Abstract
Background
Survivorship for those living with primary CNS cancers begins at diagnosis, continues throughout a person’s life, and includes caregivers. Opportunities and challenges exist to advance survivorship care for those living with primary CNS cancers that necessitate stakeholder involvement.
Methods
In June 2021, NCI-CONNECT convened a two-day virtual workshop about survivorship care in neuro-oncology. Two expert panels provided key recommendations and five working groups considered critical questions to identify strengths, weaknesses, opportunities, and threats to the advancement of survivorship care and developed recommendations and action items.
Results
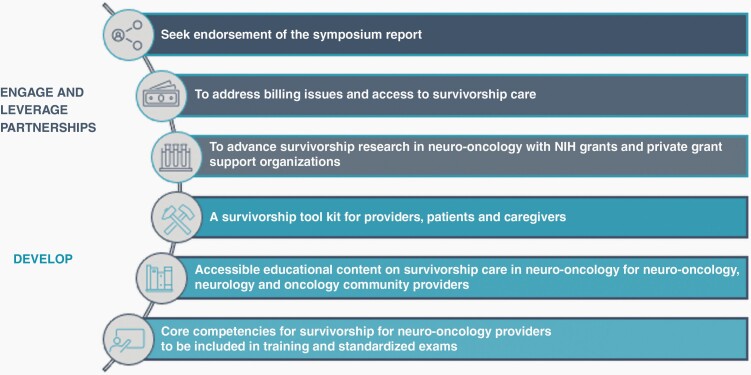
The following action items emanated from the workshop: seek endorsement of meeting report from stakeholder organizations; address barriers in access to survivorship care and provider reimbursement; advance survivorship research through NIH and private grant support; develop a survivorship tool kit for providers, people living with primary CNS cancers and their caregivers; provide accessible educational content for neuro-oncology, neurology, and oncology community providers about survivorship care in neuro-oncology; and establish core competencies for survivorship care for neuro-oncology providers to be included in training and standardized exams.
Conclusions
Action items aim to address access and reimbursement barriers, expand patient and provider education, develop core competencies, and support survivorship research through funding and other supports.
Keywords: NCI-CONNECT, patient-centered care, primary central nervous system cancer, survivorship, survivorship care
“An individual is considered a cancer survivor from the time of diagnosis, through the balance of their life. Family members, friends, and caregivers are also impacted by the survivorship experience and are therefore included in this definition.” National Coalition of Cancer Survivors and the National Cancer Institute1,2
Primary cancers of the brain and spinal cord account for less than two percent of all cancers diagnosed annually in the United States. Survivors of primary CNS cancers, together with their caregivers and loved ones, are impacted each day by one of the more than 100 different types of CNS cancers. In addition to the challenges of receiving an accurate diagnosis and navigating treatment, people living with primary CNS cancer face many ongoing challenges in learning to live their lives in adaptation following diagnosis and treatment. Common physical symptoms associated with primary CNS tumors that affect daily living include cancer- and treatment-related fatigue, weakness, seizures, difficulty with sleep, functional issues, and other treatment-specific symptoms such as nausea and constipation. Patients frequently experience cognitive challenges including difficulty thinking, remembering, seeing, speaking, and understanding. They may feel overwhelmed, anxious, and sad. These challenges are compounded by the fact that most clinicians lack experience with survivorship care issues and needs. Cancer survivorship care is defined in the seminal 2005 Institute of Medicine proceedings report “From Cancer Patient to Cancer Survivor: Lost in Transition” as including prevention and management of toxicities, surveillance for recurrence or subsequent neoplasm, and healthcare delivery.3 To be able to improve the survivorship experience of primary CNS cancer survivors through the provision of survivorship care, the first step is to raise awareness of the many challenges faced each day by people living with primary CNS tumors. The hope is that through close collaborations with patients and advocacy groups the neuro-oncology community will advance both promising new treatments for primary CNS cancers as well as new approaches to improve the daily lives of survivors across all phases of their illness.
The NCI-CONNECT Program and Survivorship Care in Neuro-Oncology Workshop
The NCI-CONNECT program (cancer.gov/nci-connect) housed in the Neuro-Oncology Branch in the National Cancer Institute’s Center for Cancer Research, was launched in 2017 with support from the National Cancer Moonshot℠ as part of the 21st Century Cures Act. NCI-CONNECT was founded under the first recommendation of the Blue Ribbon Panel, focused on enhancing patient engagement that addresses underserved patient populations, in this case patients with rare CNS cancers. The primary aim of the NCI-CONNECT program is to improve care and treatment for people living with rare CNS tumors by establishing and fostering patient-advocacy-provider partnerships, and networks. The goals of NCI-CONNECT are threefold: (1) to develop a national and international network to facilitate study of these rare cancers; (2) to utilize these networks to collect, analyze and share data to improve understanding of CNS cancers; and (3) to translate these findings into new treatments to improve patient outcomes and patient lives.
In support of its mission, NCI-CONNECT has a comprehensive clinical program that offers a skilled medical team and services to assist patients and family members cope with their illness and has identified issues salient to people living with any primary CNS tumor type that it addresses through research and both provider and lay education. The NCI-CONNECT program has undertaken multiple studies that explore patients’ experiences of living with a primary CNS tumor. For example, the “Evaluation of Natural History and Specimen Banking” study (NCT02851706; PI: TS Armstrong) has enrolled over 900 adults with primary CNS cancers. Evaluation of clinical, treatment and tumor characteristics, and patient-reported outcomes of study participants ≥5 years since initial diagnosis revealed survivors clustered into distinct cohorts based on symptom severity that was irrespective of tumor grade or molecular profile.4 Another large cohort study found that many people with primary CNS tumors reported 10 concurrent symptoms, some of which may be rated as moderate or severe, and this high symptom burden had a deleterious impact on patients’ general health status and health-related quality of life.5 These data demonstrate the critical need for holistic survivorship care programs. Longitudinal symptom assessments to better understand the trajectory of symptoms as well as studies exploring interventions to improve how people feel and function also are needed to develop comprehensive and effective approaches to survivorship care.
Numerous challenges exist in advancing survivorship care within neuro-oncology. The relative rarity of these tumors, lack of evidence-based guidance for treatment, and limited experience of the majority of clinicians who care for these patients, all contribute to survivorship care being understudied and underutilized. An important aspect of the NCI-CONNECT mission is to work collaboratively with nonprofit advocacy organizations that share a common concern for improving the outcomes and lives of patients with rare adult CNS tumors through awareness and education. These partnerships allow outreach to patients who may not be seen in centers of excellence and the provision of direct education regarding tumor types, support programs, symptom management, and approaches to survivorship care for patients, advocacy organizations, and healthcare providers.
