Abstract
Objective
To compare four different types of monolithic zirconia crowns in terms of survival rate and fracture resistance after thermocycling and/or thermo-mechanical loading in a chewing simulator.
Methods
Partially-Stabilized-Zirconia (PSZ) crowns with fiber-reinforced resin die assemblies (n = 80) were fabricated using: multi-yttria-layered 5Y-PSZ/3Y-PSZ, multi-yttria-layered 5Y-PSZ/4Y-PSZ, monolithic 4Y-PSZ and monolithic 3Y-PSZ as control (n = 20). Half of the samples in each group were subjected to thermo-mechanical loading under 110 N, 1.4 Hz, 1.2 million cycles with simultaneous thermocycling (10,000 cycles, 5–55°C). The other half were subjected to thermocycling alone. The samples were loaded to failure to measure their fracture resistance. The data were analyzed using by two-way ANOVA and Tukey’s HSD post-hoc test (α = 0.05).
Results
All specimens survived the aging protocols. The yttria content significantly affected the fracture resistance of the crowns (p < 0.0001). The mean fracture resistance, from highest to lowest: 3Y-PSZ, 4Y-PSZ, followed by the two multi-yttria-layered systems. The mean difference between the two multi-yttria-layered systems were not statistically significant (p=0.98). The mechanical loading protocol did not affect the mean fracture resistance within each group (p = 0.18).
Conclusions
Within each group, there was no difference in fracture resistance after thermocycling alone and thermo-mechanical loading. However, increasing the yttria concentration at the occlusal third of the crown decreased its fracture resistance.
Keywords: Monolithic zirconia, multi-yttria-layered zirconia, gradient zirconia, zirconia crowns, fracture load, yttria concentration, fatigue, mastication simulation, Monolithic zirconia, multilayered zirconia, gradient zirconia, zirconia crowns, fracture load, yttria concentration, fatiguing, mastication simulation
INTRODUCTION
In the last two decades, partially stabilized zirconia (PSZ)-based dental restorations have grown in popularity. This can be attributed to their lower coast and less time-consuming production process when compared to porcelain fused to metal restorations. Another factor contributing to the emergence and use of these restorations is the widespread use of CAD/CAM technology in dentistry. It is important to keep in mind that “Monolithic Zirconia” is a broad term that can refer to generations of zirconia restorations with different mechanical and optical properties, and thus varying clinical performance. The multi-yttria-layered (MYL) or gradient zirconia system is the most recent generation. This system, as the name implies, provides dental restoration that follow the gradient translucency of a natural tooth structure while maintaining high strength at the gingival third. It is composed of two types of zirconia combined in a single restoration, with an intermediate zone that follows gradual transition between the two.1, 2
It is imperative to investigate emerging dental materials by well-designed studies prior to its clinical use. While the ultimate evidence to support the usage of such materials might be randomized clinical trials, such trials are expensive, complex, and lengthy. An article stated that it takes about 10 years to conduct and publish a 5-year follow-up clinical trial. By that time, the material tested might be outdated or discontinued.3 One way to overcome the drawbacks of conducting randomized clinical trials would be testing the materials in vitro by means of artificial aging to predict its clinical behavior prior to intraoral use.
The first aim of this study is to evaluate the effect of aging method; thermocycling alone and combined thermo-mechanical loading on the fracture resistance of single unit zirconia crowns. The second aim is to evaluate the fracture resistance of four different types of single unit zirconia crowns based on their yttria concentration: 3Y-PSZ, 4Y-PSZ, MYL 5Y-PSZ/3Y-PSZ, and MYL 5Y-PSZ/4Y-PSZ. The null hypotheses are (a) there is no difference in the fracture resistance of zirconia crowns after aging by means of thermocycling alone and combined thermo-mechanical loading, and (b) there is no difference in the fracture resistance between 3Y-PSZ, 4Y-PSZ, MYL 5Y-PSZ/3Y-PSZ, and MYL 5Y-PSZ/4Y-PSZ crowns.
MATERIALS AND METHODS
A plastic Ivorine mandibular left first molar was prepared for a full coverage ceramic crown restoration. The preparation was carried out using a high-speed electric hand-piece rotating at 200,000 rpm with water-cooling and diamond modified flat-end taper burs (Brassler, Savannah, GA, USA). The preparation insured an axial reduction of 1 to 1.5 mm, a marginal rounded shoulder of 1 mm, an occlusal reduction of 1.5 mm and a taper of 10 degrees (Figure 1). This master die was scanned using a TRIOS 3 scanner (3Shape, Copenhagen, Denmark) and sent to a commercial lab. Eighty fiber reinforced resin dies (Trilor, Bioloren Srl, VA, Italy) were milled to replicate the exact preparation of the master die. Eighty full-coverage crowns were designed to fit the master die previously scanned using 3Shape Design Studio software (3Shape, Copenhagen, Denmark). The design of the crowns followed the aforementioned dimensions. The design parameters were set to 20 μm space at the margins and an internal cement space of 60 μm following the instructions of the milling unit. The crowns were milled using four different zirconia materials in a PrograMill PM7 milling machine (Ivoclar Vivadent: Schaan, Liechtenstein), twenty crowns in each group as following:
Figure 1a.

Die preparation proximal view.
Group 1 (Control) – monolithic, 3Y-PSZ (ZirCAD LT, Ivoclar Vivadent: Schaan, Liechtenstein).
Group 2 – monolithic, 4Y-PSZ (ZirCAD MT, Ivoclar Vivadent: Schaan, Liechtenstein).
Group 3 – MYL 5Y-PSZ/3Y-PSZ (ZirCAD Prime, Ivoclar Vivadent: Schaan, Liechtenstein).
Group 4 – MYL 5Y-PSZ/4Y-PSZ (ZirCAD MT Multi, Ivoclar Vivadent: Schaan, Liechtenstein).
The milling of the two MYL zirconia groups (group 3 and group 4) insured 3 mm of 5Y-PSZ occlusally.
The crowns were sintered using program 1 (IPS e.max ZirCAD standard program) in a sintering furnace (Programat S1 1600, Ivoclar Vivadent: Schaan, Liechtenstein). The crowns were polished using a two-stage polishing kit (Luster Zirconia Polishing Kit, Meisinger, USA). No stains nor glaze added. Figure 2 shows the different types of zirconia crowns after milling, sintering, and polishing.
Figure 2.

Finished monolithic zirconia crowns, from left to right, 3Y-PSZ, 4Y-PSZ, MYL 5Y-PSZ/3Y-PSZ and MYL 5Y-PSZ/4Y-PSZ. Notice the difference in optical properties between the MYL and the single-layered groups.
The fit of each crown was checked under 3.5× magnification using a sharp dental explorer number 5 (Hu-Friedy, Chicago, IL, USA). The crowns were adhesively bonded to their corresponding dies using the (A) air-particle abrasion, (P) zirconia primer, and (C) adhesive composite resin concept.4 The intaglio surface of each crown was air-particle abraded using 50-μm aluminum oxide (Danville Materials, San Ramon, CA, USA), under 2 Bar pressure for 15 seconds at a distance of 10 mm using a basic classic fine sandblaster (Renfert USA, St. Charles, IL, USA). Monobond Plus (Ivoclar Vivadent: Schaan, Liechtenstein) was applied to the fitting surface followed by Multilink Primer (Ivoclar Vivadent: Schaan, Liechtenstein). Then the crowns were bonded to the dies using a self-curing resin cement (Multilink Automix, Ivoclar Vivadent: Schaan, Liechtenstein).
The crowns in each group were further divided into two subgroups (n = 10 each). In subgroup A, the crowns were artificially aged using simultaneous thermo-mechanical loading. The loading force was set at 110 N at a frequency of 1.4 Hz for 1.2 million cycles with simultaneous thermocycling (10,000 cycles, 5–55°C) in a computer controlled multifunctional mastication simulator (SD Mechatronik, Fedkirchen- Westerham, Germany). Those parameters were reported to equal 5 years of clinical service.5 Test specimens were oriented parallel to the long axis of the tooth and embedded in auto-polymerizing acrylic resin (VariDur 200, Buehler, Lake Bluff, IL, USA) 1 mm below the crown margin in the cylinder specimen holders of the chewing simulator. A 4 mm diameter stainless steel ball was used as an antagonist at a 1 mm vertical start point. The initial contact was at the central fossa followed by a 1 mm horizontal shift towards the buccal groove (Figure 3). Wear detectors were used to monitor the samples thus, to record the number of cycles needed until failure. After 1.2 million cycles, all surviving specimens were examined under 3.5× magnification for visible damage in the crown or the die following fatigue testing. Failure was defined as crown or die complete or partial fracture, visible cracking or debonding. In subgroup B, the crowns were aged by means of thermocycling only (10,000 cycles, 5–55°C) in a computer controlled multifunctional mastication simulator (SD Mechatronik, Fedkirchen- Westerham, Germany).
Figure 3.
