Abstract
Ramadan fasting is one of the five pillars of Islam. The current study aims to examine, analyze, and identify trends of health-related publications on Ramadan fasting. In total, 1468 documents retrieved from Scopus were analyzed. The mean number of authors per document was 3.7, with an average of 13.3 citations per document. The UK ranked first (12.3%, n = 181) regarding the number of documents, followed by Iran (10.4%, n = 153) and then Saudi Arabia (9.8%, n = 144). The most active journal was “Diabetes Research and Clinical Practice” (4.9%, n = 72). Publications related to diabetes and fasting constituted around 29.7% (n = 436) of the literature. The research volume on Ramadan fasting has been noticeably growing. More reliable research is required to aid healthcare professionals in providing patient-specific care.
Keywords: Bibliometric analysis, Fasting, Islamic fasting, Ramadan
Introduction
Ramadan fasting is a form of intermittent fasting globally practiced by Muslims during the holy month of Ramadan. Fasting takes place from sunrise to sunset and consists of abstinence from foods, drinks, and sexual intercourse. The period of fasting varies between geographical areas and time of the year, with fasting hours reaching their peak in summer. According to the Islamic creed, Muslims are exempted from fasting in situations where health might be compromised by the lack of feedings, such as illness, travel, old age, and certain cases of pregnancy (Rouhani & Azadbakht, 2014).
A common practice in Ramadan is to have a meal called "Suhoor" that takes place before dawn, to provide the body with energy throughout the day. This practice alters the sleeping patterns of the practitioners, which ensues changes in circadian rhythm and physiological processes (BaHammam et al., 2010; Roky et al., 2001). Effects on insulin circulating levels, cortisol circadian secretion, and sleep cycles have been detected (Bahijri et al., 2013; Haouari et al., 2008).
The effect of Ramadan fasting on various disease states has also been studied. Interestingly, fasting has been found to cause no negative effects on chronic kidney disease (CKD) patients, or those with a transplanted kidney, while its safety has not been confirmed for nephrolithiasis patients (Bragazzi, 2014). A study on patients with stable chronic obstructive pulmonary disease (COPD) found no effects of Ramadan fasting on the spirometric data of patients enrolled (Zouari et al., 2018).
An improvement in the lipid profiles and blood glucose levels has been reported among athletes who practiced fasting during the month of Ramadan. Weight reduction has also been linked to Ramadan fasting, although only among men, and weight was regained shortly after the month (Rouhani & Azadbakht, 2014).
One study reported an increase in the number of gastric ulcer cases during the month of Ramadan compared to the preceding month, although with no effect on disease outcomes (El Mekkaoui et al., 2013). Moreover, it was concluded that fasting may have notorious impacts on patients with various gastrointestinal (GI) diseases and may increase the risk of complications (Sadeghpour et al., 2012). Effects on psoriasis, infectious diseases, cancer, pregnancy, and immune system have also been examined (Awwad et al., 2012; Bragazzi et al., 2015; Damiani et al., 2019; Develioglu et al., 2013; Faris et al., 2012; Van Ewijk et al., 2013).
The impact of Ramadan fasting on diabetes management and glycemic control has been extensively studied. Eating patterns during the month may result in alternating episodes of hyperglycemia and hypoglycemia. Although fasting and postprandial blood sugar were found to be decreased during Ramadan, the risk of hyperglycemia is still present due to overeating during feasting hours. A reschedule of insulin regimens is also warranted for type 1 and insulin-dependent type 2 diabetes mellitus (DM) patients to prevent hypoglycemia (Hassanein et al., 2017; Rouhani & Azadbakht, 2014).
Hundreds of millions of Muslims around the world practice intermittent fasting during Ramadan, yet literature assessing the impact of fasting on health and body physiology remains scarce. This is especially a matter of concern to healthcare professionals who get consulted during the month of Ramadan. In such cases, guidelines are warranted to provide patient-specific care. To this date, no bibliometric analysis has been conducted to appraise the entire literature on Ramadan fasting. An analysis was recently conducted by Husain et al. covering the top 100 cited documents on Ramadan fasting (Husain et al., 2020). However, this approach warrants the inclusion of older articles over recent ones, as the latter has had less time to gain citations. Moreover, documents written in languages other than English were not included. Another bibliometric study was conducted on Ramadan fasting and diabetes and found a total of 424 documents, with the domination of authors and institutions based in the UK (Beshyah & Beshyah, 2019). This study aims to assess and analyze research trends of all Ramadan-related literature published in the past two decades. Moreover, research growth, the geographical distribution of outputs, authorship trends, and citation analysis were examined.
Methods
Bibliographic Database
This cross-sectional study was conducted in February 2022 using a bibliometric methodology. Scopus database was used to retrieve study data considering its previous use in several bibliometric studies and 100% inclusion of PubMed, in addition to the several search and analysis functions it offers. Scopus was used because it is the largest online database with abstracts and citations of over 23,700 peer-reviewed journals (Falagas et al., 2008). Only documents published in peer-reviewed journals were included.
Research Strategy and Keywords
The study period was set from 1999 to 2021. The following search keywords were used in title/abstract search. The keywords included ("Ramadan AND fast*"), ("Islam* AND fasting"), ("Ramdan"), and (" Islam* AND diet AND restriction"). Documents were set to be retrieved if the previous keywords appeared in their title or abstract. To ensure accuracy and maximal retrieval of relevant documents, asterisks and quotation marks were used. Literature was also surveyed to obtain commonly used author keywords on Ramadan fasting. To refine the retrieved documents to health areas, results were filtered to be within the following subject areas: medicine, nursing, biochemistry, genetics, molecular biology, neuroscience, dentistry, pharmacology, immunology, microbiology, and psychology. Hirsh index (h-index) was used to assess the quality of retrieved documents (Mikhailov, 2014).
