6) | 291 (42.4) | 315 (49.1) | 0.013 |
| Coronary artery disease | 1620 (62.1) | 622 (54.9) | 998 (67.6) | <0.001 | 870 (65.5) | 399 (58.1) | 471 (73.5) | <0.001 |
| Liver disease | 116 (4.4) | 43 (3.8) | 73 (4.9) | 0.159 | 45 (3.4) | 25 (3.6) | 20 (3.1) | 0.602 |
| Lipid disorder | 1617 (62.0) | 757 (66.8) | 869 (58.2) | <0.001 | 846 (63.7) | 449 (65.4) | 397 (61.9) | 0.195 |
| Prior ischemic stroke | 766 (29.3) | 346 (30.5) | 420 (28.4) | 0.242 | 367 (27.6) | 197 (28.7) | 170 (26.5) | 0.380 |
| Chronic kidney disease | 325 (12.5) | 105 (9.3) | 220 (14.9) | <0.001 | 160 (12.0) | 65 (9.5) | 95 (14.8) | 0.003 |
| COPD | 249 (9.5) | 79 (7.0) | 170 (11.5) | <0.001 | 113 (8.5) | 48 (7.0) | 65 (10.1) | 0.040 |
| Sleep apnea | 114 (4.4) | 55 (4.9) | 59 (4.0) | 0.287 | 57 (4.3) | 34 (4.9) | 23 (3.6) | 0.221 |
| Dementia | 61 (2.3) | 15 (1.3) | 46 (3.1) | 0.003 | 23 (1.7) | 7 (1.0) | 16 (2.5) | 0.039 |
| Prior major bleeding | 88 (3.4) | 7 (0.6) | 81 (5.5) | <0.001 | 33 (2.5) | 3 (0.4) | 30 (4.7) | <0.001 |
| CHA2DS2VASc* | 3.9±1.6 | 3.9±1.6 | 3.9±1.6 | 0.743 | 4.1±1.6 | 4.0±1.6 | 4.1±1.7 | 0.142 |
| HAS‐BLED* | 2.3±1.1 | 2.1±1.1 | 2.4±1.1 | <0.001 | 2.4±1.1 | 2.2±1.0 | 2.6±1.1 | <0.001 |
| Medications | ||||||||
| OAC | 1291 (49.5) | 1119 (98.8) | 172 (11.6) | <0.001 | 740 (55.7) | 686 (99.9) | 54 (8.4) | <0.001 |
| VKA | 595 (22.8) | 517 (45.6) | 78 (5.3) | <0.001 | 348 (26.2) | 318 (46.3) | 30 (4.7) | <0.001 |
| DOAC | 695 (26.6) | 602 (53.1) | 93 (6.3) | <0.001 | 391 (29.4) | 368 (53.6) | 23 (3.6) | 0.010 |
| Antiplatelet | 1174 (45.0) | 232 (20.5) | 942 (63.8) | <0.001 | 761 (57.3) | 200 (29.1) | 561 (87.5) | <0.001 |
| Aspirin (n=2609) | 869 (33.3) | 174 (15.4) | 695 (47.1) | <0.001 | 567 (42.7) | 147 (21.4) | 420 (65.6) | <0.001 |
| Clopidogrel (n=2609) | 557 (21.3) | 90 (7.9) | 467 (31.6) | <0.001 | 370 (27.9) | 78 (11.4) | 292 (45.7) | <0.001 |
|
Ticagrelor (n=2609) |
10 (0.4) | 3 (0.3) | 7 (0.5) | 0.391 | 7 (0.5) | 1 (0.1) | 6 (0.9) | 0.047 |
|
Dual antiplatelet (n=2608) |
283 (10.9) | 39 (3.4) | 244 (16.5) | <0.001 | 198 (14.9) | 31 (4.5) | 167 (26.2) | <0.001 |
| OAC+antiplatelet | 245 (9.4) | 220 (19.4) | 25 (1.7) | <0.001 | 216 (16.3) | 199 (29.0) | 17 (2.7) | <0.001 |
| Digoxin | 279 (10.7) | 117 (10.3) | 162 (11.0) | 0.599 | 242 (18.2) | 114 (16.6) | 128 (20.0) | 0.111 |
| β‐blockers | 1558 (59.7) | 732 (64.6) | 826 (55.9) | <0.001 | 1030 (77.6) | 526 (76.6) | 504 (78.6) | 0.368 |
| Amiodarone | 439 (16.8) | 249 (22.0) | 190 (12.9) | <0.001 | 299 (22.5) | 195 (28.4) | 104 (16.2) | <0.001 |
| Propafenone | 122 (4.7) | 50 (4.4) | 72 (4.9) | 0.580 | 59 (4.4) | 31 (4.5) | 28 (4.4) | 0.899 |
| ACE‐I | 470 (18.0) | 240 (21.2) | 230 (15.6) | <0.001 | 344 (25.9) | 189 (27.5) | 155 (24.2) | 0.166 |
| ARB | 732 (28.0) | 396 (35.0) | 336 (22.7) | <0.001 | 541 (40.7) | 301 (43.8) | 240 (37.4) | 0.018 |
| Calcium channel blockers | 736 (28.2) | 313 (27.6) | 423 (28.6) | 0.569 | 524 (39.5) | 256 (37.3) | 268 (41.8) | 0.090 |
| Diuretics | 838 (32.1) | 350 (30.9) | 488 (33.0) | 0.244 | 634 (47.7) | 292 (42.5) | 342 (53.4) | <0.001 |
| Statins | 1820 (69.7) | 852 (75.2) | 968 (65.5) | <0.001 | 1123 (84.6) | 574 (83.6) | 549 (85.6) | 0.291 |
| Insulin | 232 (8.9) | 96 (8.5) | 136 (9.2) | 0.513 | 181 (13.6) | 85 (12.4) | 96 (15.0) | 0.167 |
