Abstract
Background:
The 2019 coronavirus (COVID-19) pandemic placed unprecedented strains on the U.S. health care system, putting health care workers (HCWs) at increased risk for experiencing moral injury (MI). Moral resilience (MR), the ability to preserve or restore integrity, has been proposed as a resource to mitigate the detrimental effects of MI among HCWs.
Objectives:
The objectives of this study were to investigate the prevalence of MI among HCWs, to identify the relationship among factors that predict MI, and to determine whether MR can act as buffer against it.
Design:
Web-based exploratory survey.
Setting/Subjects:
HCWs from a research network in the U.S. mid-Atlantic region.
Measurements:
Survey items included: our outcome, Moral Injury Symptoms Scale–Health Professional (MISS-HP), and predictors including demographics, items derived from the Rushton Moral Resilience Scale (RMRS), and ethical concerns index (ECI).
Results:
Sixty-five percent of 595 respondents provided COVID-19 care. The overall prevalence of clinically significant MI in HCWs was 32.4%; nurses reporting the highest occurrence. Higher scores on each of the ECI items were significantly positively associated with higher MI symptoms (p < 0.05). MI among HCWs was significantly related to the following: MR score, ECI score, religious affiliation, and having ≥20 years in their profession. MR was a moderator of the effect of years of experience on MI.
Conclusions:
HCWs are experiencing MI during the pandemic. MR offers a promising individual resource to buffer the detrimental impact of MI. Further research is needed to understand how to cultivate MR, reduce ECI, and understand other systems level factors to prevent MI symptoms in U.S. HCWs.
Keywords: COVID-19, health care worker, moral injury, moral resilience, spirituality, survey
Introduction
The 2019 coronavirus (COVID-19) pandemic has wreaked havoc on the health care workforce. The volume of people contracting and dying from the virus in the United States, coupled with complex ethical dilemmas, has contributed to a secondary pandemic composed of clinician depletion, despair, and moral suffering.1,2 Early data suggest that clinicians and other health care workers (HCWs) are experiencing a myriad of physical, psychological, financial, mental, and behavioral health consequences.1–3 Those in palliative care have carried a significant burden during the pandemic and may be at particular risk given their proximity to patient and staff suffering, cumulative death, and compounded grief.4 These findings are cumulative on a workforce already suffering from burnout.5–7
Before the pandemic, moral injury (MI) was proposed as a more robust expandatory model for the residue of consequences clinicians experience in their roles.8 A concept primarily studied in the military, MI refers to a type of moral suffering characterized by exposure to circumstances that violate one's moral values and beliefs in ways that erode integrity, moral capability, perception of basic goodness, and create distress on a psychological, behavioral, social, or spiritual level.9–11 Such circumstances involve individual responsibility (witnessing or perpetrating a moral wrong) or betrayals or transgressions by others who have responsibility—and often authority.12,13 The experience of MI may not be recognized in the moment, but rather retrospectively when an individual realizes that a moral breech has occurred.14 The impact of these moral wounds can be enduring and painful.15 Questions arise about what, if anything, can be done to stem the tide of these experiences, particularly during a pandemic.
Moral resilience (MR), “the capacity of an individual to sustain or restore their integrity in response to moral adversity,”13,16(p112) has been proposed as a means to transform moral suffering in health care.13 Among interprofessional clinicians, MR includes key components of personal and relational integrity, buoyancy, self-regulation and awareness, moral efficacy, and self-stewardship.17 By buffering against MI and its negative consequences,17,18 MR offers clinicians the capability to respond to complex, often intractable, ethical issues that arise in clinical practice and during a pandemic notwithstanding the systemic factors that produced them.13,19
Understanding how these concepts apply during the COVID-19 pandemic systems is in its early stages.20 The purpose of this study was to investigate the prevalence of MI among HCWs and to identify the relationship among various factors, including MR as a moderator or buffer against MI.21
Materials and Methods
A web-based survey using Qualtrics was conducted from June 2020 to November 2020 to elicit HCWs' experiences of MR, MI, and stressors from a cohort of HCWs amidst the COVID-19 pandemic. Nurses, physicians, advanced practice providers, and other clinical roles older than 18 years were included: pediatric providers were excluded. A convenience sample from the Johns Hopkins Clinical Research Network (JHCRN), a network of academic and community-based medical centers in Maryland, Pennsylvania, and District of Columbia, distributed the survey invitation and web-based link to the survey. The Johns Hopkins Institutional Review Board deemed this study to be exempt; completion of the survey implied consent to participate.
