Abstract
Background
Liver cirrhosis is a major burden on the health care system. Alcohol is one of the most common etiologies of cirrhosis. The aim of our article is to examine the trends of alcoholic liver cirrhosis (ALC) hospitalizations over the past two decades.
Methods
This was a retrospective longitudinal study. Using the International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System (ICD-9-CM/PCS) and the ICD-10-CM/PCS, the Nationwide Inpatient Sample (NIS) database was analyzed. We included 1998, 2003, 2008, 2013, and 2018 NIS databases. Using multivariate regression analysis, we examined trends of ALC hospitalizations including inpatient mortality, mean length of stay (LOS), and mean total hospital charges (THCs).
Results
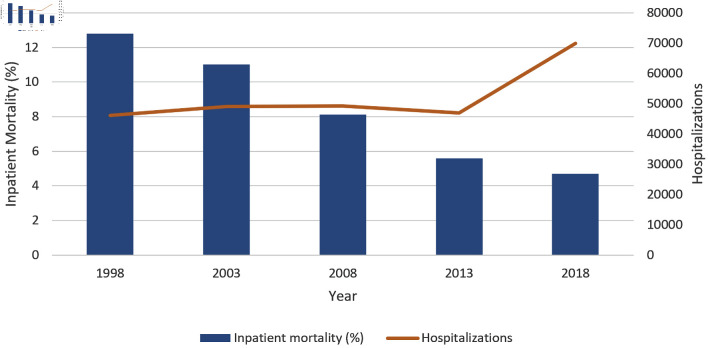
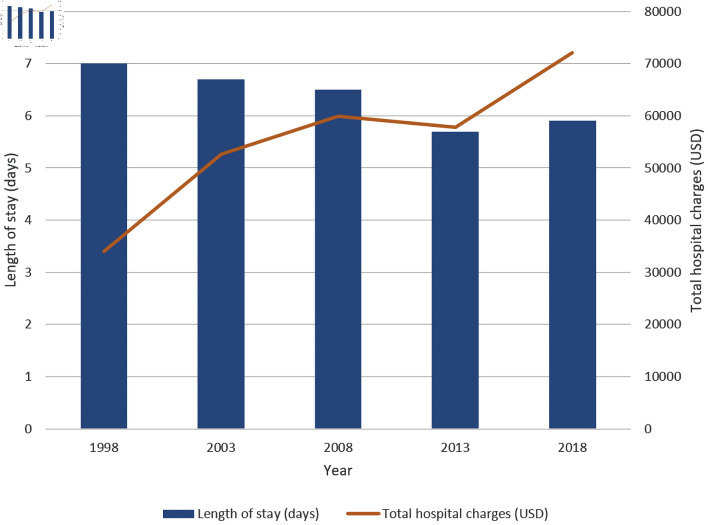
We included 261,420 hospitalizations with ALC as the primary diagnosis for admission. There was a trend toward increasing hospitalizations over that period; they increased from 46,186 in 1998 to 69,970 in 2018 (P < 0.001). Moreover, there was a 2.1-fold increase in the mean THC in 2018 compared to 1998 (P < 0.001). On the other hand, inpatient mortality decreased from 12.8% in 1998 to 4.7% in 2018 (P < 0.001), and a trend of decreasing mean LOS was observed. The mean LOS decreased from 7.0 days in 1998 to 5.9 days in 2018 (P < 0.001).
Conclusions
Over the last two decades, there was a trend of increasing hospitalizations and THC. However, we noticed a trend toward decreasing inpatient mortality and LOS over that period, which might reflect in part an improvement in the medical care provided for these patients.
Keywords: Alcoholic liver cirrhosis, Nationwide inpatient sample, Trends, Outcomes
Introduction
Alcohol use is influenced by numerous factors including religious beliefs, cultural norms, socioeconomic status, gender, ethnicity, and age [1]. Unfortunately, alcohol consumption has increased over the past 60 years [2]. In addition, there was a noticeable increase in high-risk drinking and alcohol use disorder in the last decade [3]. In the period 2006 - 2014, both acute and chronic alcohol-related emergency visits increased by 51.5% and 75.7%, respectively [4]. Alcohol is the third most common modifiable cause of death in the USA after tobacco and poor diet/physical inactivity [5]. Globally, it was responsible for nearly 3 million deaths in 1 year [1]. As expected, this resulted in tremendous hospital charges. The costs for all alcohol-related hospitalizations in 2014 in the USA were $3.4 billion [6].
There has been a dramatic increase in the number of newly diagnosed cirrhosis patients recently [7]. In addition to increased risk for hepatocellular carcinoma (HCC), cirrhosis is associated with multiple complications including variceal gastrointestinal bleeding, encephalopathy, ascites, peritonitis, and increased infections. Alcoholic liver cirrhosis (ALC) is a major health problem worldwide and it is responsible for a large portion of the healthcare burden caused by cirrhosis. Nearly half of all discharges related to cirrhosis are linked to the diagnosis of ALC [2]. In addition, cirrhosis-related mortality is the highest in patients with ALC; as it is responsible for nearly half the deaths in cirrhotic patients [2, 8, 9]. A recent study showed that in alcohol misusers, there was a 27-fold increase in mortality from ALC [10]. The proportion of alcohol-related liver disease is likely to increase in the future given the change in the patterns of alcohol consumption. In the regions of the Americas, per capita consumption of alcohol is expected to increase from 8.0 to 8.4 L before 2025 [1].