| Sulfonylureas | 158 (6.1) | 90 (7.9) | 68 (4.6) | <0.001 | 126 (9.5) | 75 (10.9) | 51 (8.0) | 0.066 |
| Biguanide | 234 (9.0) | 133 (11.7) | 101 (6.8) | <0.001 | 191 (14.4) | 119 (17.3) | 72 (11.2) | 0.002 |
| Nitrates | 798 (30.6) | 305 (26.9) | 493 (33.4) | <0.001 | 638 (48.0) | 264 (38.4) | 374 (58.3) | <0.001 |
| Polypharmacy | 1203 (46.1) | 621 (54.8) | 582 (39.4) | <0.001 | … | … | … | |
| Quality of life | ||||||||
| EHRA score* | 1.61±0.53 | 1.58±0.49 | 1.63±0.55 | 0.016 | 1.62±0.53 | 1.57±0.49 | 1.66±0.56 | 0.003 |
| EQ index* | 0.83±0.18 | 0.84±0.17 | 0.81±0.19 | <0.001 | 0.82±0.19 | 0.83±0.18 | 0.80±0.20 | 0.017 |
| AF management | ||||||||
| OAC persistence at 12‐mo (n=2559) | 1119 (43.7) | 854 (76.2) | 265 (18.4) | <0.001 | 633 (48.5) | 539 (79.3) | 94 (15.0) | <0.001 |
|
AF ablation (n=2608) |
304 (11.7) | 212 (18.7) | 92 (6.2) | <0.001 | 150 (11.3) | 125 (18.2) | 25 (3.9) | <0.001 |
|
CIED (n=2608) |
250 (9.6) | 91 (8.0) | 159 (10.8) | 0.019 | 123 (9.3) | 55 (8.0) | 68 (10.6) | 0.100 |
ABC, indicates Atrial Fibrillation Better Care; ACE‐I, angiotensin‐converting enzyme inhibitor; AF, atrial fibrillation; ARB, angiotensin II receptor blocker; BMI, body mass index; CIED, cardiac implantable electronic device; COPD, chronic obstructive pulmonary disease; DOAC, direct‐acting oral anticoagulant; EHRA, European Heart Rhythm Association; EQ, EuroQoL; OAC, oral anticoagulation; and VKA, vitamin K antagonist.
Mean±SD.
Clinical Outcomes
Among multimorbid patients with AF managed according to the ABC pathway, a lower incidence of the composite outcome (1.8% versus 4.7%; P<0.001), all‐cause death (1.1% versus 3.2%; P=0.001), and thromboembolic events (0.7% versus 1.6%; P=0.034) was observed compared with the non‐ABC group. ORs of the composite outcome (0.48; 95% CI, 0.29–0.79) and all‐cause death (0.51; 95% CI, 0.27–0.95) were lower in the ABC‐managed patients. No statistically significant differences were reported in major bleeding between the groups (Table 2).
Table 2.
Effects of ABC Compliance on Clinical Outcomes Among Patients With Multimorbidity
| Outcomes |
ABC n=1133 n (%) |
Non‐ABC n=1477 n (%) |
P value* |
Odds ratio † (95% CI) |
|---|---|---|---|---|
| Composite outcome ‡ | 20 (1.8) | 69 (4.7) | <0.001 | 0.48 (0.29–0.79) |
| All‐cause death | 13 (1.1) | 47 (3.2) | 0.001 | 0.51 (0.27–0.95) |
| Thromboembolism events | 8 (0.7) | 24 (1.6) | 0.034 | 0.48 (0.22–1.09) |
| Major bleeding | 13 (1.1) | 16 (1.1) | 0.885 | 1.28 (0.61–2.70) |
ABC indicates Atrial Fibrillation Better Care.
Between‐group comparison made by χ2 test.
Adjusted for age.
Composite outcome of all‐cause death/any thromboembolism.
Predictors of ABC Compliance
A multivariate analysis showed that (1) older age (OR, 0.98; 95% CI, 0.97–0.99), coronary artery disease (OR, 0.55; 95% CI, 0.46–0.65), prior major bleeding (OR, 0.14; 95% CI, 0.06–0.29), chronic kidney disease (OR, 0.66; 95% CI, 0.51–0.86), and chronic obstructive pulmonary disease (OR, 0.71; 95% CI, 0.53–0.96) were the independent predictors of poor compliance with the ABC pathway; while (2) hypertension (OR, 1.50; 95% CI, 1.23–1.82) and polypharmacy (OR, 2.15; 95% CI, 1.81–2.55) were associated with a better adherence to the ABC pathway among the patients with multimorbidity (Figure 2; Table S1).
