Abstract
Background
Thoracic trauma is a major cause of death in trauma patients and road traffic accident (RTA)-related thoracic injuries have different characteristics than those with non-RTA related thoracic traumas, but this have been poorly described. The main objective was to investigate the epidemiology, injury pattern and outcome of patients suffering a significant RTA-related thoracic injury. Secondary objective was to investigate the influence of serious thoracic injuries on mortality, compared to other serious injuries.
Methods
We performed a multicenter observational study including patients of the Rhône RTA registry between 1997 and 2016 sustaining a moderate to lethal (Abbreviated Injury Scale, AIS≥2) injury in any body region. A subgroup (AISThorax≥2 group) included those with one or more AIS≥2 thoracic injury. Descriptive statistics were performed for the main outcome and a multivariate logistic regression was computed for our secondary outcome.
Results
A total of 176,346 patients were included in the registry and 6,382 (3.6%) sustained a thoracic injury. Among those, median age [IQR] was 41 [25–58] years, and 68.9% were male. The highest incidence of thoracic injuries in female patients was in the 70–79 years age group, while this was observed in the 20–29 years age group among males. Most patients were car occupants (52.3%). Chest wall injuries were the most frequent thoracic injuries (62.1%), 52.4% of which were multiple rib fractures. Trauma brain injuries (TBI) were the most frequent concomitant injuries (29.1%). The frequency of MAISThorax = 2 injuries increased with age while that of MAISThorax = 3 injuries decreased. A total of 16.2% patients died. Serious (AIS≥3) thoracic injuries (OR = 12.4, 95%CI [8.6;18.0]) were strongly associated with mortality but less than were TBI (OR = 27.9, 95%CI [21.3;36.7]).
Conclusion
Moderate to lethal RTA-related thoracic injuries were rare. Multiple ribs fractures, pulmonary contusions, and sternal fractures were the most frequent anatomical injuries. The incidence, injury pattern and mechanisms greatly vary across age groups.
Introduction
In the year 2000, road traffic accidents (RTA) were the tenth leading cause of death in the world, the eighth in 2016, and could become the fifth by 2030 according to the World Health Organization [1, 2]. Victims of RTA often suffer multi-trauma and present with thoracic injuries in about 50% cases [3–5]. Furthermore, thoracic trauma are the third most common cause of death in multi-trauma patients [6] and are associated with poor short-term outcomes as they are responsible for up to 25% of trauma-related deaths [7, 8]. Therefore, thoracic traumas represent a major medical and economic problem, and providing care for those patients is challenging. Some risk factors of mortality following thoracic trauma have already been identified, including of the presence of specific structural damages to the chest wall and thoracic organs [8–10] and many studies have shown that thoracic injuries significantly contribute to the mortality of multi-trauma patients, in adults as well as in the paediatric population [11–13]. Furthermore, recent literature has shown that patients with RTA-related thoracic injuries had different clinical characteristics than those with non-RTA related thoracic traumas [5]. However, the literature on the epidemiology, injury pattern and outcome of patients with thoracic trauma following a road traffic accident is still scant.
The main objective of this study was to investigate the epidemiology, injury pattern and outcome of patients suffering one or more RTA-related thoracic injury. Secondary objective was to investigate the influence of serious thoracic injuries on traumatic mortality compared to other types of serious injuries.
Methods
Study design and setting
We conducted a retrospective study that included patients who sustained a RTA between January 1997 and December 2016.
We used prospectively recorded data from the Rhône RTA registry (Registre des victimes d’accidents de la circulation du Rhône), which was implemented in 1995. This registry covers the Rhône area of France (1.83 million inhabitants, 676 inhabitants/km2) and its use is approved by the relevant national authorities (Comité National des Registres, CNR) and data protection agency and (Commission Nationale de l’Informatique et des Libertés, CNIL; N° 999211).
The registry includes the demographic characteristics of each RTA casualty and a description of the sustained body injuries. Patient information is collected prospectively during three consecutive time periods from the accident site to hospital discharge: prehospital scene, emergency room or intensive care unit (ICU), and discharge. The registry team supervises the verification of the data from different sources about the same accident or victim, coding, storage and filing, and statistical analysis. Each injury is coded according to the Abbreviated Injury Scale, a severity score, ranging from 1 (minor) to 6 (beyond treatment) [14]; between 1996 and 2014, the 1990 AIS version was used and the 2005 AIS version was used for 2015 and 2016. The injury severity score (ISS) is calculated from the three worst-affected body regions as the sum of squares of the respective AIS severity levels. The full data collection method has been previously described [15].
