Abstract
Background/Aims:
Alcohol use disorder (AUD), since the release of DSM-V, is conceptualized and studied as a unidimensional construct. However, previous research has identified clusters of AUD symptoms related to excessive consumption/tolerance, loss of control/social dysfunction, and withdrawal/craving that have shown differential genetic risks, personality associations, and predictive ability. Although past “variable-centered” (e.g., factor-analytic) studies have demonstrated the importance of these clusters, the current study aimed to examine how these clusters commonly manifest using a “person-centered” approach (e.g., latent class).
Design:
Cross-sectional in-person assessment.
Setting:
Indiana, USA.
Participants:
A convenience-sample of 1390 young-adults (mean age = 21.43, SD = 2.47) recruited for an overrepresentation of alcohol problems (65% with AUD).
Measurements:
Latent class analysis (LCA) was conducted on 23 criteria from the Semi-Structured Interview on the Genetics of Alcoholism (SSAGA) that align with DSM-V AUD symptoms. Identified latent classes were characterized using multinomial regressions to examine the association of class and measures of alcohol use, other externalizing psychopathology, internalizing problems, and personality.
Findings:
LCA results identified a “Low Problems” class (34% of sample), a “Heavy Consumption” class (26%) characterized by high endorsement probabilities of essentially only consumption/tolerance symptoms, a “Consumption & Loss of Control” class (31%) characterized by endorsing consumption/tolerance and loss of control/social dysfunction symptoms, and finally a “Consumption, Loss of Control, and Withdrawal” class (9%) characterized by high endorsement probabilities of all symptom clusters. Multinomial regression results indicated an increasing spectrum of severity in terms of psychological impairment.
Conclusions:
Alcohol use disorder appears to manifest as different clusters of symptoms at different severity levels.
Keywords: alcohol use disorder, diagnosis, heterogeneity, classification, etiology, latent class analysis
INTRODUCTION
Alcohol Use Disorder (AUD), since DSM-V, is conceptualized and studied as a unidimensional construct. Collapsing DSM-IV alcohol abuse and dependence into a single diagnosis was primarily driven by factor-analytic and item-response theory analyses demonstrating that AUD symptoms were adequately modeled using a single factor (1–3). Although, we applaud many of the changes made in DSM-V based on rigorous analyses, there remains significant reasons to doubt the accuracy and utility of this conceptualization. Importantly, continuing to closely examine our diagnostic constructs should remain of the utmost importance as the quality of our diagnostic system serves as a foundational building block for all other clinical research.
In a recent study, Watts et al., (4) make a compelling argument that the consensus on the unidimensionality of AUD could be premature and ignores important heterogeneity within individuals with AUD. Watts and colleagues (4) discuss how unidimensionality in AUD is likely, at least, partially driven by “crude” measurement of AUD in the literature, specifically that DSM-V symptoms are a highly aggregated description of alcohol problems. In fact, many of the broad diagnostic symptoms can be satisfied by endorsement of very different criteria both in terms of content and severity (5). Consequently, if researchers rely only on DSM-V criteria when assessing AUD, they are likely to observe unidimensional solutions. However, this does not necessarily indicate support for the unidimensionality of the phenomena but is perhaps driven by the use of unidimensional assessment. The concern of premature reification of DSM-V diagnoses is not unique to AUD, but a specific instance of a more general concern with over-reliance on DSM formulations for a range of diagnoses (6).