Figure 2. Predictors of the ABC compliance among patients with atrial fibrillation and multimorbidity.
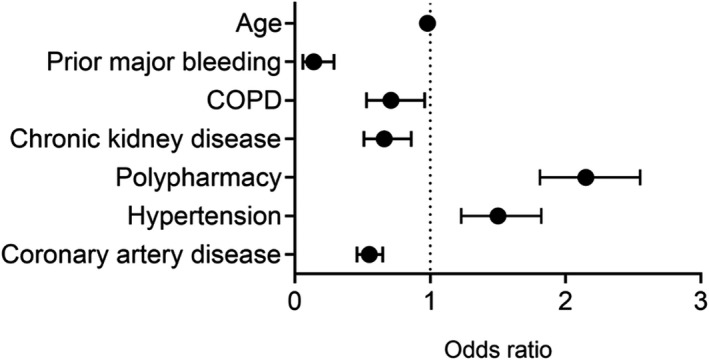
ABC indicates Atrial Fibrillation Better Care; and COPD, chronic obstructive pulmonary disease.
Polypharmacy Subgroup
Among patients with polypharmacy 687 of 1328 (51.7%) were managed according to the ABC pathway. Baseline characteristics are reported in Table 1.
Patients in the ABC group were younger (mean age, 72.9±10.1 versus 76.5±9.7; P<0.001), with a higher proportion of patients with hypertension (79.2% versus 74.6%; P=0.046), and lower HAS‐BLED score (2.2±1.0 versus 2.6±1.1; P<0.001) compared with the non‐ABC group. As expected, differences in the use of OACs were evident between groups, including direct OACs to be favored over vitamin K antagonists (53.6% versus 46.3%) in the ABC group; antiplatelet agents were used in 87.5% and OACs in 8.4% of patients in the non‐ABC group. The use of the rhythm control strategies including amiodarone (28.4% versus 16.2; P<0.001) and AF ablation (18.2% versus 3.9%; P<0.001) were more prevalent in the ABC‐adherent group. Health‐related quality of life was lower in the non–ABC‐adherent group (mean EuroQol, 0.83±0.18 versus 0.80±0.20; P=0.017) compared with the ABC‐managed patients.
Clinical Outcomes
Among the patients with AF with polypharmacy managed according to the ABC pathway, a lower incidence of the composite outcome (1.6% versus 5.1%; P<0.001), all‐cause death (1.2% versus 3.1%; P=0.013), and thromboembolic events (0.6% versus 2.3%; P=0.007) was observed compared with the non‐ABC group. ORs of the composite outcome (0.39; 95% CI, 0.19–0.78) and thromboembolic events (0.31; 95% CI, 0.10–0.95) were lower in the ABC‐managed patients. No significant differences were reported in the incidence of major bleeding between groups (Table 3).
Table 3.
Effects of ABC Compliance on Clinical Outcomes Among Patients With Polypharmacy
| Outcomes |
ABC n=687 n (%) |
Non‐ABC n=641 n (%) |
P value* |
Odds ratio † (95% CI) |
|---|---|---|---|---|
| Composite outcome ‡ | 11 (1.6) | 33 (5.1) | <0.001 | 0.39 (0.19–0.78) |
| All‐cause death | 8 (1.2) | 20 (3.1) | 0.013 | 0.48 (0.21–1.12) |
| Thromboembolic events | 4 (0.6) | 15 (2.3) | 0.007 | 0.31 (0.10–0.95) |
| Major bleeding | 10 (1.5) | 6 (0.9) | 0.388 | 2.02 (0.72–5.69) |
ABC indicates Atrial Fibrillation Better Care.
Between‐group comparison made by χ2 test.
Adjusted for age.
Composite outcome of all‐cause death/any thromboembolism.
Exploratory Analysis
A subgroup of 1203 patients had both multimorbidity and polypharmacy; among these, 621 (51.6%) were managed according to the ABC pathway. Among patients managed according to the ABC pathway, a lower incidence of the composite outcome (1.6% versus 5.3%; P<0.001), all‐cause death (1.1% versus 3.1%; P=0.017), and thromboembolic events (0.6% versus 2.6%; P=0.007) was observed compared with the non‐ABC group. ORs of the composite outcome (0.38; 95% CI, 0.18–0.79) and thromboembolic events (0.31; 95% CI, 0.10–0.94) were lower in the ABC‐adherent patients. Nonsignificant differences were reported in major bleeding (Table S2).