The burden of ALC is high and entirely preventable. It is crucial to understand the factors that are associated with worse outcomes. In this article, we studied ALC hospitalizations including demographics of patients, specific variables related to treating hospitals, and hospitalization outcomes. In addition, we examined trends of inpatient mortality, length of stay (LOS), and total hospital charges (THCs) over the last two decades.
Materials and Methods
Design and data source
This was a retrospective longitudinal trends study involving hospitalizations with ALC in the USA from 1998 to 2018. We sourced data from the Nationwide Inpatient Sample (NIS) for the studied years. The NIS is developed by the Healthcare Cost and Utilization Project (HCUP), a Federal-State-Industry partnership sponsored by the Agency for Healthcare Research and Quality (AHRQ). The NIS is a database of inpatient stays derived from billing data submitted by hospitals to statewide data organizations across the USA, covering more than 97% of the US population [11]. The provided dataset approximates a 20% stratified sample of discharges from US community hospitals, excluding rehabilitation and long-term acute care hospitals. This dataset is weighted to obtain US national estimates [12]. Databases before 2016 were coded using the International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System (ICD-9-CM/PCS). Databases from 2016 were coded using the ICD-10-CM/PCS. In the NIS, diagnoses are divided into two separate categories: principal diagnosis and secondary diagnoses. A principal diagnosis was the ICD code attributed to the reason for hospitalization. Secondary diagnoses were any ICD discharge codes other than the principal diagnosis.
Study population and variables
The study included NIS databases 1998, 2003, 2008, 2013, and 2018 selected by simple sampling. We searched the databases for hospitalizations with a principal discharge diagnosis of ALC using ICD codes (571.2 and K70.3). We excluded patients less than 18 years and elective hospitalizations. The NIS includes variables on patient demographics, including age, sex, race, median household income (income quartiles referred to patients as 1: low income, 2: middle income, 3: upper middle income, 4: high income), and primary payer. It also contains hospital-specific variables including bed size, teaching status, and location. We assessed the comorbidity burden using Sundararajan’s adaptation of the modified Deyo’s Charlson comorbidity index (CCI). This modification groups CCI into four groups in increasing risk for mortality. It has been adapted to population-based research. A score of > 3 has about a 25% 10-year mortality, while a score of 1 or 2 has a 4% and 10% 10-year mortality, respectively. This cutoff point was chosen as a mean of assessment of the increased risk of mortality [13].
Outcome measures
We highlighted the biodemographic trends over time for ALC hospitalizations. The number of all-hospitalizations per year was obtained from HCUP-US database to calculate the rate of ALC hospitalizations per 100,000 [14]. We analyzed trends of in-hospital mortality rate, mean LOS, and mean THC using multivariate logistic trend analysis. We also obtained mean THC using the HCUP cost-to-charge ratio files and adjusted for inflation using the Medical Expenditure Panel Survey index for hospital care, with 2018 as the reference point [15, 16].
Statistical analysis
Stata® Version 16 software (StataCorp, TX, USA) was used for data analysis. We analyzed and reported the weighted sample following HCUP regulations for using the NIS database. We used multivariate regression analysis to calculate the odds of trend in mortality, LOS, and THC following adjustment for age, sex, race, grouped CCI, insurance type, mean household income, and hospital characteristics. All P values were two-sided, with 0.05 set as the threshold for statistical significance.
Ethical considerations
The study was conducted in compliance with the ethical standards of the responsible institution on human subjects as well as with the Helsinki Declaration. The NIS database lacks patient and hospital level identifiers. This study, therefore, did not require Cook County Health Institutional Review Board approval or informed consents.
Results
Biodemographic analysis
The study analyzed 261,420 hospitalizations with ALC as the primary diagnosis for admission. There was a trend toward increasing hospitalizations over that period (Fig. 1 and Table 1); the annual volume increased from 46,186 hospitalizations in 1998 (136 per 100,000 hospitalizations) to 69,970 hospitalizations in 2018 (197 per 100,000 hospitalizations). This trend was statistically significant (P < 0.001). An increase in the mean age of patients was observed over that period; the mean age ranged between 52.8 and 54.4. This trend was also statistically significant (P < 0.001). The percentage of hospitalizations having a CCI score of 3 or more has increased over the study period and ranged between 68.7% and 78.5%. Male sex and White race were predominant across the study period. Patients were more likely to be hospitalized in urban teaching hospitals with large bed size.
Figure 1.
Trends of alcoholic liver cirrhosis hospitalizations (P trend < 0.001) and inpatient mortality (P trend < 0.001).
Table 1. Biodemographic Characteristics of Alcoholic Liver Cirrhosis Hospitalizations.