Data Analysis
Retrieved data were analyzed for annual growth, authorship pattern and collaboration, citation analysis, country and institution productivity, and articles with the highest number of citations. The number of citations per article and year was obtained from Scopus. Annual growth was presented as the total number of articles per year. Relative growth rates (RGR), annual growth rates (AGR), and doubling time (DT) were calculated. RGR is the increase in the number of publications in a specified time and is calculated using the following formula: RGR = [logW2 − logW1]/(T2 − T1), where loge W1 is the log of the initial number of articles; log W2 is the log of the final number of articles after the ascertained period, and T2–T1 is the difference between the initial and the final time. This was then used to calculate the doubling time, which is the time required for publications to double in number in 1 year. The following formula was used to calculate DT: DT = 0.693/RGR. The annual growth rate (AGR) (the percentage change in the number of publications over 1 year) was also calculated based on the following formula: AGR = [(Ending Value – Beginning Value)/Beginning Value] * 100. Citation analysis was presented as frequency, mean, and median of citations per year. Authorship analysis was presented as the number of single-authored and multi-authored articles. Furthermore, the degree of collaboration was calculated according to the following formula: Degree of collaboration = C = Nm/Nm + Ns, where Nm = number of multi-authored papers and Ns = number of single-authored papers (Khaparde Professor & Pawar, 2013; Santha kumar & Kaliyaperumal, 2015).
Visual maps were created using VOS viewer software (van Eck & Waltman, 2010).
Results
Description of the Retrieved Literature
In total, 1468 documents were retrieved. Most documents (91.9%, n = 1349) were in the field of medicine. Other common subject areas were nursing (14.5%, n = 213), biochemistry and molecular biology (13.7%, n = 201), and health professions (5.6%, n = 82). Areas with less than 50 publications included pharmacology, psychology, and neuroscience. Of the total number of documents, 29.7% (n = 436) were diabetes related. The remaining bulk of literature covered a wide array of topics, including general health, clinical biomarkers, physical performance, kidney disease, cardiovascular disease, pregnancy, and diet. Analysis of the retrieved documents based on the subject area indicated that medicine was the most prolific area in all years. Meanwhile, interest in psychology, immunology, and dentistry remained modest throughout the study period.
Growth of Publications
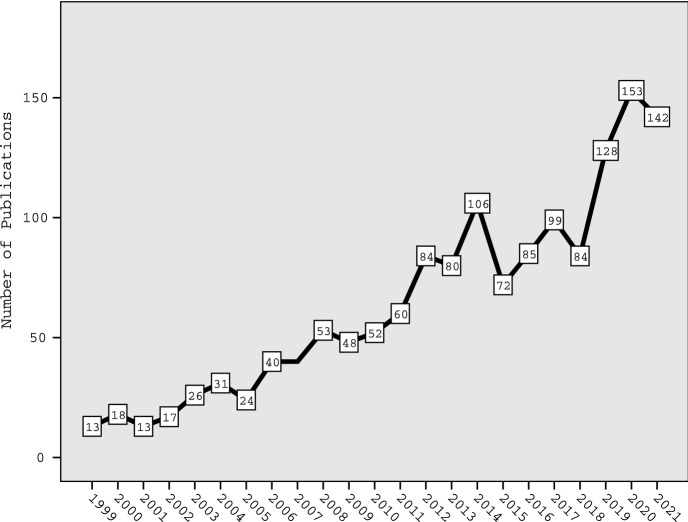
The mean number of publications during the study period was 63.8 documents per year. An increase in the number of publications with time was observed, although not without fluctuations. Table 1 shows the annual number of publications on Ramadan fasting during the study period. The highest productivity was observed in 2020, with a total of 153 (10.4%) documents, while the least number of publications was in 1999 and 2001 with 13 (0.9%) articles for each. As indicated in Table 1, AGR alternated between positive and negative values, showing a fluctuating pattern during the study period. The average AGR was 27. Meanwhile, RGR declined from 0.87 in 2000 to 0.00 in 2007 and rose slightly to 0.10 by the end of the study period (2021). These fluctuations translated into an unstable, fluctuating DT, indicating a non-exponential growth rate. Figure 1 shows the annual growth of publications during the study period. The total number of documents published from 2017 to 2021 constituted approximately 40.0% (n = 606) of the total number of retrieved documents.
Table 1.