We performed an additional analysis for patients with AF with multimorbidity managed according to the ABC pathway compared with the overall multimorbidity cohort regardless of the availability of the ABC data (Table S3). Among the ABC‐adherent group, a lower incidence of the composite outcome (1.8% versus 12.6%; P<0.001), all‐cause death (1.1% versus 10.7%; P<0.001), thromboembolic events (0.7% versus 2.4%; P<0.001), and major bleeding (1.1% versus 2.2%; P<0.001) was observed. The ABC pathway was associated with lower ORs for the composite outcome (0.19; 95% CI, 0.12–0.30), all‐cause death (0.15; 95% CI, 0.09–0.27), and thromboembolic events (0.39; 95% CI, 0.19–0.83). Analogous exploratory analysis was performed for the overall polypharmacy cohort (Table S4). ABC pathway compliance was associated with lower ORs for the composite outcome (0.19; 95% CI, 0.10–0.36), all‐cause death (0.18; 95% CI, 0.09–0.37), and thromboembolic events (0.35; 95% CI, 0.12–0.99) among the patients with AF with polypharmacy.
Discussion
To date, the implementation of the ABC pathway and its impact on management and clinical outcomes (including health‐related quality of life) among clinically complex Asian patients with AF are scarce. Herein, we demonstrate the following principal findings on the effects of usage of the ABC pathway in patients with AF with multimorbidity or polypharmacy: (1) Adherence to the ABC pathway was associated with improved clinical outcomes among complex AF patients; (2) various clinical predictors were independently associated with ABC adherence among multimorbidity patients; and (3) health‐related quality of life was lower in the non–ABC‐adherent group compared with the ABC‐managed patients.
Our results are comparable to the results of the post hoc ancillary analysis from the AFFIRM (Atrial Fibrillation Follow‐Up Investigation of Rhythm Management) trial (conducted over 2 decades ago), which showed that adherence to the ABC pathway in patients with multimorbidity, polypharmacy, and multiple hospitalizations was associated with a significantly lower cumulative risk of the composite outcome of all‐cause hospitalization and all‐cause death. 10 Our analysis adds to these findings by demonstrating that better clinical outcomes are observed in a contemporary cohort of Chinese patients with AF with both multimorbidity and polypharmacy who adhere to the ABC pathway.
Patients who received ABC management were more likely to be younger, less likely to have been diagnosed with AF for the first time, and have existing coronary artery disease or heart failure compared with those who did not receive ABC management. Likewise, multimorbidity and polypharmacy were associated with a preferential use of direct OACs in favor of vitamin K antagonists in those following the ABC pathway. Although the rhythm management strategies were scarcely used in the ChiOTEAF population, 38 they were more readily used in the ABC arm compared with the non‐ABC arm. Furthermore, the use of the ABC pathway was associated with better health‐related quality of life.
Consequently, adherence to the ABC pathway was associated with statistically lower rates of the composite outcome, all‐cause mortality, and thromboembolic events in patients with AF with multimorbidity or polypharmacy and those with both multimorbidity and polypharmacy. There was no evidence to suggest that adhering to the ABC pathway was associated with a higher risk of major bleeding events compared with standard practice in any of the subgroups studied; indeed, when compared with the overall multimorbidity group, the bleeding risks were significantly lower in the ABC‐managed multimorbidity group.
However, special attention should be paid to those with coronary artery disease, prior major bleeding, chronic kidney disease, and chronic obstructive pulmonary disease. Indeed, these comorbidities independently predict lower adherence to the ABC pathway. Prior major bleeding should not be a reason to withhold OAC, but mitigation of modifiable bleeding risks and regular review and follow‐up of patients with high bleeding risk is required. 39 , 40 , 41 In our previous report, we demonstrated the efficacy of guideline‐adherent OAC therapy among the elderly Chinese patients with AF. 42 , 43
Favorable effects of the use of the ABC pathway are evident across various geographic regions, as various large‐scale studies have demonstrated improvement in survival rates and reduction in cardiovascular events as a result of the ABC pathway implementation. 8 , 10 , 44 The mAFA‐II trial, a cluster randomized trial, showed that the use of the ABC pathway was associated with a significantly lower risk of the composite outcome of stroke/thromboembolism, mortality, bleeding, and hospitalization compared with the usual care, 9 while the analysis of the long‐term extension cohort demonstrated good adherence and persistence of use. 45 Of note, the ABC pathway is now recommended in international AF guidelines. 1 , 3
Ongoing research demonstrates reproducible and generalizable results from systematic implementation of the ABC pathway are needed to address and help reduce nonadherence among physicians and patients alike. 46 We believe our study complements the existing knowledge base on the role and the utility of the ABC pathway in managing clinically complex patients by helping us further define its effectiveness and safety profile, particularly the noninferiority of the approach with regard to bleeding risk compared with standard practice.
Limitations
The primary limitation of the ChiOTEAF registry is its observational nature; the study was not designed to assess the role of the ABC pathway adherent care on patients’ prognosis. ABC pathway adherence was assessed retrospectively on the basis of its definition published in 2017 7 and implemented into the 2020 European Society of Cardiology guideline. 1 We found that a moderate proportion of patients were lost to follow‐up (9.3%), consistent with other large registries 47 ; because of the limited availability of the data, only 56.2% of patients with multimorbidity and 58.7% of patients with polypharmacy were included in this analysis. To an extent, the observed associations of the ABC pathway with favorable clinical outcomes could have potentially been the result of patient self‐selection rather than causal impact. Additionally, the data on ABC pathway adherence was available in only approximately half of the patients studied, which might have been a potential source of bias. Furthermore, the number of adverse clinical events, as well as AF‐related procedures, may have been underreported. We did not report time‐to‐event data, and our outcomes were based on logistic regression. While competing risks of death may potentially impact on outcomes, our primary analysis focused on the OR of the composite outcome at 1 year. Finally, the data on anticoagulation monitoring and the use of traditional Chinese medicines were not available and could not be considered in the analysis.
