Abstract
Introduction:
The complexity of modern-day radiotherapy techniques calls for greater accuracy in target volume delineation which requires intensive training and expert guidance. In this study, we intend to evaluate the status of training in target delineation across radiation oncology curriculums in India and utility of webinars in teaching it.
Methodology:
We organized daily webinars on the topics of radiological anatomy and target volume delineation in common sites of cancer over a period of 2 weeks. At the end of the program, a 35 item survey questionnaire was shared with the participants. The responses were analysed and are reported here.
Results:
Out of the 797 participants that registered for the course, 356 radiation oncologists responded to the survey questionnaire. Majority (96%) of our respondents believe that there is a need for additional training in target volume delineation. Ninety percent of the participants felt that radiation oncology curriculum requires a formal radiology training but only 6.7% reported that their training consisted of a dedicated rotation and regular lectures in radiological anatomy. Majority (97%) responded that they were likely to incorporate the points learnt from the webinar sessions in their daily practice. Forty eight percent of respondents opted for attending a webinar to an in-person event in the future while 34% would like to have the option to choose between the two. Ninety four percent agreed that online webinars should be conducted routinely even after the pandemic ends.
Conclusion:
Our survey results suggest that target volume delineation training in India is deficient and virtual teaching programs can be a practical and effective way to improve it.
Key Words: Target volume delineation, webinar, education, virtual teaching
Introduction
Three-dimensional treatment techniques are the norm in current radiotherapy practice. The complexity of modern-day radiotherapy techniques including IMRT, VMAT, SRS and SRT has called for greater accuracy in target volume delineation to optimize treatment results with respect to both efficacy and toxicity (Njeh, 2008). This means that every Radiation Oncologist is now expected to supplement his academic knowledge with a certain amount of skill (Walls et al., 2020). Learning target volume delineation can be difficult due to the multiple cancer sites involved, the ever-changing nature of contouring guidelines, inter-observer variability in interpreting the same guidelines, and a lack of access to experts in the field/site concerned (Jansen et al., 2010; Segedin and Petric, 2016). The dynamic nature of the subject, the sheer volume of academic material and the practical skill component that is involved make it necessary for a trainee or an oncologist to undergo continued learning. This however is often hindered by logistic issues such as the need to travel long distances, the cost it involves, accessibility to experts etc. E-learning owing to its convenience, practicality and effectiveness has attracted significant interest in the recent past (Nadama et al., 2019). The Covid19 pandemic has further fueled interest in this area (Sleiwah et al., 2020, Dewan et al., 2020).
We felt that this is the ideal time to investigate the potential of virtual classroom techniques in teaching target volume delineation. We organized daily webinars over a period of two weeks taught by leading faculty from various institutes across the country on radiological anatomy and target volume delineation. We conducted a survey cum feedback examining the opinion of participants about training in target volume delineation, deficiencies in it, ways of addressing them and the role virtual teaching/technology can play. The responses of the attendees have been produced here.
Materials and Methods
We organized daily webinars on the topics of radiological anatomy and target volume delineation over a period of 2 weeks. The topics were selected to include the common sites of cancer seen in the clinic viz., Breast Cancer, Gliomas and Meningiomas, Head and Neck, Lung, Esophagus and Stomach, Rectum and Anal Canal, Prostate and Cervix. The advert for the sessions was sent through social media. The attendees were expected to register prior to the sessions with the course-coordinator. Study materials, mainly relevant contouring guidelines, were shared online with the participants beforehand. The participants were instructed to read through the study material and practice contouring before attending the class to facilitate discussion. The course was conducted as daily online sessions of 1.5-2 hours over 2 weeks except for weekends. The relevant schedule was shared in advance. We used Cisco-Webex as the platform for conducting these webinar sessions.
Course Objectives
1. To familiarize participants with radiological anatomy relevant to staging and target volume delineation of common cancer sites.
2.To familiarize the participants with standard contouring guidelines.
3. To provide an opportunity to the participants to interact with some of the leading national faculty in the field and clarify any doubt related to target delineation.
4. To use an online virtual platform as a teaching modality and to effectively communicate and interact with the participants on topics of radiological anatomy and target volume delineation.