Study population
Patients are included in the registry if they sustained a RTA involving at least one vehicle (motorised or not) in the Rhône area, which required institutional healthcare from one of the 245 private and public healthcare structures (including level I, II and III trauma centers) cooperating together, including prehospital primary care teams and forensic medicine institutes.
All patients included in the registry with one or more AIS≥2 injury in any body region (AIS≥2 group) were considered in our analyses.
Measures
Several variables were extracted and analysed: patient characteristics (sex, age, road user category), road network, anatomical injuries, severity score (AIS and ISS), and outcome (ICU admission and mortality). As victims could suffer from several injuries in each body region, the maximum AIS (MAIS) was scored using the injury of the highest severity.
Main outcome measure
The main outcome of our study is RTA-related thoracic injury. We have defined a subgroup of patients in the registry (AISThorax≥2), which included all patients with one or more thoracic injury (AIS≥2).
Secondary outcome measure
Death, our secondary outcome, is medically certified either at the scene or noted in medical charts during hospital stay. An autopsy is systematically undertaken in patients dying in the prehospital setting to confirm cause of death and to provide a complete injury assessment based on AIS scoring.
Ethics approval and consent to participate
The registry has been approved by the relevant French authority and national data protection commission (Comité National des Registres, CNR, and Commission Nationale de l’Informatique et des Libertés, CNIL, N° 999211). Patients, or parents/guardians received information about inclusion in the registry but the need for consent was waived. All data were fully anonymized before analysis.
Statistical analysis
Baseline characteristics were described by frequencies and percentages for categorical variables, and medians and interquartile range [IQR] for continuous variables. We compared the groups using the Pearson Chi2 test for categorical variables. We performed a multivariate logistic regression based on complete cases for our secondary outcome (mortality). The model was built using the following covariates: age, sex, global severity (ISS), road user, road network, year of inclusion. Significant prognostic variables at 5% significance on the univariate analysis were included in analysis. The odds ratio (OR) for each risk factor investigated was calculated as well as the corresponding 95% confidence intervals (CI). Missing data were not imputed Statistical analyses were performed using SAS (Statistical Analysis System v9.4, SAS Institute Inc., Cary, NC, USA). In all analyses, p<0.05 was considered as statistically significant.
Results
Patient and injury characteristics
Over the study period, a total of 176,346 RTA victims were included in the registry; 46,526 (26.4%) had at least one moderate to lethal injury (AIS≥2 group) and 6,382 (3.6%) had at least one thoracic injury AISThorax≥2 (AISThorax≥2 group). Between the first period (1997–2001) to the last one (2012–2016), we noted a 38.7% decrease of patients included in the AIS≥2 group while this was of 23.6% in the group of patients with a thoracic trauma.
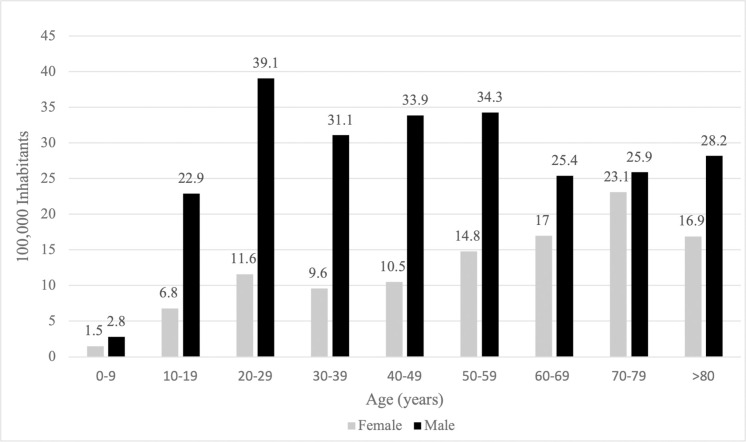
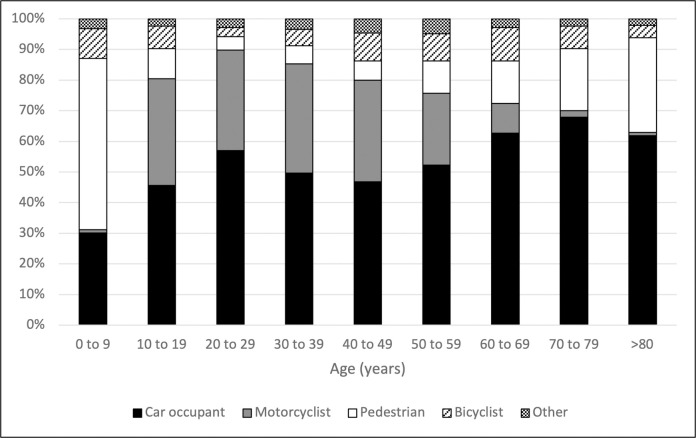
In the AISThorax≥2 group, the median [IQR] age was 41 years [25–58], and 4,400 (68.9%) patients were male. Most of patients were car occupants (52.3%, n = 3,337) and motorcyclists (25.3%, n = 1,617). In most cases (52.7%), the RTA occurred on a city street (Table 1). The highest incidence of AISThorax≥2 injuries in female patients was in the 70–79 years age group (23.1/100,000 inhabitants), while this was observed in the 20–29 years age group among males (39.1/100,000 inhabitants; Fig 1). The distribution of road user by age group is reported in the Fig 2.
