Abstract
BACKGROUND:
There are well-known disparities for patients injured in rural setting versus urban setting. Many cite access to care; however, the mechanisms are not defined. One potential factor is differences in field triage. Our objective was to evaluate differences in prehospital undertriage (UT) in rural setting versus urban settings.
METHODS:
Adult patients in the Pennsylvania Trauma Outcomes Study (PTOS) registry 2000 to 2017 were included. Rural/urban setting was defined by county according to the Pennsylvania Trauma Systems Foundation. Rural/urban classification was performed for patients and centers. Undertriage was defined as patients meeting physiologic or anatomic triage criteria from the National Field Triage Guidelines who were not initially transported to a Level I or Level II trauma center. Logistic regression determined the association between UT and rural/urban setting, adjusting for transport distance and prehospital time. Models were expanded to evaluate the effect of individual triage criteria, trauma center setting, and transport mode on UT.
RESULTS:
There were 453,112 patients included (26% rural). Undertriage was higher in rural patients (8.6% vs. 3.4%, p < 0.01). Rural setting was associated with UT after adjusting for distance and prehospital time (odds ratio [OR], 3.52; 95% confidence interval [CI], 1.82–6.78; p < 0.01). Different triage criteria were associated with UT in rural/urban settings. Rural setting was associated with UT for patients transferred to an urban center (OR, 3.32; 95% CI, 1.75–6.25; p < 0.01), but not a rural center (OR, 0.68; 95% CI, 0.08–5.53; p = 0.72). Rural setting was associated with UT for ground (OR, 5.01; 95% CI, 2.65–9.46; p < 0.01) but not air transport (OR, 1.18; 95% CI, 0.54–2.55; p = 0.68).
CONCLUSION:
Undertriage is more common in rural settings. Specific triage criteria are associated with UT in rural settings. Lack of a rural trauma center requiring transfer to an urban center is a risk factor for UT of rural patients. Air medical transport mitigated the risk of UT in rural patients. Provider and system interventions may help reduce UT in rural settings.
LEVEL OF EVIDENCE:
Care Management, Level IV
Keywords: Triage, rural, prehospital, disparities, air-medical
Mortality and morbidity have improved in the United States with the advent of trauma systems.1-3 However, patients in rural areas of the United States do not benefit from trauma systems in the same way and are known to have higher mortality after injury.4-9 The mechanisms underlying this disparity are not clear but are postulated to arise from access to care barriers. Trauma is a time-sensitive disease, and rapid definitive care is critical in severely injured patients. Patients injured in a rural setting demonstrate early mortality after injury; with most deaths occurring within 24 hours and, notably, outside of a trauma center.3
Thus, one potential contributor to these outcome disparities in rural patients is undertriage in the field. Triage requires prehospital providers to identify patients with the potential for severe injuries and direct them to the appropriate level of trauma care using limited information in the field. National Field Triage Guidelines (NFTG) were developed by the American College of Surgeons Committee on Trauma and the Centers for Disease Control to assist prehospital providers with this task.10 The NFTG is a stepwise algorithm, including physiologic, anatomic, mechanism of injury, and special consideration criteria, structured in descending specificity for severe injury. Patients with physiologic or anatomic criteria should be brought to the highest level of trauma care within the system.
Further, one study of the NFTG reported that despite a greater sensitivity in the rural setting, only 12.5% were transported to a trauma center and just 39% received definitive care at a trauma center, highlighting the significant undertriage challenge for rural patients.11
Further, others have reported substantial delays in definitive care as a result of the decision to transport to a nontrauma center despite the appropriate recognition of severe injury by prehospital providers. The destination decision is based on a number of factors but is largely impacted by proximity of the scene of injury to a trauma center.3,12-14
It is evident that prehospital providers largely rely on heuristics and personal judgment for transport destination decisions. Particularly in rural regions, the decision is often made to transport severely injured patients to nearer nontrauma centers for the intent of stabilization.11,13 While this may make intuitive sense,15 recent studies suggest this strategy simply delays definitive management and increases mortality.7,14,16 Thus, it remains unclear if and how undertriage may contribute to worse outcomes for patients in the rural setting.
It was our objective to evaluate differences and risk factors for undertriage among patients injured in rural versus urban settings. We hypothesized that undertriage would be greater among rural patients and lack of trauma system resources in rural areas would increase the risk of undertriage.
