Abstract
Purpose of Review
The purpose of this review was to describe the state-of-the-literature on research specific to cannabis vaping among youth and young adults.
Recent Findings
Out of 1801 records identified, a total of 202 articles met eligibility criteria for inclusion in this review. Most of this literature (46.0% of studies) was specific to the health effects of cannabis vaping, particularly EVALI (e-cigarette and vaping associated lung injury). Other research areas identified in the review included the etiology (24.3%) and epidemiology (24.8%) of cannabis vaping, in addition to articles on regulation (8.4%) and marketing (5.5%) of the same.
Summary
Cannabis vaping is increasingly common among youth and young adults and more prevalent is settings where recreational use for adults has been legalized. The literature documents a number of negative health effects of cannabis vaping for young people, along with risk factors and reasons for the same.
Supplementary Information
The online version contains supplementary material available at 10.1007/s40429-022-00413-y.
Keywords: Cannabis, Vaping, Health effects, Epidemiology, Etiology, Regulation
Introduction
The purpose of this review was to describe the state-of-the-literature regarding research specific to cannabis vaping among youth and young adults [1]. A recent meta-analysis found that among adolescents in the USA and Canada, lifetime, past-12 month, and 30-day prevalence of cannabis vaping increased by two- to seven-fold, from 2013 to 2020 [2•]. Preference for cannabis products, therefore, may be shifting from dried herb to cannabis oil (e.g., liquid tetrahydrocannabinol (THC), the primary psychoactive component in cannabis) — and, given the emergence [3] and predominance of e-cigarette use among young people now [4, 5], from smoking to vaping cannabis. Here, we provide a summary of results from 202 original investigations on this topic (see Supplementary Table 2), published between 2007 and 2021. These studies include information relevant to the epidemiology, health effects, etiology, marketing, and regulation of cannabis vaping and are applicable to young people less than 30 years old.
Methods
This review was conducted using methods consistent with the Preferred Reporting Items for Systematic Review and Meta-Analysis for scoping reviews (PRISMA-ScR) [6]. A scoping review was deemed appropriate, as it focuses on an assessment of the potential size and scope of available literature. We categorize the available literature into relevant sub-topics and summarize the findings in the “Results” section.
Search Strategy
Our search strategy was informed by recent published reviews of vaping among youth and young adults specific to the impact that nicotine vaping has on subsequent cannabis [7] or combustible tobacco product use [8–11]. Consistent with these reviews, the following databases were searched for studies: PubMed, Embase, and Web of Science. In addition, searches were conducted on the aforementioned reviews [7–11] and relevant summary reports [3, 12, 13] for additional studies, too. Keywords included: e-cigarettes, vaping, ENDS, JUUL; cannabis, marijuana, THC, CBD; adolescents, young adults. Keywords used for each database are provided in Supplementary Table 1. When available, we used subject headings (PubMed: MeSH; Embase: Emtree). Searches were conducted from January 2007 to December 2021. The initial date was chosen as it coincides with the appearance of the “modern” e-cigarette or vaping device on the international market [14].
Study Selection
All studies retrieved through these searches were imported into software designed to support systematic reviews (https://www.covidence.org/) [15] and study selection was done there. There were five inclusion criteria. First, we included studies that examined cannabis vaping as a central topic or had findings about cannabis vaping. Second, study participants were youth (12–18 years old) and/or young adults (18–29 years old), or the study findings were relevant for young people (e.g., the unit of analysis was advertisements, but study findings were relevant for youth and/or young adults). Third, studies were original research; fourth, studies were full-text articles; and fifth, the articles were written in English. The reasons for exclusion included studies in which cannabis was not vaped, but only consumed in some other form; studies that only addressed vaping with substances other than cannabis (e.g., nicotine, flavors only); studies whose participants were not youth or young adults; animal studies; and, finally, articles that were not original research (e.g., editorials, commentaries, and review articles).
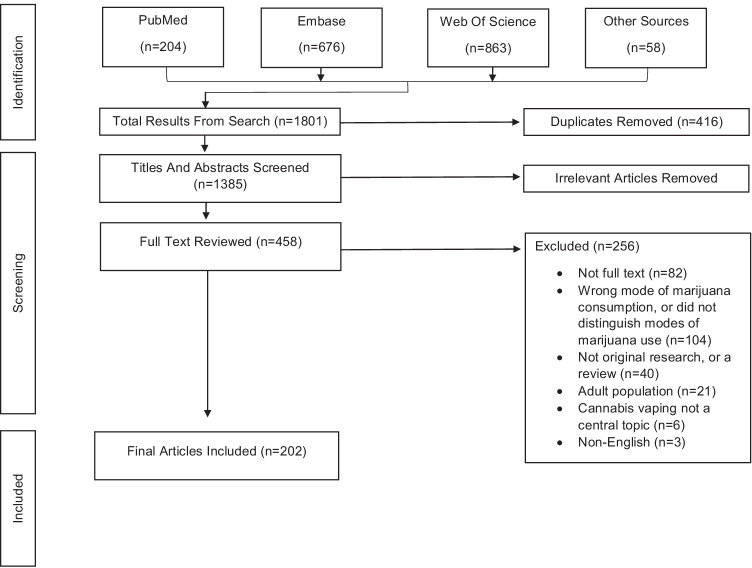
A total of 1801 articles were initially identified. After removing 416 duplicates, 1385 titles and abstracts were independently reviewed by at least 2 of the 6 co-authors to determine their suitability for full-text screening. After removing 927 articles at this stage, each of 458 articles selected for full-text screening was again independently reviewed by at least 2 co-authors for inclusion. Any discrepancies between reviewers were discussed among all co-authors until consensus was reached. Ultimately, 202 articles were deemed relevant. Figure 1 is the PRISMA flow diagram for this process. Supplementary Table 2 provides a list of these 202 articles.
Fig. 1.
PRISMA flow diagram
Extraction
Data extracted from each study included the following: study design; study sub-topic, including epidemiology, health effects, etiology, marketing, and regulation; key findings about cannabis vaping within each sub-topic area; and, where relevant, study characteristics (e.g., location, participants’ age). Typical of a scoping review, no formal assessment of the quality of the eligible manuscripts was conducted, so information on the risk of bias that may be inherent in each of these studies is not presented here.
Results
Overview
No studies that met the inclusion criteria were published from 2007 to 2013. From 2013 onwards, the rate of publication increased exponentially, reaching a peak in 2020 (Supplementary Fig. 1) that was driven, in large part, by many articles (n = 70) on EVALI (e.g., case reports). Table 1 provides a summary of the number of articles reviewed here, by study design and sub-topic. Most studies were specific to health effects and etiology.
Table 1.
Frequency of studies by study design and research area (n = 202)
| Characteristic | n | (%) |
|---|---|---|
| Study designs1 | ||
| Case-reports | 44 | (21.8%) |
| Case-series | 28 | (13.9%) |
| Randomized controlled trials | 4 | (2.0%) |
| Observational | 105 | (52.0%) |
| Cross-sectional | 84 | (41.6%) |
| Cohort/longitudinal | 21 | (10.4%) |
| Qualitative | 18 | (8.9%) |
| Mixed methods2 | 2 | (1.0%) |
| Meta-analysis | 1 | (0.5%) |
| Research areas3 | ||
| Health effects | 93 | (46.0%) |
| Etiology | 49 | (24.3%) |
| Epidemiology | 50 | (24.8%) |
| Regulatory policy | 17 | (8.4%) |
| Marketing/advertising | 11 | (5.5%) |
1Categories are mutually exclusive. 2Mixed methods studies were cross-sectional + case series and longitudinal + qualitative. 3Categories are mutually inclusive
Epidemiology
National Estimates
Annual prevalence estimates of cannabis vaping were available from Monitoring the Future (MTF) from 2017 to 2021 for youth (8th, 10th, and 12th grade) and from 2017 to 2021 for young adults (college students) and are shown in Supplementary Fig. 2 (lifetime use) and Supplementary Fig. 3 (past 30-day use) [4]. Lifetime use increased rapidly for both age groups from 2017 to 2020 then, for youth, declined in 2021. Among youth, lifetime prevalence rose from 8.5% in 2017 to 20.1% in 2020, then decreased to 15.9% in 2021. Among young adults, lifetime prevalence increased from 14.4% in 2017 to 34.6% in 2020. Notably, the doubling of past 30-day cannabis vaping observed among young adults (college students) from 2017 to 2018 was among the largest 1-year increase in any substance use ever recorded in the history of MTF (> 40 years) [4]. From 2018 to 2019, a similar doubling in the prevalence of past 30-day cannabis vaping was also observed for youth (8th, 10th, and 12th grade) [16]. Frequent vaping (defined as using ≥ 10 times in the last month) increased significantly among high school seniors from 2018 to 2019, too [17]. MTF data for young adults for 2021 were not available at this writing. (Note that the MTF publications that these prevalence estimates are derived from report data on “vaping marijuana” questions measured in the vaping section of the survey [4, 16]. One recent study shows that there is some discordance in prevalence estimates, if measures from the cannabis section on “using cannabis in a vaporizer” are used, instead [18]. Thus, researchers must take care when considering how best to ask questions about cannabis vaping and where to place them on a survey instrument [19].
Despite these alarming statistics, it is worth noting that, for each year (2017 to 2020), behavioral measure, and age group, the prevalence of cannabis vaping was less than the prevalence of nicotine vaping (data not shown) [4, 20–23]. For young adults, the prevalence of cannabis vaping was 20–30% less than that for nicotine vaping, while it was 50–60% less among youth. It is also worth reporting that from 2015 to 2018 (latest published data, among 12th graders only), cannabis smoking decreased, while cannabis vaping and the use of edibles increased [24]. From 2015 to 2018, for all students and among past-year cannabis users specifically, the prevalence of smoking cannabis was 2–3 times higher than the prevalence of vaping or use of edibles [24, 25].
This comparison across substances (nicotine vs. cannabis) and modes of consumption (smoking vs. vaping vs. edibles) helps to contextualize cannabis vaping among young people, demonstrating that, for now, it may not be as problematic as other substance use behaviors. However, given observed increases in recent years, efforts should continue to monitor cannabis vaping among young people in the future, and assessing modes of consumption may be a helpful way to guide prevention efforts [26]. Data on cannabis vaping are currently collected not only by MTF but also by the National Youth Tobacco Survey (NYTS) (youth only) [27–29], the Behavioral Risk Factor Surveillance System (BRFSS) (young adults only) [30, 31], and the Population Assessment of Tobacco Use and Health (PATH) study (youth and young adults) [32]. Each surveillance system offers unique insights into this phenomenon, given data it collects not only on cannabis vaping but also on other substance use behaviors and modes of cannabis consumption, too.
An analysis of PATH data from 2015 to 2016 for young adults (18–24 years old), for example, showed that lifetime or ever use of cigar products (e.g., cigarillos) to consume cannabis (i.e., blunt use) was 3 times more common than consuming cannabis by vaping or using a hookah to do so [32]. BRFSS surveys also include items on different modes of cannabis consumption (i.e., smoking, vaping, eating, and dabbing) [30] and can be used to compare nicotine vaping and cannabis vaping [31]. Analyses of BRFSS data from 2018 showed past 30-day dual nicotine and cannabis vaping was as common among young adults as past 30-day cannabis vaping alone [31]. Analyses of NYTS data from 2017 and 2018 showed that cannabis vaping was especially common for students who frequently use (i.e., use ≥ 20 days per month) e-cigarettes [27]. Surveillance data on lifetime or ever cannabis vaping on the 2016 [28], 2017 [29], and 2018 [29] NYTS surveys are consistent with the sustained increase reported in MTF, too. Two published studies [33, 34] specifically examined the possible impact of the COVID-19 epidemic on cannabis vaping among youth and young adults. One study showed that individual use increased, decreased, or stayed the same, depending on relevant risk factors (e.g., access, dependence) [33]. Another national study of more than 4000 adolescents and young adults showed only 6.8% of participants increased cannabis vaping during the pandemic, while 37% reduced or quit cannabis vaping, and 42.3% reported no change [34]. Though not explicitly stated by MTF, COVID-19 could be a reason for the leveling-off of past 30-day cannabis vaping from 2019 to 2021 among both age groups seen in MTF (Fig. 4).
Estimates by State
The prevalence of cannabis vaping among young people does vary by state, consistent with differences in local policies regarding age restrictions on use [35–43]. More information is provided below (see “Regulation” section). Data from the 2017 Healthy Kids Colorado survey, one of the first states to legalize recreational cannabis use for adults, showed that vaping was far less common as a mode of consumption among youth than smoking or ingesting cannabis (i.e., edible use) [44]. NYTS data from Florida (2015) [45] and North Carolina (2017) [46], where recreational cannabis use was and still is illegal, even for adults, showed 1 in 10 high students reported cannabis vaping.