Annual growth of retrieved publications on Ramadan fasting from 1999 to 2021
| Year | No | % N = 1468 | AGR | Cumulative total publications | RGR | DT |
|---|---|---|---|---|---|---|
| 1999 | 13 | 0.9 | – | 13 | – | – |
| 2000 | 18 | 1.2 | 38.46 | 31 | 0.87 | 0.80 |
| 2001 | 13 | 0.9 | − 27.78 | 44 | 0.35 | 1.98 |
| 2002 | 17 | 1.2 | 30.77 | 61 | 0.33 | 2.1 |
| 2003 | 26 | 1.8 | 52.94 | 87 | 0.35 | 1.98 |
| 2004 | 31 | 2.1 | 19.23 | 118 | 0.31 | 2.24 |
| 2005 | 24 | 1.6 | − 22.58 | 142 | 0.19 | 3.65 |
| 2006 | 40 | 2.7 | 66.67 | 182 | 0.25 | 2.77 |
| 2007 | 40 | 2.7 | 0.00 | 222 | 0.00 | – |
| 2008 | 53 | 3.6 | 32.5 | 275 | 0.21 | 3.3 |
| 2009 | 48 | 3.3 | − 9.43 | 323 | 0.16 | 4.33 |
| 2010 | 52 | 3.5 | 8.33 | 375 | 0.15 | 4.62 |
| 2011 | 60 | 4.1 | 15.38 | 435 | 0.15 | 4.62 |
| 2012 | 84 | 5.7 | 40 | 519 | 0.18 | 3.85 |
| 2013 | 80 | 5.5 | − 4.76 | 599 | 0.14 | 4.95 |
| 2014 | 106 | 7.2 | 32.5 | 705 | 0.16 | 4.33 |
| 2015 | 72 | 4.9 | − 32.08 | 777 | 0.10 | 6.93 |
| 2016 | 85 | 5.8 | 18.06 | 862 | 0.10 | 6.93 |
| 2017 | 99 | 6.7 | 16.47 | 961 | 0.12 | 5.78 |
| 2018 | 84 | 5.7 | − 15.15 | 1045 | 0.08 | '8.66 |
| 2019 | 128 | 8.7 | 52.38 | 1173 | 0.12 | 5.78 |
| 2020 | 153 | 10.4 | 19.53 | 1326 | 0.12 | 5.78 |
| 2021 | 142 | 9.7 | − 7.19 | 1468 | 0.10 | 6.93 |
Fig. 1.
Annual growth of health-related publications on Ramadan fasting (1999–2021)
Most Frequent Keywords
Figure 2 is a network visualization map of author keywords with a minimum frequency of 10 times. The map included 47 keywords. The node size is proportional to the frequency of occurrence of the keyword. The most frequent keywords were Ramadan and fasting. Other frequent keywords included diabetes-related keywords, nutrition-related keywords, blood pressure, and chronic kidney disease. The map also showed the keyword "COVID-19" indicative of publications on Ramadan fasting during the pandemic.
Fig. 2.
Network visualization map of author keywords with a minimum occurrence of 10 times. Node size correlates with the frequency of occurrence. Words that commonly co-occur tend to be located close to each other. Terms with common attributes are grouped into clusters with different colors
Authorship Pattern, Collaboration, and Prolific Authors
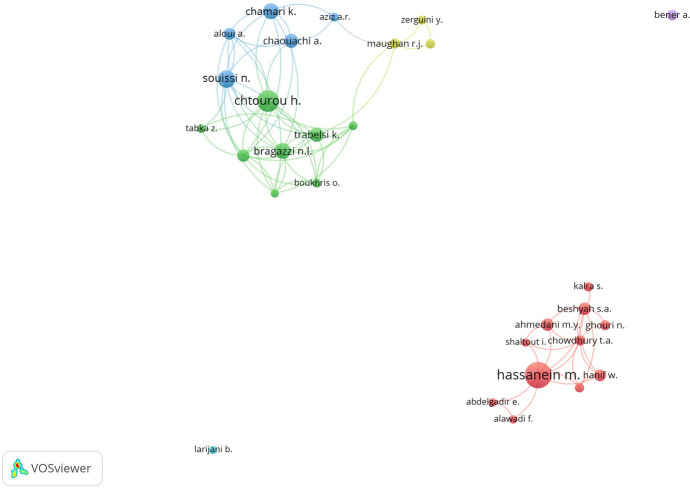
The average number of authors per document was 3.7. The vast majority of retrieved documents were multi-authored (88.6%, n = 1300), while only 11.4% (n = 168) were single-authored. The degree of collaboration was therefore 0.89 (89%). Table 2 shows the top ten productive authors. The most prolific author was Hassanein, M. (n = 42) from Dubai Hospital, Dubai, UAE, followed by Chtourou, H (n = 33) and Souissi, N.R (n = 25).
Table 2.
Top ten productive authors in the field of Ramadan fasting from 1999 to 2021
| Author’s rank* | Author | Frequency | Affiliation |
|---|---|---|---|
| 1st | Hassanein, M | 42 | Dubai Hospital, Dubai Health Authority, Dubai, United Arab Emirates |
| 2nd | Chtourou, H | 33 | High Institute of Sport and Physical Education, University of Sfax, Tunisia |
| 3rd | Souissi, N.R | 25 | Research Laboratory "Sports performance Optimization" National Center of Medicine and Science in Sports (CNMSS), Tunis, Tunisia |
| 4th | Bragazzi, N.L | 22 | Department of Health Sciences (DISSAL), Postgraduate School of Public Health, University of Genoa, 16,132, Genoa, Italy |
| 4th | Chamari, K | 22 | Research Laboratory "Sports performance Optimization" National Center of Medicine and Science in Sports (CNMSS), Tunis, Tunisia |
| 6th | Chaouachi, A | 19 | Research Unit Evaluation, Sport, Health, National Centre of Medicine and Science in Sport, Tunis, Tunisia |
| 6th | Trabelsi, K | 19 5 | University of Sfax, Laboratory of Pharmacology, Faculty of Medicine, Sfax, 3029, Tunisia |
| 8th | Ahmedani, M.Y | 16 | Department of Medicine, Baqai Institute of Diabetology and Endocrinology, Baqai Medical University, Karachi, Pakistan |
| 8th | Beshyah, S.A | 16 | Division of Endocrinology, Institute of Medicine, Sheikh Khalifa Medical City, Abu Dhabi, UAE; Department of Medicine, Dubai Medical College, Dubai, UAE |
| 10th | Aloui, A | 15 | High Institute of Sport and Physical Education, University of Sfax, Tunisia |
| 5th | |||
| 5th |
*Subjects with equal research output were given the same rank, and then, a gap was left in the ranking numbers
Figure 3 is a visualization map of author networking. Only authors with a minimum contribution of 10 documents were included. The map shows 29 scholars, distributed into six clusters. The largest cluster (red cluster) included 11 scholars. The cluster represented an international network of scholars from the Arab Gulf, Pakistan, and the UK. This cluster included the top active author; Hassanein, M. from the United Arab Emirates. The second-largest cluster (green cluster) included eight scholars including Chtourou, H. (Tunisia); one of the top active authors. The map showed no interaction between the two largest clusters.