METHODS
Study Population
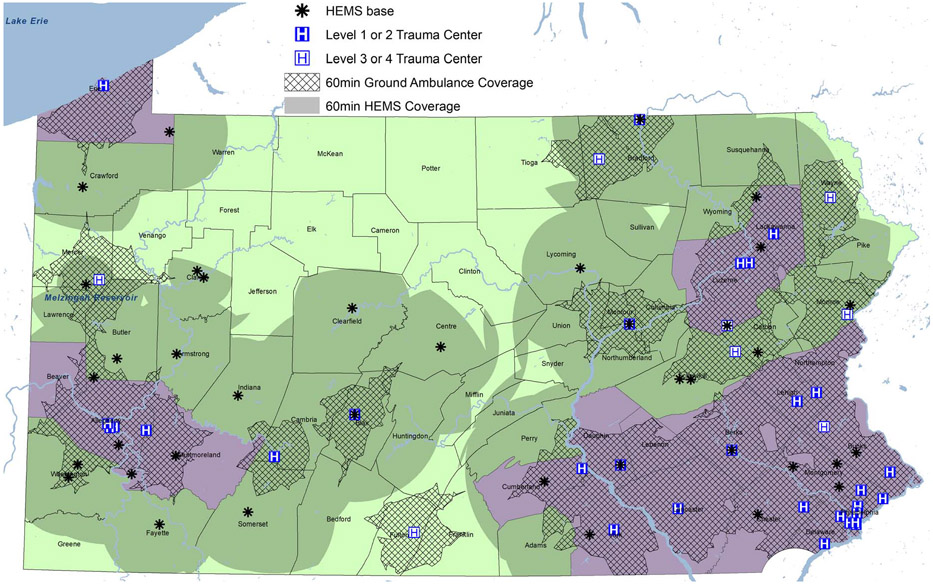
We utilized the Pennsylvania Trauma Outcomes Study (PTOS) registry and included subjects 16 years and older, who sustained blunt or penetrating trauma and were transported from the scene of injury between 2000 and 2017. Rural versus urban classification was determined at the county-level in Pennsylvania (Fig. 1). Designation was defined by county-level population density according to 2010 Pennsylvania Census data. Rural counties were defined as those with population densities less than the overall population density of the entire state and urban for county population densities exceeding this threshold (284 persons/square mile).17 Each patient was then classified as having a rural or urban location of injury based on the county where injured. For interpretation of the analyses, designation as rural or urban location of injury indicates the geographic setting, rather than confinement to a particular county within that given setting. Similarly, trauma centers were classified as located in rural or urban counties. Patients with missing county data were excluded from analysis. Demographics, injury characteristics and severity, prehospital and admission vital signs, International Classification of Diseases—9th Revision Diagnosis codes, disposition, procedures, complications, and outcomes were abstracted.
Figure 1.
Urban and rural counties with trauma center and helicopter base locations in Pennsylvania. Urban counties are shaded purple while rural counties are shaded green. Sixty-minute coverage areas are overlaid.
Geospatial Analysis
Trauma centers and helicopter emergency medical services (HEMS) bases in Pennsylvania were geocoded and mapped. Transport distance for each patient was calculated using the patient's zip code geometric centroid and receiving trauma center location. The distance between each patient zip centroid to the receiving trauma center was then calculated based on the mode of transport to the trauma center.
Patients transported by HEMS had Euclidean distance calculated for straight-line flight. Patients transported by ground ambulance had driving distance calculated using network analysis. Network analysis used street maps to connect location points from the zip centroid to the trauma center, and therefore, shortest traveling distances along the road network were estimated between these locations.
Coverage areas for HEMS and ground ambulance were devised to represent the geographic area covered by the respective transport modality within 60 minutes of injury. The 60-minute HEMS coverage represents the area that a helicopter could leave the base, go to the scene and subsequently travel to the closest Level I or Level II trauma center (assuming 120 mph cruising speed) while accounting for a 21-minute scene time and 4 minute activation time based on average prehospital times in the PTOS data. The 60-minute ground ambulance coverage represents the drive time to each trauma center. The coverage area includes a 31-minute transport time accounting for an 11-minute response time and 18-minute scene time in rural counties, and a 35-minute transport time accounting for a 9-minute response time and 16-minute scene time in urban counties based on average prehospital times in the PTOS data. All geospatial analyses were performed using ArcGIS v10.5 software (ESRI, Redlands, CA).
Triage Criteria
Positive triage criteria were identified for patients who fulfilled NFTG physiologic or anatomic criteria based on prehospital data and International Classification of Diseases—9th Rev.—Clinical Modification diagnosis codes. Physiologic criteria included Glasgow Coma Scale (GCS) total score of 13 or less, systolic blood pressure less than 90 mm Hg, respiratory rate less than 10 or greater than 29, or need for ventilator. Anatomic criteria included penetrating injury, pelvic fracture, unstable chest wall fracture, 2 or greater proximal long bone fractures, crush injury, open skull fracture, amputation, and paralysis. Patients were categorized as undertriaged if they met any of the physiologic or anatomic NFTG criteria and were not transported to a Level I or Level II trauma center initially.
