Abstract
Although stomal and parastomal varices are uncommon causes of variceal bleeding, the mortality rate might be as high as 40%. Timely intervention is essential for the management of these ectopic bleeding varices. Due to the rarity of such varices, no standard treatment guideline is available. We present three cases of bleeding stomal varices managed with an endovascular approach, one through percutaneous transhepatic and the other two through transjugular intrahepatic portosystemic shunt approach.
Keywords: stomal varices, transjugular intrahepatic portosystemic shunt (TIPS), glue
Abbreviations: APR, Abdominoperineal resection; BRTO, Balloon-occluded retrograde transvenous obliteration of stomal varices; CECT, Contrast-enhanced computed tomography; CTP score, Child-Turcotte-Pugh score; GI, Gastrointestinal; IMV, Inferior mesenteric vein; MELD, Model for end-stage liver disease; Na, Sodium; NASH, Nonalcoholic steatohepatitis; SMV, Superior mesenteric vein; SVB, Stomal variceal bleeding; TIPS, Transjugular intrahepatic portosystemic shunt; UGIE, Upper gastrointestinal endoscopy; USG, Ultrasonography
Bleeding in portal hypertensive patients is caused primarily by the rupture of gastroesophageal varices. Varices that form in an ectopic location are uncommon, accounting for only 2–5% of gastrointestinal variceal bleeding.1 Stomal and parastomal varices are ectopic varices seen in patients with prior ostomies and portal hypertension. In portal hypertension, the portal flow reverses and decompresses into low-pressure veins of the abdominal wall via the mucocutaneous venous network. This causes vein engorgement around the existing stoma, resulting in variceal formation.2 According to Saad et al., most of the stomal varices are either type 1a (nonocclusive type with porto-portal collaterals) or type 2a (nonocclusive type with porto-portal collaterals and a few portosystemic collaterals).3 These ectopic varices can cause severe bleeding due to variceal rupture, necessitating immediate medical attention.3 We present three cases of stomal variceal bleeding (SVB) successfully treated with endovascular intervention.
Case 1
A 55-year-old man with portal hypertension secondary to nonalcoholic steatohepatitis (NASH) related cirrhosis came with recurrent colostomy site bleeding (3 times; 200–300ml/episode). Five years ago, he had an abdominoperineal resection (APR) with an end colostomy for carcinoma rectum.
The patient was hemodynamically stable at the time of presentation. Except for low hemoglobin of 8.4 gm/dl, platelet count of 55000/mm3, and serum albumin of 2.9 gm/dl, laboratory results were normal. The Child-Pugh score (CTP) was 6, and the Model for End-Stage Liver Disease sodium (MELD-Na) score was 13. Upper gastrointestinal endoscopy (UGIE) revealed small low-risk esophageal varices. Ultrasonography (USG) showed multiple dilated and tortuous venous channels at stomal and parastomal locations. Because of recurrent stomal variceal bleeding, a transjugular intrahepatic portosystemic shunt (TIPS) creation was planned. Venography revealed an engorged inferior mesenteric vein (IMV) supplying the dilated tortuous stomal varices (Figure 1a, 1b). Micro coils and a glue-lipiodol mixture (0.1 ml; 25%) were used to embolize the feeding vein from IMV (Figure 1c). A 10 mm stent graft was used to create the TIPS (Figure 1d). After TIPS, the patient had no further episodes of stomal variceal bleed.
