Abstract
The open repair of groin hernias is often augmented with prosthetic biomaterials (mesh) as this favours a lower recurrence rate. The use of such prostheses may be associated with various complications including migration the frequency of which is unclear. A 29-year review of this complication after mesh plug hernioplasty is undertaken and technical advice described to avoid this.
Keywords: Open mesh plug inguinal hernioplasty, Plug migration, Mesh complications
Highlights
-
•
Open Mesh plug inguinal hernia repair needs to be performed methodically.
Open mesh plug inguinal hernioplasty, Plug migration, Mesh complications.
1. Introduction
Great strides have been accomplished in the open repair of inguinal hernias following the use of prosthetic mesh as pioneered by Lichtenstein over 40 years ago [1]. Open hernioplasty can be performed with various prostheses often described as ‘flat’, 3-dimensional ‘mesh plugs ’ or ‘bi-layered’. The use of mesh plugs (MP), originally popularized for cases of recurrence [1], remains well-liked possibly because of its simplicity, but may be associated with various complications including mesh migration and/or organ fistulation. Over the last 25 years we have used a MP (Perfix TM, BD, New Jersey) in over 3000 open repairs and have not witnessed this complication. Why is this?
2. Surgical technique
As all hernia surgeons will confirm the most important step in hernioplasty is accurate characterization of the anatomical defect. It is important to remember that a MP repair is essentially an open approach to the preperitoneal space. After carefully opening the inguinal canal in direct (medial) hernias the overlying thinned transversalis fascia needs to be excised and this space widened by blunt finger or swab dissection. Before dividing the fascia we infiltrate this area (with a mixture of 0.5% bupivacaine and 1% lignocaine with 1:200,000 adrenaline) to aid this dissection and lessen the annoying bleeding that can be encountered. With indirect (lateral) hernias it is important to reach the glistening darker yellow preperitoneal fat, which is a good indicator that the correct plane has been achieved. Any ‘lipomas’ can be excised and again we place a moist sponge into the defect (Figure 1) before choosing the correct size of the MP. One of the criticisms of the original open tension-free MP hernioplasty is that the 3-D cone shaped mesh was ‘semi-rigid’ and only supported part of the posterior wall at the defect in the preperitoneal plane. Indeed this may well play a role in the later development of migration and/or visceral fistulation if the sac has been inadvertently breached or there is poor mesh overlap of the defect. As a consequence of this fair derision, and that the inguinal canal is a multi-laminar arrangement, as opposed to a three dimensional one, we always gently stretch the inner ‘sublay’ component of the MP to make it flatter (Figure 2). This renders the MP less rigid and also allows a greater part of the posterior wall to be augmented by the prosthesis (Figure 3). When correctly positioned in this plane intra-abdominal pressure maintains this location [2]. The inner petals of the MP (Figure 4) are then carefully sutured circumferentially to the edges of the well-defined defect so as to firmly anchor the MP. With the repair complete, and tested on-table if under local anaesthesia, the accompanying patch is placed and anchored (but not sutured as in a Lichtenstein repair) behind the cord and the canal closed.
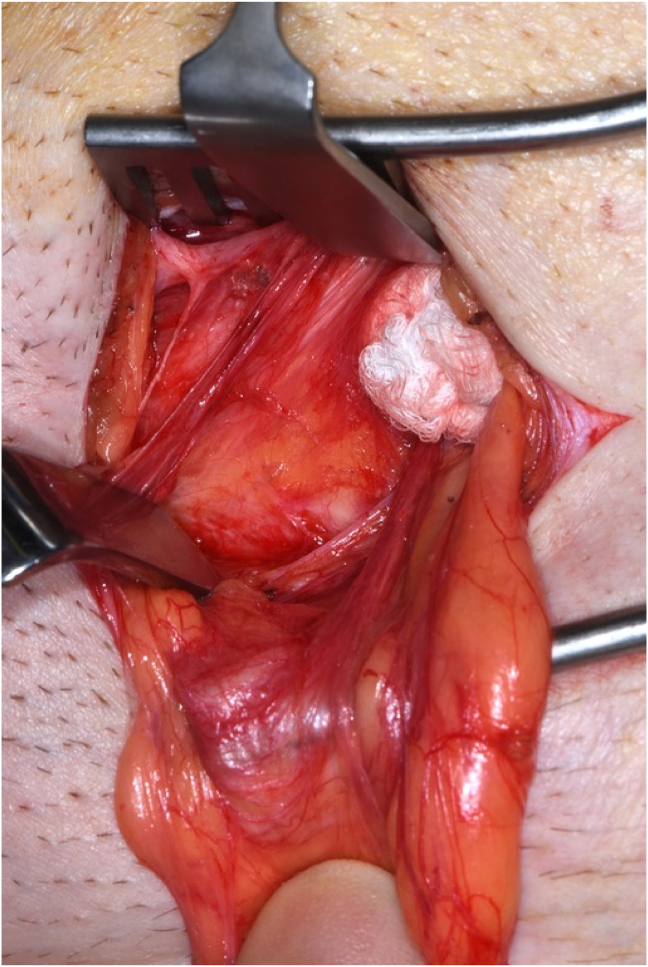
Figure 1.