Statistical Analysis
The primary outcome measure was undertriage. First, we assessed the association of in-hospital mortality and undertriage adjusted for age, Injury Severity Score (ISS), and transport distance using logistic regression to establish the importance of undertriage as a process of care outcome in our study population. Logistic regression was then used to determine the association between undertriage and patient rural versus urban setting, adjusted for transport distance and total prehospital time. Next, we evaluated the association of undertriage with the presence of each of the 11 physiologic and anatomic NFTG criteria, adjusted for transport distance and total prehospital time, to determine if rural and urban patients who were undertriaged had different triage criteria profiles.
We then repeated the model to evaluate the association between undertriage and patient setting while testing the interaction between patient setting and trauma center setting (rural versus urban), as well as the interaction between patient setting and transport mode (ground versus air transport). For significant interactions, the model was stratified to determine how the risk of undertriage was modified in these different settings or by transport mode. All models used robust variance estimators to account for clustering at the center level.
Continuous and categorical data are reported as median (interquartile range) and frequency (percentage), respectively. For univariate comparisons, χ2 or Mann-Whitney U tests were used as appropriate to the data. Results from the logistic regression models are reported as adjusted odds ratio (aOR) and 95% confidence intervals (95% CI). Absolute standardized differences were used to assess the balance of patient demographics and characteristics between groups. The standardized difference represents the difference between groups divided by the pooled standard deviation, making it insensitive to large samples sizes, and an absolute standardized difference greater than 0.1 represents significant nonoverlap in the distributions of a given variable between the two groups.18 Reported p values were two-tailed with a value less than 0.05 considered statistically significant. Data analysis was conducted using STATA 16MP (StataCorps LP, College Station, TX).
Subgroup Analysis
To further characterize how proximity of trauma system resources may impact undertriage in rural areas, we separately evaluated patients injured in rural counties in Pennsylvania. Each individual rural county was categorized as having access to trauma system resources (presence of a trauma center of any level or HEMS bases in the county) or those without access to trauma system resources. We evaluated differences in transport distances, total prehospital time, and undertriage between patients injured in the specific rural counties with and without access to trauma system resources. We then evaluated the association of undertriage with access to trauma system resources in rural counties using similar multivariable logistic regression models described above.
RESULTS
Among the 453,112 patients included, 116,501 (26%) were injured in rural counties and 336,611 (74%) were injured in urban counties. Comparisons of patient demographics and prehospital characteristics between rural and urban populations are demonstrated in Table 1. Those injured in rural counties experienced longer transport distance and prehospital time, more frequent HEMS transport, but less penetrating injury. Demographics and injury severity were similar as indicated by absolute standard differences.
TABLE 1.
Patient Demographics and Prehospital Characteristic Differences Between Rural and Urban Patients
| Rural (n = 116,501) | Urban (n = 336,611) | Absolute Standardized Difference | |
|---|---|---|---|
| Age | 52 (32–73) | 53 (32–76) | 0.052 |
| Sex (male) | 71,320 (61.2%) | 201,381 (59.8%) | 0.028 |
| ISS | 9 (5–16) | 9 (5–17) | 0.057 |
| GCS ≤ 13 | 11,643 (20.1%) | 37,018 (18.7%) | 0.034 |
| SBP <90 mmHg | 2,272 (3.7%) | 9,742 (4.9%) | 0.062 |
| RR <10 or >29 bpm | 4,832 (7.9%) | 11,746 (5.8%) | 0.083 |
| Penetrating injury | 5,438 (4.7%) | 35,423 (10.5%) | 0.222* |
| Flail chest | 1,038 (0.9%) | 2,076 (0.6%) | 0.032 |
| Open skull fracture | 1,220 (1.0%) | 4,371 (1.3%) | 0.023 |
| ≥2 long bone fractures | 2,313 (2.0%) | 6,365 (1.9%) | 0.007 |
| Pelvic fracture | 9,125 (7.8%) | 23,935 (7.1%) | 0.027 |
| Crush injury | 452 (0.4%) | 892 (0.3%) | 0.022 |
| Amputation | 259 (0.2%) | 509 (0.2%) | 0.016 |
| Paralysis | 608 (0.5%) | 1,650 (0.5%) | 0.004 |
| Distance (miles) | 30.7 (17.4, 47.9) | 7.5 (4.0, 14.9) | 1.025* |
| Prehospital time (minutes) | 59 (46, 81) | 42 (32, 54) | 0.473* |
| HEMS transport | 27,290 (31.0%) | 22,410 (8.4%) | 0.593* |
| Undertriage | 9,985 (8.6%) | 11,293 (3.4%) | 0.222* |
| Mortality | 5,911 (5.1%) | 20,041 (6.0%) | 0.039 |
Absolute values for the standardized difference > 0.1 represent significant imbalance between groups in the distributions of the variable indicated.
Continuous variables presented as median (IQR).
Categorical variables presented as n (%).
SBP, systolic blood pressure; RR, respiratory rate.