Table 1. Demographics and mechanism.
| AIS≥2 group | AISThorax≥2 group | |
|---|---|---|
| (n = 46,526) | (n = 6,382) | |
| n (%) | n (%) | |
| Year of inclusion | ||
| 1997–2001 | 14,771 (31.7) | 1,896 (29.7) |
| 2002–2006 | 12,249 (26.3) | 1,576 (24.7) |
| 2007–2011 | 10,458 (22.5) | 1,462 (22.9) |
| 2012–2016 | 9,048 (19.5) | 1,448 (22.7) |
| Agea, years median [IQR] | 28 [18–45] | 41 [25–58] |
| Sexb | ||
| Male | 33,738 (72.5) | 4,400 (68.9) |
| Female | 12,778 (27.4) | 1,982 (31.1) |
| Road user | ||
| Car occupant | 12,739 (27.4) | 3,337 (52.3) |
| Pedestrian | 6,011 (12.9) | 677 (10.6) |
| Bicyclist | 8,783 (18.9) | 439 (6.9) |
| Motorcyclist | 14,497 (31.2) | 1,617 (25.3) |
| Other | 4,496 (9.6) | 312 (4.9) |
| Road network | ||
| City street | 26,238 (56.4) | 3,361 (52.7) |
| Highway | 3,006 (6.5) | 723 (11.3) |
| Rural road | 5,745 (12.3) | 1,497 (23.4) |
| Other | 11,537 (24.8) | 801 (12.6) |
a45 missing data
b10 missing data
AIS ≥2 group: trauma patients presenting with at least one injury AIS≥2.
AISThorax≥2 group: trauma patients presenting with at least one thoracic injury AIS≥2.
AIS: abbreviated injury scale.
Fig 1. Road traffic accident among the AISThorax≥2 group per 100,000 inhabitants in the Rhône area population.
Subgroups according to the age. AISThorax≥2 group: trauma patients presenting with at least one thoracic injury AIS≥2.AIS: abbreviated injury scale.
Fig 2. Road user category distribution among the AISThorax≥2 group.
Subgroups according to the age. AISThorax≥2 group: trauma patients presenting with at least one thoracic injury AIS≥2. AIS: abbreviated injury scale. MAIS: maximum abbreviated injury scale.
Injury pattern
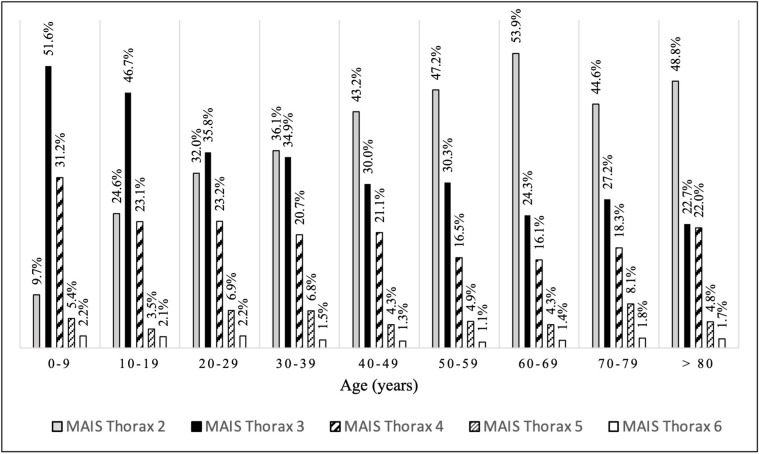
A total of 8,729 thoracic injuries were reported (some patients may have sustained multiple thoracic injuries). Of these, chest wall injuries were the most frequent (62.1%, n = 5,419), over half of which were multiple rib fractures (52.4%). Lung injuries were the second most frequent type of thoracic injuries (24.7%, n = 2,158), 88.7% of which were lung contusions. Pleural injuries (including pneumothorax and haemothorax) were found in 5.3% (n = 466) of cases (Table 2). The frequency of MAISThorax = 2 injuries increased with age while that of MAISThorax = 3 injuries decreased (Fig 3). The most frequent concomitant AIS≥2 extra-thoracic injuries affected the head (29.1%), upper extremities (26.8%) and lower extremities (25.8%) The head (19.9%) was the most serious (AIS≥3) concomitant body area injured (Table 3).