International Estimates
Several studies identified through this review provided estimates of cannabis vaping among young people from other countries [47–53]. Data for 16 to 19 year-olds from the International Tobacco Control Policy Evaluation (ITC) study showed cannabis vaping is more prevalent in the USA, followed by Canada and England, consistent with regulatory policy in each country [51–53]. From 2017 to 2019, no significant differences in the prevalence of past 30-day use of a vaporizer to heat dried herb were observed within countries (England: 8.1% (2017), 12.5% (2018), 11.1% (2019); Canada: 15.9% (2017), 19.3% (2018), 19.1% (2019); USA: 20.6% (2017), 21.5% (2018), 23.0% (2019)). However, from 2017 to 2019, significant increases were observed for each country in the prevalence of past 30-day use of an e-cigarette to vape oil or liquid (England: 9.0% (2017), 14.6% (2018), 19.0% (2019); Canada: 12.9% (2017), 18.8% (2018), 25.9% (2019); USA: 24.2% (2017), 31.0% (2018), 52.1% (2019)). In 2017, for all three countries, vaping herb or vaping oil/liquid was the least common modes of cannabis consumption; yet, from 2017 to 2019, across all three countries, vaping oil/liquid increased more than other modes of consumption (vaping herb, smoking, and edible use) [51]. In addition, while nicotine vaping was also more prevalent than cannabis vaping across these countries [53], dual use was common [52]; and, in 2018, past 30-day cannabis users in the USA were more likely to report vaping cannabis than in Canada or England [53]. Findings from the COMPASS study in Canada before legalization in 2018 showed that ingesting and/or vaping cannabis were more often in addition to smoking cannabis, rather than as a replacement [49]. Follow-up studies from COMPASS that included data from 2017 to 2018 and 2018–2019 showed multiple modes of cannabis consumption (smoking, vaping, and/or ingesting) and increased frequency of the same were more common among high school students after legalization in 2018 [54–56]. Other studies from Finland [48] and Germany [50] show cannabis vaping among young people, at < 10%, may be less prevalent in these European countries than in England [51] though differences between studies by age and year of data collection make comparison difficult. Pooled estimates across 2016–2018 from one study of youth (14–15 years old) in New Zealand show cannabis vaping is less prevalent there, too [57]. Less than 10% of students reported using cannabis in the past 30-day days and, of these, only 7% reported exclusive cannabis vaping; 90% reported smoking cannabis, in contrast [57]. Estimates from other countries were not located in this review.
Use Trajectories
Several studies reported on developmental trajectories of use that describe the onset and progression of cannabis vaping across adolescence into young adulthood [58–63]. Several of these studies focused on cannabis vaping only [60–63], while others show cannabis vaping co-occurs with other substance use behaviors [58, 59]. Studies from California [60] and Texas [63] both show variability by sub-groups of young people: some young people start cannabis vaping in adolescence, while others begin in young adulthood; and some trajectories escalate quickly, while others escalate less rapidly. However, declines in use from adolescence into young adulthood are generally not observed [60, 63]. Taken together, these studies suggest a strong, positive relationship between age and cannabis vaping that may (or may not) peak in young adulthood. No studies reported on quit intentions or behaviors, providing scope for future research.
Special Populations
Several studies reported on use in special populations [64–69], like hospitalized adolescents [69], pregnant young adults [68], young adults with asthma [67], nightclub patrons [66], young people with inflammatory bowel disease [65], and young people in substance use treatment centers [64]. The reader is directed to these publications for further information. Data for all of these studies were collected between 2015 and 2020.
Health Effects
EVALI
In Spring 2019, reports of e-cigarette, or vaping, associated lung injury (EVALI) began to emerge across the USA, with cases peaking in Summer 2019 [1, 2•]. Cases were characterized by respiratory, gastrointestinal, and/or constitutional symptoms, including cough, difficulty breathing, nausea, diarrhea, fever, chills, and/or weight loss [1, 3]. To date, the Centers for Disease Control and Prevention (CDC) has recorded 2807 EVALI cases and 68 deaths across 50 states, Puerto Rico and the US Virgin Islands. The severity of EVALI varies, with the most severe cases leading to extended ICU stays, lung transplants, and death [1, 2•]. Given the emergence of EVALI and the subsequent research that implicated vitamin E acetate found in some cannabis vape products in the outbreak, the majority of studies investigating the health effects of cannabis vaping (n = 93) focused on EVALI (n = 70), including 34 case reports [70–102], 25 case series [103–128], 8 cross-sectional studies [129•, 130–136], 1 longitudinal study [137], and 1 qualitative study [138]. One study included a case series of EVALI patients and a cross-sectional analysis of vaping devices; therefore, this was counted as both a case series and cross-sectional study [26].
The case series and case reports detailed symptoms at diagnosis including respiratory, gastrointestinal, and constitutional symptoms; and information on the treatment and outcomes of numerous patients with EVALI. Among the case reports (n = 34) [70–102, 139], 10 studies were adolescent patients (12 to 17 year olds), and 23 involved young adults (18 to 29 year olds); 31 of the 34 cases reported vaping THC or THC use was confirmed through urine analysis. Different diagnostic presentations of individuals with EVALI were provided in the articles, which aligned with the broad case definition established by the CDC, which includes (1) e-cigarette use or dabbing resin within 90 days of symptom onset, (2) pulmonary infiltrate present on radiographs, (3) no evidence of pulmonary infection with minimum workup of a viral respiratory panel and influenza testing, and (4) no evidence of alternative plausible diagnosis [4]. Studies highlighted a need to assess history of vaping use behaviors for patients with EVALI-like symptoms.
The case series papers (n = 25) provided insight into patterns of and risk factors for EVALI across individual patients [103–128, 137]. For example, among 160 patients reported to the California Department of Public Health, the median age of participants was 27 years, 62% were male, and 46% of patients were admitted to the intensive care unit [113]. Among the vaping devices gathered from participants (87 devices from 24 patients), 56% contained THC, and vitamin E acetate was found in 84% of the THC vape products [113]. Another case series of EVALI patients (n = 86) in Wisconsin and Illinois added to these findings by identifying Dank Vapes as a potential source of the contaminated cartridges; 66% of patients reported use of Dank Vapes [118]. In addition to risk factors for EVALI, case series such as Kalininsky et al. described treatment considerations and recommendations [106]. Treatment recommendations for EVALI included (1) supportive respiratory support as needed (i.e., supplemental oxygen, ventilation), (2) antibiotics for severe cases, per blood culture results, (3) antivirals until influenza is excluded (if symptoms occur during flu season), and (4) corticosteroids to treat lung inflammation.
In the cross-sectional studies (n = 9), [126, 129•, 130–136] research highlighted demographic characteristics of EVALI patients, substance use behaviors, and risk factors for EVALI. Common risk factors across studies for EVALI included younger age, cannabis vaping, higher frequency of cannabis vaping, the use of Dank Vapes (a brand of e-cigarettes only available on the black market), as well as obtaining products from informal sources. These findings are supported by current evidence from the CDC; as of the last update (data from January 14, 2020) [140], 76% of EVALI patients were under 35 years of age. Blount et al. provided the strongest evidence on the link between vitamin E acetate and development of EVALI; vitamin E acetate was found in 94% of patients’ BAL (bronchoalveolar-lavage) fluid and was in BAL fluid taken from the control participants [130].
Other Health Issues
About 24.7% (n = 23) of the studies categorized under this sub-topic examined other health effects of cannabis vaping, including oral health issues, other respiratory effects, cardiotoxicity, and seizures [65, 141–162]. Young persons who vape cannabis with oral health issues presented with conditions such as dental caries, erosions, and ulcerations [147]. Case reports of teens who vape cannabis described someone with daily use presenting with seizures [149] and someone who vaped for the first time presented with myocardial ischemia following chest pain [150]. One young who vaped cannabis who presented with respiratory issues had bronchiolitis (with mechanism distinct from EVALI) [152]; while two cases who vaped cannabis were treated for nontuberculous mycobacteria (NTM) infection [153]. Another case report of a young person who vaped cannabis oil described symptoms of catatonia, mania, and psychosis supposedly induced by previous cannabis vaping [151]. Cases of eosinophilic pneumonitis, synthetic cannabinoid intoxication, Torsades de pointes, and cardiac arrest were reported among youth who vaped various forms of marijuana [155, 160–162]. A qualitative study which interviewed cannabis vaping youth reported participants describing the physical health effects ranging from respiratory, oral, nausea, and appetite related and headaches [157].
Other observational studies examined subjective effects, functioning (physical, social, and mental), and respiratory effects such as bronchitis and wheezing [65, 144–146, 156]. An intensive longitudinal study on subjective cannabis intoxication and modes of administration found that participants reported higher intoxication on the days they used only bongs than the days they used only vapes [158].
Experimental studies examined the effects of vaporized cannabis on cognition, psychomotor performance, and physiological pain [141–143]. In a double-blind crossover study, Wilsey et al. examined analgesic efficacy of vaporized cannabis by comparing medium dose, low dose, and placebo treatment [142]. Subjects reported greater pain relief (measured by visual analog scale and Patient Global Impression of Change) by using cannabis compared to placebo, while results were almost similar for low and high dose. Spindle et al. examined acute dose effects of smoked and vaporized cannabis in a double-blind, crossover study [141]. They reported higher peak concentrations of THC in blood and stronger drug effects for pharmacodynamic outcomes (subjective drug effects, cognitive and psychomotor performance) by using vaporized cannabis as compared to equal doses of smoked cannabis. In another double-blind, crossover study, Arkell et al. examined the effects of vaporized THC-dominant cannabis (containing 11% THC and < 1% CBD), THC/CBD equivalent cannabis (containing 11% THC and 11% CBD), and placebo (containing < 1% THC/CBD) on driving and cognitive performance [143]. Compared to placebo, cognitive performance was impaired by both cannabis types, especially by the THC/CBD equivalent. Both cannabis types had little effect on driving performance, except for a car-following task, where increased lane weaving was reported for both types of cannabis. The authors conclude that adverse effects specific to cognitive and driving performance were similar for THC-dominant cannabis and THC/CBD equivalent cannabis and, in some cases, CBD may worsen THC-induced impairment. Another placebo-controlled randomized trial reported enhanced verbal episodic memory performance among those administered cannabidiol as compared to the placebo, while also indicating that CBD may not impact attention or working memory performance negatively as no significant effects were found for those outcomes [159]. Health effects associated with cannabis vaping among youth and young adults are summarized in Table 2.
Table 2.
Health effects, risk factors and reasons associated with cannabis vaping among youth and young adults
|
Health effects of cannabis vaping: • Symptoms (bronchiolitis, bronchitis, wheezing, nontuberculous mycobacteria infection) • Respiratory gastrointestinal symptoms • Constitutional symptoms (cough, difficulty breathing, nausea, diarrhea, fever, chills, and/or weight loss) • Oral health issues (dental caries, erosions, ulcerations) • Myocardial ischemia • Mental health (psychosis, mania, catatonia) • Pain relief • Impaired cognitive performance |
|
Risk factors or correlates of cannabis vaping: • Male sex • Older age (older youth or young adults relative to older adults) • Hispanic and Black race/ethnicity compared to White • Greater socio-economic status, greater parental education level • E-cigarette use with nicotine or flavors • E-cigarette use for reason trendy/cool • E-cigarette marketing exposure • Low disapproval of nicotine vaping • Other cannabis use (spliffs, blunts, pipes, bidis) • Medical cannabis use • Vaping cannabis in a vehicle • Obtaining cannabis from dispensaries or recreational retailers versus friend and family • Susceptibility to cannabis use • Low disapproval of smoking cannabis regularly • Other tobacco use (cigarette, cigars, hookah, smokeless tobacco) • Alcohol use or binge drinking • Non-medical use of prescription stimulant use or prescription opioids • Other illicit drug use • Easy access to e-cigarettes and cannabis • Lower perceived addictiveness of e-cigarettes • Lower perceived risk of cannabis use • Living with peers, parents, siblings who use cannabis • Endorsement by peers • Presence in social network • School-related factors (urban or suburban, low grade point average, skipped class, delinquent behavior) • Sensation seeking • Presence among social networks • Greater impulsivity and inattention (ADHD impulsivity) • Negative/positive urgency • Lack of perseverance • Openness to new experiences • Psychiatric symptoms (conduct problems, depressive symptoms, anhedonia, psychotic experiences) • Canadian immigration status Reasons for cannabis vaping: • To get high • Safer than smoking, combustion • Healthier than smoking • Less discomfort/irritation compared with smoking • Reduce or quit cigarette smoking, other combustible tobacco, or cannabis • Control dosage • Maintain sustained high • Experimentation • Mixing with flavors • Friend use • Looks trendy/cool • Enjoyment • Stress relief • Relaxation • Sleep improvement • Mood improvement • Efficient • Discreetness • Convenience • Circumvent smoking bans • Cheaper than smoked cannabis • Easily concealed |
Etiology
This review identified 48 studies that reported on the etiology of cannabis vaping [3, 21, 24, 28, 29, 31, 33, 43, 47, 50, 64, 163–196, 197•, 198–200]; most of these studies were cross-sectional ones (Table 1). The most commonly studied correlates were biological sex; age or grade level; race/ethnicity; socio-economic status (SES); other tobacco use, including nicotine vaping (i.e., e-cigarette use); and other modes of cannabis use (e.g., smoking). Consistent findings are summarized here. Across studies, cannabis vaping was more common among males than females [21, 24, 28, 29, 47, 170, 173, 178, 179, 182, 185, 198, 200], and among older youth (e.g., high school compared to middle school students) in most studies [21, 29, 47, 163, 167, 198], and among young adults compared to older adults [31, 50]. Cannabis vaping was also more common among Hispanic youth compared with non-Hispanic White [28, 163, 167, 190] or Black [21, 28, 167, 190, 198] youth. Some studies showed that Black youths were more likely to vape cannabis relative to White youth [64, 163], while other studies showed the reverse [21, 24, 198, 200]. Studies showed greater socio-economic status (SES) may be a risk factor for cannabis vaping [24, 47, 64, 170, 182]. E-cigarette use with nicotine only or flavors [28, 29, 163, 166, 172–174, 180, 186, 197•, 198, 200], as well as use of cigarettes, cigars, hookah, and smokeless tobacco [21, 28, 29, 50, 163, 166, 174, 178, 179, 186, 195, 197•, 199] is associated with greater odds of cannabis vaping. Former cannabis use, susceptibility to use cannabis, and peer use of cannabis, via vaping and other forms of cannabis consumption (e.g., ingesting, smoking), have also been shown to be related to greater odds of cannabis vaping [21, 169, 170, 173, 175, 179, 180, 184, 200]. Greater access to both e-cigarettes [33, 167, 197•] and cannabis [167]; and parent, sibling, and peer cannabis vaping [28, 64, 166, 180, 197•] are associated with cannabis vaping.