Patients who were undertriaged were transported farther (23.4 miles vs. 10.0 miles; p < 0.01), had longer prehospital time (218 minutes vs. 45 minutes; p < 0.01), and higher mortality rates (6.4% vs. 5.7%, p < 0.01) when compared with patients who were not undertriaged. Undertriage was associated with a 17% increase in the odds of adjusted mortality among all patients (aOR, 1.17; 95% CI, 1.09–1.25; p < 0.01).
Undertriage was higher among rural patients compared with urban patients (8.6% vs. 3.4%; p < 0.01). Patients injured in a rural setting had 3.5-fold higher odds of undertriage after adjusting for transport distance and prehospital time (OR, 3.52; 95% CI, 1.82–6.78; p < 0.01).
Evaluation of specific triage criteria confirmed different profiles of risk for undertriage among rural patients compared with urban patients (Fig. 2). These criteria overall demonstrated a pattern of higher odds of undertriage among rural patients compared with urban patients. Crush injury, GCS score 13 or less, and penetrating injury were the top criteria predicting undertriage among rural patients; while pelvic fracture, paralysis, and GCS score 13 or less were the top predictors of undertriage among urban patients.
Figure 2.
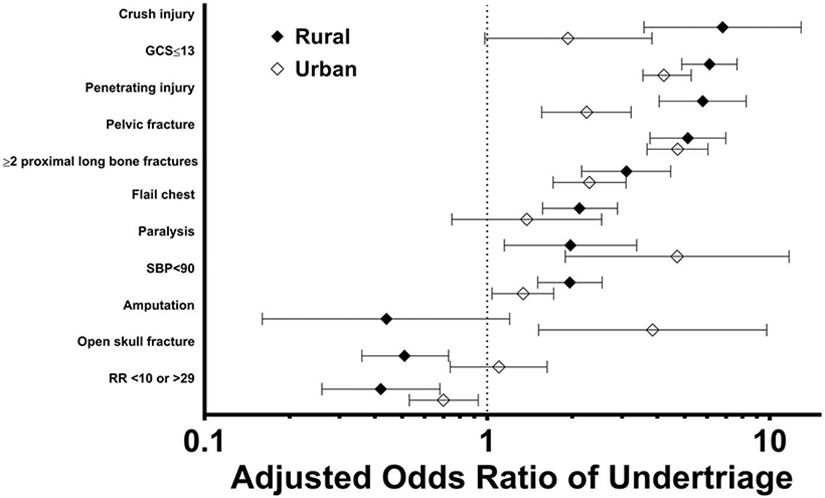
aOR and 95% CIs of undertriage for each of the physiologic and anatomic triage criteria in the National Field Triage Guidelines. Solid black diamonds represent effect in rural setting; hollow diamonds represent effect in urban setting. Error bars represent 95% CI. 95% CI crossing OR of 1.0 (vertical dotted line) are nonsignificant.
The interaction between patient setting and trauma center setting was significant (p < 0.01). When stratifying the model (Fig. 3), patients injured in a rural setting had more than threefold higher odds of undertriage when ultimately treated at a trauma center in an urban setting (aOR, 3.32; 95% CI, 1.75–6.25; p < 0.01). However, rural setting of injury was not associated with undertriage when the patient was ultimately treated at a trauma center in a rural setting (aOR, 0.68; 95% CI, 0.08–5.53; p = 0.72). Notably, this trauma center did not have to be within the county of injury, rather within any of the surrounding rural regions that contained a trauma center.
Figure 3.
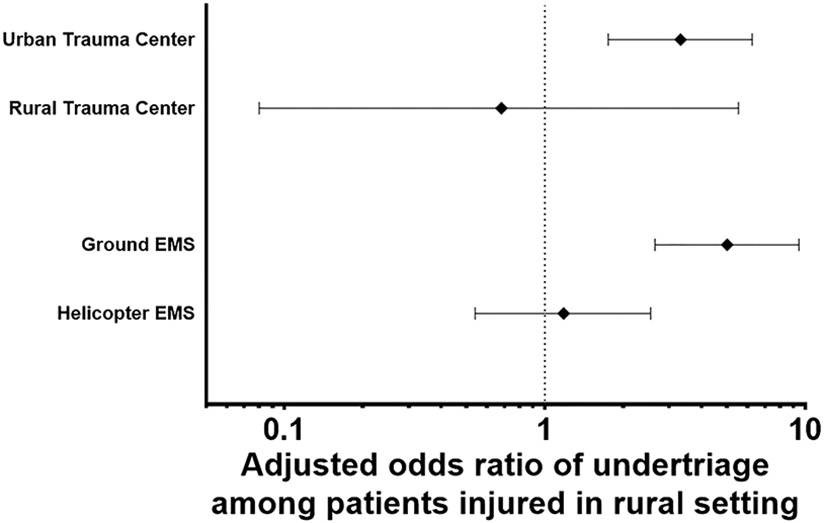
aOR and 95% CI of undertriage among patients injured in a rural setting for stratified models of urban versus rural trauma center and transport mode. Solid black diamonds represent point estimate of the OR. Error bars represent 95% CI. 95% CI crossing OR of 1.0 (vertical dotted line) are nonsignificant.