Course Requirements
The course was designed for trainees, residents, and faculties in the field of radiation oncology irrespective of experience or place of work.
The attendees were required to have a working PC or a mobile device (phone/tablet) with an active internet connection.
Assessment
At the end of the program, an online quiz was conducted for the participants to reflect on their learning. The quiz had 50 peer reviewed questions covering all the topics covered in the lectures. After the quiz, a QandA session with the teachers was conducted to facilitate the participants to actively engage in discussion with the faculty regarding new queries they might have had while trying to apply the learning into practice.
Survey
The participants were requested to fill out a feedback/survey form after the program. Consent was obtained from the participants to analyze their responses and use for publication. The survey consisted of questions about demography, feedback of the webinar series, opinion on current training in target volume delineation and utility of virtual platforms in teaching in radiation oncology. The questions were prepared by the authors and Likert scale with standard terminology for grading the responses was used where appropriate.
Results
Demographics
Out of the 797 participants that registered for the course, 356 radiation oncologists responded to the survey questionnaire. Out of 356 responders - 263 (74%) were residents in training (Junior and Senior residents), 69 (19%) were consultant radiation oncologists and 24 (7%) were working as professor in a medical college. Eighty percent of the respondents had ≤5 years of experience in oncology. Ninety one percent of the participants responded that they practice conformal radiotherapy techniques at their institute. Sixty-three percent were from a government institute while the rest practiced at private institutes. Thirty-five percent responded that they had site specific specialists available at their institute (Table 1).
Table 1.
Participant Demographics, Their Current Status on Conformal Radiotherapy Practice and Radiologic Training. Survey questionnaire (A): TVD (Target Volume Delineation) Webinar series (1st August 2020-12th August 2020)
| Designation/ you are | Consultant Radiation Oncologist | 69 | 19.38% |
| Junior Resident | 173 | 48.60% | |
| Professor at a Medical College | 24 | 6.74% | |
| Senior Resident | 90 | 25.28% | |
| Please indicate your experience in radiation oncology (including years in training) | <2yr | 157 | 44.10% |
| >10yr | 23 | 6.46% | |
| 3-5yr | 129 | 36.24% | |
| 5-10yr | 47 | 13.20% | |
| What kind of environment do you work in? | Government hospital (non-teaching) | 12 | 3.37% |
| Government hospital (teaching) | 212 | 59.55% | |
| Other | 17 | 4.78% | |
| Private hospital (non-teaching) | 30 | 8.43% | |
| Private hospital (teaching) | 85 | 23.88% | |
| Do you practice conformal radiation therapy techniques at your institute? | No | 31 | 8.71% |
| Yes | 325 | 91.29% | |
| Do you have site specific specialists available at your institute? | No | 230 | 64.61% |
| Yes | 126 | 35.39% | |
| Are you aware of the online educational resources available in India and are you satisfied with it? | No, I’m not aware of any such resource | 195 | 54.78% |
| Yes, I’m aware and satisfied | 86 | 24.16% | |
| Yes, I’m aware but they need improvement | 75 | 21.07% | |
| Have you had any formal Radiological anatomy training during residency in Radiation Oncology? | Both rotation and lectures | 24 | 6.74% |
| No, only case to case discussion if required | 164 | 46.07% | |
| Not at all | 47 | 13.20% | |
| Yes, a dedicated rotation in Radiodiagnosis department | 71 | 19.94% | |
| Yes, periodical contact sessions through webinars/seminars/lectures | 50 | 14.04% |
Survey
Tables 2 and 3 show the survey questions and responses. Of note, sixty percent of our responders favored a course covering multiple aspects of a particular cancer site while the rest favored a course covering a particular aspect of multiple cancer sites. Majority (47%) of our participants responded that they preferred a course with one session of 1-2 hours per day conducted over 1-2 weeks, similar to how our course was conducted; only 5% preferred all sessions to be conducted over a weekend.
Table 2.