Other less studied correlates of cannabis vaping included alcohol use [170, 174, 197•, 198, 200], non-medical prescription use [174], and illicit drug use [170, 188]; greater impulsivity [174, 179] and attention-related factors (e.g., inattention, perseverance) [174]; openness to new experiences [182] and sensation seeking [170, 189]; psychiatric symptoms (e.g., depressive symptoms, conduct problems) [174, 182]; delinquent behavior [196]; low grade point average and skipping class [167]; internalizing and externalizing problems [197•, 198]; more exposure to e-cigarette marketing (see “Marketing” section, below) [179]; school urbanicity (urban and suburban being greater risk versus rural) [24, 198]; using cannabis in a vehicle [170]; obtaining cannabis from dispensaries or recreational retailers versus from friends and family [171]; low disapproval of nicotine vaping [167] and of smoking cannabis regularly, [182] lower perceived risk of cannabis use [167]; lower perceived addictiveness of e-cigarettes [163]; and earlier age of initiation of cannabis use, in any form [170, 200].
Seven studies reported on youth and young adults’ reasons for cannabis vaping [50, 178, 181–183, 187, 193]. Reasons included that vaping cannabis is safer, healthier, and/or less physically irritating than cigarettes or combustible tobacco; to reduce or quit smoking cigarettes or other combustible tobacco products, as well as cannabis; to control dosage or amount of cannabis consumed and/or to maintain a sustained high; experimentation; mixing with flavors; friends’ use; because cannabis vaping is “trendy” and “cool”; because it is enjoyable; stress relief; relaxation; sleep improvement; mood improvement; and its discreetness or ability to circumvent smoking bans. One study reported a reason that may deter young adults from cannabis vaping, namely that vaping may be less safe than other forms of consuming cannabis [181].
Four studies reported on youth and young adults’ harm perceptions of cannabis vaping [176, 177, 181, 191]. One study reported that young adults perceived combustible (e.g., smoked, via a joint or pipe) cannabis as more harmful than vaporized cannabis; however, chemicals (e.g., butane) used make cannabis concentrates were thought to be a source of harm [181]. Another study reported that most participants perceived using e-cigarettes to vape cannabis to be just as harmful or more harmful than joint use. Studies also reported uncertainty about the safety and harms of cannabis vaping compared to other forms of use [177, 191]. One study reported that youth and young adult cannabis vapers had lower odds of perceiving harm from daily cannabis use in any form, when compared to never cannabis users [176]. Risk factors and reasons for use associated with cannabis vaping among youth and young adults are summarized in Table 2.
Marketing
A growing body of literature shows e-cigarette marketing is prevalent, largely unregulated, and is an important risk factor for e-cigarette use among youth and young adults, especially [201]. This review identified 11 studies that examined marketing and/or other types of messaging about using e-cigarettes and the relation to vaping cannabis-related substances. These studies primarily focused on digital media (i.e., internet and social media), which is highly utilized by e-cigarette manufacturers and other promoters due to lax regulations, low cost, and access to vast and diverse young audiences.
Most studies (n = 10) were descriptive content analyses of messaging about vaping cannabis on varied digital media platforms including e-liquid vendor online sites [202], the Google Play Store [203], YouTube [204, 205], Instagram [206–209], and Twitter [210, 211]. Together, these studies showed that content was primarily promotional, with very little prevention, cessation, or health messaging. In 2020, in an effort to combat COVID-19, South Africa restricted tobacco and e-cigarette product sales over a 5-month period. Studying this, Agaku et al. showed that among 2661 e-liquids marketed by online vendors, about 29% were cannabidiol (CBD) liquids, primarily fruit and tobacco-flavored [202]. During the restriction period, online vendors commonly promoted CBD liquids instead of nicotine-containing e-liquid, salts, and concentrates [202]. Meacham et al. identified 79 Google Play Store applications that were related to vaping, three of which were specific to cannabis vaping, with the remaining specific to nicotine or unspecified [203]. Applications were commonly categorized as “tools and lifestyle,” “health and fitness,” and “social” and included do-it-yourself content for creating e-liquids and coils, games, social networking, purchasing e-cigarette products, smoking cessation services, pairing with e-cigarettes to adjust dosage and temperature, and e-cigarette cessation [203]. Yang et al. identified 214 YouTube videos over a 1-year period in 2014–2015 related to cannabis vaping [204]. Most videos were generated and shared by lay persons and included personal experiences and tips, instructions, and product reviews related to cannabis vaping — although 21% of videos were clearly marketing a specific brand or product [204]. Over a 4-month period in 2018, Ramamurthi et al. identified 18,200 “stealth vaping” YouTube videos that touted numerous discreetly designed e-cigarettes like JUUL’s USB-like device, to enable discreet vaping of nicotine and cannabis, especially by youth [205]. E-cigarettes in these videos resembled pens, smart phones and other electronics, and even asthma inhalers [205]. Over a 2-week period in 2014, Cavazos-Rehg et al. identified over 400,000 Instagram posts with cannabis-related hashtags [206]. Of a random sample of 5000 of these posts, 2136 were explicitly about cannabis (generally) [206]. About 9% (187/2136) of cannabis-related posts were advertisements, many of which (43%; 80/187) promoted devices or tools to use cannabis including advertising vape pens to use cannabis (13%; 10/80) [206]. Majmundar et al. identified 1775 Instagram posts with the hashtag #kandypens posted over a 1-month period in 2018, and about 32% of these posts referenced using cannabis-related solutions in Kandy Pens [207]. These posts were made and distributed by laypersons, vendors, KandyPen’s official Instagram account, vaping advocates or enthusiasts, and influencers [207]. Czaplicki et al. identified over 50,000 JUUL-related Instagram posts over 2 ½ months in 2018, prior to JUUL Lab’s voluntary actions limiting their own youth-oriented Instagram content in May 2018, and over 6 months following these self-imposed restrictions in 2018 [208]. Cannabis-content in JUUL-related posts was identified as a common theme, and one that grew in prominence over time in 2018 [208]. Kostygina et al. identified cannabis vaping themes in JUUL-related Instagram posts over 2 ½ months in 2018. Cross-promotion of JUUL with cannabis products was a prominent theme in commercial posts, and youth use of JUUL with marijuana was a prominent theme in organic, non-commercial posts [209]. Two studies of e-cigarette-related tweets posted in 2019 identified cannabis vaping as a prominent theme, for example, cannabis vaping was discussed on Twitter as “the real problem” causing the EVALI outbreak [210, 211].
Only one study reported statistically significant longitudinal associations between marketing via numerous channels including digital media and cannabis vaping [179]. Kreitzberg et al. reported increased odds of using e-cigarette products with cannabis 1-year later among 3720 college students who self-reported increased exposure to e-cigarette advertising via eight channels: gas/convenience stores, drug stores, grocery stores; liquor stores; bars or clubs; music events; radio or internet radio; online; magazines or newspapers; and billboards [179].
Regulation
As of May 2021, a total of 36 states and 4 US territories allow for medical use of cannabis products and 18 states, 2 US territories, and the District of Columbia have legalized adult-use (recreational) cannabis [212]. Of note, two states (South Dakota and Mississippi) passed ballot initiatives by popular vote to legalize cannabis use (medical and adult-use in South Dakota; medical-only in Mississippi) in 2020; however, these ballot initiatives were overturned by the State Supreme Court in each state [212]. Most states set no legal age restrictions for medical cannabis, though all require a prescription from a credentialed medical professional and for minors to use under the supervision of their guardian. Legal age for purchase of adult-use cannabis is 21 years of age in all legalized states, territories, and the District of Columbia [212].
Several articles explored cannabis vaping prevalence among youth and young adults by state-level cannabis regulatory policy [213•, 214–219]. Across the USA, studies show the prevalence of any form of cannabis consumption among young people, including for cannabis vaping, is consistently higher in legalized states, relative to prohibition states [213•, 220, 221]. One study also showed that among youth who had ever used cannabis, those living in a legalized state initiated cannabis vaping at a slightly earlier age than those in prohibition states (mean age = 15.3 vs. 15.4 years; p < 0.01) [42]. Another study showed that cannabis vaping (and other forms of cannabis consumption) was more prevalent among young adults compared to older adults in states where recreational cannabis use is legal [62]. Canada legalized recreational marijuana use for adults in 2018. One study reinforced that legalization does not appear to strengthen barriers to obtaining cannabis for underage youth [55]. Increases in multimodal use of cannabis (e.g., smoking, vaping, and/or ingesting) among underage youth were observed after legislation was passed [54, 56].
Readers are referred to a summary [35] that describes the regulatory and marketing environment related to legalization of adult-use cannabis in 11 legalized states. This paper noted that regulatory approaches vary substantially but most states set standards on (1) quantity; (2) eligibility for purchase; (3) transportation; (4) retail setting; and (5) how cannabis can be grown, packaged, sold, distributed, and promoted. Regulatory approaches include rules and guidelines for cannabis vaping products, including establishing quantity limits for THC concentrates as well as requiring labels to state the same and whether concentrates have been tested for contaminants. Strong enforcement efforts are necessary, as studies report that many underage youth and young adults successfully purchase their devices online or from vape shops [222].
Discussion
From 2013 forward, consistent with increases in cannabis vaping among young people [2•], the available research literature on this topic has grown exponentially. We hope this review provides a timely summary of the state-of-the-knowledge, in ways that inform development of preventive interventions and provides direction for future studies. Clearly, surveillance of cannabis vaping among young people should continue. It would be beneficial for efforts to continue to collect information that informs comparisons by substance (e.g., THC, CBD vs. nicotine) and method (e.g., vaping vs. smoking) of use, so that other streams of research (e.g., on health effects) can anchor appropriately into this information. Although reports of EVALI have declined over time, a body of literature is starting to emerge regarding the other health effects of cannabis vaping. To date, little research has examined its impact on gastrointestinal issues, despite a larger body of evidence on the same for cannabis smoking [65, 141–153]. More studies of the impact of cannabis vaping on cognition, affect, and behavior will also be useful, given limited research to date. Preventive interventions can benefit from the information summarized here, which highlights important target audiences that can benefit given their higher prevalence of use (e.g., older youth, young adults; Hispanic youth) and risk factors (e.g., reasons for use, risk perceptions) that could be relevant to the development of program or communication campaign content.
Overall, there is a dearth of research on marketing of and/or other types of messaging about cannabis vaping. More research is needed to describe the various channels through which cannabis vaping is promoted especially via the ever-expanding world of digital media, as well as the content and source of messages about cannabis vaping. Although Apple, Facebook, and many popular, digital media companies have self-imposed policies against tobacco, e-cigarette, cannabis, and other drug use, some studies have shown these are lacking in preventing youth and young adults’ exposure to tobacco and other substance use-related content via these media [223]. Additionally, there are no federal restrictions on digital marketing to curb commercial e-cigarette marketing, at least. The nine studies identified in this review suggest e-cigarette — and particularly cannabis vaping — marketing and other promotional messaging appear to be critical factors contributing to the explosion of cannabis vaping among youth and young adults.