The interaction between patient setting and transport mode was also significant (p < 0.01). When stratifying the model (Fig. 3), patients injured in a rural setting had more than fivefold higher odds of undertriage when transported by ground ambulance (aOR, 5.01; 95% CI, 2.65–9.46; p < 0.01). Conversely, rural setting of injury was not associated with undertriage when the patient was transported by HEMS (aOR, 1.18; 95% CI, 0.54–2.55; p = 0.68).
Of the 48 rural counties, 26 did not have any trauma system resources located within them. These counties accounted for only 28.3% of the rural patient population. Patients injured in rural counties without trauma system resources had longer transport distances, prehospital time, and more frequent HEMS transport. Patients injured in rural counties without trauma systems resources also had slightly higher injury severity by absolute standardized difference, but this is likely not a clinically significant difference (Table 2). Demographics and injury characteristics were otherwise similar between the groups. Patients from rural counties with trauma system resources had lower unadjusted undertriage (8.2% vs. 9.4%, p < 0.01) and mortality (4.9% vs. 5.6%, p < 0.01) than patients from counties without trauma system resources. However, when adjusting for prehospital time, transport distance, transport mode, and ISS, the risk of undertriage was no longer associated with presence or absence of trauma system resources (aOR, 0.85; 95% CI 0.40–1.80; p = 0.67), indicating the presence of trauma system resources within the rural county of injury was not protective for undertriage compared with absence of these resources. As a point of distinction, rurally injured patients that had access to trauma system resources within a rural region (not limited to the specific rural county of injury) saw a mitigated risk of undertriage when compared with urban patients. However, as demonstrated in this subgroup analysis, these resources do not need to be located within every rural county as the differences between rural only patients showed no significance after adjustment for the presence of trauma system resources within the specific county of injury.
TABLE 2.
Patient Demographics and Prehospital Characteristic Differences Between Rural Patients With and Without County Resources
| No Resources (n = 32,980) | Resources (n = 83,521) | Absolute Standardized Difference | |
|---|---|---|---|
| Age | 52 (31–72) | 52 (32–73) | 0.039 |
| Sex (male) | 20,800 (63.1%) | 50,520 (60.5%) | 0.053 |
| ISS | 10 (5–17) | 9 (5–16) | 0.131* |
| GCS score ≤ 13 | 3,476 (21.5%) | 8,167 (19.6%) | 0.048 |
| SBP <90 mm Hg | 689 (3.9%) | 1,583 (3.6%) | 0.019 |
| RR <10 or >29 bpm | 1,592 (9.3%) | 3,240 (7.4%) | 0.07 |
| Penetrating injury | 1,582 (4.8%) | 3,856 (4.6%) | 0.009 |
| Flail chest | 341 (1.0%) | 697 (0.8%) | 0.021 |
| Open skull fracture | 420 (1.3%) | 800 (1.0%) | 0.03 |
| ≥2 long bone fractures | 768 (2.3%) | 1,545 (1.8%) | 0.033 |
| Pelvic fracture | 2,786 (8.4%) | 6,339 (7.6%) | 0.032 |
| Crush injury | 148 (0.4%) | 304 (0.4%) | 0.013 |
| Amputation | 92 (0.3%) | 167 (0.2%) | 0.016 |
| Paralysis | 193 (0.6%) | 415 (0.5%) | 0.012 |
| Distance (miles) | 40.8 (23.7, 63.1) | 27.6 (15.0, 41.3) | 0.473* |
| Prehospital time (minutes) | 69 (55, 99) | 56 (44, 75) | 0.288* |
| HEMS transport | 9,172 (36.9%) | 18,118 (28.6%) | 0.177* |
| Undertriage | 3,107 (9.4%) | 6,878 (8.2%) | 0.042 |
| Mortality | 1,840 (5.6%) | 4,071 (4.9%) | 0.032 |
Absolute values for the standardized difference > 0.1 represent significant imbalance between groups in the distributions of the variable indicated.
Continuous variables presented as median (IQR).
Categorical variables presented as n (%).
DISCUSSION
We found that undertriage is higher in the rural setting which in turn is associated with increased mortality. The injury pattern in undertriaged rural patients is distinct from those in urban settings. Additionally, availability of a trauma center in a rural region and air medical transport mitigated this risk of undertriage. Subgroup analysis demonstrated that these resources do not have to be directly located within the rural county of injury to mitigate the risk of undertriage. Rather, the availability of trauma resources within the greater rural region afforded this protection. Patients injured in a rural setting who must leave the rural region to reach the nearest trauma center located within an urban center are at highest risk of undertriage. Our findings suggest that access to trauma care does play a role in outcome disparities for rural settings. Undertriage appears to be a contributing factor when there are barriers to access whether through trauma center proximity or availability of air transport.