Comparison of Responses by Radiation Oncologists as Per Their Experience in Field. Participants’ opinion about the need and utility of webinars and guidelines for target volume delineation - Survey questionnaire (A): TVD (Target Volume Delineation) Webinar series (1st August 2020-12th August 2020)
| Questions/Statements | Response category | 0-5 Years (T-286) | 0-5 Years 0% | >5 Years (T-70) | >5 Years 0% | P-value |
|---|---|---|---|---|---|---|
| Do you agree that there is a need to supplement institutional training in target volume delineation with additional courses? | Agree | 274 | 95.80% | 68 | 97.10% | 0.008 |
| Neither Agree nor Disagree | 12 | 4.20% | 0 | 0.00% | (Fisher exact) | |
| Disagree | 0 | 0% | 2 | 2.90% | ||
| Do you agree that an online webinar with tools like chat box and voice option gives more opportunity to interact with the speakers than a live seminar? | Agree | 262 | 91.60% | 66 | 94.30% | 0.451 |
| Neither Agree nor Disagree | 15 | 5.20% | 4 | 5.70% | (Fisher exact) | |
| Disagree | 9 | 3.10% | 0 | 0.00% | ||
| Virtual meetings provide a more stress-free and comfortable environment compared to conventional teaching sessions. | Agree | 243 | 85.00% | 60 | 85.70% | 1 |
| Neither Agree nor Disagree | 3 | 1.00% | 1 | 1.40% | (Fisher exact) | |
| Disagree | 40 | 14.00% | 9 | 12.90% | ||
| Do you agree that online webinars should be conducted routinely post Covid-19 pandemic? | Agree | 267 | 93.40% | 68 | 97.10% | 0.64 |
| Neither Agree nor Disagree | 14 | 4.90% | 2 | 2.90% | (Fisher exact) | |
| Disagree | 5 | 1.70% | 0 | 0.00% | ||
| How much effect has the COVID pandemic had on training in your institute? | Major effect | 96 | 33.60% | 24 | 34.30% | 0.653 |
| Moderate effect | 141 | 49.30% | 31 | 44.30% | (Chi-Square) | |
| Minor effect | 49 | 17.10% | 15 | 21.40% | ||
| What is your opinion of having an online practical assessment course on target volume delineation? | Favour | 267 | 93.40% | 65 | 92.90% | 0.83 |
| Neutral | 18 | 6.30% | 5 | 7.10% | (Fisher exact) | |
| Oppose | 1 | 0.30% | 0 | 0% | ||
| How often do you consult target volume delineation guidelines? | Always | 167 | 58.40% | 24 | 34.30% | 0.001 |
| Often | 108 | 37.80% | 46 | 65.70% | (Fisher exact) | |
| Rarely | 11 | 3.80% | 0 | 0.00% |
Table 3.
Participants’ Attitudes and Practice on Use of Social Media/Platforms, Audio/Visual Aids and Schedule Preference for Conducting Webinars on TVD. Survey questionnaire (B): TVD (Target Volume Delineation) Webinar series (1st August 2020-12th August 2020)
| How did you come to know about the TVD2020 webinar series? | 36 | 10.11% | |||
| Friend | 43 | 12.08% | |||
| Other | 2 | 0.56% | |||
| Senior/Teacher | 64 | 17.98% | |||
| Telegram | 24 | 6.74% | |||
| WhatsApp group | 187 | 52.53% | |||
| How would you like an online course to be conducted? | A course covering a particular aspect of multiple cancer sites (Contouring/Evidence based Management etc.) | 141 | 39.61% | ||
| A course on multiple aspects of a particular cancer site (Radiology, evidence-based management, treatment techniques) | 215 | 60.39% | |||
| Which format do you prefer for such a course in future? | 2-3 sessions per week over 1 month | 94 | 26.40% | ||
| All sessions (10-12hrs) conducted over a weekend | 17 | 4.78% | |||
| One session 1-2 hrs per week over 2-3 months | 75 | 21.07% | |||
| One session of 1-2 hrs per day over 1-2 weeks | 168 | 47.19% | |||
| Other | 2 | 0.56% | |||
| Which mode of interaction do you prefer during the Q&A session with the speakers? | Chat box | 160 | 44.94% | ||
| I’d like to have both options | 154 | 43.26% | |||
| Neutral | 8 | 2.25% | |||
| Voice | 34 | 9.55% | |||
| Which online platform you will prefer for attending online sessions? | CISCO WEBEX | 208 | 58.43% | ||
| GOOGLE MEET | 32 | 8.99% | |||
| Microsoft Teams | 14 | 3.93% | |||
| Others | 2 | 0.56% | |||
| ZOOM | 100 | 28.09% | |||