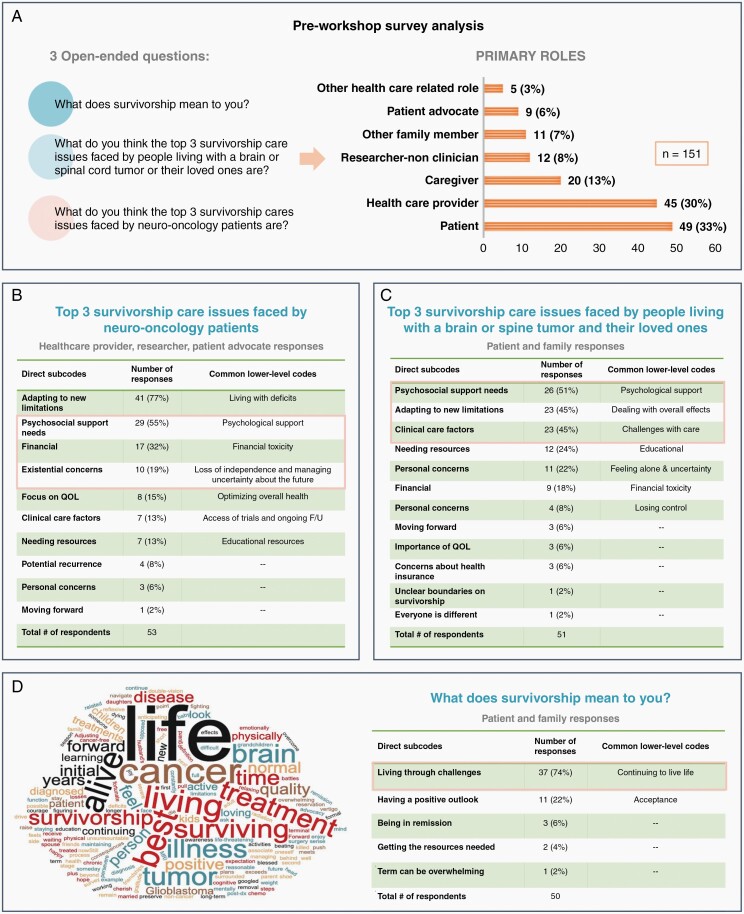
As we began planning for this collaborative workshop, we recognized the crucial importance of understanding what survivorship means to people living with a primary CNS cancer, their caregivers and family members, and neuro-oncology clinicians, and their respective views on what the top survivorship issues are. To explore these topics within the neuro-oncology community, NCI-CONNECT issued an online survey to the Neuro-Oncology Branch’s public Twitter account and NCI-CONNECT private Facebook account. Also, all symposium registrants and workshop invitees received the survey via email. The survey targeted patients and family members, patient advocacy partners, healthcare providers, and researchers, and presented open-ended questions. The survey anonymously asked respondents to identify themselves as either a patient, caregiver, family member, patient advocate, healthcare provider, or researcher so respondents could receive survey questions appropriate to their role. A total of 151 individuals responded (Figure 1A). Among healthcare provider, researcher, and patient advocate respondents, they reported the most common survivorship issues neuro-oncology patients face as learning to live with deficits (77%), need for psychological support (55%), financial toxicity (32%), loss of independence and managing uncertainty about the future (19%) (Figure 1B). When patient and family respondents were asked about the top three survivorship care issues they face, the most common responses were psychosocial support needs (51%), adapting to new limitations (45%), clinical care issues (45%), the need for educational resources (24%), feeling alone and uncertain (22%), and financial toxicity (18%) (Figure 1C). The qualitative survey results from patient and family members identified important and common themes in what survivorship means to them, including “living through challenges,” “having a positive outlook”, “continuing to live life,” “figuring out the new normal,” and “moving past surgery and diagnosis” (Figure 1D).
Figure 1.
Preworkshop survey results analysis. A) List of three open-ended questions created for the survey and reporting of the number of respondents listed by self-identified roles. B) Thematic analysis results of healthcare provider, researcher, patient advocate responses to the question asking their opinion regarding the top three survivorship care issues faced by neuro-oncology patients. C) Thematic analysis results of patient and family member responses to the question asking their opinion regarding the top three survivorship care issues faced by people living with a brain or spine tumor and their loved ones. D) Thematic analysis results and word cloud derived from patient and family responses to what survivorship means to them.
Methods
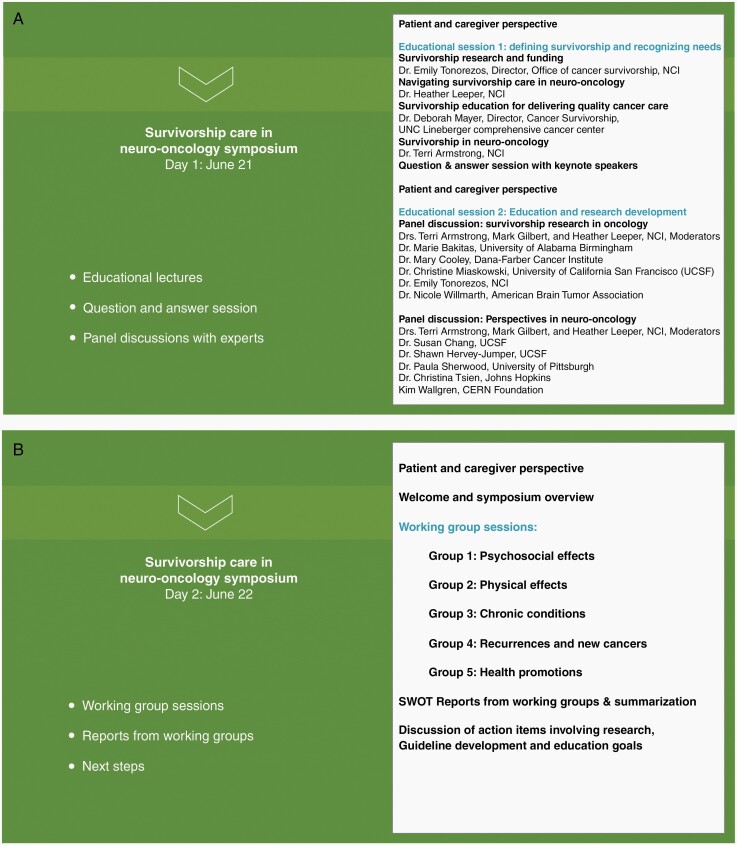
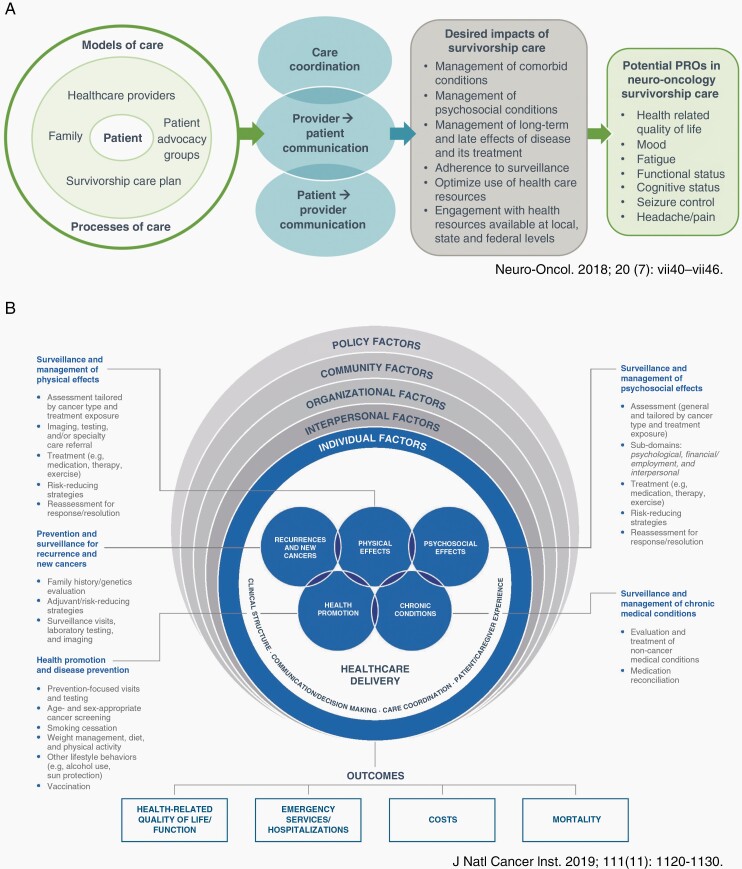
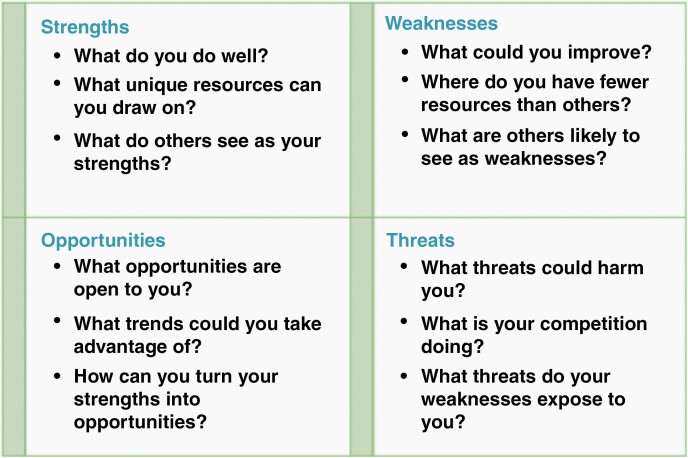
In June 2021, NCI-CONNECT convened a two-day virtual event focused on survivorship care in neuro-oncology, with the goal to identify survivorship care needs in people living with any primary CNS tumor, provide key recommendations and consider critical questions to identify strengths, weaknesses, opportunities and threats to the advancement of survivorship care, and develop recommendations and action items to address these important issues. Day 1’s educational open registration symposium (Figure 2A) featured foundational lectures and panel discussions from interprofessional, multidisciplinary expert speakers, and patient advocates with the goal to provide both lay and professional education, and identify the current ‘state of the science’ regarding oncology and neuro-oncology specific survivorship care (Figure 3A). During Day 2, invited attendees participated in small working groups (Figure 2B) defined by focused areas included in the quality cancer survivorship care framework (Figure 3B) endorsed by the National Cancer Institute Office of Cancer Survivorship.6 