A moist sponge is pressed into the perperitoneal plane of the hernial defect (left indirect). The key point is recognition of the glistening darker yellow preperitoneal fat. The ‘cavity’ for the MP may be enlarged, if necessary, by further blunt dissection to accommodate the flattened prosthesis.
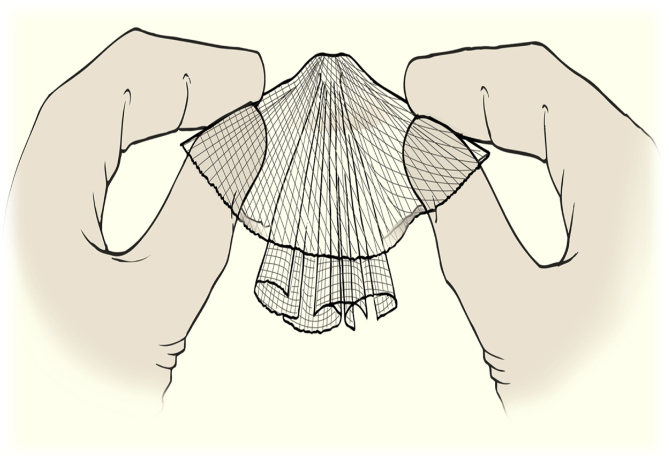
Figure 2.
Gentle stretching flattens the outer petals of the MP to increase the cross-sectional area of the sublay component before placement in the ‘cavity’ in the perperitoneal plane. [Reprinted with permission from SpringerNature: Hernia. Groin symptoms 5-7 years after a ‘modified’ plug and patch inguinal hernioplasty. Bhattacharjee A, Jayamanne H, Evans MD, Stephenson BM. 2010].
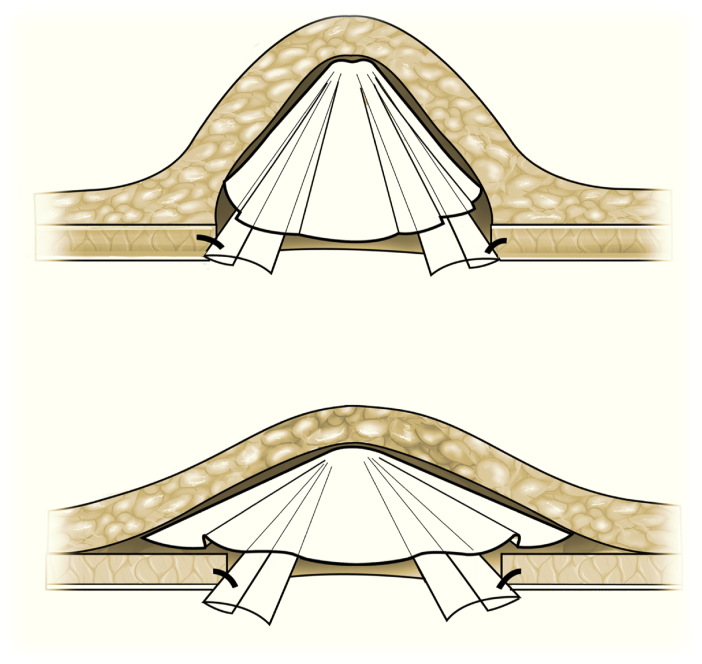
Figure 3.
The stretched and flattened sublay component now augments a greater area of the defect (lower panel). [Reprinted with permission from SpringerNature: Hernia. Groin symptoms 5-7 years after a ‘modified’ plug and patch inguinal hernioplasty. Bhattacharjee A, Jayamanne H, Evans MD, Stephenson BM. 2010].
