Summary
Background
Cardiovascular disease (CVD) is the leading cause of death (COD) in China. Understanding the characteristics of place of death (POD) among CVD deaths would be of great importance to evaluate the healthcare service utilization at the end stage of life. Limited studies have reported the POD distribution among CVD deaths, and little was known about the associated factors of hospital CVD deaths.
Methods
By using data from National Mortality Surveillance System (NMSS) in China, this study presented the characteristics of POD distribution during 2008 and 2020. Afterwards, multilevel logistic regression was used to explore associated factors of hospital CVD deaths and quantify the magnitude to which the spatial variations of hospital CVD deaths could be explained by those associated factors.
Findings
During 2008-2020, there was 7101871 CVD deaths collected by NMSS in China, with 77·13% home deaths and 18·49% hospital deaths. Shanghai (59·40%) had the highest percentage of hospital CVD deaths. Age, sex, ethnicity, marital status, education, occupation, underlying COD were significant influential factors of hospital CVD deaths. Spatial variations were shown at provincial level, with 33·88% of them being explained by factors at individual level.
Interpretation
Home was the leading POD among CVD deaths in China, those CVD decedents characterized as the female, the youngest, Han population, the married, the retiree, lived in urban areas, with higher socioeconomic status and died of chronic CVDs had a higher probability of hospital deaths. Providing accessible and available healthcare services were priorities to improve quality of end-of-life care, significant variations among provinces and sub-population also reminded us of the requirements for equal healthcare resources allocation and multiple options for minorities of POD preference at the end stage of life.
Funding
National Key Research & Development Program of China (grant number 2018YFC1315301)
Keywords: Cardiovascular disease, Place of death, China, Trends, Spatial variations, Associated factors
Research in context.
Evidence before this study
We used the key words “place of death”, “place of cardiovascular disease deaths”, “trends of place of death”, “spatial variations of place of death”, “associated factors of place of death”, “place of death and end-of-life care” and “epidemiology” to search PubMed, Science Direct, Web of Science, and the official websites of the Chinese Government and other institutions for studies and reports on place of death (POD) and POD among cardiovascular disease (CVD) deaths in China published in English or Chinese until July 31, 2021. Although previous researches have showed that over 70% deaths occurred at home, limited domestic studies were observed to report neither the spatial variations of POD distribution nor the associated factors of hospital deaths, especially among CVD decedents.
Added value of this study
China National Mortality Surveillance System (NMSS) is the most populous mortality surveillance system worldwide and the only one with provincial representativeness which covers over 300 million individuals (accounts for 24% of total Chinese population) from 31 provinces. By using data collected by NMSS, for the first time, this study comprehensively presented the POD distribution among CVD deaths and explored associated factors of hospital CVD deaths from both individual and regional level. Our study found that home was the leading POD among CVD deaths in China, which showed much disparities compared with western countries. Demographics and individual socioeconomic status explained majority of spatial variations rather than socioeconomic contextual factors among hospital CVD deaths, significant variations among provinces and sub-population were also observed.
Implications of all the available evidence
Evidence from our study indicated that, first, expanding medical and healthcare capacities, elevating efficiency and effectiveness of clinical interventions should be the priorities, especially for acute and severe CVD patients. Second, substantial provincial variations of POD distribution indicated the disparities existed in medical and healthcare resources allocation, which make the requests of tailoring regional-specific strategies to bridge the gap between different provinces and urban/rural areas. Third, personalized humanistic care should be provided for those ethnic groups in accordance with their cultural belief, and various options and additional supports should be developed to those vulnerable population for accessible and affordable healthcare services. Finally, enabling the concept of filial piety to establish an integrity of clinical care and community-based or home-based care to formulate long-term care system that supports informal care. Those experiences should also be evaluated and could be generalized to other developing countries.
Alt-text: Unlabelled box
Introduction
Cardiovascular disease (CVD) is the largest single contributor to global mortality and the leading cause of death (COD) in China that accounts for 40% of total deaths.1 In 2019, it was reported that there was 4·58 million CVD deaths and 120·33 million CVD patients in China, which have caused heavy strain to health care system.2,3 Worldwide, place of death (POD) has been considered as a valid indicator of care provided during the end-of-life (EOL) and outcome measure of healthcare services.4 China is the most populous developing country in the world with a very distinct culture and health care system.4 Therefore, understanding the characteristics of POD patterns and its associated factors would help us to evaluate the healthcare services utilization and unveil the mechanisms that determine POD among CVD deaths in China.4,5
Overseas, existed studies have reported POD distribution and its associated factors among patients died of different COD, such as CVD,6 cancer,5 dementia7 and pediatric diseases.8 They have found that most of deaths occurred in hospitals, home, nursing homes or hospice facilities, and POD were usually affected by demographics, personal preferences, disease-related factors and socioeconomic contextual factors.9,10 In China, Zhou,11,12 Jiang,13 Li14 and Gu4 have found home was the leading POD. Yet, to date, there have been limited domestic in-depth updates concerning the associated factors of POD or hospital deaths, especially among CVD deaths.11,12 Thus, in this population-based study, we presented findings by using data from National Mortality Surveillance System (NMSS) in China during 2008-2020, aimed to (i) describe the POD distribution among CVD deaths; (ii) explore the associated factors of hospital CVD deaths and provide reasonable explanations of their associations.
Methods
Data sources
Data for CVD deaths was extracted from NMSS housed in Chinese Center for Disease Control and Prevention (China CDC). NMSS was initiated in 1978 with 2 polit surveillance points in Beijing, while the urban areas were defined as districts and the rural areas were defined as counties, the Disease Surveillance Point system (DSPs) was subsequently established in 1990 with 79 points covering 10 million population and expanded in 2004 with 161 points covering 73 million population. In 2013, the National Health and Family Planning Commission (previously known as Ministry of Health) combined DSPs in China CDC and Vital Registration (VR) system hosted by Ministry of Health to create an integrated NMSS. As the most populous mortality surveillance system worldwide and the only one with provincial representativeness in China, NMSS covers over 300 million individuals from 605 surveillance points in 31 provinces that accounts for 24% of population, and routinely collects individual details of death information in real time through an internet-based approach. Detailed descriptions of NMSS representativeness determination, surveillance points selection, death information collection, coding and determining underlying COD as well as quality control procedures of NMSS, have been reported elsewhere.15
Participants
Data quality control
In order to ensure the reliability and validity of data from NMSS, we have reviewed, compared and evaluated the data quality nationally and in each of the surveillance point to exclude certain points which was considered to be seriously under-reported and might affect overall results. We made the crude mortality rate of lower than 4·5‰ as exclusion criteria for those points belongs to VR system and DSPs earlier than 2012. Since 2013, we made the criteria of 5‰.16 We also excluded death cases with missing values of key indicators like POD, sex and age.
Mortality data extraction
Underlying COD in NMSS was recorded by using International Classification of Disease 10th Edition (ICD-10). All deaths between 2008 and 2020 where CVD was identified as underlying COD were extracted. We classified total CVD as rheumatic heart disease (RHD), hypertensive heart disease (HHD), ischemic heart disease (IHD), stroke, myocarditis and myocardial disease (MMD), aortic aneurysm (AA) and other CVDs. Further, we divided IHD into acute myocardial infarction (AMI) and chronic ischemic heart disease (CIHD), stroke into hemorrhagic stroke (HS) and ischemic stroke (IS) for CVD subcategory analysis. Detailed of included number of surveillance points from NMSS and CVD deaths was reported in Table S1, the CVD classification and its ICD-10 codes was reported in Tables S2 in the Supplementary Material.