Measures
Ethical concerns index (ECI) was measured using 15 items developed by three subject matter experts in medicine, bioethics, and nursing and literature review. The response scale for the ECI items was 1 = not at all; 2 = a little; 3 = a moderate amount; 4 = a lot; and 5 = a great deal. The stem for all items was “Given the pandemic crisis right now, to what extent are you experiencing distress related to the following situations?” Construct validity was demonstrated using factor analysis: all items loaded onto a single factor with factor loadings >0.50, which explained 49.55% of the variability, alpha = 0.93. MR was measured using a shortened version of the Rushton Moral Resilience Scale (RMRS).18 Through factor analysis, the shortened scale was reduced to four items that loaded onto a single factor, which explained 65.75% of the variability in the items, all items had factor loadings >0.50, alpha = 0.74. MI was measured using the 10-item Moral Injury Symptom Scale–Health Professionals version (MISS-HP), alpha = 0.93; ≥36 as the cutoff for clinically significant MI.22
Data analysis
Data were analyzed using SPSS® statistical software (version 27.0). The PROCESS utility was used to analyze moderation.23 Descriptive statistics means and standard deviations, or percentages were summarized to characterize sample demographics. Spearman's correlation coefficients were calculated to examine the relationship between ECI and MI. A model building approach was used to understand and assess multicollinearity among variables. The bivariate ANOVA independent variables (IVs) with three or more levels or t-tests (IVs with two levels) using one or hypothesized antecedent with our dependent variable, MI, were examined. Variables that were significant in preliminary bivariate analyses were added to a multiple regression model. In the final model, MR was added as a moderator of number of years in profession. The final model is elaborated here; other analyses are briefly described.
Results
Overall, 595 respondents participated in the survey. Table 1 outlines respondents' characteristics. The majority of participants were involved in COVID-19 care (64.9%). HCWs with less experience were more likely to be providing COVID-19 care: <10 years (75.4%); 10–20 years (68.9%); and >20 years (56.8%). This association was statistically significant (p < 0.05). The overall prevalence of clinically significant MI (≥36)22 was 32.4%. Nurses had the highest MI incidence (38.1%), followed by respiratory therapists (35.5%), physicians (29.7%), and Nurse Practitioners/Physician Assistants (NP/PAs) (25%).
Table 1.
Participant Characteristics (N = 595)
| n | % | |
|---|---|---|
| What is your profession? | ||
| Nurse | 344 | 58.1 |
| Physician | 70 | 11.8 |
| Respiratory therapist | 37 | 6.3 |
| Nurse practitioner/physician assistant | 42 | 7.1 |
| Othera | 99 | 16.7 |
| How many years have you worked in this profession? | ||
| Less than 10 years | 216 | 36.4 |
| 10–20 years | 146 | 24.6 |
| Greater than 20 years | 231 | 39.0 |
| What is your spiritual/religious preference? | ||
| Buddhist | 4 | 0.7 |
| Christian/protestant | 250 | 42.2 |
| Hindu | 7 | 1.2 |
| Islam | 8 | 1.3 |
| Roman catholic | 149 | 25.1 |
| Jewish | 19 | 3.2 |
| Spiritual not religious | 70 | 11.8 |
| No religious preference | 86 | 14.5 |
| What is your ethnicity? | ||
| American Indian/Alaskan Native | 0 | 0.0 |
| Asian/Pacific Islander | 19 | 3.8 |
| Black/African American | 27 | 5.5 |
| White/Caucasian | 408 | 82.4 |
| Multiple races | 16 | 3.2 |
| Prefer not to answer | 25 | 5.1 |
| What is the highest level of education you have completed? | ||
| Associate's degree | 103 | 17.5 |
| Bachelor's degree | 238 | 40.4 |
| Master's degree | 144 | 24.4 |
| Doctorate | 104 | 17.7 |
| What is your practice location? | ||
| Emergency department | 47 | 8.0 |
| Inpatient—critical care | 120 | 20.4 |
| Inpatient—other | 242 | 41.1 |
| Operating room | 21 | 3.6 |
| Outpatient/ambulatory care | 159 | 27.0 |
| Are you involved in COVID-19 clinical care? | ||
| Yes | 386 | 64.9 |
| No | 209 | 35.1 |
| Are you involved in COVID-19 research in the response to the pandemic within your organization? | ||
| Yes | 96 | 16.1 |
| No | 499 | 83.9 |
| MI score (≥36) | ||
| Yes | 193 | 32.4 |
| No | 341 | 57.3 |
Other includes pharmacists, social workers, administrators, chaplains, and clinical support personnel.
COVID-19, 2019 coronavirus; MI, moral injury.
Correlations between the individual ECIs and MI in the 534/595 participants who completed the MI questions were examined (Table 2). Higher ECI scores were associated with significantly higher levels of MI symptoms (p < 0.05). Moderate correlations24 with MI included: (1) experiencing negative consequences at work if they voiced safety concerns; (2) working with limited resources; (3) implementing the decisions of others when it threatens their own values; (4) losing their ability to advocate for their individual patient's needs because of resource constraints; (5) making decisions to limit/forgo interventions for their patients without their usual level of involvement; and (6) being infected while performing their professional duties in the hospital. For the regression analysis, a total mean score for the ECI was computed.
Table 2.