Table 2. Description of thoracic injuries in the AISThorax≥2 group.
| Injury characteristicsa | n (%) |
|---|---|
| Chest wall injuries | 5,419/8,729 (62.1) |
| Multiple rib fracture | 2,842/5,419 (52.4) |
| Sternal fracture | 1,719/5,419 (31.7) |
| Flail chest | 478/5,419 (8.8) |
| Single rib fracture | 276/5,419 (5.1) |
| Other | 104/5,419 (2) |
| Lung injuries | 2,158/8,729 (24.7) |
| Pulmonary contusion | 1,914/2,158 (88.7) |
| Pulmonary laceration | 244/2,158 (11.3) |
| Pleural and mediastinal injuries | 466/8,729 (5.3) |
| Pneumo and/or haemothorax | 352/466 (75.5) |
| Pneumo and/or haemomediastinum | 105/466 (22.5) |
| Other | 9/466 (2) |
| Cardiac or vascular injuries | 421/8,729 (4.8) |
| Cardiac | 227/421 (54) |
| Thoracic aorta | 120/421 (28.5) |
| Pulmonary arteries/veins | 46/421 (11) |
| Coronary artery | 12/421 (2.9) |
| Subclavian artery/vein | 10/421 (2.4) |
| Other | 5/421 (1.2) |
| Other injuries | 265/8,729 (3) |
| Skin injuries | 151/265 (57) |
| Diaphragmatic injuries | 83/265 (31.3) |
| Tracheal and bronchial injuries | 21/265 (7.9) |
| Oesophageal injuries | 10/265 (3.8) |
aNo missing data
One patient could have suffered from multiple thoracic injuries, therefore the total of injuries (n = 8,729) presented in the table is greater than the number of AISThorax≥2 patients (n = 6,382).
AISThorax≥2 group: trauma patients presenting with at least one thoracic injury AIS≥2.
AIS: abbreviated injury scale.
Fig 3. Thoracic MAIS distribution among the AISThorax≥2 group.
Subgroups according to the age. AISThorax≥2 group: trauma patients presenting with at least one thoracic injury AIS≥2. AIS: abbreviated injury scale. MAIS: maximum abbreviated injury scale.
Table 3. Concomitant extra-thoracic injuries between AISThorax≥2 group and AISThorax<2 group.
| Body regiona | AIS≥2 group | AISThorax≥2 group |
|---|---|---|
| (n = 46,526) | (n = 6,382) | |
| Head | n (%) | n (%) |
| AIS≥2 | 12,096 (26) | 1,855 (29.1) |
| AIS≥3 | 3,162 (6.8) | 1,268 (19.9) |
| Face | ||
| AIS≥2 | 2,181 (4.7) | 477 (7.5) |
| AIS≥3 | 186 (0.4) | 93 (1.5) |
| Neck | ||
| AIS≥2 | 132 (0.3) | 68 (1.1) |
| AIS≥3 | 59 (0.1) | 33 (0.3) |
| Abdomen/pelvis | ||
| AIS≥2 | 2,087 (4.5) | 1,143 (17.9) |
| AIS≥3 | 1,005 (2.2) | 604 (9.5) |
| Spine | ||
| AIS≥2 | 3,438 (7.4) | 1039 (16.3) |
| AIS≥3 | 731 (1.6) | 322 (5.0) |
| Upper extremity | ||
| AIS≥2 | 19,038 (40.9) | 1,713 (26.8) |
| AIS≥3 | 3,363 (7.2) | 454 (7.1) |
| Lower extremity | ||
| AIS≥2 | 15,198 (32.7) | 1,646 (25.8) |
| AIS≥3 | 5,032 (10.8) | 987 (15.5) |
| Skin | ||
| AIS≥2 | 69 (0.1) | 5 (0.08) |
| AIS≥3 | 42 (0.09) | 2 (0.03) |
aNo missing data
AIS≥2 group: trauma patients presenting with at least one injury AIS≥2.
AISThorax≥2 group: trauma patients presenting with at least one thoracic injury AIS≥2.
AIS: abbreviated injury scale.
