Abstract
Uniatrial but biventricular atrioventricular connection is a rare congenital cardiac abnormality where the left atria-ventricular connection is absent and the right atrio-ventricular connection straddles the crest of the muscular ventricular septum. This anomaly has been referred to as double outlet right atrium and the atrio-ventricular valve as a common atrioventricular valve in the past. In the absence of a primary atrial septal defect, the atrio-ventricular junction is not a common junction and the valve cannot hence be described as a common trio-ventricular valve. We demonstrate this paradox by an illustrative case and contrast this with two other cases where a common atrio-ventricular valve was predominantly committed to the right atrium.
Keywords: Common atrioventricular junction, double-outlet right atrium, malaligned atrial septum
INTRODUCTION
The various arrangements in which one of the atrial chambers is able to communicate directly with both ventricles continue to generate misunderstanding and debate. Description of a case in which the left atrium was communicating directly with both ventricles[1] generated conflicting editorial commentaries. On the one hand, Richard Van Praagh provided an extensive review of potential developmental explanations, albeit without providing any evidence to substantiate his speculations.[2] On the other hand, one of us provided a commentary emphasizing the need to distinguish between the right and left atrioventricular (AV) junctions, as opposed to a common AV junction.[3] This was because the situation in which one or other of the atrial chambers communicates directly with both ventricles can also be produced by gross malalignment of the primary atrial septum in the setting of a common AV junction. The latter arrangement, of course, is one of the variants found in the setting of an AV septal defect. And most usually, in that latter setting, the ventricles are of comparable size, usually with concordant ventriculoarterial connections, such that it is possible to achieve surgical biventricular repair by excision of the malaligned atrial septum, with repositioning of a new septum so as to direct the venous returns to their appropriate ventricles.[4] The problem in differentiating these variants producing so-called “double-outlet atrium” arises when such hearts with AV septal defect and malaligned primary atrial septum are compared with other hearts in which there is straddling of either the right or left AV valve in the setting of absence of one of the AV connections. It was such a heart with absence of the right AV connection that stimulated the commentaries discussed above.[1] In the same issue of the journal, another heart was described with dual orifices in the tricuspid valve, but with the tongue dividing the orifices bound down to the crest of the ventricular septum such that there was no interventricular shunting.[5] As was explained in one of the commentaries, this situation produces the paradoxical situation in that, seemingly, there are three AV valves, but in the presence of only two AV junctions.[3] We have now encountered another heart with this potentially confusing arrangement, but in the setting of absence of the left AV junction with straddling of the right AV valve. It has been suggested that such hearts were no more than common atrioventricular junctions, but with the primary atrial septum fused to the parietal left atrioventricular junction so as to obliterate the “ostium primum” defect.[6,7] We do not believe this to be the explanation of the morphology found in our patient. Indeed, we will emphasise that, in the setting of absence of the left atrioventricular connection, the valve guarding the right atrial vestibule remains a right atrioventricular valve even if it is tethered in both the right and left ventricles [Figure 1C]. We compare and contrast the findings in our first patient with those from two other patients having common AV valves [Figure 1b], but in the setting of double-inlet ventricle, albeit with the primary atrial septum malaligned to produce the arrangement recognized as double-outlet right atrium.[8,9]
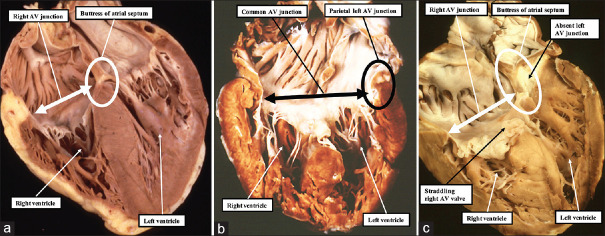
Figure 1.