Correlation (Spearman's Correlation Coefficient) between Ethical Concerns Index and Moral Injury Symptoms
| |
MI symptomsa |
|
|---|---|---|
| ECIb | ρ (95% CI) | Mean (SD) |
| Experiencing negative consequences at work (e.g., being fired, demoted, furloughed) if you voice safety concerns | 0.371 (0.289 to 0.441)c | 2.60 (1.54) |
| Working with limited resources (PPE, medications, ventilators, staff, etc.) | 0.350 (0.263 to 0.427)c | 3.29 (1.43) |
| Implementing the decisions of others when it threatens your own values | 0.295 (0.203 to 0.378)c | 2.88 (1.37) |
| Losing your ability to advocate for your individual patient's needs because of resource constraints | 0.289 (0.205 to 0.364)c | 2.80 (1.44) |
| Making decisions to limit/forgo interventions for your patients without their usual level of involvement | 0.289 (0.202 to 0.365)c | 2.50 (1.35) |
| Being infected while performing your professional duties in the hospital | 0.288 (0.200 to 0.372)c | 3.24 (1.32) |
| Spreading infection to your loved ones at home | 0.252 (0.163 to 0.346)c | 3.51 (1.27) |
| Shifting decision-making authority to hospital triage officers/teams | 0.252 (0.158 to 0.329)c | 2.41 (1.35) |
| Having your close therapeutic clinician–patient relationships being disrupted because of social distancing or hospital policy | 0.250 (0.162 to 0.330)c | 2.95 (1.30) |
| Making triage/resource allocation decisions | 0.249 (0.159 to 0.331)c | 2.47 (1.29) |
| Protecting your colleagues/staff from increased risks and exposures | 0.239 (0.149 to 0.327)c | 3.36 (1.19) |
| Communicating changes in practices/policies about limiting/forgoing interventions with patients/families | 0.224 (0.131 to 0.308)c | 2.70 (1.30) |
| Spreading infection to your patient(s) | 0.205 (0.116 to 0.290)c | 2.90 (1.32) |
| Witnessing your patients dying alone | 0.168 (0.077 to 0.245)c | 3.58 (1.49) |
| My patients not having access to their loved ones while in the hospital | 0.091 (0.001 to 0.178)d | 3.70 (1.25) |
MI symptoms overall score ranged from 10 to 98.
ECI response scale is 1 = not at all; 2 = a little; 3 = a moderate amount; 4 = a lot; and 5 = a great deal.
Significant at p < 0.001 level (two-tailed).
Significant at p < 0.05 level (two-tailed).
ECI, ethical concerns index; SD, standard deviation.
Variables significantly related to MI at the bivariate level included: years in profession, religious/spiritual preference, MR score, ECI, and COVID-19 care (Table 3). Variables significant at the bivariate level were added to a multiple regression model predicting MI. MR score, ECI score, religious/spiritual preference, and number of years in the profession statistically significantly predicted MI score [F(6, 522) = 34.60, p = 0.0001, R2 = 0.28]. All variables except involvement in COVID-19 care added statistical significance to the prediction (p < 0.05). To understand why COVID care was no longer significant in the full model, we tested models with COVID care and one other predictor. COVID care was not statistically significant when MR was added to the model predicting MI. However, COVID care remained a significant predictor when each of the other predictors was added to the model.
Table 3.
Bivariate Analysis of Demographic and Clinical Variables with Moral Injury Symptoms
| Mean (SD) | F | p | |
|---|---|---|---|
| How many years in profession? | 14.97 | <0.01 | |
| 0–10 | 36.59 (14.84) | ||
| 10–20 | 32.91 (12.04) | ||
| 20+ | 29.42 (12.12) | ||
| What is your profession? | 0.86 | 0.486 | |
| Nurse | 33.39 (13.77) | ||
| Physician | 31.07 (13.27) | ||
| Respiratory therapist | 33.28 (12.21) | ||
| Nurse practitioner/physician assistant | 29.98 (10.34) | ||
| Other | 32.96 14.21) | ||
| What is your specialty? | 1.28 | 0.195 | |
| Palliative care | 41.6 (16.64) | ||
