Summary
Background
Tobacco dependence is the key barrier to successful smoking cessation. However, little is known about its prevalence, sociodemographic characteristics and determinants. We aimed to estimate the prevalence, associated factors and burden of tobacco dependence in China.
Methods
During 2018–2019, the nationally representative 2018 China Health Literacy Survey (2018 CHLS) invited 87,708 participants to participate using a multistage stratified sampling method from 31 provinces (or equivalent) in mainland China, and 84,839 participants aged 20–69 with valid data were included in the analysis. We diagnosed tobacco dependence based on international criteria (ICD-10, DSM-4) and tailored to Chinese population according to China Clinical Guideline for Tobacco Cessation (2015 version). The prevalence of tobacco dependence was estimated overall and by sociodemographic factors. The Logistic regression was conducted to estimate odds ratios (OR) and 95% confidence intervals (CIs) for tobacco dependence and success of smoking cessation (being ex-smokers), with different levels of adjustment. These were used to estimate the total number of adults who were tobacco dependent in China.
Findings
In China, the estimated prevalence of current smoking was 25.1%, significantly higher in men than in women (47.6% vs 1.9%). The prevalence of current smoking varied approximately 3-fold (12.9% to 37.9%) across 31 provinces of China. Among general population aged 20–69 years, the prevalence of tobacco dependence was 13.1% (95% CI:12.2–14.1). Among current smokers, the prevalence of tobacco dependence was 49.7% (46.5–52.9%), with no difference between men and women (49.7% vs 50.8%). The prevalence of tobacco dependence was associated significantly with smoking intensity, defined by pack-years (1.62 [1.54–1.70] per 10 pack-years), cigarettes smoked per day (2.01 [1.78, 2.27] per 10 cigarettes), and smoking starting age (0.93 [0.90, 0.97] per 5 years). Given smoking intensity, the prevalence of tobacco dependence also varied by age, gender, certain socioeconomic status and regions. Compared with those without tobacco dependence, ever smokers with tobacco dependence were less likely to be ex-smokers (2.88, 2.59–3.21). In China, 183.5 (170.4–197.4) million adults (177.5 million were men) were tobacco dependent in 2018.
Interpretation
In China, tobacco dependence is highly prevalent, with approximately half of current smokers being addictive, highlighting the need for coordinated effort to improve awareness, diagnosis and treatment of tobacco dependence.
Funding
Chinese Academy of Medical Sciences (CAMS) Initiative for Innovative Medicine (CAMS 2021-I2M-1-010), National Key R&D Program of China (grant no 2017YFC1309400), and National Natural Science Foundation of China (grant no 81720108001).
Note
Chinese translation of abstract is available in appendix section.
Keywords: Tobacco dependence, Smoking, Prevalence, Associated factors
Research in context.
Evidence before this study
We searched PubMed and the China National Knowledge Infrastructure database for articles published up to March 31, 2020 using the terms “nicotine dependence”, “tobacco dependence”, “nicotine addiction”, “tobacco addiction”, “prevalence”, “epidemiology”, and “China”. We screened papers by reviewing abstracts to identify full-text reports that were relevant to the study aims. As a result, we found that the prevalence of nicotine dependence has been reported in studies from mostly Caucasians populations. Due to the use of these different criteria, the prevalence reported varied greatly, ranging from 22% to 69% across different studies. In China, no national data on nicotine dependence is available, with only several small epidemiological studies reporting the prevalence of this condition.
Added value of this study
To the best of our knowledge, this is the first and largest study to estimate the prevalence, associated factors, and burden of nicotine dependence in a nationally-representative sample of Chinese adult population and elsewhere. Our data indicated that approximately half of current smokers in both men and women had nicotine dependence. Apart from certain smoking characteristics (eg, younger age of initiation, heavy smokers), a number of sociodemographic factors (eg younger age, low socioeconomic status) were also associated with higher risk of being nicotine-dependent. Moreover, those with nicotine dependence were less likely to initiate quitting or to successfully quit smoking. Overall, in China, we estimated that 183.5 million adults in China, involving predominantly men, had nicotine dependence, with large variations across different areas of China. Given the neglected situation of nicotine dependence globally, we call for global coordinated effort to improve awareness, diagnosis and treatment of nicotine dependence.
Implications of all the available evidence
This present study estimated that 183.5 million Chinese current smokers had nicotine dependence, which is comparable with the numbers affected by non-communicable diseases such as heart disease, stroke, cancer, chronic respiratory diseases and diabetes in China. Considering the high prevalence and addictive nature of nicotine dependence, intensive and individualized treatment, such as pharmacological treatment of nicotine dependence, should be timely and effectively integrated into current tobacco control programmes. If the present course remains unchanged, in the near future, China and the world will face more severe challenge of epidemic proportions caused by nicotine dependence.
Alt-text: Unlabelled box
Introduction
Tobacco use is a significant threat to human health and social development, causing an estimated about 8 million annual deaths worldwide from a wide range of chronic non-communicable diseases.1 China, which accounts for ∼20% of the world population, now consumes >40% of the world's total cigarettes,2 with more than one million annual deaths from tobacco, involving mainly men.3
Although an increasing proportion of smokers are aware of the health risk of smoking and would like to quit, stopping smoking is difficult chiefly due to tobacco dependence.4 Tobacco dependence is a complex condition involving physiological, psychological, and behavioral processes, and is considered a mental disorder by the International Classification of Diseases (ICD).5 It is one of the main reasons for long-term tobacco smoking. Moreover, dependent smokers are more likely to have tobacco withdrawal symptoms when trying to quit or cut down on tobacco, which makes quitting tobacco more difficult. Although the prevalence of smoking has decreased globally, in the future, smokers might have higher dependence, as those who have difficulty quitting may remain smokers.
Despite its importance, tobacco dependence is largely ignored, both in clinical practice and in scientific studies. A better understanding of the prevalence and determinants of tobacco dependence in China and elsewhere is vital for facilitating the development and implementation of effective tobacco control strategies. Currently, several instruments have been developed to assess tobacco dependence. Amongst these, the Fagerström Test for Tobacco dependence (FTND)6 is the most widely used, compared to ICD-10,7 Diagnostic and Statistical Manual of Mental Disorders,8 Heaviness of Smoking Index (HSI),9 and Nicotine Dependence Syndrome Scale.10 Due to the use of these different instruments, the reported prevalence of tobacco dependence in current smokers varies greatly, ranging from 22% to 69% across different studies.11, 12, 13, 14, 15, 16, 17, 18, 19 In China, no national data on tobacco dependence is available, with only several small epidemiological studies reporting the prevalence of this condition.12,14
To help fill the evidence gap, we report the findings from a large nationally-representative survey, the 2018 China Health Literacy Survey (CHLS). The present study aimed to (1) estimate the prevalence of tobacco dependence, both overall and in specific population subgroups; (2) assess the determinants of tobacco dependence and failure of smoking cessation; and (3) estimate the burden of tobacco dependence in China.