Conclusions
As the regulatory environment for cannabis products continues to open up not only across many states in the USA but also in other countries like Uruguay, Canada, Mexico, and South Africa, the need for research and intervention specific to youth and young adults will become increasingly relevant. The research to-date clearly shows that cannabis vaping among young people is consistently higher in settings where use is legal for those over the age of 21 years. Therefore, additional methods for preventive interventions will be necessary in the future, and development of these must be informed by etiologic research. Already, as evidenced by EVALI, the large majority of the negative impact of cannabis vaping on health has been disproportionately experienced by young people. They will continue to require support from the scientific community in the future, in order to mitigate any additional damage to their well-being, collectively, that lies ahead.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
Research reported in this paper was supported by grant number [R01-CA239097] from the National Cancer Institute and by the Career Development Program — National Cancer Institute/NIH Grant — National Cancer Institute/NIH Grant T32/CA057712 (author: DSM). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Declarations
Conflict of Interest
Dr. Harrell reports grants from NIH/NCI, during the conduct of the study; personal fees from XX is a consultant in litigation involving the vaping industry, outside the submitted work. Dr. Clendennen reports grants from NIH/NCI, during the conduct of the study; personal fees from XX is a consultant in litigation involving the vaping industry, outside the submitted work. Sumbe A. reports grants from NIH/NCI, during the conduct of the study. Dr. Case has nothing to disclose. Dr. Mantey reports grants from NIH/NCI, during the conduct of the study; personal fees from XX is a consultant in litigation involving the vaping industry, outside the submitted work. Swan. S reports grants from NIH/NCI, during the conduct of the study.
Human and Animal Rights and Informed Consent
This article does not contain any studies with human or animal subjects performed by any of the authors.
Footnotes
This article is part of the Topical Collection on Tobacco Addiction
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Papers of particular interest, published recently, have been highlighted as: • Of importance
- 1.Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J. 2009;26(2):91–108. doi: 10.1111/j.1471-1842.2009.00848.x. [DOI] [PubMed] [Google Scholar]
- 2.•.Lim CC, Sun T, Leung J, Chung JY, Gartner C, Connor J et al. Prevalence of adolescent cannabis vaping: a systematic review and meta-analysis of US and Canadian studies. JAMA pediatrics. 2021. Lim et al. (2021) is another recent, relevant systematic review of the epidemiology of cannabis vaping. [DOI] [PMC free article] [PubMed]
- 3.U.S. Department of Health and Human Services. E-cigarette use among youth and young adults. A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2016.
- 4.Schulenberg JE, Patrick ME, Johnston LD, O’Malley PM, Bachman JG, Miech RA. Monitoring the future national survey results on drug use, 1975–2020: Volume II, college students and adults ages 19–60. Ann Arbor: Institute for Social Research, The University of Michigan. 2021. Available at http://monitoringthefuture.org/pubs.html#monographs.
- 5.Gentzke AS, Creamer M, Cullen KA, Ambrose BK, Willis G, Jamal A, et al. Vital signs: tobacco product use among middle and high school students—United States, 2011–2018. Morb Mortal Weekly Rep. 2019;68(6):157. doi: 10.15585/mmwr.mm6806e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tricco AC, Lillie E, Zarin W, O'Brien KK, Colquhoun H, Levac D, et al. PRISMA extension for scoping reviews (PRISMA-ScR): checklist and explanation. Ann Intern Med. 2018;169(7):467–473. doi: 10.7326/M18-0850. [DOI] [PubMed] [Google Scholar]
- 7.Chadi N, Schroeder R, Jensen JW, Levy S. Association between electronic cigarette use and marijuana use among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2019;173(10):e192574-e. doi: 10.1001/jamapediatrics.2019.2574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Soneji S, Barrington-Trimis JL, Wills TA, Leventhal AM, Unger JB, Gibson LA, et al. Association between initial use of e-cigarettes and subsequent cigarette smoking among adolescents and young adults: a systematic review and meta-analysis. JAMA Pediatr. 2017;171(8):788–797. doi: 10.1001/jamapediatrics.2017.1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Khouja JN, Suddell SF, Peters SE, Taylor AE, Munafò MR. Is e-cigarette use in non-smoking young adults associated with later smoking? A systematic review and meta-analysis. Tob Control. 2021;30(1):8–15. doi: 10.1136/tobaccocontrol-2019-055433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Glasser AM, Cobb CO, Teplitskaya L, Ganz O, Katz L, Rose SW, et al. Electronic nicotine delivery devices, and their impact on health and patterns of tobacco use: a systematic review protocol. BMJ open. 2015;5(4):e007688. doi: 10.1136/bmjopen-2015-007688. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Glasser AM, Collins L, Pearson JL, Abudayyeh H, Niaura RS, Abrams DB, et al. Overview of electronic nicotine delivery systems: a systematic review. Am J Prev Med. 2017;52(2):e33–e66. doi: 10.1016/j.amepre.2016.10.036. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.National Academies of Sciences, Engineering, and Medicine . Public Health Consequences of E-Cigarettes. Washington, DC: The National Academies Press; 2018. [PubMed] [Google Scholar]
- 13.National Academies of Sciences, Engineering, and Medicine . The health effects of cannabis and cannabinoids: the current state of evidence and recommendations for research. Washington, DC: The National Academies Press; 2017. [PubMed] [Google Scholar]
- 14.Bhatnagar A, Whitsel LP, Ribisl KM, Bullen C, Chaloupka F, Piano MR, et al. Electronic cigarettes: a policy statement from the American Heart Association. Circulation. 2014;130(16):1418–1436. doi: 10.1161/CIR.0000000000000107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Covidence [computer software]. Retrieved from https://www.covidence.org/.
- 16.Miech RA, Patrick ME, O'Malley PM, Johnston LD, Bachman JG. Trends in reported marijuana vaping among US adolescents, 2017–2019. JAMA. 2020;323(5):475–476. doi: 10.1001/jama.2019.20185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Palamar JJ. Increases in frequent vaping of cannabis among high school seniors in the United States, 2018–2019. J Adolesc Health. 2021;69(1):153–156. doi: 10.1016/j.jadohealth.2021.03.034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Palamar JJ, Le A. Discordant reporting of vaping of cannabis among high school seniors in the United States. Am J Drug Alcohol Abuse. 2021:1–10. [DOI] [PMC free article] [PubMed]
- 19.Watkins SL, Karliner-Li P, Lee YO, Koester KA, Ling PM. A mixed-methods study to inform the clarity and accuracy of cannabis-use and cannabis-tobacco co-use survey measures. Drug Alcohol Depend. 2021;224:108697. doi: 10.1016/j.drugalcdep.2021.108697. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Miech R, Johnston LD, O’Malley PM, Terry-McElrath YM. The national prevalence of adolescent nicotine use in 2017: estimates taking into account student reports of substances vaped. Addict Behav Rep. 2019;9:100159. doi: 10.1016/j.abrep.2019.100159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Dai H, Siahpush M. Use of e-cigarettes for nicotine, marijuana, and just flavoring among U.S. youth. Am J Prev Med. 2020;58(2):244–9. doi: 10.1016/j.amepre.2019.09.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Monitoring The Future. National Institute on Drug Abuse. Table 5 trends in lifetime prevalence of use of various drugs for grades 8,10, and 12 combined. Available from http://monitoringthefuture.org/data/20data/table5.pdf.
- 23.Monitoring The Future. National Institute on Drug Abuse. Table 7 trends in 30-day prevalence of use of various drugs for grades 8, 10, and 12 combined. Available from http://monitoringthefuture.org/data/20data/table7.pdf.
- 24.Patrick ME, Miech RA, Kloska DD, Wagner AC, Johnston LD. Trends in marijuana vaping and edible consumption from 2015 to 2018 among adolescents in the US. JAMA Pediatr. 2020;174(9):900–902. doi: 10.1001/jamapediatrics.2020.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Tai H, Swartz MD, Marsden D, Perry CL. The future of substance abuse now: relationships among adolescent use of vaping devices, marijuana, and synthetic cannabinoids. Subst Use Misuse. 2021;56(2):192–204. doi: 10.1080/10826084.2020.1849305. [DOI] [PubMed] [Google Scholar]
- 26.Romm KF, West CD, Berg CJ. Mode of marijuana use among young adults: perceptions, use profiles, and future use. Subst Use Misuse. 2021;56(12):1765–1775. doi: 10.1080/10826084.2021.1949724. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Farsalinos K, Barbouni A, Niaura R. Changes from 2017 to 2018 in e-cigarette use and in ever marijuana use with e-cigarettes among US adolescents: analysis of the National Youth Tobacco Survey. Addiction. 2021;116(1):139–149. doi: 10.1111/add.15162. [DOI] [PubMed] [Google Scholar]
- 28.Trivers KF, Phillips E, Gentzke AS, Tynan MA, Neff LJ. Prevalence of cannabis use in electronic cigarettes among US youth. JAMA Pediatr. 2018;172(11):1097–1099. doi: 10.1001/jamapediatrics.2018.1920. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Dai H. Self-reported marijuana use in electronic cigarettes among US youth, 2017 to 2018. JAMA. 2020;323(5):473–474. doi: 10.1001/jama.2019.19571. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Schauer GL, Njai R, Grant-Lenzy AM. Modes of marijuana use - smoking, vaping, eating, and dabbing: results from the 2016 BRFSS in 12 States. Drug Alcohol Depend. 2020;209:107900. doi: 10.1016/j.drugalcdep.2020.107900. [DOI] [PubMed] [Google Scholar]
- 31.Uddin SMI, Osei AD, Obisesan OH, El-Shahawy O, Dzaye O, Cainzos-Achirica M, et al. Prevalence, trends, and distribution of nicotine and marijuana use in e-cigarettes among US adults: the behavioral risk factor surveillance system 2016–2018. Prev Med. 2020;139:106175. doi: 10.1016/j.ypmed.2020.106175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Seaman EL, Stanton CA, Edwards KC, Halenar MJ. Use of tobacco products/devices for marijuana consumption and association with substance use problems among U.S. young adults (2015–2016) Addict Behav. 2020;102:106133. doi: 10.1016/j.addbeh.2019.106133. [DOI] [PubMed] [Google Scholar]
- 33.Gaiha SM, Lempert LK, Halpern-Felsher B. Underage youth and young adult e-cigarette use and access before and during the coronavirus disease 2019 pandemic. JAMA Netw Open. 2020;3(12):e2027572. doi: 10.1001/jamanetworkopen.2020.27572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Nguyen N, Gaiha SM, Halpern-Felsher B. Self-reported changes in cannabis vaping among US adolescents and young adults early in the COVID-19 pandemic. Prev Med Rep. 2021;24:101654. doi: 10.1016/j.pmedr.2021.101654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Kelly K, Berry C, Comello MLG, Ray HB. The regulatory and marketing environment surrounding the legalization of retail marijuana and the impact on youth. J Public Policy Mark. 2021;40(1):62–82. doi: 10.1177/0743915620911632. [DOI] [Google Scholar]
- 36.Kotlaja MM, Carson JV. Cannabis prevalence and national drug policy in 27 countries: an analysis of adolescent substance use. Int J Offender Ther Comp Criminol. 2019;63(7):1082–1099. doi: 10.1177/0306624x18814184. [DOI] [PubMed] [Google Scholar]
- 37.Lenk KM, Wiens T, Fabian LEA, Erickson DJ. Practices and policies of marijuana retail stores in the first two US states to legalize recreational marijuana sales. Drugs Educ Prev Policy 9. 10.1080/09687637.2020.1822781.
- 38.Goodman S, Wadsworth E, Leos-Toro C, Hammond D. Prevalence and forms of cannabis use in legal vs. illegal recreational cannabis markets. Int J Drug Policy. 2020;76:102658. doi: 10.1016/j.drugpo.2019.102658. [DOI] [PubMed] [Google Scholar]
- 39.Shi YY. Heterogeneities in administration methods among cannabis users by use purpose and state legalization status: findings from a nationally representative survey in the United States, 2020. Addiction. 2021;116(7):1782–1793. doi: 10.1111/add.15342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Steigerwald S, Wong PO, Cohen BE, Ishida JH, Vali M, Madden E, et al. Smoking, vaping, and use of edibles and other forms of marijuana among U.S. adults. Ann Intern Med. 2018;169(12):890–2. doi: 10.7326/m18-1681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Nicksic NE, Do EK, Barnes AJ. Cannabis legalization, tobacco prevention policies, and cannabis use in e-cigarettes among youth. Drug Alcohol Depend. 2020;206:107730. doi: 10.1016/j.drugalcdep.2019.107730. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Borodovsky JT, Lee DC, Crosier BS, Gabrielli JL, Sargent JD, Budney AJUS. cannabis legalization and use of vaping and edible products among youth. Drug Alcohol Depend. 2017;177:299–306. doi: 10.1016/j.drugalcdep.2017.02.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Kolar K, Elton-Marshall T, Mann RE, Hamilton HA. Routes of cannabis administration among adolescents during criminal prohibition of cannabis in Canada. Drugs Educ Prev Policy. 2020;27(5):421–426. doi: 10.1080/09687637.2020.1715920. [DOI] [Google Scholar]
- 44.Schneider KE, Tormohlen KN, Brooks-Russell A, Johnson RM, Thrul J. Patterns of co-occurring modes of marijuana use among Colorado high school students. J Adolesc Health. 2019;64(6):807–809. doi: 10.1016/j.jadohealth.2018.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Eggers ME, Lee YO, Jackson K, Wiley JL, Porter L, Nonnemaker JM. Youth use of electronic vapor products and blunts for administering cannabis. Addict Behav. 2017;70:79–82. doi: 10.1016/j.addbeh.2017.02.020. [DOI] [PubMed] [Google Scholar]
- 46.Kowitt SD, Osman A, Meernik C, Zarkin GA, Ranney LM, Martin J, et al. Vaping cannabis among adolescents: prevalence and associations with tobacco use from a cross-sectional study in the USA. BMJ Open. 2019;9(6):e028535. doi: 10.1136/bmjopen-2018-028535. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Mammen G, Rehm J, Rueda S. Vaporizing cannabis through e-cigarettes: prevalence and socio-demographic correlates among Ontario high school students. Can J Public Health. 2016;107(3):e337–e8. doi: 10.17269/cjph.107.5747. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hakkarainen P. Vaporizing the pot world–easy, healthy, and cool. Drugs Alcohol Today. 2016.