Trauma system implementation has clearly reduced mortality in urban centers1-3; however, our results corroborate prior evidence that this mortality benefit has not yet translated to the rural setting.4-9,19,20 Only a fraction of the US population resides in rural counties, yet there is a disproportionately high mortality rate.5 The mechanism of this disparity among rurally injured patients has not been well delineated. Previous authors postulate factors, such as unwitnessed injuries resulting in delayed EMS dispatch (delayed discovery), greater injury severity owing to higher velocity vehicle collisions and heavy machinery injuries, increased prehospital time, and decreased geographic access to trauma system resources play a role.5,9
Our and other results would suggest that field undertriage contributes to the increased mortality in rural settings,7 with a nearly 20% increase in mortality among undertriaged patients. Undertriage rates up to 70% in rural regions3 have been reported. The danger of undertriage in rural settings is further underscored by several groups reporting more emergency department deaths in nontrauma centers compared with trauma centers.5,16,19 Additionally, several reports demonstrate higher transfusion requirements and mortality among severely injured patients not directly transported to a trauma center.1,14,16,21
There are two possible scenarios that may underlie our findings contributing to high undertriage in the rural setting. First, the patients are not recognized by providers as requiring trauma center care in the field. This may be due to underappreciation of the anatomic injury criteria or transient abnormal vital signs that meet criteria but normalize on repeat measurement. Despite evidence that even a single episode of field hypotension is a marker of severe injury,22,23 providers may believe transient abnormal physiology does not warrant the investment of time to transport the patient with seemingly normal vital signs to a distant trauma center. Rural EMS is often staffed with volunteer providers who are less experienced and may simply not recognize injuries that indicate a patient should be transported to a trauma center.
Second, and perhaps more common, EMS providers appropriately recognize severe injury that warrant trauma center care but transport the patient to the closest hospital under the guise of stabilization. Rurally injured patients who had access to a trauma center within a rural setting were not subject to increased undertriage. This observation appears consistent with EMS preference for minimizing transport distance, irrespective of trauma center needs or hospital designation.13 Further, in our analysis of individual triage criteria most associated with undertriage, criteria for rural patients were ostensibly the more overt severe injuries including crush injuries, multiple long bone fractures, and penetrating injuries. It appears, in some circumstances when faced with these obvious severe injury patterns, EMS providers weigh hospital proximity above trauma center need.
A qualitative study of EMS providers by Jones et al.13 provides additional insight into the field triage process. The EMS providers often deviate from triage guidelines and choose hospital destination based on dispatch information prior to scene arrival, on their initial scene assessment with priority given to mechanism and obvious anatomic injuries as well as their overall gestalt. In fact, the first vital signs are often obtained after the triage decision is made, and the patient is en route to the hospital. Particularly among rural providers, the self-reported priority was to deliver the patient to the nearest hospital. They cited concerns for lengthier transport times acknowledging that subsequent transfer to a trauma center would likely be required, with little concern expressed for the time to definitive care. Newgard et al.11 conducted a validation study of the NFTG, reporting that rural EMS providers demonstrate comparable sensitivity to detect trauma center need. Subsequent work by their group demonstrated that despite appropriate recognition of severe injury, only 29% of these patients were initially transported to a trauma center and that provider judgment and specifically proximity to hospital was the most common reason for transport to a nontrauma center.
Rural providers, again with exposure to a limited volume of severely injured patients, may be uncomfortable with the prospect of a prolonged transport of these patients to a trauma center.24 They may also believe that there is a benefit of physician evaluation and stabilization at a nontrauma center prior to transfer to higher-level care despite the fact this has not been corroborated in the literature.14,16
Our findings have implications for trauma systems to improve outcomes. Undertriage is a potential actionable target in rural regions to reduce mortality. Prehospital provider education focused on improved triage criteria guideline adherence while emphasizing potential detriments of initial transport to a nontrauma center is one strategy to mitigate undertriage. Certainly, there are scenarios in which transport to a nontrauma center is unavoidable, such as adverse weather precluding air transport, but for a significant proportion, this “pitstop” should be avoided. There also are super-rural or frontier regions of the country where the distance for ground transport to a trauma center is prohibitively far. For these situations, it is critical that the role of the nontrauma center is well defined. These centers must quickly stabilize the patient and prioritize transfer to the trauma center while limiting tests that will not change management at the nontrauma center.7,25
Further, we identified air transport as a mitigating factor for rural undertriage. Helicopter emergency medical services overcome the geographic barrier of trauma access for rural EMS providers owing to speed and straight-line flight path to the nearest trauma center. Branas et al.26 showed that approximately a quarter of the US population has access to a Level I or Level II trauma center within 60 minutes only by HEMS, representing nearly 82 million people. Given the population that relies on air transport for timely access to definitive trauma care, strategic geographic placement of new bases or relocation of existing ones represents the most feasible modification to trauma systems compared with trauma center placement.27 Geospatial analysis of trauma system resources can help systems optimize the distribution of HEMS bases and predict potential outcomes of resource allocation changes.28 Our results also indicate that the presence of trauma centers or HEMS bases directly within every rural county was not necessary to mitigate undertriage. Rather than necessarily adding new trauma centers or HEMS bases in counties without them, a robust assessment of HEMS base service areas with optimization of rural coverage is the goal.