Workgroups were formed with consideration of key representation based on expertise in clinical care and research, diversity of professions, and inclusion of an advocacy representative in each group. Members were provided reference material prior to the workshop, including manuscripts discussing the survivorship framework and the S.W.O.T method for organizing the discussion of barriers and opportunities within working groups (Figure 4). Day 2 concluded with presentations by each working group, discussion of recommendations with final action items recommended. The workshop’s discussion of survivorship care focused on the US healthcare system, recognizing differences in cultures and healthcare systems impact the provision survivorship care, and planning for future collaborative expansion with strategic partners outside the US as part of next steps. This manuscript summarizes the proceedings of the workshop and presents the action items.
Figure 2.
Workshop Agenda. (A) Event Day 1 symposium agenda featured expert speakers and panelists who provided foundational education and recommendations to advancing survivorship care and research. (B) Event Day 2 working group agenda included individual group discussion sessions with SWOT reports to the whole group and discussion of action items focused on research, guideline development and education goals with summary of next steps.
Figure 3.
Survivorship care models. A) Proposed model of survivorship care in neuro-oncology leveraging high-quality communication facilitated by survivorship care plans and use of patient-reported outcomes to achieve person-centered outcomes prioritized by neuro-oncology patients. Reprinted with permission. B) Cancer survivorship care quality framework featuring the five domains of individual patient factors corresponding to the workshop’s five working groups. Open use copyright.
Figure 4.
SWOT analysis matrix for assessing the advancement of survivorship care in neuro-oncology.
Event Summary and Results
Event Day 1: Virtual Open Registration Symposium
Foundational Lectures on Defining Survivorship and Recognizing Needs
As a result of cancer survivorship beginning from the time of diagnosis, there are many experiences within survivorship. As survivorship care begins from the time of diagnosis, there are a myriad of issues faced early versus late in the disease trajectory, for those with brain versus spinal cord tumors, and for those facing multiple treatments versus surgery alone or faced with a shorter versus longer disease course or trajectory. In addition, many different types of survivors exist ranging from those living with their cancer to those with no evidence of disease following treatment. Use of the term “cancer survivor” is meant to capture the population with a history of cancer rather than provide a label that may or may not resonate with individuals.
A key concept distinguishing the provision of survivorship care from the provision of usual cancer care is that survivorship care is ultimately about the person who is living with the cancer and the consequences of its diagnosis and treatment. To fully accommodate cancer survivors and the continuum of their unique experiences within the provision of survivorship care, the conceptualization of survivorship care as focused on the illness experience of the person living with the disease is advantageous. From this perspective, the illness experience is influenced by multiple factors (e.g. physical deficits and symptoms, social roles, psychological considerations unique to the individual such as personality traits, beliefs, and sense of purpose and meaning, experiences with past life challenges). This conceptualization of survivorship allows inclusion of individuals receiving continuous treatment to lower the risk of recurrence or progression as well as cancer survivors who have a diagnosis that is likely incurable, which is critically important for neuro-oncology patients for whom “remission” is not applicable in most cases.