| Variables | 1998 | 2003 | 2008 | 2013 | 2018 |
|---|---|---|---|---|---|
| ALC hospitalizations | 46,186 | 49,144 | 49,254 | 46,864 | 69,970 |
| ALC hospitalizations per 100,000a | 136 | 133 | 129 | 132 | 197 |
| Mean age (years) ± SE | 53.3 ± 0.2 | 52.8 ± 0.2 | 53.3 ± 0.2 | 53.6 ± 0.1 | 54.4 ± 0.1 |
| Males (%) | 72.9 | 74.9 | 74.7 | 72.8 | 70.5 |
| Females (%) | 27.1 | 25.1 | 25.3 | 27.2 | 29.5 |
| Race (%) | |||||
| White | 55.0 | 49.5 | 56.8 | 63.7 | 64.1 |
| Black | 8.6 | 8.4 | 6.9 | 8.2 | 8.4 |
| Hispanic | 12.1 | 17.9 | 14.2 | 18.4 | 18.7 |
| Others | 24.3 | 24.2 | 22.2 | 9.7 | 8.8 |
| Charlson comorbidity index score | |||||
| 0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 |
| 1 | 23.1 | 22.1 | 18.8 | 15.3 | 15.4 |
| 2 | 7.8 | 9.2 | 7.1 | 6.2 | 6.9 |
| ≥ 3 | 69.1 | 68.7 | 74.1 | 78.5 | 77.7 |
| Median household income quartiles for patient’s zip code (%) | |||||
| 1 | 11.6 | 33.5 | 32.1 | 33.5 | 32.3 |
| 2 | 34.9 | 27.9 | 28.8 | 26.5 | 27.5 |
| 3 | 29.4 | 23.7 | 21.5 | 23.6 | 22.9 |
| 4 | 24.2 | 14.9 | 17.7 | 16.5 | 17.3 |
| Insurance (%) | |||||
| Medicare | 31.0 | 27.6 | 27.6 | 27.8 | 28.1 |
| Medicaid | 27.5 | 30.9 | 28.9 | 31.8 | 36.9 |
| Private | 29.2 | 27.8 | 29.0 | 23.0 | 24.0 |
| Self-pay | 12.3 | 13.8 | 14.5 | 17.5 | 10.9 |
| Bed size of the hospital (%) | |||||
| Small | 13.1 | 9.8 | 8.6 | 11.2 | 17.8 |
| Medium | 25.5 | 27.0 | 23.3 | 27.2 | 28.6 |
| Large | 61.4 | 63.3 | 68.1 | 61.6 | 53.6 |
| Location/Teaching status of the hospital (%) | |||||
| Rural | 11.2 | 11.9 | 8.1 | 7.2 | 4.9 |
| Urban non-teaching | 38.8 | 40.2 | 41.0 | 37.2 | 20.2 |
| Urban teaching | 50.0 | 47.9 | 50.9 | 55.6 | 74.9 |
| Region of the hospital (%) | |||||
| Northeast | 17.9 | 19.3 | 17.4 | 17.4 | 17.4 |
| Midwest | 19.7 | 16.5 | 18.4 | 18.4 | 20.0 |
| South | 38.2 | 39.4 | 41.4 | 40.8 | 40.0 |
| West | 24.4 | 24.8 | 22.8 | 23.4 | 22.6 |
aPer 100,000 hospitalizations; derived from HCUP-US database. SE: standard error.
Mortality analysis
Over the two decades, there was a statistically significant trend of decreasing inpatient mortality (Fig. 1 and Table 2); mortality decreased from 12.8% in 1998 to 4.7% in 2018 (P < 0.001). On multivariate analysis, variables that were associated with decreased inpatient mortality were Hispanic race (odds ratio (OR): 0.82, confidence interval (CI): 0.73 - 0.91; P < 0.001), median household income in the third quartile (OR: 0.88, CI: 0.80 - 0.97; P = 0.012), median household income in the fourth quartile (OR: 0.87, CI: 0.78 - 0.97; P = 0.014), and Midwest hospital region (OR: 0.80, CI: 0.71 - 0.91; P < 0.001). Contrastingly, variables that were associated with increased inpatient mortality were Black race (OR: 1.15, CI: 1.01 - 1.29; P = 0.024), age (OR: 1.01, CI: 1.01 - 1.02; P < 0.001), CCI score of 3 or more (OR: 2.16, CI: 1.93 - 2.41; P < 0.001), urban teaching hospitals (OR: 1.17, CI: 1.02 - 1.34; P = 0.022), large hospital bed size (OR: 1.12, CI: 1.00 - 1.26; P = 0.045), private insurance (OR: 1.29, CI: 1.17 - 1.43; P < 0.001), and lack of insurance (OR: 1.41, CI: 1.24 - 1.60; P < 0.001). There was no statistically significant difference in mortality between males and females (P = 0.411).
Table 2. Outcomes for Alcoholic Liver Cirrhosis Hospitalizations.
| 1998 | 2003 | 2008 | 2013 | 2018 | P value | |
|---|---|---|---|---|---|---|
| Inpatient mortality (%) | 12.8 | 11.0 | 8.1 | 5.6 | 4.7 | < 0.001 |
| LOS (days) | 7.0 | 6.7 | 6.5 | 5.7 | 5.9 | < 0.001 |
| THC ($) | 33,940 | 52,589 | 59,853 | 57,864 | 72,062 | < 0.001 |
LOS: length of stay; THC: total hospital charge.
LOS analysis
There was a trend of decreasing LOS over the study period (Fig. 2 and Table 2). The mean LOS decreased from 7.0 days in 1998 to 5.9 days in 2018. This trend was statistically significant (P < 0.001). On multivariate analysis, variables that were associated with decreased LOS were Hispanic race, hospital region other than Northeast, and lack of insurance. On the other hand, variables that were associated with increased LOS were age, female gender, median household income in the second or fourth quartile, CCI score of 3 or more, treatment in an urban hospital, and treatment in a hospital with medium or large bed size.
Figure 2.
Trends of length of stay (P trend < 0.001) and total hospital charges (P trend < 0.001).
THC analysis
The THC increased over the study period (Fig. 2 and Table 2); the mean THC reached the peak in 2018 at $72,062, representing a 2.1-fold increase from 1998. This trend was statistically significant (P < 0.001). On multivariate analysis, variables that were associated with decreased THC were age, Midwest hospital region, Medicaid insurance, and lack of insurance. On the other hand, median household income in the second or fourth quartile, CCI score of 3 or more, private insurance, treatment in an urban hospital, and treatment in a hospital with medium or large bed size were associated with increased THC. There was no statistically significant difference in THC between males and females (P = 0.172).