Variables
We grouped POD of CVD deaths into five categories: hospitals, home, nursing homes, on the way to hospitals and others/unknown. For explanatory variables, we included: location (which we defined districts as urban areas and counties as rural areas), demographics (sex, age, ethnicity, marital status), socioeconomic status (SES, including the level of education attainment and occupation), disease-related factors (underlying COD, highest diagnostic institutions, highest diagnosis basis). We analyzed age (years old) as an ordered four category (0-14, 15-64, 65-84, 85 and above) rather than a continuous variable to facilitate interpretation and comparison with other studies.5,6,17 Besides, socioeconomic contextual factors at provincial level were included and were classified by four quartiles during 2008-2020: region (western, central and eastern), per capita gross domestic product (GDP, 10000 yuan per person), average years of education attainment (years), number of beds in healthcare institutions per 100000 persons (units). For GDP at provincial level, in the consideration of discount rate during the study period, we used a 3% (0-6% for recommended range) discount rate to translate cash (GDP) at the end of each time point (from 2009 to 2020) into present value in 2008.18 We also included a dummy variable to examine the change before and after NMSS expansion in 2013.
Statistical analysis
We first presented POD distribution among CVD deaths by important characteristics during 2008-2020. We used χ2 test to compare the differences of characteristics distribution among nominal categories and logistic regression to test their trends for ordered variables. Subsequently, we conducted multilevel logistic regression to explore the individual factors and socioeconomic contextual correlates of hospital CVD deaths, thus we defined home, nursing homes, on the way to hospitals and others/unknown as “out-of-hospital CVD deaths”. Several models were constructed separately. First, a two-level null model (Model 1) that included fixed and random intercepts was fitted to investigate spatial variations across multiple scales, among which, random intercepts accounted for the clustering of participants (level 1) within provinces (level 2). Random effects at individual level thus were translated into median odds ratio (MOR) which indicated median value of the odds between the area with the highest outcome probability and the area with the lowest.19 To explore to what extent those personal and contextual factors explained the spatial variations of hospital CVD deaths, demographics (Model 2), SES (Model 3), underlying COD (Model 4) and contextual phenomena (Model 5) were stepwise entered into the multilevel logistic model and the proportional change in variance (PCV) was calculated for each step. PCV reflects the proportion of variation that can be explained by newly-added variables to the model.20, 21, 22 Afterwards, we added two-way interaction terms of individual level factors and separate provincial level characteristics to the models to examine whether the effects of contextual variables on hospital CVD deaths were modified by personal variables (Model 6).23,24 For detailed CVD subcategories, we performed a similar analysis among IHD and stroke deaths specifically to identify associated factors in two leading causes of CVD deaths. A P value<0·05 was considered statistically significant and all tests were two sided. The analysis was performed in SAS 9·4 (SAS Institute Inc., Cary, North Carolina USA).25
Role of the funding source
The funders of the study have no role in study design, data collection, data analysis, data interpretation, or writing of the report. The corresponding authors have full access to all the data in the study and have final responsibility for the decision to submit for publication.
Results
Characteristics of POD distribution among CVD deaths
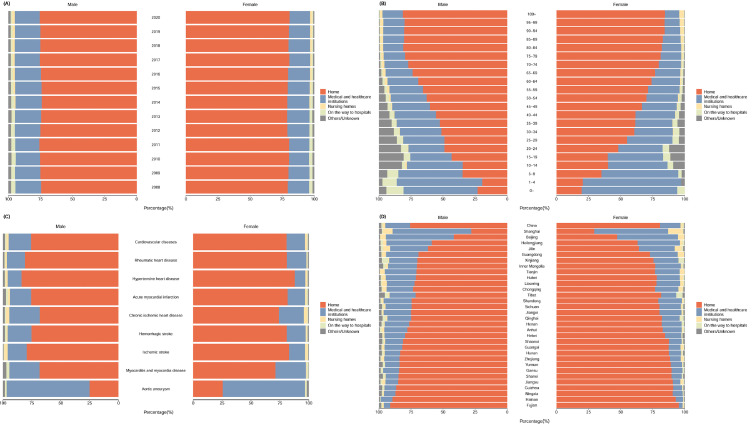
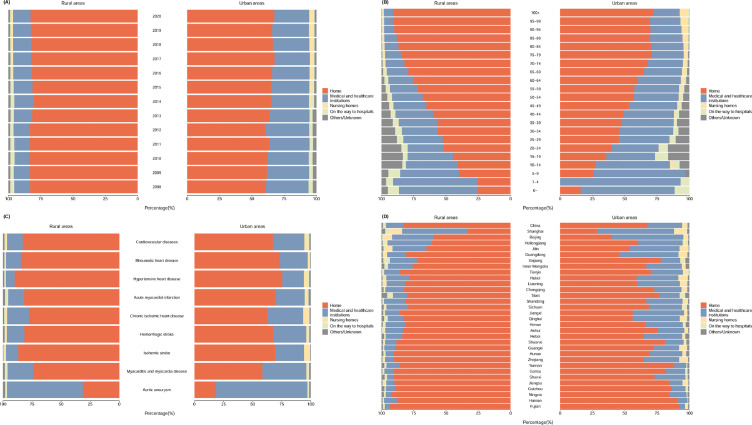
During 2008-2020, as shown in Table 1, there were 7101871 CVD deaths collected by NMSS, among them, home was the leading POD (77·13%), followed by hospitals (18·49%) and nursing homes (1·69%). Meanwhile, the disparities of POD distribution among those CVD deaths by important characteristics was also presented in Table 1, and all of them showed significant differences between each group. In 2020, for CVD subcategories specifically, IHD and stroke were two leading causes of CVD deaths, with substantial provincial variations between male and female, urban and rural population (Figure S1 in the Supplementary Materials). Nationwide, as shown in Figure 1, Figure 2, in 2020, the percentage of home deaths increased with age and reached its peak among 100 years old and above (83·68%). Patients died of HHD (85·67%) had the highest proportion of home deaths while AA (71·57%) were highest in hospital deaths. Shanghai (59·40%) and Beijing (50·32%) were top two provinces with highest proportion of hospital deaths, on the contrary, Fujian (93·14%) and Hainan (90·97%) had the highest proportion of home deaths. Apart from these, female CVD patients and those who lived in urban areas showed a relatively higher proportion of hospital deaths compared with their counterparts in each of the characteristics. During 2008-2020, the time trends of POD distribution were observed to be nearly unchanged in the aspects of age groups, CVD and its main subcategories as well as provinces (Figure 1, Figure 2, and Figure S3-1 to Figure S3-7 in the Supplementary Materials). We also added a choropleth map to demonstrate spatial variations of average percentage of hospital CVD deaths during 2008 and 2020 (Figure S4 in the Supplementary Materials).
Table 1.