- 49.Doggett A, Battista K, Leatherdale ST. Modes of cannabis use among Canadian youth in the COMPASS study; using LCA to examine patterns of smoking, vaping, and eating/drinking cannabis. Drugs Educ Prev Policy. 2021;28(2):156–164. doi: 10.1080/09687637.2020.1769560. [DOI] [Google Scholar]
- 50.Kastaun S, Hildebrandt J, Kotz D. Electronic cigarettes to vaporize cannabis: prevalence of use and associated factors among current electronic cigarette users in Germany (DEBRA study) Subst Use Misuse. 2020;55(7):1106–1112. doi: 10.1080/10826084.2020.1729197. [DOI] [PubMed] [Google Scholar]
- 51.Hammond D, Wadsworth E, Reid JL, Burkhalter R. Prevalence and modes of cannabis use among youth in Canada, England, and the US, 2017 to 2019. Drug Alcohol Depend. 2021;219:108505. doi: 10.1016/j.drugalcdep.2020.108505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Smith DM, Miller C, O'Connor RJ, Kozlowski LT, Wadsworth E, Fix BV et al. Modes of delivery in concurrent nicotine and cannabis use (“co-use”) among youth: findings from the International Tobacco Control (ITC) survey. Subst Abus 9. 10.1080/08897077.2019.1709603. [DOI] [PMC free article] [PubMed]
- 53.Fataar F, Hammond D. The prevalence of vaping and smoking as modes of delivery for nicotine and cannabis among youth in Canada, England and the United States. Int J Environ Res Public Health. 2019;16(21):4111. doi: 10.3390/ijerph16214111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Doggett A, Battista K, Jiang Y, de Groh M, Leatherdale ST. Patterns of cannabis use among canadian youth over time; examining changes in mode and frequency using latent transition analysis. Subst Use Misuse. 2021:1–11. [DOI] [PubMed]
- 55.Fischer B, Lee A, Robinson T, Hall W. An overview of select cannabis use and supply indicators pre-and post-legalization in Canada. Subst Abuse Treat Prev Policy. 2021;16(1):1–7. doi: 10.1186/s13011-021-00405-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Zuckermann AM, Gohari MR, Romano I, Leatherdale ST. Changes in cannabis use modes among Canadian youth across recreational cannabis legalization: data from the COMPASS prospective cohort study. Addict Behav. 2021;122:107025. doi: 10.1016/j.addbeh.2021.107025. [DOI] [PubMed] [Google Scholar]
- 57.Ball J, Zhang J, Hammond D, Boden J, Stanley J, Edwards R. The rise of cannabis vaping: implications for survey design. N Z Med J (Online) 2021;134(1540):95–98. [PubMed] [Google Scholar]
- 58.Dunbar MS, Davis JP, Tucker JS, Seelam R, Shih RA, D'Amico EJ. Developmental trajectories of tobacco/nicotine and cannabis use and patterns of product co-use in young adulthood. Tob Use Insights. 2020;13:10. doi: 10.1177/1179173x20949271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Lanza HI, Bello MS, Cho J, Barrington-Trimis JL, McConnell R, Braymiller JL, et al. Tobacco and cannabis poly-substance and poly-product use trajectories across adolescence and young adulthood. Prev Med. 2021;148:106545. doi: 10.1016/j.ypmed.2021.106545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Lanza HI, Barrington-Trimis JL, McConnell R, Cho J, Braymiller JL, Krueger EA, et al. Trajectories of nicotine and cannabis vaping and polyuse from adolescence to young adulthood. JAMA Netw Open. 2020;3(10):e2019181. doi: 10.1001/jamanetworkopen.2020.19181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Barrington-Trimis JL, Cho J, Ewusi-Boisvert E, Hasin D, Unger JB, Miech RA, et al. Risk of persistence and progression of use of 5 cannabis products after experimentation among adolescents. JAMA Netw Open. 2020;3(1):e1919792. doi: 10.1001/jamanetworkopen.2019.19792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Ueno LF, Mian MN, Altman BR, Giandelone E, Luce M, Earleywine M. Age-related differences in cannabis product use. J Psychoactive Drugs 7. 10.1080/02791072.2020.1870778. [DOI] [PubMed]
- 63.Harrell MB, Chen B, Clendennen SL, Sumbe A, Case KR, Wilkinson AV, et al. Longitudinal trajectories of e-cigarette use among adolescents: a 5-year, multiple cohort study of vaping with and without marijuana. Prev Med. 2021;150:106670. doi: 10.1016/j.ypmed.2021.106670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Young-Wolff KC, Adams SR, Sterling SA, Tan ASL, Salloum RG, Torre K, et al. Nicotine and cannabis vaping among adolescents in treatment for substance use disorders. J Subst Abuse Treat. 2021;125:108304. doi: 10.1016/j.jsat.2021.108304. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hoffenberg EJ, McWilliams SK, Mikulich-Gilbertson SK, Murphy BV, Lagueux M, Robbins K, et al. Marijuana use by adolescents and young adults with inflammatory bowel disease. J Pediatr. 2018;199:99–105. doi: 10.1016/j.jpeds.2018.03.041. [DOI] [PubMed] [Google Scholar]
- 66.Thurtle N, Abouchedid R, Archer JR, Ho J, Yamamoto T, Dargan PI, et al. Prevalence of use of electronic nicotine delivery systems (ENDS) to vape recreational drugs by club patrons in South London. J Med Toxicol. 2017;13(1):61–65. doi: 10.1007/s13181-016-0583-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Clawson AH, Ruppe NM, Nwankwo CN, Blair AL. Profiles of nicotine and cannabis exposure among young adults with asthma. Behav Med. 2020 doi: 10.1080/08964289.2020.1763904. [DOI] [PubMed] [Google Scholar]
- 68.Young-Wolff KC, Adams SR, Wi S, Weisner C, Conway A. Routes of cannabis administration among females in the year before and during pregnancy: results from a pilot project. Addict Behav. 2020;100:106125. doi: 10.1016/j.addbeh.2019.106125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Masonbrink AR, Hunt JA, Bhandal A, Randell KA, Mermelstein S, Wells S, et al. Self-reported and documented substance use among adolescents in the pediatric hospital. Pediatrics. 2021;147(6):e2020031468. doi: 10.1542/peds.2020-031468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Abeles M, Popofsky S, Wen A, Valsamis C, Webb A, Halaby C, et al. Vaping-associated lung injury caused by inhalation of cannabis oil. Pediatr Pulmonol. 2020;55(1):226–228. doi: 10.1002/ppul.24579. [DOI] [PubMed] [Google Scholar]
- 71.Aberegg SK, Maddock SD, Blagev DP, Callahan SJ. Diagnosis of EVALI: general approach and the role of bronchoscopy. Chest. 2020;158(2):820–827. doi: 10.1016/j.chest.2020.02.018. [DOI] [PubMed] [Google Scholar]
- 72.Adhikari R, Koritala T, Gotur R, Malayala SV, Jain NK. EVALI - e-cigarette or vaping product use-associated lung injury: a case report. Cureus. 2021;13(4):8. doi: 10.7759/cureus.13541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Ahmed A, Shapiro D, Su J, Nelson LP. Vaping cannabis butane hash oil leads to severe acute respiratory distress syndrome—a case of EVALI in a teenager with hypertrophic cardiomyopathy. J Intensive Care Med. 2021;36(5):617–621. doi: 10.1177/0885066620941004. [DOI] [PubMed] [Google Scholar]
- 74.Aldy K, Cao DJ, McGetrick M, Willcutts D, Verbeck G, de Silva I, et al. Severe e-cigarette, or vaping, product use associated lung injury requiring venovenous extracorporeal membrane oxygenation. Pediatr Crit Care Med. 2020;21:385–8. doi: 10.1097/PCC.0000000000002264. [DOI] [PubMed] [Google Scholar]
- 75.Amin AA, Haught E, Mousattat Y. Do not huff, puff, or vape that stuff: interstitial airspace disease in a teenager. Case Rep Pediatrics. 2020;2020:4. doi: 10.1155/2020/8822362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Espinosa SM, Harper EP, Phillips MB. 19-year-old man with fevers, abdominal pain, and cough. Mayo Clin Proc. 2020;95(10):e103–e108. doi: 10.1016/j.mayocp.2020.02.036. [DOI] [PubMed] [Google Scholar]
- 77.Fedt A, Bhattarai S, Oelstrom MJ. Vaping-associated lung injury: a new cause of acute respiratory failure. J Adolesc Health. 2020;66(6):754–757. doi: 10.1016/j.jadohealth.2020.03.019. [DOI] [PubMed] [Google Scholar]
- 78.Ghinai I, Layden JE. Inpatient notes: clinical pearls-e-cigarette, or vaping, product use-associated lung injury. Ann Intern Med. 2019;171(12):HO2–HO3. doi: 10.7326/M19-3574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Harada HA, Liu J, Shortell JD, Beesley SJ. A 20-year-old man with e-cigarette or vaping product use-associated lung injury (EVALI) and thrombotic coagulopathy. Am J Case Rep. 2021;22:e929915. doi: 10.12659/ajcr.929915. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Israel AK, Velez MJ, Staicu SA, Ambrosini R, McGraw M, Agrawal T. A unique case of secondary pulmonary alveolar proteinosis after e-cigarette, or vaping, product use-associated lung injury. Am J Respir Crit Care Med. 2020;202(6):890–893. doi: 10.1164/rccm.202002-0252LE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Kelley BP, Prakash PB. Vaping-associated lung injury: should we consider screening adolescents who vape? Clin Pediatr (Phila) 2020;59(11):1033–1035. doi: 10.1177/0009922820927039. [DOI] [PubMed] [Google Scholar]
- 82.Khiatah B, Murdoch A, Hubeny C, Constantine C, Frugoli A. Vaping-induced lung injury: brief report for the practicing clinician. Oxf Med Case Reports. 2020;2020(8):267–270. doi: 10.1093/omcr/omaa060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Kooragayalu S, El-Zarif S, Jariwala S. Vaping associated pulmonary injury (VAPI) with superimposed mycoplasma pneumoniae infection. Respir Med Case Rep. 2020;29:100997. doi: 10.1016/j.rmcr.2020.100997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Lucero A, Eriksson N, Nichta C, Sokol K. A 23-year-old man with acute lung injury after using a tetrahydrocannabinol-containing vaping device: a case report. J Med Case Rep. 2021;15(1):70. doi: 10.1186/s13256-020-02549-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.McClelland M, McClelland S. Case of a 21-year-old man with persistent lung collapse leading to a pericardectomy linked to vape use. Heart Lung. 2021;50(2):262–267. doi: 10.1016/j.hrtlng.2020.12.012. [DOI] [PubMed] [Google Scholar]
- 86.Messina MD, Levin TL, Blumfield E. Cytotoxic lesion of the splenium of the corpus callosum in a patient with EVALI. Clin Imaging. 2020;66:73–76. doi: 10.1016/j.clinimag.2020.05.009. [DOI] [PubMed] [Google Scholar]
- 87.Mull ES, Erdem G, Nicol K, Adler B, Shell R. Eosinophilic pneumonia and lymphadenopathy associated with vaping and tetrahydrocannabinol use. Pediatrics. 2020;145(4):e20193007. doi: 10.1542/peds.2019-3007. [DOI] [PubMed] [Google Scholar]
- 88.O'Carroll O, Sharma K, Fabre A, Murphy DJ, Keane MP, McCarthy C. Vaping-associated lung injury. Thorax. 2020;75(8):706–707. doi: 10.1136/thoraxjnl-2020-214762. [DOI] [PubMed] [Google Scholar]
- 89.Ocampo-Gonzalez FA, Park JW. Cytologic features of vaping-induced lung injury: a case report. Diagn Cytopathol. 2020;48(2):174–176. doi: 10.1002/dc.24343. [DOI] [PubMed] [Google Scholar]
- 90.Odish MF, Bellinghausen A, Golts E, Owens RL. E-cigarette, or vaping, product use-associated lung injury (EVALI) treated with veno-venous extracorporeal membrane oxygenation (VV-ECMO) and ultra-protective ventilator settings. BMJ Case Rep. 2020;13(7):e234771. doi: 10.1136/bcr-2020-234771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Perrenoud A, Vetos D, Wabwire G. Vaping-induced lung injury in a 21-year-old woman. BMJ Case Rep. 2020;13(11):e238671. doi: 10.1136/bcr-2020-238671. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Phung B, Lam A. Pediatric acute respiratory distress syndrome and hypersensitivity pneumonitis related to e-cigarette vaping. J Pediatr Intensive Care. 2020;9(2):128–134. doi: 10.1055/s-0039-3400961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Puebla Neira D, Tambra S, Bhasin V, Nawgiri R, Duarte AG. Discordant bilateral bronchoalveolar lavage findings in a patient with acute eosinophilic pneumonia associated with counterfeit tetrahydrocannabinol oil vaping. Respir Med Case Rep. 2020;29:101015. doi: 10.1016/j.rmcr.2020.101015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94.Rasmussen C, Balachandran Nair G, Al-Katib S. A case of vaping-associated acute lung injury. Clin Pulm Med. 2020;27(3):79–82. doi: 10.1097/CPM.0000000000000346. [DOI] [Google Scholar]
- 95.Rodriguez JA, Roa AA, Lemos-Ramirez JC. E-cigarette or vaping product use-associated lung injury (EVALI) mimicking COVID-19 disease. Case Rep Pulmonol. 2020;2020. 10.1155/2020/8821289. [DOI] [PMC free article] [PubMed]
- 96.Ronald AA, Defta D, Wright J, Rothstein B. Extensive pneumorrhachis associated with vaping-induced lung injury. World Neurosurg. 2020;140:308–311. doi: 10.1016/j.wneu.2020.05.176. [DOI] [PubMed] [Google Scholar]