Discussion
Over the studied period, there was a noticeable increase in ALC hospitalizations. According to the global status report on alcohol and health [1], the European region and the region of the Americas have the highest per capita consumption of alcohol. Globally, alcohol consumers decreased from 47.6% to 43.0% in the period 2000 - 2016. However, given the increase in the world’s population, this did not translate into fewer active drinkers. In addition, the total alcohol consumption per capita has been increasing globally and nationally [1, 17]. Globally, the per capita consumption increased from 5.5 L in 2005 to 6.4 L in 2016 [1]. Moreover, between 2001 - 2002 and 2012 - 2013, high-risk alcohol drinking and alcohol use disorder increased by 29.9% and 49.4%, respectively [3]. Given the dose-dependent association between alcohol consumption and the risk of alcoholic cirrhosis [18, 19], the recent changes in the patterns of alcohol consumption might in part account for our observation. Given the fact that NIS reports information on hospitalizations rather than individual patients, we calculated the rates of ALC hospitalizations per 100,000 to provide another way to look at the trends and the burden of ALC.
Women are more vulnerable to the acute and chronic complications of alcohol including liver cirrhosis [20-22]. In addition, women die of alcoholic liver disease about 2 - 3 years earlier than men [23]. This might be in part the result of higher alcohol levels in women as they are known to have decreased gastric oxidation of ethanol [24]. Most of the hospitalizations in the studied years were for males. The higher male to female ratio in our analysis might stem from the fact that women are more likely to be lifetime abstainers or former drinkers than men. About 54.6% of the world’s female population are lifetime abstainers, compared to only 34.5% for men. In addition, when females drink alcohol, they drink less on average and engage less often in heavy episodic drinking [1]. Recently, this gender gap in alcohol use and alcohol-related harms has been closing. There was a significant decrease in the male to female ratio for alcohol use and related harms by the end of the 20th century [25]. Our analysis showed the female gender was associated with increased LOS; a finding consistent with the available evidence of worse outcomes in females as discussed above.
The observed increase in the mean age over the study period might be reflective of the recent changes in consumption patterns, manifested by an increase in alcohol consumption and binge drinking among middle-aged and elderly individuals. Breslow et al found that between 1997 and 2014, there was a 0.7% yearly increase in the prevalence of alcohol drinking in men over the age of 60 [26]. In addition, a meta-analysis that studied the trends of alcohol use and binge drinking in the USA showed a substantial increase in binge drinking in middle-aged and old adults [27]. As expected, our analysis showed that advanced age was associated with worse outcomes in terms of increased inpatient mortality and increased LOS. This is consistent with the available data which showed significantly worse outcomes in elderly patients. It has been found that the 1-year mortality from ALC in patients over the age of 60 was close to 50% [28, 29].
Studies reached conflicting results for the effect of ethnicity on outcomes in cirrhotic patients [9, 30-32]. Studies that investigated this effect in ALC patients also reached conflicting results [23, 33]. Yoon et al found that White patients had higher mortality than Black non-Hispanics and Hispanics [23]. Another study that utilized NIS database found higher mortality in African Americans compared to non-Hispanic Whites [33]. We found that Hispanic race was associated with lower inpatient mortality and shorter LOS. This variation in the available data is likely the result of the numerous factors that come into play. Different races and ethnicities have different genetic composition, biology, and a significant variation in the behavioral, social, environmental, and cultural dimensions. Genes influence the toxic effect of alcohol on the liver. Mexican and Black drinkers are more likely to have a two-fold elevation in AST when compared to White Americans [34]. Age of presentation for ALC is different among different ethnicities; Hispanics presented 4 to 10 years before Whites [35] and died younger compared to Whites and Blacks [23]. Furthermore, there are significant differences between ethnic subgroups. Among Hispanics, it has been found that Mexicans and Puerto Ricans had the highest alcohol consumption [36]. Death rates from cirrhosis, in general, were highest for Mexicans and Puerto Ricans and lowest for Cubans [9]. Moreover, drinking patterns and trends are different across ethnicities. According to the Centers for Disease Control and Prevention (CDC) National Health Interview Survey, Whites were more likely to have had five or more drinks in 1 day at least once a year compared to Hispanics and Black adults [37]. There was also variation in the trends of consumption; reduction in heavy drinking was observed among Whites but not among Blacks and Hispanics in the period 1984 - 1992 [38].
The percentage of patients having a CCI score of 3 or more has increased over the studied period. Possible explanations for this trend include the observed increase in mean age, as it has been shown that the number of comorbid diseases increases with age [39, 40]. In addition, alcohol consumption is associated with an increased risk for many diseases. Evidence suggests a causal effect for cardiovascular diseases (hypertensive heart disease, ischemic heart disease, conduction disorders, and stroke), infections (tuberculosis (TB) and pneumonia), diabetes, epilepsy, and numerous malignancies [19]. As expected, having a score of 3 or more was associated with worse outcomes in terms of higher inpatient mortality, higher THC, and longer LOS.