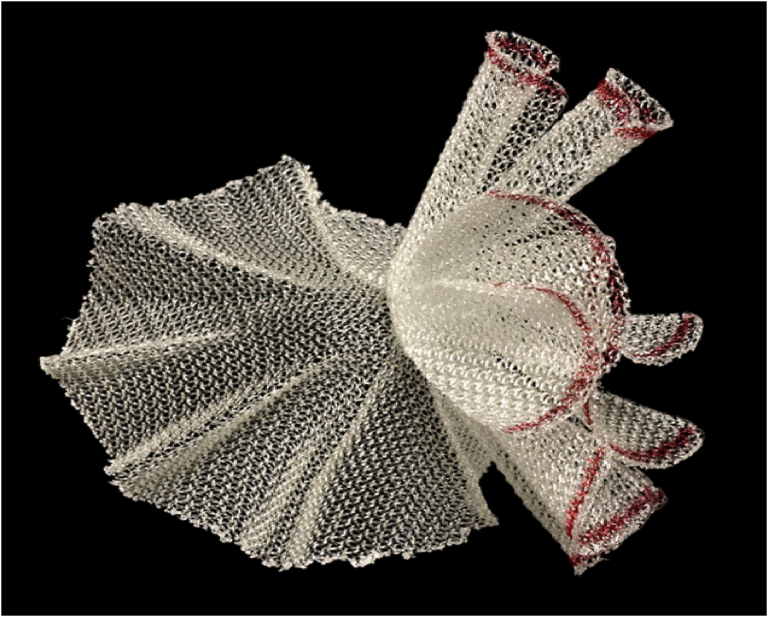
Figure 4.
The inner petals (coloured here) are anchored circumferentially to the well defined defect.
2.1. Incidence of mesh plug migration
With this approach, and in over 3000 open MP (primary and recurrent) repairs over 25 years, we have not observed a single case of migration. Is that because our patients have had their complications managed elsewhere? This is most unlikely given the litigious society that we are all in but we concur that patients are indeed likely to seek the help of another surgeon as is apparent from the published literature. Indeed this might be considered a limitation here, as we do not have complete long-term follow-up for all our MP repairs [2]. Nevertheless it is clear that such cases do occur although most infrequently given that since 1993 over 5 million Perfix MPs have been implanted worldwide (BD; New Jersey, USA. http://www.bd.com). Indeed when we critically scrutinised the literature we identified only 26 well-documented published cases during the last 29 years (Table 1). No doubt there have been other such cases, probably unreported for various reasons, but the incidence of such a problem is undoubtedly low. Furthermore, it is worthy of note that many of these cases occurred many years after the original MP hernioplasty where fistulation was probably of a response to a later near-by intra-abdominal inflammatory process. With respect to those cases of bladder fistulation it would be of interest to know whether the primary MP repair was for a direct (medial) hernia that is later repeatedly compressed by an obstructed bladder in elderly men. Furthermore it would be of interest to know if the original 3D MP had been gently flattened as we advise. Similarly it is noteworthy that reports where there was small bowel obstruction the elapsed interval is relatively short further strengthening the case for modifying or ‘flattening’ the rigidity of the MP with reliable anchoring at the deep inguinal ring. Unfortunately we will never know these answers as that the original procedures were performed at “St Elsewhere”! Finally and possibly as a consequence of these conjectures, a lighter-weight ‘softer’ version of the MP is marketed to reduce the quantity of the polypropylene prosthesis. We tend to reserve the use of this prosthesis for patients with lean groins. Whilst this MP is more malleable the operative steps required for a sound repair remain unaltered.
Table 1.
Reports of MP migration/fistulation.