Beyond measurement concerns, and most germane to the current study, is the concern that the unidimensional AUD conceptualization ignores theoretically meaningful symptom clusters within AUD (4). Previous studies have identified symptom clusters of AUD symptoms related to tolerance/excessive consumption, withdrawal/continued use despite problems, and loss of control/social dysfunction (7, 8). Furthermore, behavior genetic studies have indicated that there are disparate, although correlated, genetic risk for alcohol tolerance/excessive consumption versus other types of alcohol problems (7, 9). Interestingly, studies have shown that these symptom clusters have differing predictive validity, specifically that tolerance/excessive consumption symptoms are a poor predictor of overall AUD severity and other forms of psychopathology (4, 10, 11). Wakefield & Schmitz (10, 11) posited that individuals who only have problems with excessive consumption (i.e., tolerance and habitual use) are etiologically and qualitatively different than individuals who also have “harmful use” (i.e., drinking that affects social and professional functioning) and “dysfunction” (i.e., withdrawal, craving, and inability to reduce). Specifically, these individuals may have different risk and/or protective factors that allow them to contain their heavy use to personally and socially acceptable levels. Similarly, research has shown differential personality profiles associated with these clusters, specifically more severe alcohol problems were strongly associated with social deviance (a personality trait associated with externalizing psychopathology), while excessive consumption was more closely linked to excitement seeking, a disinhibitory personality trait (9, 12, 13). Furthermore, a recent study by Müller et al., (14) identified differential patterns of alcohol problems with comorbid psychopathology, specifically observing the highest levels of alcohol consumption, acute problems (e.g., blackouts), and withdrawal in those with comorbid antisocial personality disorder and other substance use disorders, while observing the highest levels of harm problems (i.e., impairment at work/school) in individuals with comorbid anxiety/depression (14). Taken together, it appears that AUD may be best characterized not as a unitary construct, but as the intersection of three theoretically distinct dimensions: (1) an excessive consumption/tolerance cluster (2) a loss of control/social dysfunction cluster and (3) a withdrawal/continued use cluster.
Although substantial research has pointed to the importance of these clusters in variable-centered analyses, it remains unclear how these symptom clusters vary within individuals with alcohol use problems. “Person-centered” analyses, such as latent class analysis (LCA), provide a useful complement to examine how these clusters vary and present within individuals. Early studies on subtypes within AUD identified two types: (1) a more severe manifestation with earlier onset and more comorbid pathology, and (2) a less severe manifestation with later onset and lower overall severity (15, 16). Subsequent work has since identified as many as four possible AUD subtypes including a chronic/severe, depressed/anxious, antisocial, and mild type (17). Most important for the current study, these subtypes may indicate limitations for our diagnostic formulation. For example, Lynskey et al., (18) examined latent patterns of DSM-IV symptoms and found that the patterns identified were not consistent with the DSM-IV formulation of alcohol abuse and dependence. Interestingly, Lynskey et al., (18) found that about a quarter of individuals had a mild presentation (labeled as “Heavy Drinkers”), characterized by problems with tolerance/excessive consumption with low likelihood of most other symptomology. In contrast, the DSM-V is formulated to suggest that mild AUD is simply a quantitatively less severe AUD manifestation compared with moderate and then severe AUD. This formulation neglects to consider that there are qualitatively different AUD presentations at different severity levels that are related to disparate risks factors and outcomes.
The current study extends the literature by examining multivariate patterns of AUD symptomology using an in-depth 23-item set related to DSM-V diagnostic criteria in a high externalizing (65% with AUD) large sample of young-adults (n = 1390). In addition, the current study examines how these aforementioned symptom clusters manifest across identified classes. The study has three primary aims
Identify common AUD presentations using a detailed measure of AUD.
Examine how symptom presentations vary across different severity levels, specifically the prevalence of excessive consumption/tolerance (labeled as consumption going forward), loss of control/social dysfunction (labeled loss of control), and withdrawal/craving (labeled withdrawal) symptom clusters across severity.
Characterize the identified patterns using measures of alcohol use, externalizing symptoms and disinhibited personality, and other measures of psychological dysfunction known to be associated with AUD.
METHODS
Sample characteristics
The sample was originally recruited for a cross-sectional study on alcohol misuse, co-occurring psychopathology, and risky decision making (19). A convenience sample was recruited to have an overrepresentation and wide variety of alcohol problems. This study was reviewed and approved by the Indiana University-Bloomington Institutional Review Board (IRB) and all participants gave informed consent.
Recruitment
Participants were recruited using flyers, business cards placed around the community, along with postings on the Indiana University classifieds web page. The flyers and postings were designed to obtain a sample with a large proportion and range of individuals with alcohol problems varying from no problems to severely impaired. Individuals were not retained if they had other externalizing disorders without AUD, but could have other externalizing disorders in addition to AUD. Although this may lead to an underrepresentation of illicit drug use disorders without comorbid alcohol problems, research has noted that this presentation is quite rare (20).
Test session exclusion criteria
Before every testing session participants were required to meet a set of criteria before proceeding. All participants were asked a standardized set of question to confirm that they: (1) have had no self-reported use of drugs or alcohol within the past 12 hours prior to testing, (2) have gotten at least 6 hours of sleep the previous night, and (3) were not experiencing symptoms of withdrawal or of any acute illness that they believed could affect their assessment. In addition, participants had to have a breath alcohol level of 0.0% (tested with an AlcoSensor IV, Intoximeters Inc., St. Louis MO). In total, 6 participants failed to meet the above criteria and were rescheduled to a later date where they met the above criteria.
