Abstract
The COVID-19 pandemic has led to increased mental health concerns, including depression and anxiety among parents and internalizing and externalizing problems among youth. To better understand the mechanisms and moderators of child mental health during the pandemic, the current study tested two moderated mediation models in which parent depression and anxiety indirectly impacted child internalizing and externalizing problems through negative effects on multiple parenting variables, with these associations moderated by families’ exposure to COVID-19-stressors. A national sample representative of U.S. parents (N = 796, 48.2% female, Mage = 38.87 years, 60.3% Non-Hispanic white, 18.1% Hispanic/Latinx, 13.2% Non-Hispanic Black/African-American, 5.7% Asian, 2.8% Other Race) completed a cross-sectional online survey in February-April 2021. Children ranged from 5–16 years old (Mage = 10.35 years, 59.8% Non-Hispanic white, 17.2% Hispanic/Latinx, 13.7% Non-Hispanic Black/African-American, 4.5% Asian, 4.8% Other Race). Parent depression/anxiety was directly and indirectly associated with child internalizing and externalizing problems. For both internalizing and externalizing problems, indirect associations occurred by means of increased parent hostility and inconsistent discipline and decreased routines and parent supportiveness. There were also specific indirect effects through decreased monitoring (internalizing problems) and parenting self-efficacy (externalizing problems). Multiple indirect effects were moderated by number of COVID-19-stressors experienced. Notably, COVID-19-stressors did not have direct effects on child mental health when other variables were considered. Findings highlight the buffering effects of parents for child mental health, the need to address parent depression/anxiety in child interventions, the utility of existing evidence-based parent interventions during the pandemic, and the need to assess families’ level of exposure to COVID-19-stressors.
Supplementary Information
The online version contains supplementary material available at 10.1007/s10802-022-00920-6.
Keywords: Parent depression, Parent anxiety, Families, Child mental health, Moderated mediation, COVID-19 pandemic
The COVID-19 pandemic has resulted in unprecedented levels of illness and significant mortality, changed day-to-day life for families across the world, and led to adverse outcomes for many families, including detrimental consequences for the mental health of many children and parents (Alzueta et al., 2021; Gadermann et al., 2021; Patrick et al., 2020). Parents have reported increased mental health concerns relative to non-parent adults (Gadermann et al., 2021; Pierce et al., 2020), particularly depression and anxiety (Cameron et al., 2020; Feinberg et al., 2021). Research on child mental health during the pandemic has shown impacts in terms of increased behavior problems (externalizing) as well as depression and anxiety symptoms (internalizing) (Feinberg et al., 2021; Glynn et al., 2021; Khoury et al., 2021; Waller et al., 2021). At the same time, a few studies have also demonstrated reductions, no change, or both increases and decreases in youth mental health symptoms (e.g. Breaux et al., 2021; Penner et al., 2021). Overall, research is increasingly illustrating heterogeneity in the mental health consequences of the pandemic (Shevlin et al., 2021). Given this variability, and in order to effectively intervene in mental health concerns for youth and families going forward, it is important to further examine mechanisms and moderators of child mental health during the pandemic to understand how and for whom poor mental health has occurred. To do so, the current study evaluated two moderated mediation models in which parent depression and anxiety indirectly impact child internalizing and externalizing problems through negative effects on multiple parenting variables, with these associations moderated by families’ level of COVID-19-stressors.
The current study anchors to and builds on a conceptual model of family risk and resilience during the COVID-19 pandemic put forward by Prime and colleagues (2020). Based on extant models and literature on adversity and family well-being, Prime et al. outlined a conceptual framework which suggested that child mental health during the pandemic would be impacted by parents’ mental health symptoms through the effects of parent mental health on multiple family subsystems (parent–child, marital, sibling, and whole family). With regard to the parent–child subsystem specifically—the focus of the current study—Prime and colleagues discussed how stress related to the pandemic could drain the mental health resources of parents and lead to ineffective parenting behaviors, such as increases in harsh and coercive parenting, decreases in warmth, and disruptions in home routines. These parenting factors have been robustly linked to poor outcomes for child mental health (Prime et al., 2020), and therefore, alteration of these processes during the pandemic may detrimentally impact child mental health.
Several studies have since begun to empirically test paths within Prime and colleagues’ proposed model. For example, recent research has demonstrated links between parent and child mental health during the pandemic, in terms of parents’ worries about COVID-19 and child conduct problems (Waller et al., 2021), parents’ emotional health and children’s emotional and behavioral health (Bate et al., 2021), and parent depression and anxiety and child psychological difficulties (Moulin et al., 2021). Poor parent mental health prior to the pandemic has also been associated with children’s internalizing and externalizing during the pandemic (Fosco et al., 2021). In another longitudinal study, maternal anxiety was associated with greater increases in child internalizing behaviors during the pandemic, and parent hostility was associated with greater increases in child externalizing behaviors (Khoury et al., 2021). More family routines during the pandemic have been associated with fewer internalizing and externalizing problems in children (Glynn et al., 2021), and greater family functioning has also been associated with fewer mental health problems in youth during the pandemic (Penner et al., 2021). In addition, parent depression during the COVID-19 pandemic has been associated with lower quality parenting (Roos et al., 2021) and with greater child-parent relationship conflict (Russell et al., 2020). The collective body of this emerging literature provides evidence for individual links within the Prime et al. (2020) model. The current study builds on this prior literature by concurrently testing multiple links within the model.
Parenting variables as mediating and moderating influences for child mental health during the pandemic are also beginning to be identified. For instance, recent COVID-19-focused studies have found that parenting self-efficacy mediates the relationship between parents’ psychological distress and children’s emotion regulation and lability/negativity (Morelli et al., 2020), and that decreases in family cohesion and increases in conflict, harsh discipline, and lax discipline are associated with increases in child internalizing and externalizing problems during the pandemic (Fosco et al., 2021). In addition, stronger links between parent and child emotional health were observed among families with greater relationship conflict and lower positivity during the pandemic (Bate et al., 2021), and COVID-19-related family stress had stronger impacts on children’s mental health for families who reported less frequent emotion coaching of their children’s negative emotions (Cohodes et al., 2021).
Taken together, this growing evidence confirms that parent mental health during COVID-19 may have direct, detrimental impacts on parenting quality and on child mental health, and that parenting quality, and change in parenting quality during the pandemic, also significantly impacts child mental health. This research has also begun to identify parent and family factors (e.g., routines, family functioning, parent self-efficacy, family conflict and cohesion, harsh and lax discipline, relationship conflict, positivity, emotion coaching) that appear to exacerbate or protect child mental health during the pandemic. A primary limitation of the above, however, which we also aim to address in the current study, is that parenting behavioral, emotional, and cognitive processes have been effectively tested in isolation, preventing a comprehensive test of their relative influence on child mental health.
The current study aims to add to this growing research by evaluating the impact of parent depression and anxiety on children’s internalizing and externalizing problems during the pandemic, and specifically by testing whether these relationships are mediated through the impact of parent depression and anxiety on multiple parenting variables. This research was designed to test a key portion of Prime and colleagues’ (2020) conceptual model, focusing on mediators specifically within the parent–child subsystem (versus marital, sibling, or family-level factors), based on the model’s hypothesized direction of influence among constructs. The current study is unique in that it simultaneously tests multiple parenting constructs as mediators in order to understand which are most important mechanistically in the path between parent depression/anxiety and child mental health during the pandemic, and therefore which are most important to address in the context of child mental health interventions. Further, we focused on behavioral (e.g. discipline, supervision, positive reinforcement, routines), affective (harsh parenting, emotional support), and cognitive (parenting self-efficacy) parenting mediators in order to pinpoint modifiable factors that can be addressed with existing evidence-based parent interventions (Arnsten et al., 2021). The present study also sought to uniquely add to the literature by testing how exposure to COVID-19 stressors affects the pathways between parent mental health, parenting, and child mental health during the pandemic. An absence of associations in the context of direct influences of COVID-19 impacts would indicate that modifications to existing programs or additional COVID-19 specific interventions would be necessary to develop. Given that some families have experienced more COVID-19-related events than others (e.g. illness, death, job loss; Kazak et al., 2021), family pathways to child internalizing and externalizing during the pandemic likely vary as a function of level of exposure to COVID-19 stressors (Cohodes et al., 2021), and it is important to understand how differing levels of exposure to COVID-19 events modulates these pathways.