The panels show the key morphological distinction between separate right and left atrioventricular junctions (a), a common atrioventricular junction (b), and a right atrioventricular junction in the setting of absence of the left atrioventricular connection (c)
DEFINITIONS
Understanding of the different arrangements producing the situation in which one or other of the atrial chambers is able to communicate directly with both ventricles across the AV junctions requires a precise definition of what is meant by the AV junctions and, by extension, the valves which guard them. In the normal heart, of course, there are two AV junctions, which are readily described as being right and left [Figure 1a]. In this normal setting, the leftward margin of the right AV junction is formed by the buttress of the atrial septum, which interposes between the cavities of the right and left atrial chambers. By virtue of the integrity of the atrial and ventricular septal structures, this means that the right atrium is able to communicate only with right ventricle across the right AV junction, while the left atrium communicates with the left ventricle across the left AV junction [Figure 1a]. In the majority of hearts with deficient AV septation, there is a common AV junction. Usually, in this setting, the atrial and ventricular chambers are arranged such that the right atrium continues to communicate with the right ventricle, and the left atrium with the left ventricle, but across the common junction [Figure 1b]. The leftward margin of the common junction is then formed by the parietal left AV wall. It is possible in this arrangement for the primary atrial septum to be deviated leftward such that the systemic venous return entering the right atrium is able to pass directly into both ventricles, with the pulmonary venous return exiting the left atrium by passing between the leading edge of the atrial septum and the parietal left AV junction. This is the situation producing double-outlet right atrium in the setting of an AV septal defect.[9] Despite the double-outlet right atrium, however, the AV junction is still common, and is limited to the left side by the AV junction. In the arrangement encountered in our first patient, there was absence of the left AV connection, as in the heart shown in Figure 1c. This is the arrangement described, by virtue of the fact that the solitary AV valve is straddling, and hence tethered in both ventricles, as producing a uniatrial and biventricular connection.[10] The key feature that distinguishes this arrangement from the common AV junction is that the straddling valve is attached exclusively to the vestibule of the right atrium, with its leftward margin formed by the buttress of the atrial septum [compare Figure 1a and c]. Hence, it is a right AV valve, despite the fact that it is tethered in both ventricles. It cannot be a common valve, since it does not drain directly the blood from the left atrium. An understanding of these definitions is essential if we are to explain the differing morphologies found in our three patients, all of whom have the flow patterns described as double-outlet right atrium.
DESCRIPTION OF CASES
Our first patient was a 15-day-old boy, initially diagnosed as having an AV septal defect, and referred for elective surgery. Transthoracic echocardiography revealed usual arrangement of the abdominal organs and the atrial chambers, with normal systemic and pulmonary venous connections. The key feature was the finding of straddling and overriding of the right AV valve, with absence of the left AV connection. The leftward margin of the straddling AV valve was formed by the buttress of the atrial septum [Figures 2a, 3a and Video 1]. The only outlet from the left atrium was a moderately sized defect within the oval fossa [Figure 3b and c]. One of the bridging leaflets of the straddling right valve was attached to the crest of the muscular ventricular septum, but the valve was competent [Figure 4a and Video 2]. The ventricles were balanced, and showed right-handed topology. The ventriculoarterial connections were concordant [Figure 5a], and the outflow tracts were unobstructed. The aortic arch was left sided, with a normal branching pattern, and the arterial duct was no longer patent. The family was advised of the need for early surgery because of concerns about the atrial communication becoming more restrictive. They chose, however, against surgical intervention. The baby was referred again at 2 months of age because of poor weight gain and worsening respiratory distress. As predicted, the atrial communication had become more restrictive, with the symptoms now attributable to pulmonary venous hypertension. The parents again refused surgical intervention, and the infant died 1 week later at the referring hospital.
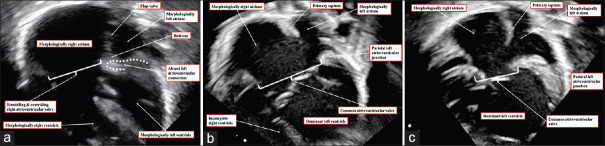
Figure 2.