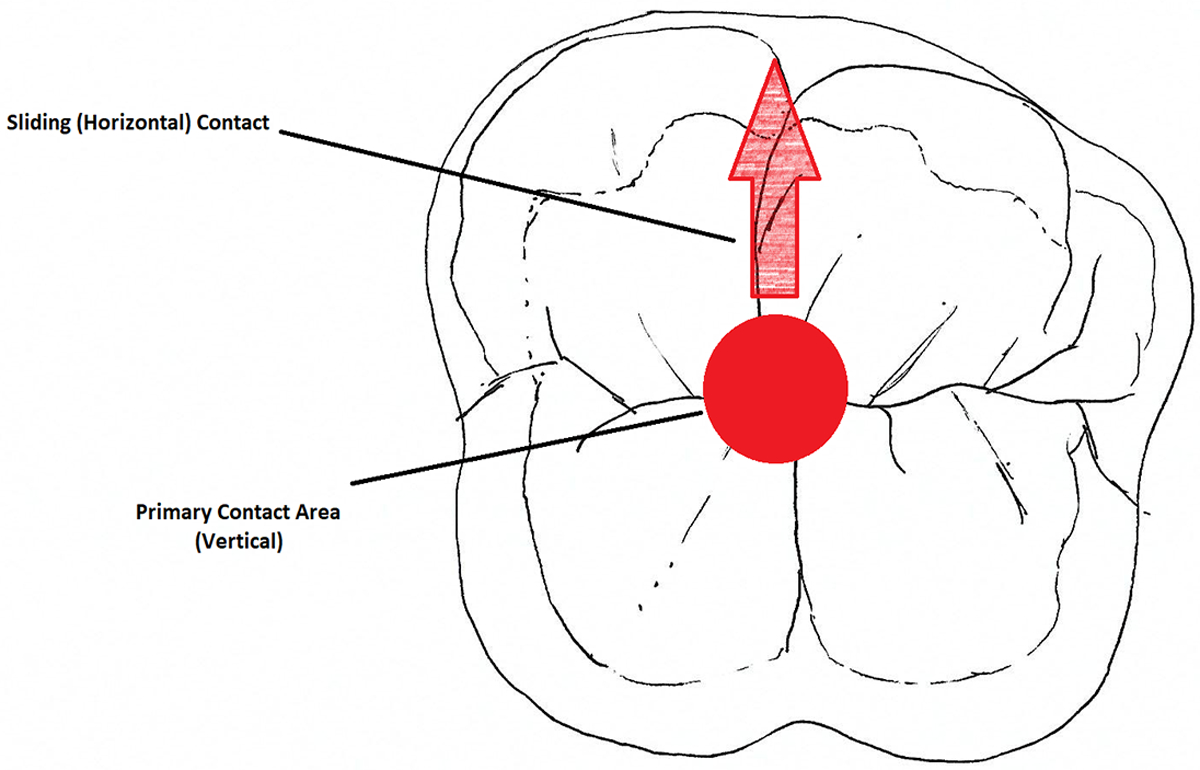
Vertical and lateral contact motion during chewing simulation.
Random samples from each group were selected for further analysis under up to 700 times magnification under scanning electron microscope, SEM (FEI Quanta 600 FEG Mark II Environmental Scanning Electron Microscope, Hillsboro, OR, USA). The SEM analysis looked into microcracks at both the axial and sliding contacts.
After aging, the fracture resistance of each sample was carried out by loading the crowns directly at the central fossa using a 4 mm diameter stainless steel cone antagonist at a speed of 1 mm/min until fracture occurred using a universal testing machine (Instron, Norwood, MA, USA). During loading, the antagonist was contacting the crown in 3 points at the triangular ridges of the cusps at the fossa. After loading the samples to failure, the fractured pieces were collected for further fractographic analysis. An optical microscope (Zeiss Stereo Discovery V. 20 Microscope, Carl Zeiss, LLC, USA) under 7.5- and 11.5-times magnification was used to detect the origin of fracture.
Two-way Analysis of Variance (ANOVA) and Tukey’s Studentized Range test were used to assess the effect of aging method and zirconia yttria content on the fracture resistance of crowns. The level of significance was set at α = 0.05.
RESULTS
All specimens, regardless of the type of zirconia used, survived the 1.2 million cycles and thermocycling. There were no visible cracks or fractures seen on the dies nor the crowns. The mean difference in fracture resistance was not statistically significant after thermocycling alone compared to thermo-mechanical loading within each type of zirconia p = 0.18. However, a significant variation in fracture resistance means among zirconia groups based on yttria concentration was seen p < 0.0001 (Table 1).
Table 1.
Two-way analysis of variance summary analyzing the effect of aging method and yttria content on the fracture resistance of the zirconia crowns.
| Source | SS | DF | MS | F | P |
|---|---|---|---|---|---|
| Aging Method | 301461.72 | 1 | 301461.74 | 1.81 | 0.1827 |
| Yttria Content | 21070226.19 | 3 | 7023408.7 | 42.15 | <.0001* |
| Interaction | 82448.21 | 3 | 27482.74 | 0.16 | 0.9229 |
| Error | 11998099.94 | 72 | 166640.28 | ||
| Total | 33452236.08 | 79 |
indicates statistical significance (p<0.05)
The mean values of fracture load for each group are listed in Table 2. A statistically significant difference was found in the means of fracture resistance between group 1 (3Y-PSZ) and group 2 (4Y-PSZ) p=0.019, group 1 (3Y-PSZ) and group 3 (5Y-PSZ/3Y-PSZ) p<0.0001, group 1 (3Y-PSZ) and group 4 (5Y-PSZ/4Y-PSZ) p<0.0001, group 2 (4Y-PSZ) and group 3 (5Y-PSZ/3Y-PSZ) p=0.001, group 2 (4Y-PSZ) and group 4 (5Y-PSZ/4Y-PSZ) p<0.0001. The difference in means of fracture resistance between groups 3 (5Y-PSZ/3Y-PSZ) and 4 (5Y-PSZ/4Y-PSZ) p=0.98 was not statistically significant. Figure 4 shows the relation between the types of zirconia used and fracture resistance of the crowns.
Table 2.
Mean and standard deviation of fracture load in newtons of zirconia crowns as a function of yttria content after two aging methods.
| Zirconia Content | Aging Method | |
|---|---|---|
| Thermocycling Only | Thermo-Mechanical Loading | |
| 3Y-PSZ | 3728.6±463.1 A,a | 3708.4±479.9 A,a |
| 4Y-PSZ | 3309.9±397.0 B,b | 3172.9±427.6 B,b |
| 5Y-PSZ/3Y-PSZ | 2597.8±333.5 C,c | 2461.3±332.1 C,c |
| 5Y-PSZ/4Y-PSZ | 2591.1±503.4 C,c | 2393.6±270.0 C,c |
- Capitol letter superscript indicates statistical significance in fracture resistance as a function of yttria content (p<0.05).
- Lower case letter superscript indicates statistical significance in fracture as a function of aging method (p<0.05).
Figure 4.
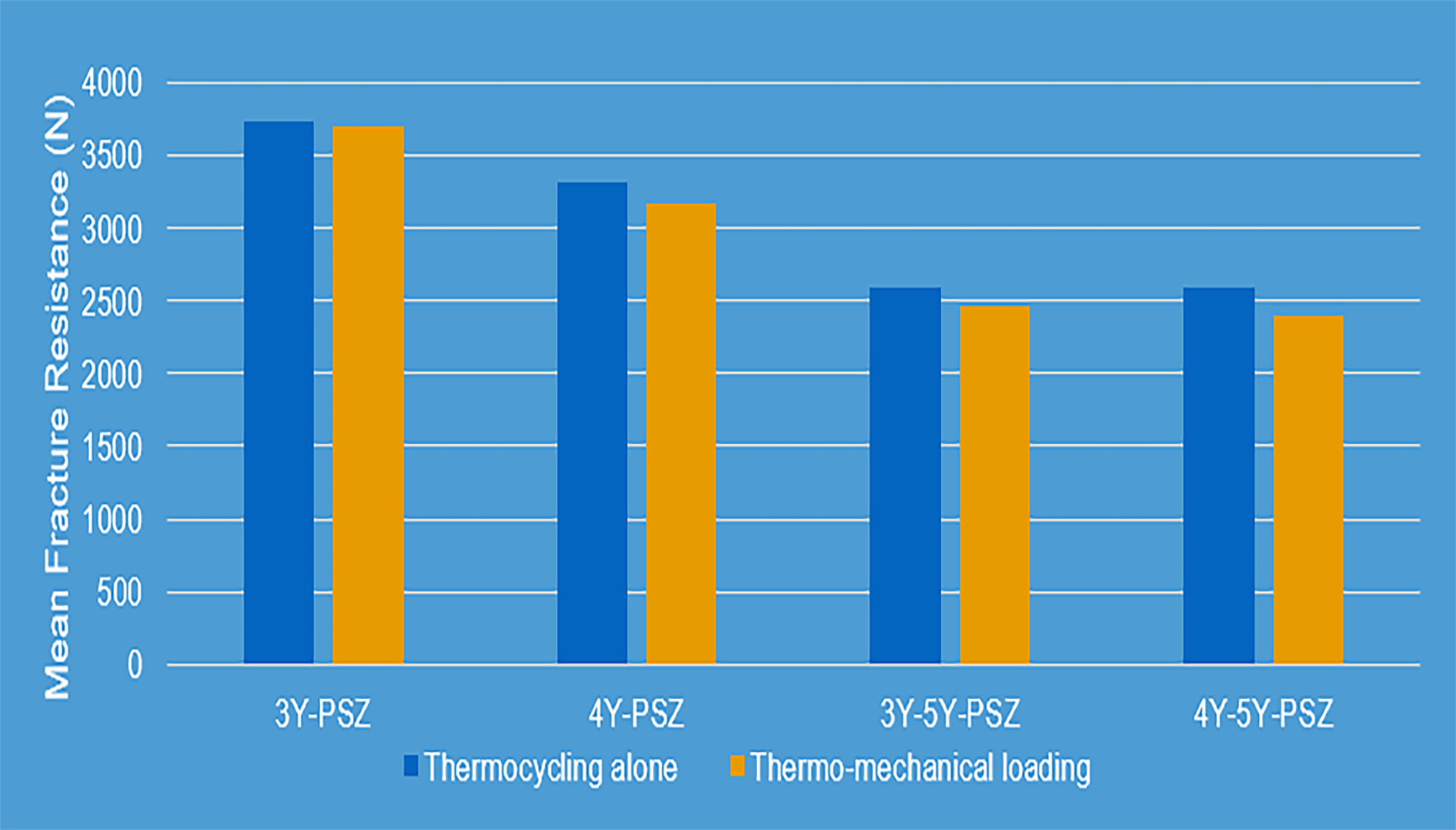
Fracture resistance of different types of zirconia crowns after aging.