Fig. 3.
Network visualization map of author networking. Only authors with a minimum contribution of 10 documents were included. The map shows 29 scholars, distributed into six clusters
Geographical Distribution of Publications
Authors from 87 countries contributed to the retrieved literature. Table 3 shows the top ten active countries in the field of Ramadan fasting. The UK ranked first with 181 (12.3%) publications, followed by Iran (10.4%, n = 153) and Saudi Arabia (9.8%, n = 144). The top ten most productive countries were distributed across West Asia, the Middle East and North Africa, and Western Europe.
Table 3.
Top ten active countries in the field of Ramadan fasting from 1999 to 2021
| Countries Rank* | Country | Number of publications (%); N = 1468 |
|---|---|---|
| 1st | UK | 181 (12.3) |
| 2nd | Iran | 153 (10.4) |
| 3rd | Saudi Arabia | 144 (9.8) |
| 4th | Turkey | 139 (9.5) |
| 5th | USA | 137 (9.3) |
| 6th | Tunisia | 128 (8.7) |
| 7th | United Arab Emirates | 106 (7.2) |
| 8th | Pakistan | 93 (6.3) |
| 9th | Egypt | 87 (5.9) |
| 10th | France | 70 (4.7) |
*Subjects with equal research output were given the same rank, and then, a gap was left in the ranking numbers
N = number of retrieved research articles
Figure 4 shows cross-country (international) research collaboration among countries with a minimum contribution of 10 publications. The map included 35 countries. Three countries showed a large node size indicative of high research connections with other countries. These countries were the United Arab Emirates, Saudi Arabia, and the UK. The UK exists in the center of the map with connections links with most countries on the map. The map showed Tunisia with connections to France and Canada indicative of research collaboration among these countries. The green cluster included several Islamic countries with close research collaboration.
Fig. 4.
Cross-country (international) research collaboration among countries with a minimum contribution of 10 publications. The map included 35 countries
Most Active Institutions
Table 4 shows the top ten most active institutions in the field of Ramadan fasting. Eight of the most active institutions were academic, while three were hospitals. The University of Sfax ranked first with 46 (3.1%) publications, followed by Dubai Hospital (2.9%, n = 42), and King Saud University (2.8%, n = 41).
Table 4.
Top ten active institutions in the field of Ramadan fasting from 1999 to 2021
| Institution’s Rank* | Institution | Number of publications (%); N = 1468 | Country of Institution |
|---|---|---|---|
| 1st | University of Sfax | 46 (3.1) | Tunisia |
| 2nd | Dubai Hospital | 42 (2.9) | UAE |
| 3rd | King Saud University | 41 (2.8) | Saudi Arabia |
| 4th | Tehran University of Medical Sciences | 38 (2.6) | Iran |
| 5th | Baqai Medical University | 26 (1.8) | Pakistan |
| 6th | Aspetar Orthopaedic and Sports Medicine Hospital | 24 (1.6) | Qatar |
| 7th | University of Toronto | 23 (1.6) | Canada |
| 7th | Università degli Studi di Genova | 23 (1.6) | Italy |
| 7th | Hamad Medical Corporation | 23 (1.6) | Qatar |
| 10th | Imperial College London | 22 (1.5) | UK |
| 10th | King Saud bin Abdulaziz University for Health Sciences | 22 (1.5) | Saudi Arabia |
*Subjects with equal research output were given the same rank, and then, a gap was left in the ranking numbers
N = number of retrieved research articles
Preferred Journals
The top 10 productive journals are listed in Table 5. The most active journal was “Diabetes Research and Clinical Practice” (4.9%, n = 72), followed by “Saudi Medical Journal” (2%, n = 30) and “Tunisie Medicale” (1.5%, n = 22). Most of the top ten productive journals were categorized in the subject area of medicine. Others also published in the subject area of biochemistry, genetics, molecular biology, food sciences and nutrition, and multidisciplinary areas.
Table 5.