Diagnoses and alcohol/substance use measures
Participants were administered the Semi-Structured Assessment for the Genetics of Alcoholism (SSAGA;21) to obtain DSM-V diagnoses of AUD, cannabis use disorder (CUD), and other illicit drug use disorders (DUD). For AUD symptom analyses, 23-items were selected that provided multiple criteria per symptom when possible. Items are listed in Table 1. This was done as research has shown substantial variability between different criterion that satisfy a given symptom (5) and that this aggregation may bias studies towards overly-simplistic solutions (4).
Table 1.
AUD Items for Analysis
| AUD Sx. # | Sx. Cluster | Item | Endorsement Rate (%) |
|---|---|---|---|
|
| |||
| 1a | C | Drank more than intended, more days in a row than intended, or when promised self wouldn’t 3+ times | 60 |
| 1b | C | Became drunk when didn’t want to 3+ times | 32 |
| 2a | L | Wanted to stop or cut down 3+ times | 34 |
| 2b | L | Tried but was unable to stop or cut down | 29 |
| 3 | C | Drinking or recovering from effects left little time for anything else for 1+ month or 3+ times | 27 |
| 4 | W | Such a strong desire to drink you cannot think of anything else | 11 |
| 5a | L | Neglected responsibilities when binging 3+ times | 9 |
| 5b | L | Drinking or being hung over often interfered with responsibilities | 30 |
| 5c | L | Drinking caused problems with work/school 3+ times | 14 |
| 6a | L | Drinking caused problems with family or friends 3+ times | 22 |
| 6b | L | Lost friends because of drinking 3+ times | 3 |
| 6c | L | Drinking caused problems in love relationships 3+ times | 11 |
| 7 | L | Gave up or greatly reduced important activities to drink 3+ times or for 1+ month | 23 |
| 8a | L | Mixed alcohol & medications/drugs when knew this was dangerous 3+ times | 31 |
| 8b | L | Negative effects from mixing alcohol and drugs when knew it was dangerous | 11 |
| 8c | L | Was drunk in situations where could have injured self 3+ times | 25 |
| 9a | L | Continued to drink knowing alcohol caused health problems | 9 |
| 9b | L | Continued to drink despite serious physical illness | 12 |
| 9c | L | Continued to drink knowing alcohol caused emotional problems | 17 |
| 10a | C | Needed 50% more alcohol to get an effect | 30 |
| 10b | C | Could drink 50% more alcohol before getting drunk | 26 |
| 11a | W | Experienced withdrawal symptoms | 10 |
| 11b | W | Drank to relieve or avoid withdrawal symptoms 3+ times | 10 |
AUD Sx. #: Refers to the DSM-V AUD symptom the item satisfies. Letters distinguish different items that relate to the same diagnostic criteria. Sx. Cluster = the theoretical symptom cluster the item correspond with, C = consumption symptom cluster, L = loss of control, W = withdrawal
Class validation measures
Alcohol use was assessed using a timeline follow-back procedure to assess the frequency (# of drinking occasions per week), quantity (# of total drinks per week), and binges (# drinking occasions consuming 4+ for women and 5+ for men per week). To examine more acute alcohol problems, a brief scale, labeled “Acute Alc. Problems” was created by summing four common alcohol problems assessed from the SSAGA: (1) Arrested for public intoxication, (2) Arrested for drunk driving, (3) Suffered significant injuries while drinking, (4) Blackouts on 3+ occasions. These items were selected because they are common public health concerns associated with drinking (22–25). Treatment seeking was assessed using a single item from the SSAGA asking individuals whether they had ever spoken with a professional about their drinking.
Illicit drug use severity for validation analyses was assessed by producing factor scores from a unidimensional confirmatory factor analysis (CFA) model using DSM-V symptom counts of cannabis, stimulant, sedative, opiate, and other (e.g., inhalants) use disorders. This was done to provide a general estimate of illicit drug use given past research that demonstrated the importance of integrating information across substances to gain an accurate estimate of overall substance use problems (20, 26, 27). CFA was conducted using a maximum likelihood estimator with robust (Huber-White) standard errors (28) to account for non-normality of symptom counts, called “MLR” estimator in “lavaan” package (29). Adequate fit is reflected by a root mean squared error of approximation (RMSEA) < .08 and a Comparative Fit Index (CFI) >.94 (30, 31). Factor scores were generated using the Empirical Bayes Modal method (32).