Studies have shown variable results for mortality trends in cirrhosis and ALC [9, 30, 41, 42]. Our analysis showed a remarkable decrease in ALC mortality. In addition, LOS decreased from 7.0 days in 1998 to 5.9 days in 2018. Consistent with our data, available evidence suggests a trend of decreasing LOS for ALC patients [6]. This improvement in outcomes might be the result of the refinement of inpatient cirrhosis care and the management of common complications like esophageal varices [43], ascites [44, 45], hepatorenal syndrome [46], bacterial peritonitis [47], and hepatic encephalopathy [48]. In addition, timely administration of antibiotics in cirrhotic patients with upper gastrointestinal bleeding was associated with a 30% reduction in 30-day mortality. The proportion of patients receiving timely antibiotics nearly doubled from 2005 to 2013 [49]. However, a recent study showed that the reduction in inpatient mortality for patients hospitalized with cirrhosis was associated with a less marked reduction in 1-year mortality. The authors of this study suggested that some of the mortality has shifted from inpatient to outpatient [50].
Hospital charges for ALC in the USA exceeded charges for all other cirrhosis etiologies combined [51]. Total aggregate charges for ALC in the USA increased from $1.4 billion in 2002 to $2.8 billion by 2014. This trend has been attributed to higher total volume and higher readmission rates of these patients rather than a change in charges per admission [51]. However, our study showed that the increase was also at the level of each hospitalization. Desai et al found that the increase in the THC was the result of increasing procedures such as mechanical ventilation and hemodialysis in addition to increasing portal and nonportal hypertensive complications [52].
Patients without insurance had higher inpatient mortality. Contrastingly, being in the higher income quartiles was associated with lower mortality. Consistent with our finding, a recent study showed that low socioeconomic status leads to a two-fold increase in alcohol-related mortality [53]. Desai et al studied the geographic variability in liver disease mortality and found that income is lower in states with higher liver disease mortality [32]. The disparity in access to healthcare is a major problem in the USA. Patients without insurance were less likely to have a standard site of care and less likely to visit a health professional [54]. Interestingly, income and educational level influence the patterns of alcohol consumption. It has been shown that the increase in alcohol use and high-risk drinking in the last two decades was most pronounced in individuals with lower educational levels and family income [3]. Yoon et al found that having a college degree raises the mean age of death from alcoholic liver disease [23]. Lack of insurance was associated with low THC and shorter LOS in our analysis. Further studies are needed to clarify if this observation is merely the result of higher inpatient mortality.
Hospitalizations in Midwest hospitals were associated with better outcomes in terms of inpatient mortality, LOS, and THC in our analysis. This is consistent with the available data for cirrhotic patients in general. It has been found that Southern states have the highest liver disease-related mortality rates, while Northeast and Midwest states have the lowest rates [32]. Mellinger et al found that cirrhotic patients hospitalized in Midwest hospitals had the lowest OR for inpatient mortality [55]. On multilevel modeling, 4% of mortality was attributable to the hospital level, demonstrating the significant hospital to hospital variation in cirrhosis outcomes.
Our study has some important limitations. The NIS reports information on hospitalizations rather than individual patients. The etiology of decompensation and the severity of ALC could not be determined from the NIS. In addition, we could not determine what proportion of patients were managed in the intensive care setting, which may impact outcomes. Therapeutic interventions and their impact on outcomes could not be determined. Finally, the study used ICD codes; therefore, the database may contain errors related to miscoding.
Our study showed a steady increase in the rates of ALC hospitalizations over the past two decades that resulted in a significant healthcare system utilization. It is projected that the rates will increase even further due to the changes in alcohol consumption seen over the past years. This will increase the burden on an already crippled healthcare system. There is an imminent need to address the causes of the increase in alcohol use given the detrimental outcomes. The regional variation in outcomes warrants further research on the practice of care in different areas of the country to implement the best practice across the board. Moreover, the disproportionate mortality rate in specific racial and socio-economic groups might reflect in part the disparity in healthcare access, which necessitates the implementation of policies to prevent that.
Acknowledgments
We would like to thank the Gastroenterology and Hepatology Department at John H. Stroger, Jr. Hospital of Cook County for the tremendous support and help in completing this project.
Financial Disclosure
None to declare.
Conflict of Interest
None to declare.
Informed Consent
The NIS database lacks patient and hospital level identifiers. This study, therefore, did not require Cook County Health Institutional Review Board approval or informed consents.
Author Contributions
Laswi and Shaka designed the study, performed data analysis, and reviewed the final manuscript. Abusalim contributed to the design and implementation of the study. Warraich and Khoshbin wrote the manuscript in consultation with Laswi.
Data Availability
The NIS is a large publicly available all-payer inpatient care database in the USA, containing data on more than 7 million hospital stays per year. Its large sample size is ideal for developing national and regional estimates and enables analyses of rare conditions, uncommon treatments, and special populations.