Top ten active journals in the field of Ramadan fasting from 1999 to 20,212,018
| Journal’s activity rank* | Journal | Number of publications (%) N = 14,681,042 |
Subject area (category) | Journal rank** | Country | IF*** |
|---|---|---|---|---|---|---|
| 1st | Diabetes Research And Clinical Practice | 72 (4.9) | Biochemistry, Genetics, Molecular Biology, Endocrinology, and Medicine | Q1 | Netherlands | 5.602 |
| 2nd | Saudi Medical Journal | 30 (2) | Medicine (miscellaneous) | Q3 | Saudi Arabia | 1.484 |
| 3rd | Tunisie Medicale | 22 (1.5) | Medicine (miscellaneous) | Q4 | Tunisia | NA |
| 4th | Journal Of Sports Sciences | 21 (1.4) | Health professions and medicine | Q1 | UK | 3.337 |
| 4th | Pakistan Journal Of Medical Sciences | 21 (1.4) | Medicine (miscellaneous) | Q3 | Pakistan | 1.088 |
| 6th | Eastern Mediterranean Health Journal | 19 (1.3) | Medicine (miscellaneous) | Q3 | Switzerland | 1.628 |
| 7th | International Journal Of Clinical Practice | 18 (1.2) | Medicine (miscellaneous) | Q2 | US | NA |
| 7th | Plos One | 18 (1.2) | Multidisciplinary | Q1 | US | 3.240 |
| 9th | Nutrients | 17 (1.2) | Agricultural and Biological Sciences ( Food Science), Nursing ( Nutrition and Dietetics) | Q1 | Switzerland | 5.717 |
| 10th | Diabetes And Metabolic Syndrome Clinical Research And Reviews | 15 (1) | Medicine | Q2 | Netherlands | NA |
N = total number of retrieved literatures, IF = impact factor, Q = quartile
*Subjects with equal research output were given the same rank, and then, a gap was left in the ranking numbers
**Journal rank was obtained from Scimago Journal rank. Q1 = highest rank; Q4 = lowest rank
***Obtained from the 20,212,018 Journal Citation Reports by Clarivate Thomson Reuters
Growth of Citations and Top-Cited Documents
Retrieved publications were cited 19,585 times in total, with a mean of 13.3 citations per document. The h-index of retrieved documents was 60. An increase in citations can be observed from 1999 to 2014, with a decline in 2015, followed by another increase for the rest of the study period. The top 10 cited documents in the field of Ramadan fasting are listed in Table 6. The most cited publication was "A Population-Based Study of Diabetes and Its Characteristics During the Fasting Month of Ramadan in 13 Countries", published in 2004 in Diabetes Care journal and received 452 citations. The number of citations per document was highest for documents published in 2004 (36.6 citations per document), while the lowest was for those published in 2021 (0.85 citations per document). Six of the top 10 cited documents were DM-related, while the other four discussed general health.
Table 6.
Top ten cited articles in the field of Ramadan fasting from 1999 to 2021
| Article rank* | Title | Subject theme | Cited by |
|---|---|---|---|
| 1st | "A Population-Based Study of Diabetes and Its Characteristics During the Fasting Month of Ramadan in 13 Countries" | Diabetes Mellitus | 452 |
| 2nd | " Recommendations for management of diabetes during Ramadan: Update 2010” | Diabetes Mellitus | 242 |
| 3rd | "The changes of metabolic profile and weight during Ramadan fasting" | General Health | 192 |
| 4th | "The impact of religious fasting on human health" | General Health | 191 |
| 5th | "Recommendations for management of diabetes during Ramadan" | Diabetes Mellitus | 177 |
| 5th | "Effects on health of fluid restriction during fasting in Ramadan" | General Health | 177 |
| 5th | "Effects on health of fluid restriction during fasting in Ramadan" | General Health | 177 |
| 7th | Ramadan Education and Awareness in Diabetes (READ) programme for Muslims with type 2 diabetes who fast during Ramadan | Diabetes Mellitus | 157 |
| 8th | “Diabetes and Ramadan: Practical guidelines” | Diabetes Mellitus | 153 |
| 9th | “Impact of caloric and dietary restriction regimens on markers of health and longevity in humans and animals: A summary of available findings” | General Health | 139 |
| 10th | “Diabetes and Ramadan: Review of the literature” | Diabetes Mellitus | 116 |
*Subjects with equal research output were given the same rank, and then, a gap was left in the ranking numbers
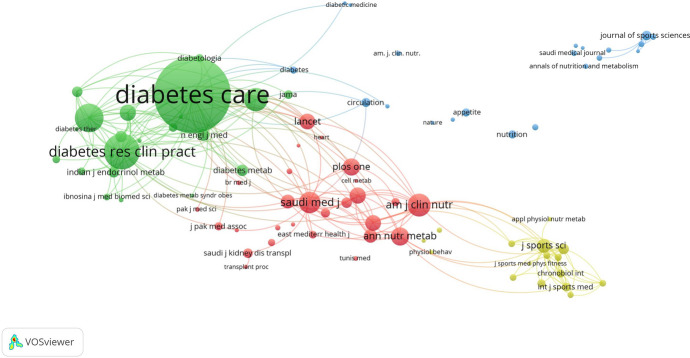
Co-citation Analysis
Figure 5 is a co-citation analysis of journals that received a minimum of 50 citations. The map included 86 journals. The clusters in the map represent scientific disciplines that helped in the emergence of the field of health issues and Ramadan fasting. The map shows three main clusters. The first cluster is related to diabetic medicine. The second cluster is related to nutrition, while the third cluster is related to sports medicine. These three disciplines were the foundation of the field: diabetes, nutrition, and sports.
Fig. 5.
Co-citation analysis of journals that received a minimum of 50 citations. The map included 86 journals. The clusters in the map represent scientific disciplines that helped in the emergence of the field of health issues in the context of Ramadan fasting
Discussion
In this study, we describe the bibliometric indicators of literature on Ramadan fasting. With the vast majority of documents being multi-authored, the degree of collaboration reached as high as 89%. Asian countries contributed the most to literature. This can be justified by the nature of the topic, which may be more relevant to countries with Muslim majorities. A progressive increase in the number of publications on Ramadan fasting was observed.