Apical four-chamber echocardiographic images are shown of all three infants. (a) The apical four-chamber view of the first case. The buttress of the atrial septum is completely fused with the parietal atrioventricular junction. Hence, there is no direct communication between the cavity of the left atrium and the ventricles. The right atrium has a biventricular atrioventricular connection. (b and c) The apical four-chamber views in the second (b) and third (c) cases. The atrial septum is deviated to the left, but is not fused to the parietal atrioventricular junction, permitting flow beneath the leading edge of the primary atrial septum
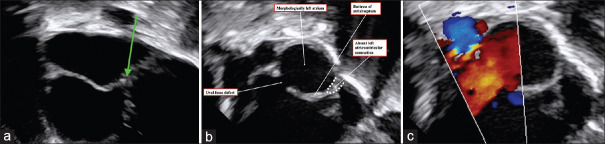
Figure 3.
(a) An echocardiographic image from our first patient as obtained using the modified subcostal view. It demonstrates the fusion of the lower edge of the atrial septum to the parietal atrioventricular junction (green arrow). Additional imaging from the subcostal region shows the presence of a defect within the oval fossa (b), with color Doppler imaging revealing the left-to-right shunt (c)
Figure 4.
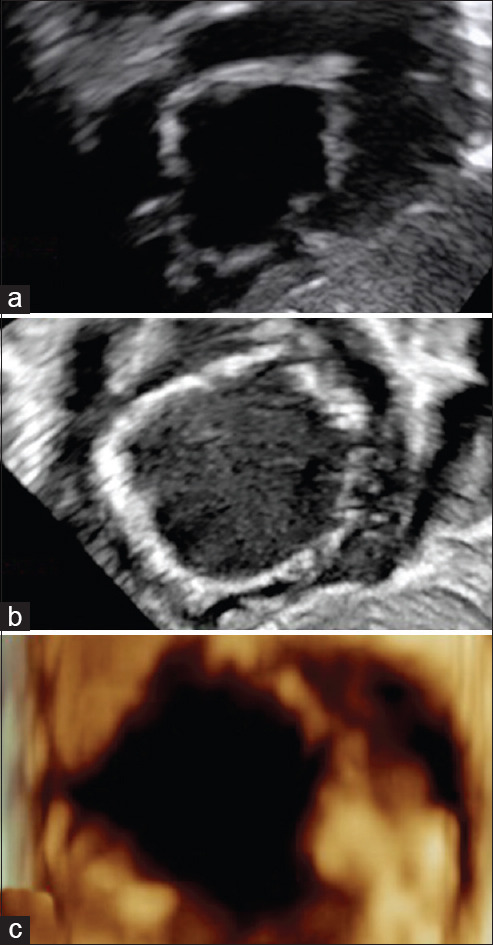
The short-axis images of the atrioventricular valve as taken in subcostal fashion are shown for the three cases, (a) from the first case, (b) from the second, and (c) from the third. The similarities resulted in misclassification of our first case as representing a common atrioventricular valve in the setting of an atrioventricular septal defect
Figure 5.