Conduct disorder symptoms, a measure of externalizing psychopathology, were assessed by summing conduct disorder symptoms obtained from the SSAGA. Disinhibited personality traits were assessed using the 19 dichotomous-item Impulsivity I7 Questionnaire (33) and the 10 forced-choice item Experience Seeking subscale of the Sensation-Seeking Scale (34).
Measures of other relevant psychological dysfunction included (1) trait anxiety was assessed with the 20 Likert-item Trait Anxiety scale of the State-Trait Anxiety Inventory (35), (2) depression was assessed with the 21 Likert-item Beck Depression Inventory-II (36), and (3) Borderline Personality Disorder (BPD) symptoms were assessed using 15 dichotomous-item SCID-II (Structured Clinical Interview for DSM-IV Axis II Personality Disorders) screening questionnaire for BPD symptomatology (37).
Statistical analyses
R version 3.6.1 was used for all analyses (38) including the “poLCA” package for LCA (39), the “VGAM” package for multinomial regression (40), the “missForest” package for data imputation (41), and the “ggplot2” package for figure creation (42). These analyses were not pre-registered and therefore results should be considered exploratory.
Missing data
Data were imputed using a random forest algorithm using all other non-missing items or measures. Random forest imputation has shown to outperform other commonly used methods of imputation, especially when using categorical data as with the current diagnostic data (41, 43). Data was not imputed for the BDI (65% missing) and BPD measure (38% missing) because these data were missing due to structural changes to the study protocol to reduce participant burden.
Latent class analysis
LCA was conducted using the 23 items related to AUD diagnostic criteria (Table 1), using the expectation maximization (EM) algorithm (44). Models ranging from 2 to 6 classes were evaluated based on the theoretical interpretability of the classes, Akaike’s Information Criterion (AIC), Sample Size Adjusted Bayesian Information Criteria (SSABIC) (45), entropy statistic (46), Lo-Mendell-Rubin likelihood ratio test (LMRT) (47), and the size of identified classes. Lower values indicate better fit for both AIC and SSABIC. Entropy serves as an index of the precision of assigning latent class membership (ranges from 0 to 1) with values near 1 indicating high precision of assignment.
Multinomial regression
Class membership was assigned based on the highest modal probability of each participant (39). Separate univariable multinomial regressions were used to assess the association between age, drinking patterns, acute alcohol problems, conduct disorder symptoms, impulsive and experience-seeking personality, anxiety, depression, BPD symptoms, and class membership. Separate univariable multinomial regressions were used to provide the most easily interpretable description of the classes across measures. Furthermore given the exploratory nature of our analyses, our primary aim is to provide overall description and not to test any specific causal relationships between covariates and class membership (48).
RESULTS
Sample Characteristics Results
The sample consisted of 1390 (674 female, 716 male) young adults with a mean age of 21.43 (SD=2.47) ranging from 18 to 30 years old. Sample contained an overrepresentation of alcohol problems with 65% with an AUD, 40% with a CUD, and 18% with a DUD. The sample was predominantly college-students (82%) and was 78% White, 7% Black, 7% Asian, 5% Latino, and 3% other (e.g., multi-racial). The diagnostic interview used for LCA analysis and for diagnoses consisted of <1% imputed data and the validation measures had <2% imputed data
Substance use factor CFA results
The CFA of illicit drug use measures fit the data well (RMSEA=.046 and a CFI=.97). All substances were robust indicators of this general Drug Use factor with loadings of .49, .73, .72, .73, and .63, for cannabis, stimulants, sedatives, opiates, and other substances, respectively.
Latent class analysis results
Table 2 presents the fit statistics for the models from 2 to 6 classes. AIC, SSABIC, LMRT statistics showed improvement with each subsequent class. Entropy statistics indicated all solutions had high to moderately-high confidence in class membership. However, the four-class solution provided the most interpretable and theoretically meaningful solution. The five-class solution added another class that was not meaningfully different and appeared to simply bifurcate an existing class in the four-class solution into subclasses with little theoretical difference. The six-class solution also had limited theoretical meaning and resulted in some very small classes (i.e., <5% of the total sample). Supplementary figures 1 and 2 depict the five-class and six-class solutions respectively. We decided to primarily examine the four-class solution as we believe it provided the most theoretically meaningfully solution within the greater AUD literature, despite the fit statistics indicating superior fit when adding more classes.