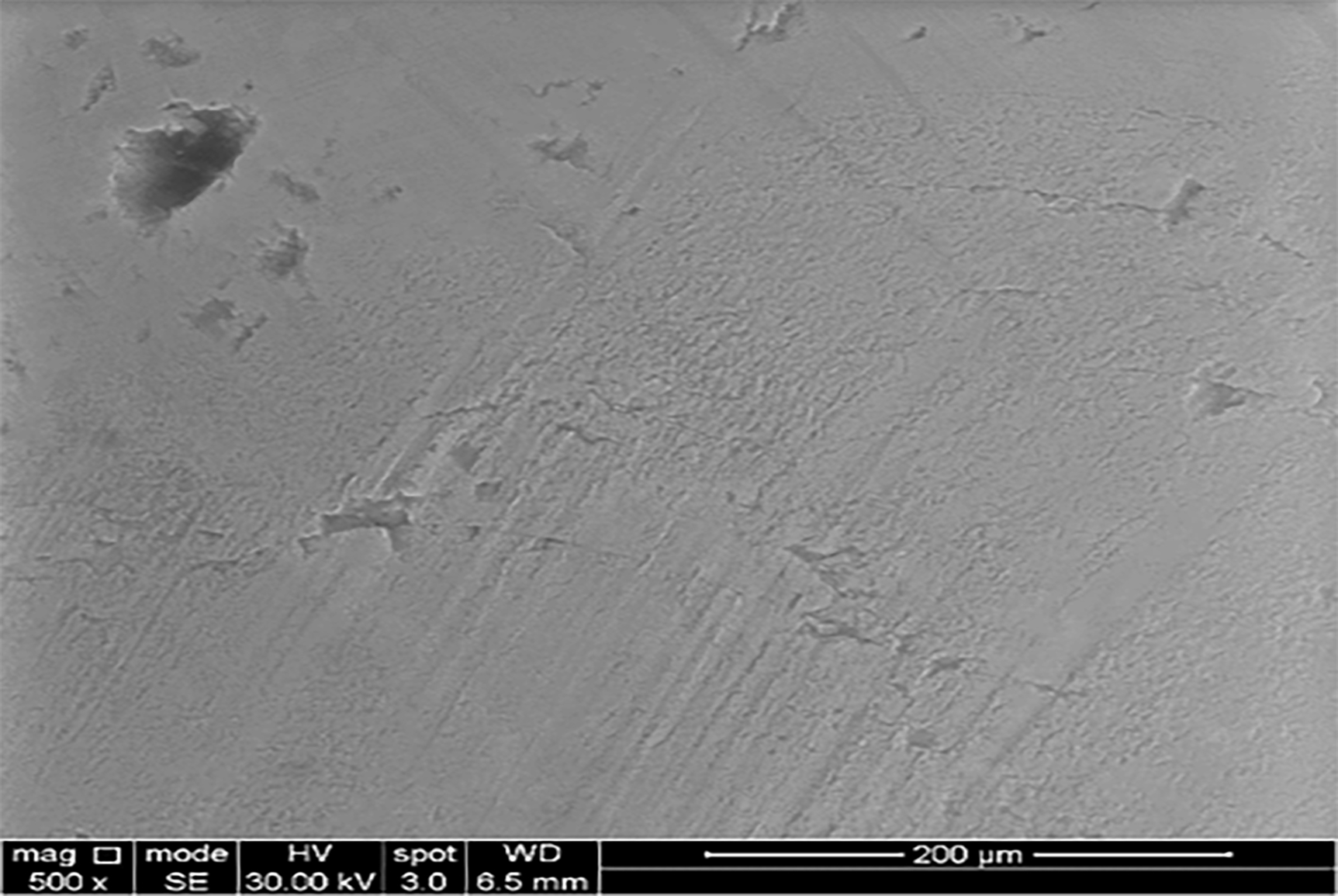
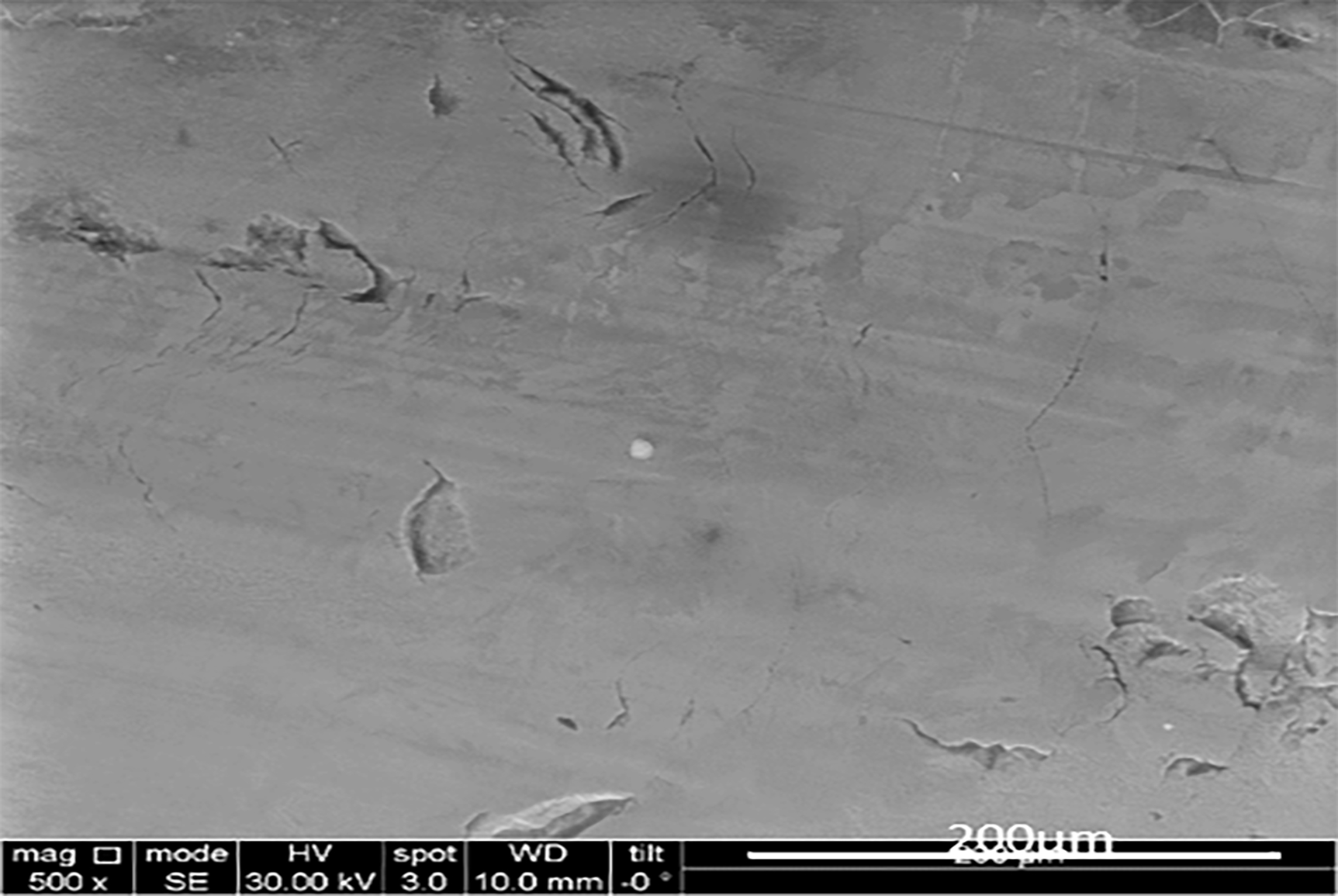
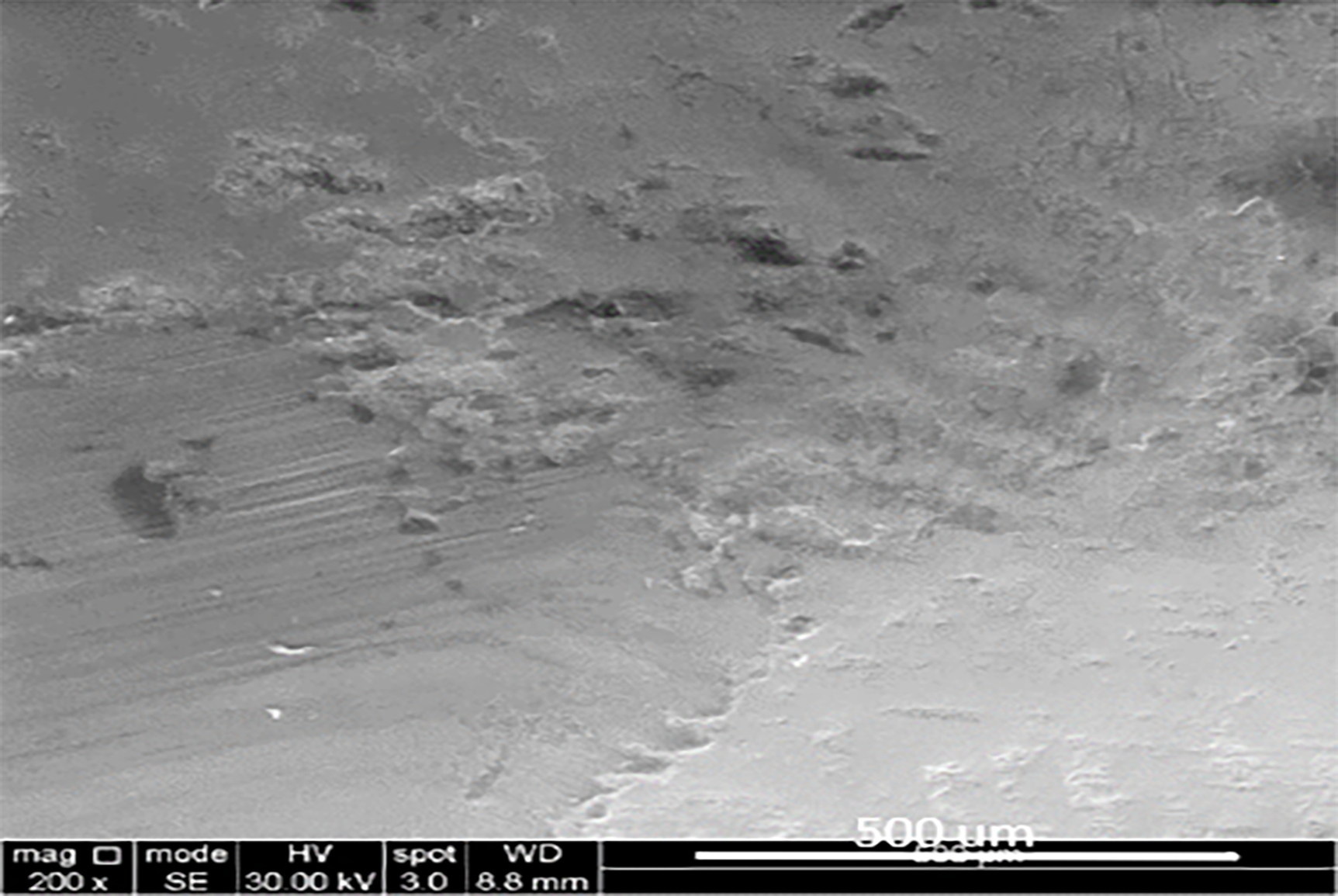
Microcracks were seen under scanning election microscope in all fatigued specimens. The microcracks were associated with the sliding contacts mainly (Figure 5). More microcracks were seen in the MYL zirconia groups (Groups 3 and 4) followed