Many survivors are unprepared to cope with and manage the panoply of symptoms, functional impairments, shifts in roles, unemployment, or changes in sense of meaning and purpose that arise following their diagnosis or during and after cancer treatment. Cancer survivors have expressed challenges and needs in learning how to live with having cancer in the long term, how to navigate care options and access mental health and psychosocial support, where to obtain relevant, accessible information and resources to manage their care, and find peer support networks.7 Adults living with cancer report having unmet needs warranting earlier intervention, a desire to know more about the realities of living with cancer earlier in their disease trajectory, and better continuity of care across providers and specialties.8
Previous efforts within neuro-oncology to provide education and guidance for survivorship care have included a 2018 CME-approved Neuro-Oncology journal supplement dedicated to survivorship (Neuro-oncology journal supplement), the development of a neuro-oncology patient-specific survivorship care plan endorsed by the Society for Neuro-Oncology available for free as a downloadable PDF from the resources tab at Society for Neuro-Oncology website (Neuro-Oncology Patient Survivorship Care Plan) to be used either in part or whole to guide neuro-oncology providers in survivorship care discussions with their patients and caregivers,9 and a proposed model of survivorship care for neuro-oncology10 (Figure 3A). The recognition that the needs and concerns of people living with a primary CNS tumor may differ from other cancer patient populations in light of the high burden of neurologic symptoms and functional impairments concurrent with cancer- and treatment-related symptoms of the primary CNS tumor patient population led to the development of the neuro-oncology patient-specific survivorship care plan.8
The effects of cancer and its treatment within the survivorship experience can be broadly categorized into physical, cognitive, emotional, social, and financial effects. Patient-centered communication during clinical encounters is essential for high-quality discussions about these effects to take place. Patient-centered survivorship care includes treatment of pain and anxiety as well as discussions about prognosis, goals of treatment, suffering, and advance directives to allow patients and their family members to make well-informed healthcare decisions that are consistent with their values, goals, and preferences. In fact, patient-centered communication is strongly aligned with shared decision-making.11 High-quality survivorship care has the potential to improve patient satisfaction by identifying survivors’ problems, concerns, and issues, increase treatment adherence, improve survivors’ health outcomes and quality of life, and enhance provider well-being.
Foundational Lecture on Survivorship Research and Funding
The National Cancer Institute Office of Cancer Survivorship has updated the scope of survivorship research to be commensurate with the broadening of their definition of cancer survivor and “aims to improve understanding of the sequelae of cancer and its treatment and to identify methods to prevent and mitigate adverse outcomes arising from functional, physical, psychosocial, and economic effects. Survivorship research encompasses and informs the design, delivery, and implementation of evidence-based strategies and the coordination of healthcare services to optimize survivors’ health and quality of life from the time of diagnosis through the remainder of the survivors’ life.”2
The imperative within high-quality survivorship research should be to gain a better understanding of the needs and values of primary CNS cancer survivors and their caregivers in addition to improving how they feel and function. It should focus on approaches to optimize care during and after cancer-directed treatments, including coping with the cumulative stress of living with cancer and fear of recurrence, and aim to address the priorities cited by patients and their families. Survivorship research should decrease healthcare disparities through the inclusion of understudied populations and develop innovative inclusive survivorship care delivery methods. It should also leverage prior symptom research using patient-reported outcomes, particularly in the context of the 2014 Jumpstarting Brain Tumor Drug Development Coalition and FDA clinical trials clinical outcome assessment endpoints workshop, where patients identified quality of life, mood, fatigue, function, cognition, management of seizures, headache, and pain as being outcomes most important to them.12
Panel discussions 1 and 2: Survivorship Research in Oncology and Perspectives in Neuro-oncology
Expert speakers from the fields of oncology and neuro-oncology and patient advocates participated in two panel discussions focused on survivorship research in the field of oncology and perspectives about survivorship care and research in neuro-oncology, respectively (Figure 2A). The panelists were asked to about their perspectives regarding the challenges and opportunities in developing survivorship care guidelines and survivorship research in neuro-oncology, immediate next steps to improve survivorship and support for survivorship research in neuro-oncology, and their recommended next steps to enact change locally and globally. The expert recommendations of Panels and II are respectively provided in Tables 1 and 2.
Table 1.
Recommendations of Expert Panel 1
| The identified challenges and opportunities: |
| • Improve the understanding and awareness of people living with primary CNS tumors and their caregivers as well as their providers about the importance of early and continuous palliative and psychosocial care. |
| • Include caregivers in the neuro-oncology’s further development of survivorship care. |
| • Identify risks for high-symptom burden and optimize the use of health informatics technology to integrate clinical decision support and uniform measures of patient symptom reports into clinical care, which can be leveraged by specialists and community physicians alike. |
| • Create dynamic systems to respond to changing needs of the survivor over time using implementation science and patient-reported outcomes data to promote individualized guideline-based care across health systems, which is critical to optimize health and patient-centered outcomes. |
| • Manage the cost and funding opportunities associated with longitudinal epidemiological studies across the continuum of cancer care and comparisons of common and distinct characteristics among survivors from diverse backgrounds and with different tumor types especially those understudied. |
| • Understand the association of symptom burden with social determinants of health, including race, ethnicity, annual income, caring for children, living alone, unemployment, and stress, all of which may be more impactful on symptoms than clinical characteristics and treatment factors. |
| • Advance toward greater understanding of physiologic mechanisms underlying common symptoms, including cognitive dysfunction and fatigue, to develop more targeted and effective interventions. |
| • Develop more accurate and adequate means for measuring the survivor and caregiver experience about toxicities such as hearing loss and tinnitus to facilitate care independent of complex testing procedures. |
| • Explore opportunities for neuro-oncology to engage with survivorship research and survivorship researchers to engage with neuro-oncology survivors as well as multidisciplinary research. |
| • Increase awareness and education among providers, survivors, and their caregivers about survivors’ care needs regarding delayed effects, health and psychosocial concerns occurring months to years following upfront diagnosis and treatment, and their need for continuity of care, monitoring visits, and referrals to palliative care and psychosocial support resources. |
| • Consider dedicated multidisciplinary survivorship clinics, including neuropsychology, endocrinology, neurology, fertility services, among others to allow survivors and caregivers to see multiple providers and access resources in one visit. |
| • Increase awareness about financial hardships faced by those living with primary CNS tumors especially among those aged 18 to 39 arising from increased healthcare expenses and decreased health insurance access in the face of decreased to no income due to under- or unemployment stemming from their cancer. |
| The following points highlight immediate next steps identified by the expert panelists to improve survivorship and support for survivorship research in neuro-oncology: |
| • Explore opportunities for interventions to address adverse outcomes among CNS tumor survivors, such as technology interventions that track physical activities, including sleep quality and healthful eating. |
| • Improve and establish benefit of survivorship care plans to help patients navigate the healthcare system and understand personalized care recommendations. |
| • Foster collaborative work and alignment with those working on survivorship care plans within oncology survivorship. |
| • Establish and/or expand patient registries to better understand long-term survivorship experiences and needs to enable research and interventions according to identified needs. |
| • Develop patient-reported measures to study symptoms, functional status, and quality of life and to connect them with underlying molecular mechanisms to develop and test treatments for pain, fatigue, and other symptoms. |
| • Align key stakeholders, including survivors, caregivers, and specialty and primary care clinicians, such that the goals and priorities for quality care are both clear and consistent. |
| • Involve end users (clinicians, caregivers, and survivors) in the design and development of health information technology interventions to ensure they are beneficial and useful in practice. |
| • Dedication of more new funding to survivorship research in neuro-oncology and highlighting the applicability of current NCI funding opportunities to neuro-oncology survivorship research such as caregiver, multimorbidity, team-based care. |
| • Develop funding mechanisms that support essential survivorship care research and trials, as well as training grants to engage researchers early in their careers to develop a workforce who are involved survivorship and survivorship care issues. |
Table 2.