Characteristics of POD distribution among CVD death from NMSS in China, 2008-2020 (Death counts (person), %)
| Characteristics | Total (Death counts (person), %) | Medical and healthcare institutions (Death counts (person), %) | Out of medical and healthcare institutions (Death counts (person), %) |
|||
|---|---|---|---|---|---|---|
| Home | Nursing homes | On the way to hospitals | Others/Unknown | |||
| Total | 7101871 (100·00) | 1312850 (18·49) | 5477427 (77·13) | 119896 (1·69) | 80578 (1·13) | 111120 (1·56) |
| Location | ||||||
| Rural | 4972998 (70·02) | 695221 (52·96) | 4083287 (74·55) | 86134 (71·84) | 34430 (42·73) | 73926 (66·53) |
| Urban | 2128873 (29·98) | 617629 (47·04) | 1394140 (25·45) | 33762 (28·16) | 46148 (57·27) | 37194 (33·47) |
| P for differenceb | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Region a | ||||||
| Western | 1669095 (23·50) | 256303 (19·52) | 1340500 (24·47) | 26219 (21·87) | 13715 (17·02) | 32358 (29·12) |
| Central | 2672896 (37·64) | 549425 (41·85) | 2002981 (36·57) | 56582 (47·19) | 25788 (32·00) | 38120 (34·31) |
| Eastern | 2759880 (38·86) | 507122 (38·63) | 2133946 (38·96) | 37095 (30·94) | 41075 (50·98) | 40642 (36·57) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Sex | ||||||
| Male | 3860831 (54·36) | 771294 (58·75) | 2891030 (52·78) | 73731 (61·50) | 46523 (57·74) | 78253 (70·42) |
| Female | 3241040 (45·64) | 541556 (41·25) | 2586397 (47·22) | 46165 (38·50) | 34055 (42·26) | 32867 (29·58) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Age groups, years old | ||||||
| 0-14 | 3721 (0·05) | 2068 (0·16) | 1043 (0·02) | 335 (0·28) | 1 (0·00) | 274 (0·25) |
| 15-64 | 1331828 (18·75) | 350745 (26·72) | 874114 (15·96) | 43117 (35·96) | 10281 (12·76) | 53571 (48·21) |
| 65-84 | 4004276 (56·38) | 707383 (53·88) | 3151142 (57·53) | 59445 (49·58) | 42569 (52·83) | 43737 (39·36) |
| 85 and above | 1762046 (24·81) | 252654 (19·24) | 1451128 (26·49) | 16999 (14·18) | 27727 (34·41) | 13538 (12·18) |
| P for trendc | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Ethnicity | ||||||
| Han | 6681073 (94·07) | 1256756 (95·73) | 5134034 (93·73) | 112926 (94·19) | 74500 (92·46) | 102857 (92·56) |
| Other ethnics | 420798 (5·93) | 56094 (4·27) | 343393 (6·27) | 6970 (5·81) | 6078 (7·54) | 8263 (7·44) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Marital status | ||||||
| Married | 4460593 (62·81) | 961501 (73·24) | 3311712 (60·46) | 88165 (73·53) | 25329 (31·43) | 73886 (66·49) |
| Unmarried | 194097 (2·73) | 37993 (2·89) | 130946 (2·39) | 3633 (3·03) | 13327 (16·54) | 8198 (7·38) |
| Widowed/Divorced | 2397127 (33·75) | 304469 (23·19) | 2002333 (36·56) | 27247 (22·73) | 40927 (50·79) | 22151 (19·93) |
| Unknown | 50054 (0·70) | 8887 (0·68) | 32436 (0·59) | 851 (0·71) | 995 (1·23) | 6885 (6·20) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Education | ||||||
| Junior high school and below | 6451663 (90·84) | 1021065 (77·77) | 5170385 (94·39) | 99515 (83·00) | 70497 (87·49) | 90201 (81·17) |
| Senior high school | 529794 (7·46) | 222315 (16·93) | 265834 (4·85) | 17200 (14·35) | 7394 (9·18) | 17051 (15·34) |
| College and above | 120414 (1·70) | 69470 (5·29) | 41208 (0·75) | 3181 (2·65) | 2687 (3·33) | 3868 (3·48) |
| P for trend | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Occupation | ||||||
| Agricultural-related personnel | 5253275 (73·97) | 568941 (43·34) | 4505919 (82·26) | 80973 (67·54) | 30332 (37·64) | 67110 (60·39) |
| Retired | 611319 (8·61) | 274054 (20·87) | 299824 (5·47) | 9229 (7·70) | 21212 (26·32) | 7000 (6·30) |
| Unemployment/Student | 409474 (5·77) | 122344 (9·32) | 260643 (4·76) | 8542 (7·12) | 9511 (11·80) | 8434 (7·59) |
| Worker/Self-employed/Enterprise manager | 319004 (4·49) | 135422 (10·32) | 155978 (2·85) | 9294 (7·75) | 6661 (8·27) | 11649 (10·48) |
| Professional/Staff/Civil servant | 132868 (1·87) | 67153 (5·12) | 55276 (1·01) | 4065 (3·39) | 1955 (2·43) | 4419 (3·98) |
| Others/Unknown | 375931 (5·29) | 144936 (11·04) | 199787 (3·65) | 7793 (6·50) | 10907 (13·54) | 12508 (11·26) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Underlying cause of death | ||||||
| Rheumatic heart disease | 95272 (1·34) | 17546 (1·34) | 74826 (1·37) | 1255 (1·05) | 472 (0·59) | 1173 (1·06) |
| Hypertensive heart disease | 404892 (5·70) | 47809 (3·64) | 341582 (6·24) | 5871 (4·90) | 4467 (5·54) | 5163 (4·65) |
| Ischemic heart disease | 2569847 (36·19) | 517092 (39·39) | 1920166 (35·06) | 53946 (44·99) | 30537 (37·90) | 48106 (43·29) |
| Stroke | 3213270 (45·25) | 564317 (42·98) | 2528016 (46·15) | 43666 (36·42) | 37242 (46·22) | 40029 (36·02) |
| Myocarditis and myocardial disease | 12672 (0·18) | 2876 (0·22) | 9208 (0·17) | 315 (0·26) | 31 (0·04) | 242 (0·22) |
| Aortic aneurysm | 15750 (0·22) | 11699 (0·89) | 3526 (0·06) | 273 (0·23) | 35 (0·04) | 217 (0·20) |
| Other cardiovascular diseases | 790168 (11·13) | 151511 (11·54) | 600103 (10·96) | 14570 (12·15) | 7794 (9·67) | 16190 (14·57) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Highest diagnostic institutions | ||||||
| Village clinics | 1302619 (18·34) | 162073 (12·35) | 1086865 (19·84) | 29283 (24·42) | 8924 (11·07) | 15474 (13·93) |
| Primary institutions | 3024159 (42·58) | 530942 (40·44) | 2378482 (43·42) | 47212 (39·38) | 25749 (31·96) | 41774 (37·59) |
| Secondary institutions | 1892106 (26·64) | 592140 (45·10) | 1208397 (22·06) | 27050 (22·56) | 37982 (47·14) | 26537 (23·88) |
| Tertiary institutions | 489988 (6·90) | 20685 (1·58) | 453089 (8·27) | 8919 (7·44) | 1263 (1·57) | 6032 (5·43) |
| Other institutions | 41330 (0·58) | 5201 (0·40) | 28031 (0·51) | 720 (0·60) | 2083 (2·59) | 5295 (4·77) |
| Undiagnosed | 351669 (4·95) | 1809 (0·14) | 322563 (5·89) | 6712 (5·60) | 4577 (5·68) | 16008 (14·41) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
| Highest diagnosis basis | ||||||
| Autopsy | 3610 (0·05) | 398 (0·03) | 1598 (0·03) | 152 (0·13) | 14 (0·02) | 1448 (1·30) |
| Pathology | 29138 (0·41) | 4316 (0·33) | 23652 (0·43) | 474 (0·40) | 199 (0·25) | 497 (0·45) |
| Surgery | 33918 (0·48) | 14113 (1·07) | 18637 (0·34) | 405 (0·34) | 285 (0·35) | 478 (0·43) |
| Clinical and physicochemical examination | 4391504 (61·84) | 949831 (72·35) | 3290991 (60·08) | 54386 (45·36) | 50416 (62·57) | 45880 (41·29) |
| Clinical examination | 1918375 (27·01) | 310917 (23·68) | 1523166 (27·81) | 39602 (33·03) | 17065 (21·18) | 27625 (24·86) |
| Diagnosis after death | 670670 (9·44) | 30382 (2·31) | 574711 (10·49) | 23889 (19·92) | 11994 (14·88) | 29694 (26·72) |
| Other ways | 54656 (0·77) | 2893 (0·22) | 44672 (0·82) | 988 (0·82) | 605 (0·75) | 5498 (4·95) |
| P for difference | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 | <0·001 |
Region: Western: Inner Mongolia, Guangxi, Chongqing, Sichuan, Guizhou, Yunnan, Tibet, Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang; Central: Shanxi, Jilin, Heilongjiang, Anhui, Jiangxi, Henan, Hubei, Hunan; Eastern: Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan.
P for difference: We used χ2 test to compare the differences of characteristics distribution among nominal categories
P for trend: We used logistic regression to test the trends of characteristics distribution for ordered variables.
Figure 1.
Percentage of POD distribution among CVD deaths from NMSS in China, by sex.
(A) Percentage of POD among CVD deaths in China, 2008-2020; (B) Percentage of POD among CVD deaths in China, by age, 2020; (C) Percentage of POD among CVD deaths in China, by CVD subcategories, 2020; (D) Percentage of POD among CVD deaths in China, by province, 2020.
Figure 2.
Percentage of POD distribution among CVD deaths from NMSS in China, by rurality status.