by the 4Y-PSZ (group 2) then 3Y-PSZ (control) (Figure 6).
Figure 5.
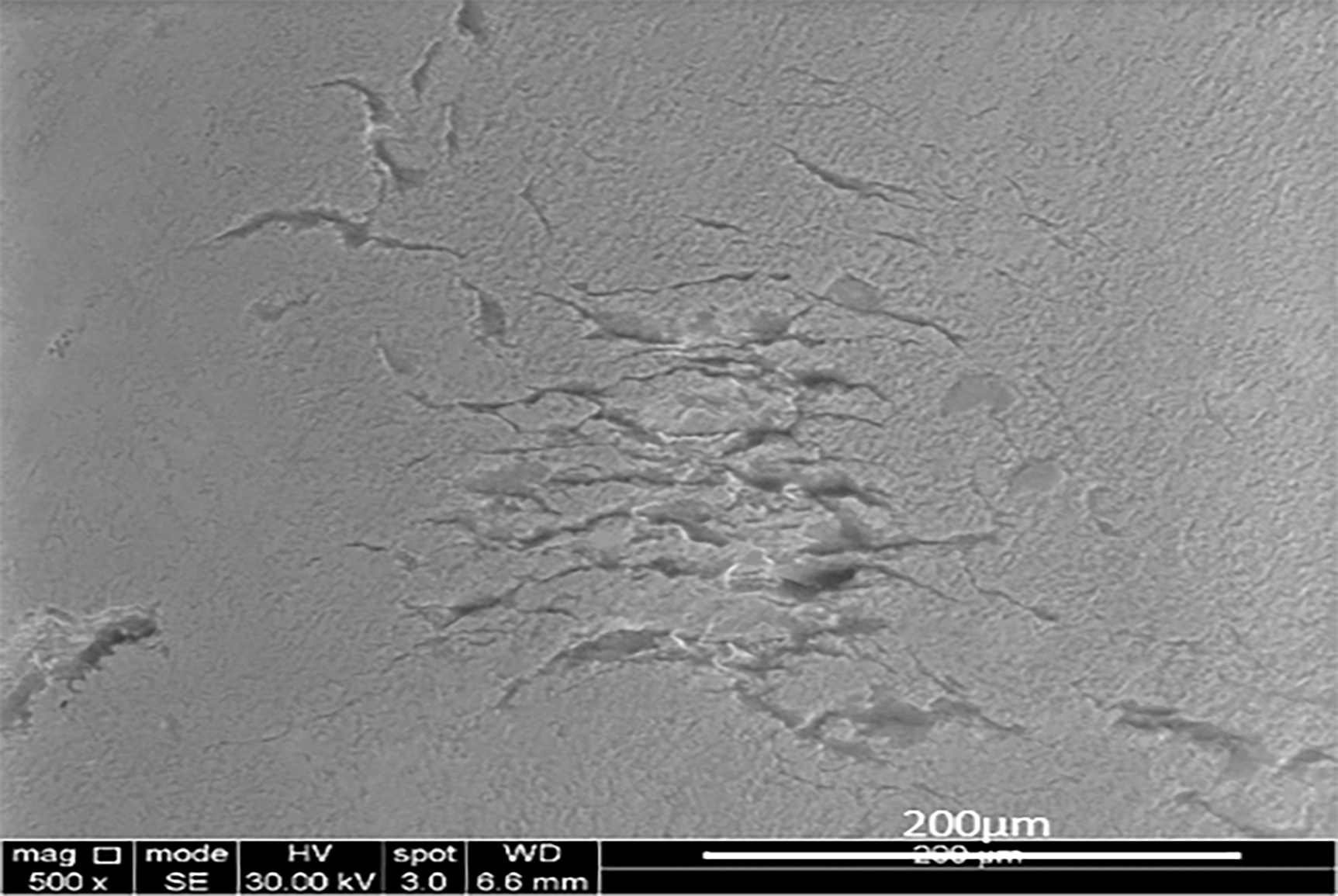
Scanning electron microscope analysis of areas of impact on MYL 5Y-PSZ/3Y-PSZ crown under up to 700× magnification:
(a) area of contact after sliding movement of the antagonist
(b) Area of contact after vertical movement of antagonist
Figure 6.