Table 2.
LCA model results table
| Model | df | AIC | SSABIC | Entropy | LMR (df) | p-value |
|---|---|---|---|---|---|---|
|
| ||||||
| 2-class | 1343 | 25159.65 | 25069.71 | 0.91 | ||
| 3-class | 1319 | 24082.16 | 23944.22 | 0.87 | 1075.93 | p < .001 |
| 4-class | 1295 | 23785.96 | 23600.02 | 0.82 | 329.05 | p < .001 |
| 5-class | 1271 | 23539.66 | 23305.72 | 0.81 | 281.34 | p < .001 |
| 6-class | 1247 | 23435.08 | 23153.14 | 0.83 | 145.86 | p < .001 |
df = degrees of freedom. AIC = Akaike Information Criteria, SSABIC = Sample Sized Adjusted Bayesian Information Criteria, LMR = Lo-Mendell-Rubin likelihood test statistic with degrees of freedom for that test in parentheses. p-value is the p-value for the LMR test.
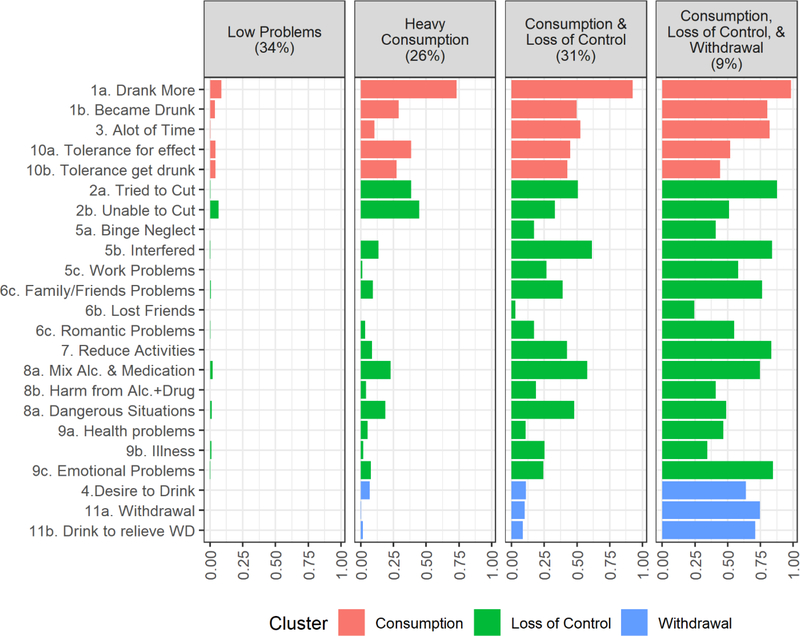
The four-class solutions consisted of the following classes (predicted probabilities for each class presented in supplementary Table 1 and visual representation in Figure 1): a “Low Problems” class (34% of sample) characterized by low probabilities of endorsing consumption items and extremely low probabilities of any other types of problems; a “Heavy Consumption” class (26%) characterized by low to moderate probabilities of endorsing consumption items, low probabilities of most loss of control items, and very low probabilities of withdrawal items; a “Consumption & Loss of Control ” class (31%) characterized by moderate to high probabilities of endorsing consumption items, low to moderate endorsement of loss of control items, and very low probability of withdrawal items; a “Consumption, Loss of Control, & Withdrawal” class (9%) characterized by moderate to very high probabilities of consumption items, moderate to high endorsement of loss of control items, and moderate to high endorsement of withdrawal items. The average latent class probabilities for each class were .95, .85, .90, .95 for the “Low Problems”, “Heavy Consumption”, “Consumption & Loss of Control”, and “Consumption, Loss of Control, & Withdrawal” classes, respectively.
Figure 1.
Item probabilities by latent class
See table 1 for unabbreviated items used in analyses. Items are listed on the y-axis. Each column (vertical panel) depicts a different identified latent class. Bars were colored based on what theoretical symptom cluster that item relates to.