This study has several important limitations to acknowledge. This is a retrospective study, and we were unable to evaluate the rationale of prehospital providers for triage decision making. Additionally, the triage criteria used may elicit some artifactual interpretation as they are established retrospectively based on International Classification of Diseases—9th Rev.—Clinical Modification coding of hospital diagnoses, and not necessarily diagnosed in the field by EMS. As a result, individual ORs may be difficult to interpret for these criteria; however, we believe that the value lies in the distinct injury patterns of undertriaged patients in urban and rural settings. There is a wide variation in the definition of urban and rural among studies evaluating this issue, making comparison difficult. We chose to use the definitions utilized by the Pennsylvania Trauma Systems Foundation which accredits trauma centers in the state and administers the Pennsylvania Trauma Outcomes Study.
CONCLUSION
This study confirms the ongoing outcome disparities among patients injured in rural settings. Undertriage is more common in rural settings and associated with increased mortality, offering insight into a possible mechanism for these disparities. Lack of a rural region trauma center requiring transfer to an urban trauma center is a risk factor for undertriage of rural patients. Air transport mitigated the risk of undertriage in rural patients. Poor trauma center access resulting in undertriage plays a role in rural disparities. Educational interventions and optimizing system resource organization may reduce undertriage and help close the gap between rural and urban communities in the United States.
ACKNOWLEDGMENTS
These data were provided by the Pennsylvania Trauma Systems Foundation, Mechanicsburg, PA. The Foundation specifically disclaims responsibility for any analyses, interpretations, or conclusions.
Footnotes
DISCLOSURE
The authors declare no funding or conflicts of interest.
This paper was presented as a Quick Shot presentation at the 33rd Annual Scientific Assembly of the Eastern Association for the Surgery of Trauma, January 14–18, 2020; Orlando, FL.
REFERENCES
- 1.MacKenzie EJ, Rivara FP, Jurkovich GJ, Nathens AB, Frey KP, Egleston BL, Salkever DS, Scharfstein DO. A national evaluation of the effect of traumacenter care on mortality. N Engl J Med. 2006;354(4):366–378. [DOI] [PubMed] [Google Scholar]
- 2.Mullins RJ, Veum-Stone J, Helfand M, Zimmer-Gembeck M, Hedges JR, Southard PA, Trunkey DD. Outcome of hospitalized injured patients after institution of a trauma system in an urban area. JAMA. 1994;271(24):1919–1924. [DOI] [PubMed] [Google Scholar]
- 3.Newgard CD, Fu R, Bulger E, et al. Evaluation of rural vs urban trauma patients served by 9-1-1 emergency medical services. JAMA Surg. 2017;152(1):11–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Clay Mann N, Mullins RJ, Hedges JR, Rowland D, Arthur M, Zechnich AD. Mortality among seriously injured patients treated in remote rural trauma centers before and after implementation of a statewide trauma system. Med Care. 2001;39(7):643–653. [DOI] [PubMed] [Google Scholar]
- 5.Gomez D, Berube M, Xiong W, Ahmed N, Haas B, Schuurman N, Nathens AB. Identifying targets for potential interventions to reduce rural trauma deaths: a population-based analysis. J Trauma. 2010;69(3):633–639. [DOI] [PubMed] [Google Scholar]
- 6.Grossman DC, Kim A, Macdonald SC, Klein P, Copass MK, Maier RV. Urban-rural differences in prehospital care of major trauma. J Trauma. 1997;42(4):723–729. [DOI] [PubMed] [Google Scholar]
- 7.Jarman MP, Castillo RC, Carlini AR, Kodadek LM, Haider AH. Rural risk: geographic disparities in trauma mortality. Surgery. 2016;160(6):1551–1559. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Jarman MP, Hashmi Z, Zerhouni Y, Udyavar R, Newgard C, Salim A, Haider AH. Quantifying geographic barriers to trauma care: urban-rural variation in prehospital mortality. J Trauma Acute Care Surg. 2019;87(1):173–180. [DOI] [PubMed] [Google Scholar]
- 9.Rogers FB, Shackford SR, Hoyt DB, Camp L, Osler TM, Mackersie RC, Davis JW. Trauma deaths in a mature urban vs rural trauma system. A comparison. Arch Surg. 1997;132(4):376–381; discussion 81-2. [DOI] [PubMed] [Google Scholar]