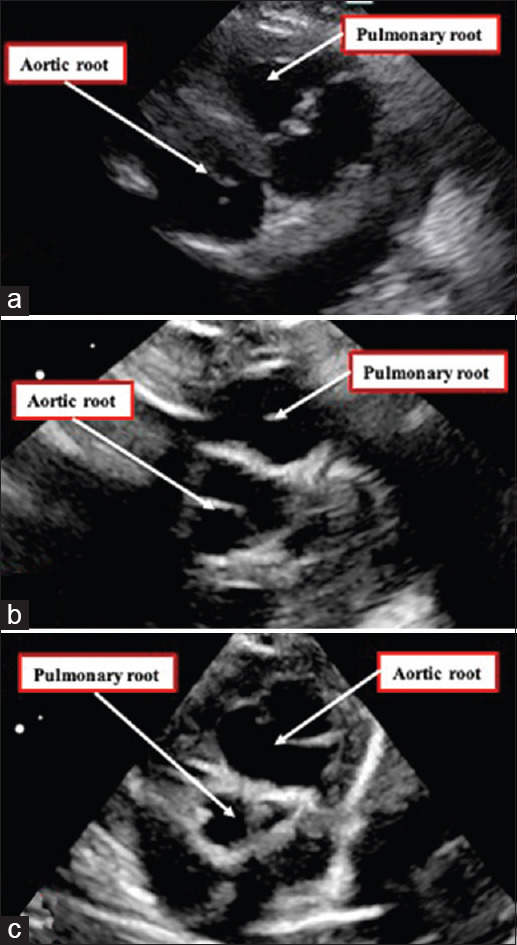
Images taken to provide the parasternal short-axis view show the relationships of the arterial roots. The roots are normally related, with the pulmonary root anterior and to the left of the aortic root in the first (a) and second (b) cases, but the aortic root is anterior and left-sided in the third case (c)
We were then confronted by a second case, a 4-month-old infant with trisomy 21 referred to us for evaluation of the heart. In this infant, transthoracic echocardiography again revealed normal arrangement of the abdominal organs and the atrial chambers, with normal systemic and pulmonary venous connections. In this patient, although the atrial septum, as in the first patient, was deviated to the left, it was not fused to the parietal left AV junction [Figure 2b and Video 3]. Thus, flow from the left atrium was between the leading edge of the primary atrial septum and the summit of the parietal wall of the left ventricle. The flow patterns, therefore, were again that of double-outlet right atrium, but this time in the setting of a common AV valve [Figure 4b and Video 4]. We found a further complication, however, in that the left ventricle was dominant, with a small incomplete right ventricle positioned anterior and to the right of the dominant left ventricle. The ventriculoarterial connections were concordant [Figure 5b], with an interventricular communication of moderate size providing the only source of flow to the incomplete right ventricle [Figure 6]. The aortic arch was left sided, with normal branching pattern, and the arterial duct was no longer patent. The morphological diagnosis, acknowledging the physiological flow patterns of double-outlet right atrium, was double-inlet left ventricle through a common AV valve, but with concordant ventriculoarterial connections, in other words a variant of the so-called “Holmes heart.” The parents were advised to proceed along a path of staged functionally univentricular palliation, with early banding of the pulmonary trunk.
Figure 6.
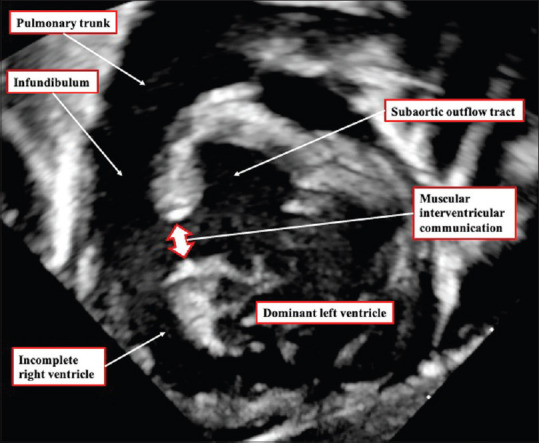
The echocardiographic image, taken from the subcostal view, in the second case shows the muscular interventricular communication, with the pulmonary trunk arising from the hypoplastic anteriorly located incomplete right ventricle
Our experience of morphological variants producing the flow patterns of double-outlet right atrium was then extended when another 4-day-old baby was referred to us for evaluation. In this neonate, transthoracic echocardiography revealed the liver to be right sided, but the spleen could not be visualized. The heart was in the left side of the thorax. The atrial appendages could not be satisfactorily imaged, but the venoatrial connections were normal. The atrial septum was again deviated markedly to the left, such that flow from the left atrium was between the leading edge of the primary atrial septum and the left AV mural junction [Figure 2c and Video 5]. In other words, all the blood entering directly to the ventricular mass was again passing from the vestibule of the right atrium [Figure 4c]. As with the second patient, the morphologically left ventricle was dominant, but this time the incomplete right ventricle was anterior and to the left of the dominant ventricle. The aorta arose anteriorly from the incomplete morphologically right ventricle [Figure 5c], and there was pulmonary atresia. The aortic arch was left sided, and branched in normal fashion. A vertically aligned arterial duct was the only source of pulmonary blood flow to confluent pulmonary arteries. As with the second patient, the morphological diagnosis was double-inlet left ventricle, but with discordant ventriculoarterial connections, or in other words transposition. Since the common AV valve originated predominantly from the vestibule of the morphologically right atrium, the lesion once more could again be described as producing the flow pattern of double-outlet right atrium. The baby was commenced on an infusion of prostaglandin E1, which resulted in an improvement of oxygen saturation. A systemic-to-pulmonary arterial shunt was created 48 h later, and the baby had an uneventful recovery