Conclusions
This nationwide real‐world registry shows that adherence to the ABC pathway is associated with improved clinical outcomes and health‐related quality of life in clinically complex Chinese patients with AF with multimorbidity or polypharmacy.
Sources of Funding
The study was supported by Beijing Natural Science Foundation, China (Z141100002114050), and Chinese Military Health Care (17BJZ08).
Disclosures
Dr Lip is a consultant and speaker for BMS/Pfizer, Boehringer Ingelheim, and Daiichi‐Sankyo. No fees are received personally. The remaining authors have no disclosures to report.
Supporting information
Appendix S1
Tables S1–S4
Acknowledgments
The authors thank all the participants into the ChiOTEAF for their contributions and the National Institute for Health Research Global Health Research Group on Atrial Fibrillation Management for the technical support and peer interactive communication. Dr Lip is co–principal investigator of the Atrial Fibrillation integrated approach in FraIl, multimoRbid and polyMedicated Older people project on multimorbidity in AF, which has received funding from the European Union’s Horizon 2020 research and innovation program under grant agreement No. 899871. All authors made a significant contribution and read and approved the final draft. Drs Kotalczyk and Guo designed the study, interpreted data, and drafted the manuscript (joint first authors); M. Stefil drafted the manuscript; Drs Wang and Lip contributed to the interpretation of data and revised the manuscript critically for important intellectual content (joint senior authors).
Supplemental Material for this article is available at https://www.ahajournals.org/doi/suppl/10.1161/JAHA.121.024319
For Sources of Funding and Disclosures, see page 9.
Contributor Information
Yutang Wang, Email: wyt301@yeah.net.
Gregory Y. H. Lip, Email: gregory.lip@liverpool.ac.uk.
References
- 1. Hindricks G, Potpara T, Dagres N, Arbelo E, Bax JJ, Blomström‐Lundqvist C, Boriani G, Castella M, Dan G‐A, Dilaveris PE, et al. 2020 ESC Guidelines for the diagnosis and management of atrial fibrillation developed in collaboration with the European Association for Cardio‐Thoracic Surgery (EACTS). Eur Heart J. 2021;42:373–498. doi: 10.1093/eurheartj/ehaa612 [DOI] [PubMed] [Google Scholar]
- 2. Potpara TS, Lip GYH, Blomstrom‐Lundqvist C, Boriani G, Van Gelder IC, Heidbuchel H, Hindricks G, Camm AJ. The 4S‐AF scheme (stroke risk; symptoms; severity of burden; substrate): a novel approach to in‐depth characterization (rather than classification) of atrial fibrillation. Thromb Haemost. 2021;121:270–278. doi: 10.1055/s-0040-1716408 [DOI] [PubMed] [Google Scholar]
- 3. Chao T‐F, Joung B, Takahashi Y, Lim TW, Choi E‐K, Chan Y‐H, Guo Y, Sriratanasathavorn C, Oh S, Okumura K, et al. 2021 Focused update consensus guidelines of the Asia Pacific Heart Rhythm Society on stroke prevention in atrial fibrillation: executive summary. Thromb Haemost. 2022;122:20–47. doi: 10.1055/s-0041-1739411 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Rocks S, Berntson D, Gil‐Salmerón A, Kadu M, Ehrenberg N, Stein V, Tsiachristas A. Cost and effects of integrated care: a systematic literature review and meta‐analysis. Eur J Heal Econ. 2020;21:1211–1221. doi: 10.1007/s10198-020-01217-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Allen D, Gillen E, Rixson L. The effectiveness of integrated care pathways for adults and children in health care settings: a systematic review. JBI Database Syst Rev Implement Reports. 2009;7:80–129. doi: 10.11124/01938924-200907030-00001 [DOI] [PubMed] [Google Scholar]
- 6. Stevens D, Harrison SL, Kolamunnage‐Dona R, Lip GYH, Lane DA. The Atrial Fibrillation Better Care pathway for managing atrial fibrillation: a review. EP Eur. 2021;86:1–11. doi: 10.1093/europace/euab092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lip GYH. The ABC pathway: an integrated approach to improve AF management. Nat Rev Cardiol. 2017;14:627–628. doi: 10.1038/nrcardio.2017.153 [DOI] [PubMed] [Google Scholar]