| Which platform of communication would you prefer for notification during future courses? | 185 | 51.97% | |||
| 1 | 0.28% | ||||
| Telegram | 4 | 1.12% | |||
| WhatsApp Group | 138 | 38.76% | |||
| WhatsApp Personal | 28 | 7.87% | |||
| After the pandemic ends, between an online webinar or an in-person event, what would you prefer? | I’d like to have option to choose between online and in-person for the same event | 121 | 33.99% | ||
| I’d prefer to attend an in-person event | 57 | 16.01% | |||
| I’d prefer to attend an online event | 171 | 48.03% | |||
| No preference | 7 | 1.97% | |||
| How many webinar sessions you were able to attend from 1st August to 12th August on Target Volume delineation? | <5 | 46 | 12.92% | ||
| >5 | 48 | 13.48% | |||
| 5 | 152 | 42.70% | |||
| ALL | 110 | 30.90% | |||
Webinar feedback
Table 4 shows the feedback questions and responses. Ninety percent of the responders felt that the webinars helped in improving their knowledge of radiological anatomy and target volume delineation to a large extent. More than 90% answered that they were satisfied with the utilization of time during the webinar sessions and the time allotted for interaction with the speakers. Ninety two percent of responders benefitted from the study material that was shared before the webinars while 89% found the quiz conducted at the end of the program to be useful.
Table 4.
Comparison of Responses by Radiation Oncologists as per Their Experience in Field. Participants feedback on target volume delineation webinar series-Survey questionnaire (B): TVD (Target Volume Delineation) Webinar series (1st August 2020-12th August 2020)
| Questions/Statements | Response category | 0-5 Years (T-286) | 0-5 Years 0% |
>5 Years (T-70) |
>5 Years 0% |
P value |
|---|---|---|---|---|---|---|
| How useful did you find the study material shared before the webinars in understanding the classes? | Very useful | 266 | 93.00% | 63 | 90.00% | 0.445(Fisher exact) |
| Moderately useful | 15 | 5.20% | 6 | 8.60% | ||
| Slightly useful | 5 | 1.70% | 1 | 1.40% | ||
| How useful was the online quiz in revising the points learned during the webinar? | Very useful | 257 | 89.90% | 59 | 84.30% | 0.172(Fisher exact) |
| Moderately useful | 25 | 8.70% | 8 | 11.40% | ||
| Slightly useful | 4 | 1.40% | 3 | 4.30% | ||
| To what extent do you think this webinar help in improving your knowledge of Radiological Anatomy and Target Volume Delineation? | To a very large extent | 134 | 46.90% | 30 | 42.90% | 0.795 (ChiSqu) |
| To large extent | 128 | 44.80% | 33 | 47.10% | ||
| To some extent | 24 | 8.40% | 7 | 10.00% | ||
| How do you rate the overall quality- (Topics chosen and time duration) of the webinar sessions? | Excellent | 173 | 60.50% | 48 | 68.60% | 0.452(Fisher exact) |
| Good | 107 | 37.40% | 21 | 30.00% | ||
| Fair | 6 | 2.10% | 1 | 1.40% | ||
| How likely are you to incorporate the points learnt from this webinar into your daily practice? | Extremely likely | 170 | 59.40% | 38 | 54.30% | 0.100(Fisher exact) |
| Likely | 110 | 38.50% | 27 | 38.60% | ||
| Less likely | 6 | 2.10% | 5 | 7.10% | ||
| Whether the session time during webinar was effectively utilized | Agree | 283 | 99.00% | 69 | 98.60% | 0.585(Fisher exact) |
| Neutral | 1 | 0.30% | 1 | 1.40% | ||
| Disagree | 2 | 0.70% | 0 | 0% | ||
| Time given for interaction with the speaker was adequate | Agree | 264 | 92.30% | 64 | 91.40% | 0.793(Fisher exact) |
| Neutral | 15 | 5.20% | 4 | 5.70% | ||
| Disagree | 7 | 2.40% | 2 | 2.90% |
Statistical Analysis
Based on participants experience in radiation field i.e., (< 5 years or >5 years) Fisher exact test and Chi-square test were used to statistically compare the opinions of participants on survey questions related to need and utility of webinars and guidelines for target volume delineation. feedback on this webinar series was also compared using these tests.