- 97.Sarel E, Hoppenstein DR, Lahav M, Ifrach N, Fanadka F, Fredman BD. Respiratory failure induced by vaping-associated pulmonary injury: case report of a new entity. Isr Med Assoc J. 2021;23(1):59–60. [PubMed] [Google Scholar]
- 98.Shah J, Mullen M, Lu M. E-cigarette or vaping product use–associated lung injury: a case study and review of the literature. J Radiol Nurs. 2020;39(4):305–308. doi: 10.1016/j.jradnu.2020.09.005. [DOI] [Google Scholar]
- 99.Smith E, Cherian R, McGillen B. A case of e-cigarette, or vaping, product use–associated lung injury (EVALI) in a previously healthy patient: case report and literature review. J Gen Intern Med. 2020;35(9):2767–2770. doi: 10.1007/s11606-020-05909-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Wekon-Kemeni C, Santhanam P, Halani P, Bradford L, Loughlin CE. A gut feeling: abdominal symptoms as an initial presentation of EVALI. Pediatrics. 2021;147(1):e20193834. doi: 10.1542/PEDS.2019-3834. [DOI] [PubMed] [Google Scholar]
- 101.Wieckowska J, Assaad U, Aboudan M. Pneumothorax secondary to vaping. Respir Med Case Rep. 2021;33:101421. doi: 10.1016/j.rmcr.2021.101421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Trickett JS, Seaberg PH, editors. 21-year-old man with fever, night sweats, productive cough, and diarrhea. Mayo Clinic Proceedings; 2021: Elsevier. [DOI] [PubMed]
- 103.Artunduaga M, Rao D, Friedman J, Kwon JK, Pfeifer CM, Dettori A, et al. Pediatric chest radiographic and CT findings of electronic cigarette or vaping product use–associated lung injury (EVALI) Radiology. 2020;295(2):430–438. doi: 10.1148/radiol.2020192778. [DOI] [PubMed] [Google Scholar]
- 104.Conuel EJ, Chieng HC, Fantauzzi J, Pokhrel K, Goldman C, Smith TC, et al. Cannabinoid oil vaping-associated lung injury and its radiographic appearance. Am J Med. 2020;133(7):865–867. doi: 10.1016/j.amjmed.2019.10.032. [DOI] [PubMed] [Google Scholar]
- 105.Chidambaram AG, Dennis RA, Biko DM, Hook M, Allen J, Rapp JB. Clinical and radiological characteristics of e-cigarette or vaping product use associated lung injury. Emerg Radiol. 2020;27(5):495–501. doi: 10.1007/s10140-020-01796-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Kalininskiy A, Bach CT, Nacca NE, Ginsberg G, Marraffa J, Navarette KA, et al. E-cigarette, or vaping, product use associated lung injury (EVALI): case series and diagnostic approach. Lancet Respir Med. 2019;7(12):1017–1026. doi: 10.1016/s2213-2600(19)30415-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Kass AP, Overbeek DL, Chiel LE, Boyer EW, Casey AMH. Case series: adolescent victims of the vaping public health crisis with pulmonary complications. Pediatr Pulmonol. 2020;55(5):1224–1236. doi: 10.1002/ppul.24729. [DOI] [PubMed] [Google Scholar]
- 108.Mull ES, Shell R, Adler B, Holtzlander M. Bronchiectasis associated with electronic cigarette use: a case series. Pediatr Pulmonol. 2020;55(12):3443–3449. doi: 10.1002/ppul.25062. [DOI] [PubMed] [Google Scholar]
- 109.Wang KY, Jadhav SP, Yenduri NJS, Lee SA, Farber HJ, Guillerman RP. E-cigarette or vaping product use-associated lung injury in the pediatric population: imaging features at presentation and short-term follow-up. Pediatr Radiol. 2020;50(9):1231–1239. doi: 10.1007/s00247-020-04698-x. [DOI] [PubMed] [Google Scholar]
- 110.Reddy A, Jenssen B, Chidambaram A, Yehya N, Lindell RB. Characterizing e-cigarette vaping-associated lung injury in the pediatric intensive care unit. Pediatr Pulmonol. 2021;56(1):162–170. doi: 10.1002/ppul.25086. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Doukas SG, Kavali L, Menon RS, Izotov BN, Bukhari A. E-cigarette or vaping induced lung injury: a case series and literature review. Toxicol Rep. 2020;7:1381–1386. doi: 10.1016/j.toxrep.2020.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Fryman C, Lou B, Weber AG, Steinberg HN, Khanijo S, Iakovou A, et al. Acute respiratory failure associated with vaping. Chest. 2020;157(3):e63–e68. doi: 10.1016/j.chest.2019.10.057. [DOI] [PubMed] [Google Scholar]
- 113.Heinzerling A, Armatas C, Karmarkar E, Attfield K, Guo W, Wang Y, et al. Severe lung injury associated with use of e-cigarette, or vaping, products-California, 2019. JAMA Intern Med. 2020;180(6):861–869. doi: 10.1001/jamainternmed.2020.0664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Darmawan DO, Gwal K, Goudy BD, Jhawar S, Nandalike K. Vaping in today’s pandemic: e-cigarette, or vaping, product use–associated lung injury mimicking COVID-19 in teenagers presenting with respiratory distress. SAGE Open Med Case Rep. 2020;8:2050313X20969590. doi: 10.1177/2050313X20969590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Thakrar PD, Boyd KP, Swanson CP, Wideburg E, Kumbhar SS. E-cigarette, or vaping, product use-associated lung injury in adolescents: a review of imaging features. Pediatr Radiol. 2020;50(3):338–344. doi: 10.1007/s00247-019-04572-5. [DOI] [PubMed] [Google Scholar]
- 116.Rao DR, Maple KL, Dettori A, Afolabi F, Francis JKR, Artunduaga M, et al. Clinical features of e-cigarette, or vaping, product use–associated lung injury in teenagers. Pediatrics. 2020;146(1):e20194104. doi: 10.1542/peds.2019-4104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Pray IW, Atti SK, Tomasallo C, Meiman JG. E-cigarette, or vaping, product use-associated lung injury among clusters of patients reporting shared product use – Wisconsin, 2019. MMWR Morb Mortal Wkly Rep. 2020;69(9):236–40. doi: 10.15585/mmwr.mm6909a4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Ghinai I, Pray IW, Navon L, O'Laughlin K, Saathoff-Huber L, Hoots B, et al. E-cigarette product use, or vaping, among persons with associated lung injury - Illinois and Wisconsin, April-September 2019. MMWR Morb Mortal Wkly Rep. 2019;68(39):865–9. doi: 10.15585/mmwr.mm6839e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Silverman AL, Siddique H, Kumar V, Le TH, Ng J. Vaping induced pneumonitis: a small community hospital’s case series and analysis. BMC Pulm Med. 2020;20(1):118. doi: 10.1186/s12890-020-1158-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.MacMurdo M, Lin C, Saeedan MB, Doxtader EE, Mukhopadhyay S, Arrossi V, et al. e-Cigarette or vaping product use-associated lung injury: clinical, radiologic, and pathologic findings of 15 cases. Chest. 2020;157(6):e181–e187. doi: 10.1016/j.chest.2020.01.030. [DOI] [PubMed] [Google Scholar]
- 121.Layden JE, Ghinai I, Pray I, Kimball A, Layer M, Tenforde MW, et al. Pulmonary illness related to e-cigarette use in Illinois and Wisconsin - final report. N Engl J Med. 2020;382(10):903–916. doi: 10.1056/NEJMoa1911614. [DOI] [PubMed] [Google Scholar]
- 122.Lewis N, McCaffrey K, Sage K, Cheng CJ, Green J, Goldstein L, et al. E-cigarette use, or vaping, practices and characteristics among persons with associated lung injury – Utah, April-October 2019. MMWR Morb Mortal Wkly Rep. 2019;68(42):953–6. doi: 10.15585/mmwr.mm6842e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Corcoran A, Carl JC, Rezaee F. The importance of anti-vaping vigilance-EVALI in seven adolescent pediatric patients in Northeast Ohio. Pediatr Pulmonol. 2020;55(7):1719–1724. doi: 10.1002/ppul.24872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hilton R, Summer R, Roman J, Sundaram B, George G. E-cigarettes and vaping associated lung injury: a case series and brief review. Am J Med Sci. 2020;359(3):137–139. doi: 10.1016/j.amjms.2020.01.003. [DOI] [PubMed] [Google Scholar]
- 125.Gaub KL, Hallyburton S, Samanic C, Paddack D, Clark CR, Pence S, et al. Patient characteristics and product use behaviors among persons with e-cigarette, or vaping, product use-associated lung injury - Indiana, June - October 2019. MMWR Morb Mortal Wkly Rep. 2019;68(49):1139–41. doi: 10.15585/mmwr.mm6849a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Taylor J, Wiens T, Peterson J, Saravia S, Lunda M, Hanson K, et al. Characteristics of e-cigarette, or vaping, products used by patients with associated lung injury and products seized by law enforcement – Minnesota, 2018 and 2019. MMWR Morb Mortal Wkly Rep. 2019;68(47):1096–100. doi: 10.15585/mmwr.mm6847e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 127.Kligerman SJ, Kay FU, Raptis CA, Henry TS, Sechrist JW, Walker CM, et al. CT findings and patterns of e-cigarette or vaping product use-associated lung injury: a multicenter cohort of 160 cases. Chest. 2021;160(4):1492–1511. doi: 10.1016/j.chest.2021.04.054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Pitlick MM, Lang DK, Meehan AM, McCoy CP. EVALI: a mimicker of COVID-19. Mayo Clin Proc: Innov Qual Outcomes. 2021;5(3):682–687. doi: 10.1016/j.mayocpiqo.2021.03.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.•.Adkins SH, Anderson KN, Goodman AB, Twentyman E, Danielson ML, Kimball A, et al. Demographics, substance use behaviors, and clinical characteristics of adolescents with e-cigarette, or vaping, product use-associated lung injury (EVALI) in the United States in 2019. JAMA Pediatr. 2020;174(7):e200756. doi: 10.1001/jamapediatrics.2020.0756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Blount BC, Karwowski MP, Shields PG, Morel-Espinosa M, Valentin-Blasini L, Gardner M, et al. Vitamin E acetate in bronchoalveolar-lavage fluid associated with EVALI. N Engl J Med. 2020;382(8):697–705. doi: 10.1056/NEJMoa1916433. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 131.Ellington S, Salvatore PP, Ko J, Danielson M, Kim L, Cyrus A, et al. Update: product, substance-use, and demographic characteristics of hospitalized patients in a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury - United States, August 2019-January 2020. MMWR Morb Mortal Wkly Rep. 2020;69(2):44–9. doi: 10.15585/mmwr.mm6902e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Krishnasamy VP, Hallowell BD, Ko JY, Board A, Hartnett KP, Salvatore PP, et al. Update: characteristics of a nationwide outbreak of e-cigarette, or vaping, product use-associated lung injury - United States, August 2019-January 2020. MMWR Morb Mortal Wkly Rep. 2020;69(3):90–4. doi: 10.15585/mmwr.mm6903e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Moritz ED, Zapata LB, Lekiachvili A, Glidden E, Annor FB, Werner AK, et al. Update: characteristics of patients in a national outbreak of e-cigarette, or vaping, product use-associated lung injuries - United States, October 2019. MMWR Morb Mortal Wkly Rep. 2019;68(43):985–9. doi: 10.15585/mmwr.mm6843e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Navon L, Jones CM, Ghinai I, King BA, Briss PA, Hacker KA, et al. Risk factors for e-cigarette, or vaping, product use-associated lung injury (EVALI) among adults who use e-cigarette, or vaping, products – Illinois, July-October 2019. MMWR Morb Mortal Wkly Rep. 2019;68(45):1034–9. doi: 10.15585/mmwr.mm6845e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Perrine CG, Pickens CM, Boehmer TK, King BA, Jones CM, DeSisto CL, et al. Characteristics of a multistate outbreak of lung injury associated with e-cigarette use, or vaping - United States, 2019. MMWR Morb Mortal Wkly Rep. 2019;68(39):860–4. doi: 10.15585/mmwr.mm6839e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Werner AK, Koumans EH, Chatham-Stephens K, Salvatore PP, Armatas C, Byers P, et al. Hospitalizations and deaths associated with EVALI. N Engl J Med. 2020;382(17):1589–1598. doi: 10.1056/NEJMoa1915314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Blagev DP, Harris D, Dunn AC, Guidry DW, Grissom CK, Lanspa MJ. Clinical presentation, treatment, and short-term outcomes of lung injury associated with e-cigarettes or vaping: a prospective observational cohort study. Lancet. 2019;394(10214):2073–2083. doi: 10.1016/s0140-6736(19)32679-0. [DOI] [PubMed] [Google Scholar]
- 138.Algiers O, Wang Y, Laestadius L. Content analysis of US newspaper coverage of causes and solutions to vaping-associated lung injury. Subst Use Misuse. 2021;56(4):522–528. doi: 10.1080/10826084.2021.1883663. [DOI] [PubMed] [Google Scholar]
- 139.Kupelian C, Kim A, Vijayan V. E-cigarette or vaping product use-associated lung injury complicated by pulmonary aspergillosis. Cureus. 2021;13(12):e20075. doi: 10.7759/cureus.20075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Centers for Disease Control and Prevention. Outbreak of lung injury associated with the use of e-cigarette, or vaping, products. . https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. Accessed 4 Nov 2021.