Recommendations of Expert Panel 2
| Identified challenges and opportunities to develop robust survivorship care guidelines in neuro-oncology: |
| • Find practical ways to develop, support, and implement personalized risk-stratified survivorship and caregiver care by including palliative care, neuropsychological care, and rehabilitation. |
| • Prioritize new ways to care for patients focused not just on treatment but on their whole lives. |
| • Develop common language across neuroscience, cancer, cognitive science, psychology, patients, and advocates to understand one another and define primary endpoints. |
| • Shift focus from overall survival and disease-free survival to what patients find meaningful, including the ability to work and have relationships. |
| • Incorporate survivorship measures and endpoints into therapeutic clinical trials. |
| • Study primary CNS patients prospectively to develop a database of information highlighting unique challenges in living with primary CNS cancer. |
| • Equip patients with information and tools to advocate for themselves to redefine what it means to be a brain tumor survivor and combat the tendency to disregard survivors with terminal disease. |
| • Address survivorship challenges related to long-term neurological and cognitive effects of treatment and provide education to neuro-oncology providers to improve awareness. |
| • Inspired by advocacy groups, bring people together to address challenges in caregiver research related to limited sample sizes and the need to work across various ethnic and cultural backgrounds. |
| The following highlights ideas from panelists on what can be done locally and globally to improve survivorship care: |
| • Establish ongoing, concrete, and regular collaborations. |
| • Familiarize all stakeholders with definitions of survivorship and outcomes to measure. |
| • Engage local providers in the community in research efforts to meet survivors where they are and develop approaches to improve survivorship care that works outside of cancer centers. |
| • Collect survivorship and outcomes data in accurate and consistent ways to enable comparisons across institutions and studies. |
| • Maximize electronic health records, insurance databases, data science, and genome sequencing, as resources to expedite achieving results. |
| • Reach out to underserved groups with concrete steps and clear metrics for success to ensure that advances in survivorship care are accessible to all patients. |
| • Expand and capitalize on the realization that some of the challenges in primary CNS cancer survivors occur in survivors of other cancers, related to chemo-brain, immunotherapy side effects, such that progress in survivorship care for CNS cancers will have an impact in the larger cancer community. |
Event Day 2: Working Groups on Advancing Survivorship Research and Care
Event Day 2 was dedicated to discussions focused on advancing survivorship research and care within five small workgroups corresponding to the quality cancer survivorship care framework’s five domains: (1) psychosocial effects, (2) physical effects, (3) chronic conditions, (4) recurrences and new cancers, and (5) health promotion (Figure 2B).6 Groups were charged with working collaboratively to develop key action items to expedite and support survivorship care and research in neuro-oncology focusing their discussions within their specific domain (Figure 3B). Participants were invited clinicians, researchers, and patient advocates from across the neuro-oncology community; they along with supporting Neuro-Oncology Branch staff are coauthors in recognition of their important contributions with their names listed in alphabetical order by working group in the Acknowledgements section. A total of 82 individuals participated in the working groups. Group members were asked to share their perspectives and the SWOT analysis framework was used to facilitate discussions and identify Strengths, Weaknesses, Opportunities, and Threats (Figure 4). Summaries of each working group’s SWOT analysis discussions are as follows:
Group 1: Psychosocial Effects
Session Lead: Dr. Heather Leeper, NOB, CCR, NCI
Co-lead: Alvina Acquaye, NOB, CCR, NCI
A diagnosis of a primary CNS cancer comes with many psychological and social effects worsened by stress, fatigue, and anxiety. The diagnosis can lead to challenges related to finances, employment, and interpersonal difficulties. Strengths and opportunities identified for improving survivorship care in this domain include the ability to follow survivors across their illness trajectories and engage them in holistic clinical interactions, the deep passion and interest among neuro-oncology care providers to work together with their patients and caregivers and collaborate across specialties, and the ability to leverage patient advocacy groups and patient navigators to deliver first line psychosocial support. Telehealth, social media and online platforms, and funding for training opportunities represent additional opportunities for advances in survivorship care aimed at addressing the psychosocial effects of rare CNS cancers.
Challenges to overcome in addressing psychosocial effects of CNS cancers include a sense of nihilism, or the notion that such cancers are a “death sentence” and therefore survivorship is not applicable. Patients with primary CNS cancers often are excluded from clinical research because they may have cognitive impairments related to the cancer and its treatment. Other obstacles include a lack of training and funding for survivorship care. Despite the advantages of telehealth for reaching patients where they are, it may contribute to inequities if not implemented appropriately.
Group 2: Physical Effects
Session Lead: Dr. Terri Armstrong, NOB, CCR, NCI
Co-lead: Elizabeth Vera, NOB, CCR, NCI
Survivors of cancers including CNS cancers are at increased risk for a variety of physical effects. Neuro-oncology is a small, tight-knit field with an emphasis on multidisciplinary and collaborative care with strong patient advocacy groups. While these strengths should facilitate the delivery of survivorship care, numerous challenges need to be overcome related to the fact that most patients do not receive neuro-oncologic care at academic Centers of Excellence, and when they do it is often after initial diagnosis and treatment. Many patients would benefit from survivorship care to address physical effects of the cancer and its treatment earlier in their survivorship experience.
Even after patients begin seeing providers at Centers of Excellence, a disconnect exists between community and academic providers. Survivors may struggle with disjointed or conflicting opinions from multiple providers, contributing to survivors and their caregivers feeling overwhelmed and uncertain. Some providers may not address symptom burden or the burdens on caregivers. Limited research funding, training, insurance coverage, and awareness present significant hurdles to survivorship care focused on the physical effects of CNS cancers. Significant opportunities exist to develop survivorship care recommendations focused on CNS cancers and include survivorship principles in neuro-oncology NCCN guidelines.