Out of 356 total participants- 286 participants had < 5 year of experience in radiation oncology field and 70 had >5 years. However, there was much concordance in their opinions and p values were not statistically significant as shown in tables 2 and 4 except one category i.e., on consult of target volume delineation guidelines (p = 0.001). Participants with <5 years’ experience stated to use target volume delineation guidelines 58% ‘‘always’’ and 38% ‘‘often’’ compared to 34% and 66% respectively participants with >5 years of experience. This difference obviously reflects their experience in conformal radiotherapy. However, 4% of participants among <5 years’ experience rarely used contouring guidelines in their practice.
Discussion
The largest uncertainty in the process of radiotherapy is imputed to variability in target volume delineation, underscoring the imperative need of greater accuracy in this step to favorably impact the therapeutic ratio (Njeh, 2008).
The major source that guides target volume delineation worldwide is international consensus guidelines by expert groups. Eighty-eight percent of our survey participants responded that they routinely consult contouring guidelines in the clinic. However, it is important to acknowledge that these guidelines on their own are not adequate (van der Veen et al., 2019). Several studies show that the use of contouring guidelines alone is associated with significant inter-operator variability that stems from differences in interpretation and thereby strongly suggest supplementation with additional standardized teaching and resources such as auto-contours, three-dimensional atlas, peer review etc. to guarantee uniformity and accuracy (Bekelman et al., 2009; Szumacher et al., 2010; D’Souza et al., 2014; Labranche et al., 2015; Gillespie et al., 2017). The PETPLAN study group from Germany, for instance, observed that there was great interobserver variability in lung cancer volumes delineated by oncologists across 14 participating centers; this variability was significantly reduced when contouring followed a formal teaching intervention (Schimek-Jasch et al., 2015). They concluded that despite detailed contouring guidelines, differences in interpretation lead to significant variability that could effectively be reduced by additional teaching. Another study by Onal et al., (2017) also demonstrated that a teaching intervention by an experienced radiation oncologist significantly reduced interobserver variability and improved the accuracy in target delineation among a group of practicing radiation oncologists who had a minimum experience of 5 years. The same is strongly represented in our survey by the fact that 96% of our respondents agreed that there was a need for additional training in target volume delineation. Despite the uniform recognition of this fact, there exist a very few resources for radiation oncologists aimed at target volume delineation. Fifty-five percent of our participants said that they were not aware of any online oncology education resources available in India; whereas 21% of the participants were aware of certain resources but felt that there was a need for improvement.
Accurate target volume delineation, as we pointed out as the single most critical step in the radiotherapy process, requires sound knowledge in radiological anatomy in addition to strict adherence to practice guidelines. Canadian investigators evaluated the impact of an integrated course conducted by a multidisciplinary group consisting of anatomists, radiologists and radiation oncologists that focused on teaching anatomy and radiology in addition to target volume delineation (with the objective of improving contouring accuracy) (Jaswal et al., 2015) They found that such a form of integrated teaching improved the participant’s knowledge of anatomy and radiology and significantly increased their contouring accuracy (The participants also reported increased confidence). This study highlights the need for radiology training for precise target volume delineation. However, most radiation oncology programs across the world are deficient in this regard. In a survey conducted among radiation oncology residents in the USA, most residents felt that radiological anatomy training during residency was suboptimal and a dedicated training curriculum preferably including didactic lectures co-taught by radiologists and radiation oncologists was necessary (Matalon et al., 2019). A similar survey of radiation oncologists from U.K. also highlighted the lack of radiology training in NHS institutes with only 10% of the respondents having some form of training; only 4% had formal radiological training, while 6% had informal interactions with radiologists (Jefferies et al., 2009). Ninety percent of the participants in this survey felt that formal radiology training was necessary. Our survey results are in accordance with the aforementioned data. Only 7% of our participants reported that they had a formal training in radiological anatomy that consisted of a dedicated rotation and regular lectures in radiology. Twenty percent had a dedicated rotation but no systematic teaching in the form of lectures or seminars and another 14% had only periodical lectures with no dedicated rotation. The majority (59%) however, had no formal training in the subject. The outcome of incorporating radiological anatomy teaching in our course is firmly highlighted by the fact that 100% of the responders felt that the webinars helped them at least to some extent in improving their knowledge of radiological anatomy in addition to target volume delineation. The introduction of newer techniques and technologies in diagnostic radiology and their incorporation into target delineation further accentuates the need for continued learning in radiological anatomy (Segedin and Petric, 2016).