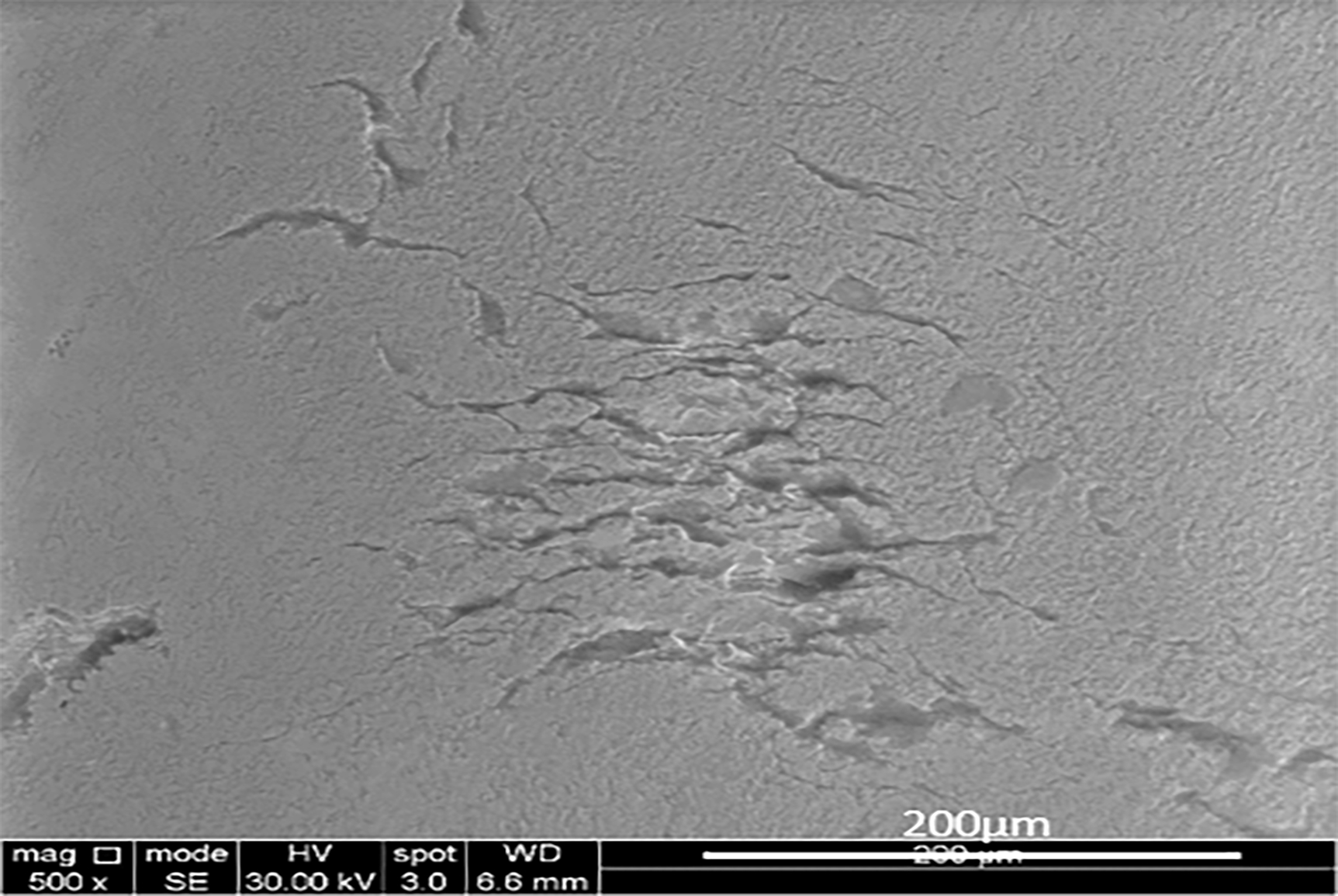
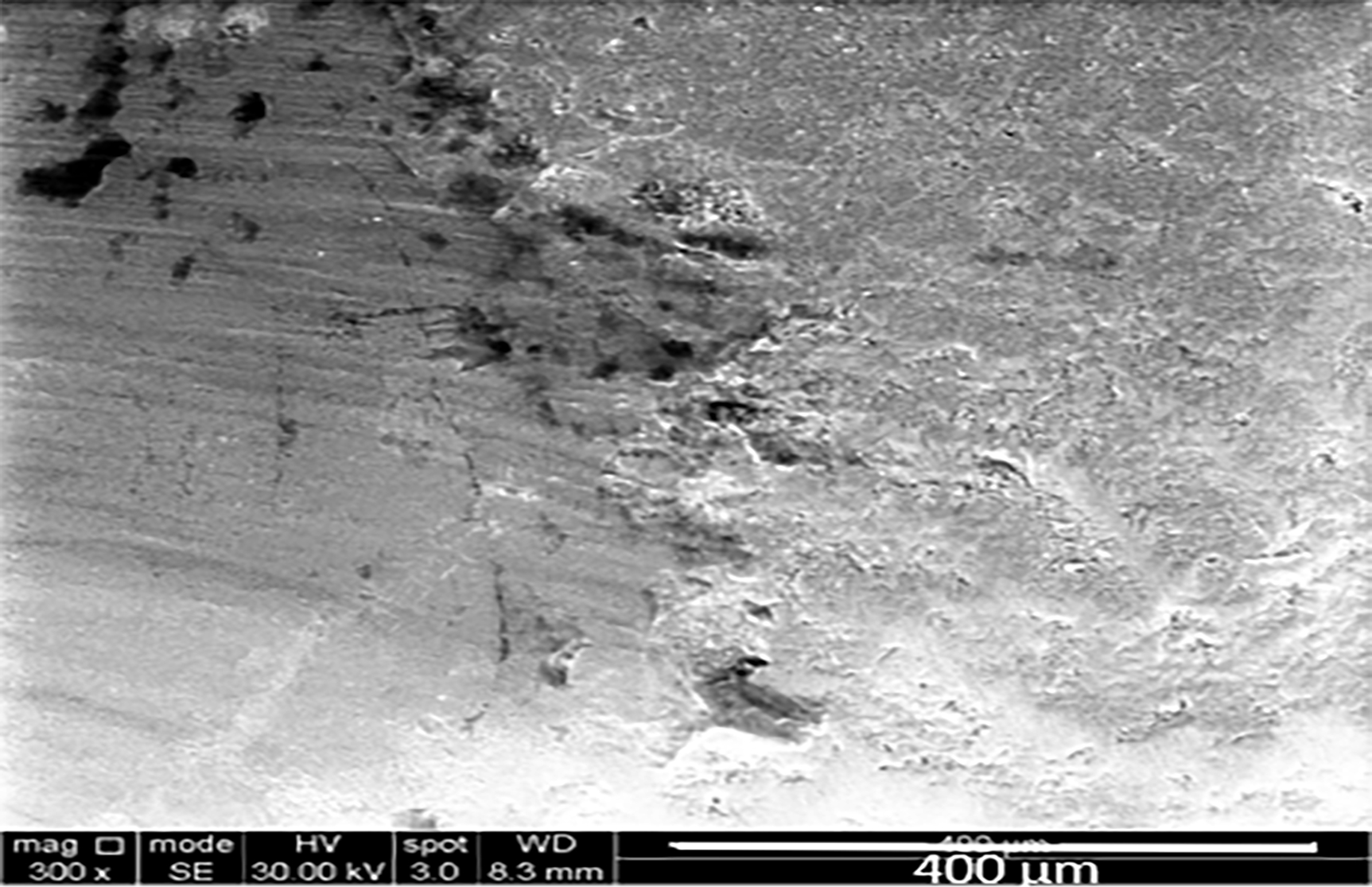
Scanning electron microscope analysis of areas of impact after sliding movement of the antagonist on zirconia crowns under up to 700× magnification:
(a) 3Y-PSZ
(b) 4Y-PSZ
(c) 5Y-PSZ/3Y-PSZ
(d) 5Y-PSZ/4Y-PSZ
The fractographic analysis indicated that the fracture originated from the contact surface of all fractured crowns (Figure 7). An interesting finding that was seen when the fractured pieces of the crowns were collected for fractographic analysis. The number of fragments was different among the groups. Less number of fragments was seen with 3Y-PSZ when compared to 4Y-PSZ and both of those had a smaller number of fragments when compared to the MYL zirconia with no apparent difference seen between the last two.
Figure 7.