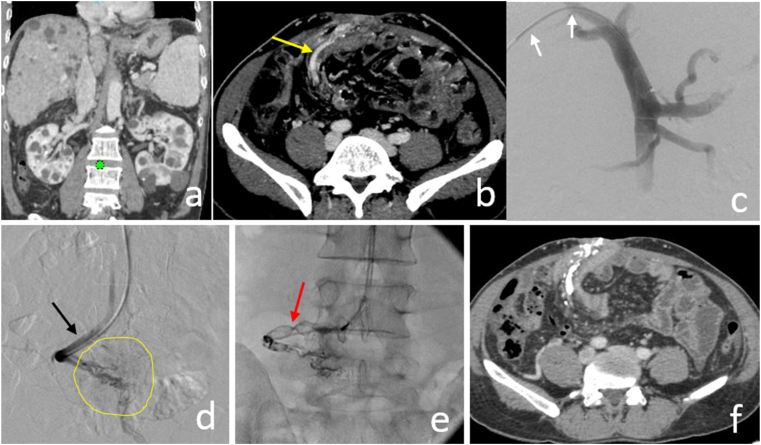
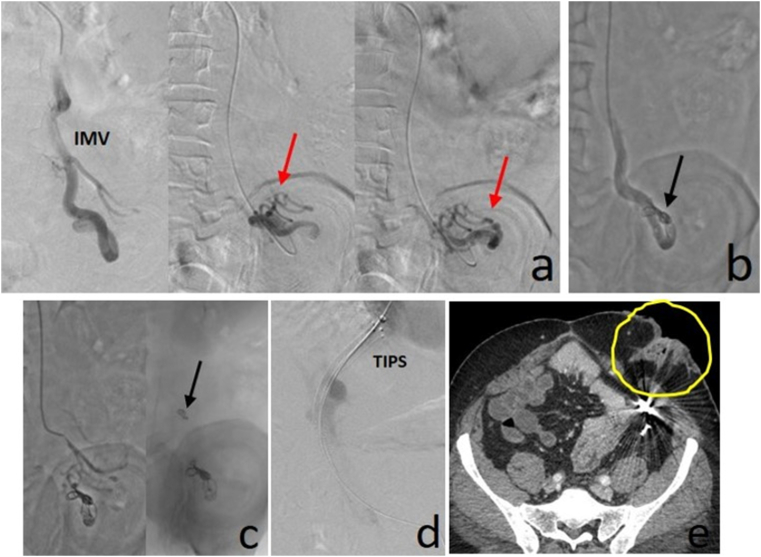
Figure 1.
Recurrent variceal bleeding from the sigmoid colostomy site in a patient with liver cirrhosis. Venographic images (a) and (b) shows a dilated inferior mesenteric vein (IMV) leading to the tortuous stomal varices (red arrows a, b). Image (c) shows embolization of inflow vein from distal IMV using microcoils and glue (black arrow c), followed by TIPS creation (d).
Case 2
A 45-year-old woman presented with intermittent bleeding from her ileostomy site twice in the previous six months. Ileostomy was performed for bowel perforation 15 years back. She had ethanol-related cirrhosis and had one episode of upper GI variceal bleed five years back. In addition, the patient had polycystic liver and kidney disease.
The patient was hemodynamically stable at the time of presentation. Local examination showed a purple hue on and around the stomal site with few prominent superficial veins. She had low hemoglobin of 8.9 gm/dl and elevated total bilirubin of 1.4 mg/dl. The rest of the laboratory parameters were normal. The CTP and MELD-Na scores were 7 and 12, respectively.
Contrast-enhanced computed tomography (CECT) of the abdomen showed liver changes consistent with cirrhosis and multiple varying-sized cysts in the liver and kidneys (Figure 2a). Multiple engorged venous channels were noted in and around the stoma with a dilated venous afferent from the distal superior mesenteric vein (SMV) (Figure 2b).
Figure 2.
Stomal varices at ileostomy site in a patient with cirrhosis and portal hypertension. Coronal portal venous CT image (a) shows multiple cysts in the liver and kidneys. Axial CT image (b) shows a dilated branch of distal SMV (yellow arrow b) feeding the stomal varices. Image c and d showing a 6F 45 cm long vascular sheath advanced into the distal-most SMV (black arrow d). Venography showing variceal opacification (yellow circle d). A 14 mm vascular plug was deployed at the origin of the feeding vein (red arrow e), followed by distal glue embolization. Follow up CECT image (f) showing complete obliteration of feeder and varices by glue.
TIPS was ruled out due to polycystic liver disease. Local sclerotherapy was not done due to clumped bowel loops at the stoma site. Therefore, percutaneous transhepatic variceal embolization was planned. After portal vein access, a 6F 45 cm long vascular access sheath was placed into the distal SMV (Figure 2c, 2d). A dilated branch of SMV was supplying the varices (Figure 2d). This feeding vein was occluded with a 14 mm vascular plug (AVP II, Abbott cardiovascular, IL), and the varices distal to the plug were embolized with a 25% glue-lipiodol mixture (Figure 2e). The postembolization venogram revealed completely obliterated varices (Figure 2f). No recurrence has been reported further.