Abbreviations
- AHRQ
Agency for Healthcare Research and Quality
- ALC
alcoholic liver cirrhosis
- AST
aspartate aminotransferase
- CCI
Charlson comorbidity index
- CDC
Centers for Disease Control and Prevention
- CI
confidence interval
- HCC
hepatocellular carcinoma
- HCUP
Healthcare Cost and Utilization Project
- ICD
International Classification of Diseases
- ICD-10-CM/PCS
International Classification of Diseases, Tenth Revision, Clinical Modification/Procedure Coding System
- ICD-9-CM/PCS
International Classification of Diseases, Ninth Revision, Clinical Modification/Procedure Coding System
- LOS
length of stay
- NIS
Nationwide Inpatient Sample
- OR
odds ratio
- THC
total hospital charge
References
- 1.Dawson DA, Stinson FS, Chou SP, Grant BF. Three-year changes in adult risk drinking behavior in relation to the course of alcohol-use disorders. J Stud Alcohol Drugs. 2008;69(6):866–877. doi: 10.15288/jsad.2008.69.866. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Guirguis J, Chhatwal J, Dasarathy J, Rivas J, McMichael D, Nagy LE, McCullough AJ. et al. Clinical impact of alcohol-related cirrhosis in the next decade: estimates based on current epidemiological trends in the United States. Alcohol Clin Exp Res. 2015;39(11):2085–2094. doi: 10.1111/acer.12887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Grant BF, Chou SP, Saha TD, Pickering RP, Kerridge BT, Ruan WJ, Huang B. et al. Prevalence of 12-month alcohol use, high-risk drinking, and DSM-IV alcohol use disorder in the United States, 2001-2002 to 2012-2013: results from the national epidemiologic survey on alcohol and related conditions. JAMA Psychiatry. 2017;74(9):911–923. doi: 10.1001/jamapsychiatry.2017.2161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.White AM, Slater ME, Ng G, Hingson R, Breslow R. Trends in alcohol-related emergency department visits in the United States: results from the nationwide emergency department sample, 2006 to 2014. Alcohol Clin Exp Res. 2018;42(2):352–359. doi: 10.1111/acer.13559. [DOI] [PubMed] [Google Scholar]
- 5.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291(10):1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 6. Trends in alcohol-related morbidity among community hospital discharges, United States, 2000-2014. https://Pubs.Niaaa.Nih.Gov/Publications/Surveillance106/HDS14.Pdf.
- 7.Orman ES, Roberts A, Ghabril M, Nephew L, Desai AP, Patidar K, Chalasani N. Trends in characteristics, mortality, and other outcomes of patients with newly diagnosed cirrhosis. JAMA Netw Open. 2019;2(6):e196412. doi: 10.1001/jamanetworkopen.2019.6412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rehm J, Samokhvalov AV, Shield KD. Global burden of alcoholic liver diseases. J Hepatol. 2013;59(1):160–168. doi: 10.1016/j.jhep.2013.03.007. [DOI] [PubMed] [Google Scholar]
- 9. Liver cirrhosis mortality in the United States: National, State, and Regional Trends, 2000-2013. https://Pubs.Niaaa.Nih.Gov/Publications/Surveillance105/Cirr13.Pdf.
- 10.Kamper-Jorgensen M, Gronbaek M, Tolstrup J, Becker U. Alcohol and cirrhosis: dose—response or threshold effect? J Hepatol. 2004;41(1):25–30. doi: 10.1016/j.jhep.2004.03.002. [DOI] [PubMed] [Google Scholar]
- 11. Healthcare cost and utilization project. Introduction to the HCUP National Inpatient Sample (NIS). The National (Nationwide) inpatient sample database documentation. Rockville, MD: Agency for Healthcare Research and Quality. Available at: https://www.Hcup-Us.Ahrq.Gov/Db/Nation/Nis/NIS_Introduction_2018.Jsp. Accessed October 10, 2021. (unpublished)
- 12.Houchens R, Ross D, Elixhauser A, Jiang J. 2014 Nationwide inpatient sample (NIS) redesign final report. 2014. HCUP Methods Series Report # 2014-04 ONLINE. U.S. Agency for Healthcare Research and Quality. Available: http://www.Hcup-Us.Ahrq.Gov/Reports/Methods/Methods.Jsp. Accessed October 10, 2021. (unpublished)
- 13.Sundararajan V, Quan H, Halfon P, Fushimi K, Luthi JC, Burnand B, Ghali WA. et al. Cross-national comparative performance of three versions of the ICD-10 Charlson index. Med Care. 2007;45(12):1210–1215. doi: 10.1097/MLR.0b013e3181484347. [DOI] [PubMed] [Google Scholar]
- 14. https://www.Hcup-Us.Ahrq.Gov/Faststats/NationalTrendsServlet?Measure1=01&characteristic1=01&time1=20&measure2=&characteristic2=01&time2=10&expansionInfoState=hide&dataTablesState=hide&definitionsState=hide&exportState=hide. (unpublished)
- 15. HCUP Cost-to-Charge Ratio (CCR). 2008-2018. Agency for healthcare research and quality, Rockville, MD. https://www.Hcup-Us.Ahrq.Gov/Db/Ccr/Costtocharge.Jsp. Accessed February 10, 2021. (unpublished)
- 16.Dunn A, Grosse SD, Zuvekas SH. Adjusting health expenditures for inflation: a review of measures for health services research in the United States. Health Serv Res. 2018;53(1):175–196. doi: 10.1111/1475-6773.12612. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Apparent per capita alcohol consumption: National, State, and Regional Trends, 1977-2012. https://Pubs.Niaaa.Nih.Gov/Publications/Surveillance98/Cons12.Htm.