- 8. Proietti M, Lip GYH, Laroche C, Fauchier L, Marin F, Nabauer M, Potpara T, Dan G‐A, Kalarus Z, Tavazzi L, et al. Relation of outcomes to ABC (Atrial Fibrillation Better Care) pathway adherent care in European patients with atrial fibrillation: an analysis from the ESC‐EHRA EORP Atrial Fibrillation General Long‐Term (AFGen LT) Registry. Eur Eur Pacing, Arrhythmias, Card Electrophysiol J Work Groups Card Pacing, Arrhythmias, Card Cell Electrophysiol Eur Soc Cardiol. 2021;23:174–183. doi: 10.1093/europace/euaa274 [DOI] [PubMed] [Google Scholar]
- 9. Guo Y, Lane DA, Wang L, Zhang H, Wang H, Zhang W, Wen J, Xing Y, Wu F, Xia Y, et al. Mobile health technology to improve care for patients with atrial fibrillation. J Am Coll Cardiol. 2020;75:1523–1534. doi: 10.1016/j.jacc.2020.01.052 [DOI] [PubMed] [Google Scholar]
- 10. Proietti M, Romiti GF, Olshansky B, Lane DA, Lip GYH. Comprehensive management with the ABC (Atrial Fibrillation Better Care) pathway in clinically complex patients with atrial fibrillation: a post hoc ancillary analysis from the AFFIRM trial. J Am Heart Assoc. 2020;9:e014932. doi: 10.1161/JAHA.119.014932 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Yoon M, Yang P‐S, Jang E, Yu HT, Kim T‐H, Uhm J‐S, Kim J‐Y, Sung J‐H, Pak H‐N, Lee M‐H, et al. Improved population‐based clinical outcomes of patients with atrial fibrillation by compliance with the simple ABC (Atrial Fibrillation Better Care) pathway for integrated care management: a nationwide cohort study. Thromb Haemost. 2019;19:1695–1703. doi: 10.1055/s-0039-1693516 [DOI] [PubMed] [Google Scholar]
- 12. Romiti GF, Pastori D, Rivera‐Caravaca JM, Ding WY, Gue YX, Menichelli D, Gumprecht J, Koziel M, Yang P‐S, Guo Y, et al. Adherence to the “Atrial Fibrillation Better Care” (ABC) pathway in patients with atrial fibrillation. Thromb Haemost. 2022;122:406–414. doi: 10.1055/a-1515-9630 [DOI] [PubMed] [Google Scholar]
- 13. Proietti M, Marzona I, Vannini T, Tettamanti M, Fortino I, Merlino L, Basili S, Mannucci PM, Boriani G, Lip GYH, et al. Long‐term relationship between atrial fibrillation, multimorbidity and oral anticoagulant drug use. Mayo Clin Proc. 2019;2427–2436. doi: 10.1016/j.mayocp.2019.06.012 [DOI] [PubMed] [Google Scholar]
- 14. Jani BD, Nicholl BI, McQueenie R, Connelly DT, Hanlon P, Gallacher KI, Lee D, Mair FS. Multimorbidity and co‐morbidity in atrial fibrillation and effects on survival: findings from UK Biobank cohort. Europace. 2018;20:f329–f336. doi: 10.1093/europace/eux322 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Proietti M, Raparelli V, Olshansky B, Lip GYH. Polypharmacy and major adverse events in atrial fibrillation: observations from the AFFIRM trial. Clin Res Cardiol. 2016;105:412–420. doi: 10.1007/s00392-015-0936-y [DOI] [PubMed] [Google Scholar]
- 16. Piccini JP, Hellkamp AS, Washam JB, Becker RC, Breithardt G, Berkowitz SD, Halperin JL, Hankey GJ, Hacke W, Mahaffey KW, et al. Polypharmacy and the efficacy and safety of rivaroxaban versus warfarin in the prevention of stroke in patients with nonvalvular atrial fibrillation. Circulation. 2016;133:352–360. doi: 10.1161/CIRCULATIONAHA.115.018544 [DOI] [PubMed] [Google Scholar]
- 17. Jaspers Focks J, Brouwer MA, Wojdyla DM, Thomas L, Lopes RD, Washam JB, Lanas F, Xavier D, Husted S, Wallentin L, et al. Polypharmacy and effects of apixaban versus warfarin in patients with atrial fibrillation: post hoc analysis of the ARISTOTLE trial. BMJ. 2016;353:i2868. doi: 10.1136/bmj.i2868 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Steinberg BA, Kim S, Fonarow GC, Thomas L, Ansell J, Kowey PR, Mahaffey KW, Gersh BJ, Hylek E, Naccarelli G, et al. Drivers of hospitalization for patients with atrial fibrillation: results from the Outcomes Registry for Better Informed Treatment of Atrial Fibrillation (ORBIT‐AF). Am Heart J. 2014;167:735–742.e2. doi: 10.1016/j.ahj.2014.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Burdett P, Lip GYH. Atrial fibrillation in the United Kingdom: predicting costs of an emerging epidemic recognising and forecasting the cost drivers of atrial fibrillation‐related costs. Eur Hear J ‐ Qual Care Clin Outcomes. 2022;8:187–194. doi: 10.1093/ehjqcco/qcaa093 [DOI] [PubMed] [Google Scholar]