- 10.Sasser SM, Hunt RC, Faul M, et al. Guidelines for field triage of injured patients: recommendations of the National Expert Panel on Field Triage, 2011. MMWR Recomm Rep. 2012;61(RR-1):1–20. [PubMed] [Google Scholar]
- 11.Newgard CD, Fu R, Zive D, et al. Prospective validation of the National Field Triage Guidelines for identifying seriously injured persons. J Am Coll Surg. 2016;222(2):146–58.e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Byrne JP, Mann NC, Dai M, Mason SA, Karanicolas P, Rizoli S, Nathens AB. Association between emergency medical service response time and motor vehicle crash mortality in the United States. JAMA Surg. 2019;154(4):286–293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jones CM, Cushman JT, Lerner EB, Fisher SG, Seplaki CL, Veazie PJ, Wasserman EB, Dozier A, Shah MN. Prehospital trauma triage decisionmaking: a model of what happens between the 9-1-1 call and the hospital. Prehosp Emerg Care. 2016;20(1):6–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Nirula R, Maier R, Moore E, Sperry J, Gentilello L. Scoop and run to the trauma center or stay and play at the local hospital: hospital transfer's effect on mortality. J Trauma. 2010;69(3):595–599; discussion 9-601. [DOI] [PubMed] [Google Scholar]
- 15.Wild J, Younus JM, Malekpour M, et al. The effect of interhospital transfers on the outcome of rural trauma. Am Surg. 2017;83(1):39–44. [PubMed] [Google Scholar]
- 16.Haas B, Stukel TA, Gomez D, Zagorski B, De Mestral C, Sharma SV, Rubenfeld GD, Nathens AB. The mortality benefit of direct trauma center transport in a regional trauma system: a population-based analysis. J Trauma Acute Care Surg. 2012;72(6):1510–1515; discussion 5-7. [DOI] [PubMed] [Google Scholar]
- 17.Center for Rural Pennsylvania. Rural / Urban PA 2010. [Available from: https://www.rural.palegislature.us/rural_urban.html#maps.
- 18.Austin PC. Using the standardized difference to compare the prevalence of a binary variable between two groups in observational research. Commun Stat-Simul C. 2009;38(6):1228–1234. [Google Scholar]
- 19.Fleet R, Lauzier F, Tounkara FK, et al. Profile of trauma mortality and trauma care resources at rural emergency departments and urban trauma centres in Quebec: a population-based, retrospective cohort study. BMJ Open. 2019;9(6):e028512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Svenson J. Trauma systems and timing of patient transfer: are we improving? Am J Emerg Med. 2008;26(4):465–468. [DOI] [PubMed] [Google Scholar]
- 21.Haas B, Gomez D, Zagorski B, Stukel TA, Rubenfeld GD, Nathens AB. Survival of the fittest: the hidden cost of undertriage of major trauma. J Am Coll Surg. 2010;211(6):804–811. [DOI] [PubMed] [Google Scholar]
- 22.Lipsky AM, Gausche-Hill M, Henneman PL, Loffredo AJ, Eckhardt PB, Cryer HG, de Virgilio C, Klein SL, Bongard FS, Lewis RJ. Prehospital hypotension is a predictor of the need for an emergent, therapeutic operation in trauma patients with normal systolic blood pressure in the emergency department. J Trauma. 2006;61(5):1228–1233. [DOI] [PubMed] [Google Scholar]
- 23.Schenarts PJ, Phade SV, Agle SC, Goettler CE, Sagraves SG, Newell MA, Rotondo MF. Field hypotension in patients who arrive at the hospital normotensive: a marker of severe injury or crying wolf? N C Med J. 2008;69(4):265–269. [PubMed] [Google Scholar]
- 24.Smith RM, Conn AK. Prehospital care—scoop and run or stay and play? Injury. 2009;40(Suppl 4):S23–S26. [DOI] [PubMed] [Google Scholar]
- 25.Newgard CD, McConnell KJ, Hedges JR. Variability of trauma transfer practices among non-tertiary care hospital emergency departments. Acad Emerg Med. 2006;13(7):746–754. [DOI] [PubMed] [Google Scholar]
- 26.Branas CC, MacKenzie EJ, Williams JC, Schwab CW, Teter HM, Flanigan MC, Blatt AJ, ReVelle CS. Access to trauma centers in the United States. JAMA. 2005;293(21):2626–2633. [DOI] [PubMed] [Google Scholar]
- 27.Uribe-Leitz T, Esquivel MM, Knowlton LM, Ciesla D, Lin F, Hsia RY, Spain DA, Winchell RJ, Staudenmayer KL. The American College of Surgeons Needs-Based Assessment of Trauma Systems: estimates for the State of California. J Trauma Acute Care Surg. 2017;82(5):861–866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown JB, Rosengart MR, Billiar TR, Peitzman AB, Sperry JL. Distance matters: effect of geographic trauma system resource organization on fatal motor vehicle collisions. J Trauma Acute Care Surg. 2017;83(1):111–118. [DOI] [PMC free article] [PubMed] [Google Scholar]