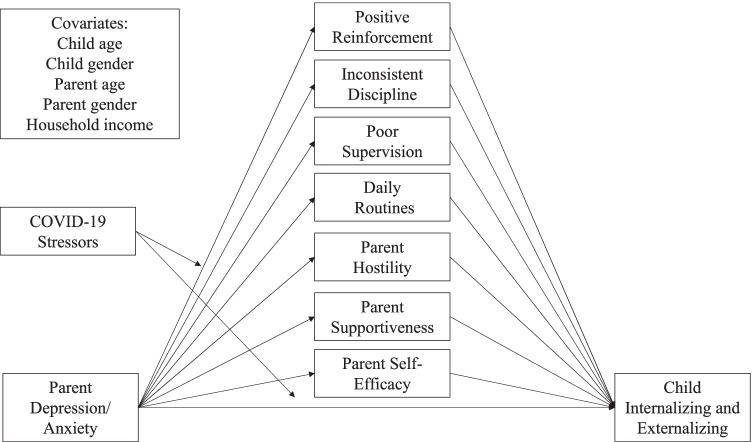
Therefore, the aim of this study was to test two moderated mediation models explaining variation in child internalizing (Model 1) and externalizing (Model 2) problems during the pandemic (see Fig. 1 for conceptual models). We hypothesized that greater levels of parent depression and anxiety would be a) directly associated with greater levels of child internalizing and externalizing and b) indirectly associated with greater levels of child internalizing and externalizing through negative impacts on parenting factors (i.e., higher levels of inconsistent discipline, poor supervision, and parent hostility; lower levels of positive reinforcement, routines, parent supportiveness, and parenting self-efficacy). We also hypothesized that level of exposure to COVID-19 stressors would moderate these associations, such that parent depression and anxiety would have c) stronger associations with negative parenting outcomes as well as stronger d) direct and e) indirect effects on child internalizing and externalizing when families’ exposure to COVID-19 stressors was higher. To understand specificity in terms of which parenting variables play mechanistic roles in child internalizing and externalizing, and to permit mapping onto parenting mechanisms emphasized in existing clinical interventions, we utilized independent observed parenting variables rather than taking a latent variable approach, and tested internalizing and externalizing in separate models. To evaluate these questions as they pertain to parents and children in the U.S. broadly, the study used a national sample of parents, with income, race/ethnicity, and regional distributions matching U.S. demographics, including representation from mothers and fathers and from parents of children 5–16 years old. Further, because child internalizing and externalizing presentation and incidence differ across child and adolescent development (Merikangas et al., 2010), including during the pandemic, when older youth have reported greater mental health concerns (Stinson et al., 2021), and because parenting variables may differ by developmental period of the child—particularly behavioral factors such as reinforcement, discipline, supervision, and routines (Locke & Prinz, 2002; Parent & Forehand, 2017), we also conducted supplemental multi-group analysis in which both internalizing and externalizing models were tested separately in the three age groups (ages 5–8, 9–12, and 13–16). We hypothesized that parenting behaviors reflecting more parental control (e.g. reinforcement, discipline, routines) would have stronger effects in the younger age groups whereas supervision and supportiveness would have stronger effects in the adolescent group, when youth typically spend more time independent from parents. Overall, this study sought to shed light on individual differences in family pathways to child mental health problems during the COVID-19 pandemic.
Fig. 1.
Conceptual moderated mediation model 1 (child internalizing) and 2 (child externalizing)
Methods
Participants and Procedure
Participant characteristics are shown in Table 1. Participants were U.S. parents of 5–16-year-old children, recruited online through Qualtrics as part of a study on parenting and mental health during the COVID-19 pandemic. The study took place between February 2nd-April 4th, 2021. Non-probability quota sampling was used to collect a sample of parents that matched U.S. national demographics in terms of household income, race/ethnicity, and regional distribution. In addition, quota sampling was used to collect an equal number of fathers and mothers and equal distribution of parents of 5–8-year-olds, 9–12-year-olds, and 13–16-year-olds.
Table 1.
Participant characteristics and descriptive statistics
| Parents | Children | ||||
|---|---|---|---|---|---|
| No.(%) | No.(%) | ||||
| Female | 384 (48.2%) | 335 (42.1%) | |||
| Male | 412 (51.8%) | 461 (57.9%) | |||
| Age (M (SD)) | 38.87 (8.96) | 10.35 (3.16) | |||
| Race | |||||
| Non-Hispanic African-American or Black | 105 (13.2%) | 109 (13.7%) | |||
| Hispanic or Latinx | 144 (18.1%) | 137 (17.2%) | |||
| Asian | 45 (5.7%) | 36 (4.5%) | |||
| Other Race | 22 (2.8%) | 38 (4.8%) | |||
| Non-Hispanic White | 480 (60.3%) | 476 (59.8%) | |||
| Household Income | |||||
| $0–50000 | 294 (36.9%) | – | |||
| $50000–99999 | 283 (35.6%) | – | |||
| $100–150000 | 120 (15.1%) | – | |||
| $150000 or more | 99 (12.4%) | – | |||
| U.S. Region | |||||
| South | 318 (39.9%) | – | |||
| West | 173 (21.7%) | – | |||
| Midwest | 151 (19.0%) | – | |||
| Northeast | 154 (19.3%) | – | |||
| Marital Status | – | ||||
| Never married | 128 (16.1%) | – | |||
| Married | 586 (73.6%) | – | |||
| Separated | 11 (1.4%) | – | |||
| Divorced | 60 (7.5%) | – | |||
| Widowed | 11 (1.4%) | – | |||
| Employment Status | |||||
| Working virtually | 205 (25.8%) | ||||
| Working hybrid virtual/in-person | 170 (21.4%) | ||||
| Working in person | 238 (29.9%) | ||||
| Not employed | 183 (23.0%) | ||||
| Possible Range | Sample Min | Sample Max | M | SD | |
| Parent Depression/Anxiety Symptoms | 8–40 | 8.00 | 40.00 | 17.95 | 8.45 |
| COVID-19 Stressors | 0–25 | 0.00 | 25.00 | 9.49 | 4.80 |
| Positive Reinforcement | 3–15 | 3.00 | 15.00 | 13.01 | 2.15 |
| Inconsistent Discipline | 3–15 | 3.00 | 15.00 | 8.09 | 2.80 |
| Poor Supervision | 3–15 | 3.00 | 15.00 | 5.67 | 3.04 |
| Daily Routines | 0–55 | 4.00 | 44.00 | 32.75 | 7.36 |
| Parent Hostility | 1–5 | 1.00 | 5.00 | 2.23 | 0.82 |
| Parent Supportiveness | 1–5 | 1.00 | 5.00 | 4.33 | 0.75 |
| Parenting Self-Efficacy | 7–42 | 10.00 | 42.00 | 32.43 | 6.06 |
| Child Internalizing | 0–20 | 0.00 | 20.00 | 5.36 | 4.10 |
| Child Externalizing | 0–20 | 0.00 | 20.00 | 5.93 | 4.20 |
Parents were invited to participate through emails sent by Qualtrics. Inclusion criteria for the study included that parents were ≥ 18 years old, had at least one child between the ages of 5–16-years-old, and lived with the child ≥ 75% of the time. If inclusion criteria were met, parents read a consent cover letter and provided consent electronically before continuing. Parents answered survey questions about only one child. If parents had multiple children in the age range, the child of interest was randomly selected. Exclusion criteria included completing the survey in less than one-half the median time, not completing the entire survey, invalid responses, or failing three quality check questions (e.g., “Please choose ‘probably yes’ for this question”). Of 2767 invitations sent, 397 did not meet inclusion criteria and 67 did not consent. Of 2219 individuals who consented, 1411 were excluded based on exclusion criteria or not meeting open survey quotas, resulting in 796 in the final sample. See Supplemental Materials (SM) for more detail on survey validity checks and exclusions. Median completion time was 26.71 min. Study data are openly available at https://bit.ly/3eO72EY. This study was approved by the University of Mississippi Medical Center Institutional Review Board, study #2020V0322.
Measures
Children’s Internalizing and Externalizing Problems
Parents completed the Strengths and Difficulties Questionnaire (SDQ; Goodman, 1997), a 25-item mental health and behavioral screening measure for 3–16 year old children that includes subscales of emotional symptoms (“Many worries or often seems worried”), conduct problems (“Often loses temper”), hyperactivity/inattention (“Restless, overactive, cannot stay still for long”), peer relationship problems (“Would rather be alone than with other youth”), and prosocial behavior (“Kind to younger children”). Items are rated from 0—Not True to 2—Certainly True. Wording slightly differs across 4–10 and 11–17-year-old versions of the SDQ and parents were shown the appropriate items based on their child’s reported age. The emotional symptoms and peer relationship problems scales, and the conduct problems and hyperactivity/inattention problems scales, can be combined to create internalizing and externalizing problems scales, respectively; these scales were used in the present study. Higher scores indicate higher levels of internalizing (α = 0.81) and externalizing problems (α = 0.82).
Parent Depressive and Anxiety Symptoms
To assess parents’ current depressive and anxiety symptoms, parents completed the 4-item Short Forms of the Patient-Reported Outcomes Measurement Information System (PROMIS)-Depression and PROMIS-Anxiety (Pilkonis et al., 2011). Sample items include “In the past 7 days, I felt worthless” (Depression) and “In the past 7 days, my worries overwhelmed me” (Anxiety). The four items in each measure are rated from 1—Never to 5—Always and summed. In the present study, anxiety and depression scores were highly correlated (r = 0.87), so the scores from the two scales were summed for a total Parent Depression/Anxiety score (α = 0.95).
Parenting Behavior, Affect, and Cognitions
Parents completed scales from widely used parenting measures to assess modifiable parenting behaviors and cognitive/affective aspects of parenting. Parents completed the short form of the Alabama Parenting Questionnaire (APQ; Elgar et al., 2007), a nine-item measure of parenting behaviors that produces three-item subscales of positive reinforcement (e.g. “you let your child know when he/she is doing a good job with something”), inconsistent discipline (e.g. “you threaten to punish your child and then do not actually punish him/her”), and poor monitoring (e.g. “Your child is out with friends you don’t know”). Items are rated from 1—Never to 5—Always and summed for subscale scores (α = 0.79 for positive reinforcement, α = 0.71 for inconsistent discipline, α = 0.84 for poor supervision). Parents also completed the Daily Living Routines subscale of the Child Routines Inventory (CRI; Sytsma et al., 2001). This scale contains 11 items (e.g. “My child wakes up at about the same time on weekdays”) rated from 0—Almost Never to 5—Almost Always, and scores are summed for a subscale score (α = 0.88).