Case 3
A 44-year-old patient with cryptogenic cirrhosis and portal hypertension experienced colostomy site bleeding, resulting in a blood loss of about 1200 ml. Colostomy was done for carcinoma rectum. The patient had an esophageal variceal bleed 3 years ago, which was managed by endoscopic variceal ligation.
On presentation, the patient was hypotensive (76/62 mm Hg). Initially, he was managed with intravenous fluids and blood products. Local compression was used to control the bleeding temporarily. The patient was of Child-Pugh class B (CTP score 9) and had a MELD-Na score of 15. Complete blood count (CBC) and liver function test were unremarkable except for low hemoglobin of 7.2 gm/dl and serum albumin of 2.7 gm/dl. Bedside USG showed cirrhotic liver with patent spleno-portal axis and moderate ascites.
Venography during TIPS revealed two distal branches of IMV feeding the stomal varices (Figure 3a). Both the feeders were embolized using coils (Figure 3b, 3c), and then an 8 mm stent was used to complete the TIPS procedure (Figure 3d). Three days after the procedure, the patient developed hepatic encephalopathy managed with lactulose and rifaximin. There was no recurrent bleed from the stomal site. He died after 9 months of TIPS due to progressive liver failure.
Figure 3.
Acute variceal bleeding from colonic stoma site in a patient with portal hypertension. Venography (a) showing tortuous varices (red arrow a) supplied by dilated and tortuous IMV. Initially, the more prominent supplying vein was embolized with coils (b). Subsequent DSA run showed residual supply through a small vein embolized with a coil (black arrow c). TIPS was created (d). Follow up CECT image (e) showing complete obliteration of varices (yellow circle). Note metallic streak artifacts from coils in image e.
Discussion
Although stomal varices rarely cause bleeding, mortality might be as high as 40%.3 The rate of rebleeding is also high.3 Treatment options range from local measures to surgery. Local conservative methods include applying pressure to the area and suturing or cauterizing the varices.4 Most of the time, these methods efficiently control stomal variceal bleeding immediately, but recurrence is common.4 Stomal revisions have also been shown to be beneficial, but with a definite risk of surgery.5 However, none of these methods addresses the underlying cause of the varices that is portal hypertension.
TIPS lowers the increased portal pressure, allowing the stomal varices to decompress. It is the most widely used intervention in SVB.5 Despite lowering the portosystemic gradient to <12 mm Hg, studies have reported varying recurrence rates after TIPS ranging from 20 to 40%.5,6 In addition to TIPS, variceal embolization further reduces the recurrence rate. A study by Vangeli et al. demonstrated that the combined TIPS plus embolization group had a lower recurrence rate (28%) than the TIPS alone group (42%).7 Embolization with glue (N-butyl cyanoacrylate) achieves a better variceal obliteration than coil embolization. Glue more effectively obliterates the tiny and distal venous channels, in contrast to more proximal embolization by coils.5,7,8 Proper patient selection is critical before TIPS since TIPS worsens the existing liver function and may result in hepatic decompensation. Every patient of SVB may not be a candidate for TIPS due to baseline liver function or other associated comorbidities.6,9
When TIPS is not an option, a percutaneous transhepatic approach may be considered.9 However, intra-abdominal bleeding and hepatic injury are possible complications.
Under USG guidance, direct percutaneous embolization of stomal varices with glue, coil, or a combination of both has also been described with good results.10 When a single dominant varix is discovered on USG, this approach works well. The embolization segment should extend from the origin of the major varix to as distally as possible. Placing a coil at the proximal end helps avoid inadvertent glue embolization.10 Even though this method provides adequate embolization, there is a risk of recurrence because it does not address the primary cause of varix, i.e., portal hypertension.5
Local sclerotherapy has also been used to treat SVB with mixed outcomes; however, sclerosant can induce stomal damage.4,8 Balloon occluded retrograde transvenous obliteration of stomal varices (BRTO) and retrograde venous access through the left superficial epigastric vein have also been employed.11
Because of the increased morbidity and mortality, surgical portosystemic shunts are rarely recommended. The most effective treatment is liver transplantation. However, many of these patients have comorbidities that may prohibit liver transplantation and the construction of surgical shunts.4,8
TIPS in combination with variceal embolization is a successful treatment option for SVB. Owing to various contraindications to TIPS, some patients may require an alternative treatment technique. In this situation, percutaneous transhepatic plug-assisted glue embolization is a viable alternative.