Methods
Study population
The China Health Literacy Survey (CHLS) is a nationally-representative household survey of non-institutionalized men and women aged 15 to 69 years old. Since 2012, a total of six waves of CHLS have been conducted.20, 21, 22, 23 In the 2018 CHLS, questionnaires regarding smoking behaviors and tobacco dependence were included for the first time, which provided a unique opportunity to estimate the prevalence and associated factors of tobacco dependence in China (study protocol).
In brief, the 2018 CRHLS study covered 31 provinces, autonomous regions, and municipalities in China. All the permanent residents (i.e., those living in their current residence for 1 year or longer) in the selected study areas were invited to participate. We only included permanent residents aged 15–69 years old (those living in their current residence for 1 year or longer) in the sampling frame. In addition, military personnel, armed policemen, and elderly retired cadres in army were not included. The trained health workers at local community health centers administered a standardized questionnaire, including information on sociodemographic status, medical history, lifestyle (e.g., smoking) factors. The questionnaire on smoking was adopted from the Global Adult Tobacco Survey (GATS)24 and China Adult Tobacco Survey.25
The study was approved by the Ethics Review Committee of the China Health Education Center (Beijing, China). All study participants provided written informed consent.
Sampling method
The sampling procedure of 2018 CRHLS was shown in Appendix Figure 1, which involved four stages to ensure nationally representativeness of the selected study population. First, the population proportionate sampling (PPS) method was used to randomly select a total of 336 urban districts or rural counties from the 31 provinces (or equivalent) in China. The population size of each districts (or counties) was based on the total number of households from the Sixth National Population Census of China.27 Second, the PPS method was used to randomly select three streets (or towns) at each district or county level, which included a total of 1008 streets or towns. Third, at each urban street or rural town, two urban neighborhood committees or rural villages was randomly selected, which included 2016 neighborhood committees or villages. Fourth, in each neighborhood committee or villages, a total of 55 households were randomly selected and one resident from each of the selected household is surveyed according to the KISH method, until the neighborhood committee (or villages) completed at least 40 questionnaires.
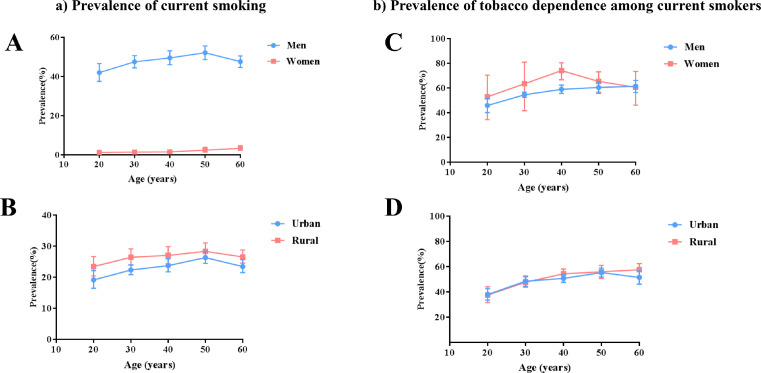
Figure 1.
Estimated prevalence of smoking and tobacco dependence in Chinese population aged 20 to 69 years. A and B, the prevalence of smoking by gender and residence; C and D, the prevalence of tobacco dependence by gender and residence. Bars represent proportion or mean; error bars represent 95% CI.
The field work took place during August 2018 and August 2019. Overall, a total of 87,708 individual were invited to participate in the survey, with 84,886 (96.8%) responding. A further 2189 individuals were excluded from the analysis consisting of those who provided unreliable results or provided no information on tobacco dependence and of the underrepresented 15–19 year age group. This study finally included 84,839 participants (40,517 men and 44,268 women) aged 20 to 69 years (Appendix Figure 2).
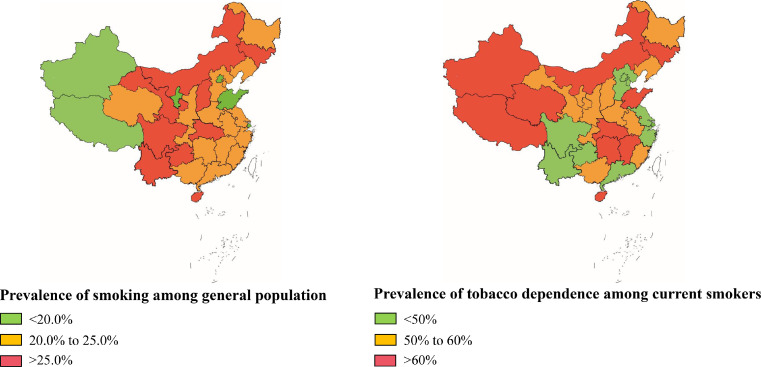
Figure 2.
The geographical distribution of smoking and tobacco dependence in Chinese population aged 20 to 69 years. The prevalence of smoking and tobacco dependence was calculated for each province according to the 2015 National Population Census. Hong Kong, Macao, and Taiwan were not included in this survey.
Data collection
The demographic questionnaire collected sociodemographic information, including age, gender, educational level and yearly income. For this study, current smoking was defined as currently smoking at the time of survey; former smoking was defined as previously smoking but no longer smoking at the time of the survey. Both former and current smokers were counted as ever smokers. Ever smokers were asked what types of tobacco products they used, the age they started smoking, the duration of smoking (current age minus the age of smoking initiation), number of cigarettes smoked per day. The severity of tobacco dependence was assessed by FTND. Previous studies have demonstrated this measure's reliability and validity.6
Diagnosis of tobacco dependence
The diagnosis criteria of tobacco dependence were based on international criteria (ICD-10,7 DSM-48) and tailored to Chinese population according to China Clinical Guideline for Tobacco Cessation (2015 version).26
For ever-smokers, tobacco dependence was diagnosed if they had 3 or more of the following 6 symptoms or signs: (1) craving, or a strong desire or urge to use tobacco; (2) a persistent desire or unsuccessful efforts to cut down or control tobacco use; (3) experiencing tobacco withdrawal symptoms (such as irritability, frustration, anger, anxiety, difficulty concentrating, increased appetite, restlessness, insomnia) after abrupt cessation of tobacco use, or reduction in the amount of tobacco used; (4) tolerance, defined as the need for markedly increased amounts of tobacco to achieve the desired effect; (5) given up or reduced important social, occupational, or recreational activities because of tobacco use; and (6) continued tobacco use despite knowledge of having a persistent or recurrent physical or psychological problem that is likely to have been caused or exacerbated by tobacco.
Statistical analysis
According to China Health Literacy level in 2016, the prevalence was 11.58%.23 In order to have sufficient statistical power, we assumed the China Health Literacy prevalence in this study to be 11.58%, so the permissible error δ was 11.58% × 10%=0.01158; we set deff to be 3.5, and α to be 0.05, so the minimum sample size of each layer was 10,266. According to the stratification of urban and rural (2 levels) and geography (eastern, central and western, 3 levels), and considering the invalid questionnaire is no more than 15%, the minimum sample size was 10266 × (3 × 2) ÷ (1–15%) =72,466. As a result, 87,708 adults were invited to participate, and 2,189 individuals who had no information on tobacco dependence were excluded. After these exclusions, 84,839 (40,517 men and 44,268 women) participants aged 20 to 69 years were included in the present study (Appendix Figure 2). Given the extremely low prevalence of smoking in women, all the analyses were done separately by sex.