Severity and mortality
The median ISS [IQR]was 14 [6–27]. A total of 30.8% (n = 1,968) thoracic trauma patients were admitted to an ICU, and 16.2% (n = 1,031) patients died (respectively 17.4%, 16.6%, 16.8%, 13.5% of included patients by time-period as described in Table 1). Of those, 61.5% (n = 634) died on-scene. Among those admitted to hospital (n = 397), 37.3% (n = 148) died during the first 24 hours, and 75.6% (n = 300) died within the first three days. Thoracic injuries were the cause of death for 42.7% (n = 440) of our 1,031 deceased patients. Pedestrians had the highest mortality proportion (30.6%, n = 207), followed by motorcyclists (17.6%, n = 285), car occupants (13.6%, n = 455) and cyclists (10.5%, n = 46). A total of 1.4% (n = 36) MAISThorax = 2 patients died while 7.9% (n = 164) with MAISThorax = 3 died, and 47.3% (n = 831/1757) patients with MAISThorax ≥4 died.
Impact of thoracic trauma on mortality and other factors associated with mortality
We investigated the influence of serious (AIS ≥ 3) thoracic injuries on traumatic mortality compared to other serious injuries. Our multivariate analysis revealed that patients with serious traumatic brain injuries were associated with a higher risk of death (OR = 27.9, 95%CI [21.3–36.7]) than those with serious thoracic injuries (OR = 12.4, 95%CI [8.6–18.0]).
Other factors associated with mortality in the AIS≥2 group were all age groups above 39 years compared to 20–39 years group, male sex (OR = 1.4, 95%CI [1.2–1.7]), RTA occurring in a highway (OR = 1.8, 95%CI [1.5–2.3]) or a rural road (OR = 1.8, 95%CI [1.5–2.1]) compared to those in a city street (Table 4).
Table 4. Predictors of mortality in multivariate analysis in AIS≥2 group.
| OR [95%CI] | |
|---|---|
| Body region a | |
| Head | 27.9 [21.3–36.7] |
| Face | 11.5 [7.3–18.2] |
| Neck | 2.4 [0.8–6.8] |
| Thorax | 12.4 [8.6–18.0] |
| Abdomen and pelvis | 10.8 [7.5–15.4] |
| Spine | 3.4 [2.4–4.7] |
| Upper extremity | 2.7 [2.1–3.5] |
| Lower extremity | 5.2 [4.1–6.5] |
| Age, years | |
| 0–9 | 0.5 [0.3–0.8] |
| 10–19 | 0.7 [0.5–0.8] |
| 20–39 | 1 |
| 40–59 | 1.3 [1.1–1.6] |
| 60–79 | 2.1 [1.7–2.6] |
| ≥ 80 | 6.1 [4.6–8.0] |
| Sex, male | 1.4 [1.2–1.7] |
| Road user | |
| Car occupants | 1 |
| Pedestrians | 1.1 [0.9–1.4] |
| Bicyclists | 0.4 [0.3–0.6] |
| Motorcyclists | 0.8 [0.7–1.0] |
| Other | 0.8 [0.6–1.1] |
| Road network | |
| City street | 1 |
| Highway | 1.8 [1.5–2.3] |
| Rural road | 1.8 [1.5–2.1] |
| Other | 0.5 [0.4–0.6] |
| Year of inclusion | 0.95 [0.94–0.96] |
a Impact of a MAIS ≥3 injury compared to a MAIS = 2 injury in the same body region
AIS≥2 group: trauma patients presenting with at least one injury AIS≥2, MAIS: Maximum abbreviated injury scale. p<0.001 for all variables.
Discussion
The results of our study show that moderate to lethal RTA-related thoracic injuries were surprisingly rare, affecting less than four out of every 100 patients, and most frequently occurred in middle-aged male patients.
