Abstract
We report an extremely rare case of extranodal B-cell NHL: DLBCL (diffuse large B-cell non-Hodgkin lymphoma), stage IVE, presenting with heart and bilateral adrenal involvement. On admission, adrenal and thorax imaging identified large bilateral adrenal masses and a 4.6 cm mass in the right atrium wall. An adrenal biopsy revealed the presence of a DLBCL, with triple expression of bcl2, bcl6, C-MYC(+70%). Following six cycles of systemic immunochemotherapy with R-DA-EPOCH, and high methotrexate dose for CNS prophylaxis a marked decrease of lymphoma infiltration was observed. The selection of the appropriate treatment modality can lead to profound response and improve patient's outcome.
Keywords: Non-hodgkin's lymphoma, Cardiac lymphoma, Adrenal lymphoma, Diffuse large b-cell non-hodgkin lymphoma
Abbreviations: PCL, primary cardiac lymphoma
1. Introduction
Non-Hodgkin lymphoma (NHL) is the most commonly occurring type of lymphoma, that affects 386,000 cases worldwide per year [1]. Although lymph node involvement is more commonly encountered, extranodal localization is a rare condition that accounts for less than one-third of patients with NHL at diagnosis. The most common site of extranodal localization is the gastrointestinal tract whereas the heart or the endocrine organs such as adrenal glands and thyroid may be involved rarely.
Malignant cardiac lymphoma accounts for 1.3% of primary cardiac tumors and 0.5% of all extranodal lymphomas whereas, secondary cardiac involvement by disseminated lymphomas has been observed in 20% of autopsy cases. The incidence of primary cardiac lymphomas (PCL) is 0.011 per 100,000 people and the most common type is the diffuse large B-cell lymphoma (DLBCL). Extranodal adrenal involvement is reported in less than 1% of all NHL and 3% of primary extranodal lymphomas and the most common type is DLBCL.
This report describes an unusual case of extranodal NHL presented with heart and bilateral adrenal involvement.
2. Case presentation
A 72-year-old patient (BMI:26Kg/m2) referred to our Endocrinology Unit for investigation of a 3.8 cm right adrenal mass diagnosed by abdominal ultrasound and thereafter by computed tomography (CT) because of abdominal pain that was subsequently resolved. He did not report night sweats or fever, dyspnea, or precordial pain. His-medical history included a diagnosis of hypertension and atrial fibrillation the last 10 years. On admission, a repeated adrenal CT scan showed large bilateral adrenal masses of 6.7 cm on the right adrenal gland compressing the inferior vena cava and of 3.7 cm on the left adrenal gland (Fig. 1A). There was increased precontrast CT attenuation (31–35HU), heterogeneous enhancement and no substantial contrast washout on delayed imaging.
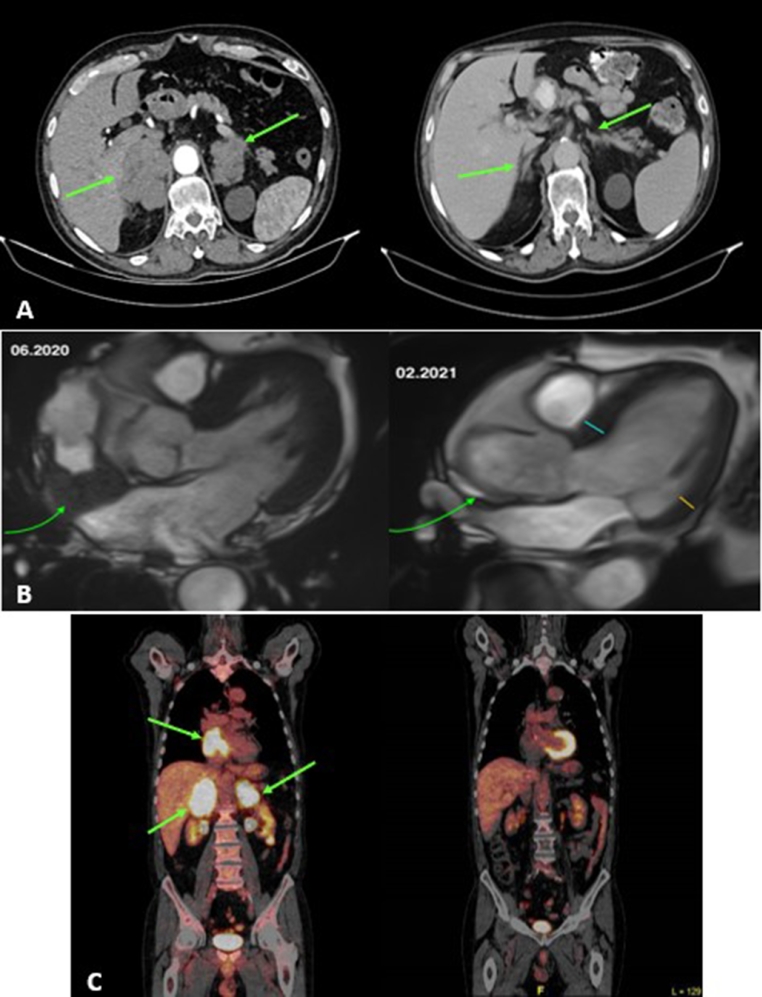
Fig. 1.