(A) Percentage of POD among CVD deaths in China, 2008-2020; (B) Percentage of POD among CVD deaths in China, by age, 2020; (C) Percentage of POD among CVD deaths in China, by CVD subcategories, 2020; (D) Percentage of POD among CVD deaths in China, by province, 2020.
Associated factors of hospital CVD deaths
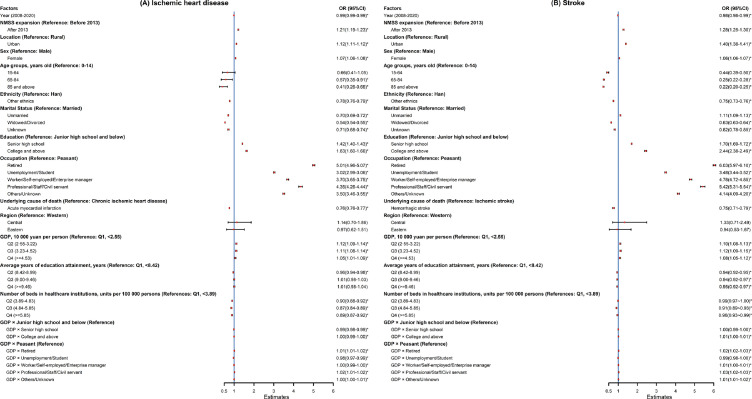
During 2008-2020, multilevel modelling results demonstrated that differences of demographics (age, sex, ethnicity, marital status) and individual SES (education, occupation) substantially contributed to explain 33·88% of spatial variations among hospital CVD deaths below province scale when compared Model 1 with Model 3 (Table 2), meanwhile, the result of MOR of Model 3 (1·73, greater than 1) also indicated significant regional variations and helped to explain individual differences in POD. In Model 5, 29·95% of the variation (the MOR was 1·76) were explained by both individual factors and contextual factors like GDP, average years of education attainment and number of beds in healthcare institutions locally. Specifically, CVD patients who were female (OR: 1·08, 95%CI:1·07-1·08), with higher level of education attainment (OR: 1·92, 95%CI: 1·90-1·95), the retired personnel (OR: 5·62, 95%CI:5·58-5·66), died of AA (OR: 7·03, 95%CI:6·73-7·34), lived in the central areas of the country (OR: 1·26, 95%CI: 0·73-2·20) have higher probability of dying in hospitals compared with their counterparts. Besides, the probability of hospital CVD deaths was lower among those unmarried (OR: 0·90, 95%CI: 0·89-0·91) and widowed/divorced (OR: 0·59, 95%CI: 0·58-0·59) population compared with the married, and ethnic minorities (OR: 0·74, 95%CI:0·73-0·75) were also estimated to have lower odds of dying in hospitals. In Model 6, a comparatively higher level of GDP was estimated to still positively associated with hospital CVD deaths, and this relationship was increased by adding up individual SES (GDP at its Q2 increased from OR: 1·12, 95%CI:1·11-1·14 to OR: 1·14, 95%CI:1·12-1·15). Besides, all models also examined a nearly unchanged odds (OR: 0·99, 95%CI:0·98-1·00) of hospital CVD deaths nationally over time, and NMSS expansion in 2013 increased the probability of reporting hospital deaths (OR: 1·22, 95%CI: 1·21-1·24). Additionally, we used Model 6 to further explore the associations between factors and hospital IHD and stroke deaths (Figure 3), and the magnitude of correlations was estimated to be similar with that of total CVD deaths. Compared with CIHD and IS patients, AMI (OR: 0·76, 95%CI: 0·76-0·77) and HS (OR: 0·75, 95%CI: 0·71-0·79) patients have lower odds of dying in hospitals.
Table 2.
Associated factors of hospital CVD deaths from NMSS in China, 2008-2020: estimated from multilevel logistics regression
| Factors | Model 1 OR (95%CI) | Model 2 OR (95%CI) | Model 3 OR (95%CI) | Model 4 OR (95%CI) | Model 5 OR (95%CI) | Model 6 OR (95%CI) |
|---|---|---|---|---|---|---|
| Fixed effect | ||||||
| Constant | 0·20 (0·16-0·26) * | 0·32 (0·25-0·40) * | 0·17 (0·14-0·21) * | 0·15 (0·12-0·18) * | 0·14 (0·10-0·19) * | 0·14 (0·10-0·20) * |
| Year (2008-2020) | – | 0·99 (0·99-1·00) * | 0·99 (0·98-1·00) * | 0·99 (0·99-0·99) * | 0·99 (0·99-1·00) * | 0·99 (0·98-1·00) * |
| NMSS expansion (Reference: Before 2013) | ||||||
| After 2013 | – | 1·14 (1·13-1·15) * | 1·20 (1·19-1·21) * | 1·20 (1·19-1·21) * | 1·22 (1·20-1·23) * | 1·22 (1·21-1·24) * |
| Location (Reference: Rural) | ||||||
| Urban | – | 2·40 (2·38-2·41) * | 1·24 (1·24-1·25) * | 1·24 (1·23-1·25) * | 1·24 (1·23-1·25) * | 1·24 (1·23-1·25) * |
| Sex (Reference: Male) | ||||||
| Female | – | 0·94 (0·94-0·95) * | 1·08 (1·07-1·08) * | 1·08 (1·07-1·08) * | 1·08 (1·07-1·08) * | 1·08 (1·07-1·08) * |
| Age groups, years old (Reference: 0-14) | ||||||
| 15-64 | – | 0·18 (0·17-0·19) * | 0·40 (0·37-0·43) * | 0·46 (0·43-0·50) * | 0·46 (0·43-0·49) * | 0·46 (0·43-0·49) * |
| 65-84 | – | 0·12 (0·11-0·13) * | 0·27 (0·25-0·29) * | 0·31 (0·29-0·33) * | 0·31 (0·29-0·33) * | 0·31 (0·29-0·33) * |
| 85 and above | – | 0·10 (0·09-0·11) * | 0·22 (0·20-0·23) * | 0·25 (0·24-0·27) * | 0·25 (0·24-0·27) * | 0·25 (0·24-0·27) * |
| Ethnicity (Reference: Han) | ||||||
| Other ethnics | – | 0·72 (0·71-0·73) * | 0·74 (0·73-0·75) * | 0·74 (0·74-0·75) * | 0·74 (0·73-0·75) * | 0·74 (0·73-0·75) * |
| Marital Status (Reference: Married) | ||||||
| Unmarried | – | 0·79 (0·78-0·80) * | 0·90 (0·89-0·91) * | 0·90 (0·89-0·91) * | 0·90 (0·89-0·91) * | 0·90 (0·89-0·91) * |
| Widowed/Divorced | – | 0·57 (0·57-0·57) * | 0·58 (0·58-0·59) * | 0·59 (0·58-0·59) * | 0·59 (0·58-0·59) * | 0·59 (0·58-0·59) * |
| Unknown | – | 0·78 (0·76-0·79) * | 0·72 (0·71-0·74) * | 0·73 (0·71-0·74) * | 0·73 (0·71-0·74) * | 0·73 (0·71-0·75) * |
| Education (Reference: Junior high school and below) | ||||||
| Senior high school | – | – | 1·57 (1·56-1·58) * | 1·56 (1·55-1·57) * | 1·56 (1·55-1·57) * | 1·56 (1·55-1·57) * |
| College and above | – | – | 1·94 (1·92-1·97) * | 1·92 (1·90-1·95) * | 1·92 (1·90-1·95) * | 1·92 (1·89-1·95) * |