- 20. Piazza G, Hurwitz S, Harrigan L, Jenkins K, Hohlfelder B, Fanikos J, Goldhaber S. Anticoagulation and mortality rates among hospitalized patients with atrial fibrillation. TH Open. 2018;02:e33–e38. doi: 10.1055/s-0038-1626732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Proietti M, Laroche C, Nieuwlaat R, Crijns HJGM, Maggioni AP, Lane DA, Boriani G, Lip GYH. Increased burden of comorbidities and risk of cardiovascular death in atrial fibrillation patients in Europe over ten years: a comparison between EORP‐AF pilot and EHS‐AF registries. Eur J Intern Med. 2018;55:28–34. doi: 10.1016/j.ejim.2018.05.016 [DOI] [PubMed] [Google Scholar]
- 22. Proietti M, Laroche C, Opolski G, Maggioni AP, Boriani G, Lip GYH. ‘Real‐world’ atrial fibrillation management in Europe: observations from the 2‐year follow‐up of the EURObservational Research Programme‐Atrial Fibrillation General Registry Pilot Phase. Europace. 2016;euw112. doi: 10.1093/europace/euw112 [DOI] [PubMed] [Google Scholar]
- 23. Fauchier L, Villejoubert O, Clementy N, Bernard A, Pierre B, Angoulvant D, Ivanes F, Babuty D, Lip GYH. Causes of death and influencing factors in patients with atrial fibrillation. Am J Med. 2016;129:1278–1287. doi: 10.1016/j.amjmed.2016.06.045 [DOI] [PubMed] [Google Scholar]
- 24. Marijon E, Le Heuzey J‐Y, Connolly S, Yang S, Pogue J, Brueckmann M, Eikelboom J, Themeles E, Ezekowitz M, Wallentin L, et al. Causes of death and influencing factors in patients with atrial fibrillation. Circulation. 2013;128:2192–2201. doi: 10.1161/CIRCULATIONAHA.112.000491 [DOI] [PubMed] [Google Scholar]
- 25. Gómez‐Outes A, Lagunar‐Ruíz J, Terleira‐Fernández A‐I, Calvo‐Rojas G, Suárez‐Gea ML, Vargas‐Castrillón E. Causes of death in anticoagulated patients with atrial fibrillation. J Am Coll Cardiol. 2016;68:2508–2521. doi: 10.1016/j.jacc.2016.09.944 [DOI] [PubMed] [Google Scholar]
- 26. Guo Y, Wang Y, Li X, Shan Z, Shi X, Xi G, Lip GYH. Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry: protocol for a prospective, observational nationwide cohort study. BMJ Open. 2018;8:e020191. doi: 10.1136/bmjopen-2017-020191 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Guo Y, Imberti JF, Kotalczyk A, Wang Y, Lip GYH. 4S‐AF scheme and ABC pathway guided management improves outcomes in atrial fibrillation patients. Eur J Clin Invest. 2022;e13751. doi: 10.1111/eci.13751 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Kotalczyk A, Guo Y, Wang Y, Lip GYH. Investigators on behalf of the CR . Impact of multimorbidity and polypharmacy on clinical outcomes of elderly Chinese patients with atrial fibrillation. J Clin Med. 2022;11:1370. doi: 10.3390/jcm11051370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Diederichs C, Berger K, Bartels DB. The measurement of multiple chronic diseases–a systematic review on existing multimorbidity indices. J Gerontol A Biol Sci Med Sci. 2011;66:301–311. doi: 10.1093/gerona/glq208 [DOI] [PubMed] [Google Scholar]
- 30. van den Akker M, Buntinx F, Knottnerus JA. Comorbidity or multimorbidity. Eur J Gen Pract. 1996;2:65–70. doi: 10.3109/13814789609162146 [DOI] [Google Scholar]
- 31. Viktil KK, Blix HS, Moger TA, Reikvam A. Polypharmacy as commonly defined is an indicator of limited value in the assessment of drug‐related problems. Br J Clin Pharmacol. 2007;63:187–195. doi: 10.1111/j.1365-2125.2006.02744.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Lip GYH, Laroche C, Dan G‐A, Santini M, Kalarus Z, Rasmussen LH, Oliveira MM, Mairesse G, Crijns HJGM, Simantirakis E, et al. A prospective survey in European Society of Cardiology member countries of atrial fibrillation management: baseline results of EURObservational Research Programme Atrial Fibrillation (EORP‐AF) Pilot General Registry. EP Eur. 2014;16:308–319. doi: 10.1093/europace/eut373 [DOI] [PubMed] [Google Scholar]
- 33. Lip GYH, Nieuwlaat R, Pisters R, Lane DA, Crijns HJGM, Andresen D, Camm AJ, Davies W, Capucci A, Olsson B, et al. Refining clinical risk stratification for predicting stroke and thromboembolism in atrial fibrillation using a novel risk factor‐based approach: the Euro Heart Survey on atrial fibrillation. Chest. 2010;137:263–272. doi: 10.1378/chest.09-1584 [DOI] [PubMed] [Google Scholar]
- 34. Pisters R, Lane DA, Nieuwlaat R, de Vos CB, Crijns HJ, Lip GY. A novel user‐friendly score (HAS‐BLED) to assess 1‐year risk of major bleeding in patients with atrial fibrillation: the Euro Heart Survey. Chest. 2010;138:1093–1100. doi: 10.1378/chest.10-0134 [DOI] [PubMed] [Google Scholar]