| Author | Time to setback | Presentation | Comment |
|---|---|---|---|
| Dieter | 15 months | Hernia Recurrence | Poor initial operation |
| Chuback | 2 years | Small Bowel Obstruction | Poor anchoring of MP |
| Tokunaga | 7 years | Bleeding/stricture | Not true migration |
| Moorman | 1.5 years | Abdominal pain | Poor anchoring of MP |
| Benedetti | 2 years | Rectal bleeding | MP migration ‘possible’ |
| Ojo | 8 years | Caecal mass | ‘Not true migration’ |
| Murphy | 3 years | Recurrent diverticulitis | MP migration ‘possible’ |
| Zubaidi | 3 years | Cutaneous fistula | MP migration ‘possible’ |
| Stout | uncertain | Small bowel obstruction | Poor anchoring of MP |
| Liang | 4 years | Small bowel obstruction | Poor anchoring of MP |
| Ishiguro | 3 years | Cutaneous fistula | MP migration confirmed |
| Rettermaier | 3 years | Adnexal mass on CT | MP migration confirmed |
| Chen | 2 years | Small bowel perforation | MP migration confirmed |
| Ratajczak | 2 years | Sigmoid mass | MP migration confirmed |
| Yilmaz | 3 years | Sigmoid obstruction | MP migration confirmed |
| Ishikawa | 5 years | Urinary fistula | MP migration confirmed |
| Sekiguchi | 13 years | Cutaneous fistula | MP migration confirmed |
| Yamamoto | 2 years | Small bowel obstruction | MP migration confirmed |
| Scaringi | 26 years | Cutaneous fistula | Diverticulitis as pathology |
| Sevilla | 15 years | Haematuria | MP migration confirmed |
| Okada | 11 years | Haematuria | MP not anchored |
| Hamada | 7 years | Anaemia | MP migration confirmed |
| Liu | 10 years | Cutaneous fistula | MP migration confirmed |
| Zwaans | 10 years | RIF pain | MP migration confirmed |
| Gosetti | 5 years | Cutaneous fistula | MP migration confirmed |
| Zhang | 8 years | Cutaneous fistula | MP migration confirmed |
After careful scrutiny by all authors a comment was added to the table to summarise the correctness of the publication.
2.2. Alternatives
The MP approach is only one of many open techniques for repairing groin hernias and trainees should be shown and carefully taught how to perform all types of repair. Indeed residents may need a little more supervision [3] and intra-operative tutoring with regard to the correct placement (and fixation) of the MP prosthesis, which is indeed the motivation for this piece of writing. Furthermore we believe trainees should be encouraged to perform all types of open repair under local anaesthesia albeit initially at general anaesthesia [4, 5].
Mesh migration and organ fistulation is not unique to MP repairs as documented by Gossetti et al [6] and is even documented after traditional open flat-mesh repairs. Indeed this complication is also acknowledged after laparoscopic (preperitoneal) procedures, especially in TAPP as opposed to TEP repairs [6]. Nevertheless, given the number of inguinal hernia repairs carried out annually this complication is however rare. Nevertheless it should be noted that the HerniaSurge Group [7] has been vigilant in their recommendations regarding MP because of these issues. Clearly teaching and careful surgical technique (as outlined here) is essential even if the operative time for a MP repair is shorter when compared with other open techniques. Finally it is important to note that meta-analyses have suggested that there is no appreciative differences in risks/outcomes such as chronic pain or recurrence when MP repairs are compared to more traditional flat mesh repairs [8, 9].
3. Conclusions
The MP approach remains our choice in the repair of primary and recurrent inguinal hernias. In nearly 25 years we have not had a case of migration and at this point it seems pertinent to recall the words of Sir Cecil Wakely [10], who in 1948 said “ A surgeon can do more for the community by operating on hernia cases, and seeing that his recurrence rate is lower, than by operating on cases of malignant disease”. The same applies to a careful surgical technique to obtain a sound result and avoid this most unusual complication. Maybe we could do with remembering the aphorism “A good surgeon must not blame his tools”.
Declarations
Author contribution statement
All authors listed have significantly contributed to the development and the writing of this article.
Funding statement
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Data availability statement
No data was used for the research described in the article.
Declaration of interests statement
The authors declare no conflict of interest.
Additional information
No additional information is available for this paper.