To assess affective aspects of parenting, parents completed the Hostility and Supportiveness subscales of the Multidimensional Assessment of Parenting Scale (MAPS; Parent & Forehand, 2017). The Hostility subscale includes seven items assessing intrusive, harsh, coercive, and irritable parenting behaviors (e.g. “I explode in anger toward my child”). The Supportiveness subscale includes three items assessing interest in the child and encouragement of the child’s emotions and thoughts (e.g. “I encourage my child to talk about her/his troubles”). MAPS items are rated from 1—Never to 5—Always and averaged to compute subscale scores (α = 0.88 for hostility, α = 0.79 for supportiveness).
To assess parenting cognitions, parents completed the 7-item Efficacy subscale of the Parenting Sense of Competence Scale (PSOC; Johnston & Mash, 1989). This subscale assesses parents’ self-efficacy in the parenting role (e.g. “I would make a fine model for a new parent to follow in order to learn what they would need to know in order to be a good parent”). Items were rated from 1—Strongly Disagree to 6—Strongly Agree and summed (α = 0.85).
COVID-19-Related Stressors
Parents completed Part 1 (Exposures) of the COVID-19 Exposure and Family Impact Survey (CEFIS; Kazak et al., 2021). Part 1 of the CEFIS includes 25 items assessing whether the family had experienced different stressful events related to the COVID-19 pandemic since March 2020. Items include events such as “We had a stay-at-home order,” “Our family income decreased,” and “Someone in the family died from COVID-19.” For each question, parents answered Yes or No, and “Yes” responses were summed for a total COVID-19 Exposures score. The CEFIS was created during the pandemic and recent evidence from 1805 caregivers recruited at 15 sites across the United States in 2020 supports the internal consistency of the Exposures scale (α = 0.80) and its validity in terms of significant positive correlations with Impact and Distress scales (Kazak et al., 2021).
Data Analytic Strategy
SPSS Version 27 was used for all analyses. Descriptive statistics were first calculated. Skewness and kurtosis values were within the range of -2 to 2 (skewness) and -3 to 3 (kurtosis), indicating variables could be analyzed using parametric statistics. Next, Pearson correlations were calculated to assess bivariate associations. For main analyses, two moderated mediation models were tested using the SPSS PROCESS macro (Hayes, 2013). In Model 1, parent depression/anxiety was the independent variable (X), child internalizing problems was the dependent variable (Y), parenting variables of interest (positive reinforcement, inconsistent discipline, poor supervision, routines, hostility, supportiveness, parenting self-efficacy) were the mediating variables (M1-M7), and COVID-19 stressors was the moderating variable (W). In Model 2, variables were the same except that the dependent variable (Y) was child externalizing problems. Covariates included parent age and gender, child age and gender, and household income due to significant bivariate associations between each of these variables and mediator and/or dependent variables (see Table 2).1 Indirect effects were tested using bootstrapping procedures (samples = 5000) with 95th percentile bootstrap confidence intervals. Of note, multiple mediator models in PROCESS test the specific effects of each mediator while holding all other mediators constant, and are therefore appropriate for correlated mediators (Hayes, 2013). PROCESS Model 8 was used to test moderated mediation. This model includes moderation of the a (X to M paths) and c (X to Y path) mediation paths by one moderator variable (W), and produces an index of moderated mediation (Hayes, 2015). The conceptual model is presented in Fig. 1. Model 8 was chosen because we hypothesized that COVID-19 stressors would have direct and interactive (with parent mental health) impacts on parenting factors and child mental health. In addition, Model 8 was chosen over a moderated mediation model in which the b paths (M to Y) are moderated (Models 14 or 59 in PROCESS); in preliminary analyses, Model 14 was tested separately and no significant moderation was observed in any M1-7 to Y path. Because at least one mediation path must be moderated to achieve moderated mediation (Hayes, 2015), we did not include any moderation of the M to Y paths in final models.
Table 2.
Bivariate correlations between study variables and demographic covariates
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Parent Depression/Anxiety | |||||||||||||||
| 2. COVID-19-Stressors | 0.46** | ||||||||||||||
| 3. Positive Reinforcement | -0.07 | -0.03 | |||||||||||||
| 4. Inconsistent Discipline | 0.34** | 0.37** | -0.11** | ||||||||||||
| 5. Poor Supervision | 0.33** | 0.38** | -0.33** | 0.55** | |||||||||||
| 6. Daily Routines | -0.15** | 0.03 | 0.48** | -0.20** | -0.22** | ||||||||||
| 7. Parent Hostility | 0.46** | 0.41** | -0.22** | 0.54** | 0.48** | -0.24** | |||||||||
| 8. Parent Supportiveness | -0.08* | -0.00 | 0.58** | -0.12** | -0.27** | 0.43** | -0.21** | ||||||||
| 9. Parent Self-Efficacy | -0.24** | 0.06 | 0.34** | -0.05 | -0.01 | 0.41** | -0.19** | 0.37** | |||||||
| 10. Child Internalizing | 0.55** | 0.43** | -0.29** | 0.44** | 0.49** | -0.30** | 0.54** | -0.28** | -0.22** | ||||||
| 11. Child Externalizing | 0.54** | 0.33** | -0.27** | 0.41** | 0.39** | -0.32** | 0.55** | -0.30** | -0.33** | 0.69** | |||||
| 12. Parent Age | -0.14** | -0.09* | -0.04 | -0.10** | 0.00 | 0.00 | -0.04 | -0.03 | -0.01 | -0.07* | -0.11** | ||||
| 13. Parent Gender | 0.10** | -0.09** | 0.16** | -0.17** | -0.29** | 0.02 | -0.07* | 0.05 | -0.11** | -0.07* | -0.03 | -0.04 | |||
| 14. Child Age | -0.06 | -0.03 | -0.12** | -0.03 | 0.10** | -0.13** | 0.02 | -0.07* | -0.01 | 0.06 | -0.07* | 0.35** | -0.04 | ||
| 15. Child Gender | 0.01 | -0.07 | 0.07 | -0.06 | -0.18** | -0.01 | -0.10** | 0.04 | -0.03 | -0.06 | -0.04 | 0.04 | 0.37** | -0.06 | |
| 16. Household Income | -0.13** | 0.05 | -0.16** | 0.14** | 0.25** | 0.00 | 0.11** | -0.10** | 0.11** | 0.08* | -0.04 | 0.03 | -0.30** | 0.06 | -0.12** |
For parent and child gender: 0 = Male, 1 = Female
*Correlation is significant at the 0.05 level (2-tailed)
**Correlation is significant at the 0.01 level (2-tailed)
Results
Descriptive and Bivariate Statistics
Descriptive and bivariate statistics are presented in Tables 1 and 2. See Table S1 in the SM for how sample means compared to previously reported scores for all measures. Both parent and child mental health symptoms were higher than norm scores reported prior to the pandemic. In terms of parenting measures, scores appeared slightly higher for negative parenting measures (hostility, poor supervision, inconsistent discipline) and lower for positive parenting measures (positive reinforcement, daily routines, but not supportiveness) compared to previously reported scores. However, overall we emphasize that all means in our sample were within one standard deviation of the mean or norm scores reported in prior studies, except for poor supervision which was higher than 1 SD above the mean reported by Elgar et al. (2007).
Significant positive correlations were observed between parent depression/anxiety symptoms and inconsistent discipline, poor supervision, parent hostility, and child internalizing and externalizing, and negative correlations were observed between parent depression/anxiety and daily routines, parent supportiveness, and parent self-efficacy. Number of COVID-19 stressors was significantly correlated with higher levels of parent depression/anxiety, inconsistent discipline, poor supervision, parent hostility, and child internalizing and externalizing. Higher levels of child internalizing and externalizing problems were associated with lower levels of positive reinforcement, daily routines, parent supportiveness, and parent self-efficacy, and higher levels of inconsistent discipline, poor supervision, and parent hostility.
Moderated Mediation Models
Results are presented in Tables 3 and 4 (internalizing) and Tables 3 and 5 (externalizing).
Table 3.