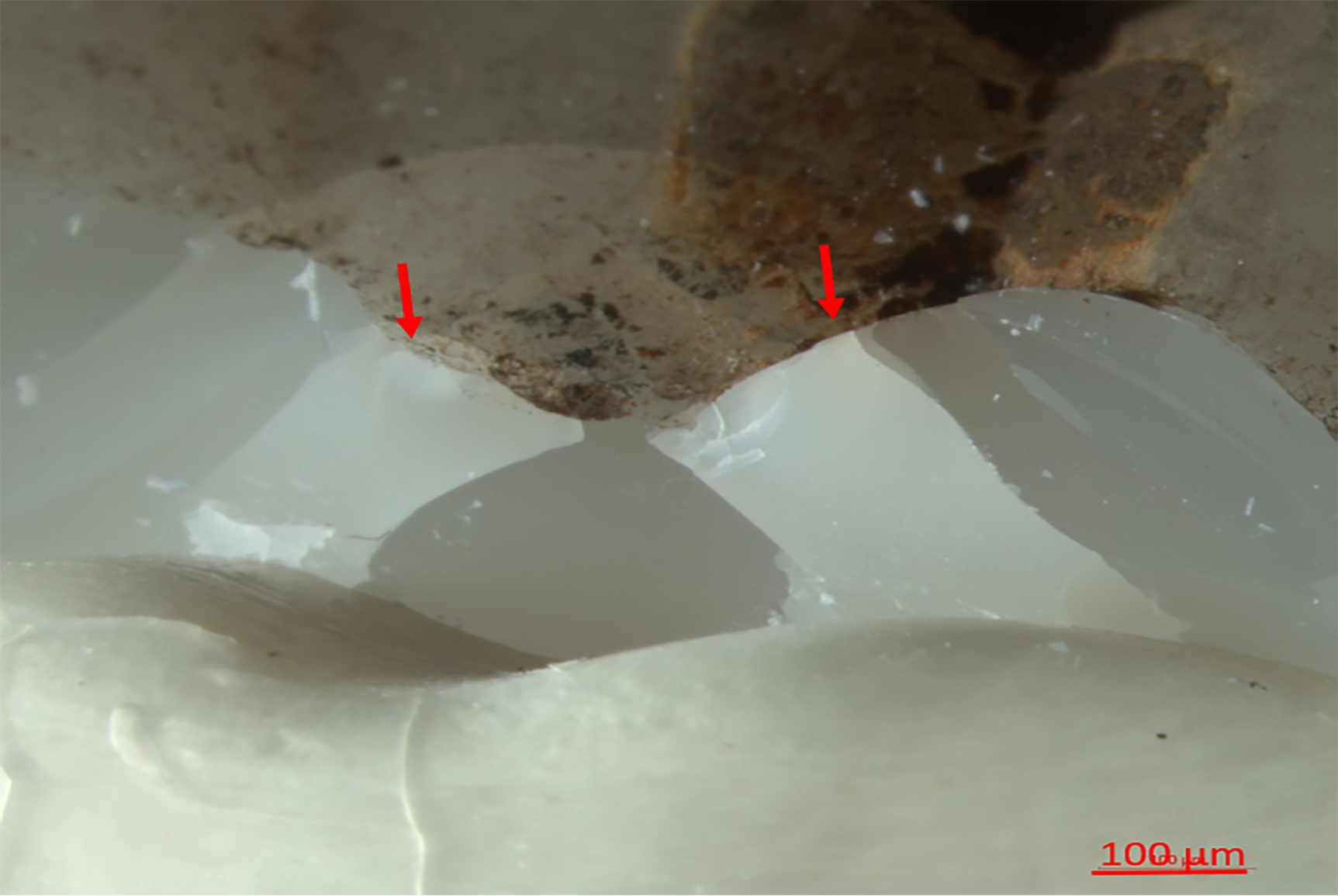
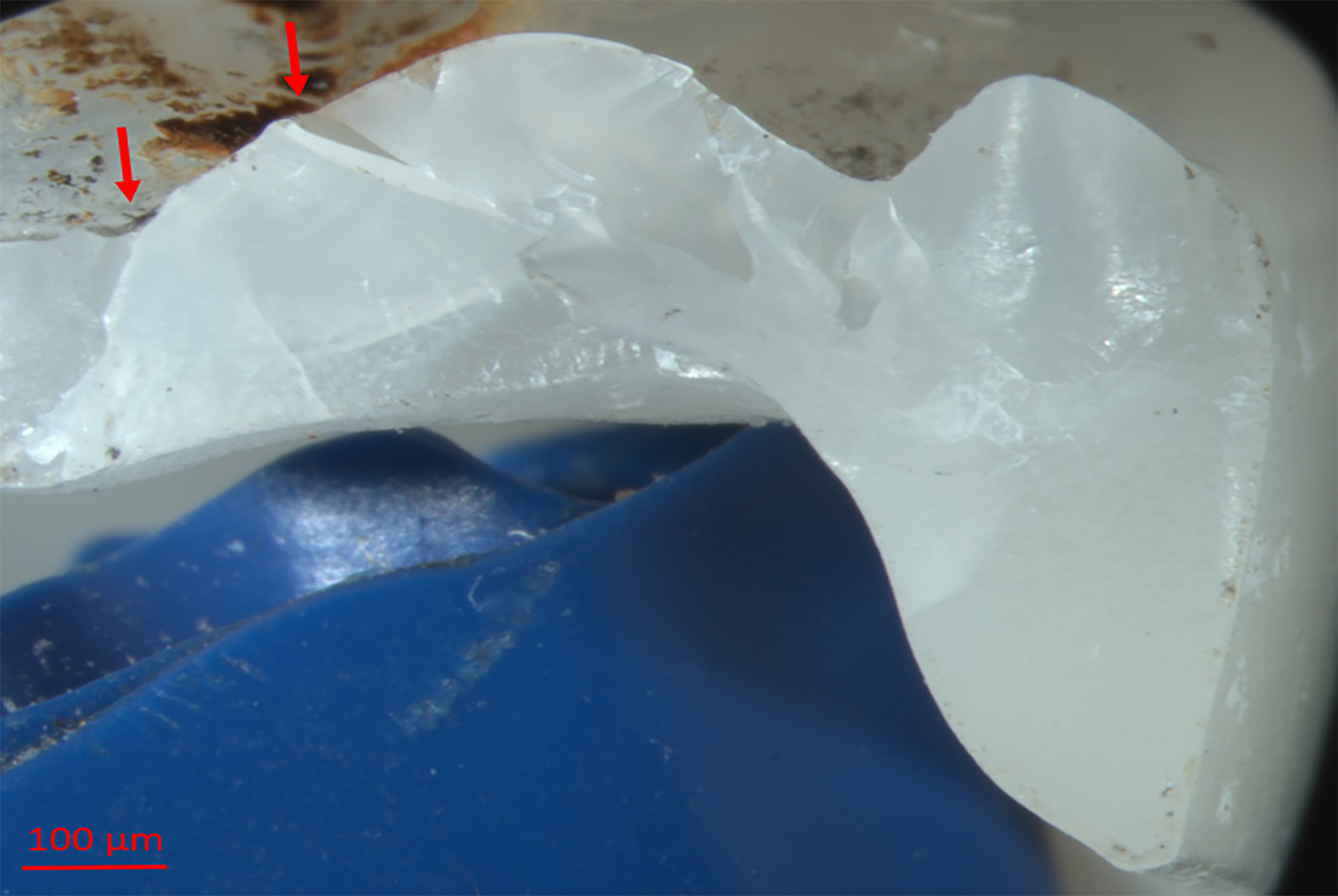
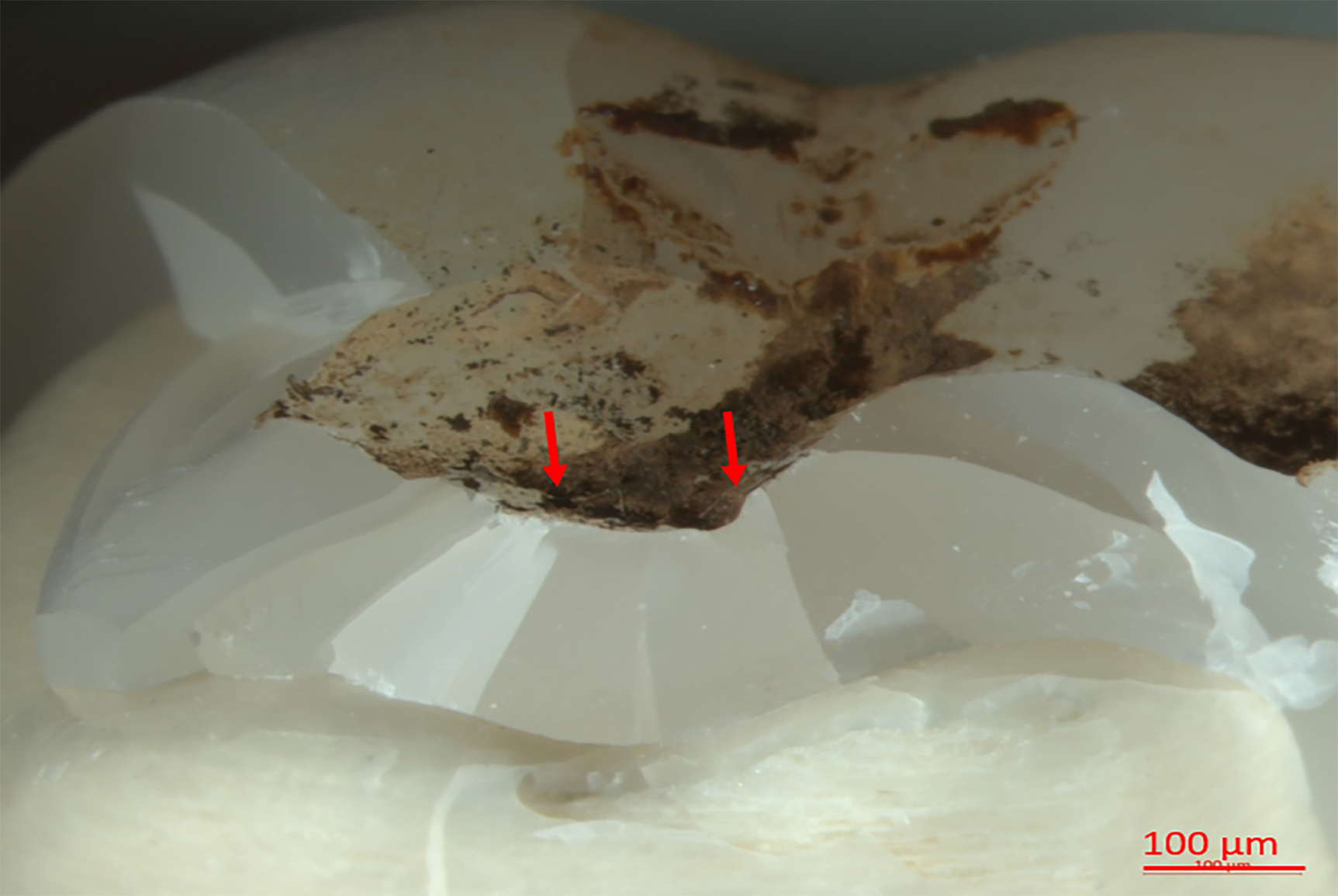
Fracture origin (arrow):
(a) 3Y-PSZ
(b) 4Y-PSZ,
(c) 5Y-PSZ/3Y-PSZ
(d) 5Y-PSZ/4Y-PSZ
DISCUSSION
The first null hypothesis was accepted as the mean fracture resistance for zirconia crowns within each type was not different between the two aging methods. A similar finding was reported in other studies were fracture resistance of zirconia was compared before and after mastication-relevant, low-load fatiguing and thermocycling.1,2,6,7 In one study, fatiguing and thermocycling of zirconia disks made from 3Y-PSZ and 5Y-PSZ in two different thicknesses did not affect the mean biaxial fracture loads of those two materials.6 Another study compared the biaxial fracture loads of 3Y-PSZ, 4Y-PSZ and 5Y-PSZ disks in 0.7- and 1.2-mm thicknesses before and after thermo-mechanical loading and found no difference in the mean biaxial fracture loads of those disks before and after fatiguing.7 The same finding was seen when the fracture resistance of zirconia anatomic crowns was tested. The thermo-mechanical loading did not affect the mean fracture resistance of zirconia crowns made from 3Y-PSZ and MYL 5Y-PSZ/4Y-PSZ.1 Similar results were seen when the fracture resistance of 3Y-PSZ, 4Y-PSZ and MYL 5Y-PSZ/5Y-PSZ zirconia crowns was compared before and after fatiguing.2
The second null hypothesis was rejected since the mean fracture load values were different among the groups. Monolithic 3Y-PSZ had the highest mean fracture load values, followed by monolithic 4Y-PSZ and then the two gradient MYL systems: 5Y-PSZ/3Y-PSZ and 5Y-PSZ/4Y-PSZ. The mean facture load values between the two gradient systems were not statistically different. The yttria content at the occlusal surface was the main factor in determining the zirconia’s fracture resistance regardless of its yttria content at the cervical and middle thirds of the crown. To the best of knowledge, this is the first study that investigated the effect of thermomechanical cyclic loading of monolithic zirconia crowns on the survival rate of two MYL zirconia systems: 5Y-PSZ/3Y-PSZ and 5Y-PSZ/4Y-PSZ and compared them to their “mono-yttria” counterparts 3Y-PSZ and 4Y-PSZ. The fracture resistance of the two multilayered groups was similar regardless of using a different yttria concentration at the cervical part of the crown. It is well-established that fracture of dental crowns can initiate either at the occlusal contact surface or cementation intaglio surface.8,9 In MYL systems, the strength of 3Y-PSZ or 4Y-PSZ at the cervical and middle thirds of the crown provided excellent resistance to flexural fracture at the cementation intaglio surface.10 However, the weak phase of zirconia (5Y-PSZ) at the occlusal third of those crowns offered little resistance to contact damage.11
In terms of chewing simulation parameters, there are no strict standards on the amount of force, frequency or number of cycles that can accurately mimic represent the clinical situation. However, the fatiguing parameters used in this research were based on a study that compared the success rate of dental ceramics intraorally to the success rate of the same types of dental ceramics by means of fatiguing. An agreement of 75% to 100% was seen between the two after 5 years of clinical/ artificial aging.12 While the most common mastication force used in the literature was 49 N.13 The simulated chewing force in this study was set at 110 N, which is closer to the physiological chewing force in humans.14 This was selected to ensure an aging situation that is similar to the oral environment. Also, the dies used in this study were made from fiber-reinforced resin. This material was chosen as a crown abutment instead of natural teeth because it is easy to standardize and has the same key physical properties as natural dentin.15–17 This would ensure a decent representation of the oral tissues without the use of natural teeth. Natural teeth can complicate the testing since it comes in variable sizes, shapes, and compositions (e.g., the enamel layer thickness).18, 19
The microcracks seen under the microscope were mainly herringbone cracks associated with lateral forces, similar to what has been confirmed in previous studies.20, 21 This can be explained by the nature of dental ceramics, dental ceramics behave better on compression, when compared to tension. Tensile forces are intensified under lateral occlusal loading.22–25 Thus, applying horizontal forces during in vitro fatiguing of dental ceramics is important to subject the material to cycles of tensile forces, which contribute more to the nature of failure with such material.26