Group 3: Chronic Conditions
Session Lead: Dr. Mark Gilbert, NOB, CCR, NCI
Many people with CNS cancers have other chronic conditions that may be preexisting or arise following cancer diagnosis and treatment. While neuro-oncology providers may be skilled in listening to patient concerns and working together in a multidisciplinary approach to care, the neuro-oncology teams tend not to have close working relations with their patients’ primary care providers. Furthermore, gaps in communication may occur during patient transitions from inpatient to outpatient care and a lack of consistent follow-up care may exist. Too few patients are offered and receive needed rehabilitation services and care.
Opportunities exist to work toward policy changes to improve medication reconciliation and develop multidisciplinary survivorship clinics that implement consistent strategies to monitor patients’ long-term health and treatment effects. Questions related to survivorship need to be incorporated into clinical trials and electronic health records should be leveraged for outcomes research. Opportunities exist for research into genetic assessments of toxicity risks and for studies to evaluate the underlying determinants of chronic conditions related to long-term sequelae of CNS cancer and cancer treatment to develop and test more targeted interventions.
Group 4: Recurrences and New Cancers
Session Lead: Dr. Marta Penas-Prado, NOB, CCR, NCI
In CNS cancers, differentiation of the effects of a recurrence from the effects of prior treatments is often challenging. New imaging techniques and other tools, such as liquid biopsy, may become opportunities due to lower cost and/or greater access, but lack validation, standardization, and guidance for their use in CNS cancers. To identify those at risk for developing additional cancers due to hereditary conditions, family history is important. However, use of family history information is not standardized in clinical practice. Similarly, no clear guidance is available regarding genetic counseling and testing for CNS cancer survivors. These weaknesses present opportunities for improvement in survivorship care to address recurrences and new cancers.
The neuro-oncology community should leverage genetic counselors as a resource and incorporate them into their teams. Genetic counselors could advise on genetic testing and family history and aid in interpreting the results along with providing counseling. Molecular testing including germline genetic testing may be useful for guiding surveillance and assessing risks and yet a lack of insurance coverage currently limits their use. Neuro-oncology providers also may hesitate to obtain the tissue needed for such testing, which may benefit from improved systems for communication to resolve. There are challenges when it comes to ensuring that patients understand their risks and need for ongoing surveillance without feeling paralyzed by the prospect of their cancer coming back.
Group 5: Health Promotions
Session Lead: Dr. Emily Tonorezos, NCI
Co-lead: Dr. Amanda King, NOB, CCR, NCI
Important strengths exist in the relationships between the neuro-oncology team, patients, and caregivers, who are often very engaged. The window of time prior to surgery presents an opportunity for health behavior interventions or “pre-hab.” Germline genetic testing and association between CNS cancers and heritable cancer syndromes present opportunities for interventions to reduce the risk of subsequent cancer. Interventions for preventive care, such as increasing availability of high-dose flu vaccination, could also benefit this population.
Challenges occur in the conduct of research focused on health promotion in CNS cancer survivors. CNS cancer survivors may be susceptible to misinformation as they look for opportunities to improve their own health. Rapid changes in patient care needs and difficulties in other domains, including mental health and economic hardship, may make lifestyle interventions such as tobacco cessation, healthy diet, and physical activity seem less important. A substantial opportunity exists to improve survivorship care through greater use of interventions including cognitive rehabilitation, reaching more patients with specialized care via telehealth, and group visits to highlight wellness. Follow-up clinic visits for follow-up care and cancer surveillance that are often life-long could provide opportunities for interventions focused on exercise, nutrition, and wellness.
Workshop Conclusions, Recommendations, and Action Plan
This report summarizes the discussion and recommendations from the NCI-CONNECT Survivorship Care in Neuro-Oncology Workshop. While survivorship and survivorship care in primary CNS cancers present many challenges, many strengths can be leveraged to advance survivorship care across the five domains. Neuro-oncology is a small, multidisciplinary field with providers who are deeply engaged in working together with patients and their families. NCI-CONNECT makes an important contribution to advancing the field and survivorship care through its ability to bring together patients, caregivers, advocacy groups, clinicians, and researchers as demonstrated by this workshop focused on survivorship and survivorship care. These efforts are an extremely important step toward developing a common understanding and standardized language for survivorship care that can be shared and used to inform the core curriculum in educating healthcare providers and the neuro-oncology community at large.
CNS cancers come with inherent challenges for survivorship, including the incurable nature of most cancer types, rare incidence, and their highly varied consequences and outcomes. Though a specialty with strong foundations in both oncology and neurology, neuro-oncology largely lacks evidence to support clinical recommendations and established guidelines for survivorship care for its unique patient population. A need exists to establish evidence-based recommendations and identify areas that warrant additional evidence through research that will enable the development of comprehensive survivorship care. The growing use of telehealth presents important opportunities to improve the delivery of survivorship care, particularly if these opportunities expand access and improve provider reimbursement. However, survivorship and survivorship care need to be incorporated into neuro-oncology clinical trials, training, funding, and other supports need to be expanded.
The NCI-CONNECT program within the Neuro-Oncology Branch at the National Cancer Institute is well-positioned to address survivorship care needs through leveraging partnerships and continue engagement of stakeholders in key areas addressed in the action items. Strategic partnerships are being formed based on these action items to further define measurable and achievable short and long-term goals and form working groups. Ongoing work will be shared through public and professional forums and publications. The action items and next steps to advance survivorship care and research in neuro-oncology developed during the workshop include (Figure 5):
Figure 5.
Summary of workshop action items.
Engage and leverage partnerships to seek endorsement of this report.
Engage and leverage partnerships to decrease barriers to and provider reimbursement for survivorship care (including but not limited to: advanced care planning, acute and chronic illness management, and management of symptoms and side effects of disease and treatment).
Engage and leverage partnerships to advance survivorship research in neuro-oncology with NIH grants and private grant support organizations.
Develop a survivorship tool kit for providers, people living with primary CNS cancers, and their caregivers
Develop accessible educational content on survivorship care in neuro-oncology as guidance for neuro-oncology, neurology, oncology, and primary care providers as part of standardized resources such as NCCN’s guidelines for Central Nervous System Cancers.
Develop core competencies for survivorship care for neuro-oncology providers to be included in training and standardized exams.
NCI-CONNECT regularly holds workshops to address important issues and needs in the diagnosis, treatment, care, and fundamental understanding of rare CNS cancers. The goal of this workshop is to bring important information and needs forward, to develop a toolkit to engage others working in this arena as well as key stakeholders, and to develop collaborations to address important issues and improve survivorship and survivorship care. Future plans include collaborative expansion beyond the US healthcare system through the NCI-CONNECT program’s partnership with international patient advocacy organizations. Living with a rare brain or spinal cord tumor impacts all aspects of a person’s life in many ways. To advance the understanding of rare CNS cancers and improve approaches to its care and treatment, it is essential to keep survivorship and survivorship care concerns at the forefront.