- 141.Spindle TR, Cone EJ, Schlienz NJ, Mitchell JM, Bigelow GE, Flegel R, et al. Acute effects of smoked and vaporized cannabis in healthy adults who infrequently use cannabis: a crossover trial. JAMA Netw Open. 2018;1(7):e184841. doi: 10.1001/jamanetworkopen.2018.4841. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142.Wilsey B, Marcotte T, Deutsch R, Gouaux B, Sakai S, Donaghe H. Low-dose vaporized cannabis significantly improves neuropathic pain. J Pain. 2013;14(2):136–148. doi: 10.1016/j.jpain.2012.10.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Arkell TR, Lintzeris N, Kevin RC, Ramaekers JG, Vandrey R, Irwin C, et al. Cannabidiol (CBD) content in vaporized cannabis does not prevent tetrahydrocannabinol (THC)-induced impairment of driving and cognition. Psychopharmacology. 2019;236(9):2713–2724. doi: 10.1007/s00213-019-05246-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Boisvert EE, Bae D, Pang RD, Davis JP, Kelley-Quon LI, Barrington-Trimis JL, et al. Subjective effects of combustible, vaporized, and edible cannabis: results from a survey of adolescent cannabis users. Drug Alcohol Depend. 2020;206:6. doi: 10.1016/j.drugalcdep.2019.107716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Tucker JS, Pedersen ER, Seelam R, Dunbar MS, Shih RA, D'Amico EJ. Types of cannabis and tobacco/nicotine co-use and associated outcomes in young adulthood. Psychol Addict Behav. 2019;33(4):401–411. doi: 10.1037/adb0000464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Braymiller JL, Barrington-Trimis JL, Leventhal AM, Islam T, Kechter A, Krueger EA, et al. Assessment of nicotine and cannabis vaping and respiratory symptoms in young adults. JAMA Netw Open. 2020;3(12):e2030189. doi: 10.1001/jamanetworkopen.2020.30189. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Irusa KF, Vence B, Donovan T. Potential oral health effects of e-cigarettes and vaping: a review and case reports. J Esthet Restor Dent. 2020;32(3):260–264. doi: 10.1111/jerd.12583. [DOI] [PubMed] [Google Scholar]
- 148.Ali NS, Billings ML, Tollefson MM, Davis DMR, Hand JL. Oral erosions associated with surreptitious marijuana vaping in an adolescent boy. Pediatr Dermatol. 2020;37(2):347–349. doi: 10.1111/pde.14101. [DOI] [PubMed] [Google Scholar]
- 149.Kahan MD, Breithaupt A, Nash K, Numis AL. Seizure and interictal electroencephalographic (Eeg) changes with cannabinoid concentrate use. Am J Case Rep. 2021;22(1):e931360. doi: 10.12659/AJCR.931360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150.Mehta JJ, Mahendran AK, Bajaj RK, Doshi AR. Myocardial ischemia with cannabinoid use in an adolescent. Cureus. 2017;9(11):4. doi: 10.7759/cureus.1899. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Manning T, Bartow C, McNaughton M, Reynolds E, Chen Z. Vaping cannabis oil: a case of catatonia associated with use of high-potency cannabis. Psychosomatics. 2020;61(6):745–751. doi: 10.1016/j.psym.2020.06.012. [DOI] [PubMed] [Google Scholar]
- 152.Landman ST, Dhaliwal I, MacKenzie CA, Martinu T, Steele A, Bosma KJ. Life-threatening bronchiolitis related to electronic cigarette use in a Canadian youth. CMAJ. 2019;191(48):E1321–E1331. doi: 10.1503/cmaj.191402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 153.Chen L, Arens R, Chidambaram AG, Capponi S, Alshawa L, Claeys TA, et al. Vaping associated pulmonary nontuberculous mycobacteria. Lung. 2021;199(1):21–27. doi: 10.1007/s00408-020-00414-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Rickner SS, Cao DZ, Kleinschmidt K, Fleming S. A little “dab” will do ya’ in: a case report of neuro-and cardiotoxicity following use of cannabis concentrates. Clin Toxicol. 2017;55(9):1011–3. doi: 10.1080/15563650.2017.1334914. [DOI] [PubMed] [Google Scholar]
- 155.Antwi-Amoabeng D, Islam R. vaping is not safe: a case of acute eosinophilic pneumonia following cannabis vapor inhalation. Case Rep Pulmonol. 2020;2020:9496564. doi: 10.1155/2020/9496564. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Boyd CJ, McCabe SE, Evans-Polce RJ, Veliz PT. Cannabis, vaping, and respiratory symptoms in a probability sample of US youth. J Adolesc Health. 2021;69(1):149–152. doi: 10.1016/j.jadohealth.2021.01.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Clendennen SL, Rangwala S, Sumbe A, Case KR, Wilkinson AV, Loukas A et al. Understanding college students’ experiences using e-cigarettes and marijuana through qualitative interviews. J Am Coll Health. 2021:1–11. [DOI] [PMC free article] [PubMed]
- 158.Cloutier RM, Calhoun BH, Linden-Carmichael AN. Associations of mode of administration on cannabis consumption and subjective intoxication in daily life. Psychol Addict Behav. 2021. [DOI] [PMC free article] [PubMed]
- 159.Hotz J, Fehlmann B, Papassotiropoulos A, de Quervain DJ, Schicktanz NS. Cannabidiol enhances verbal episodic memory in healthy young participants: a randomized clinical trial. J Psychiatr Res. 2021;143:327–333. doi: 10.1016/j.jpsychires.2021.09.007. [DOI] [PubMed] [Google Scholar]
- 160.Lee MH, Cool CD, Maloney JP. Histopathological correlation of acute on chronic eosinophilic pneumonitis caused by vaporized cannabis oil inhalation. Chest. 2021;159(3):e137–e139. doi: 10.1016/j.chest.2020.10.016. [DOI] [PubMed] [Google Scholar]
- 161.Salle S, Sevestre C, Richeval C, Hakim F, Allorge D, Gaulier J-m. Involuntary 5F-ADB-related intoxication following e-cigarette use. Int J Legal Med. 2021;135(4):1467–70. doi: 10.1007/s00414-021-02561-8. [DOI] [PubMed] [Google Scholar]
- 162.Shah VD, Mohammad A, Nandkeolyar S, Stoletniy L, Contractor T. Torsades de Pointes due to excessive marijuana use in a susceptible patient. Case Rep Cardiol. 2021;2021:6621496. doi: 10.1155/2021/6621496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 163.Ben Taleb Z, Kalan ME, Bahelah R, Boateng GO, Rahman M, Alshbool FZ. Vaping while high: factors associated with vaping marijuana among youth in the United States. Drug Alcohol Depend. 2020;217:108290. doi: 10.1016/j.drugalcdep.2020.108290. [DOI] [PubMed] [Google Scholar]
- 164.Moustafa AF, Rodriguez D, Mazur A, Audrain-McGovern J. Adolescent perceptions of e-cigarette use and vaping behavior before and after the EVALI outbreak. Prev Med. 2021;145:106419. doi: 10.1016/j.ypmed.2021.106419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Wardell JD, Rueda S, Elton-Marshall T, Mann RE, Hamilton HA. Prevalence and correlates of medicinal cannabis use among adolescents. J Adolesc Health. 2021;68(1):103–109. doi: 10.1016/j.jadohealth.2020.07.032. [DOI] [PubMed] [Google Scholar]
- 166.Pokhrel P, Fagan P, Kawamoto CT, Okamoto SK, Herzog TA. Predictors of marijuana vaping onset and escalation among young adults. Drug Alcohol Depend. 2020;216:108320. doi: 10.1016/j.drugalcdep.2020.108320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Kritikos AF, Johnson JK, Hodgkin D. Past 30–day marijuana vaping: prevalence and predictors of use in a nationally representative study of U.S. youth. Am J Prev Med. 2021;60(2):258–66. doi: 10.1016/j.amepre.2020.06.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Kaur N, Rutherford CG, Martins SS, Keyes KM. Associations between digital technology and substance use among U.S. adolescents: results from the 2018 Monitoring the Future survey. Drug Alcohol Depend. 2020;213:108124. doi: 10.1016/j.drugalcdep.2020.108124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Campbell BK, Le T, Kapiteni K, Gubner NR, Guydish J. Correlates of lifetime blunt/spliff use among cigarette smokers in substance use disorders treatment. J Subst Abuse Treat. 2020;116:7. doi: 10.1016/j.jsat.2020.108064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 170.Jones CB, Meier MH, Pardini DA. Comparison of the locations where young adults smoke, vape, and eat/drink cannabis: implications for harm reduction. Addict Behav Rep. 2018;8:140–146. doi: 10.1016/j.abrep.2018.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 171.D'Amico EJ, Rodriguez A, Dunbar MS, Firth CL, Tucker JS, Seelam R, et al. Sources of cannabis among young adults and associations with cannabis-related outcomes. Int J Drug Policy. 2020;86:9. doi: 10.1016/j.drugpo.2020.102971. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Merianos AL, Jandarov RA, Klein JD, Mahabee-Gittens EM. Characteristics of daily e-cigarette use and acquisition means among a national sample of adolescents. Am J Health Promot. 2019;33(8):1115–1122. doi: 10.1177/0890117119854051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Morean ME, Kong G, Camenga DR, Cavallo DA, Krishnan-Sarin S. High school students’ use of electronic cigarettes to vaporize cannabis. Pediatrics. 2015;136(4):611–616. doi: 10.1542/peds.2015-1727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Leventhal AM, Bae D, Kechter A, Barrington-Trimis JL. Psychiatric comorbidity in adolescent use and poly-use of combustible, vaporized, and edible cannabis products. J Psychiatr Res. 2020;124:91–98. doi: 10.1016/j.jpsychires.2020.02.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Frohe T, Leeman RF, Patock-Peckham J, Ecker A, Kraus S, Foster DW. Correlates of cannabis vape-pen use and knowledge among U.S. college students. Addict Behav Rep. 2018;7:32–9. doi: 10.1016/j.abrep.2017.11.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Leos-Toro C, Fong GT, Meyer SB, Hammond D. Cannabis health knowledge and risk perceptions among Canadian youth and young adults. Harm Reduct J. 2020;17(1):54. doi: 10.1186/s12954-020-00397-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 177.Yoo SR, Dollinger C, Vali M, Steigerwald S, Cohen BE, Ishida JH, et al. Perceptions of the comparative safety of different forms of marijuana use among the adult US population. J Gen Intern Med. 2019;34(4):504–506. doi: 10.1007/s11606-018-4741-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 178.Kenne DR, Fischbein RL, Tan ASL, Banks M. The use of substances other than nicotine in electronic cigarettes among college students. Subst Abuse: Res Treat. 2017;11:1178221817733736. doi: 10.1177/1178221817733736. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 179.Kreitzberg DS, Hinds JT, Pasch KE, Loukas A, Perry CL. Exposure to ENDS advertising and use of marijuana in ENDS among college students. Addict Behav. 2019;93:9–13. doi: 10.1016/j.addbeh.2019.01.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 180.Cassidy RN, Meisel MK, DiGuiseppi G, Balestrieri S, Barnett NP. Initiation of vaporizing cannabis: individual and social network predictors in a longitudinal study of young adults. Drug Alcohol Depend. 2018;188:334–340. doi: 10.1016/j.drugalcdep.2018.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Popova L, McDonald EA, Sidhu S, Barry R, Maruyama TAR, Sheon NM, et al. Perceived harms and benefits of tobacco, marijuana, and electronic vaporizers among young adults in Colorado: implications for health education and research. Addiction. 2017;112(10):1821–1829. doi: 10.1111/add.13854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Jones CB, Hill ML, Pardini DA, Meier MH. Prevalence and correlates of vaping cannabis in a sample of young adults. Psychol Addict Behav. 2016;30(8):915–921. doi: 10.1037/adb0000217. [DOI] [PubMed] [Google Scholar]
- 183.McDonald EA, Popova L, Ling PM. Traversing the triangulum: the intersection of tobacco, legalised marijuana and electronic vaporisers in Denver, Colorado. Tob Control. 2016;25(Suppl 1):i96–i102. doi: 10.1136/tobaccocontrol-2016-053091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 184.Barrington-Trimis JL, Bae D, Schiff S, Davis J, Unger JB, Leventhal AM. Characterizing the predictive validity of measures of susceptibility to future use of combustible, vaporized and edible cannabis products in adolescent never-users. Addiction. 2020;115(12):2339–2348. doi: 10.1111/add.15078. [DOI] [PubMed] [Google Scholar]
- 185.Peters EN, Bae D, Barrington-Trimis JL, Jarvis BP, Leventhal AM. Prevalence and sociodemographic correlates of adolescent use and polyuse of combustible, vaporized, and edible cannabis products. JAMA Netw Open. 2018;1(5):12. doi: 10.1001/jamanetworkopen.2018.2765. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 186.Nguyen N, Barrington-Trimis JL, Urman R, Cho J, McConnell R, Leventhal AM, et al. Past 30-day co-use of tobacco and marijuana products among adolescents and young adults in California. Addict Behav. 2019;98:106053. doi: 10.1016/j.addbeh.2019.106053. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 187.Wheeler M, Merten JW, Gordon BT, Hamadi H. CBD (cannabidiol) product attitudes, knowledge, and use among young adults. Subst Use Misuse. 2020;55(7):1138–1145. doi: 10.1080/10826084.2020.1729201. [DOI] [PubMed] [Google Scholar]
- 188.Boccio CM, Jackson DB. Adolescent nicotine and marijuana vaping activity and the use of other illicit substances. Drug Alcohol Depend. 2021;219:108469. doi: 10.1016/j.drugalcdep.2020.108469. [DOI] [PubMed] [Google Scholar]
- 189.Hoffmann JP. Sensation seeking and adolescent e-cigarette use. J Subst Use 7. 10.1080/14659891.2020.1856209.