The high survival rate of the traditional monolithic 3Y-PSZ was projected. This is mainly due to the transformation toughening phenomena.27 Transformation toughening happens by changing the phase of zirconia crystal structure around the crack from the tetragonal phase to the larger monoclinic phase, thus introducing compressive stresses that arrest the crack and prevent further propagation. This can also explain the high success rate of 4Y-PSZ since it has high amount of the tetragonal phase (75%).28 Whereas, the high survival rate of the two MYL zirconia groups can be attributed to two factors; the thickness of those crowns at the occlusal surface (1.5 mm) 6, 7 and, potentially, the effect of bonding the crowns to their corresponding dies rather than using conventional cementation.29
Thickness plays an important role for the success of dental restoration. In one study, the recommended minimal thickness for different types of zirconia as the following: 1 mm for 3Y-PSZ, 1.2 mm for 4Y-PSZ, and 1.5 mm for 5Y-PSZ.7 Since the minimal thickness of all the crowns regardless of zirconia used was 1.5 mm. The minimal thickness for all zirconia type was insured.
While bonding of glass dental ceramics to dental enamel increased its survival rates and fracture resistance.30 The enhancement in mechanical properties of those ceramics can be seen when fragile feldspathic veneers are bonded to dental enamel. Such procedure can result in high success rate over 15 years.31, 32 However, it is unknown whether bonding zirconia crowns to their substructure aids in their high survival rates. It is worth mentioning that bonding of zirconia is different from the bonding of other dental ceramics.4, 29, 33 The role of bonding was not investigated in this study.
Milling of the gradient zirconia systems can result in different composition and concentration of each layer. This can result of restorations with no or minimal translucent 5Y-PSZ zirconia. Luckily, the technician can control this by choosing where the restoration will be milled whiten the puck. Thus, those MYL zirconia restorations can be used as universal crown material depending on the esthetic and mechanical needs in each situation. However, in this study, the milling of the two MYL zirconia groups (group 3 and group 4) insured 3 mm of 5Y-PSZ occlusally. This was done to standardize and ensure the maximum concentration of the weakest zirconia phase in each crown, assuming that any difference in orientation will result in crowns with better mechanical properties.
Looking into the number of fragments after loading the crowns to failure. This number increased when the yttria content was increased. This can be explained by the fragile nature of zirconia when the yttria content is increased. Also, when increasing the yttria content, the amount of tetragonal phase that is unique of being able to undergo transformation toughening to stop or slow crack propagation decrease. Therefore, it can be proposed that when multiple cracks initiate in higher yttria content zirconia, it is more likely for all of those to propagate and create multiple fracture lines and more fragments. While when those cracks start in more predominantly tetragonal zirconia, some of them might arrest or collide into less major crack creating less fracture lines and less fragments.34
The fracture resistance of each layer in the MYL zirconia was not tested as a stand-alone material in this study. In addition, the hardness, yttrium content and Weibull modulus of each material were not investigated. Further research into the behavior of zirconia using other artificial aging methods, such as autoclaving, is suggested.35
The main limitation of this study is situated in its nature as an in vitro study, in spite of all the efforts made to simulate the harsh oral environment. In addition, a monolithic single-layer 5Y-PSZ group was not included in this study to conclusively eliminate the potential effect of the stronger 3Y-PSZ or 4Y-PSZ at the cervical third in reinforcing the crowns. The origin of failure at the contact surface rather than the intaglio surface is another limitation of this study. Further clinical studies are needed to investigate the in vivo behavior of those different zirconia materials.
CONCLUSIONS
Within the limitation of this in vitro study, the following can be concluded:
After the two methods of artificial aging, the survival rate of four different types of monolithic and multi-yttria-layered zirconia crowns with different yttria content was similar. Within each group, there was no difference in fracture resistance between thermocycling alone and thermo-mechanical loading.