X➜M paths of child internalizing and externalizing moderated mediation models
| B (SE) | β (SE) | p | 95% CI Lower | 95% CI Upper | |
|---|---|---|---|---|---|
| 1. Positive Reinforcement (M1): F(8,787) = 7.26, p < 0.001, R2 = 0.07 | |||||
| Parent Depression/Anxiety (X) | -0.07 (0.02) | -0.28 (0.07) | 0.0003 | -0.11 | -0.03 |
| COVID-19-Stressors (W) | -0.07 (0.04) | -0.15 (0.09) | 0.102 | -0.14 | 0.01 |
| Interaction (X*W) | 0.00 (0.00) | 0.30 (0.12) | 0.020 | 0.00 | 0.01 |
| Parent Age | -0.00 (0.01) | -0.01 (0.04) | 0.815 | -0.02 | 0.02 |
| Parent Gender | 0.60 (0.17) | 0.14 (0.04) | 0.0003 | 0.27 | 0.93 |
| Child Age | -0.08 (0.03) | -0.11 (0.04) | 0.003 | -0.13 | -0.03 |
| Child Gender | 0.00 (0.16) | 0.00 (0.04) | 0.995 | -0.32 | 0.32 |
| Household Income | -0.27 (0.08) | -0.13 (0.04) | 0.001 | -0.42 | -0.12 |
| 2. Inconsistent Discipline (M2): F(8,787) = 27.31, p < 0.001, R2 = 0.22 | |||||
| Parent Depression/Anxiety (X) | 0.09 (0.02) | 0.27 (0.08) | 0.0001 | 0.04 | 0.13 |
| COVID-19-Stressors (W) | 0.14 (0.05) | 0.23 (0.09) | 0.005 | 0.04 | 0.23 |
| Interaction (X*W) | -0.00 (0.00) | -0.01 (0.13) | 0.918 | -0.00 | 0.00 |
| Parent Age | -0.02 (0.01) | -0.06 (0.04) | 0.093 | -0.04 | 0.00 |
| Parent Gender | -0.82 (0.20) | -0.15 (0.04) | < 0.001 | -1.22 | -0.43 |
| Child Age | 0.01 (0.03) | 0.01 (0.03) | 0.88 | -0.05 | 0.06 |
| Child Gender | 0.17 (0.19) | 0.03 (0.04) | 0.392 | -0.21 | 0.54 |
| Household Income | 0.34 (0.09) | 0.12 (0.03) | 0.0003 | 0.16 | 0.52 |
| 3. Poor Supervision (M3): F(8,787) = 47.13, p < 0.001, R2 = 0.32 | |||||
| Parent Depression/Anxiety (X) | 0.034 (0.02) | 0.09 (0.07) | 0.153 | -0.01 | 0.08 |
| COVID-19-Stressors (W) | -0.01 (0.05) | -0.01 (0.07) | 0.856 | -0.10 | 0.09 |
| Interaction (X*W) | 0.01 (0.00) | 0.38 (0.11) | 0.0005 | 0.00 | 0.01 |
| Parent Age | -0.00 (0.01) | -0.00 (0.03) | 0.987 | -0.02 | 0.02 |
| Parent Gender | -1.29 (0.20) | -0.21 (0.03) | < 0.001 | -1.69 | -0.89 |
| Child Age | 0.09 (0.03) | 0.10 (0.03) | 0.002 | 0.03 | 0.15 |
| Child Gender | -0.29 (0.20) | -0.05 (0.03) | 0.132 | -0.68 | 0.09 |
| Household Income | 0.60 (0.09) | 0.20 (0.03) | < 0.001 | 0.42 | 0.79 |
| 4. Daily Routines (M4): F(8,787) = 6.87, p < 0.001, R2 = 0.07 | |||||
| Parent Depression/Anxiety (X) | -0.34 (0.07) | -0.39 (0.08) | < 0.001 | -0.47 | -0.21 |
| COVID-19-Stressors (W) | -0.13 (0.14) | -0.08 (0.09) | 0.343 | -0.40 | 0.14 |
| Interaction (X*W) | 0.02 (0.01) | 0.35 (0.13) | 0.007 | 0.00 | 0.03 |
| Parent Age | 0.02 (0.03) | 0.03 (0.04) | 0.461 | -0.04 | 0.08 |
| Parent Gender | 0.91 (0.57) | 0.06 (0.04) | 0.113 | -0.22 | 2.04 |
| Child Age | -0.35 (0.09) | -0.15 (0.04) | 0.0001 | -0.52 | -0.18 |
| Child Gender | -0.34 (0.56) | -0.02 (0.04) | 0.539 | -1.43 | 0.75 |
| Household Income | -0.06 (0.27) | -0.01 (0.04) | 0.813 | -0.59 | 0.46 |
| 5. Parent Hostility (M5): F(8,787) = 41.34, p < 0.001, R2 = 0.30 | |||||
| Parent Depression/Anxiety (X) | 0.02 (0.01) | 0.19 (0.07) | 0.005 | 0.01 | 0.03 |
| COVID-19-Stressors (W) | -0.00 (0.01) | -0.02 (0.08) | 0.818 | -0.03 | 0.02 |
| Interaction (X*W) | 0.00 (0.00) | 0.38 (0.13) | 0.001 | 0.00 | 0.00 |
| Parent Age | 0.00 (0.00) | 0.00 (0.03) | 0.928 | -0.01 | 0.01 |
| Parent Gender | -0.04 (0.06) | -0.02 (0.03) | 0.501 | -0.15 | 0.07 |
| Child Age | 0.01 (0.01) | 0.03 (0.03) | 0.286 | -0.01 | 0.03 |
| Child Gender | -0.09 (0.05) | -0.05 (0.03) | 0.115 | -0.19 | 0.02 |
| Household Income | 0.10 (0.03) | 0.13 (0.03) | 0.0001 | 0.05 | 0.15 |
| 6. Parent Supportiveness (M6): F(8,787) = 2.88, p = 0.004, R2 = 0.03 | |||||
| Parent Depression/Anxiety (X) | -0.02 (0.01) | -0.20 (0.08) | 0.012 | -0.03 | -0.00 |
| COVID-19-Stressors (W) | -0.00 (0.01) | -0.02 (0.10) | 0.824 | -0.03 | 0.03 |
| Interaction (X*W) | 0.00 (0.00) | 0.13 (0.13) | 0.309 | -0.00 | 0.00 |
| Parent Age | -0.00 (0.00) | -0.02 (0.04) | 0.677 | -0.01 | 0.01 |
| Parent Gender | 0.05 (0.06) | 0.03 (0.04) | 0.389 | -0.07 | 0.17 |
| Child Age | -0.02 (0.01) | -0.07 (0.04) | 0.085 | -0.03 | 0.00 |
| Child Gender | 0.02 (0.06) | 0.02 (0.04) | 0.694 | -0.09 | 0.14 |
| Household Income | -0.08 (0.03) | -0.10 (0.04) | 0.007 | -0.13 | -0.02 |
| 7. Parent Self-Efficacy (M7): F(8,787) = 14.01, p < 0.001, R2 = 0.13 | |||||
| Parent Depression/Anxiety (X) | -0.45 (0.05) | -0.63 (0.08) | < 0.001 | -0.55 | -0.34 |
| COVID-19-Stressors (W) | -0.22 (0.11) | -0.18 (0.09) | 0.040 | -0.44 | -0.01 |
| Interaction (X*W) | 0.02 (0.01) | 0.60 (0.14) | < 0.001 | 0.01 | 0.03 |
| Parent Age | -0.04 (0.03) | -0.06 (0.03) | 0.119 | -0.09 | 0.01 |
| Parent Gender | -0.49 (0.46) | -0.04 (0.04) | 0.287 | -1.38 | 0.41 |
| Child Age | -0.02 (0.07) | -0.01 (0.04) | 0.821 | -0.15 | 0.12 |
| Child Gender | 0.21 (0.44) | 0.02 (0.04) | 0.633 | -0.66 | 1.08 |
| Household Income | 0.33 (0.21) | 0.06 (0.03) | 0.123 | -0.09 | 0.74 |
X to M paths were the same in child internalizing and externalizing moderated mediation models. Bolded variables are significant
Parent and Child Gender: 0 = male, 1 = female
Table 4.
X➜Y and M➜Y paths and indices of moderated mediation, child internalizing moderated mediation model
| Child Internalizing | B (SE) | β (SE) | p | 95% CI Lower | 95% CI Upper |
|---|---|---|---|---|---|
| Parent Depression/Anxiety (X) | 0.14 (0.03) | 0.30 (0.07) | < 0.001 | 0.08 | 0.19 |
| Positive Reinforcement (M1) | -0.11 (0.07) | -0.06 (0.04) | 0.101 | -0.23 | 0.02 |
| Inconsistent Discipline (M2) | 0.10 (0.05) | 0.07 (0.04) | 0.036 | 0.01 | 0.20 |
| Poor Supervision (M3) | 0.19 (0.05) | 0.14 (0.04) | 0.0001 | 0.09 | 0.28 |
| Daily Routines (M4) | -0.05 (0.02) | -0.10 (0.03) | 0.003 | -0.09 | -0.02 |
| Parent Hostility (M5) | 0.82 (0.17) | 0.17 (0.04) | < 0.001 | 0.48 | 1.16 |
| Parent Supportiveness (M6) | -0.45 (0.18) | -0.09 (0.04) | 0.011 | -0.79 | -0.10 |
| Parent Self-Efficacy (M7) | -0.02 (0.02) | -0.03 (0.04) | 0.293 | -0.06 | 0.02 |
| COVID-19-Stressors (W) | 0.09 (0.06) | 0.11 (0.07) | 0.112 | -0.02 | 0.20 |
| Interaction (X*W) | 0.00 (0.00) | 0.06 (0.11) | 0.546 | -0.00 | 0.01 |
| Parent Age | -0.01 (0.01) | -0.03 (0.03) | 0.253 | -0.04 | 0.01 |
| Parent Gender | 0.00 (0.24) | 0.00 (0.03) | 0.996 | -0.47 | 0.48 |
| Child Age | 0.07 (0.04) | 0.06 (0.03) | 0.047 | 0.00 | 0.14 |
| Child Gender | 0.04 (0.23) | 0.01 (0.03) | 0.851 | -0.40 | 0.49 |
| Household Income | 0.16 (0.11) | 0.04 (0.03) | 0.148 | -0.06 | 0.38 |
| Index of Moderated Mediation | |||||
| X➜M1➜Y | -0.00 (0.00) | -0.00 | 0.00 | ||
| X➜M2➜Y | 0.00 (0.00) | -0.00 | 0.00 | ||
| X➜M3➜Y | 0.00 (0.00) | 0.00 | 0.00 | ||
| X➜M4➜Y | -0.00 (0.00) | -0.00 | -0.00 | ||
| X➜M5➜Y | 0.00 (0.00) | 0.00 | 0.00 | ||
| X➜M6➜Y | -0.00 (0.00) | -0.00 | 0.00 | ||
| X➜M7➜Y | -0.00 (0.00) | -0.00 | 0.00 | ||
F (15,780) = 53.10, p < 0.001, R2 = 0.51. Bolded variables or indices are significant
Parent and child gender: 0 = male, 1 = female
Table 5.