- 18.Askgaard G, Gronbaek M, Kjaer MS, Tjonneland A, Tolstrup JS. Alcohol drinking pattern and risk of alcoholic liver cirrhosis: a prospective cohort study. J Hepatol. 2015;62(5):1061–1067. doi: 10.1016/j.jhep.2014.12.005. [DOI] [PubMed] [Google Scholar]
- 19.Rehm J, Baliunas D, Borges GL, Graham K, Irving H, Kehoe T, Parry CD. et al. The relation between different dimensions of alcohol consumption and burden of disease: an overview. Addiction. 2010;105(5):817–843. doi: 10.1111/j.1360-0443.2010.02899.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Rehm J, Taylor B, Mohapatra S, Irving H, Baliunas D, Patra J, Roerecke M. Alcohol as a risk factor for liver cirrhosis: a systematic review and meta-analysis. Drug Alcohol Rev. 2010;29(4):437–445. doi: 10.1111/j.1465-3362.2009.00153.x. [DOI] [PubMed] [Google Scholar]
- 21.Ashley MJ, Olin JS, le Riche WH, Kornaczewski A, Schmidt W, Rankin JG. Morbidity in alcoholics. Evidence for accelerated development of physical disease in women. Arch Intern Med. 1977;137(7):883–887. doi: 10.1001/archinte.1977.03630190041012. [DOI] [PubMed] [Google Scholar]
- 22.Saunders JB, Davis M, Williams R. Do women develop alcoholic liver disease more readily than men? Br Med J (Clin Res Ed) 1981;282(6270):1140–1143. doi: 10.1136/bmj.282.6270.1140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Yoon YH, Chen CM, Slater ME, Jung MK, White AM. Trends in premature deaths from alcoholic liver disease in the U.S., 1999-2018. Am J Prev Med. 2020;59(4):469–480. doi: 10.1016/j.amepre.2020.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Frezza M, di Padova C, Pozzato G, Terpin M, Baraona E, Lieber CS. High blood alcohol levels in women. The role of decreased gastric alcohol dehydrogenase activity and first-pass metabolism. N Engl J Med. 1990;322(2):95–99. doi: 10.1056/NEJM199001113220205. [DOI] [PubMed] [Google Scholar]
- 25.Slade T, Chapman C, Swift W, Keyes K, Tonks Z, Teesson M. Birth cohort trends in the global epidemiology of alcohol use and alcohol-related harms in men and women: systematic review and metaregression. BMJ Open. 2016;6(10):e011827. doi: 10.1136/bmjopen-2016-011827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Breslow RA, Castle IP, Chen CM, Graubard BI. Trends in alcohol consumption among older Americans: National Health Interview Surveys, 1997 to 2014. Alcohol Clin Exp Res. 2017;41(5):976–986. doi: 10.1111/acer.13365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Grucza RA, Sher KJ, Kerr WC, Krauss MJ, Lui CK, McDowell YE, Hartz S. et al. Trends in Adult Alcohol Use and Binge Drinking in the Early 21st-Century United States: A Meta-Analysis of 6 National Survey Series. Alcohol Clin Exp Res. 2018;42(10):1939–1950. doi: 10.1111/acer.13859. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Potter JF, James OF. Clinical features and prognosis of alcoholic liver disease in respect of advancing age. Gerontology. 1987;33(6):380–387. doi: 10.1159/000212907. [DOI] [PubMed] [Google Scholar]
- 29.Woodhouse KW, James OF. Alcoholic liver disease in the elderly: presentation and outcome. Age Ageing. 1985;14(2):113–118. doi: 10.1093/ageing/14.2.113. [DOI] [PubMed] [Google Scholar]
- 30.Kim D, Li AA, Perumpail BJ, Gadiparthi C, Kim W, Cholankeril G, Glenn JS. et al. Changing trends in etiology-based and ethnicity-based annual mortality rates of cirrhosis and hepatocellular carcinoma in the United States. Hepatology. 2019;69(3):1064–1074. doi: 10.1002/hep.30161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Stinson FS, Grant BF, Dufour MC. The critical dimension of ethnicity in liver cirrhosis mortality statistics. Alcohol Clin Exp Res. 2001;25(8):1181–1187. doi: 10.1111/j.1530-0277.2001.tb02333.x. [DOI] [PubMed] [Google Scholar]
- 32.Desai AP, Mohan P, Roubal AM, Bettencourt R, Loomba R. Geographic Variability in Liver Disease-Related Mortality Rates in the United States. Am J Med. 2018;131(7):728–734. doi: 10.1016/j.amjmed.2018.01.047. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Shirazi F, Singal AK, Wong RJ. Alcohol-associated cirrhosis and alcoholic hepatitis hospitalization trends in the United States. J Clin Gastroenterol. 2021;55(2):174–179. doi: 10.1097/MCG.0000000000001378. [DOI] [PubMed] [Google Scholar]
- 34.Stewart SH. Racial and ethnic differences in alcohol-associated aspartate aminotransferase and gamma-glutamyltransferase elevation. Arch Intern Med. 2002;162(19):2236–2239. doi: 10.1001/archinte.162.19.2236. [DOI] [PubMed] [Google Scholar]
- 35.Levy R, Catana AM, Durbin-Johnson B, Halsted CH, Medici V. Ethnic differences in presentation and severity of alcoholic liver disease. Alcohol Clin Exp Res. 2015;39(3):566–574. doi: 10.1111/acer.12660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Lee DJ, Markides KS, Ray LA. Epidemiology of self-reported past heavy drinking in Hispanic adults. Ethn Health. 1997;2(1-2):77–88. doi: 10.1080/13557858.1997.9961817. [DOI] [PubMed] [Google Scholar]
- 37. CDC/NCHS National Health Interview Survey, 1997-2009, Sample Adult Core Component. Available at: http://www.cdc.gov/nchs/data/nhis/earlyrelease/201006_09.pdf.