The fracture resistance of zirconia crowns was as follow (from most to least resistant): 3Y-PSZ> 4Y-PSZ> (5Y-PSZ, 3Y-PSZ = 5Y-PSZ, 4Y-PSZ). There is an inverse relationship between the facture resistance of zirconia and its yttria concentration.
Figure 1b:

Die preparation occlusal view.
Clinical Significance.
The term “monolithic zirconia” alone without specifying the actual yttria content is misleading. This term represents different materials with different mechanical properties. The yttria content has an inverse relationship with the fracture resistance of zirconia crowns. The fracture resistance of multi-layer zirconia crowns is determined by the amount of the weaker zirconia phase at the occlusal part of the restoration rather than enforced by the stronger zirconia at the cervical part of the crown.
Acknowledgments
The authors would like to express their sincere gratitude to Brandon Rodgers, Matt Stone, Sonaj Vardhaman, and Manal Hamdan for their help and support conducting this research. YZ would like to thank the U.S. National Institutes of Health/National Institute of Dental and Craniofacial Research for their support (grant numbers R01DE026279 and R01DE026772).
Footnotes
Conflict of Interest Declaration: The authors declare no conflict of interest.
Data Availability Statement:
The data that support the findings of this study are available from the corresponding author upon reasonable request.
REFERENCES
- 1.Vardhaman S, Borba M, Kaizer MR, et al. Wear behavior and microstructural characterization of translucent multilayer zirconia. Dent Mater. 2020; 36(11):1407–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Michailova M, Elsayed A, Fabel G, et al. Comparison between novel strength-gradient and color-gradient multilayered zirconia using conventional and high-speed sintering. J Mech Behav Biomed Mater. 2020; 111(1):103977. [DOI] [PubMed] [Google Scholar]
- 3.Donovan TE, Alraheam IA, Sulaiman TA. An evidence-based evaluation of contemporary dental ceramics. Dental Update. 2018; 45(6):541–546 [Google Scholar]
- 4.Blatz MB, Alvarez M, Sawyer K, Brindis M. How to Bond Zirconia: The APC Concept. Compend Contin Educ Dent. 2016; 37(9):611–616. [PubMed] [Google Scholar]
- 5.Zhao K, Wei YR, Pan Y, et al. Influence of veneer and cyclic loading on failure behavior of lithium disilicate glass-ceramic molar crowns. Dent Mater. 2014; 30(2):164–171. [DOI] [PubMed] [Google Scholar]
- 6.Alraheam IA, Donovan T, Boushell L, et al. Fracture load of two thicknesses of different zirconia types after fatiguing and thermocycling. J Prosthet Dent. 2020; 123(4):635–640. [DOI] [PubMed] [Google Scholar]
- 7.Abdulmajeed A, Sulaiman T, Abdulmajeed A, et al. Fracture Load of Different Zirconia Types: A Mastication Simulation Study. J Prosthodont. 2020. Dec; 29(9):787–791. [DOI] [PubMed] [Google Scholar]
- 8.Zhang Y, Lawn BR. Evaluating dental zirconia. Dent Mater. 2019. Jan;35(1):15–23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Rekow ED, Silva NR, Coelho PG, et al. Performance of dental ceramics: challenges for improvements. J Dent Res. 2011. Aug;90(8):937–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Bhowmick S, Zhang Y, Lawn BR. Competing Fracture Modes in Brittle Materials Subject to Concentrated Cyclic Loading in Liquid Environments: Bilayer Structures. Journal of Materials Research. 2005. 20(10):2792–2800. [Google Scholar]
- 11.Zhang Y, Bhowmick S, Lawn BR. Competing Fracture Modes in Brittle Materials Subject to Concentrated Cyclic Loading in Liquid Environments: Monoliths. Journal of Materials Research. 2005. 20(8):2021–2029. [Google Scholar]
- 12.Rosentritt M, Siavikis G, Behr M, et al. Approach for evaluating the significance of laboratory simulation. J Dent. 2008; 36(12):1048–1053. [DOI] [PubMed] [Google Scholar]
- 13.Nawafleh N, Hatamleh M, Elshiyab S, Mack F. Lithium Disilicate Restorations Fatigue Testing Parameters: A Systematic Review. J Prosthodont. 2016; 25(2):116–126. [DOI] [PubMed] [Google Scholar]
- 14.Abe I, Milczewski MS, Souza MA, et al. The force magnitude of a human bite measured at the molar intercuspidation using fiber Bragg gratings. Journal of Microwaves, Optoelectronics and Electromagnetic Applications. 2017; 16(1):434–444. [Google Scholar]
- 15.El Ghoul WA, Özcan M, Ounsi H, et al. Effect of different CAD-CAM materials on the marginal and internal adaptation of endocrown restorations: An in vitro study. J Prosthet Dent. 2020; 123(1):128–134. [DOI] [PubMed] [Google Scholar]
- 16.Xu H, Smith D, Jahanmir S, et al. Indentation damage and mechanical properties of human enamel and dentin. J Dent Res. 1998; 77(3):472–480. [DOI] [PubMed] [Google Scholar]
- 17.Yan J, Kaizer MR, Zhang Y. Load-bearing capacity of lithium disilicate and ultra-translucent zirconias. J Mech Behav Biomed Mater. 2018. Dec;88:170–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Smith TM, Olejniczak AJ, Reid DJ, et al. Modern human molar enamel thickness and enamel-dentine junction shape. Arch Oral Biol. 2006; 51(11):974–995. [DOI] [PubMed] [Google Scholar]
- 19.Ferrari M, Patroni S, Balleri P. Measurement of enamel thickness in relation to reduction for etched laminate veneers. Int J Periodontics Restorative Dent. 1992; 12(5):407–413. [PubMed] [Google Scholar]
- 20.Ren L, Zhang Y. Sliding contact fracture of dental ceramics: Principles and validation. Acta Biomater. 2014. Jul;10(7):3243–53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Ren L, Liu L, Bhowmick S, et al. Improving fatigue damage resistance of alumina through surface grading. J Dent Res. 2011. Aug;90(8):1026–30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Yoshinari M, Dérand T. Fracture strength of all-ceramic crowns. International Journal of Prosthodontics. 1994; 7(4):329–338. [PubMed] [Google Scholar]
- 23.Sobrinho LC, Cattel MJ, Glover RH, Knowles JC. Investigation of the dry and wet fatigue properties of three all-ceramic crown systems. Int J Posthodont. 1988; 11(3): 255–262. [PubMed] [Google Scholar]
- 24.Zhang Y, Sailer I, Lawn BR. Fatigue of Dental Ceramics, J Dent. 2013; 41(12):1135–1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kim JW, Kim JH, Thompson VP, Zhang Y. Sliding Contact Fatigue Damage in Layered Ceramic Structures. Journal of Dental Research. 2027; 86(11):1046–1050. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Borba M, Okamoto TK, Zou M, et al. Damage sensitivity of dental zirconias to simulated occlusal contact. Dent Mater. 2021. Jan;37(1):158–167. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Garvie RC, Hannink RH, Pascoe RT. Ceramic steel?. Nature 1990; 258(5537):253–257. [Google Scholar]
- 28.Zhang Y, Lawn BR. Novel Zirconia Materials in Dentistry. J Dent Res. 2018; 97(2):140–147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Gupta S, Abdulmajeed A, Donovan T, et al. Monolithic Zirconia Partial Coverage Restorations: An In Vitro Mastication Simulation Study. Journal of Prosthodontics. 2021; 30(1):76–82. [DOI] [PubMed] [Google Scholar]
- 30.Krummel A, Garling A, Sasse M, Kern M. Influence of bonding surface and bonding methods on the fracture resistance and survival rate of full-coverage occlusal veneers made from lithium disilicate ceramic after cyclic loading. Dent Mater. 2019; 35(10):1351–1359. [DOI] [PubMed] [Google Scholar]
- 31.Friedman MJ. A 15-year review of porcelain veneer failure--a clinician’s observations. Compend Contin Educ Dent. 1998; 19(6):625–632 [PubMed] [Google Scholar]
- 32.Dumfahrt H, Schäffer H. Porcelain laminate veneers. A retrospective evaluation after 1 to 10 years of service: Part II--Clinical results. Int J Prosthodont. 2000; 13(1):9–18. [PubMed] [Google Scholar]
- 33.Inokoshi M, De Munck J, Minakuchi S, Van Meerbeek B. Meta-analysis of bonding effectiveness to zirconia ceramics. J Dent Res. 2014; 93(4):329–334. [DOI] [PubMed] [Google Scholar]
- 34.Denry I, Kelly JR. State of the art of zirconia for dental applications. Dent Mater. 2008; 24(3):299–307. [DOI] [PubMed] [Google Scholar]
- 35.Elsaka SE. Optical and mechanical properties of newly developed monolithic multilayer zirconia. Journal of Prosthodontics. 2019;28(1):e279–284. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The data that support the findings of this study are available from the corresponding author upon reasonable request.