The vast majority of literature discussed Ramadan fasting and diabetes, while the rest covered various areas of disease and physiology. While most diabetic patients are exempt from fasting, many still desire to participate. A study found that 42.8% and 78.7% of type 1 and type 2 diabetics, respectively, fasted for at least 15 days of Ramadan (Salti et al., 2004). Another study reported fasting rates of 94.2% and 63.6% for 15 and 30 days, respectively, among type 2 diabetics (Babineaux et al., 2015).
Patients with diabetes may experience episodes of both hypo- and hyperglycemia because of fasting-associated glycogenolysis and gluconeogenesis (Karamat et al., 2010). The risk of diabetic ketoacidosis also increases during Ramadan due to the increased ketogenesis (Al-Arouj et al., 2010). Evidence-based guidelines are therefore warranted for the management of DM patients who desire to fast during Ramadan. This has led to the development of the IDF-DAR Practical Guidelines for the management of diabetic patients during Ramadan (Hassanein et al., 2017). The guidelines stratify diabetic patients into risk categories and provide treatment recommendations accordingly. Insulin and hypoglycemic agent regimens may require modifications during the month of Ramadan in cases where patients decide to fast (sometimes against medical advice) (Hassanein et al., 2017).
Other health states on which the impact of Ramadan fasting has been studied include CKD, nephrolithiasis, COPD, psoriasis, cancer, and gastrointestinal diseases (Rouhani & Azadbakht, 2014). However, literature on these illnesses remains scarce. Moreover, some of the studies lack optimal control of confounders, which calls for more accurate and reliable studies to derive clinical guidelines (Rouhani & Azadbakht, 2014).
The impact of Ramadan fasting on healthy individuals was also studied. Weight loss during Ramadan was reported by several studies, although only to be regained shortly over the course of the following months (Faris et al., 2012; Kul et al., 2014). Beneficial effects of fasting on lipid profile were seen in men, mainly as a decrease in total cholesterol and triglycerides levels. HDL was increased in women after Ramadan compared with pre-Ramadan values (Kul et al., 2014). Studies on pregnant women showed no fasting-associated negative health outcomes on offspring. However, due to the limitations of those studies, fasting is not recommended during pregnancy (Rouhani & Azadbakht, 2014).
Muslims consider Ramadan as a month of blessing, and very few studies have been published to investigate the negative psychological impact of fasting on Muslims. Ramadan tends to have a positive psychological impact on Muslims due to social gatherings and religious activities all during the month (Bayani et al., 2020).
In this study, seven of the most published authors were active in the area of sports. In addition, 4th top journal is sports-related. As Muslim athletes may observe the month of Ramadan during game season, several studies have assessed the effect of Ramadan fasting on physical performance and risk of injury (Memari et al., 2011). Zerguini et al. conducted a study on football players undergoing training camp 3 weeks before Ramadan and during the month (Zerguini et al., 2008). None of the parameters assessed during training, including performance, biochemical, and nutritional variables, were found to be negatively affected by fasting. This was supported by another study that found no effect of fasting on mood states of football players training in the morning period (Chtourou et al., 2014). However, results from a study on untrained persons show negative effects of Ramadan fasting on aerobic fitness, agility, and flexibility scores (Roy & Bandyopadhyay, 2015). Moreover, a study on martial arts competitors has shown a decrease in cognitive function in the form of lowered verbal learning and memory abilities during Ramadan (Tian et al., 2011).
It is estimated that there are around 1.5 billion Muslims around the world (Kul et al., 2014). With globalization, many Muslims now live in western societies, making Ramadan fasting an area relevant not only to countries with Muslim majorities but to societies worldwide. However, research in the field remains to be centralized in areas of south and East Asia, with very little contribution from Europe or North America. No definite explanation can be given for this finding except that non-Muslim researchers and funding agencies might not be interested or are not aware of health-related issues of Ramadan fasting. Muslim researchers in these regions need to focus on the positive psychological aspects of Ramadan fasting on Muslim families in non-Muslim countries. This is an important aspect of religion in general where rates of depression, suicide, and other mental health disorders might be high (Steel et al., 2014).
Limitations
Despite the wide inclusion of the Scopus database, the presence of unindexed journals is still a possibility. The bibliometric nature of the study also carries a risk of both false negatives and positives. However, the search strategy was designed to increase accuracy as much as attainable. The presence of multiple names or different spellings of an author's name may also negatively affect the productivity of the author. Data retrieval was limited to articles published from 1999 to 2021. However, the number of articles published before 1999 was determined to be too little to affect results.
Conclusion
There are around 1.5 billion Muslims around the world, more and more of whom now live in western societies. Fasting during the month of Ramadan is one of the five pillars of Islam. Understanding the impact of Ramadan fasting on body physiology and mental health is vital to the development of clinical recommendations for Muslim populations. Moreover, providing evidence-based guidelines is required to aid physicians in providing patient-specific care during the month of Ramadan. To ensure treatment efficacy and fasting safety among patients who desire to fast, modifications to drug regimens may be required. Many other patients may be advised not to fast during the month. We conclude that there is a progressive growth in the number of publications on Ramadan fasting. However, more data are still required, and more reliable research is important for evidence-based disease management.
Funding
The authors have not disclosed any funding.
Declarations
Conflict of interest
The authors declare no conflicts of interest.