We have found a lower incidence of thoracic trauma compared to the numbers previously reported [10, 16, 17]. Peek et al. recently reported that single rib fracture accounted for 20% of rib fracture cases [18, 19]. This difference may be explained by the fact that we chose not to include these patients. Indeed, we did not include minor injuries because previous studies have demonstrated that these single rib fractures were not associated with mortality [10]. Another explanation could be that the present study may suffer a measurement bias in the late 90’s and early 2000s because some patient may have undergone a traditional selected CT scan that did not explore the thorax. The recent democratization of whole body computed tomography (WBCT) which became standard practice in many centers over the world in the last two decades resulted in more diagnosed injuries [20]. Another interesting finding of the present study is the evolution of AISThorax 2 and 3 with age. Children aged between 0 and 9 years had the highest incidence of AIS 3 injuries, and this decreased with age. This finding is similar to Samarasekera et al.’s, as they reported a very high incidence of AIS>2 thoracic injuries (88%) among children aged under 15years, 65% of which being lung contusions. The more compressible and incompletely calcified thoracic skeleton of children, which allows the transmission of large forces to the thoracic cavity structures, making rib fractures uncommon, may partially explain this. Thus, high-energy impact trauma may cause major internal injuries with little evidence of external injuries or fractures of the bony thorax as reported by many authors [12, 21, 22]. Furthermore, since children are more frequently involved in RTA as pedestrians, they may be at higher risk of projection and severe trauma as a result of a direct impact with the front bumper because of their height. In contrast, the incidence of moderate (AIS = 2) thoracic injuries increased with age. These injuries are mainly rib fractures. which, in older patients, were reported to be a frequent consequence of a RTA [23]. With muscle atrophy and osteoporosis, which are commonly associated with older age, less force may be required to cause rib fractures in this population. Herein, mortality was similar to that reported by several authors [7, 10, 24]. Other studies showed lower mortality rates (5% and 5.5%) [13, 25] but these only included patients reaching the hospital with vital signs, whereas on-scene dead patients were not excluded from our analyses. Had these patients been excluded, our mortality rate would have been 6.2%. Similarly to other authors [10], we have found serious thoracic trauma were also strongly associated with patient mortality, as three-quarters serious thoracic trauma-related deaths occurred within the first 24 hours. This contradicts Grubmüller et al.’s results, which found no association between the presence of serious thoracic trauma and mortality [24]. This may be explained by the potential limited external validity of their results, as their study included patients from a single high-volume level-I trauma center. It was indeed suggested in the literature that the hospital volume of severely injured patients may be an independent predictor of survival [26, 27]. In addition to the fact that our study included data from multiple centers with different levels of trauma care designation, their population is different than ours as they excluded patients with penetrating trauma and those in whom resuscitation efforts outside the hospital have failed.
One major strength of the present study was the inclusion of on-scene deceased patients without inducing any misclassification bias because an autopsy was systematically undertaken in those patients to confirm the cause of death and provide a complete injury assessment based on AIS scoring. Furthermore, our large multicenters cohort which includes consecutive patients from the past 20 years is a non-negligeable strength.
This study has several limitations, including the update of AIS during the study period [28]. Nevertheless, we chose to base severity assessment on the widely used AIS because it is an accurate, objective and validated method to independently evaluate the impact of each body region on mortality [29]. Besides, Hsu et al. [30] found that the AIS update had no impact on mean ISS when considering the thoracic body region. Furthermore, our retrospective study design, with its known weaknesses, may be considered a limit. However, the present study is based on prospectively collected multicenters data over a 20-year-period including level I to III trauma centers and included patients of all ages whereas many studies focused on thoracic trauma are single center studies and only included patients ≥16 years [7, 9, 13, 16, 24, 31]. Also, our secondary outcome relies on an anatomic system of injury classification (AIS and ISS) since the database does not report physiological assessment nor medical management. Therefore, there is no data regarding prehospital management, time to surgery, ICU management such as airway and ventilation management, use of vasopressors or massive blood transfusion, and no detail on organ and respiratory failure or pre-existing chronic comorbid diseases which have been reported to influence outcome in thoracic trauma patients [8–10, 24]. The value of anatomic scoring systems in outcome prediction of trauma patients has been debated and compared to physiological scores. Some authors found the ISS to be a better severity predictor than the revised Trauma Scale (RTS) and the simplified acute physiology scale II (SAPS II) [32]. Hence, we believe that using anatomic scoring in the present study is as efficient as physiological scoring in predicting outcomes. At last, we included patients prior to the adoption of WBCT which may have contributed to underreporting of some injuries such as pulmonary contusions and rib fractures.
Conclusion
Moderate to lethal RTA-related thoracic injuries were rare. Multiple ribs fractures, pulmonary contusions, and sternal fractures were the most frequent anatomical injuries. The incidence, injury pattern and mechanisms greatly vary across age groups.
Acknowledgments
The authors would like to thank Philip Robinson for his linguistic advice with this manuscript and everyone who participated in the data collection and data recording for the Rhône Road Accident Registry Association (ARVAC: president, E. Javouhey), and University Gustave Eiffel–campus of Lyon–TS2-Umrestte (scientific coordinator, B. Laumon, medical coordinator, A. Ndiaye and administrative coordinator, B. Gadegbeku).
Data Availability
All relevant data are within the paper.
Funding Statement
The Rhône registry is supported by the Gustave Eiffel university, the French public health agency and the road safety directorate (ministry of the interior). The authors declare that the funding sources had no role in the conduct, analysis, interpretation, or writing of this manuscript.