| Neurology/neuroscience | 39.11 (18.85) | ||
| Surgery | 35.01 (13.41) | ||
| Pharmacy | 34.99 (16.59) | ||
| Orthopedics | 34.5 (13.2) | ||
| Ophthalmology | 34 (5.66) | ||
| Internal medicine—all specialties | 34.49 (13.4) | ||
| Nephrology | 34.33 (11.93) | ||
| Other | 32.58 (15.27) | ||
| Oncology | 29.97 (12.24) | ||
| Pediatrics | 29.28 (10.43) | ||
| Family medicine | 28.14 (4.49) | ||
| Psychiatry | 27.37 (9.23) | ||
| OB/GYN | 27.17 (9.58) | ||
| What is your religious/spiritual preference? | 2.06 | 0.047 | |
| Buddhist | 50.25 (38.39) | ||
| Christian/protestant | 32.15 (13.09) | ||
| Hindu | 27.00 (8.03) | ||
| Islam | 35.29 (16.08) | ||
| Roman catholic | 32.72 (13.21) | ||
| Jewish | 29.19 (12.34) | ||
| Spiritual/not religious | 31.86 (12.60) | ||
| No religious preference | 35.95 (13.51) | ||
| What is the highest level of education you have completed? | 0.09 | 0.968 | |
| Associate's degree | 32.76 (12.60) | ||
| Bachelor's degree | 33.03 (13.02) | ||
| Master's degree | 32.85 (14.69) | ||
| Doctorate | 32.19 (13.64) | ||
| What is your practice location? | 1.67 | 0.156 | |
| Emergency department | 33.19 (11.65) | ||
| Inpatient—critical care | 34.34 (13.09 | ||
| Inpatient—other | 33.43 (13.79) | ||
| Operating room | 34.90 (15.01) | ||
| Outpatient/ambulatory care | 30.50 (13.44) | ||
| Are you involved in COVID-19 clinical care? | −3.94 | <0.01 | |
| Yes | 34.50 (3.47) | ||
| No | 29.81 (13.00) | ||
| What is your religious/spiritual preference? | |||
| Religious/spiritual | 32.31 (13.42) | 2.20 | 0.03 |
| Not religious/spiritual | 35.95 (13.51) | ||
One-way ANOVA, post hoc analysis with the Bonferroni corrections shows significant difference between 0 and 10 years of experience and 10–20 years of experience and 20+ years of experience (p = 0.037 and p ≤ 0.01, respectively), and 10–20 years experience and 20+ years experience (p = 0.044).
Only one respondent in this specialty.
Religious/spiritual preference was dichotomized as 0 = not religious/spiritual preference and 1 = spiritual/religious.
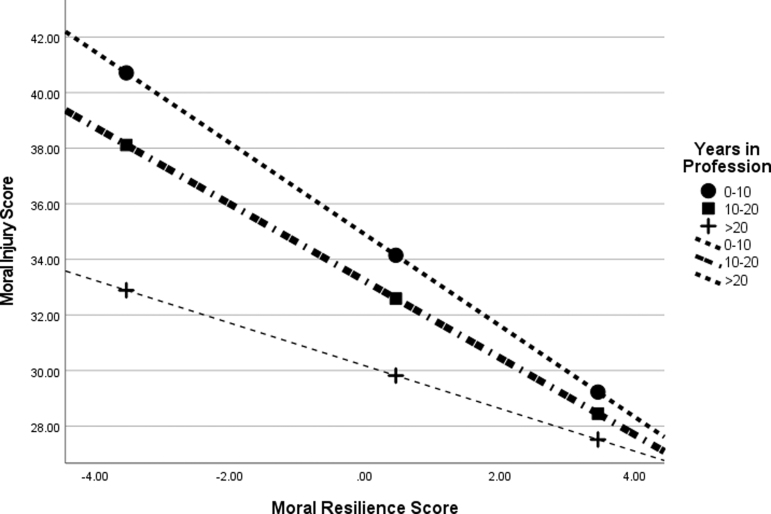
In the final model, MR was added as a moderator of the relationship between number of years in the profession and MI. The final model explained 30% of the variability in MI score [F(8, 520) = 27.43, p = 0.0001, R2 = 0.30] (Table 4). All variables added statistical significance to the prediction (p < 0.05). Specifically, having a spiritual or religious belief system versus not and experiencing fewer ethical concerns were associated with lower MI. Respondents who indicated that they had a religious affiliation, or were spiritual but not religious, had lower MI scores. MR buffered the negative relationship between years of experience and MI. Higher levels of MR decreased the tendency of less experienced HWCs to suffer and report higher levels of MI symptoms, as shown in Figure 1.
Table 4.
Final Regression Model (n = 529)
| Factor | Adjusted b (95% CI)a | Standard Error | t | p b |
|---|---|---|---|---|
| Religion/spirituality | −3.41 (−6.27 to −0.54) | 1.46 | −2.33 | 0.02 |
| Moral resilience score | −1.64 (−2.12 to −1.17) | 0.17 | −6.77 | <0.01 |
| 10–20 Years in profession | −1.68 (−4.33 to 0.98) | 1.35 | −1.24 | 0.22 |
| >20 Years in profession | −4.73 (−7.11 to −2.35) | 1.21 | −3.90 | <0.01 |
| ECI score | 0.14 (0.07 to 0.23) | 0.04 | 3.51 | <0.01 |
| 10–20 Years in profession × Resilience | 0.26 (−0.52 to 1.04) | 0.40 | 0.65 | 0.51 |
| >20 Years in profession × Resilience | 0.87 (0.20 to 1.55) | 0.34 | 2.55 | 0.01 |
| COVID-19 care | 1.61 (−0.54 to 3.8) | 1.1 | 1.50 | 0.14 |
Religious/spiritual was coded 0 = not religious/spiritual and 1 = religious/spiritual.
Adjusted regression coefficients.
Multiple linear regression (R2 = 0.26).
FIG. 1.