A: Contrast-enhanced adrenal CT: comparisons of adrenal masses before and after treatment. i: bilateral ill defined adrenal masses of 6.7 cm on the right and of 3.7 cm on the left adrenal and ii: significant bilateral masses’ regression post-treatment. B: Cardiac MRI (balanced SSFP sequences): Comparisons of cardiac mass before and after treatment i: mass of 4.6 × 5.5 cm of reduced signal surrounding the right atrium and ii: significant mass regression post-treatment C: PET-CT scan. i: High accumulation of FDG in both the cardiac atrium (SUVmax 21.2) and adrenals tumors (SUVmax 20.5). ii: The abnormal uptake disappeared after 6 cycles of immunochemotherapy.
The biochemical and hormonal work-up were unremarkable except for mild anemia (Hb 11.8 g/dl, Ht 36%, MCV 79fL, MCH 25.5pg) and mildly increased lactate dehydrogenase [LDH 299 U/L (NR:134–279 U/L]. The morning cortisol and adrenocorticotropin hormone levels were within normal range [324 nmol/L (NR:138–745 nmol/L), and 13 nmol/L (NR:10–60pg/ml), respectively]. Cortisol response after a Short Synacthen Test (0 min 274 nmol/L, 30 min 454 nmol/L and 60 min 789 nmol/L) excluded adrenal insufficiency. Cortisol after overnight dexamethasone suppression test (48 nmol/L) and aldosterone after saline infusion test (21.5 pmol/L) were suppressed excluding autonomous cortisol or aldosterone secretion. Twenty-four-hours urinary metanephrine and normetanephrine excretion were normal [220 μg/24 h (NR<341 μg/24 h) and 311 μg/24 h (NR<444 μg/24 h) respectively].
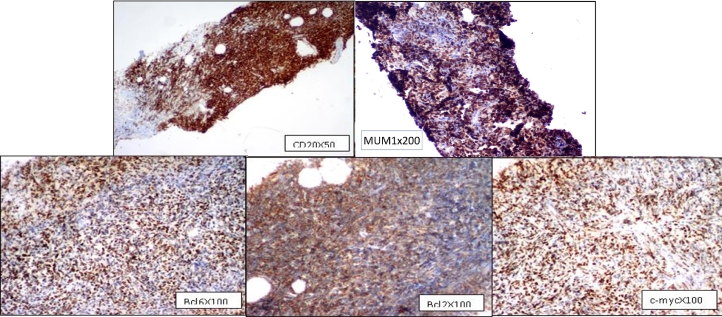
A systemic-metastatic disease was very likely and the patient underwent evaluation with thorax, CT scan that revealead a 4.6 × 5.5 × 2.6 cm mass in the right atrium wall which extends from the superior vena cava junction to the inferior vena cava junction. Subsequent cardiac magnetic resonance imaging (MRI) confirmed the previous finding (Fig. 1B). Left ventricular ejection fraction was 55%. The CT-guided adrenal biopsy and the immunohistochemistry investigation revealed the presence of a DLBCL with triple expression of bcl2, bcl6, c-myc (+70%). MUM1 was positive and Ki-67 was 99% (Fig. 2). LCA, CD20, bcl2, bcl6, CD79a, PAX5 were positive, whereas CD3, CD5, CyclinD1, CD10, κ/λ, CD30 were negative. Fluorescence in situ hybridization for bcl-2, bcl-6 and c-myc oncogenes was performed on the adrenal biopsy, but results were unreliable due to technical reasons. The CNS International Prognostic Index (CNS-IPI) score was 5 suggesting an increased risk for CNS progression/reccurence [2]. Virology tests for Epstein Barr virus and HIV were negative. Bone marrow aspiration, trephine biopsy and cerebrospinal fluid analysis were negative for lymphoma infiltration. Karyotype was normal and MRI brain spectroscopy was negative for CNS lymphoma detection.