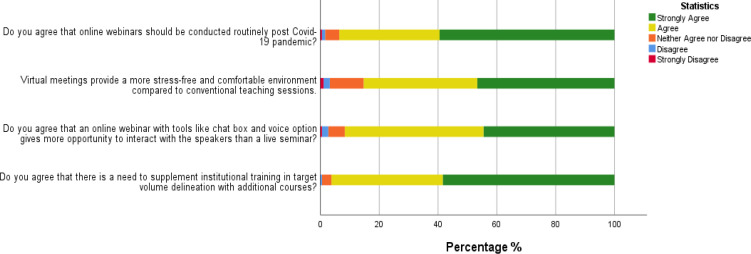
Virtual conferences carry several inherent advantages such as accessibility, the ability to attend at the comfort of one’s home or workplace, the avoidance of hassles of travel especially in the case of international conferences and the availability of tools such as chat box that make it easier to interact with the speaker in real-time (Liu, n.d.; Lecueder and Manyari, 2000; Kimura et al., 2018; Porpiglia et al., 2020) All these factors make virtual conferences practical, effective, convenient and an attractive way of conducting conferences and teaching programs. But, the shift from conventional meetings to virtual ones has been a slow and gradual process over the last few years and this could possibly be attributed to various factors such as unawareness of their availability, hesitation to embrace newer methods or resistance to accept change. However, the COVID pandemic has facilitated this transition and has resulted in sudden and widespread adoption of this highly efficient tool of communication and learning (Sleiwah et al., 2020). In an online poll conducted by Nature, over 40% of the participants responded that they had attended an online scientific meeting during the COVID pandemic and more than 80% agreed that some conferences should continue to remain virtual even after the pandemic ends (Anon, 2020). In our survey, 85% believed that virtual meetings provide a more stress free and comfortable environment compared to conventional teaching sessions and 92% agreed that online webinar tools like chat box and voice option make it easier to interact with the speakers. Their experience with webinar-based teaching is unambiguously reflected in the fact that 94% of our respondents agreed that online webinars should be conducted routinely even after the pandemic ends (Figure 1). Approximately 48% of our participants said that they would prefer attending a webinar to an in-person event in the future while 34% said they would like to have the option to choose between the two. However, virtual teaching programs do carry certain disadvantages such as the lack of physical interaction, the inability to control the audience’s environment and the possibility of technical glitches such as network interruptions, software compatibility issues and hardware malfunction.
Figure 1.
Stacked Bar Chart Representing the Responses of Radiation Oncologists Regarding Use of Webinar for Training in Target Volume Delineation (Survey Questionnaire (A): TVD (Target Volume Delineation) Webinar series (1st August 2020-12th August 2020)
Our teaching course was scrupulously designed after taking into consideration all the above factors. We designed the program with the objective of improving the standard of target volume delineation among residents and consultants through a systematic approach wherein we conducted daily webinars over a period of 2 weeks by experienced radiation oncologists. The webinars were focused on target volume delineation in the light of international consensus contouring guidelines while also providing a comprehensive overview of CT and MRI based radiological anatomy with particular emphasis on patterns of spread and nodal pathways. We collected feedback of the participants on their experience with the way we designed our course This information would be valuable in designing our future courses better. Overall, the webinar sessions were rated excellent by 62% of our participants and 36% felt they were good. Ninety-seven percent responded that they were likely to incorporate the points learnt from the webinar sessions in their daily practice.