| Occupation (Reference: Agricultural-related personnel) | ||||||
| Retired | – | – | 5·66 (5·62-5·70) * | 5·62 (5·58-5·66) * | 5·62 (5·58-5·66) * | 5·57 (5·53-5·61) * |
| Unemployment/Student | – | – | 3·21 (3·19-3·24) * | 3·19 (3·17-3·22) * | 3·19 (3·17-3·22) * | 3·21 (3·18-3·23) * |
| Worker/Self-employed/Enterprise manager | – | – | 4·20 (4·16-4·23) * | 4·16 (4·12-4·20) * | 4·16 (4·12-4·20) * | 4·20 (4·17-4·24) * |
| Professional/Staff/Civil servant | – | – | 4·85 (4·79-4·92) * | 4·81 (4·74-4·87) * | 4·81 (4·74-4·87) * | 4·87 (4·81-4·93) * |
| Others/Unknown | – | – | 3·81 (3·78-3·84) * | 3·78 (3·75-3·81) * | 3·79 (3·76-3·82) * | 3·79 (3·75-3·82) * |
| Underlying cause of death (Reference: Rheumatic heart disease) | ||||||
| Hypertensive heart disease | – | – | – | 0·63 (0·62-0·64) * | 0·63 (0·62-0·64) * | 0·63 (0·62-0·65) * |
| Ischemic heart disease | – | – | – | 0·85 (0·84-0·87) * | 0·85 (0·84-0·87) * | 0·85 (0·84-0·87) * |
| Stroke | – | – | – | 0·82 (0·80-0·83) * | 0·82 (0·80-0·83) * | 0·82 (0·80-0·83) * |
| Myocarditis and myocardial disease | – | – | – | 1·17 (1·11-1·23) * | 1·16 (1·11-1·23) * | 1·16 (1·10-1·22) * |
| Aortic aneurysm | – | – | – | 7·02 (6·72-7·34) * | 7·03 (6·73-7·34) * | 7·05 (6·75-7·37) * |
| Other cardiovascular diseases | – | – | – | 0·98 (0·96-1·00) * | 0·98 (0·96-1·00) * | 0·98 (0·96-1·00) * |
| Region (Reference: Western) | ||||||
| Central | – | – | – | – | 1·26 (0·73-2·20) | 1·26 (0·74-2·17) |
| Eastern | – | – | – | – | 0·99 (0·60-1·65) | 0·97 (0·59-1·59) |
| GDP, 10 000 yuan per person (Reference: Q1, <2·55) | ||||||
| Q2 (2·55-3.22) | – | – | – | – | 1·12 (1·11-1·14) * | 1·14 (1·12-1·15) * |
| Q3 (3.23-4.52) | – | – | – | – | 1·11 (1·09-1·13) * | 1·14 (1·12-1·16) * |
| Q4 (>=4.53) | – | – | – | – | 1·06 (1·03-1·08) * | 1·09 (1·07-1·11) * |
| Average years of education attainment, years (Reference: Q1, <8·42) | ||||||
| Q2 (8·42-8·99) | – | – | – | – | 0·96 (0·95-0·97) * | 0·96 (0·95-0·97) * |
| Q3 (9·00-9·46) | – | – | – | – | 0·96 (0·94-0·97) * | 0·96 (0·95-0·98) * |
| Q4 (>=9·46) | – | – | – | – | 0·95 (0·93-0·97) * | 0·96 (0·94-0·98) * |
| Number of beds in healthcare institutions, units per 100 000 persons (References: Q1, <3·89) | ||||||
| Q2 (3·89-4·83) | – | – | – | – | 0·97 (0·95-0·98) * | 0·97 (0·96-0·98) * |
| Q3 (4·84-5·85) | – | – | – | – | 0·90 (0·89-0·92) * | 0·91 (0·89-0·92) * |
| Q4 (>=5·85) | – | – | – | – | 0·95 (0·93-0·97) * | 0·96 (0·94-0·98) * |
| GDP × Junior high school and below (Reference) | ||||||
| GDP × Senior high school | – | – | – | – | – | 1·00 (0·99-1·00) * |
| GDP × College and above | – | – | – | – | – | 1·01 (1·00-1·01) * |
| GDP × Agricultural-related personnel (Reference) | ||||||
| GDP × Retired | – | – | – | – | – | 1·02 (1·02-1·03) * |
| GDP × Unemployment/Student | – | – | – | – | – | 0·99 (0·98-1·00) * |
| GDP × Worker/Self-employed/Enterprise manager | – | – | – | – | – | 1·01 (1·00-1·01) * |
| GDP × Professional/Staff/Civil servant | – | – | – | – | – | 1·03 (1·02-1·03) * |
| GDP × Others/Unknown | – | – | – | – | – | 1·01 (1·01-1·02) * |
| Random effects | ||||||
| Variance among provinces (SE) | 0·50 (0·13) | 0·42 (0·11) | 0·33 (0·09) | 0·33 (0·09) | 0·35 (0·09) | 0·33 (0·09) |
| MOR | 1·96 | 1·85 | 1·73 | 1·73 | 1·76 | 1·74 |
| PCV (%) | 16·61 | 33·88 | 33·32 | 29·95 | 32·80 | |
Abbreviations: OR, odds ratio; CI, confidence interval; Q1, 1st quantile; Q2, 2nd quantile; Q3, 3rd quantile; Q4, 4th quantile; SE, standard error; MOR, median odds ratio; PCV, Proportional change in variance
aP<0·05.
bRegion: Western: Inner Mongolia, Guangxi, Chongqing, Sichuan, Guizhou, Yunnan, Tibet, Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang; Central: Shanxi, Jilin, Heilongjiang, Anhui, Jiangxi, Henan, Hubei, Hunan; Eastern: Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan.
Figure 3.
Associated factors of hospital IHD and stroke deaths in China, 2008-2020: estimated from multilevel logistics regression
(A) Ischemic heart disease; (B) Stroke.
Abbreviations: OR, odds ratio; CI, confidence interval; Q1, 1st quantile; Q2, 2nd quantile; Q3, 3rd quantile; Q4, 4th quantile
a *P<0.05. b Region: Western: Inner Mongolia, Guangxi, Chongqing, Sichuan, Guizhou, Yunnan, Tibet, Shaanxi, Gansu, Qinghai, Ningxia, Xinjiang; Central: Shanxi, Jilin, Heilongjiang, Anhui, Jiangxi, Henan, Hubei, Hunan; Eastern: Beijing, Tianjin, Hebei, Liaoning, Shanghai, Jiangsu, Zhejiang, Fujian, Shandong, Guangdong, Hainan.
Discussion
In this population-based study, by using data from NMSS in China, we demonstrated the distribution of POD among CVD deaths and explored the associated factors of hospital CVD deaths. We found that during 2008-2020, home was the leading POD among CVD deaths, meanwhile, those CVD decedents characterized as the female, the youngest, Han population, the married, the retiree, lived in urban areas, with higher level of SES and died of chronic CVD, were reported to have a higher probability of dying in hospitals than their counterparts.