References
- 1.World Health Organization, issuing body. Global status report on road safety 2018. 2018. [Google Scholar]
- 2.World Health Organization. Global status report on road safety 2013: supporting a decade of action. Geneva, Switzerland: WHO; 2013. [Google Scholar]
- 3.Vécsei V, Arbes S, Aldrian S, Nau T. Chest Injuries in Polytrauma. Eur J Trauma Emerg Surg. 2005; 31:239–243. 10.1007/s00068-005-2033-9 [DOI] [Google Scholar]
- 4.van Rein EAJ, Lokerman RD, van der Sluijs R, Hjortnaes J, Lichtveld RA, Leenen LPH, et al. Identification of thoracic injuries by emergency medical services providers among trauma patients. Injury. 2019; 50(5):1036–41. doi: 10.1016/j.injury.2018.12.003 [DOI] [PubMed] [Google Scholar]
- 5.Zhang S, Xiao X, Wang J, Hu C, Du Q, Fu Z, et al. Epidemiological and clinical characteristics of road traffic crashes related thoracic traumas: analysis of 5095 hospitalized chest injury patients. J Cardiothorac Surg. 2021; 16:220. doi: 10.1186/s13019-021-01599-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lecky FE, Bouamra O, Woodford M, Alexandrescu R, O’Brien SJ. In: Pape H-C, Peitzman AB, Schwab CW, Giannoudis PV, editors. Epidemiology of polytrauma. New York: Springer: Damage Control Management in the Polytrauma Patient; 2010. p. 13–24.4. [Google Scholar]
- 7.Veysi VT, Nikolaou VS, Paliobeis C, Efstathopoulos N, Giannoudis PV. Prevalence of chest trauma, associated injuries and mortality: a level I trauma centre experience. Int Orthop. 2009; 33:1425–33. doi: 10.1007/s00264-009-0746-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Battle CE, Hutchings H, Evans PA. Risk factors that predict mortality in patients with blunt chest wall trauma: A systematic review and meta-analysis. Injury. 2012; 43:8–17. doi: 10.1016/j.injury.2011.01.004 [DOI] [PubMed] [Google Scholar]
- 9.Battle CE, Hutchings H, Lovett S, Bouamra O, Jones S, Sen A, et al. Predicting outcomes after blunt chest wall trauma: development and external validation of a new prognostic model. Crit Care. 2014; 18(3):R98. doi: 10.1186/cc13873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Huber S, Biberthaler P, Delhey P, Trentzsch H, Winter H, van Griensven M, et al. Predictors of poor outcomes after significant chest trauma in multiply injured patients: a retrospective analysis from the German Trauma Registry (Trauma Register DGU®). Scand J Trauma Resusc Emerg Med. 2014; 22:52. doi: 10.1186/s13049-014-0052-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.TraumaRegister DGU, Bayer J, Lefering R, Reinhardt S, Kühle J, Zwingmann J, et al. Thoracic trauma severity contributes to differences in intensive care therapy and mortality of severely injured patients: analysis based on the TraumaRegister DGU®. World J Emerg Surg. 2017;12:43. doi: 10.1186/s13017-017-0154-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ostermann RC, Joestl J, Lang N, Tiefenboeck TM, Ohnesorg S, Platzer P, et al. Thoracic Injuries in Pediatric Polytraumatized Patients: Epidemiology, Treatment and Outcome. Injury. 2021; S0020138321001364. doi: 10.1016/j.injury.2021.02.033 [DOI] [PubMed] [Google Scholar]
- 13.Chrysou K, Halat G, Hoksch B, Schmid RA, Kocher GJ. Lessons from a large trauma center: impact of blunt chest trauma in polytrauma patients—still a relevant problem? Scand J Trauma Resusc Emerg Med. 2017;25(1):42. doi: 10.1186/s13049-017-0384-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Abbreviated Injury Scale (AIS). Association for the Advancement of Automotive Medicine. 2019. [cited 7 December 2021]. Available from: https://www.aaam.org/abbreviated-injury-scale-ais/ [Google Scholar]
- 15.Paparel P, N’Diaye A, Laumon B, Caillot J-L, Perrin P, Ruffion A. The epidemiology of trauma of the genitourinary system after traffic accidents: analysis of a register of over 43 000 victims. BJU Int. 2006; 97:338–41. doi: 10.1111/j.1464-410X.2006.05900.x [DOI] [PubMed] [Google Scholar]