X➜Y and M➜Y paths and indices of moderated mediation, child externalizing moderated mediation model
| Child Externalizing | B (SE) | β (SE) | p | 95% CI Lower | 95% CI Upper |
|---|---|---|---|---|---|
| Parent Depression/Anxiety (X) | 0.16 (0.03) | 0.35 (0.06) | < 0.001 | 0.11 | 0.22 |
| Positive Reinforcement (M1) | -0.07 (0.07) | -0.04 (0.04) | 0.304 | -0.20 | 0.06 |
| Inconsistent Discipline (M2) | 0.12 (0.05) | 0.08 (0.04) | 0.020 | 0.02 | 0.22 |
| Poor Supervision (M3) | 0.09 (0.05) | 0.07 (0.04) | 0.081 | -0.01 | 0.19 |
| Daily Routines (M4) | -0.05 (0.02) | -0.09 (0.04) | 0.009 | -0.08 | -0.01 |
| Parent Hostility (M5) | 1.38 (0.18) | 0.28 (0.04) | < 0.001 | 1.03 | 1.73 |
| Parent Supportiveness (M6) | -0.56 (0.18) | -0.11 (0.04) | 0.002 | -0.92 | -0.20 |
| Parent Self-Efficacy (M7) | -0.08 (0.02) | -0.12 (0.04) | 0.0003 | -0.12 | -0.04 |
| COVID-19-Stressors (W) | 0.07 (0.06) | 0.09 (0.06) | 0.206 | -0.04 | 0.19 |
| Interaction (X*W) | -0.00 (0.00) | -0.09 (0.09) | 0.415 | -0.01 | 0.00 |
| Parent Age | -0.01 (0.01) | -0.02 (0.03) | 0.455 | -0.04 | 0.02 |
| Parent Gender | -0.21 (0.25) | -0.03 (0.03) | 0.396 | -0.71 | 0.28 |
| Child Age | -0.10 (0.04) | -0.08 (0.03) | 0.009 | -0.17 | -0.03 |
| Child Gender | 0.04 (0.24) | 0.00 (0.03) | 0.878 | -0.43 | 0.50 |
| Household Income | -0.27 (0.12) | -0.07 (0.03) | 0.022 | -0.50 | -0.04 |
| Index of Moderated Mediation | |||||
| X➜M1➜Y | -0.00 (0.00) | -0.00 | 0.00 | ||
| X➜M2➜Y | 0.00 (0.00) | -0.00 | 0.00 | ||
| X➜M3➜Y | 0.00 (0.00) | -0.000 | 0.00 | ||
| X➜M4➜Y | -0.00 (0.00) | -0.00 | -0.00 | ||
| X➜M5➜Y | 0.00 (0.00) | 0.00 | 0.00 | ||
| X➜M6➜Y | -0.00 (0.00) | -0.00 | 0.00 | ||
| X➜M7➜Y | -0.00 (0.00) | -0.00 | -0.00 | ||
F (15,780) = 49.93, p < 0.001, R2 = 0.49. Bolded variables or indices are significant
Parent and child gender: 0 = male, 1 = female
Direct Effects
Findings for paths predicting parenting (mediator) variables, which were the same in both models and are shown in Table 3, panels 1–7, demonstrated a significant interaction between parent depression/anxiety and COVID-19 stressors in predicting positive reinforcement, poor supervision, daily routines, parent hostility, and parent self-efficacy. Interaction plots can be seen in Figure S1 in the SM. Conditional effects analysis using 16th, 50th, and 84th percentile values of the moderator indicated that greater parent depression/anxiety was more strongly associated with lower levels of positive reinforcement, daily routines, and parent self-efficacy at lower levels of COVID-19 stressors, and more strongly associated with greater levels of hostility and poor supervision at higher levels of COVID-19 stressors. This suggests that COVID-19 stressors may have exacerbated the effects of parent depression/anxiety on negative parenting variables, but not for positive parenting features.
For inconsistent discipline, both parent depression/anxiety and COVID-19 stressors were significant, but not their interaction, such that higher levels of parent depression/anxiety and COVID-19 stressors were independently related to higher levels of inconsistent discipline. For parent supportiveness, only parent depression/anxiety was significant, such that higher levels of parent depression/anxiety were associated with lower levels of supportiveness.
Paths predicting child internalizing (Table 4) were positive and significant for parent depression/anxiety, inconsistent discipline, poor supervision, and parent hostility, and negative and significant for daily routines and parent supportiveness. Paths predicting child externalizing (Table 5) were positive and significant for parent depression/anxiety, inconsistent discipline, and parent hostility, and negative and significant for daily routines, parent supportiveness, and parent self-efficacy. Notably, COVID-19 stressors, and the interaction between COVID-19 stressors and parent depression/anxiety, were not significantly associated with child internalizing (Table 4) or externalizing problems (Table 5) over and above other predictors and covariates. Direct effects of parent depression/anxiety on child internalizing and externalizing remained significant when mediators were included, and these effects were not moderated by COVID-19 stressors.
Indirect Effects and Conditional Indirect Effects
In the child internalizing moderated mediation model, there was an unmoderated indirect effect for parent supportiveness such that the relationship between parent depression/anxiety and child internalizing was partially mediated through lower levels of parent supportiveness (B = 0.01, SE = 0.01, 95% CI [0.00, 0.02]), regardless of families’ level of exposures to COVID-19-related stressors. In this model, indices of moderated mediation (see Table 4, lower panel) were significant for poor supervision, daily routines, and parent hostility, suggesting that the indirect effects of parent depression/anxiety on child internalizing through these three mediators were conditional on level of COVID-19 stressors. Specifically, the indirect effects through poor supervision and hostility were stronger, and the indirect effect through daily routines weaker, when higher levels of COVID-19 stressors were reported.
In the child externalizing moderated mediation model, there were unmoderated indirect effects of inconsistent discipline (B = 0.01, SE = 0.01, 95% CI [0.00, 0.02]) and parent supportiveness (B = 0.01, SE = 0.01, 95% CI [0.00, 0.02]), such that the relationship between parent depression/anxiety and child externalizing problems was partially mediated through higher levels of inconsistent discipline and lower levels of parent supportiveness, regardless of families’ level of COVID-19 stressors. There was also significant moderated mediation (Table 5, lower panel) for daily routines, parent hostility, and parent self-efficacy. In particular, there was a stronger indirect effect of parent depression/anxiety on child externalizing through hostility when greater COVID-19 stressors were reported, and weaker indirect effects through daily routines and parent self-efficacy when greater COVID-19 stressors were reported.
Supplemental Multi-Group Analyses
Detailed results and discussion for the supplemental multi-group analyses can be found in the SM. We first tested whether model paths would differ across the three child age groups (5–8, 9–12, and 13–16 years), finding that model fit improved when paths were allowed to vary across the three groups. We then conducted separate analyses by group. We suggest caution in interpreting results given the smaller sub-group sample sizes and the number of paths in our models, which reduced power relative to whole-group analyses. A finding that remained consistent across groups was that parent depression/anxiety was directly associated with child internalizing and externalizing and this was not moderated by COVID-19 stressors, nor did COVID-19 stressors have direct effects. Another consistent effect was that across age groups, parent hostility, routines, and self-efficacy were significantly predicted by parent depression/anxiety or its interaction with COVID-19 stressors. However, for the older age groups (9–12 and 13–16 years), there were additional direct or interactive of parent depression/anxiety on other features of parenting (positive reinforcement and supportiveness for 9–12-year-olds; positive reinforcement and inconsistent discipline for 13–16-year-olds), suggesting that for parents of older children, depression/anxiety symptoms had a broader impact on parenting. Parent hostility remained significant across ages and internalizing and externalizing, with the exception of 13–16-year-old internalizing. Routines were significant for 9–12-year-old externalizing, supportiveness for 5–8-year-old internalizing and 13–16-year-old externalizing, and consistent discipline for 5–8-year-old externalizing. Parent self-efficacy was again significant for externalizing problems (5–8-year-olds and 9–12-year-olds) and poor supervision for internalizing problems (5–8-year-olds and 13–16-year-olds); poor supervision was also significant for externalizing problems in the adolescent group. Moderated mediation was observed for poor supervision (internalizing, 5–8-year-olds), parent self-efficacy (externalizing, 5–8 and 9–12-year-olds), and hostility (internalizing and externalizing, 9–12-year-olds).
Discussion
This study sought to better understand individual differences in child mental health during the COVID-19 pandemic and pinpoint parent-level risk and resilience factors underlying differences to target in clinical interventions with families. Based partly on the conceptual model set forward by Prime and colleagues (2020), this study tested two moderated mediation models in which parent depression and anxiety indirectly impacted child internalizing (Model 1) and externalizing (Model 2) problems during the pandemic through negative effects on multiple aspects of parenting, with these relationships moderated by families’ exposure to COVID-19-stressors. These relationships were tested in a large national U.S. sample of parents of 5–16-year-old children with income, race/ethnicity, and regional distribution matching the U.S. population.