Moral resilience moderates the relationship between number of years in profession and moral injury.
Discussion
Clinicians and other HCWs caring for patients with COVID-19 reported experiencing more MI in our initial analyses than those not providing COVID-19-related care. However, this relationship was eclipsed by MR, indicating that it is not simply providing COVID-19 care that leads to MI but also the HCWs level of MI when faced with these challenges. Rapid decline of patients with moderate and/or severe COVID-19 infections has placed urgency on palliative care clinicians to step into complex situations and swiftly discern patient and family goals of care, potentially placing them at higher risk for experiencing symptoms of distress and MI.25 Given the myriad ethical challenges and policy changes that all HCWs have faced throughout the pandemic, the finding that COVID-19 care, and more importantly, the ethical concerns that come with it are associated with MI provides evidence to support what others have theorized.26
The MISS-HP22 adapted the original MI scale designed for veterans27,28 and validated it for use among health care clinicians.22 The MISS-HP measures the psychological and religious dimensions of MI that primarily reflect the individual responsibility aspect of MI; it measures symptoms rather than events.22 The prevalence of clinically significant MI (≥36) in this sample (32.4%) is greater than previously reported in a U.S. sample (7.8%),22 a Chinese sample (20.4%),29 and a global sample of health care professionals where 23.9% reported MI symptoms associated with moderate functional impairment.30 Explanation for this increase in prevalence is likely multifactorial. Understanding these trends is vital in identifying clinicians at risk of significant MI symptoms to proactively intervene to reduce the likelihood of consequences such as medical errors,30 burnout,30 suicidal ideation,22 and other negative outcomes. Recent studies have proposed that MI is distinct from burnout and will require targeted interventions to address the unique factors that contribute to it.30
Our findings expand upon the understanding of MI in the health care workforce. Our sample was composed of a wider range of HCWs (nurses, physicians, social workers, chaplains, technicians, etc.) from five different hospitals, whereas their sample was drawn from one hospital and was physician-centric in nature.22 Zhizhong et al. tested the MISS-HP among Chinese physicians and nurses.29 Although given the contrasts across health care systems globally, it is difficult to draw any comparisons as our study sample is focused on the mid-Atlantic region of the United States. Hines et al. conducted a similar study but assessed MI among HCWs (primarily physicians) using the Moral Injury Events Scale (MIES),21 which has previously been used in military service personnel but not validated in HCWs.31 Their results showed that MI scores remained consistent and overall distress decreased longitudinally.21 In contrast, MI scores using the MISS-HP demonstrated significant increases during the pandemic.30 General acknowledgement of MI is increasing; however, further work is needed to comprehensively understand the range of moral injurious events and symptoms HCWs are experiencing and the impact of them on their health, well-being, work environment, and patient care.
In our sample, the results demonstrate that MR and MI are negatively correlated. These findings suggest that MR may be important in addressing the personal responsibility aspect of MI while system reforms are implemented.12,13 How clinicians appraise and respond to challenges, threats, or violations of their values, beliefs, or integrity may be amenable to intervention.32 Cultivating capacities associated with MR may offer HCWs individual resources to help mitigate the impact of ethical challenges faced in their work.13,17 Proactive programs such as the Mindful Ethical Practice and Resilience Academy (MEPRA) for nurses have been shown to cultivate mindfulness, ethical competence and confidence, resilience, and work engagement.33 Such programs are designed to harness clinicians' foundational resilience and amplify skills, tools, and resources they need to meet the ethical challenges inevitable in clinical practice without extensive cost to personal well-being or integrity. These approaches can support HCWs who are experiencing MI to heal their moral wounds and restore moral wholeness and agency while large-scale reforms within health care systems are undertaken. Although harnessing MR capacities can help mitigate detrimental MI symptoms in response to potentially morally injurious events, targeted interventions to address the systemic root causes of these events is critically important.34 Preserving or restoring integrity in HCWs not only serves their well-being but also promotes conditions where they are able to partner with leaders and other key stakeholders to design solutions to these systemic obstacles. Without the engagement of frontline clinicians, the solutions designed to address the systemic contributors to MI may fall short in effectiveness and sustainability.13
The ECI factors that most highly correlated with increased MI symptoms reflect select system contributions during the pandemic. Working with limited resources such as personal protective equipment (PPE) was clinical realities that were intensified at the beginning of the pandemic and persisted for some HWCs throughout the pandemic35 Losing the ability to advocate for an individual patient was likely associated with significant resource constraints (particularly in high COVID-19 prevalence areas) and the shift to a population-focused allocation strategy.36 Severe visitor restrictions changed the usual decision-making process and may have contributed to the MI symptoms associated with making decisions to limit or forgo interventions without family's usual level of involvement.37 Experiencing negative consequences at work if safety concerns were voiced reflects a potentially morally injurious event when HCWs may feel betrayed by their organization to create a “just culture” where speaking up is expected and valued but instead is penalized.15,35,37,38 Taken together, the ECIs point to the sources of potentially injurious events that arise from the organizational aspect of MI during a pandemic. Further research is needed to understand more fully (1) the contributions of ethical concerns factors to MI symptoms, (2) what organizational resources are valued and highly utilized by clinicians, and (3) the relationship of these factors with development of MI and cultivation of MR.