References
- 1.Lichtenstein I.L., Shore J.M. Simplified repair of femoral and recurrent inguinal hernias by a “plug” technique. Am. J. Surg. 1974;128:439–444. doi: 10.1016/0002-9610(74)90189-5. [DOI] [PubMed] [Google Scholar]
- 2.Bhattacharjee A., Jayamanne H., Evans M.D., Stephenson B.M. Groin symptoms 5-7 years after a 'modified' plug and patch inguinal hernioplasty. Hernia. 2010;14:171–174. doi: 10.1007/s10029-009-0591-1. [DOI] [PubMed] [Google Scholar]
- 3.Takahashi T., Kaneoka Y., Maeda A., Takayama Y., Fukami Y., Uji M. Feasibility study of open inguinal hernia repair using mesh plug by residents. Asian J. Surg. 2020;43:304–310. doi: 10.1016/j.asjsur.2019.05.011. [DOI] [PubMed] [Google Scholar]
- 4.Radwan R.W., Gardner A., Jayamanne H., Stephenson B.M. Benefits of pre-emptive analgesia by local infiltration at day-case general anaesthetic open inguinal hernioplasty. Ann. R. Coll. Surg. Engl. 2018;100:450–453. doi: 10.1308/rcsann.2018.0059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Singh R., Byam J., Radwan R.W., Stephenson B.M. Local or general anesthesia when repairing inguinal hernias? Am. J. Surg. 2021;222:52. doi: 10.1016/j.amjsurg.2020.11.017. [DOI] [PubMed] [Google Scholar]
- 6.Gossetti F., D'Amore L., Annesi E., Bruzzone P., Bambi L., Grimaldi M.R., Ceci F., Negro P. Mesh-related visceral complications following inguinal hernia repair: an emerging topic. Hernia. 2019;23:699–708. doi: 10.1007/s10029-019-01905-z. [DOI] [PubMed] [Google Scholar]
- 7.HerniaSurge Group International guidelines for groin hernia management. Hernia. 2018;22:1–165. doi: 10.1007/s10029-017-1668-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Li J., Ji Z., Li Y. Comparison of mesh-plug and Lichtenstein for inguinal hernia repair: a meta-analysis of randomized controlled trials. Hernia. 2012;16:541–548. doi: 10.1007/s10029-012-0974-6. [DOI] [PubMed] [Google Scholar]
- 9.Ran K., Wang X., Zhao Y. Open tensionless repair techniques for inguinal hernia: a meta-analysis of randomized controlled trials. Hernia. 2020;24:733–745. doi: 10.1007/s10029-019-02106-4. [DOI] [PubMed] [Google Scholar]
- 10.Glassow F. Inguinal hernia repair using local Anaesthesia. Ann. R. Coll. Surg. Engl. 1984;66:382–387. [PMC free article] [PubMed] [Google Scholar]
Supplementary file
- Benedetti M., Albertario S., Niebel T., Bianchi C., Tinozzi F.P., Moglia P., Arcidiaco M., Tinozzi S. Intestinal perforation as a long-term complication of plug and mesh inguinal hernioplasty: case report. Hernia. 2005;9:93–95. doi: 10.1007/s10029-004-0256-z. [DOI] [PubMed] [Google Scholar]
- Chen M.J., Tian Y.F. Intraperitoneal migration of a mesh plug with a small intestinal perforation: report of a case. Surg. Today. 2010;40:566–568. doi: 10.1007/s00595-009-4107-5. [DOI] [PubMed] [Google Scholar]
- Chuback J.A., Singh R.S., Sills C., DiVck L.S. Small bowel obstruction resulting from mesh plug migration after open inguinal hernia repair. Surgery. 2000;127:475–476. doi: 10.1067/msy.2000.104122. [DOI] [PubMed] [Google Scholar]
- Dieter R.A. Mesh plug migration into scrotum: a new complication of hernia repair. Int Surg. 1999;84:57–59. [PubMed] [Google Scholar]
- Gossetti F., D'Amore L., Annesi E., Bruzzone P., Bambi L., Grimaldi M.R., Ceci F., Negro P. Mesh-related visceral complications following inguinal hernia repair: an emerging topic. Hernia. 2019;23:699–708. doi: 10.1007/s10029-019-01905-z. [DOI] [PubMed] [Google Scholar]
- Hamada Y., Tanaka K., Katsurahara M., Nakamura M. Mesh plug migration into the small intestine: an unusual cause of chronic anemia. Dig. Liver Dis. 2019;51:1062. doi: 10.1016/j.dld.2019.03.009. [DOI] [PubMed] [Google Scholar]
- Ishiguro Y., Horie H., Satoh H., Miyakura Y., Yasuda Y., Lefor A.T. Colocutaneous fistula after left inguinal hernia repair using the mesh plug technique. Surgery. 2009;145:120–121. doi: 10.1016/j.surg.2007.07.028. [DOI] [PubMed] [Google Scholar]