Home was the leading POD among CVD deaths
During 2008-2020, it was demonstrated that home was the leading POD among CVD deaths (higher than 70%) in China, followed by hospital deaths (lower than 20%), which showed that there were no obvious change of POD distribution in comparison with the 3rd national retrospective COD sample survey from 2004 to 2005 in China, indicating that our study could be regarded as an update information in describing POD pattern during past decade.11,12 However, the findings we concluded were markedly different from those in other developed countries. For example, by using Mortality Multiple Cause-of-Death Public Use Record from Nation Center for Health Statistics in United States (US), Cross6 reported that hospital CVD deaths decreased from 36·5% in 2003 to 27·3% in 2017, which was substantially higher than that in China. Meanwhile, home CVD deaths increased from 21·3% in 2003 to 30·9% in 2017 and thus far below the level in China. Besides, a considerate amount of CVD deaths occurred in nursing facilities (22·7%) and hospice facilities (3·2%) were also reported in US studies, and those results showed large disparities compared with that in China.6 Other than US, it was also found that for chronic conditions occurred in developed countries, like CVD and main cancers, home deaths often occupied nearly a half of total deaths and increased with the time trends gradually, which either showed disparities in contrast with that in China.5,8,26,27 Previous studies have proposed a three-stage evolutionary hypothesis which might be used to interpret those national variations of POD distribution over the past 100 years.4,28 At the first stage, home deaths accounted for more than 90% of all deaths early in 20th century because of limited healthcare resources and underdeveloped medical technologies. Afterwards, the proportion of hospital deaths have steadily increased and skyrocketed to 70% to 80% of all deaths after 1970s among most developed countries mainly due to advancements in medical technologies and accessibility to healthcare services. In recent decades, a leveling off or declining trend in hospital deaths has been observed in US and other western countries as a result of the increase in home deaths because of emphasis on quality of EOL care. According to the hypothesis, most developed countries were in stage 2 or at the beginning of or in a transition from stage 2 to stage 3 depending on the stage of development of palliative care, which could be explained by local socioeconomic development and operating mechanism of health care system that formulate the historical trajectory of POD distribution.4,28
From the perspective of three-stage trajectory of POD distribution, we speculated that China is at its first stage or at the beginning of or in a transition from stage 1 to stage 2, currently. Although a higher level of home deaths at stage 1 was regarded as the offspring of inadequate healthcare resources, the underlying explanations that affected POD distribution in China might be different from other developed countries: First, China is ageing much faster than most of other western countries, the soaring elderly was the target population with increased chronic disease burden, thus their urgent demands for healthcare services have increased.3,29 Second, although both the quantity and quality of healthcare resources have been largely improved at national level, gaps still remained in efficiency of delivery and control of health expenditures among the elderly per capita, the accessibility, availability and affordability of receiving multiple healthcare services largely relied on personal capacity of what they owned for, how they aware of and where they lived in.29 Therefore, the high proportion of home deaths in China was supposed to be associated with counterbalance between substantial population ageing and mismatched healthcare system capacity per capita rather than merely lack of healthcare resources and medical technologies in developed countries. During the following years, with the spread of advanced science and medical technologies and programs of palliative care from developed regions to less developed regions, we speculated that, developing countries like China would be likely to witness a shorter transition period from Stage 1 to Stage 2 and a relatively lower proportion of hospital deaths than the level that developed countries ever had, especially for those regions where the home death is culturally favorable.4
Associated factors of hospital CVD deaths
In order to make it clear to promote rationale allocation of healthcare services at the end stage of life, we have identified associated factors of hospital CVD deaths at both individual and provincial level. Overall, individual factors explained nearly half of the interprovincial differences of hospital CVD deaths, while socioeconomic contextual factors did not explain much of the differences.
At individual level, we found that demographics were associated with hospital CVD deaths, which included sex, age, marital status and ethnic group. Female was observed to have higher odds of dying in hospitals, one reasonable explanation was that they have longer life expectancy than male. Usually, the elderly men live more often in a multi-person household possibly together with a younger female partner. In contrast, the elderly women more often survive their spouses or stay divorced. We thus hypothesized that the elderly men often continue to live at their home even when their health status is getting worse and healthcare is needed, whereas the single elderly women with similar health status are more inclined to receive medical treatment in hospitals.30 For age disparities, we speculated that it may be related to the disease characteristics among children, for most of them suffered from congenital diseases that required to receive timely medical treatment. In spite of this, the higher odds of hospital CVD deaths of children was largely explained by the family-based culture and social structure in China: Children's health is not only highly valued by family members, but also can drive the family's choice of healthcare services and mobilize various resources to receive higher quality medical treatment.31 While most of the elderly have the consciousness of returning to their roots and hope to spend their EOL at their hometown, and choose to die at home.32 Compared with unmarried population, the relatively higher odds of hospital CVD deaths of married ones may be explained by having the continuous family support.30,32 Ethnic group was also reported to have lower probability of hospital CVD deaths which might be related to their cultural background and social custom. For example, some population of ethnic minorities refused to die in hospitals, which may help to explain relative 5.94-9.05% hospital deaths in Yunnan, which have more than 10% of Yi population.33
Apart from demographics, education attainment, occupation and place of residence could be regarded as specific dimensions of social stratification, and hospital CVD deaths presented a gradient situation based on this social stratification. Concepts of Social Gradient in Health Outcome was thus introduced to interpret the rules of such feature: social stratification rooted by personal SES considered that the higher of SES, the more probability of dying in hospitals, and it could be explained by their awareness, capacity and accessibility to receive adequate medical services.32 Notably, although China is a large agricultural country, agricultural-related individuals having the lowest odds of dying in hospitals compared with other groups, which reminded us to focus on utilization of healthcare service resources among disadvantaged group without decent level of SES. However, on the contrary, a review by Mette34 pointed out that people with higher levels of social deprivation in western countries were more likely to die in hospitals, and studies by Berger35 and Bruera36 also concluded that people with lower education levels, lack of social support and care were more likely to die in hospital. Although researches at home and abroad have reached opposite conclusions, the mechanism may theoretically be the same: In most of cultural backgrounds, people tend to spend their EOL in a place where they are relatively safe, comfortable and could receive good care.4
POD distribution was also affected by the nature of the disease. Compared with CIHD and IS, AMI and HS patients have lower odds of dying in hospitals. Related studies have proved those findings, as CVD with chronic and irregular progression generally leave patients time to choose POD, probably in hospitals· But for patients with sudden cardiac events, they may die at home or on the way to hospitals due to lack of time for emergency treatment.32,37,38 A lower odds of hospital CVD deaths with insufficient prehospital care like low rate of cardiopulmonary resuscitation still remained a widespread problem with little improvement, especially in rural areas.3,39, 40, 41 Efforts are urgently needed to improve the provision of prehospital care such as the introduction and practice of chest-pain centers across the country.3,40,41 Besides, it is also the necessities to improve CVD treatment and timely emergency through elevating the capacity of medical professionals, healthcare resource, socially supportive environment, and public awareness of first-aid either at the home or in communities.
Further, we have identified significant spatial variations of hospital CVD deaths across provinces· For developed provinces like Beijing and Shanghai, they have implemented community-based hospice care system with all community health centers provided hospice care services, and this measure were probability related to greatest capacity of deal with severe CVDs patients with surgical services and increased the odds of dying in hospitals.42 Hubei, similarly, also has top hospitals with first-class CVDs services in China and has a relatively higher odds of hospital deaths. On the contrary, among developing areas, the relatively lower odds of hospital CVD deaths were related to limited healthcare resources and underdeveloped medical technologies. But for some of the ethnic minorities like Yi population in Yunnan, the lower probability of hospital CVD deaths was affected by cultural background and traditional custom which we mentioned before.33 However, things were not always the case in certain special provinces. For some developed areas like Jiangsu and Zhejiang which presented lower odds of hospital deaths, we speculated that it may related to cultural beliefs, personal preferences and relevant policies.43 For some developing areas showed comparatively higher odds of hospital deaths like Heilongjiang, Jilin, Liaoning and Inner Mongolia, since there were no obvious associations between POD distribution and specific spectrum of CVDs, there was still lack of comprehensive explanations to unveil the reasons. Therefore, in the near future, we suggested to conduct studies on characteristic province-specific POD distribution to acquire in-depth understanding of its spatial variations in China. Additionally, this study have pointed out that the interactions between factors at regional level and individual level could help to identify how individual factors modified regional factors on health outcomes, namely background effects.23,24,44 Therefore, we found that individual factors have strengthen the magnitude of effects socioeconomic contextual factors exerted on hospital CVD deaths, in other words, individuals with higher SES who also lived in areas with higher socioeconomic development conditions were more inclined to die in hospitals, which also confirmed the previous findings in this study.
Implications
Current characteristics of POD distribution among CVD deaths might be an interplay between multiple factors. As the most populous country worldwide facing population ageing, especially deeply embed in a core value of Confucianism which advocate moral injunctions of loyalty and filial piety to one's parents, brothers and friends in Chinese culture, we supposed that, home deaths might sustain its unchanged patterns in the near future, and the individual level factors would remain the largest contributor of its variations.6,35,45,53 Therefore, we suggested that, first, expanding medical and healthcare capacities, elevating efficiency and effectiveness of clinical interventions should be the priorities, especially for acute and severe CVD patients. Second, substantial provincial variations of POD distribution indicated the disparities existed in medical and healthcare resources allocation, which making the requests of tailoring regional-specific strategies to bridge the gap between provinces and urban/rural areas. Third, personalized humanistic care should be provided for those ethnic groups in accordance with their cultural belief, and various options and additional supports should be developed to those vulnerable population with lower SES for accessible and affordable healthcare services. Finally, enabling the concept of filial piety to establish an integrity of clinical care and community- or home-based care to formulate long-term care system that supports informal care.