Tenure in the profession was identified as a protective factor for developing MI. Fewer years of experience in the profession was related to higher levels of MI. These findings are consistent with other studies that have reported clinicians with more years of experience have lower levels of MI.30 The negative relationship between time in position and MI is buffered by MR. MR is more important in reducing MI for those with less experience than it is for those with more experience who already experience less MI (Fig. 1). Clinicians with less experience in this sample (75.4% <10 years) reported providing care of patients with COVID-19. Alongside their patient-facing duties, HCWs may have taken on additional responsibilities for adapting system processes, training other clinicians to care for critically ill and/or dying patients with COVID-19, allocating scarce resources, and implementing changes in standards of care.35,38,39 Given the fragility of the health care workforce, these findings point to an urgent need to invest in individual and organizational resources to bolster clinicians' MR and personal well-being, particularly those with less experience.4,19,34
Spiritual or existential conflict has been theoretically recognized as a core symptom in MI.40 Our findings corroborate this theoretically recognized symptom with data showing those reporting spirituality or religious affiliation had lower MI scores than those without and higher MR scores. Our findings are consistent with another MI study reporting an inverse relationship between MI scores and religiosity and the potential protective effect on HCWs.30 Morally injurious events have the potential to erode one's sense of purpose and meaning in one's work9 and may be related to spiritual or existential conflict. Although MI is not considered a mental illness, additional expertise in processing complex ethical issues that are foundational to such events is vital to helping HCWs heal from moral wounds. Collaboration with ethics consultants to facilitate dialogue with clinicians experiencing moral injurious events by clinicians is important to avoid a one-size-fits-all approach to HCW distress.41 HCWs, particularly those specializing in palliative care, may want to intensify practices that create opportunities to explicitly connect to why they have chosen their path of service and why it matters to their life and work.15,42 Explicitly cultivating spaces and processes within the health care environment, where spiritual and faith-based resources can be easily accessed rather than hidden, may help foster ethical work environments.43–45
Limitations
The results of the study represent a convenience sample of HCWs with similar geographic and organizational environments within the Johns Hopkins Clinical Research Network and may not be representative or generalizable. Future research could expand the study design by powering the study to represent all HCWs in the mid-Atlantic region and comparing specific religious/spiritual belief systems to understand individual differences and the impact of geography. As an exploratory survey, the end-denominator of survey participants is unknown; power and sample size calculations cannot be calculated or reported. The COVID-19 pandemic-specific survey includes multiple items from validated and unvalidated non-pandemic-specific survey instruments. Further factor analysis and correlation studies are required to establish reliability and validation of the survey.
Conclusions
The validated MI symptom scale (MISS-HP) offers valuable insights into sources of MI among HCWs during a global pandemic. Although there is limited pre-pandemic MI data collected in HCWs,22 the prevalence of symptoms of MI in this sample is likely associated with the COVID-19 pandemic.30 The higher levels of MI particularly among nurses warrants greater scrutiny to understand the factors that intensify their MI symptoms. HCWs, particularly those with less work experience, are experiencing significantly greater MI. Future investigations should prioritize this population to determine which factors are amenable to intervention. Further work is needed to comprehensively understand additional sources of MI among different professions and work settings and to distinguish MI from other concepts such as burnout or post-traumatic stress disorder.30 Use of the validated moral resilience scale (RMRS) can guide the development of MR to moderate the detrimental consequences of MI13,18 particularly HCWs with less work experience. Further research is needed to understand the relationships between MI, spirituality and religious affiliation, and MR.
Future studies should evaluate the impact of individual and systemic interventions aimed at redressing the impact of morally injurious events and symptoms on clinicians and HCWs by amplifying their MR.15 Developing specific interventions aimed at the root causes of MI and expanding the repertoire of MR skills and resources that clinicians can draw upon during the COVID-19 pandemic and beyond is essential. Palliative care clinicians are uniquely poised to address key aspects of the practice environment that impact the sources of MI, particularly aspects of end-of-life care.46
Acknowledgments
We acknowledge and honor the incredible service that clinicians have provided during the pandemic and their willingness to participate in this study.
Disclaimer
The contents are solely the responsibility of the authors and do not necessarily represent the official view of the Johns Hopkins Institute for Clinical and Translational Research (ICTR), Johns Hopkins Clinical Research Network (JHCRN), National Center for Advancing Translational Sciences (NCATS), or National Institutes of Health (NIH).
Authors' Contributions
T.A.T. conceptualized the overall study. T.A.T. and C.H.R. developed the study design. I.M.A., D.S., C.D.L., and A.V. were responsible for data collection. G.C.H. was responsible for overall data analysis design. C.H.R. and D.B. assisted with data analysis. C.H.R., I.M.A., K.E.N., and G.C.H. were responsible for writing and editing the article. D.S., C.D.L., and A.V. were responsible for reviewing and editing of the article.