Acknowledgments
Brittany Cordeiro, Program Manager; Katie Blackburn, Business Manager; Kristin Odom, Communications Editor; Kendall Morgan, Freelance Writer/Editor; Alexa Christ, Research Associate; Tuesday Haynes, Summer Intern; Varna Jammula, CRTA Fellow; McKenzie Kauss, Summer Intern; Yeonju Kim, CRTA Fellow; Edina Komlodi-Pasztor, Clinical Fellow; Molly Maher, Communications Fellow; Hope Miller, CRTA Fellow; Kayla Roche, CRTA Fellow; James Rogers, CRTA Fellow; Michael Timmer, CRTA Fellow; Alex Wollet, CRTA Fellow.
Contributor Information
NCI-CONNECT Survivorship Care in Neuro-Oncology Workshop:
Terri S Armstrong, Heather E Leeper, Mark R Gilbert, Alvina Acquaye, Jean Arzbaecher, Marie Bakitas, J Nicholas Dionne-Odom, Karen Fink, Christi Hayes, Heather Leeper, Nicole Lollo, Ashlee Loughan, Kathy Oliver, Kayla Roche, Paula Sherwood, Sylvia Stearn, Michael Timmer, Christina Amidei, Jaishri Blakeley, David Cachia, Laura Cooke, Mary Cooley, Vinai Gondi, Danielle Leach, Tito Mendoza, Christine Miaskowski, Kendall Morgan, Burt Nabors, Kristie Naines, James Rogers, Akanksha Sharma, Elizabeth Vera, Kathleen Wall, Shiao-Pei Weathers, Alex Wollet, David Arons, Maria Boccia, Kevin Camphausen, Alexa Christ, Karl Cristie Figuracion, Mark Gilbert, Shawn Hervey-Jumper, Edina Komlodi-Pasztor, Frank Lieberman, Mark Malkin, Hope Miller, Nina Paleologos, Marissa Panzer, Nicole Stout, Patrick Wen, Sarah Beam, Lisa Boris, Ekokobe Fonkem, Varna Jammula, McKenzie Kauss, Yeonju Kim, Byram H Ozer, Edward Pan, Marta Penas-Prado, Stephanie Pugh, Roy Strowd, Christina Tsien, Kimberly Wallgren, Jing Wu, Kareem Zaghloul, Susan Bell, Susan Chang, Erin M Dunbar, Chas Haynes, Tuesday Haynes, Amanda L King, Glenn Lesser, Deborah Mayer, Molly Maher, Lily Polskin, Tina Pillai, and Emily Tonorezos
Funding
The NCI Comprehensive Oncology Network for Evaluating Rare CNS Tumors (NCI-CONNECT) is a program within the Rare Tumor Patient Engagement Network (RTPEN), an initiative supported by Cancer Moonshot℠ funds and managed at the National Institutes of Health, National Cancer Institute, Center for Cancer Research, Neuro-Oncology Branch.
NCI-CONNECT Adult Survivorship Workshop—Full List of Participants
Workshop Chairs
Terri S. Armstrong, PhD, ANP-BC, FAAN, FAANP, Patient Outcomes Team Lead, Deputy Chief
Heather E. Leeper, MD, MSc, Associate Research Physician, Patient Outcomes Team
Mark R. Gilbert MD, Branch Chief
NIH/NCI/CCR/NOB
NCI-CONNECT Co-leaders:
Terri S. Armstrong PhD, ANP-BC, FAAN, FAANP
Mark R. Gilbert MD
NIH/NCI/CCR/NOB
Workshop Participants (in alphabetical order by last name):
Working Group 1: Psychosocial Effects
Alvina Acquaye, LCPC, Psychosocial Behavioral Specialist (Group Co-leader), NOB, CCR, NCI, NIH
Jean Arzbaecher, APN, Neuro-Oncology, University of Illinois at Chicago
Marie Bakitas, DNC, Palliative Care, University of Alabama at Birmingham
J Nicholas Dionne-Odom, PhD, RN, School of Nursing, University of Alabama at Birmingham
Karen Fink, MD, Neuro-Oncology, Baylor University Medical Center
Christi Hayes, APN, Neurosurgery, NIH
Heather Leeper, MD, Neuro-Oncology (Group Leader), NOB, CCR, NCI, NIH
Nicole Lollo, NP, Neuro-Oncology, NOB, CCR, NCI, NIH
Ashlee Loughan, PhD, Neuropsychology, Virginia Commonwealth University
Kathy Oliver, Patient Advocate, International Brain Tumour Alliance
Kayla Roche, CRTA Fellow, NOB, CCR, NCI, NIH
Paula Sherwood, PhD, RN, Nursing Science Researcher, University of Pittsburgh
Sylvia Stearn, MSW, LICSW, Clinical Social Worker, SWD, Clinical Center, NIH
Michael Timmer, CRTA Fellow, NOB, CCR, NCI, NIH
Working Group 2: Physical Effects
Terri Armstrong, PhD, Neuro-Oncology (Group Leader), NOB, CCR, NCI, NIH
Christina Amidei, PhD, Neurosurgery, Northwestern Medicine
Jaishri Blakeley, MD, Neuro-Oncology, Johns Hopkins University
David Cachia, MD, Neuro-Oncology, Medical University of South Carolina
Laura Cooke, Patient Advocate, Brains for the Cure
Mary Cooley, PhD, RN, Oncology, Dana-Farber Cancer Center
Vinai Gondi, MD, Radiation Oncology, Northwestern
Danielle Leach, Patient Advocate, National Brain Tumor Society
Tito Mendoza, PhD, Health Outcomes Research, The University of Texas MD Anderson Cancer Center
Christine Miaskowski, PhD, RN, School of Nursing, University of California San Francisco
Kendall Morgan, Freelance Writer/Editor, NIH
Burt Nabors, MD, Neuro-Oncology, University of Alabama Birmingham
Kristie Naines, Patient Advocate, Brain Tumor Network
James Rogers, CRTA Fellow, NOB, CCR, NCI, NIH
Akanksha Sharma. MD, Neuro-Oncology, Pacific Neuroscience Institute
Elizabeth Vera, Bio-Behavioral Research Analyst (Group Co-leader), NOB, CCR, NCI, NIH
Kathleen Wall, RN, Neuro-Oncology, NOB, CCR, NCI, NIH
Shiao-Pei Weathers, MD, Neuro-Oncology, The University of Texas MD Anderson Cancer Center
Alex Wollet, CRTA Fellow, NOB, CCR, NCI, NIH
Working Group 3: Chronic Conditions
David Arons, JD, Patient Advocate, National Brain Tumor Society
Maria Boccia, PhD, Neuroscience and Psychology, Baylor University
Kevin Camphausen, MD, Radiation Oncology, NIH
Alexa Christ, Research Associate, NOB, CCR, NCI, NIH
Karl Cristie Figuracion, APN, Neuro-Oncology, University of Washington Seattle
Mark Gilbert, MD, Neuro-Oncology (Group Leader), NOB, CCR, NCI, NIH
Shawn Hervey-Jumper, MD, Neurosurgery, University of California San Francisco
Edina Komlodi-Pasztor, PhD, MD, Neuro-Oncology Fellow, NOB, CCR, NCI, NIH
Frank Lieberman, MD, Neuro-Oncology, University of Pittsburgh