Parent Mental Health Effects on Parenting During the COVID-19 Pandemic
In moderated mediation models, controlling for parent and child gender and age and household income, greater levels of parental depression/anxiety were directly associated with greater inconsistent discipline and less parent supportiveness. Parent depression/anxiety also interacted with COVID-19 stressors; this interaction was characterized by stronger, positive associations between parents’ depression/anxiety symptoms and both parent hostility and poor supervision when greater levels of COVID-19 stressors were reported. On the other hand, depression/anxiety symptoms were more strongly, negatively associated with positive reinforcement, daily routines, and parenting self-efficacy when fewer COVID-19 stressors were reported. This pattern of findings seems to suggest that the combination of high COVID-19 stressors and greater depression/anxiety for parents may have influenced greater frequency of negative parenting (poor supervision, hostility), whereas for parents who reported high COVID-19 stressors, depression/anxiety symptoms had less of an influence on positive aspects of parenting (routines, self-efficacy, positive reinforcement). This may have occurred because greater level of COVID-19 stressors resulted in families spending more time together or needing to provide more support for each other, such that positive parenting behaviors were maintained regardless of parents’ level of depression/anxiety, or that at high levels of COVID-19 stressors, the disruption/stress due to these COVID-19 events was all that influenced these particular parenting variables. Notably, one exception to this pattern was parent supportiveness, which was not associated with COVID-19 stressors but was negatively associated with parent depression/anxiety. This may suggest that parents did not alter their support of children’s thoughts and feelings based on COVID-19 disruptions and stressors. Inconsistent discipline was independently predicted by both parent depression/anxiety and COVID-19 stressors such that higher levels of either were associated with more inconsistent discipline. This makes sense given that disruptions due to pandemic stressors likely impacted parents’ discipline practices and consistency, and concerns over COVID-19 impacts on children may have also made parents feel guilty about following through with punishments. At the same time, parents who were experiencing more depression/anxiety may also have had difficulty following through with discipline or may have threatened punishments that they did not mean.
These findings add further evidence in support of recent research that has indicated negative impacts of parent mental health on parenting during the pandemic (Fosco et al., 2021; Roos et al., 2021; Russell et al., 2020), but adds to this prior research by showing that detrimental effects of parent mental health on parenting can vary as a function of families’ differing exposures to COVID-19 stressors. In particular, these findings confirm that negative features of parenting (e.g., hostility) are particularly sensitive to the combination of COVID-19 stressors and parent depression/anxiety, and should be monitored, especially for families who have experienced more pandemic stressors. Conversely, interventions aimed at improving positive parenting features (e.g., positive reinforcement) should attend to parent depression/anxiety and also consider how COVID-19 stressors may have already brought the family together or increased family support in ways that could be capitalized on. Implications of this bifurcation of COVID-19 stressors’ impact on parenting are important, given evidence for some differential associations between negative and positive parenting and important child outcomes (e.g. Dallaire et al., 2006).
Parenting Effects on Child Mental Health during the COVID-19 Pandemic
Direct links between parenting variables and child mental health were observed in moderated mediation models, regardless of level of COVID-19 stressors, parent mental health symptoms, and covariates. Specifically, more inconsistent discipline, poorer supervision, greater hostility, fewer routines, and less parent supportiveness were associated with worse child internalizing problems. More inconsistent discipline, greater hostility, fewer routines, less parental supportiveness, and lower levels of parenting self-efficacy were associated with worse child externalizing problems. It is interesting to note that with the exception of poor supervision for child internalizing, and parent self-efficacy for child externalizing, there was overlap of the parenting variables predicting internalizing and externalizing (though this was less consistent when models were examined by child age group, see SM). This may have occurred because these factors (consistent discipline, low hostility, routines, supportiveness) generally support well-being for children and may therefore represent transdiagnostic parenting factors. Critically, Prime and colleagues (2020) noted harsh and coercive parenting (i.e., hostility) and routines as especial areas of concern for child mental health during the pandemic, and others have also highlighted the importance of family routines, the regulatory role of parents (i.e., consistent discipline), and emotional support—as a feature of the attachment system—during times of stress (Masten & Cicchetti, 2016). Therefore, the crosscutting importance of these parenting factors are consistent with prior family resilience theories. Shared findings across internalizing and externalizing may also have occurred because of the high correlation between these symptom domains in our sample (r = 0.69), which we discuss further in the limitations section.
In contrast, poor supervision was uniquely associated with child internalizing and parent self-efficacy uniquely with child externalizing. We note that the effects of supervision/monitoring on child internalizing appear to be driven by the youngest (ages 5–8) and oldest (ages 13–16) age groups (see SM). For younger children, low supervision may represent less time spent together with their parent, perhaps leading to increased withdrawn behavior or feelings of sadness or anxiety for the child. For adolescents, low supervision may result in adolescents spending more time alone at home, withdrawing from others, or increasing phone or social media use, which may result in greater internalizing symptoms. This also may be in part bidirectional, wherein adolescents’ withdrawal/internalizing symptoms occurred first and led to lower supervision/monitoring. The unique effects of parent self-efficacy on child externalizing appear to be driven by the 5–8 year old and 9–12 year old groups (see SM). This is consistent with previous parenting literature: low parenting self-efficacy, as a feature of parents’ sense of competence, has often been associated with more behavior problems in children, although it is thought that this operates in a bidirectional fashion (Colalillo & Johnston, 2016). This may have been driven by the younger age groups because parents of older children have more experience and therefore experience greater self-efficacy in the parenting role.
It is also notable that, in preliminary analyses testing moderation of the M1-7 to Y paths, there was no significant moderation of any path by number of COVID-19 stressors experienced, suggesting that the well-documented pathways between parenting and child internalizing and externalizing behaviors were maintained regardless of level of exposures to COVID-19 stressors. This information is critical in terms of underlining the utility of existing evidence-based parenting interventions during the pandemic that emphasize changes in these parenting factors. This provides reassuring evidence insofar as clinical practice may lean on the existing evidence-based intervention armamentarium rather than redirect crucial resources to the development and implementation of new COVID-19 informed interventions and protocols.
Parent Mental Health Effects on Child Mental Health during the COVID-19 Pandemic
That parenting mediators did not fully explain the association between parent depression/anxiety and internalizing and externalizing problems in children (i.e., direct links remained) is an important finding as it suggests that parent and child mental health are linked through additional mechanisms other than parenting behavior. Considering this finding in the context of Prime and colleagues’ (2020) model, the present study considered only the parent–child “subsystem.” It could be that additional consideration of indirect paths through other family subsystems (marital, sibling, whole family) would more fully explain the link between parent and child mental health. Nevertheless, this finding also strongly suggests that interventions would benefit from addressing the individual parent’s mental health alongside their parenting.
It is also important to note the particular pathways through which parent depression/anxiety exerted influence on child internalizing and externalizing problems. Parent depression/anxiety was associated with worse child internalizing problems by means of lower parent supportiveness, poorer supervision, fewer daily routines, and increased parent hostility. However, indirect paths through supervision, daily routines, and hostility were moderated such that for families with higher exposure to COVID-19 stressors, there were stronger effects through hostility and poor supervision and weaker effects through daily routines. Lower parent supportiveness, more inconsistent discipline, fewer routines, increased parent hostility, and lower parenting self-efficacy mediated the association between parent depression/anxiety and child externalizing; however, again families with greater exposure to COVID-19 stressors had weaker indirect effects through routines and self-efficacy and stronger indirect effects through hostility. These models identify parent hostility, parent supportiveness, and daily routines as important avenues for intervention across child mental health domains. Additionally, they pinpoint supervision/monitoring as a specific target for child internalizing problems, and inconsistent discipline and parenting self-efficacy as specific targets for child externalizing problems.
Critically, reducing parent hostility appears particularly important for child internalizing and externalizing difficulties in families with greater exposure to COVID-19 stressors. This finding aligns with Prime and colleagues’ (2020) hypothesis that increases in coercive and harsh parenting were likely to be observed when parents’ well-being is detrimentally impacted by the pandemic. In addition, for families with greater exposure to COVID-19 stressors, supervision/monitoring appears to be important to understand and address for child internalizing difficulties. This observation may reflect families who had to continue working in person while children were at home, or families in which children were withdrawing from parental monitoring more often due to increased time at home, contributing to depression symptoms.
Effects of COVID-19 Stressors
The level of COVID-19 stressors that families experienced did not directly contribute to child mental health problems; rather, parent depression/anxiety showed significant effects. This emphasizes the importance of parents as a buffer for child mental health in times of adversity, consistent with decades of research (Masten & Narayan, 2012). However, it also highlights that COVID-19 stress is likely impacting children indirectly through parents, and therefore that parents’ stress and mental health is important to continue to investigate and address (Peris & Ehrenreich-May, 2021). It is notable that COVID-19 stressors also interacted with parent mental health in predicting a variety of parenting variables, or were directly associated with parenting behaviors, indicating that family risk and resilience pathways do differ based on COVID-19 events experienced. We observed either direct or interactive effects of COVID-19 stressors on every parenting variable except parent supportiveness, revealing pandemic-related effects across behavioral, affective, and cognitive features of parenting. Future research should evaluate to what extent this is due to the effects of specific stressors (e.g., death or severe illness in the family, reduction in income, parent essential worker) or cumulative stressors as measured here, particularly given that certain events—such as a death in the family—are likely to affect families more heavily or in different ways than other pandemic events, such as a stay-at-home order.