The characteristics of study population and prevalence of tobacco dependence were assessed and compared using ANOVA or Student's t test for continuous variables and by the χ² test for categorical variables. All calculations were weighted to represent the general adult population aged 20 years or above in China, according to the 2010 population census, with further stratification by sampling clusters. The sample weights are calculated by using the software SUDAAN 11.0. We firstly calculated the design weight; then age and gender were included to calculate the non-response weight, and finally the sample weights are post-stratified to match the 2010 Chinese population census.
The weighted prevalence of tobacco dependence was calculated based on the census population data. A technique appropriate for the complex survey design (the Taylor series linearization method) was used to calculate SEs. The number of people with tobacco dependence was calculated based on the 2018 Chinese population.27
The Logistic regression was conducted to estimate odds ratios (OR) and 95% confidence intervals (CIs) for tobacco dependence among current smokers and success of smoking cessation (defined as being ex-smokers) among ever smokers, with different levels of adjustment. In model 1, only age was adjusted, while in model 2 age, urbanization, education level, ethnicity, marriage status, annual family yearly income, self-reported overall health status, and smoking pack-years were adjusted.
In sensitivity analyses, we repeated similar analyses for tobacco dependence using five different criteria applied in other studies. Our analyses used all participants for whom the variables of interest were available, with no imputation for missing data.
All statistical analyses were done with SAS 9.4 and SUDAAN 11.0 (Research Triangle Institute, NC, USA). All reported p values were two sided, and significance was set at P < 0.05.
Role of the funding source
The funders of the study had no role in study design, data collection, data analysis, data interpretation, or writing of the report. DX and CW had full access to all the data and responsibility for the decision to submit for publication.
Results
Of the 84,839 participants included, 47.8% were men, the mean age (SD) was 48.3 (12.5) years, 45.7% resided in urban areas, and 24.3% currently smoked (48.1% in men vs 2.5% in women). Among male current smokers, 54.1% could be classified as tobacco dependence, compared with 53.6% among female current smokers (Table 1).
Table 1.
Sociodemographic characteristics of study population.
| Variables | Men (n = 40,517) |
Women (n = 44,268) |
Overall (n = 84,839) | ||
|---|---|---|---|---|---|
| With tobacco dependence (n = 11,219) | Without tobacco dependence (n = 29,298) | With tobacco dependence (n = 629) | Without tobacco dependence (n = 43,693) | ||
| Age (years), % | |||||
| 20–29 | 624 (5.6) | 2872 (9.8) | 25 (4.0) | 4452 (10.2) | 7973 (9.4) |
| 30–39 | 1482 (13.2) | 4752 (16.2) | 57 (9.1) | 7796 (17.8) | 14087 (16.6) |
| 40–49 | 2749 (24.5) | 7005 (23.9) | 137 (21.8) | 10754 (24.6) | 20645 (24.3) |
| 50–59 | 3397 (30.3) | 7495 (25.6) | 198 (31.5) | 11233 (25.7) | 22323 (26.3) |
| 60–69 | 2967 (26.4) | 7174 (24.5) | 212 (33.7) | 9458 (21.6) | 19811 (23.4) |
| Mean age (SD) | 50.4 (11.5) | 48.4 (12.7) | 52.7 (11.0) | 47.6 (12.6) | 48.3 (12.5) |
| Urbanization, % | |||||
| Urban | 4515 (40.2) | 13445 (45.9) | 216 (34.3) | 20565 (47.1) | 38741 (45.7) |
| Rural | 6704 (59.8) | 15853 (54.1) | 413 (65.7) | 23128 (52.9) | 46098 (54.3) |
| Ethnicity, % | |||||
| Han | 10015 (89.3) | 25878 (88.4) | 561 (89.2) | 38785 (88.9) | 75239 (88.8) |
| Others | 1194 (10.7) | 3381 (11.6) | 68 (10.8) | 4850 (11.1) | 9493 (11.2) |
| Marriage status, % | |||||
| Single | 744 (6.6) | 2771 (9.5) | 18 (2.9) | 1847 (4.2) | 5380 (6.3) |
| Married | 9617 (85.8) | 24699 (84.4) | 537 (85.4) | 38230 (87.6) | 73083 (86.2) |
| Separated/divorced/widowed | 853 (7.6) | 1798 (6.1) | 74 (11.8) | 3588 (8.2) | 6313 (7.4) |
| Education level, % | |||||
| Primary school or less | 3936 (35.1) | 8490 (29.1) | 375 (59.6) | 17648 (40.5) | 30449 (36.0) |
| Middle and high school | 6211 (55.4) | 15874 (54.3) | 221 (35.1) | 19767 (45.3) | 42073 (49.7) |
| College and higher | 1060 (9.5) | 4856 (16.6) | 33 (5.2) | 6185 (14.2) | 12134 (14.3) |
| Annual family income (RMB/year), % | |||||
| <20,000 | 3681 (32.8) | 8421 (28.7) | 303 (48.2) | 12459 (28.5) | 24864 (29.3) |
| 20,000–49,999 | 3923 (35.0) | 9552 (32.6) | 196 (31.2) | 15058 (34.5) | 28729 (33.9) |
| ≥50,000 | 3615 (32.2) | 11325 (38.7) | 130 (20.7) | 16176 (37.0) | 31246 (36.8) |
| Self-reported health status, % | |||||
| Good | 6070 (54.3) | 18009 (61.7) | 283 (45.2) | 24335 (55.9) | 48697 (57.6) |
| Average | 4187 (37.4) | 9417 (32.3) | 240 (38.3) | 15714 (36.1) | 29558 (35.0) |
| Poor | 926 (8.3) | 1747 (6.0) | 103 (16.5) | 3497 (8.0) | 6273 (7.4) |
| Smoking status, % | |||||
| Current smokers | 10538 (93.9) | 8953 (30.6) | 583 (92.7) | 504 (1.2) | 20578 (24.3) |
| Ex-smokers | 681 (6.1) | 1758 (6.0) | 46 (7.3) | 121 (0.3) | 2606 (3.1) |
| Never smokers | 0 (0.0) | 18587 (63.4) | 0 (0.0) | 43068 (98.6) | 61655 (72.7) |
| FTND, % | |||||
| 0–3 | 3942 (37.4) | 7822 (66.9) | 241 (41.3) | 1191 (85.9) | 13196 (54.5) |
| 4–6 | 5420 (51.4) | 3494 (29.9) | 295 (50.6) | 176 (12.7) | 9385 (38.8) |
| ≥7 | 1176 (11.2) | 370 (3.2) | 47 (8.1) | 19 (1.4) | 1612 (6.7) |
Note: Data are shown as number (%) or mean (SD). The differing denominators used in the calculation of percentages are because of missing data.