- 16.Beshay M, Mertzlufft F, Kottkamp HW, Reymond M, Schmid RA, Branscheid D, et al. Analysis of risk factors in thoracic trauma patients with a comparison of a modern trauma centre: a mono-centre study. World J Emerg Surg. 2020; 15: 45. doi: 10.1186/s13017-020-00324-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.TraumaRegister DGU, Bayer J, Lefering R, Reinhardt S, Kühle J, Südkamp NP, et al. Severity-dependent differences in early management of thoracic trauma in severely injured patients—Analysis based on the TraumaRegister DGU®. Scand J Trauma Resusc Emerg Med. 2017; 25(1):10. doi: 10.1186/s13049-017-0354-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peek J, Ochen Y, Saillant N, Groenwold RHH, Leenen LPH, Uribe-Leitz T, et al. Traumatic rib fractures: a marker of severe injury. A nationwide study using the National Trauma Data Bank. Trauma Surg Acute Care Open. 2020; 5: e000441. doi: 10.1136/tsaco-2020-000441 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Peek J, Beks RB, Hietbrink F, De Jong MB, Heng M, Beeres FJP, et al. Epidemiology and outcome of rib fractures: a nationwide study in the Netherlands. Eur J Trauma Emerg Surg. 2020. doi: 10.1007/s00068-020-01412-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.TraumaRegistrer DGU®, Palm H-G, Kulla M, Wettberg M, Lefering R, Friemert B, et al. Changes in trauma management following the implementation of the whole-body computed tomography: a retrospective multi-centre study based on the trauma registry of the German Trauma Society (TraumaRegister DGU®). Eur J Trauma Emerg Surg. 2018; 44:759–66. doi: 10.1007/s00068-017-0870-y [DOI] [PubMed] [Google Scholar]
- 21.Balcı AE, Kazez A, Eren Ş, Ayan E, Özalp K, Eren MN. Blunt thoracic trauma in children: review of 137 cases. Eur J Cardiothoracic Sur. 2004; 26:387–92. doi: 10.1016/j.ejcts.2004.04.024 [DOI] [PubMed] [Google Scholar]
- 22.Bliss D, Silen M. Pediatric thoracic trauma: Critical Care Med. 2002; 30:S409–15. doi: 10.1097/00003246-200211001-00005 [DOI] [PubMed] [Google Scholar]
- 23.Lee WY, Yee WY, Cameron PA, Bailey MJ. Road traffic injuries in the elderly. Emerg Med J. 2006; 23:42–6. doi: 10.1136/emj.2005.023754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Grubmüller M, Kerschbaum M, Diepold E, Angerpointner K, Nerlich M, Ernstberger A. Severe thoracic trauma–still an independent predictor for death in multiple injured patients? Scand J Trauma Resusc Emerg Med. 2018; 26(1):6. doi: 10.1186/s13049-017-0469-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Horst K, Andruszkow H, Weber CD, Pishnamaz M, Herren C, Zhi Q, et al. Thoracic trauma now and then: A 10 year experience from 16,773 severely injured patients. Puebla I, editor. PLoS One. 2017; 12:e0186712. doi: 10.1371/journal.pone.0186712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sewalt CA, Wiegers EJA, Venema E, Lecky FE, Schuit SCE, Hartog DD, et al. The volume-outcome relationship in severely injured patients: A systematic review and meta-analysis. J Trauma Acute Care Surg. 2018; 85:810–9. doi: 10.1097/TA.0000000000002043 [DOI] [PubMed] [Google Scholar]
- 27.Zacher MT, Kanz K-G, Hanschen M, Häberle S, van Griensven M, Lefering R, et al. Association between volume of severely injured patients and mortality in German trauma hospitals. Br J Surg. 2015; 102:1213–9. doi: 10.1002/bjs.9866 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Loftis KL, Price J, Gillich PJ. Evolution of the Abbreviated Injury Scale: 1990–2015. Traffic Inj Prev. 2018; 19:S109–13. doi: 10.1080/15389588.2018.1512747 [DOI] [PubMed] [Google Scholar]
- 29.Clarke JR, Ragone AV, Greenwald L. Comparisons of survival predictions using survival risk ratios based on International Classification of Diseases, Ninth Revision and Abbreviated Injury Scale trauma diagnosis codes. J Trauma. 2005; 59:563–7; discussion 567–9. [PubMed] [Google Scholar]
- 30.Hsu S-Y, Wu S-C, Rau C-S, Hsieh T-M, Liu H-T, Huang C-Y, et al. Impact of Adapting the Abbreviated Injury Scale (AIS)-2005 from AIS-1998 on Injury Severity Scores and Clinical Outcome. Int J Environ Res Public Health. 2019;16(24):5033. doi: 10.3390/ijerph16245033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Söderlund T, Ikonen A, Pyhältö T, Handolin L. Factors associated with in-hospital outcomes in 594 consecutive patients suffering from severe blunt chest trauma. Scan J Surg. 2015; 104(2):115–20. doi: 10.1177/1457496914543976 [DOI] [PubMed] [Google Scholar]
- 32.Kahloul M, Bouida W, Boubaker H, Toumi S, Grissa MH, Jaafar A, et al. Value of anatomic and physiologic scoring systems in outcome prediction of trauma patients. Eur J Emerg Med. 2014; 21(2): 125–9. doi: 10.1097/MEJ.0b013e32836188ce [DOI] [PubMed] [Google Scholar]