Informed consent
Informed consent was obtained from the patient in the first two cases and the patient’s family in the last case for publication of this case series and accompanying images.
Credit authorship contribution statement
Ranjan K. Patel: Writing – original draft. Karamvir Chandel: Literature review. Taraprasad Tripathy: Literature review. Ashok Choudhury: Writing – review and editing. Amar Mukund: Writing – review and editing
Conflicts of interest
The authors have none to declare.
Acknowledgement
None.
Funding
None.
References
- 1.Kochar N., Tripathi D., McAvoy N.C., Ireland H., Redhead D.N., Hayes P.C. Bleeding ectopic varices in cirrhosis: the role of transjugular intrahepatic portosystemic stent shunts. Aliment Pharmacol Ther. 2008;28:294–303. doi: 10.1111/j.1365-2036.2008.03719.x. [DOI] [PubMed] [Google Scholar]
- 2.Yao D.H., Luo X.F., Zhou B., Li X. Ileal conduit stomal variceal bleeding managed by endovascular embolization. World J Gastroenterol. 2013;19:8156–8159. doi: 10.3748/wjg.v19.i44.8156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Saad W.E., Lippert A., Saad N.E., Caldwell S. Ectopic varices: anatomical classification, hemodynamic classification, and hemodynamic-based management. Tech Vasc Interv Radiol. 2013;16:158–175. doi: 10.1053/j.tvir.2013.02.004. [DOI] [PubMed] [Google Scholar]
- 4.Spier B.J., Fayyad A.A., Lucey M.R., et al. Bleeding stomal varices: case series and systematic review of the literature. Clin Gastroenterol Hepatol. 2008;6:346–352. doi: 10.1016/j.cgh.2007.12.047. the official clinical practice journal of the American Gastroenterological Association. [DOI] [PubMed] [Google Scholar]
- 5.de Hoog J., Yong T.L., Yellapu S. Novel surgical control of bleeding para-stomal varices. ANZ J Surg. 2010;80:469–470. doi: 10.1111/j.1445-2197.2010.05323.x. [DOI] [PubMed] [Google Scholar]
- 6.Deipolyi A.R., Kalva S.P., Oklu R., Walker T.G., Wicky S., Ganguli S. Reduction in portal venous pressure by transjugular intrahepatic portosystemic shunt for treatment of hemorrhagic stomal varices. AJR Am J Roentgenol. 2014;203:668–673. doi: 10.2214/AJR.13.12211. [DOI] [PubMed] [Google Scholar]
- 7.Vangeli M., Patch D., Terreni N., et al. Bleeding ectopic varices--treatment with transjugular intrahepatic porto-systemic shunt (TIPS) and embolisation. J Hepatol. 2004;41:560–566. doi: 10.1016/j.jhep.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 8.Romano J., Welden C.V., Orr J., McGuire B., Shoreibah M. Case series regarding parastomal variceal bleeding: presentation and management. Ann Hepatol. 2019;18:250–257. doi: 10.5604/01.3001.0012.7934. [DOI] [PubMed] [Google Scholar]
- 9.Sniderman K., Simons M., Rajan D., Jaskolka J., Wong F., Boudreau H.S. Management of bleeding stomal varices. J Vasc Interv Radiol. 2014;25:S135–S136. doi: 10.1016/j.jvir.2013.12.365. [DOI] [Google Scholar]
- 10.Thouveny F., Aubé C., Konaté A., Lebigot J., Bouvier A., Oberti F. Direct percutaneous approach for endoluminal glue embolization of stomal varices. J Vasc Interv Radiol. 2008;19:774–777. doi: 10.1016/j.jvir.2008.01.018. [DOI] [PubMed] [Google Scholar]
- 11.Minami S., Okada K., Matsuo M., Kamohara Y., Sakamoto I., Kanematsu T. Treatment of bleeding stomal varices by balloon-occluded retrograde transvenous obliteration. J Gastroenterol. 2007;42:91–95. doi: 10.1007/s00535-006-1960-5. [DOI] [PubMed] [Google Scholar]