The comparisons of smoking behaviors between current smokers with tobacco dependence and those without were shown in Appendix Table 1. Among male current smokers, compared with those without tobacco dependence, those with tobacco dependence had more smoking pack-years (27.8 ± 20.8 vs. 17.3 ± 16.4, P < 0.0001), more cigarettes smoked per day (18.2 ± 9.7 vs. 12.5 ± 8.5, P < 0.0001), earlier smoking starting age (21.4 ± 5.8 vs. 22.3 ± 6.7, P < 0.0001), longer smoking duration (29.1 ± 12.1 vs. 25.8 ± 13.0, P < 0.0001), and higher FTND (4.1 ± 1.9 vs. 2.7 ± 1.8, P < 0.0001). Moreover, the proportion who responded that they would continue to smoke even after it caused health or mental problems was significantly higher in those with tobacco dependence than those without (P < 0.0001); 73.7% of those with tobacco dependence reported they have tried to quit or cut down on tobacco but failed, which was significantly higher than 46.3% in those without (P < 0.0001). Among female current smokers, although the number of tobacco dependence was small, similar patterns of difference were observed between those with tobacco dependence and those without.
In the multivariable-adjusted analyses, tobacco dependence was significantly associated with smoking intensity, defined by pack-years (1.62 [1.54–1.70] per 10 pack-years), cigarettes smoked per day (2.01 [1.78, 2.27] per 10 cigarettes), smoking starting age (0.93 [0.90, 0.97] per 5 years), FTND (1.45 [1.39, 1.51] per 1 point), still using tobacco after it caused health (2.78 [2.58, 3.01]) or mental problems (2.86 [2.64, 3.09]), and failed attempts to quit or cut down consumption (3.05 [2.85, 3.27]) (Table 2). In addition, tobacco dependence was also significantly associated with younger age, women, living in the rural, being married, lower annual family yearly income, poorer self-reported health status (Appendix Table 2). When restricting analyses to men and women, the associated factors for tobacco dependence were not substantially altered. Moreover, there was a dose-response association between cigarette smoking and tobacco dependence (Appendix Figure 3).
Table 2.
Adjusted ORs for tobacco dependence associated with patterns of smoking.
| Variables | Men |
Women |
Overall |
||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. of cases | Model 1 (OR, 95% CI) | P | Model 2 (OR, 95% CI) | P | No. of cases | Model 1 (OR, 95% CI) | P | Model 2 (OR, 95% CI) | P | No. of cases | Model 1 (OR, 95% CI) | P | Model 2 (OR, 95% CI) | P | |
| Smoking pack-years | |||||||||||||||
| <10 | 1571 | Ref | Ref | 145 | Ref | Ref | 1716 | Ref | Ref | ||||||
| 10–19 | 1873 | 2.27 (2.06, 2.50) | <0.0001 | 2.27 (2.06, 2.51) | <0.0001 | 114 | 2.49 (1.71, 3.64) | <0.0001 | 2.56 (1.75, 3.79) | <0.0001 | 1987 | 2.25 (2.05, 2.47) | <0.0001 | 2.28 (2.08, 2.51) | <0.0001 |
| ≥20 | 5121 | 4.72 (4.30, 5.18) | <0.0001 | 4.69 (4.27, 5.16) | <0.0001 | 221 | 4.74 (3.28, 6.89) | <0.0001 | 4.73 (3.25, 6.94) | <0.0001 | 5342 | 4.61 (4.22, 5.04) | <0.0001 | 4.67 (4.26, 5.12) | <0.0001 |
| Each 10 pack-years difference | — | 1.61 (1.54, 1.69) | <0.0001 | 1.62 (1.54, 1.70) | <0.0001 | — | 1.72 (1.39, 2.14) | <0.0001 | 1.70 (1.40, 2.08) | <0.0001 | — | 1.61 (1.54. 1.69) | <0.0001 | 1.62 (1.54, 1.70) | <0.0001 |
| Cigarettes smoked per day | |||||||||||||||
| 1–9 | 1223 | Ref | Ref | 134 | Ref | Ref | 1357 | Ref | Ref | ||||||
| 10–19 | 3069 | 2.51 (2.31, 2.73) | <0.0001 | 1.94 (1.73, 2.18) | <0.0001 | 192 | 3.20 (2.35, 4.36) | <0.0001 | 2.45 (1.63, 3.69) | <0.0001 | 3261 | 2.53 (2.33, 2.74) | <0.0001 | 1.98 (1.77, 2.21) | <0.0001 |
| 20 and above | 6177 | 5.19 (4.79, 5.63) | <0.0001 | 3.21 (2.78, 3.71) | <0.0001 | 252 | 5.78 (4.19, 8.05) | <0.0001 | 3.11 (1.79, 5.42) | <0.0001 | 6429 | 5.16 (4.77, 5.58) | <0.0001 | 3.24 (2.82, 3.72) | <0.0001 |
| Each 10 cigarettes difference | — | 2.27 (2.08, 2.48) | <0.0001 | 1.98 (1.75, 2.24) | <0.0001 | — | 3.48 (2.41, 5.03) | <0.0001 | 3.29 (2.01, 5.37) | <0.0001 | — | 2.30 (2.11, 2.51) | <0.0001 | 2.01 (1.78, 2.27) | <0.0001 |
| Smoking starting age | |||||||||||||||
| ≥25 | 2274 | Ref | Ref | 221 | Ref | Ref | 2495 | Ref | Ref | ||||||
| 20–24 | 4186 | 1.40 (1.30, 1.51) | <0.0001 | 1.14 (1.04, 1.25) | 0.0057 | 166 | 1.89 (1.34, 2.68) | 0.0004 | 1.35 (0.90, 2.05) | 0.1507 | 4352 | 1.40 (1.30, 1.51) | <0.0001 | 1.14 (1.05, 1.25) | 0.0032 |
| <20 | 3424 | 1.55 (1.43, 1.68) | <0.0001 | 1.17 (1.06, 1.29) | 0.0016 | 146 | 1.57 (1.11, 2.22) | 0.0113 | 1.21 (0.79, 1.85) | 0.3746 | 3570 | 1.54 (1.42, 1.67) | <0.0001 | 1.17 (1.06, 1.29) | 0.0013 |
| Each 5 years difference | — | 0.84 (0.81, 0.87) | <0.0001 | 0.93 (0.89, 0.97) | <0.0001 | — | 0.85 (0.77, 0.93) | <0.0001 | 0.90 (0.81, 1.00) | 0.0500 | — | 0.84 (0.81, 0.87) | <0.0001 | 0.93 (0.90, 0.97) | <0.0001 |