- 190.Watson CV, Puvanesarajah S, Trivers KF. Racial and ethnic differences in marijuana use in e-cigarettes among US youth in 2017, 2018, and 2020. JAMA Pediatr 2. 10.1001/jamapediatrics.2021.0305. [DOI] [PMC free article] [PubMed]
- 191.Sharma P, Philpot LM, Rosedahl JK, Jose T, Ebbert JO. Electronic vaping product use among young adults who receive care at a major medical institution. Subst Use Misuse. 2020;56(2):224–237. doi: 10.1080/10826084.2020.1853777. [DOI] [PubMed] [Google Scholar]
- 192.Dugas EN, Sylvestre MP, O'Loughlin J. Type of e-liquid vaped, poly-nicotine use and nicotine dependence symptoms in young adult e-cigarette users: a descriptive study. BMC Public Health. 2020;20(1):8. doi: 10.1186/s12889-020-09056-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 193.Sakuma KLK, Dolcini MM, Seifert J, Bean MM, Fagan P, Wilson M, et al. Hookah and electronic inhalant device use and perceptions among African American youth and young adults: are we asking the right questions? Health Educ Behav. 2020;47(3):391–401. doi: 10.1177/1090198119876977. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 194.Terry-McElrath YM, O'Malley PM, Johnston LD. Changes in the order of cigarette and marijuana initiation and associations with cigarette use, nicotine vaping, and marijuana use: US 12th grade students, 2000–2019. Prev Sci. 2020;21(7):960–971. doi: 10.1007/s11121-020-01150-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 195.Tam J, Warner KE. Students’ cigarette smoking and the perceived nicotine content of their e-cigarettes. Am J Prev Med. 2018;55(3):376–383. doi: 10.1016/j.amepre.2018.04.034. [DOI] [PubMed] [Google Scholar]
- 196.Jackson DB, Boccio CM, Leal WE, Vaughn MG. It’s all the rage! Exploring the nuances in the link between vabing and adolescent delinquency. J Crim Just. 2019;63:58–69. doi: 10.1016/j.jcrimjus.2019.04.004. [DOI] [Google Scholar]
- 197.•.Lee J, Kong G, Kassas B, Salloum RG. Predictors of vaping marijuana initiation among US adolescents: results from the Population Assessment of Tobacco and Health (PATH) study wave 3 (2015–2016) and wave 4 (2016–2018) Drug Alcohol Depend. 2021;226:108905. doi: 10.1016/j.drugalcdep.2021.108905. [DOI] [PubMed] [Google Scholar]
- 198.Parks MJ, Patrick ME. Protective Factors for Nicotine and Marijuana Vaping Among US Adolescents. Am J Prev Med. 2021. [DOI] [PMC free article] [PubMed]
- 199.Reboussin BA, Wagoner KG, Ross JC, Suerken CK, Sutfin EL. Tobacco and marijuana co-use in a cohort of young adults: patterns, correlates and reasons for co-use. Drug Alcohol Depend. 2021;227:109000. doi: 10.1016/j.drugalcdep.2021.109000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 200.Morean ME, Davis DR, Kong G, Bold KW, Camenga DR, Suttiratana S, et al. Demographic and substance use-related differences among high school adolescents who vape cannabis versus use other cannabis modalities. Drug Alcohol Depend. 2021;228:109104. doi: 10.1016/j.drugalcdep.2021.109104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 201.Mantey DS, Cooper MR, Clendennen SL, Pasch KE, Perry CL. E-cigarette marketing exposure is associated with e-cigarette use among US youth. J Adolesc Health. 2016;58(6):686–690. doi: 10.1016/j.jadohealth.2016.03.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 202.Agaku IT, Egbe CO, Ayo-Yusuf OA. Circumvention of COVID-19-related restrictions on tobacco sales by the e-cigarette industry in South Africa and comparative analyses of heated tobacco product vs combustible cigarette volume sales during 2018–2020. Prev Med. 2021;148:106526. doi: 10.1016/j.ypmed.2021.106526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 203.Meacham MC, Vogel EA, Thrul J. Vaping-related mobile apps available in the Google Play Store after the Apple ban: content review. J Med Internet Res. 2020;22(11):13. doi: 10.2196/20009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 204.Yang QH, Sangalang A, Rooney M, Maloney E, Emery S, Cappella JN. How is marijuana vaping portrayed on youtube? Content, features, popularity and retransmission of vaping marijuana YouTube videos. J Health Commun. 2018;23(4):360–369. doi: 10.1080/10810730.2018.1448488. [DOI] [PubMed] [Google Scholar]
- 205.Ramamurthi D, Chau C, Jackler RK. JUUL and other stealth vaporisers: hiding the habit from parents and teachers. Tob Control. 2019;28(6):610–616. doi: 10.1136/tobaccocontrol-2018-054455. [DOI] [PubMed] [Google Scholar]
- 206.Cavazos-Rehg PA, Krauss MJ, Sowles SJ, Bierut LJ. Marijuana-related posts on Instagram. Prev Sci. 2016;17(6):710–720. doi: 10.1007/s11121-016-0669-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 207.Majmundar A, Kirkpatrick M, Cruz TB, Unger JB, Allem J-P. Characterising KandyPens-related posts to Instagram: implications for nicotine and cannabis use. Tob Control. 2020;29(4):472–474. doi: 10.1136/tobaccocontrol-2019-055006. [DOI] [PubMed] [Google Scholar]
- 208.Czaplicki L, Tulsiani S, Kostygina G, Feng M, Kim Y, Perks SN, et al. #toolittletoolate: JUUL-related content on Instagram before and after self-regulatory action. PLoS ONE. 2020;15(5):9. doi: 10.1371/journal.pone.0233419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 209.Kostygina G, Feng M, Czaplicki L, Tran H, Tulsiani S, Perks SN, et al. Exploring the discursive function of hashtags: a semantic network analysis of JUUL-related Instagram messages. Soc Media Society. 2021;7(4):20563051211055442. [Google Scholar]
- 210.Kasson E, Singh AK, Huang M, Wu D, Cavazos-Rehg P. Using a mixed methods approach to identify public perception of vaping risks and overall health outcomes on Twitter during the 2019 EVALI outbreak. Int J Med Inform. 2021;155:104574. doi: 10.1016/j.ijmedinf.2021.104574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 211.Kirkpatrick MG, Dormanesh A, Rivera V, Majmundar A, Soto DW, Chen-Sankey JC, et al. # FlavorsSaveLives: an analysis of Twitter posts opposing flavored e-cigarette bans. Nicotine Tob Res. 2021;23(8):1431–1435. doi: 10.1093/ntr/ntaa276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 212.National Conference of State Legislatures. State medical cannabis laws. https://www.ncsl.org/research/health/state-medical-cannabis-laws.aspx. Accessed 19 Oct 2021.
- 213.•.Smart R, Pacula RL. Early evidence of the impact of cannabis legalization on cannabis use, cannabis use disorder, and the use of other substances: findings from state policy evaluations. Am J Drug Alcohol Abuse. 2019;45(6):644–63. doi: 10.1080/00952990.2019.1669626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 214.Hall W, Lynskey M. Assessing the public health impacts of legalizing recreational cannabis use: the US experience. World Psychiatry. 2020;19(2):179–186. doi: 10.1002/wps.20735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 215.Kerr WC, Ye Y, Subbaraman MS, Williams E, Greenfield TK. Changes in marijuana use across the 2012 Washington State Recreational Legalization: is retrospective assessment of use before legalization more accurate? J Stud Alcohol Drugs. 2018;79(3):495–502. doi: 10.15288/jsad.2018.79.495. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 216.Sarvet AL, Wall MM, Fink DS, Greene E, Le A, Boustead AE, et al. Medical marijuana laws and adolescent marijuana use in the United States: a systematic review and meta-analysis. Addiction. 2018;113(6):1003–1016. doi: 10.1111/add.14136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 217.Hasin DS, Wall M, Keyes KM, Cerdá M, Schulenberg J, O'Malley PM, et al. Medical marijuana laws and adolescent marijuana use in the USA from 1991 to 2014: results from annual, repeated cross-sectional surveys. Lancet Psychiatry. 2015;2(7):601–608. doi: 10.1016/S2215-0366(15)00217-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 218.Keyes KM, Wall M, Cerdá M, Schulenberg J, O’malley PM, Galea S, et al. How does state marijuana policy affect US youth? Medical marijuana laws, marijuana use and perceived harmfulness: 1991–2014. Addiction. 2016;111(12):2187–95. doi: 10.1111/add.13523. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 219.Cerdá M, Mauro C, Hamilton A, Levy NS, Santaella-Tenorio J, Hasin D, et al. Association between recreational marijuana legalization in the United States and changes in marijuana use and cannabis use disorder from 2008 to 2016. JAMA Psychiatry. 2020;77(2):165–171. doi: 10.1001/jamapsychiatry.2019.3254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 220.Hall W, Stjepanović D, Caulkins J, Lynskey M, Leung J, Campbell G, et al. Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet. 2019;394(10208):1580–1590. doi: 10.1016/S0140-6736(19)31789-1. [DOI] [PubMed] [Google Scholar]
- 221.Dilley JA, Richardson SM, Kilmer B, Pacula RL, Segawa MB, Cerdá M. Prevalence of cannabis use in youths after legalization in Washington state. JAMA Pediatr. 2019;173(2):192–193. doi: 10.1001/jamapediatrics.2018.4458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 222.Cwalina SN, Braymiller JL, Leventhal AM, Unger JB, McConnell R, Barrington-Trimis JL. Prevalence of young adult vaping, substance vaped, and purchase location across five categories of vaping devices. Nicotine Tob Res. 2021;23(5):829–835. doi: 10.1093/ntr/ntaa232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 223.Jackler RK, Li VY, Cardiff RA, Ramamurthi D. Promotion of tobacco products on Facebook: policy versus practice. Tob Control. 2019;28(1):67–73. doi: 10.1136/tobaccocontrol-2017-054175. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.