Funding Information
This publication was made possible by the Johns Hopkins ICTR, which is funded in part by grant number UL1 TR003098 from the NCATS, a component of the NIH, and NIH Roadmap for Medical Research, and the JHCRN.
Author Disclosure Statement
No competing financial interests exist.
References
- 1. Robert R, Kentish-Barnes N, Boyer A, et al. : Ethical dilemmas due to the Covid-19 pandemic. Ann Intensive Care 2020;10:84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Azoulay E, De Waele J, Ferrer R, et al. : Symptoms of burnout in intensive care unit specialists facing the COVID-19 outbreak. Ann Intensive Care 2020;10:1–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Robillard R, Saad M, Edwards J, et al. : Social, financial and psychological stress during an emerging pandemic: Observations from a population survey in the acute phase of COVID-19. BMJ Open 2020;10:e043805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Dijxhoorn AQ, Brom L, van der Linden YM, et al. : Prevalence of burnout in healthcare professionals providing palliative care and the effect of interventions to reduce symptoms: A systematic literature review. J Palliat Med 2021;35:6–26. [DOI] [PubMed] [Google Scholar]
- 5. Dyrbye LN, Shanafelt TD, Sinsky CA, et al. : Burnout Among Health Care Professionals: A Call to Explore and Address this Underrecognized Threat to Safe, High-Quality Care. Washington, DC: National Academy of Medicine, NAM Perspectives; 2017. Discussion paper. [Google Scholar]
- 6. McHugh MD, Kutney-Lee A, Cimiotti JP, et al. : Nurses' widespread job dissatisfaction, burnout, and frustration with health benefits signal problems for patient care. Health Aff 2011;30:202–210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Moss M, Good VS, Gozal D, et al. : An official critical care societies collaborative statement: Burnout syndrome in critical care health care professionals: A call for action. Crit Care Med 2016;25:368–376. [DOI] [PubMed] [Google Scholar]
- 8. Dean W, Talbot S, Dean A: Reframing clinician distress: Moral injury not burnout. Fed Pract 2019;36:400–402. [PMC free article] [PubMed] [Google Scholar]
- 9. Litz BT, Stein N, Delaney E, et al. : Moral injury and moral repair in war veterans: a preliminary model and intervention strategy. Clin Psychol Rev 2009;29:695–706. [DOI] [PubMed] [Google Scholar]
- 10. Griffin BJ, Purcell N, Burkman K, et al. : Moral injury: An integrative review. J Trauma Stress 2019;32:350–362. [DOI] [PubMed] [Google Scholar]
- 11. Shay J: Moral injury. Psychoanal Psychol 2014;31:182–191. [Google Scholar]
- 12. Barnes HA, Hurley RA, Taber KH: Moral injury and PTSD: Often co-occurring yet mechanistically different. J Neuropsychiatry Clin Neurosci 2019;31:A4–A103. [DOI] [PubMed] [Google Scholar]
- 13. Rushton CH: Moral Resilience: Transforming Moral Suffering in Healthcare. New York, NY: Oxford University Press, 2018. [Google Scholar]
- 14. Dean W, Jacobs B, Manfredi RA: Moral injury: the invisible epidemic in COVID health care workers. Ann Emerg Med 2020;76:385–386. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Rushton C, Turner K, Brock R, et al. : The invisible moral wounds of the pandemic: Are we experiencing moral injury? AACN Adv Crit Care 2021;32:119–125. [DOI] [PubMed] [Google Scholar]
- 16. Rushton CH: Moral resilience: A capacity for navigating moral distress in critical care. AACN Adv Crit Care 2016;27:11–119, p. 112. [DOI] [PubMed] [Google Scholar]
- 17. Holtz H, Heinze K, Rushton C: Interprofessionals' definitions of moral resilience. J Clin Nurs 2018;27:3–4. [DOI] [PubMed] [Google Scholar]
- 18. Heinze KE, Hanson G, Holtz H, et al. : Measuring healthcare interprofessionals' moral resilience: Validation of the Rushton Moral Resilience Scale. J Palliat Med 2021;24:865–872. [DOI] [PubMed] [Google Scholar]
- 19. Rosa WE, Schlak A, Rushton CH: A blueprint for leadership during COVID-19. Nurs Manage 2020;51:28–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Hines SE, Chin KH, Levine AR, Wickwire EM: Initiation of a survey of healthcare worker distress and moral injury at the onset of the COVID-19 surge. Am J Ind Med 2020;63:830–833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Hines SE, Chin KH, Glick DR, Wickwire EM: Trends in moral injury, distress, and resilience factors among healthcare workers at the beginning of the COVID-19 pandemic. Int J Environ Res Public Health 2021;18:488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mantri S, Lawson JM, Wang Z, Koenig HG: Identifying moral injury in healthcare professionals: The moral injury symptom scale-hp. J Relig Health 2020;59:2323–2340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Hayes AF, Little TD: Introduction to Mediation, Moderation, and Conditional Process Analysis: A Regression-Based Approach, 2nd edition. New York, New York: The Guilford Press, 2018. [Google Scholar]