| Smoking duration | |||||||||||||||
| 1–9 | 449 | Ref | Ref | 35 | Ref | Ref | 484 | Ref | Ref | ||||||
| 10–19 | 1304 | 1.87 (1.60, 2.19) | <0.0001 | 1.29 (1.09, 1.52) | 0.0031 | 89 | 2.17 (1.29, 3.69) | 0.0037 | 1.86 (1.08, 3.24) | 0.0259 | 1393 | 1.90 (1.63, 2.21) | <0.0001 | 1.34 (1.14, 1.57) | 0.0003 |
| 20 and above | 6669 | 2.76 (2.33, 3.28) | <0.0001 | 0.83 (0.69, 1.01) | 0.0632 | 344 | 3.00 (1.79, 5.10) | <0.0001 | 1.16 (0.63, 2.14) | 0.6364 | 7013 | 2.76 (2.35, 3.25) | <0.0001 | 0.86 (0.72, 1.04) | 0.1110 |
| Each 10 years difference | — | 1.44 (1.34, 1.54) | <0.0001 | 0.98 (0.91, 1.06) | 0.6007 | — | 1.64 (1.38, 1.94) | <0.0001 | 1.26 (1.02, 1.55) | 0.0318 | — | 1.45 (1.35, 1.54) | <0.0001 | 0.99 (0.93–1.07) | 0.8600 |
| FTND | |||||||||||||||
| 0–3 | 3942 | Ref | Ref | 241 | Ref | Ref | 4183 | Ref | Ref | ||||||
| 4–6 | 5420 | 3.05 (2.87, 3.25) | <0.0001 | 2.34 (2.17, 2.53) | <0.0001 | 295 | 3.32 (2.55, 4.35) | <0.0001 | 2.23 (1.61, 3.08) | <0.0001 | 5715 | 3.06 (2.88, 3.25) | <0.0001 | 2.34 (2.17, 2.52) | <0.0001 |
| ≥7 | 1176 | 7.64 (6.60, 8.88) | <0.0001 | 5.07 (4.28, 6.04) | <0.0001 | 47 | 4.99 (2.71, 9.85) | <0.0001 | 2.61 (1.24, 5.94) | 0.0154 | 1223 | 7.48 (6.49, 8.66) | <0.0001 | 4.94 (4.19, 5.86) | <0.0001 |
| Each 1-point difference | — | 1.54 (1.50, 1.59) | <0.0001 | 1.45 (1.39, 1.51) | <0.0001 | — | 1.64 (1.46, 1.84) | <0.0001 | 1.56 (1.37, 1.76) | <0.0001 | — | 1.55 (1.50, 1.59) | <0.0001 | 1.45 (1.39, 1.51) | <0.0001 |
| Continue to use tobacco after it caused health problems | |||||||||||||||
| No | 6333 | Ref | Ref | 331 | Ref | Ref | 6664 | Ref | Ref | ||||||
| Yes | 4203 | 3.36 (3.13, 3.59) | <0.0001 | 2.83 (2.61, 3.06) | <0.0001 | 252 | 2.77 (2.11, 3.65) | <0.0001 | 2.23 (1.62, 3.09) | <0.0001 | 4455 | 3.31 (3.10, 3.54) | <0.0001 | 2.78 (2.58, 3.01) | <0.0001 |
| Continue to use tobacco after it caused mental problems | |||||||||||||||
| No | 6501 | Ref | Ref | 324 | Ref | Ref | 6825 | Ref | Ref | ||||||
| Yes | 4031 | 3.36 (3.13, 3.60) | <0.0001 | 2.90 (2.67, 3.14) | <0.0001 | 259 | 3.24 (2.46, 4.30) | <0.0001 | 2.40 (1.75, 3.31) | <0.0001 | 4290 | 3.35 (3.13, 3.58) | <0.0001 | 2.86 (2.64, 3.09) | <0.0001 |
| Trying to quit or cut down on tobacco but failed | |||||||||||||||
| No | 2775 | Ref | Ref | 140 | Ref | Ref | 2915 | Ref | Ref | ||||||
| Yes | 7760 | 3.21 (3.03, 3.41) | <0.0001 | 3.03 (2.82, 3.25) | <0.0001 | 443 | 4.10 (3.16, 5.35) | <0.0001 | 3.51 (2.59, 4.78) | <0.0001 | 8203 | 3.26 (3.07, 3.45) | <0.0001 | 3.05 (2.85, 3.27) | <0.0001 |
Note: Model 1 was adjusted for gender and age; model 2 was adjusted for gender, age, urbanization, education level, ethnicity, marriage status, annual family yearly income, self-reported overall health status, and smoking pack-years. FTND=Fagerström Test for Tobacco dependence.
In another multivariable-adjusted analyses (Appendix Table 3), successful smoking cessation (defined as being ex-smokers) was significantly associated with no tobacco dependence (OR: 2.88, 95% CI: 2.59–3.21), smoking pack-years <10, (OR: 1.36, 95% CI: 1.20–1.54), would not continue to use tobacco after it caused health (OR: 2.06, 95% CI: 1.82–2.34) or mental problems (OR: 1.98, 95% CI: 1.74–2.25), and no experience of trying to quit or cut down on tobacco but failed (OR: 1.97, 95% CI: 1.79–2.17), and certain socioeconomic status (being older, higher education level, higher annual family yearly income, poorer self-reported health status). When restricting analyses to men, the associated factors for successful smoking cessation (defined as being ex-smokers) were not substantially altered. However, when restricting analyses to women, only without tobacco dependence (OR: 2.51, 95% CI: 1.64–3.91), less smoking pack-years, would not continue to use tobacco after it caused health (OR: 1.61, 95% CI: 1.02–2.61) or mental problems (OR: 1.63, 95% CI: 1.04–2.63), and no experience of trying to quit or cut down on tobacco but failed (OR: 1.55, 95% CI: 1.05–2.30) were associated with successful smoking cessation (defined as being ex-smokers).
In Chinese adults aged 20-69 years, the estimated prevalence of current smoking was 25.1% (23.4–26.8) in overall population, 47.6% (44.6–50.5) in men and 1.9% (1.3–2.6) in women. The prevalence of tobacco dependence among general population aged 20–69 years was 13.1% (95% CI:12.2–14.1). More importantly, the prevalence of tobacco dependence among current smoker aged 20–69 years was 49.7% (46.5–52.9) in overall population, (46.5–52.8) in men and 50.8% (43.5–58.1) in women (Table 3). The estimated prevalence of tobacco dependence among current smoker increased with age, but similar between men and women, urban and rural resident (Figure 1).
Table 3.
Estimated prevalence and total number of current smokers and tobacco dependence in China in 2018.