- 38.Caetano R, Kaskutas LA. Changes in drinking patterns among whites, blacks and Hispanics, 1984-1992. J Stud Alcohol. 1995;56(5):558–565. doi: 10.15288/jsa.1995.56.558. [DOI] [PubMed] [Google Scholar]
- 39.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40(5):373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 40.van den Akker M, Buntinx F, Metsemakers JF, Roos S, Knottnerus JA. Multimorbidity in general practice: prevalence, incidence, and determinants of co-occurring chronic and recurrent diseases. J Clin Epidemiol. 1998;51(5):367–375. doi: 10.1016/S0895-4356(97)00306-5. [DOI] [PubMed] [Google Scholar]
- 41.Schmidt ML, Barritt AS, Orman ES, Hayashi PH. Decreasing mortality among patients hospitalized with cirrhosis in the United States from 2002 through 2010. Gastroenterology. 2015;148(5):967–977.e962. doi: 10.1053/j.gastro.2015.01.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Tapper EB, Parikh ND. Mortality due to cirrhosis and liver cancer in the United States, 1999-2016: observational study. BMJ. 2018;362:k2817. doi: 10.1136/bmj.k2817. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Garcia-Tsao G, Sanyal AJ, Grace ND, Carey W, Practice Guidelines Committee of the American Association for the Study of Liver D, Practice Parameters Committee of the American College of G. Prevention and management of gastroesophageal varices and variceal hemorrhage in cirrhosis. Hepatology. 2007;46(3):922–938. doi: 10.1002/hep.21907. [DOI] [PubMed] [Google Scholar]
- 44.Runyon BA, Committee APG. Management of adult patients with ascites due to cirrhosis: an update. Hepatology. 2009;49(6):2087–2107. doi: 10.1002/hep.22853. [DOI] [PubMed] [Google Scholar]
- 45.Bernard B, Grange JD, Khac EN, Amiot X, Opolon P, Poynard T. Antibiotic prophylaxis for the prevention of bacterial infections in cirrhotic patients with gastrointestinal bleeding: a meta-analysis. Hepatology. 1999;29(6):1655–1661. doi: 10.1002/hep.510290608. [DOI] [PubMed] [Google Scholar]
- 46.Gines P. Pharmacological management of hepatorenal syndrome: lessons from non-responders. J Hepatol. 2011;55(2):268–269. doi: 10.1016/j.jhep.2011.02.006. [DOI] [PubMed] [Google Scholar]
- 47.Sort P, Navasa M, Arroyo V, Aldeguer X, Planas R, Ruiz-del-Arbol L, Castells L. et al. Effect of intravenous albumin on renal impairment and mortality in patients with cirrhosis and spontaneous bacterial peritonitis. N Engl J Med. 1999;341(6):403–409. doi: 10.1056/NEJM199908053410603. [DOI] [PubMed] [Google Scholar]
- 48.Bass NM, Mullen KD, Sanyal A, Poordad F, Neff G, Leevy CB, Sigal S. et al. Rifaximin treatment in hepatic encephalopathy. N Engl J Med. 2010;362(12):1071–1081. doi: 10.1056/NEJMoa0907893. [DOI] [PubMed] [Google Scholar]
- 49.Moon AM, Dominitz JA, Ioannou GN, Lowy E, Beste LA. Use of antibiotics among patients with cirrhosis and upper gastrointestinal bleeding is associated with reduced mortality. Clin Gastroenterol Hepatol. 2016;14(11):1629–1637.e1621. doi: 10.1016/j.cgh.2016.05.040. [DOI] [PubMed] [Google Scholar]
- 50.Kanwal F, Tansel A, Kramer JR, Feng H, Asch SM, El-Serag HB. Trends in 30-day and 1-year mortality among patients hospitalized with cirrhosis from 2004 to 2013. Am J Gastroenterol. 2017;112(8):1287–1297. doi: 10.1038/ajg.2017.175. [DOI] [PubMed] [Google Scholar]
- 51.Barritt ASt, Jiang Y, Schmidt M, Hayashi PH, Bataller R. Charges for Alcoholic Cirrhosis Exceed All Other Etiologies of Cirrhosis Combined: A National and State Inpatient Survey Analysis. Dig Dis Sci. 2019;64(6):1460–1469. doi: 10.1007/s10620-019-5471-7. [DOI] [PubMed] [Google Scholar]
- 52.Desai AP, Mohan P, Nokes B, Sheth D, Knapp S, Boustani M, Chalasani N. et al. Increasing economic burden in hospitalized patients with cirrhosis: analysis of a national database. Clin Transl Gastroenterol. 2019;10(7):e00062. doi: 10.14309/ctg.0000000000000062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Probst C, Roerecke M, Behrendt S, Rehm J. Socioeconomic differences in alcohol-attributable mortality compared with all-cause mortality: a systematic review and meta-analysis. Int J Epidemiol. 2014;43(4):1314–1327. doi: 10.1093/ije/dyu043. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wilper AP, Woolhandler S, Lasser KE, McCormick D, Bor DH, Himmelstein DU. A national study of chronic disease prevalence and access to care in uninsured U.S. adults. Ann Intern Med. 2008;149(3):170–176. doi: 10.7326/0003-4819-149-3-200808050-00006. [DOI] [PubMed] [Google Scholar]
- 55.Mellinger JL, Richardson CR, Mathur AK, Volk ML. Variation among United States hospitals in inpatient mortality for cirrhosis. Clin Gastroenterol Hepatol. 2015;13(3):577–584. doi: 10.1016/j.cgh.2014.09.038. quiz e530. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The NIS is a large publicly available all-payer inpatient care database in the USA, containing data on more than 7 million hospital stays per year. Its large sample size is ideal for developing national and regional estimates and enables analyses of rare conditions, uncommon treatments, and special populations.