Fig. 2.
Immunohistochemistry of adrenal neoplastic tissue establishing the diagnosis of a DLBCL. The neoplastic cells show positivity for CD20, bcl2, bcl6 and MUM1 whereas c-myc is positive in 70% of the neoplastic nuclei.
A week later, a positron emission tomography (PET-CT) scan showed hyper-metabolic infiltrative masses involving the right atrium and both adrenal glands (Fig. 1C). The Deauville score was 5. The patient continued to be asymptomatic
The final diagnosis was primary extranodal lymphoma, DLBCL type, with cardiac and bilateral adrenal involvement, stage IVE.
Although there was not performed a biopsy of the infiltrative mass involving the right atrium, the clinical findings were compatible with lymphoma infiltration as the patient had neither thrombosis of the right atrium or infection. On the contrary, he was afebrile and CRP and d-Dimers levels were within normal limits.
Under the care of the hematology team, systemic immunochemotherapy with R-DA-EPOCH and high dose of methotrexate for CNS prophylaxis were administrated. The regimen was as follows: Rituximab 375 mg/m2 iv Day (D) 1, Etoposide 50 mg/m2 iv D1-D4, Doxorubicin 10 mg/m2 iv D1-D4, Vincristine 0.4 mg/m2 iv D1-D4. Prednisolone 60 mg/m2 iv D1-D5, Cyclophospamide 480 mg/m2 iv D5. Filgrastim amp sc 48IU, initiating from D6 until neutrophil count>1500/μL. The R-DA-EPOCH regimen was escalated from level −1 to level 1 in the subsequent cycles. The patient received six cycles of R-DA-EPOCH and two cycles of high dose Methotrexate (3 gr/m2), after the 5th and 6th cycle of R-DA-EPOCH. Three months after the completion of six cycles of immunochemotherapy, a marked decrease of lymphoma infiltration in the post-chemotherapy imaging was found (Fig. 1A,B,C). The Deauville score in PET-CT scan was 1. Left ventricular ejection fraction was increased at 64%. The treatment was complicated (D12) with reversible paralytic ileus, due to vincristine neurotoxicity (grade III), which was discontinued after the first cycle and with choledocholithiasis (D24) which was resolved with ERCP. The patient has been stable, with performance status (ECOG:0) in complete response, 14 months after the treatment completion.
3. Discussion
At presentation, the imaging characteristics of the patient's adrenal masses made the differential diagnosis of an adrenocortical carcinoma or a metastatic or infiltrative disease. Thereafter, the imaging findings of the heart mass put the diagnosis of a malignant cardiac tumor and the biopsy revealed a lymphoma. We could not predict which of the two lesions (heart or adrenals involvement) was developed first. However, the detection of a cardiac tumor and in particular the involvement of the right atrium, which is the most common site of PCL, led us to the assumption of a PCL in advanced stage, with secondary adrenal involvement. However, neither adrenal hyperfunction nor hypofunction were found.
Cardiac NHLs are associated with a poor prognosis with a median survival of 7 months after initial diagnosis [3]. From 1949 to 2009 and from 2009 to 2019, 19 [4] and 101 [5] PCL cases were reported, respectively. Right atrium is the most common site in 77% of cases.