| Characteristics | Current smoking |
Tobacco dependence |
||
|---|---|---|---|---|
| Prevalence (95% CI) | Total number (million, 95% CI) | Prevalence among current smoking (95% CI) | Total number (million, 95% CI) | |
| Age | ||||
| 20–29 | 21.9 (19.4–24.5) | 42.9 (38.2–48.1) | 37.8 (33.7–42.2) | 17.0 (14.9–19.3) |
| 30–39 | 25.1 (23.2–27.1) | 53.5 (49.4–57.8) | 48.2 (45.6–50.7) | 26.8 (24.9–28.8) |
| 40–49 | 26.1 (23.9–28.4) | 59.1 (54.3–64.3) | 53.5 (50.6–56.3) | 33.1 (30.4–35.9) |
| 50–59 | 27.8 (26.0–29.8) | 56.6 (52.7–60.6) | 55.9 (51.5–60.2) | 33.5 (30.7–36.5) |
| 60–69 | 25.8 (24.2–27.5) | 38.7 (36.3–41.2) | 56.3 (51.6–60.9) | 24.0 (21.9–26.2) |
| Gender | ||||
| Men | 47.6 (44.6–50.5) | 339.5 (318.5–360.5) | 49.7 (46.5–52.8) | 177.5 (165.7–189.9) |
| Women | 1.9 (1.3–2.6) | 12.9 (9.2–18.0) | 50.8 (43.5–58.1) | 7.1 (4.9–10.4) |
| Locality | ||||
| Urban | 22.5 (21.5–23.7) | 187.4 (178.4–196.7) | 48.2 (46.0–50.4) | 95.6 (89.3–102.4) |
| Rural | 26.3 (24.2–28.6) | 148.4 (136.4–161.2) | 50.3 (46.1–54.5) | 78.6 (72.3–85.4) |
| Overall | 25.1 (23.4–26.8) | 338.7 (315.7–361.6) | 49.7 (46.5–52.9) | 183.5 (170.4–197.4) |
When the prevalence of current smoking and tobacco dependence was divided into three categories respectively (for current smoking: <20.0%, 20.0% to 25.0%, and >25.0%; for tobacco dependence, <50%, 50% to 60%, >60%), it was found that prevalence of current smoking and tobacco dependence varied in different areas of China. First, several provinces had both relatively high prevalence of smoking and tobacco dependence, such as Hainan Province (33.5% and 57.7%), Jilin Province (29.1% and 58.9%), and Inner Mongolia Autonomous Region (29.1% and 61.8%); second, several provinces had both relatively low prevalence of smoking and tobacco dependence, such as Beijing City (19.9% and 39.2%) and Shanghai City (19.6% and 41.1%); third, relatively high smoking prevalence but relatively low prevalence of tobacco dependence was observed in Guizhou Province (37.9% and 39.2%), Yunnan Province (33.7% and 45.2%) and Sichuan Province (29.0% and 47.1%); last, relatively low smoking prevalence but relatively high prevalence of tobacco dependence were found in Xizang Autonomous Region (12.9% and 58.5%), Xinjiang Uygur Autonomous Region (14.7% and 66.9%), and Shandong Province (19.9% and 64.1%) (Figure 2).
In China, an estimated 183.5 (170.4–197.4) million people had tobacco dependence, involving predominantly men (177.5 [165.7–189.9] million), but with similar numbers in urban and rural areas (95.6 [89.3–102.4] million vs. 78.6 [72.3–85.4] million). The estimated total number of tobacco dependence showed an inverted U-shaped relationship with age, with the highest number seen at 50–59 years of age (Table 3).
Using sensitivity analyses, we further evaluated tobacco dependence using different criteria,12, 13, 14, 15, 16, 17, 18 and found that the prevalence of tobacco dependence defined as smoking within 30 min of waking had the best agreement with our criteria (Appendix Table 4).
Discussion
To the best of our knowledge, this is the first and largest study to estimate the prevalence, associated factors, and burden of tobacco dependence in a nationally-representative sample of Chinese adult population and elsewhere. Our data indicated that approximately half of current smokers in both men and women had tobacco dependence. Apart from certain smoking characteristics (e.g., younger age of initiation, heavy smokers), a number of sociodemographic factors (e.g. younger age, low socioeconomic status) were also associated with higher risk of being tobacco-dependent. Moreover, those with tobacco dependence were less likely to initiate quitting or to successfully quit smoking. Overall, in China, we estimated that 183.5 million adults in China, involving predominantly men, had tobacco dependence, with large variations across different areas of China.
The 2018 China Adult Tobacco Survey estimated the prevalence of current smoking was 26.6% in overall population, 50.5% in men and 2.1% in women, which was consistent with 25.1% in overall population, 47.6% in men and 1.9% in women in our study. However, the prevalence of tobacco dependence was far less clear in previous studies. Among numerous tobacco surveys,28 only a few cross-sectional surveys have reported the prevalence of tobacco dependence with different diagnostic criteria. As expected, using different diagnostic criteria lead to substantial variability in the prevalence of tobacco dependence. The estimated prevalence of tobacco dependence in our study was 49.7% among current smoker, which was in line with 50.9% in one study of non-nationally representative 500,000 US adults (defined as HSI≥3),17 51.2% in one study of 489 Canadians (defined as FTND≥6),15 and 45.8% in one study of 5000 European adults (defined as smoking within 30 min of waking).11 However, several previous studies have shown mixed results. The prevalence of tobacco dependence (defined as HSI≥4) was 25.0% in one study of 8,229 European adults29 and 31.6% in one study of 17,158 Chinese adults (defined as FTND≥5).12 This inconsistency was largely due to the difference of diagnostic criteria used. The diagnostic criteria in our study were based on the recommendations of international criteria (ICD-10,7 DSM-48) and characteristics of Chinese smoking population,26 which we reasoned would accurately reflect tobacco dependence in Chinese smoking population. In addition, genetic and sociocultural differences may also have contributed to the inconsistency.
Smoking is the direct cause of tobacco dependence. As expected, smokers were becoming more dependent with increased smoking amount and duration. Compared with those without tobacco dependence, current smokers with tobacco dependence were less likely to be ex-smokers. This result supported the ‘hardening’ hypothesis37 that as overall tobacco use declines, less dependent smokers will quit, leaving a growing proportion of severely dependent smokers who may be less likely to quit, resulting in a leveling-off of the reduction in smoking rates. Thus, smoking prevention and cessation remain the major important strategies for reducing tobacco dependence.
Our study identified several major associated factors of tobacco dependence. Previous study has showed that adolescents and young adults appeared to be particularly vulnerable to the adverse effects of tobacco on the central nervous system.30 The 2012 Report of the Surgeon General concluded that “Among adults who become daily smokers, nearly all first use of cigarettes occurs by 18 years of age (88%), with 99% of first use by 26 years of age”.31 Our study showed that younger age is strongly associated with the persistence of tobacco dependence, which is consistent with the findings of previous studies on predictors of smoking.13, 14, 15, 16 This information underlines the importance of actively preventing smoking uptake and tobacco dependence among young people, and services that can effectively help adolescents are urgently needed. There are few tasks that are more urgent for improving public health in China than that of keeping adolescents away from tobacco.32
There is evidence from human and laboratory animal studies that gender is also an important factor that influences vulnerability to tobacco addiction. Historically, smoking has always been more common among male than female in China, but previous researches have indicated that it was more difficult for females to quit smoking.33 This is in line with our study which showed that female was associated with increased risk of tobacco dependence, although female smokers tended to start at later age and to smoke less compared with their male counterparts. One possible explanation to this finding is the gender variation in nicotine metabolism variability. Women metabolize nicotine more quickly than men, which may contribute to their increased susceptibility to nicotine addiction.4 In addition, women also exhibit more negative affect after exposure to a cue associated with nicotine withdrawal than men.34 This information may be particularly useful in planning family-based smoke-free strategies and targeting high-risk female populations.