Response to open ended questions
AVARO Project, ICRO, RTOG Guidelines, E-Contour were among the few names listed by 45% participants who were aware of online resources. Suggestions were given to continue regular update through webinars on contouring guidelines as well as on other topics such as plan evaluation, pediatric cancers, stereotactic radiotherapy guidelines etc.
Junior residents requested to cover radiological anatomy for staging and contouring purpose in detail. Considering this we have included site wise modules cum workshop to cover radiological anatomy and staging in addition to target volume delineation webinar series in the upcoming webinar program.
In conclusion, our survey that focused on training in radiation oncology in India highlighted the various deficiencies and hurdles that exist. Despite the availability of various guidelines, there exist significant challenges in implementing them. Additional learning in the form of teaching programs by experts can help in filling up the existing lacunae. However, this is often hindered by logistic issues and inaccessibility to experts. These issues can be effortlessly mitigated with the help of virtual teaching programs, that our respondents find comfortable and stress-free with a better opportunity to interact with the speaker.
Author Contribution Statement
The authors confirm contribution to the paper as follows: Study conception and Design: Pooja Sethi, Syed Touseef Ahmed Hussain, Pragna Sagar Rapole; Data collection: Pooja Sethi, Pragna Sagar Rapole, Syed Touseef Ahmed Hussain, Aswin Chandran Veluthattil, Ninad Patil, Chandramouli Ramalingam ; Analysis and Interpretation of results: Pooja Sethi, Thulasingam Mahalakshmy, Pragna Sagar Rapole, Syed Touseef Ahmed Hussain; Draft manuscript preparation: Syed Touseef Ahmed Hussain, Pooja Sethi, Pragna Sagar Rapole, Aswin Chandran Veluthattil. All authors reviewed the results and approved the final version of the manuscript.
Consent
Informed consent is obtained from all the participants responding to the survey. Institute ethical clearance (JIPMER) obtained for publication purpose of this survey(Enclosed). (IEC Protocol No: JIP/IEC/2021/287). Supplement file - Enclosed.
Declaration for conflict of interest
The authors declare no conflicts of interest.
Acknowledgements
We acknowledge All teachers, RCC Faulty and Residents who coordinated in conducting online course on Target volume delineation.
References
- Anon Coronavirus in charts: the fact-checkers correcting falsehoods. Nature. 2020;2020:1–22. doi: 10.1038/d41586-020-01136-8. [DOI] [PubMed] [Google Scholar]
- Bekelman JE, Wolden S, Lee N. Head-and-neck target delineation among radiation oncology residents after a teaching intervention: A Prospective, Blinded Pilot Study. Int J Radiat Oncol Biol Phys. 2009;73:416–23. doi: 10.1016/j.ijrobp.2008.04.028. [DOI] [PubMed] [Google Scholar]
- D’Souza L, Jaswal J, Chan F, et al. Evaluating the impact of an integrated multidisciplinary head and neck competency-based anatomy and radiology teaching approach in radiation oncology: A prospective cohort study. BMC Med Educ. 2014;2014 doi: 10.1186/1472-6920-14-124. DOI: 10.1186/1472-6920-14-124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dewan A, Dewan AK, Mitra S. Life of an oncologist after COVID-19 pandemic. Asian Pac J Cancer Care. 2020;5:179–81. [Google Scholar]
- Gillespie EF, Panjwani N, Golden DW, et al. Multi-institutional randomized trial testing the utility of an interactive three-dimensional contouring atlas among radiation oncology residents. Int J Radiat Oncol Biol Phys. 2017;98:547–54. doi: 10.1016/j.ijrobp.2016.11.050. [DOI] [PubMed] [Google Scholar]
- Jansen EPM, Nijkamp J, Gubanski M, et al. Interobserver Variation of clinical target volume delineation in gastric cancer. Int J Radiat Oncol Biol Phys. 2010;77:1166–70. doi: 10.1016/j.ijrobp.2009.06.023. [DOI] [PubMed] [Google Scholar]