Clinical Implications
Findings help speak to the “how” of child mental health during the pandemic by suggesting particular cognitive (self-efficacy), affective (hostility, parent supportiveness), and behavioral (routines, consistent discipline, monitoring) aspects of parenting, along with parent depression and anxiety, as important areas for intervention to support children’s emotional and behavioral health. Findings also speak to “for whom” by suggesting that, for families who have experienced more COVID-19-related stressors, there may be more particular need to address parent hostility and supervision/monitoring, and by demonstrating specificity in terms of particular parenting mediators of child internalizing (supervision/monitoring) vs. child externalizing (parenting self-efficacy, inconsistent discipline) problems. Behavioral parenting interventions such as Parent Management Training or PMT (e.g. Barkley, 2013; McMahon & Forehand, 2003) and Parent–Child Interaction Therapy (Eyberg, 1988) that are widely disseminated have documented evidence for addressing parenting behaviors such as consistent discipline, routines, supervision, and supportiveness; notably, PMTs have also demonstrated positive effects for parenting cognitions (Colalillo & Johnston, 2016). Parents may also benefit from treatments to address their own symptoms and improve emotion regulation (in order to reduce hostility), such as Dialectical Behavioral Therapy (Linehan, 1993). Mentalization-based parent interventions may also be important for increasing parents’ supportiveness, identification and management of emotions, and understanding of children’s emotions and behavior (Arnsten et al., 2021). The findings reported here support a recent comprehensive review of evidence-based interventions, including family- and parent-based interventions, recommended for addressing child mental health problems from the pandemic (Arnsten et al., 2021). Yet, in leveraging or adapting existing evidence-based interventions to address pandemic mental health, the current findings clearly demonstrate it is important for clinicians to assess families’ level of exposure to COVID-19 stressors given its impact on family pathways to child mental health.
Limitations, Alternative Models, and Directions for Future Research
Data were collected at one time point and therefore mediational findings cannot speak to effects over time, only to explanation of variance at the time when data was collected. In addition, though our study focuses only on the paths from parent to child mental health in keeping with Prime and colleagues’ model, there are likely bidirectional effects between parent and child mental health (and between child mental health and parenting variables). It is possible that current findings were partially a result of child to parent effects, and future research on this topic would benefit from using longitudinal data to evaluate competing models and reciprocal parent–child influences. Another alternative is that effects could be driven by shared biological factors between parents and children (genes, temperament, etc.): for example, shared genetic risks could increase vulnerability to psychopathology for both parent and child during COVID-19, representing possible gene by environment interactions. In addition, other shared traits such as emotion regulation behaviors, which children often learn through parents’ modeling (Hajal & Paley, 2020), may result in increased parent–child psychopathology during times of stress. Collectively, it is important to consider both alternative causal directions of influence and potential shared underlying mechanisms that may influence parent and child mental health.
Another limitation is that data presented here are only a snapshot of one period during the pandemic (February-April 2021). One benefit of the study’s time period, however, is that the COVID-19 stressors measure included a year of pandemic-related events, increasing variability and supporting the variable as a predictor. Data were collected only by parent report, meaning that shared method variance likely effects the magnitude of associations. A related limitation is that the child internalizing and externalizing variables were strongly associated in our sample (r = 0.69), which may have led to a similar pattern of findings across the two models. Correlations of r = 0.45-0.54 have been reported between internalizing and externalizing problems in a large review of studies (Achenbach et al., 2016). It is possible that parents were reporting problems more consistently across domains due to observing children’s behavior more during increased time at home, or perceiving that in general their child’s behavior was more problematic during the pandemic, leading to a large correlation in our sample. Future studies would benefit from multi-method and multi-rater assessment to reduce shared method variance.
A crucial need for future research is also to understand social and cultural influences within Prime’s model by testing differences based on family racial/ethnic background. This is particularly important given past research showing racial/ethnic differences in parenting styles (Smetana, 2017) and their association with child mental health (e.g. Greening et al., 2010). Such research could help advise culturally informed adaptations of evidence-based mental health interventions.
Conclusion
Findings of this study align strongly with decades of research showing that parents buffer children’s risk for mental health problems during times of adversity. Further, results provide validation of a key portion of the conceptual model of family risk during the pandemic that was set forth by Prime and colleagues (2020). There is a clear need to address parent depression and anxiety symptoms in the context of parent interventions during and following the pandemic. Negative parenting including parent hostility, particularly for families who have experienced more COVID-19 stressors, is also particularly important to monitor and address. Parental supervision/monitoring and parenting self-efficacy may be important intervention targets specific to child internalizing and externalizing problems, respectively. Daily routines, consistent discipline, and supportiveness of children’s thoughts and emotions also emerged as important mediators and intervention targets across mental health domains.
Supplementary Information
Below is the link to the electronic supplementary material.
Funding
This work was funded by a grant from the Pediatrics Discovery Council, Department of Pediatrics, University of Mississippi Medical Center (no grant number, awarded to Penner and Elzaki) and research incentive funds from University of Mississippi Medical Center (awarded to Sarver). Dr. Penner received funding support from T32 MH018268 during manuscript preparation.
Compliance with Ethical Standards
Conflict of Interest
Drs. Contreras, Elzaki, and Penner report no conflicts of interest.
Disclosures
Dr. Sarver received grants from SAMHSA, HRSA, Simons Foundation, and industry-sponsored sources during the conduct of the study. Dr. Santos received grant funding from HRSA during the study period. Dr. Santos received honoraria from the American Board of Pediatrics and the American Academy of HIV Medicine during 2020–21.
Ethical Approval
This study was approved by the University of Mississippi Medical Center Institutional Review Board, study #2020V0322.
Consent to Participate
Informed consent was obtained from all participants in this study.
Footnotes
Analyses conducted without covariates showed minimal changes. Specifically, the interaction between COVID-19 stressors and parent depression/anxiety was only marginally significant (p = 0.07) in predicting positive reinforcement. For internalizing problems, there was significant (unmoderated) mediation through inconsistent discipline. For externalizing problems, mediation was significant for daily routines at all levels of COVID-19 stressors; the moderated mediation index was not significant.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Achenbach TM, Ivanova MY, Rescorla LA, Turner LV, Althoff RR. Internalizing/Externalizing Problems: Review and Recommendations for Clinical and Research Applications. Journal of the American Academy of Child & Adolescent Psychiatry. 2016;55:647–656. doi: 10.1016/j.jaac.2016.05.012. [DOI] [PubMed] [Google Scholar]
- Alzueta E, Perrin P, Baker FC, Caffarra S, Ramos-Usuga D, Yuksel D, Arango-Lasprilla JC. How the COVID-19 pandemic has changed our lives: A study of psychological correlates across 59 countries. Journal of Clinical Psychology. 2021;77(3):556–570. doi: 10.1002/jclp.23082. [DOI] [PubMed] [Google Scholar]
- Arnsten, A. F. T., Condon, E. M., Dettmer, A. M., Gee, D. G., Lee, K. S., Mayes, L. C., Stover, C. S., & Tseng, W. L. (2021). The prefrontal cortex in a pandemic: Restoring functions with system-, family-, and individual-focused interventions. American Psychologist. 10.1037/amp0000823 [DOI] [PMC free article] [PubMed]
- Barkley RA. Defiant Children: A Clinician’s Manual for Assessment and Parent Training. Guilford Press; 2013. [Google Scholar]
- Bate J, Pham PT, Borelli JL. Be My Safe Haven: Parent-Child Relationships and Emotional Health During COVID-19. Journal of Pediatric Psychology. 2021;46(6):624–634. doi: 10.1093/jpepsy/jsab046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Breaux, R., Dvorsky, M. R., Marsh, N. P., Green, C. D., Cash, A. R., & Becker, S. P. (2021). Prospective impact of COVID‐19 on mental health functioning in adolescents with and without ADHD: Protective role of emotion regulation abilities. Journal of Child Psychology and Psychiatry. 10.1111/jcpp.13382 [DOI] [PMC free article] [PubMed]
- Cameron EE, Joyce KM, Delaquis CP, Reynolds K, Protudjer JLP, Roos LE. Maternal psychological distress & mental health service use during the COVID-19 pandemic. Journal of Affective Disorders. 2020;276:765–774. doi: 10.1016/j.jad.2020.07.081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohodes, E. M., McCauley, S., & Gee, D. G. (2021). Parental Buffering of Stress in the Time of COVID-19: Family-Level Factors May Moderate the Association Between Pandemic-Related Stress and Youth Symptomatology. Research on Child and Adolescent Psychopathology, 49(7), 935–948. 10.1007/s10802-020-00732-6 [DOI] [PMC free article] [PubMed]
- Colalillo, S., & Johnston, C. (2016). Parenting Cognition and Affective Outcomes Following Parent Management Training: A Systematic Review. Clinical Child & Family Psychology Review, 216–235. 10.1007/s10567-016-0208-z [DOI] [PubMed]
- Dallaire DH, Pineda AQ, Cole DA, Ciesla JA, Jacquez F, LaGrange B, Bruce AE. Relation of Positive and Negative Parenting to Children’s Depressive Symptoms. Journal of Clinical Child & Adolescent Psychology. 2006;35(2):313–322. doi: 10.1207/s15374424jccp3502_15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elgar, F. J., Waschbusch, D. A., Dadds, M. R., & Sigvaldason, N. (2007). Development and Validation of a Short Form of Alabama Parenting Questionnaire. Journal of Child & Family Studies, 243–259. 10.1007/s10826-006-9082-5
- Eyberg S. Parent-Child Interaction Therapy. Child & Family Behavior Therapy. 1988;10(1):33–46. doi: 10.1300/J019v10n01_04. [DOI] [Google Scholar]
- Feinberg, M. E., A. Mogle, J., Lee, J.-K., Tornello, S. L., Hostetler, M. L., Cifelli, J. A., Bai, S., & Hotez, E. (2021). Impact of the COVID-19 Pandemic on Parent, Child, and Family Functioning. Family Process, 61(1), 361–374. 10.1111/famp.12649 [DOI] [PMC free article] [PubMed]
- Fosco, G. M., Sloan, C. J., Fang, S., & Feinberg, M. E. (2021). Family vulnerability and disruption during the COVID‐19 pandemic: Prospective pathways to child maladjustment. Journal of Child Psychology & Psychiatry. 10.1111/jcpp.13458 [DOI] [PMC free article] [PubMed]
- Gadermann, A. C., Thomson, K. C., Richardson, C. G., Gagné, M., McAuliffe, C., Hirani, S., & Jenkins, E. (2021). Examining the impacts of the COVID-19 pandemic on family mental health in Canada: Findings from a national cross-sectional study. BMJ Open, 11(1), e042871. 10.1136/bmjopen-2020-042871 [DOI] [PMC free article] [PubMed]
- Glynn, L. M., Davis, E. P., Luby, J. L., & Sandman, C. A. (2021). A predictable home environment may protect child mental health during the COVID-19 pandemic. Neurobiology of Stress, 14, 100291. 10.1016/j.ynstr.2020.100291 [DOI] [PMC free article] [PubMed]
- Goodman R. The Strengths and Difficulties Questionnaire: A research note. Journal of Child Psychology and Psychiatry, and Allied Disciplines. 1997;38(5):581–586. doi: 10.1111/j.1469-7610.1997.tb01545.x. [DOI] [PubMed] [Google Scholar]
- Greening, L., Stoppelbein, L., & Luebbe, A. (2010). The moderating effects of parenting styles on African-American and Caucasian children’s suicidal behaviors. Journal of Youth & Adolescence, 357–369. 10.1007/s10964-009-9459-z [DOI] [PubMed]
- Hajal, N. J., & Paley, B. (2020). Parental emotion and emotion regulation: A critical target for research and intervention to promote child emotion socialization. Developmental Psychology, 403–417. 10.1037/dev0000864 [DOI] [PubMed]
- Hayes, A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. Guilford Press.