Cardiac tumors could be asymptomatic and found incidentally or more frequently, are symptomatic and related to the tumor's size and location which can lead to pericardial effusion, acute heart failure or sudden death. Dyspnea is the most common symptom (64% of cases) followed by chest pain (14%) and syncope (11%), whereas atrial fibrillation (26%) and atrioventricular block (26%) are the most common abnormalities in ECG [5].
Regarding adrenal lymphoma, about 200 cases of primary adrenal lymphoma have been reported [6]. The most common symptoms are B-symptoms, pain and fatigue. They are large tumors, bilateral in about 70% of cases, DLBCL in 78%, with elevated LDH in 88% cases and complete or partial adrenal insufficiency in 61%.
Chemotherapy is the treatment of choice for primary cardiac or adrenal lymphomas. There are no specific treatment protocols. Systemic immunochemotherapy with CHOP, R-CHOP [4] or R-EPOCH are used for patients with DLBCL and have improved survival rates. Radiotherapy alone or in combination with chemotherapy has also been implemented in some patients [3]. Surgical intervention was offered as rescue strategy in selective cases with extremely large cardiac masses which cause obstruction or pericardial tamponade [7]. In a previous systematic review, 89% of the patients received chemotherapy, 28% underwent surgery and 20% radiotherapy [4]. Only 38% of them were treated with rituximab, whereas in a recent review, 70% of them were treated with rituximab[5]. In our case, a standard protocol with R-DA-EPOCH plus high dose of methotrexate was used and our patient remains in complete remission up to now, fourteen months post-chemotherapy. The reasons of the high dose of methotrexate administration were the high-risk of CNS relapse rates (12%−25%) even in stage I of DLBCL with triple expression [8], the high CNS-IPI score and the extranodal involvement in the adrenal glands [6,9]. Recent data suggests that CNS prophylaxis is necessary in such cases, regardless of the CNS-IPI score [2,10].
The optimal approach to prophylaxis for patients at high risk for CNS involvement is controversial and varies between institutions. We favor high-dose systemic methotrexate (MTX), but we consider intrathecal (IT) MTX to be an acceptable option; some experts favor treatment with both IT and systemic MTX
According to the Surveillance, Epidemiology and End Results Program database between 1973 and 2015 [11], in a total of 144 patients with PCL, more than 70% received chemotherapy. The 5-year overall survival and cause-specific survival rates were 36.1% and 47.2%, respectively. Age, stage, and chemotherapy were the main factors affecting prognosis. The complete response rate and overall response rate to chemotherapy were 60% and 82%, respectively [5], which were similar to previous data [4].
After a literature search, we identified two males with similar presentations. The first one was a case of malignant lymphoma infiltrating the right ventricle, tricuspid valve, the interventricular septum, and the left adrenal. He was presented with cardiac heart failure [12]. The second was a case with malignant lymphoma involving the right atrium and right ventricle with hemopericardium and bilateral adrenal glands [13]. Both patients received chemotherapy (CHOP or R-CHOP) and had remarkable improvement. However, despite the good initial response to chemotherapy, the second patient refused a 2nd cycle of treatment and died few months later. According to the literature review, our case is the third one worldwide of a primary extranodal NHL with cardiac and adrenal glands involvement.
In this report the asymptomatic clinical presentation of an extranodal DLBCL, the challenges faced in the differential diagnosis and the marked response to immunochemotherapy are described. The selection of the appropriate treatment modality can lead to profound response and improve patient's outcome and quality of life. Clinical experience and awareness as well as a multidisciplinary approach in such complex cases is mandatory.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statment
LP, EM: wrote and revised the article, NS, MV, AD, PL, AP, EV, IAV: collected and interpreted the data, TC, TM, TK: revised and edited the article
Informed consent
The patient has submitted written informed consent to publish this observation.
Declarations of Competing Interest
The authors declare no conflict of interest.