- Jaswal J, D’Souza L, Johnson M, et al. Evaluating the impact of a Canadian national anatomy and radiology contouring boot camp for radiation oncology residents. Int J Radiat Oncol Biol Phys. 2015;91:701–7. doi: 10.1016/j.ijrobp.2014.11.009. [DOI] [PubMed] [Google Scholar]
- Jefferies S, Taylor A, Reznek R. Results of a national survey of radiotherapy planning and delivery in the UK in 2007. Clin Oncol. 2009;21:204–17. doi: 10.1016/j.clon.2008.11.017. [DOI] [PubMed] [Google Scholar]
- Kimura S, Onishi H, Kawamata M. Characteristics and perceptions of twice-weekly webinars for primary care physicians in Japan: a qualitative study. Int J Med Educ. 2018;9:229–38. doi: 10.5116/ijme.5b6b.21e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Labranche L, Johnson M, Palma D, D’Souza L, Jaswal J. Integrating anatomy training into radiation oncology residency: Considerations for developing a multidisciplinary, interactive learning module for adult learners. Anat Sci Educ. 2015;8:158–65. doi: 10.1002/ase.1472. [DOI] [PubMed] [Google Scholar]
- Lecueder S, Manyari DE. Virtual congresses. J Am Med Informatics Assoc. 2000;7:21–7. doi: 10.1136/jamia.2000.0070021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matalon SA, Howard SA, Abrams MJ. Assessment of radiology training during radiation oncology residency. J Cancer Educ. 2019;34:691–5. doi: 10.1007/s13187-018-1357-1. [DOI] [PubMed] [Google Scholar]
- Nadama HH, Tennyson M, Khajuria A. Evaluating the usefulness and utility of a webinar as a platform to educate students on a UK clinical academic programme. J R Coll Physicians Edinb. 2019;49:317–22. doi: 10.4997/JRCPE.2019.415. [DOI] [PubMed] [Google Scholar]
- Njeh CF. Tumor delineation: The weakest link in the search for accuracy in radiotherapy. J Med Phys. 2008;33:136–40. doi: 10.4103/0971-6203.44472. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Porpiglia F, Checcucci E, Autorino R, et al. Traditional and virtual congress meetings during the COVID-19 pandemic and the post-COVID-19 Era: Is it Time to Change the Paradigm? Eur Urol. 2020;78:301–3. doi: 10.1016/j.eururo.2020.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schimek-Jasch T, Troost EGC, Rücker G, et al. A teaching intervention in a contouring dummy run improved target volume delineation in locally advanced non-small cell lung cancer. Strahlentherapie und Onkol. 2015;191:525–33. doi: 10.1007/s00066-015-0812-8. [DOI] [PubMed] [Google Scholar]
- Segedin B, Petric P. Uncertainties in target volume delineation in radiotherapy - Are they relevant and what can we do about them? Radiol Oncol. 2016;50:254–62. doi: 10.1515/raon-2016-0023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sleiwah A, Mughal M, Hachach-Haram N, Roblin P. COVID-19 lockdown learning: The uprising of virtual teaching. J Plast Reconstr Aesthetic Surg. 2020;73:1575–92. doi: 10.1016/j.bjps.2020.05.032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szumacher E, Harnett N, Warner S, et al. Effectiveness of educational intervention on the congruence of prostate and rectal contouring as compared with a gold standard in three-dimensional radiotherapy for prostate. Int J Radiat Oncol Biol Phys. 2010;76:379–85. doi: 10.1016/j.ijrobp.2009.02.008. [DOI] [PubMed] [Google Scholar]
- van der Veen J, Gulyban A, Nuyts S. Interobserver variability in delineation of target volumes in head and neck cancer. Radiother Oncol. 2019;137:9–15. doi: 10.1016/j.radonc.2019.04.006. [DOI] [PubMed] [Google Scholar]
- Walls GM, Hanna GG, McAleer JJ. Learning radiotherapy: The state of the art. BMC Med Educ. 2020 doi: 10.1186/s12909-020-02054-z. DOI: 10.1186/s12909-020-02054-z. [DOI] [PMC free article] [PubMed] [Google Scholar]