- 35. Schulman S, Kearon C. Definition of major bleeding in clinical investigations of antihemostatic medicinal products in non‐surgical patients. J Thromb Haemost. 2005;3:692–694. doi: 10.1111/j.1538-7836.2005.01204.x [DOI] [PubMed] [Google Scholar]
- 36. Dyer MTD, Goldsmith KA, Sharples LS, Buxton MJ. A review of health utilities using the EQ‐5D in studies of cardiovascular disease. Health Qual Life Outcomes. 2010;8:13. doi: 10.1186/1477-7525-8-13 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Luo N, Liu G, Li M, Guan H, Jin X, Rand‐Hendriksen K. Estimating an EQ‐5D‐5L value set for China. Value Heal. 2017;20:662–669. doi: 10.1016/j.jval.2016.11.016 [DOI] [PubMed] [Google Scholar]
- 38. Guo Y, Wang H, Kotalczyk A, Wang Y, Lip GYH. One‐year follow‐up Results of the Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. J Arrhythmia. 2021;37:1227–1239. doi: 10.1002/joa3.12608 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Kotalczyk A, Mazurek M, Kalarus Z, Potpara TS, Lip GYH. Stroke prevention strategies in high‐risk patients with atrial fibrillation. Nat Rev Cardiol. 2021;18:276–290. doi: 10.1038/s41569-020-00459-3 [DOI] [PubMed] [Google Scholar]
- 40. Proietti M, Romiti GF, Vitolo M, Potpara TS, Boriani G, Lip GYH. Investigators on behalf of E‐EE‐AL‐TGR . Comparison of HAS‐BLED and ORBIT bleeding risk scores in AF patients treated with NOACs: a report from the ESC‐EHRA EORP‐AF general long‐term registry. Eur Hear J ‐ Qual Care Clin Outcomes. 2021. [epub ahead of print]. doi: 10.1093/ehjqcco/qcab069 [DOI] [PubMed] [Google Scholar]
- 41. Guo Y, Lane DA, Chen Y, Lip GYH. Regular bleeding risk assessment associated with reduction in bleeding outcomes: the mAFA‐II randomized trial. Am J Med. 2020;133:1195–1202.e2. doi: 10.1016/j.amjmed.2020.03.019 [DOI] [PubMed] [Google Scholar]
- 42. Guo Y, Kotalczyk A, Imberti JF, Wang Y, Lip GYH, ChiOTEAF Registry Investigators . Poor adherence to guideline‐directed anticoagulation in elderly Chinese patients with atrial fibrillation. A report from the Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. Eur Hear Journal Qual Care Clin Outcomes. 2021. [epub ahead of print]. doi: 10.1093/ehjqcco/qcab054 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Guo Y, Kotalczyk A, Imberti JF, Wang Y, Lip GYH. Oral anticoagulation improves survival in very elderly Chinese patients with atrial fibrillation: a report from the Optimal Thromboprophylaxis in Elderly Chinese Patients with Atrial Fibrillation (ChiOTEAF) registry. Int J Stroke. 2021. [epub ahead of print]. doi: 10.1177/17474930211046743 [DOI] [PubMed] [Google Scholar]
- 44. Yoon M, Yang P‐S, Jang E, Yu HT, Kim T‐H, Uhm J‐S, Kim J‐Y, Sung J‐H, Pak H‐N, Lee M‐H, et al. Improved population‐based clinical outcomes of patients with atrial fibrillation by compliance with the simple ABC (Atrial Fibrillation Better Care) pathway for integrated care management: a nationwide cohort study. Thromb Haemost. 2019;119:1695–1703. doi: 10.1055/s-0039-1693516 [DOI] [PubMed] [Google Scholar]
- 45. Guo Y, Guo J, Shi X, Yao Y, Sun Y, Xia Y, Yu B, Liu T, Chen Y, Lip GYH. Mobile health technology‐supported atrial fibrillation screening and integrated care: a report from the mAFA‐II trial long‐term extension cohort. Eur J Intern Med. 2020;82:105–111. doi: 10.1016/j.ejim.2020.09.024 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Kozieł M, Simovic S, Pavlovic N, Kocijancic A, Paparisto V, Music L, Trendafilova E, Dan AR, Kusljugic Z, Dan G‐A, et al. Adherence to the ABC (Atrial fibrillation Better Care) pathway in the Balkan region: the BALKAN‐AF survey. Polish Arch Intern Med. 2020;130:187–195. doi: 10.20452/pamw.15146 [DOI] [PubMed] [Google Scholar]
- 47. Boriani G, Proietti M, Laroche C, Fauchier L, Marin F, Nabauer M, Potpara T, Dan G‐A, Kalarus Z, Tavazzi L, et al. Association between antithrombotic treatment and outcomes at 1‐year follow‐up in patients with atrial fibrillation: the EORP‐AF general long‐term registry. EP Eur. 2019;21:1013–1022. doi: 10.1093/europace/euz032 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1
Tables S1–S4
Data Availability Statement
The data sets used and analyzed during the current study are available from the corresponding author on reasonable request.