Acknowledgements
None
References
- 1.Ferlay J., Soerjomataram I., Dikshit R., Eser S., Mathers C., Rebelo M., Parkin D.M., Forman D., Bray F. Cancer incidence and mortality worldwide: sources, methods and major patterns in GLOBOCAN 2012. Int. J. Cancer. 2015;136:359–386. doi: 10.1002/ijc.29210. [DOI] [PubMed] [Google Scholar]
- 2.Schmitz N., Zeynalova S., Nickelsen M., Kansara R., Villa D., Sehn L.H., Glass B., Scott D.W., Gascoyne R.D., Connors J.M., Ziepert M., Pfreundschuh M., Loeffler M., Savage K.J. CNS international prognostic index: a risk model for CNS relapse in patients with diffuse large B-cell lymphoma treated with R-CHOP. J. Clin. Oncol. 2016;34:3150–3156. doi: 10.1200/JCO.2015.65.6520. [DOI] [PubMed] [Google Scholar]
- 3.Miguel C.E., Bestetti R.B. Primary cardiac lymphoma. Int. J. Cardiol. 2011;149:358–363. doi: 10.1016/j.ijcard.2010.02.016. [DOI] [PubMed] [Google Scholar]
- 4.Petrich A., Cho S.I., Billett H. Primary cardiac lymphoma: an analysis of presentation, treatment, and outcome patterns. Cancer. 2011;117:581–589. doi: 10.1002/cncr.25444. [DOI] [PubMed] [Google Scholar]
- 5.Chen H., Qian S., Shi P., Liu L., Yang F. A presentation, treatment, and survival analysis of primary cardiac lymphoma cases reported from 2009 to 2019. Int. J. Hematol. 2020;112:65–73. doi: 10.1007/s12185-020-02881-2. [DOI] [PubMed] [Google Scholar]
- 6.Rashidi A., Fisher S.I. Primary adrenal lymphoma: a systematic review. Ann. Hematol. 2013;92:1583–1593. doi: 10.1007/s00277-013-1812-3. [DOI] [PubMed] [Google Scholar]
- 7.J. Xia, L. Song, B. Wang, Y. He, X. Ma, Surgical treatment of a primary cardiac lymphoma presenting with cardiac tamponade Gen Thorac Cardiovasc Surg. 69 (2021) 356–359. doi: 10.1007/s11748-020-01455-7. [DOI] [PubMed]
- 8.Qualls D., Abramson J.S. Advances in risk assessment and prophylaxis for central nervous system relapse in diffuse large B-cell lymphoma. Haematologica. 2019;104:25–34. doi: 10.3324/haematol.2018.195834. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grigg A.P. JM connors primary adrenal lymphoma. Clin. Lymphoma. 2003;4:154–160. doi: 10.3816/clm.2003.n.024. [DOI] [PubMed] [Google Scholar]
- 10.El-Galaly T.C., Villa D., Michaelsen T.Y., Hutchings M., Mikhaeel N.G., Savage K.J., Sehn L.H., Barrington S., Hansen J.W., Smith D., Rady K., Mylam K.J., Larsen T.S., Holmberg S., Juul M.B., Cordua S., Clausen M.R., Jensen K.B., Johnsen H.E., Seymour J.F., Connors J.M., de Nully Brown P., Bøgsted M. Cheah CY The number of extranodal sites assessed by PET/CT scan is a powerful predictor of CNS relapse for patients with diffuse large B-cell lymphoma: an international multicenter study of 1532 patients treated with chemoimmunotherapy. Eur. J. Cancer. 2017;75:195. doi: 10.1016/j.ejca.2016.12.029. [DOI] [PubMed] [Google Scholar]
- 10.Xiao M., Lin J., Xiao T., Lin Y., Ye Y. The incidence and survival outcomes of patients with primary cardiac lymphoma: a SEER-based analysis. Hematol. Oncol. 2020;38:334–343. doi: 10.1002/hon.2741. [DOI] [PubMed] [Google Scholar]
- 11.Memon A.Q., Xavier L. Malignant lymphoma of the heart. Featured echocardiogram and case report. Cardiol. Rev. 2002;10:323–325. doi: 10.1097/00045415-200211000-00003. [DOI] [PubMed] [Google Scholar]
- 13.Chen C.F., Hsieh P.P., Lin S.J. Primary cardiac lymphoma with unusual presentation: a report of two cases. Mol. Clin. Oncol. 2017;6:311–314. doi: 10.3892/mco.2017.1131. [DOI] [PMC free article] [PubMed] [Google Scholar]