Strengths and limitations
A strength was that NMSS was designed to achieve national and provincial representativeness under a unified procedure that assumed validity and reliability.15 To our knowledge, this was the first study to demonstrate the trends of POD distribution among CVD patients in China. Meanwhile, the usage of multilevel analysis facilitated the study to demonstrate the spatial variations of hospital CVD deaths and interpret the contributions of individual and regional level factors to those variations.46,47 However, there were still some limitations: we failed to include potential factors that might influence hospital CVD deaths, such as personal preference,30,47, 48, 49, 50 distance to hospitals,45,51,52 family care and social support.32,45,50 Therefore, it was necessary to collect adequate relevant information affecting POD and conduct reclassification on the basis of exploration standards.32,45
Conclusion
In China, home was the leading POD among CVD patients, demographics and individual SES were important factors associated with hospital CVD deaths rather than socioeconomic contextual factors. Providing accessible and available of healthcare services were priorities to improve quality of EOL among CVD deaths, significant variations among provinces and sub-population reminded us of the requirements for equal healthcare resources allocation and multiple options for minorities. Suggestions for POD decision and improving quality of end-of-life care among CVD patients requires a wide range of involvement from different stakeholders, and those experiences should be evaluated and could be generalized to other developing countries.53
Declaration of interests
This research was supported by the National Key Research & Development Program of China (grant number 2018YFC1315301). The funders of the study have no role in study design, data collection, data analysis, data interpretation, or writing of the report. Thus, there are no conflicts of interest to declare.
Acknowledgments
Contributors
MZ had full access to all the data in the study and take responsibility for the integrity of the data and the accuracy of the data analysis. MZ and WW conceived and designed the study. All authors acquired, analyzed, or interpreted data. WW drafted the manuscript. MZ, YH, PYe and YL critically revised the manuscript for intellectual content. WW and YL statistically analyzed the data. MZ, LW and PYin obtained funding. MZ, LW, PYin, YL, JL, JQ, JY, LL provided administrative, technical, or material support. MZ and YH supervised the study.
Acknowledgements
The authors thank all involved provincial and local health administrative departments, and local centers for disease control and prevention for their participation and contributions.
Ethics approval and consent participate
The ethic committee at the Chinese Center for Disease Control and Prevention approved this study. All study procedures involving human subjects conformed to the ethical standards of the ethics committee of the Chinese Center for Disease Control and Prevention and the 1964 Helsinki Declaration and its subsequent amendments or similar ethical standards. As mortality data we used in this study was aggregated data derived from National Mortality Surveillance System hosted in Chinese Center for Disease Control and Prevention, and we have no access to information that could identify individual participants, so our research did not involve patients' personal information and written informed consent was waived by the ethics committee of the Chinese Center for Disease Control and Prevention.
Data sharing statement
The datasets generated and/or analyzed during the current study are not publicly available due to data sharing regulations established by the Chinese Center for Disease Control and Prevention on National Mortality Surveillance System, but are available from the corresponding authors on reasonable request.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100383.
Appendix. Supplementary materials
References
- 1.National Center for Cardiovascular Diseases, China . Encyclopedia of China Publishing House; Beijing: 2019. Report on Cardiovascular Diseases in China 2018. [Google Scholar]
- 2.Institution of Health Metrics and Evaluation. GBD results tool [EB/OL]. http://ghdx.healthdata.org/gbd-results-tool. Accessed 8 December 2021
- 3.Zhao D, Liu J, Wang M, Zhang X, Zhou M. Epidemiology of cardiovascular disease in China: Current features and implications. Nat Rev Cardiol. 2019;16(4):203–212. doi: 10.1038/s41569-018-0119-4. [DOI] [PubMed] [Google Scholar]
- 4.Danan G, Guangya L, Denese AV, Zeng Y. Factors associated with place of death among the Chinese oldest old. J Appl Gerontol. 2007;26(1):34–57. [Google Scholar]
- 5.Gao W, Ho YK, Verne J, Glickman M, Higginson IJ. Changing patterns in place of cancer death in England: A population-based study. PloS Med. 2013;10(3) doi: 10.1371/journal.pmed.1001410. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Cross SH, Kaufman BG, Mentz RJ, Kamal AH, Taylor DJ, Warraich HJ. Trends in place of death for individuals with cardiovascular disease in the United States. J Am Coll Cardiol. 2019;74(15):1943–1946. doi: 10.1016/j.jacc.2019.08.1015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reed J. Place of death preference among people with dementia: An important conversation. Evid Based Nurs. 2019 doi: 10.1136/ebnurs-2019-103163. [DOI] [PubMed] [Google Scholar]
- 8.Feudtner C, Feinstein JA, Satchell M, Zhao H, Kang TI. Shifting place of death among children with complex chronic conditions in the United States, 1989-2003. JAMA. 2007;297(24):2725–2732. doi: 10.1001/jama.297.24.2725. [DOI] [PubMed] [Google Scholar]
- 9.Gomes B, Higginson IJ. Factors influencing death at home in terminally ill patients with cancer: Systematic review. BMJ. 2006;332(7540):515–521. doi: 10.1136/bmj.38740.614954.55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cross SH, Warraich HJ. Changes in the place of death in the United States. N Engl J Med. 2019;381(24):2369–2370. doi: 10.1056/NEJMc1911892. [DOI] [PubMed] [Google Scholar]
- 11.Zhou M, Yang G. Factors associated with place of death in China. Disease Surveillance. 2009;24(05):382–385. [Google Scholar]
- 12.Zhou M. Chinese Center for Disease Control and Prevention; 2009. Establishment and Validation of the model of Estimating Population Cause-Specific Mortality Fractions from in-Hospital Mortality. [Thesis] [Google Scholar]
- 13.Jiang S, Wu B, Yu X. Analysis of place of death among urban and rural residents with cardiovascular disease in China. Chinese Journal of Health Statistics. 2020;37(03):448–451. [Google Scholar]
- 14.Li Z, Jiang S, Xu C, et al. Determinants of place of death for end-stage cancer patients: Evidence from China. Int J Qual Health Care. 2020;32(1):41–47. doi: 10.1093/intqhc/mzz064. [DOI] [PubMed] [Google Scholar]
- 15.Liu S, Wu X, Lopez AD, et al. An integrated national mortality surveillance system for death registration and mortality surveillance. China. Bull World Health Organ. 2016;94(1):46–57. doi: 10.2471/BLT.15.153148. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.National Center of Chronic and Noncommunicable Disease Control and Prevention . Science and Technology Press of China; Beijing: 2019. Chinese Center for Disease Control and Prevention, National Health Statistics Information Center, National Health Commission. China Mortality Surveillance Yearbook; p. 2020. [Google Scholar]
- 17.Chino F, Kamal AH, Leblanc TW, SY Zafar, Suneja G, Chino JP. Place of death for patients with cancer in the United States, 1999 through 2015: Racial, age, and geographic disparities. Cancer-Am Cancer Soc. 2018;124(22):4408–4419. doi: 10.1002/cncr.31737. [DOI] [PubMed] [Google Scholar]
- 18.World Health Organization. Making choices in health: WHO guide to cost-effectiveness analysis. Geneva: 2003.