DISCUSSION
The anatomical arrangements producing the flow patterns of so-called double-outlet atrium have generated significant discussion.[2,3,8,11] It is now accepted that the arrangement is produced most frequently by deviation of the atrial septum in the setting of a common AV junction such that the flow from one of the atrial chambers is between the leading edge of the atrial septum and the parietal AV mural junction.[8] The arrangement that continues to produce controversy and discussion is the one found in our first patient, in which there is straddling and overriding of a solitary AV valve in the setting of absence of one of the AV connections, or AV valve atresia. This is the arrangement that is appropriately described as producing a uniatrial but biventricular AV connection.[10] The problem that has existed with appropriately describing such cases reflects the fact that the straddle and override of the valve generates the temptation to presume that the valve is guarding a common AV junction. Indeed, some have suggested that the arrangement is no more than an extreme form of AV septal defect, but with the primary atrial septum deviated to the left to such an extent that it has fused completely with the parietal wall of the left-sided AV junction.[7,8] Those promoting this developmental explanation, based on their own experience in which they were able to achieve biventricular surgical correction, point to a previous description. They failed to note, however, that in the earlier description, the authors described the flow from the left atrium as passing through an “ostium primum” defect, hence suggesting that the patient did, indeed, have a common AV junction.[12]
The essence of a common AV valve is that it guards a common AV junction [Figure 1b]. Such a common valve itself usually straddles and overrides. As we discovered in our second and third patients, however, this is not always the case. As we found in our first patient, furthermore, because the buttress of the atrial septum had fused with the parietal left-sided AV junction, there was no AV septal defect. Instead, the only outlet from the left atrium was through a defect in the oval fossa. Even though the AV valve was straddling and overriding the crest of the muscular ventricular septum, it remained a right AV valve. There is a further paradox in our second 2 infants. Although the common AV junction was supported exclusively by the vestibule of the right atrium, with marked deviation of the primary atrial septum, and thus producing the physiological flow pattern of double-outlet right atrium, the AV connection was exclusively to the dominant left ventricle. In other words, there was double-outlet right atrium, but also double inlet through a common AV valve. In the more usual variant of double-outlet right atrium produced by deviation of the atrial septum in the setting of a common AV junction, the common valve is supported by balanced right and left ventricles.[4,9] It is the balanced arrangement of the ventricular mass that usually permits biventricular surgical correction subsequent to excision of the primary atrial septum. In all of our patients, in contrast, the only option for treatment would be functionally univentricular palliation. In the case reported by Perez-Martinez et al., nonetheless, it did prove possible to achieve biventricular surgical repair, despite the absence of the left AV connection. This is very much the exception that tests the rule.