- Hayes AF. An Index and Test of Linear Moderated Mediation. Multivariate Behavioral Research. 2015;50(1):1–22. doi: 10.1080/00273171.2014.962683. [DOI] [PubMed] [Google Scholar]
- Johnston C, Mash EJ. A Measure of Parenting Satisfaction and Efficacy. Journal of Clinical Child Psychology. 1989;18(2):167–175. doi: 10.1207/s15374424jccp1802_8. [DOI] [Google Scholar]
- Kazak, A. E., Alderfer, M., Enlow, P. T., Lewis, A. M., Vega, G., Barakat, L., Kassam-Adams, N., Pai, A., Canter, K. S., Hildenbrand, A. K., McDonnell, G. A., Price, J., Schultz, C., Sood, E., & Phan, T. L. (2021). COVID-19 Exposure and Family Impact Scales: Factor Structure and Initial Psychometrics. Journal of Pediatric Psychology, 46(5), 504–513. 10.1093/jpepsy/jsab026 [DOI] [PMC free article] [PubMed]
- Khoury JE, Kaur H, Gonzalez A. Parental Mental Health and Hostility Are Associated With Longitudinal Increases in Child Internalizing and Externalizing Problems During COVID-19. Frontiers in Psychology. 2021;12:3132. doi: 10.3389/fpsyg.2021.706168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Linehan, M. M. (1993). Cognitive-behavioral treatment of borderline personality disorder. Guilford Press.
- Locke LM, Prinz RJ. Measurement of parental discipline and nurturance. Clinical Psychology Review. 2002;22(6):895–929. doi: 10.1016/s0272-7358(02)00133-2. [DOI] [PubMed] [Google Scholar]
- Masten, A. S., & Cicchetti, D. (2016). Resilience in Development: Progress and Transformation. In Developmental Psychopathology: Vol. Four. Risk, Resilience, and Intervention (3rd Edition, pp. 271–333). John Wiley & Sons, Ltd. 10.1002/9781119125556.devpsy406
- Masten AS, Narayan AJ. Child Development in the Context of Disaster, War, and Terrorism: Pathways of Risk and Resilience. Annual Review of Psychology. 2012;63:227–257. doi: 10.1146/annurev-psych-120710-100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McMahon, R. J., & Forehand, R. L. (2003). Helping the noncompliant child: Family-based treatment for oppositional behavior, 2nd ed. Guilford Press.
- Merikangas KR, He J-P, Burstein M, Swanson SA, Avenevoli S, Cui L, Benjet C, Georgiades K, Swendsen J. Lifetime prevalence of mental disorders in U.S. adolescents: Results from the National Comorbidity Survey Replication-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49:980–989. doi: 10.1016/j.jaac.2010.05.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morelli, M., Cattelino, E., Baiocco, R., Trumello, C., Babore, A., & Chirumbolo, A. (2020). Parents and Children During the COVID-19 Lockdown: The Influence of Parenting Distress and Parenting Self-Efficacy on Children’s Emotional Well-Being. Frontiers in Psychology, 11. https://www.frontiersin.org/article/10.3389/fpsyg.2020.584645 [DOI] [PMC free article] [PubMed]
- Moulin, F., El-Aarbaoui, T., Bustamante, J. J. H., Héron, M., Mary-Krause, M., Rouquette, A., Galéra, C., & Melchior, M. (2021). Risk and protective factors related to children’s symptoms of emotional difficulties and hyperactivity/inattention during the COVID-19-related lockdown in France: Results from a community sample. European Child & Adolescent Psychiatry. 10.1007/s00787-021-01752-3 [DOI] [PMC free article] [PubMed]
- Parent J, Forehand R. The Multidimensional Assessment of Parenting Scale (MAPS): Development and Psychometric Properties. Journal of Child & Family Studies. 2017;26:2136–2151. doi: 10.1007/s10826-017-0741-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick, S. W., Henkhaus, L. E., Zickafoose, J. S., Lovell, K., Halvorson, A., & Davis, M. M. (2020). Well-being of Parents & Children During the COVID-19 Pandemic: A National Survey. Pediatrics, 146(4), e2020016824. 10.1542/peds.2020-016824 [DOI] [PubMed]
- Penner F, Ortiz JH, Sharp C. Change in Youth Mental Health During the COVID-19 Pandemic in a Majority Hispanic/Latinx US Sample. Journal of the American Academy of Child & Adolescent Psychiatry. 2021;60(4):513–523. doi: 10.1016/j.jaac.2020.12.027. [DOI] [PubMed] [Google Scholar]
- Peris TS, Ehrenreich-May J. The Parents Are Not Alright: A Call for Caregiver Mental Health Screening During the COVID-19 Pandemic. Journal of the American Academy of Child & Adolescent Psychiatry. 2021;60(6):675–677. doi: 10.1016/j.jaac.2021.02.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pierce M, Hope H, Ford T, Hatch S, Hotopf, M & Abel, K. M. Mental health before and during the COVID-19 pandemic: A longitudinal probability sample survey of the UK population. The Lancet Psychiatry. 2020;7(10):883–892. doi: 10.1016/S2215-0366(20)30308-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pilkonis PA, Choi SW, Reise SP, Stover AM, Riley WT, Cella D. Item Banks for Measuring Emotional Distress From the Patient-Reported Outcomes Measurement Information System (PROMIS®): Depression, Anxiety, and Anger. Assessment. 2011;18(3):263–283. doi: 10.1177/1073191111411667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prime H, Wade M, Browne DT. Risk and resilience in family well-being during the COVID-19 pandemic. The American Psychologist. 2020;75(5):631–643. doi: 10.1037/amp0000660. [DOI] [PubMed] [Google Scholar]
- Roos, L. E., Salisbury, M., Penner-Goeke, L., Cameron, E. E., Protudjer, J. L. P., Giuliano, R., Afifi, T. O., & Reynolds, K. (2021). Supporting families to protect child health: Parenting quality and household needs during the COVID-19 pandemic. PLoS One, 16(5), e0251720. 10.1371/journal.pone.0251720 [DOI] [PMC free article] [PubMed]
- Russell, B. S., Hutchison, M., Tambling, R., Tomkunas, A. J., & Horton, A. L. (2020). Initial Challenges of Caregiving During COVID-19: Caregiver Burden, Mental Health, and the Parent–Child Relationship. Child Psychiatry & Human Development, 51(5), 671–682. 10.1007/s10578-020-01037-x [DOI] [PMC free article] [PubMed]
- Shevlin, M., Butter, S., McBride, O., Murphy, J., Gibson-Miller, J., & Bentall, R. P. (2021). Refuting the myth of a ‘tsunami’ of mental ill-health in populations affected by COVID-19: Evidence that response to the pandemic is heterogeneous, not homogeneous. Psychological Medicine, 1–9. 10.1017/S0033291721001665 [DOI] [PMC free article] [PubMed]
- Smetana JG. Current research on parenting styles, dimensions, and beliefs. Current Opinion in Psychology. 2017;15:19–25. doi: 10.1016/j.copsyc.2017.02.012. [DOI] [PubMed] [Google Scholar]
- Stinson EA, Sullivan RM, Peteet BJ, Tapert SF, Baker FC, Breslin FJ, Lisdahl KM. Longitudinal Impact of Childhood Adversity on Early Adolescent Mental Health During the COVID-19 Pandemic in the ABCD Study Cohort: Does Race or Ethnicity Moderate Findings? Biological Psychiatry Global Open Science. 2021;1(4):324–335. doi: 10.1016/j.bpsgos.2021.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sytsma SE, Kelley ML, Wymer JH. Development and Initial Validation of the Child Routines Inventory. Journal of Psychopathology and Behavioral Assessment. 2001;23(4):241–251. doi: 10.1023/A:1012727419873. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Waller, R., Powell, T., Rodriguez, Y., Corbett, N., Perlstein, S., White, L. K., Barzilay, R., & Wagner, N. J. (2021). The Impact of the COVID-19 Pandemic on Children’s Conduct Problems and Callous-Unemotional Traits. Child Psychiatry & Human Development, 52(6), 1012–1023. 10.1007/s10578-020-01109-y [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.