In our study, those with lower socioeconomic status (such as living in rural areas with low income) tended to have greater risk of tobacco dependence, which was consistent with a cross-sectional, nationally representative surveys in Armenia, Azerbaijan, Belarus, Georgia, Kazakhstan, Kyrgyzstan, Moldova, Russia, and Ukraine.35 The possible reasons included smoking may make rural residents easier to socialize and increase the sense of belonging; less educated people may be less responsive to health promotion and have less information about the health consequences of smoking and less access to cessation services, leading to more cigarettes smoked and tobacco dependence.36 In addition, studies have shown that married persons have a lower smoking rate and a higher smoking cessation rate.38 However, only a few studies explored the relationship between marriage and tobacco dependence. In our study married men were significantly associated with higher risk of tobacco dependence. The possible explanation was that Chinese tobacco control program encourages men to quit smoking before marriage, however, it is difficult for man with tobacco dependence to quit smoking on their own and they might continue to smoke after marriage; another possible explanation was that Chinese men generally had more responsibilities for the family, and they were more likely than women to continue or return to smoking in the presence of adverse family events.39 Nevertheless, there is a need to examine the results via a longitudinal design.
The prevalence of smoking and tobacco dependence varied widely across provinces. The prevalence of smoking and tobacco dependence in Beijing City and Shanghai City remained well below the national average, which might be related to the better implementation of tobacco control policy, better accessibility and affordability of tobacco dependence treatment, and local anti-tobacco culture and customs. On the contrary, approximately 60% of current smokers in Xinjiang Uygur Autonomous Region, Jiangxi Province, Qinghai Province, Inner Mongolia Autonomous Region and Xizang Autonomous Region, etc. had tobacco dependence. As more ethnic minorities lived in these areas, the data revealed possible ethnic differences in prevalence of tobacco dependence. Nevertheless, tobacco control program tailored according to the prevalence of tobacco dependence in different areas of China, is greatly needed.
Our study has several strengths, including large sample size, nationally representative, well-validated questionnaires, and stringent quality control process. In addition, the prevalence of smoking in our study is similar to the findings of the 2018 China Adult Tobacco Survey, indicating the accuracy and reliability of our study. Several potential limitations of our study should be considered while interpreting the results. Firstly, the study design was cross-sectional and no causal interpretations can be made. Second, recall bias in smoking prevalence and patterns could exist because they were based on self-administrated questionnaires without objective validation. Moreover, for former smokers, we did not consider the duration of cessation. Third, because the number of individuals younger than 20 years was underrepresented, we cannot provide information on teenagers who might also have tobacco dependence. Fourth, although we have considered many associated factors, other potentially important factors such as genetics, attempting and motivation to quit, duration of quitting, Russell Reason for Smoking Questionnaire (RRSQ), were not assessed.
Our study has important public health implications. This present study estimated that 183.5 million Chinese current smokers had tobacco dependence, which is comparable with the numbers affected by non-communicable diseases such as heart disease, stroke, cancer, chronic respiratory diseases and diabetes in China. Considering the high prevalence and addictive nature of tobacco dependence, intensive and individualized treatment, such as pharmacological treatment of tobacco dependence, should be timely and effectively integrated into current tobacco control programmes.5 If the present course remains unchanged, in the near future, China and the world will face more severe challenge of epidemic proportions caused by tobacco dependence.
In summary, this is the first and largest study to characterize the prevalence, associated factors and burden of tobacco dependence in Chinese population and elsewhere. Considering the high prevalence and addictive nature of tobacco dependence, it will be difficult to accomplish the government's goal of reducing smoking prevalence among people aged 15 years or older to 20% in 2030 unless decisive and immediate action was taken. Our findings call for an increased focus on awareness, diagnosis and treatment for tobacco dependence to reduce the burden of this condition not only in China but also in the rest of the world.
Contributors
All authors were involved in the planning of the study, literature review, interpretation of the findings, and manuscript preparation. Chen W, Dan X and Ying-hua Li conceived and designed the study. Dan X supervised the study. Dan X, ZM C, Zhao L drafted the report. Cheng-dong Yu, Xin-mei Zhou, Nie Xue-qiong and Li Li did the statistical analysis. All authors contributed to data collection, analysis, and interpretation. All authors revised the report and approved the final version before submission. Chen W and Dan X are the guarantors and attest that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Data sharing statement
Data will be available upon reasonable request to the corresponding author immediately following publication to anyone wishing to access the data.
Editor note: The Lancet Group takes a neutral position with respect to territorial claims in published maps and institutional affiliations.
Declaration of interests
The authors declared no conflicts of interest.
Acknowledgments
We thank the participants of the 2018 China Health Literacy Survey. The authors appreciate every supporter from the local health administrations, health education institutes, centers for disease control and prevention, and primary care institutions across 31 provinces in China who contributed to the 2018 China Health Literacy Survey.
Footnotes
Supplementary material associated with this article can be found in the online version at doi:10.1016/j.lanwpc.2022.100464.
Contributor Information
Dan Xiao, Email: danxiao@263.net.
Chen Wang, Email: wangchen@pumc.edu.cn.
Appendix. Supplementary materials
References
- 1.World Health Organization. WHO report on the global tobacco epidemic, 2019. Geneva: World Health Organization, 2019.
- 2.World Health Organization. The bill China cannot afford: health, economic and social costs of China's tobacco epidemic. Manila, Philippines: World Health Organization Regional Office for the Western Pacific, 2017.