Our experience, taken overall, serves to illustrate the problems that continue to exist in the setting of straddling and overriding AV valves. So-called double-outlet right atrium is no more than the physiological situation produced when the valve supported by the vestibule of the morphologically right atrium connects to both the morphologically right and morphologically left ventricles. The flow pattern produced is always present in the setting of straddling and overriding of the tricuspid valve, irrespective of whether the tricuspid valve coexists with a mitral valve, or is found, as in our first patient, with absence of the left AV connection. As we found in our second and third patients, the same flow pattern can be found in the setting of a common AV junction even when the valve guarding the junction is neither straddling nor overriding. In both of our patients, because the common valve connected only with the dominant left ventricle, there was effectively a uniatrial and univentricular connection across the common AV junction, but again producing the flow patterns of double-outlet right atrium. Our experience confirms our earlier suggestions,[3,11] namely that appropriate description of these rare cases depends on the distinction between a common AV junction and a solitary junction in the setting of an absent connection. We now appreciate that it also requires careful attention to the support provided by the ventricular mass to the AV valve that is present.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Videos Available on: www.annalspc.com
REFERENCES
- 1.Shetkar S, Kothari SS. Double-outlet left atrium: Ventriculo-atrial malalignment defect. Ann Pediatr Cardiol. 2013;6:158–61. doi: 10.4103/0974-2069.115266. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.van Praagh R. What are double-outlet left atrium and double-outlet right atrium. Ann Pediatrc Cardiol. 2013;6:155–7. [PMC free article] [PubMed] [Google Scholar]
- 3.Anderson RH. How best to explain unexpected arrangements of the atrioventricular valves. Ann Pediatr Cardiol. 2013;6:152–4. [PMC free article] [PubMed] [Google Scholar]
- 4.Alivizatos P, Anderson RH, Macartney FJ, Zuberbuhler JR, Stark J. Atrioventricular septal defect with balanced ventricles and malaligned atrial septum: Double-outlet right atrium. Report of two cases. J Thorac Cardiovasc Surg. 1985;89:295–7. [PubMed] [Google Scholar]
- 5.Sapre A, Gopalraj SS, Kottayil BP, Kumar RK. An unusual example of isolated double-orifice tricuspid valve. Ann Pediatr Cardiol. 2013;6:162–3. doi: 10.4103/0974-2069.115269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nuñez L, Aguado MG, Sanz E, Perez Martinez V. Surgical repair of double-outlet right atrium. Ann Thorac Surg. 1984;37:164–6. doi: 10.1016/s0003-4975(10)60308-6. [DOI] [PubMed] [Google Scholar]
- 7.Pérez-Martínez VM, García-Fernandez F, Oliver-Ruiz J, Nuñez-Gonzalez L. Double-outlet right atrium with two atrioventricular valves and left atrial outlet atresia. J Am Coll Cardiol. 1984;3:375–80. doi: 10.1016/s0735-1097(84)80022-4. [DOI] [PubMed] [Google Scholar]
- 8.Edwin F, Kinsley RH, Mamorare HM, Govendrageloo K. The spectrum of double-outlet right atrium including hearts with three atrioventricular valves. Eur J Cardiothorac Surg. 2012;41:947–9. doi: 10.1093/ejcts/ezr073. [DOI] [PubMed] [Google Scholar]
- 9.Brancaccio G, Amodeo A, Rinelli G, Filippelli S, Sanders SP, Di Donato RM. Double-outlet right atrium: Anatomic and clinical considerations. Ann Thorac Surg. 2007;83:619–21. doi: 10.1016/j.athoracsur.2006.09.080. [DOI] [PubMed] [Google Scholar]
- 10.Kiraly L, Hubay M, Cook AC, Ho SY, Anderson RH. Morphologic features of the uniatrial but biventricular atrioventricular connection. J Thorac Cardiovasc Surg. 2007;133:229–34. doi: 10.1016/j.jtcvs.2006.08.067. [DOI] [PubMed] [Google Scholar]
- 11.Gupta SK, Gupta A, Ramakrishnan S, Anderson RH. Clarifying the atrioventricular junctional anatomy in the setting of double outlet right atrium. Ann Pediatr Cardiol. 2015;8:233–9. doi: 10.4103/0974-2069.164688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Utley JR, Noonan JA, Walters LR, Frist RA. Anomalous position of atrial septum with anomalous pulmonary and systemic venous drainage. Correction including ligation of persistent left superior vena cava. J Thorac Cardiovasc Surg. 1974;67:730–2. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.