Ethical approval
The study was based on bibliometric data and did not involve any human subjects. Therefore, no ethical approval was required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Al-Arouj M, Assaad-Khalil S, Buse J, Fahdil I, Fahmy M, Hafez S, Hassanein M, Ibrahim MA, Kendall D, Kishawi S, Al-Madani A, Nakhi AB, Tayeb K, Thomas A. Recommendations for management of diabetes during Ramadan: Update 2010. Diabetes Care. 2010;33:1895–1902. doi: 10.2337/dc10-0896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Awwad J, Usta IM, Succar J, Musallam KM, Ghazeeri G, Nassar AH. The effect of maternal fasting during Ramadan on preterm delivery: A prospective cohort study. BJOG: an International Journal of Obstetrics and Gynaecology. 2012;119:1379–1386. doi: 10.1111/j.1471-0528.2012.03438.x. [DOI] [PubMed] [Google Scholar]
- Babineaux SM, Toaima D, Boye KS, Zagar A, Tahbaz A, Jabbar A, Hassanein M. Multi-country retrospective observational study of the management and outcomes of patients with Type 2 diabetes during Ramadan in 2010 (CREED) Diabetic Medicine. 2015;32:819–828. doi: 10.1111/dme.12685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- BaHammam A, Alrajeh M, Albabtain M, Bahammam S, Sharif M. Circadian pattern of sleep, energy expenditure, and body temperature of young healthy men during the intermittent fasting of Ramadan. Appetite. 2010;54:426–429. doi: 10.1016/j.appet.2010.01.011. [DOI] [PubMed] [Google Scholar]
- Bahijri S, Borai A, Ajabnoor G, Abdul Khaliq A, AlQassas I, Al-Shehri D, Chrousos G. Relative metabolic stability, but disrupted circadian cortisol secretion during the fasting month of ramadan. PLoS ONE. 2013;8:e60917. doi: 10.1371/journal.pone.0060917. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayani AA, Esmaeili R, Ganji G. The Impact of fasting on the psychological well-being of muslim graduate students. Journal of Religion and Health. 2020;59:3270–3275. doi: 10.1007/S10943-018-00740-3. [DOI] [PubMed] [Google Scholar]
- Beshyah WS, Beshyah SA. Bibliometric analysis of the literature on Ramadan fasting and diabetes in the past three decades (1989–2018) Diabetes Research and Clinical Practice. 2019;151:313–322. doi: 10.1016/J.DIABRES.2019.03.023. [DOI] [PubMed] [Google Scholar]
- Bragazzi NL. Ramadan fasting and chronic kidney disease: A systematic review. Journal of Research in Medical Sciences. 2014;19:665–676. [PMC free article] [PubMed] [Google Scholar]
- Bragazzi NL, Briki W, Khabbache H, Rammouz I, Mnadla S, Demaj T, Zouhir M. Ramadan fasting and infectious diseases: A systematic review. Journal of Infection in Developing Countries. 2015;9:1186–1194. doi: 10.3855/jidc.5815. [DOI] [PubMed] [Google Scholar]
- Chtourou H, Briki W, Hammouda O, Aloui A, Souissi N, Chaouachi A. The effect of the time-of-day of training during Ramadan on soccer players’ chronotype and mood states. Sport Sciences for Health. 2014;10:143–147. doi: 10.1007/S11332-014-0185-X. [DOI] [Google Scholar]
- Damiani G, Watad A, Bridgewood C, Pigatto PDM, Pacifico A, Malagoli P, Bragazzi NL, Adawi M. The impact of ramadan fasting on the reduction of PASI score, in moderate-to-severe psoriatic patients: A real-life multicenter study. Nutrients. 2019;11:277. doi: 10.3390/nu11020277. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Develioglu ON, Kucur M, Ipek HD, Celebi S, Can G, Kulekci M. Effects of ramadan fasting on serum immunoglobulin g and m, and salivary immunoglobulin a concentrations. Journal of International Medical Research. 2013;41:463–472. doi: 10.1177/0300060513476424. [DOI] [PubMed] [Google Scholar]
- El MekkaouiKaoutar AS, Ihssane M, Adil I, Dafr-Allah B. Effect of Ramadan fasting on acute upper gastrointestinal bleeding. Journal of Research in Medical Sciences. 2013;18:230–233. [PMC free article] [PubMed] [Google Scholar]
- Falagas ME, Pitsouni EI, Malietzis GA, Pappas G. Comparison of PubMed, Scopus, Web of Science, and Google Scholar: Strengths and weaknesses. The FASEB Journal. 2008;22:338–342. doi: 10.1096/fj.07-9492LSF. [DOI] [PubMed] [Google Scholar]
- Faris MAIE, Kacimi S, Al-Kurd RA, Fararjeh MA, Bustanji YK, Mohammad MK, Salem ML. Intermittent fasting during Ramadan attenuates proinflammatory cytokines and immune cells in healthy subjects. Nutrition Research. 2012;32:947–955. doi: 10.1016/j.nutres.2012.06.021. [DOI] [PubMed] [Google Scholar]
- Haouari M, Haouari-Oukerro F, Sfaxi A, Ben Rayana MCH, Kâabachi N, Mbazâa A. How ramadan fasting affects caloric consumption, body weight, and circadian evolution of cortisol serum levels in young, healthy male volunteers. Hormone and Metabolic Research. 2008;40:575–577. doi: 10.1055/s-2008-1065321. [DOI] [PubMed] [Google Scholar]