- 19.Merlo J, Chaix B, Ohlsson H, et al. A brief conceptual tutorial of multilevel analysis in social epidemiology: Using measures of clustering in multilevel logistic regression to investigate contextual phenomena. J Epidemiol Community Health. 2006;60(4):290–297. doi: 10.1136/jech.2004.029454. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Li Y. Chinese Center for Disease Control and Prevention; 2016. Multilevel spatial analysis of hypertension prevalence, awareness, treatment and control in China. [Thesis] [Google Scholar]
- 21.Merlo J, Chaix B, Yang M, Lynch J, Rastam L. A brief conceptual tutorial of multilevel analysis in social epidemiology: Linking the statistical concept of clustering to the idea of contextual phenomenon. J Epidemiol Community Health. 2005;59(6):443–449. doi: 10.1136/jech.2004.023473. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yang M, Li X. Peking University Medical Press; Beijing: 2007. Multilevel statistical models in medical and public health research. [Google Scholar]
- 23.Chuang YC, Li YS, Wu YH, Chao HJ. A multilevel analysis of neighborhood and individual effects on individual smoking and drinking in Taiwan. BMC Public Health. 2007;7:151. doi: 10.1186/1471-2458-7-151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Diez-Roux AV, Link BG, Northridge ME. A multilevel analysis of income inequality and cardiovascular disease risk factors. Soc Sci Med. 2000;50(5):673–687. doi: 10.1016/s0277-9536(99)00320-2. [DOI] [PubMed] [Google Scholar]
- 25.SAS Institute Inc . second edition. SAS Institute Inc; Cary, NC, USA: 2016. SAS SHARE User'S guide. [Google Scholar]
- 26.Cross SH, Ely EW, Kavalieratos D, Tulsky JA, Warraich HJ. Place of death for individuals with chronic lung disease: Trends and associated factors from 2003 to 2017 in the United States. Chest. 2020;158(2):670–680. doi: 10.1016/j.chest.2020.02.062. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Costa V, Earle CC, Esplen MJ, et al. The determinants of home and nursing home death: A systematic review and meta-analysis. BMC Palliat Care. 2016;15:8. doi: 10.1186/s12904-016-0077-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Tang ST, Mccorkle R. Determinants of place of death for terminal cancer patients. Cancer Invest. 2001;19(2):165–180. doi: 10.1081/cnv-100000151. [DOI] [PubMed] [Google Scholar]
- 29.Yip W, Fu H, Chen AT, et al. 10 years of health-care reform in China: Progress and gaps in Universal Health Coverage. Lancet. 2019;394(10204):1192–1204. doi: 10.1016/S0140-6736(19)32136-1. [DOI] [PubMed] [Google Scholar]
- 30.Hedinger D, Braun J, Zellweger U, Kaplan V, Bopp M. Moving to and dying in a nursing home depends not only on health - an analysis of socio-demographic determinants of place of death in Switzerland. PloS One. 2014;9(11) doi: 10.1371/journal.pone.0113236. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yuan Z, Gao L. The social ladder and cultural choice of medicalization of death: A analysis for place of death in a city of Yunnan Province, 2009-2014. Soc Sci Beijing. 2018;(01):86–93. [Google Scholar]
- 32.Zhou M, Yang G. Progress in research for associated factors of place of death. Chin J Prev Med. 2009;(06):535–537. [Google Scholar]
- 33.Jazz Mujeer. On the liangshan yi's traditional practice of hospice care. Journal of Social Sciences. 2007;(9):124–128. [Google Scholar]
- 34.Mette AN, Anne HB, Marianne HS, Mette KN. What socio-economic factors determine place of death for people with life-limiting illness? A systematic review and appraisal of methodological rigour. Palliative Med. 2019;33(8) doi: 10.1177/0269216319847089. [DOI] [PubMed] [Google Scholar]
- 35.Berger A, Pereira D, Baker K, O'Mara A, Bolle J. A commentary: Social and cultural determinants of end-of-life care for elderly persons. Gerontologist. 2002:49–53. doi: 10.1093/geront/42.suppl_3.49. 42 Spec No 3. [DOI] [PubMed] [Google Scholar]
- 36.Bruera E, Russell N, Sweeney C, Fisch M, Palmer JL. Place of death and its predictors for local patients registered at a comprehensive cancer center. J Clin Oncol. 2002;20:2127–2133. doi: 10.1200/JCO.2002.08.138. [DOI] [PubMed] [Google Scholar]
- 37.Hayashi M, Shimizu W, Albert CM. The spectrum of epidemiology underlying sudden cardiac death. Circ Res. 2015;116(12):1887–1906. doi: 10.1161/CIRCRESAHA.116.304521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Poole JE, Prutkin JM. Subcutaneous implantable Cardioverter-Defibrillator finding a place in sudden cardiac death prevention: Emerging or emerged? J Am Coll Cardiol. 2017;70(7):842–844. doi: 10.1016/j.jacc.2017.06.055. [DOI] [PubMed] [Google Scholar]
- 39.Gao Y, Su J, Wei Z, Liu J, Wang J. Characteristics of out-of-hospital acute coronary heart disease deaths of Beijing permanent residents at the age of 25 or more from 2007 to 2009. Chinese Journal of Cardiology. 2012 [PubMed] [Google Scholar]
- 40.Shao F, Li CS, Liang LR, Li D, Ma SK. Outcome of out-of-hospital cardiac arrests in Beijing. China. Resuscitation. 2014;85(11):1411–1417. doi: 10.1016/j.resuscitation.2014.08.008. [DOI] [PubMed] [Google Scholar]
- 41.Fan F, Li Y, Zhang Y, et al. Chest pain center accreditation is associated with improved In-Hospital outcomes of acute myocardial infarction patients in China: Findings from the CCC-ACS project. J Am Heart Assoc. 2019;8(21) doi: 10.1161/JAHA.119.013384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhou M, Wang H, Zeng X, et al. Mortality, morbidity, and risk factors in China and its provinces, 1990-2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet. 2019;394(10204):1145–1158. doi: 10.1016/S0140-6736(19)30427-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Broad JB, Gott M, Kim H, Boyd M, Chen H, Connolly MJ. Where do people die? An international comparison of the percentage of deaths occurring in hospital and residential aged care settings in 45 populations, using published and available statistics. Int J Public Health. 2013;58(2):257–267. doi: 10.1007/s00038-012-0394-5. [DOI] [PubMed] [Google Scholar]
- 44.He L, Shi X, Hu Y. Progress of study on regional socioeconomic level and cardiovascular disease. Chin J Publ Heal. 2014;(7):936–939. [Google Scholar]
- 45.Gao W, Chukwusa E, Verne J, Yu P, Polato G, Higginson IJ. NIHR Journals Library; Southampton (UK): 2019. The role of service factors on variations in place of death: An observational study. [PubMed] [Google Scholar]
- 46.Li Y, Wang L, Feng X, et al. Geographical variations in hypertension prevalence, awareness, treatment and control in China: Findings from a nationwide and provincially representative survey. J Hypertens. 2018;36(1):178–187. doi: 10.1097/HJH.0000000000001531. [DOI] [PubMed] [Google Scholar]
- 47.Ali M, Capel M, Jones G, Gazi T. The importance of identifying preferred place of death. BMJ Support Palliat Care. 2019;9(1):84–91. doi: 10.1136/bmjspcare-2015-000878. [DOI] [PubMed] [Google Scholar]
- 48.Evans R, Finucane A, Vanhegan L, Arnold E, Oxenham D. Do place-of-death preferences for patients receiving specialist palliative care change over time? Int J Palliat Nurs. 2014;20(12):579–583. doi: 10.12968/ijpn.2014.20.12.579. [DOI] [PubMed] [Google Scholar]
- 49.Tan WS, Bajpai R, Low CK, Ho A, Wu HY, Car J. Individual, clinical and system factors associated with the place of death: A linked national database study. PloS One. 2019;14(4) doi: 10.1371/journal.pone.0215566. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Gomes B, Calanzani N, Gysels M, Hall S, Higginson IJ. Heterogeneity and changes in preferences for dying at home: A systematic review. BMC Palliat Care. 2013;12:7. doi: 10.1186/1472-684X-12-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kalseth J, Halvorsen T. Relationship of place of death with care capacity and accessibility: A multilevel population study of system effects on place of death in Norway. BMC Health Serv Res. 2020;20(1):454. doi: 10.1186/s12913-020-05283-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Chukwusa E, Yu P, Verne J, Taylor R, Higginson IJ, Wei G. Regional variations in geographic access to inpatient hospices and Place of death: A Population-based study in England. UK. PloS One. 2020;15(4) doi: 10.1371/journal.pone.0231666. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.World Health Organization. China country assessment report on ageing and health. Geneva: 2016.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.