- 3.Chen Z., Peto R., Zhou M., et al. Contrasting male and female trends in tobacco-attributed mortality in China: evidence from successive nationwide prospective cohort studies. Lancet. 2015;386:1447–1456. doi: 10.1016/S0140-6736(15)00340-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Benowitz N.L. Nicotine addiction. N Engl J Med. 2010;362:2295–2303. doi: 10.1056/NEJMra0809890. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xiao D., Wang C. Tobacco dependence should be recognised as a lethal non-communicable disease. BMJ. 2019;365:l2204. doi: 10.1136/bmj.l2204. [DOI] [PubMed] [Google Scholar]
- 6.Fagerstrom K.O., Heatherton T.F., Kozlowski L.T. Nicotine addiction and its assessment. Ear Nose Throat J. 1990;69(11):763–765. [PubMed] [Google Scholar]
- 7.World Health Organization . World Health Organization; Switzerland: 1992. The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines. [Google Scholar]
- 8.American Psychological Association . American Psychiatric Association Publishing; Washington DC: 1994. Diagnostic and Statistical Manual of Mental Disorders. [Google Scholar]
- 9.Heatherton T.F., Kozlowski L.T., Frecker R.C., et al. Measuring the heaviness of smoking: using self-reported time to the first cigarette of the day and number of cigarettes smoked per day. Br J Addict. 1989;84(7):791–799. doi: 10.1111/j.1360-0443.1989.tb03059.x. [DOI] [PubMed] [Google Scholar]
- 10.Shiffman S., Waters A., Hickcox M. The tobacco dependence syndrome scale: a multidimensional measure of tobacco dependence. Nicotine Tob Res. 2004;6(2):327–348. doi: 10.1080/1462220042000202481. [DOI] [PubMed] [Google Scholar]
- 11.Allen J.A., Gritz E.R., Xiao H., et al. Impact of tobacco control policy on quitting and tobacco dependence among women in five European countries. Tob Control. 2014;23(2):173–177. doi: 10.1136/tobaccocontrol-2011-050391. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cai L., Cui W., You D., et al. Vol. 15. BMC Public Health; 2015. p. 1158. (Socioeconomic Variations in Tobacco Dependence in Rural Southwest China). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Goodwin R.D., Pagura J., Spiwak R., Lemeshow A.R., Sareen J. Predictors of persistent tobacco dependence among adults in the United States. Drug Alcohol Depend. 2011;118(2-3):127–133. doi: 10.1016/j.drugalcdep.2011.03.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ma Y., Wen L., Cui W., et al. Prevalence of cigarette smoking and tobacco dependence in men and women residing in two provinces in China. Front Psychiatry. 2017;8:254. doi: 10.3389/fpsyt.2017.00254. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Torchalla I., Strehlau V., Okoli C.T., et al. Smoking and predictors of tobacco dependence in a homeless population. Nicotine Tob Res. 2011;13(10):934–942. doi: 10.1093/ntr/ntr101. [DOI] [PubMed] [Google Scholar]
- 16.Roberts B., Gilmore A., Stickley A., et al. Prevalence and psychosocial determinants of tobacco dependence in nine countries of the former Soviet Union. Nicotine Tob Res. 2013;15(1):271–276. doi: 10.1093/ntr/nts100. [DOI] [PubMed] [Google Scholar]
- 17.Schnoll R.A., Goren A., Annunziata K., et al. The prevalence, predictors and associated health outcomes of high tobacco dependence using three measures among US smokers. Addiction. 2013;108(11):1989–2000. doi: 10.1111/add.12285. [DOI] [PubMed] [Google Scholar]
- 18.Grant B.F., Shmulewitz D., Compton W.M. Nicotine use and DSM-IV Tobacco dependence in the United States, 2001–2002 and 2012–2013. Am J Psychiatry. 2020;177(11):1082–1090. doi: 10.1176/appi.ajp.2020.19090900. [DOI] [PubMed] [Google Scholar]
- 19.Shahwan S., Abdin E., Shafie S., et al. Prevalence and correlates of smoking and tobacco dependence: results of a nationwide cross-sectional survey among Singapore residents. BMJ Open. 2019;9(10) doi: 10.1136/bmjopen-2019-032198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ping W., Qun-an M.A.O., Mao-xuan T.A.O., et al. Survey on the status of health literacy of Chinese residents in 2008. Chin J Health Educ. 2010;26(4):243. -216 (Chinese) [Google Scholar]
- 21.Ying-hua L.I., Qun-an M.A.O., Qi S.H.I., et al. The level of health literacy of Chinese residents in 2012: surveillance results. Chin J Health Educ. 2015;(2):99–103. (Chinese) [Google Scholar]
- 22.Wei W.E.I., Ying-hua L.I., Fang-bo L.I., et al. Health literacy condition analysis on 15 -24 years old Chinese residents. Chin J Health Educ. 2015;146(2):125–128. (Chinese) [Google Scholar]
- 23.Li L.I., Ying-hua L.I., Xue-qiong N.I.E., et al. The level of health literacy and its influencing factors of women in childbearing age in 2017. Chin J Health Educ. 2020;36(7):587–591. 630 (Chinese) [Google Scholar]
- 24.Palipudi K.M., Morton J., Hsia J., et al. Methodology of the global adult tobacco survey 2008–2010. Glob Health Promot. 2016;23(suppl 2):3–23. doi: 10.1177/1757975913499800. [DOI] [PubMed] [Google Scholar]
- 25.Li Q., Hsia J., Yang G. Prevalence of smoking in China in 2010. N Engl J Med. 2011;364:2469–2470. doi: 10.1056/NEJMc1102459. [DOI] [PubMed] [Google Scholar]
- 26.China National Health and Family Planning Commission . People's Medical Publishing House; Beijing: 2015. China Clinical Guidelines for Tobacco Cessation (2015 version) [Google Scholar]
- 27.National Bureau of Statistics of China. 2016 China statistical yearbook. 2016. http://www.stats.gov.cn/tjsj/ndsj/2016/indexeh.htm (accessed Sept 1, 2020).
- 28.GBD 2015 Tobacco Collaborators Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet. 2017;389(10082):1885–1906. doi: 10.1016/S0140-6736(17)30819-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Kaleta D., Polańska K., Korytkowski P., et al. Vol. 15. BMC Public Health; 2015. p. 1189. (Patterns of Tobacco Dependence in four Eastern European Countries). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yuan M., Cross S.J., Loughlin S.E., et al. Nicotine and the adolescent brain. J Physiol. 2015;593(16):3397–3412. doi: 10.1113/JP270492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.U.S. Department of Health and Human Services. 2 012 Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health, 2012.
- 32.Xiao D., Wang C. Rising smoking epidemic among adolescents in China. Lancet Respir Med. 2019;7(1):3–5. doi: 10.1016/S2213-2600(18)30509-5. [DOI] [PubMed] [Google Scholar]
- 33.Grant B.F., Hasin D.S., Chou S.P., et al. Tobacco dependence and psychiatric disorders in the United States: results from the National Epidemiologic survey on alcohol and related conditions. Arch Gen Psychiatry. 2004;61:1107–1115. doi: 10.1001/archpsyc.61.11.1107. [DOI] [PubMed] [Google Scholar]
- 34.Perkins K.A., Jacobs L., Sanders M., et al. Sex differences in the subjective and reinforcing effects of cigarette nicotine dose. Psychopharmacology. 2002;163:194–201. doi: 10.1007/s00213-002-1168-1. (Berl) [DOI] [PubMed] [Google Scholar]
- 35.Roberts B., Gilmore A., Stickley A., et al. Prevalence and psychosocial determinants of tobacco dependence in nine countries of the former Soviet Union. Nicotine Tob Res. 2013;15(1):271–276. doi: 10.1093/ntr/nts100. [DOI] [PubMed] [Google Scholar]
- 36.El-Khoury Lesueur F., Bolze C., Melchior M. Factors associated with successful vs. unsuccessful smoking cessation: data from a nationally representative study. Addict Behav. 2018;80:110–115. doi: 10.1016/j.addbeh.2018.01.016. [DOI] [PubMed] [Google Scholar]
- 37.Costa M.L., Cohen J.E., Chaiton M.O., et al. Hardcore” definitions and their application to a population-based sample of smokers. Nicotine Tob Res. 2010;12:860–864. doi: 10.1093/ntr/ntq103. [DOI] [PubMed] [Google Scholar]
- 38.Broms U., Silventoinen K., Lahelma E., et al. Smoking cessation by socioeconomic status and marital status: the contribution of smoking behavior and family background. Nicotine Tob Res. 2004;6(3):447–455. doi: 10.1080/14622200410001696637. [DOI] [PubMed] [Google Scholar]
- 39.Cho H.J., Khang Y.H., Jun H.J., et al. Marital status and smoking in Korea: the influence of gender and age. Soc Sci Med. 2008;66(3):609–619. doi: 10.1016/j.socscimed.2007.10.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.