- Ishikawa S., Kawano T., Karashima R., Arita T., Yagi Y., Hirota M. A case of mesh plug migration into the bladder 5 years after hernia repair. Surg. Case Rep. 2015;1:4. doi: 10.1186/s40792-014-0004-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koichi Okada K, Nakayama J, Adachi S, Miyake O. Unfixed mesh plug migration from inguinal ring to urinary bladder. Acta Urol. Jpn.2018; 64: 63–66 [DOI] [PubMed]
- Liang X., Cai X.J., Yu H., Wang Y.F. Strangulated bowel obstruction resulting from mesh plug migration after open inguinal hernioplasty: case report. Chin. Med. J. 2008;121:183–184. [PubMed] [Google Scholar]
- Liu H., Liu X., Zheng G., Ye B., Chen W., Xie H., Liu Y., Guo Y. Chronic mesh infection complicated by an enterocutaneous fistula successfully treated by infected mesh removal and negative pressure wound therapy: a case report. Medicine (Baltim.) 2019;98:e18192. doi: 10.1097/MD.0000000000018192. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moorman M.L., Price P.D. Migrating mesh plug: complication of a well- established hernia repair technique. Am. Surg. 2004;70:298–299. [PubMed] [Google Scholar]
- Murphy J.W., Misra D.C., Silverglide B. Sigmoid colonic fistula secondary to Perfix-plug, left inguinal hernia repair. Hernia. 2006;10:436–438. doi: 10.1007/s10029-006-0113-3. [DOI] [PubMed] [Google Scholar]
- Ojo P., Abenthroth A., Fiedler P., Yavorek G. Migrating mesh mimicking colonic malignancy. Am. Surg. 2006;73:1210–1211. [PubMed] [Google Scholar]
- Ratajczak A., Kościński T., Banasiewicz T., Lange-Ratajczak M., Hermann J., Bobkiewicz A., Drews M. Migration of biomaterials used in gastroenterological surgery. Pol. Przegl. Chir. 2013;85:377–380. doi: 10.2478/pjs-2013-0057. [DOI] [PubMed] [Google Scholar]
- Rettenmaier M.A., Heinemann S., Truong H., Micha J.P., Brown J.V., 3rd, Goldstein B.H. Marlex mesh mimicking an adnexal malignancy. Hernia. 2009;13:221–223. doi: 10.1007/s10029-008-0426-5. [DOI] [PubMed] [Google Scholar]
- Scaringi S., Ardu M., Zambonin D., Giudici F., Bechi P. Sigmoidocutaneous fistula 26 Years after left inguinal hernia repair with mesh-plug technique. Am. Surg. 2016;82:E52–E53. [PubMed] [Google Scholar]
- Sekiguchi K., Mizuguchi Y., Mamada Y., Koizumi M., Uchida E. Intraperitoneal migration of a mesh plug from a hernioplasty forming a colocutaneous fistula with the cecum: report of a case. J. Nippon Med. Sch. 2015;82:246–249. doi: 10.1272/jnms.82.246. [DOI] [PubMed] [Google Scholar]
- Sevilla C., Dajani D., Aron M. Migrated mesh plug masquerading as a bladder tumor. J. Endourol. Case Rep. 2017;3:1–3. doi: 10.1089/cren.2016.0125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout C.L., Foret A., Christie D.B., Mullis E. Small bowel volvulus caused by migrating mesh plug. Am. Surg. 2007;73:796–797. [PubMed] [Google Scholar]
- Tokunaga Y., Tokuka A., Ohsumi K. Sigmoid colon diverticulosis adherent to mesh plug migration after open inguinal hernia repair. Curr. Surg. 2001;58:493–494. doi: 10.1016/s0149-7944(01)00495-0. [DOI] [PubMed] [Google Scholar]
- Yamamoto S., Kubota T., Abe T. A rare case of mechanical bowel obstruction caused by mesh plug migration. Hernia. 2015;19:983–985. doi: 10.1007/s10029-014-1247-3. [DOI] [PubMed] [Google Scholar]
- Yilmaz I., Karakaş D.O., Sucullu I., Ozdemir Y., Yucel E. A rare cause of mechanical bowel obstruction: mesh migration. Hernia. 2013;17:267–269. doi: 10.1007/s10029-011-0867-0. [DOI] [PubMed] [Google Scholar]
- Zhang J., Hu Z., Lin X., Chen B. Late-onset ileocutaneous fistula eight years after plug repair with polypropylene mesh: a case report. Front.Surg. 2021;8:785087. doi: 10.3389/fsurg.2021.785087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zubaidi A.M., Al Saghier M., Kabbani M., Abdo A. Colocutaneous fistula after mesh plug inguinal hernia repair- a delayed complication. Ann. Saudi Med. 2006;26:385–387. doi: 10.5144/0256-4947.2006.385. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zwaans W.A., Scheltinga M.R., Roumen R.M. Symptomatic attachment of appendix vermiformis following a plug inguinal hernia repair. BMJ Case Rep. 2019;12:e220408. doi: 10.1136/bcr-2017-220408. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
No data was used for the research described in the article.