- 24. Cohen J: A power primer. Psychol. Bull. 1992;112:155. [DOI] [PubMed] [Google Scholar]
- 25. Wallace CL, Wladkowski SP, Gibson A, et al. : Grief during the COVID-19 pandemic: Considerations for palliative care providers. J Pain Symptom Manag 2020;60:e70–e76. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Greenberg N, Docherty M, Gnanapragasam S, Wessely S: Managing mental health challenges faced by healthcare workers during covid-19 pandemic. BMJ 2020;368:m1211. [DOI] [PubMed] [Google Scholar]
- 27. Koenig HG, Ames D, Youssef NA, et al. : The moral injury symptom scale-military version. J Relig Health 2018;57:249–265. [DOI] [PubMed] [Google Scholar]
- 28. Koenig HG, Ames D, Youssef NA, et al. : Screening for moral injury: the moral injury symptom scale—Military version short form. Mil Med 2018;183:e659–e665. [DOI] [PubMed] [Google Scholar]
- 29. Zhizhong W, Koenig HG, Yan T, et al. : Psychometric properties of the moral injury symptom scale among Chinese health professionals during the COVID-19 pandemic. BMC Psychiatry 2020;20:556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Mantri S, Song YK, Lawson JM, et al. : Moral injury and burnout in health care professionals during the COVID-19 pandemic. J Nerv Mental Dis 20211;209:720–726. [DOI] [PubMed] [Google Scholar]
- 31. Nash WP, Marino Carper TL, Mills MA, et al. : Psychometric evaluation of the moral injury events scale. Mil Med 2013;178:646–652. [DOI] [PubMed] [Google Scholar]
- 32. Thomas TA, McCullough LB: A philosophical taxonomy of ethically significant moral distress. J Med Philos 2015;40:102–120. [DOI] [PubMed] [Google Scholar]
- 33. Rushton CH, Swoboda SM, Reller N, et al. : Mindful ethical practice and resilience academy: Equipping nurses to address ethical challenges. Am J Crit Care 2021;30:e1–e11. [DOI] [PubMed] [Google Scholar]
- 34. National Academies of Sciences, Engineering, and Medicine (NAM): Taking Action against Clinician Burnout: A Systems Approach to Professional Well-Being. Washington DC: National Academies Press, 2019. [PubMed] [Google Scholar]
- 35. Ulrich C, Rushton C, Grady C: Nurses confronting the Coronavirus: Challenges met and lessons learned to date. Nursing Outlook 202;68:838–844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Benishek LE, Kachalia A, Daugherty Biddison L, Wu AW: Mitigating health-care worker distress from scarce medical resource allocation during a public health crisis. Chest 2020;158:2285–2287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Morley G, Grady C, McCarthy J, Ulrich CM: Covid-19: Ethical challenges for nurses. Hastings Cent Rep 2020;50:35–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Garros D. Austin W, Dodek P: How can I survive this? Coping during COVID-19 pandemic. Chest 2021;159:1484–1492. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. Wu KJ: Covid combat fatigue: “I would come home with tears in my eyes.” NY Times. https://www.nytimes.com/2020/11/25/health/doctors-nurses-covid-stress.html. 2020. (Last accessed October 17, 2021).
- 40. Jinkerson JD: Defining and assessing moral injury: A syndrome perspective. Traumatology 2016;22:122. [Google Scholar]
- 41. Koenig HG, Al-Zaben F, VanderWeele TJ: Religion and psychiatry: Recent developments in research. BJ Psych Adv 2020;26:262–272. [Google Scholar]
- 42. Rego F, Rego G, Nunes R: Moral agency and spirituality in palliative care. Ann Palliat Med 2020;9:2286–2293. [DOI] [PubMed] [Google Scholar]
- 43. Carey LB, Hodgson TJ, Krikheli L, et al. : Moral injury, spiritual care and the role of chaplains: An exploratory scoping review of literature and resources. J Relig Health 2016;55:1218–1245. [DOI] [PubMed] [Google Scholar]
- 44. Kopacz MS, Ducharme C, Ani D, Atlig A: Towards a faith-based understanding of moral injury. J Pastoral Care Counsel 2017;71:217–219. [DOI] [PubMed] [Google Scholar]
- 45. Hodgson TJ, Carey LB: Moral injury and definitional clarity: Betrayal, spirituality and the role of chaplains. J Relig Health 2017;56:1212–1228. [DOI] [PubMed] [Google Scholar]
- 46. Bosshardt MH, Coyne PJ, Marsden J, et al. : Palliative care consultation policy change and its effect on nurses' moral distress in an academic medical center. J Hosp Palliat Nurs 2018;20:325–329. [DOI] [PubMed] [Google Scholar]