- Hassanein M, Al-Arouj M, Hamdy O, Bebakar WMW, Jabbar A, Al-Madani A, Hanif W, Lessan N, Basit A, Tayeb K, Omar MAK, Abdallah K, Al Twaim A, Buyukbese MA, El-Sayed AA, Ben-Nakhi A. Diabetes and Ramadan: Practical guidelines. Diabetes Research and Clinical Practice. 2017;126:303–316. doi: 10.1016/j.diabres.2017.03.003. [DOI] [PubMed] [Google Scholar]
- Husain S, Zafar M, Ullah R. Ramadan and public health: A bibliometric analysis of top cited articles from 2004 to 2019. Journal of Infection and Public Health. 2020;13:275–280. doi: 10.1016/J.JIPH.2019.11.006. [DOI] [PubMed] [Google Scholar]
- Karamat MA, Syed A, Hanif W. Review of diabetes management and guidelines during Ramadan. Journal of the Royal Society of Medicine. 2010;103:139–147. doi: 10.1258/jrsm.2010.090254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khaparde Professor V, Pawar S. Authorship Pattern and Degree of Collaboration in Information Technology. Journal of Computer Science & Information Technology. 2013;1:46–54. [Google Scholar]
- Kul S, Savaş E, Öztürk ZA, Karadağ G. Does ramadan fasting alter body weight and blood lipids and fasting blood glucose in a healthy population? A meta-analysis. Journal of Religion and Health. 2014;53:929–942. doi: 10.1007/s10943-013-9687-0. [DOI] [PubMed] [Google Scholar]
- Memari AH, Kordi R, Panahi N, Nikookar LR, Abdollahi M, Akbarnejad A. Effect of ramadan fasting on body composition and physical performance in female athletes. Asian Journal of Sports Medicine. 2011;2:161–166. doi: 10.5812/ASJSM.34754. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mikhailov OV, evich A new version of the Hirsh index: The j-index. Herald of the Russian Academy of Sciences. 2014;84:217–220. doi: 10.1134/S1019331614030101. [DOI] [Google Scholar]
- Roky R, Chapotot F, Hakkou F, Benchekroun MT, Buguet A. Sleep during Ramadan intermittent fasting. Journal of Sleep Research. 2001;10:319–327. doi: 10.1046/j.1365-2869.2001.00269.x. [DOI] [PubMed] [Google Scholar]
- Rouhani MH, Azadbakht L. Is Ramadan fasting related to health outcomes? A review on the related evidence. Journal of Research in Medical Sciences. 2014;19:987–992. [PMC free article] [PubMed] [Google Scholar]
- Roy AS, Bandyopadhyay A. Effect of Ramadan intermittent fasting on selective fitness profile parameters in young untrained Muslim men. BMJ Open Sport and Exercise Medicine. 2015;1:e000020. doi: 10.1136/bmjsem-2015-000020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeghpour S, Keshteli AH, Daneshpajouhnejad P, Jahangiri P, Adibi P. Ramadan fasting and digestive disorders: SEPAHAN systematic review no. 7. Journal of Research in Medical Sciences. 2012;17:S150–S158. [Google Scholar]
- Salti I, Bénard E, Detournay B, Bianchi-Biscay M, Le Brigand C, Voinet C, Jabbar A. A population-based study of diabetes and its characteristics during the fasting month of ramadan in 13 countries: Results of the epidemiology of diabetes and ramadan 1422/2001 (EPIDIAR) study. Diabetes Care. 2004;27:2306–2311. doi: 10.2337/diacare.27.10.2306. [DOI] [PubMed] [Google Scholar]
- Santha kumar R, Kaliyaperumal K. A scientometric analysis of mobile technology publications. Scientometrics. 2015;105:921–939. doi: 10.1007/s11192-015-1710-7. [DOI] [Google Scholar]
- Steel Z, Marnane C, Iranpour C, Chey T, Jackson JW, Patel V, Silove D. The global prevalence of common mental disorders: A systematic review and meta-analysis 1980–2013. International Journal of Epidemiology. 2014;43:476–493. doi: 10.1093/IJE/DYU038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tian HH, Aziz AR, Png W, Wahid MF, Yeo D, Png ALC. Effects of fasting during ramadan month on cognitive function in muslim athletes. Asian Journal of Sports Medicine. 2011;2:145. doi: 10.5812/ASJSM.34753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Eck NJ, Waltman L. Software survey: VOSviewer, a computer program for bibliometric mapping. Scientometrics. 2010;84:523. doi: 10.1007/S11192-009-0146-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van Ewijk RJG, Painter RC, Roseboom TJ. Associations of prenatal exposure to ramadan with small stature and thinness in adulthood: Results from a large indonesian population-based study. American Journal of Epidemiology. 2013;177:729–736. doi: 10.1093/aje/kwt023. [DOI] [PubMed] [Google Scholar]
- Zerguini Y, Dvorak J, Maughan RJ, Leiper JB, Bartagi Z, Kirkendall DT, Al-Riyami M, Junge A. Influence of Ramadan fasting on physiological and performance variables in football players: Summary of the F-MARC 2006 Ramadan fasting study. Journal of Sports Sciences. 2008;26:S3–S6. doi: 10.1080/02640410802614944. [DOI] [PubMed] [Google Scholar]
- Zouari H, Latiri I, Mahjoub M, Boussarsar M, Benzarti M, Abdelghani A, Ben Saad H. The Effects of Ramadan Intermittent Fasting (RIF) on Spirometric Data of Stable COPD Patients: A Pilot Study. American Journal of Men’s Health. 2018;12:359–369. doi: 10.1177/1557988317734131. [DOI] [PMC free article] [PubMed] [Google Scholar]