Mark Malkin, MD, Neuro-Oncology, Virginia Commonwealth University
Hope Miller, CRTA Fellow, NOB, CCR, NCI, NIH
Nina Paleologos, MD, Neuro-Oncology, Advocate Health Care
Marissa Panzer, DNP, AGNP, Neuro-Oncology, NOB, CCR, NCI, NIH
Nicole Stout, DPT, FAPTA, Function and Rehabilitation, West Virginia University
Patrick Wen. MD, Neuro-Oncology, Dana-Farber Cancer Institute
Working Group 4: Recurrences and New Cancers
Sarah Beam, APRN, Neurosurgery, OSF HealthCare
Lisa Boris, NP, Neuro-Oncology, NOB, CCR, NCI, NIH
Ekokobe Fonkem, MD, Neuro-Oncology, Barrow Neurological Institute
Varna Jammula, CRTA Fellow, NOB, CCR, NCI, NIH
McKenzie Kauss, Summer Intern, NOB, CCR, NCI, NIH
Yeonju Kim, CRTA Fellow, NOB, CCR, NCI, NIH
Byram H. Ozer, PhD, MD, Neuro-Oncology, Johns Hopkins University
Edward Pan, MD, Neuro-Oncology, University of Texas Southwestern Medical Center
Marta Penas-Prado, MD, Neuro-Oncology (Group Leader), NOB, CCR, NCI, NIH
Stephanie Pugh, PhD, Health Outcomes Research, NRG Oncology
Roy Strowd, MD, Neuro-Oncology, Wake Forest University
Christina Tsien, MD, Radiation Oncology, Johns Hopkins University
Kimberly Wallgren, Patient Advocate, CERN Foundation, a program of the National Brain Tumor Society
Jing Wu, MD, Neuro-Oncology, NOB, CCR, NCI, NIH
Kareem Zaghloul, MD, Neurosurgery, NIH
Working Group 5: Health Promotions
Susan Bell, APRN, Neuro-Oncology, Allied Health Representative, Society for Neuro-oncology
Susan Chang, MD, Neuro-Oncology, University of California San Francisco
Erin M. Dunbar, MD, Neuro-Oncology, Piedmont Brain Tumor Center, Piedmont Healthcare
Chas Haynes, Executive Director, Society for Neuro-Oncology
Tuesday Haynes, Summer Intern, NOB, CCR, NCI, NIH
Amanda L. King, PhD, iCURE Fellow, Health Outcomes Research (Group Co-leader), NOB, CCR, NCI, NIH
Glenn Lesser, MD, Neuro-Oncology, Wake Forest University
Deborah Mayer, PhD, RN, Oncology, University of North Carolina at Chapel Hill
Molly Maher, Communications Fellow, NOB, CCR, NCI, NIH
Lily Polskin, NP, Neuro-Oncology, NOB, CCR, NCI, NIH
Tina Pillai, NP, Neuro-Oncology, NOB, CCR, NCI, NIH
Emily Tonorezos, MD, Office of Cancer Survivorship (Group Leader), NCI, NIH
Conflict of interest statement: SC: Agios (institutional research support), AstraZeneca (scientific advisory board member). No conflicts: HL, ET, DM, MB, MC, SHJ, CM, PS, CT, KW, NW, DA, AA, AK, MPP, EV, MG, TA and all other workshop attendees listed at the end of the manuscript.
Authorship statement. All listed authors participated in the Survivorship Workshop, have been involved in the writing of the manuscript, and have read and approved the final version.
References
- 1. National Coalition for Cancer Survivorship: Our history. Available at https://canceradvocacy.org/about/our-history/. Accessed November 3, 2021.
- 2. National Cancer Institute Office of Cancer Survivorship. Statistics, graphs and definitions. Available at https://cancercontrol.cancer.gov/ocs/statistics#definitions. Accessed November 3, 2021.
- 3. Hewitt M, Greenfield S, Stovall E, et al. From cancer patient to cancer survivor: Lost in transition. Washington DC:National Academies Press; 2006. Available at https://canceradvocacy.org/wp-content/uploads/2013/01/From-Cancer-Patient-to-Cancer-Survivor-Lost-in-Transition-Summary-.pdf. Accessed on December 3, 2021. [Google Scholar]
- 4. Rogers JL, Vera E, Acquaye A, Briceno N, et al. Living with a central nervous system (CNS) tumor: findings on long-term survivorship from the NIH Natural History Study. Neurooncol Pract. 2021; 8(4):460–474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Armstrong TS, Vera-Bolanos E, Acquaye AA, et al. The symptom burden of primary brain tumors: evidence for a core set of tumor- and treatment-related symptoms. Neuro-Oncol. 2016; 18(2):252–260. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Nekhlyudov L, Mollica MA, Jacobsen PB, et al. Developing a quality of cancer survivorship care framework: implications for clinical care, research, and policy. J Natl Cancer Inst. 2019; 111(11):1120–1130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Mead KH, Raskin S, Willis A, et al. Identifying patients’ priorities for quality survivorship: conceptualizing a patient-centered approach to survivorship care. J Cancer Surviv. 2020; 14(6):939–958. [DOI] [PubMed] [Google Scholar]
- 8. Shakeel S, Tung J, Rahal R, Finley C.. Evaluation of factors associated with unmet needs in adult cancer survivors in Canada. JAMA Netw Open. 2020; 3(3):e200506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Leeper HE, Acquaye AA, Bell S, et al. Survivorship care planning in neuro-oncology. Neuro-Oncol Pract. 2018; 5(1):3–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Leeper HE, Milbury K. Survivorship care planning and implementation in neuro-oncology. Neuro-Oncol. 2018; 20(7):vii40–vii46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Levit L, Balogh E, Nass S, et al. , eds. Delivering High-Quality Cancer Care: Charting a New Course for a System in Crisis. Washington, D.C.: National Academies Press (US); 2013. [PubMed] [Google Scholar]
- 12. Helfer JL, Wen PY, Blakeley J, Gilbert MR, Armstrong TS. Report of the jumpstarting brain tumor drug development coalition and FDA clinical trials clinical outcome assessment endpoints workshop (October 15, 2014, Bethesda MD). Neuro-Oncology. 2016; 18(2): ii26–ii36. [DOI] [PMC free article] [PubMed] [Google Scholar]