Post-hoc LCA: Split-half replication
To examine the robustness of the identified solution, split-half replication was conducted by splitting the data into random halves (n=695) and the above LCA was repeated in each split-half (49). See supplementary tables 2 and 3 for fit statistics for both split-half LCAs and supplementary table 4 for agreement between class membership in the full-sample and split-half four-class solutions. See supplementary figures 3 and 4 for item probabilities from the four-class solution for each split-halves. Overall, split-half analyses supported the robustness of the four-class solution as essentially identical classes were uncovered in each split-half.
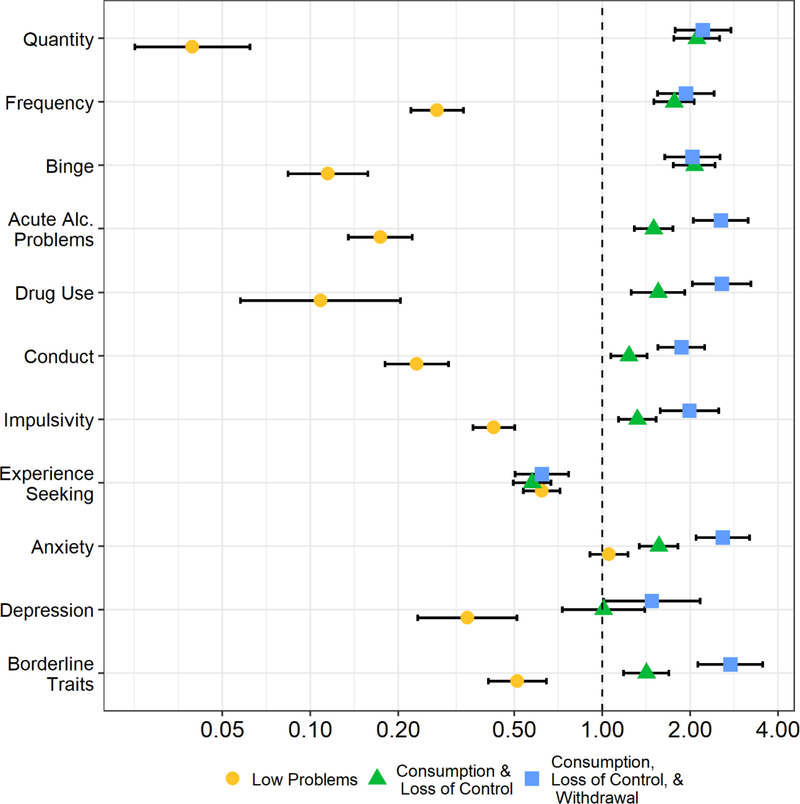
Multinomial regression results
Table 3 provides descriptive statistics and diagnostic breakdown by latent class. Table 4 provides Odds Ratios (OR) of each measure used in univariable multinomial regression with the “Heavy Consumption” group serving as the reference group. In summary, multinomial regressions indicated a general continuum of psychological dysfunction across identified classes, with the “Low Problems” group being significantly lower in almost all measures of alcohol consumption, other externalizing and internalizing problems, and BPD symptoms followed by the “Heavy Consumption”, then “Consumption & Loss of Control”, and then the “Consumption, Loss of Control, & Withdrawal” class. Figure 2 provides a visualization of ORs from analyses where all variables have been standardized and presented on a logarithmic scale for ease of interpretation.
Table 3.
Descriptives of measures broken down by latent class
| Measure | Low Problems | Heavy Consumption | Consumption and Harm | Consumption, Harm, and Dysfunction |
|---|---|---|---|---|
|
| ||||
| N (# female) | 471(259) | 363(171) | 433(192) | 123(52) |
| % AUD Dx. AUD Sx. | 1% .29 (1.00) | 94% 3.00 (2.00) | 100% 6.00 (2.00) | 100% 10.00 (2.00) |
| % Can. Dx. Can. Sx. | 10% 0.00 (0.00) | 48% 1.00 (4.00) | 60% 3.00 (6.00) | 70% 5.00 (7.50) |
| % Drug Dx. | 3% | 16% | 29% | 50% |
| % Talk to Professional | <1% | 8% | 17% | 43% |
| Age | 21.00 (3.00) | 21.00 (2.00) | 21.00 (2.00) | 22.00 (4.00) |
| Quantity per week | 2.00 (4.50) | 12.50 (15.88) | 22.50 (22.50) | 20.50 (26.63) |
| Frequency per week | 1.00 (1.00) | 2.00 (1.75) | 3.00 (2.00) | 3.50 (2.50) |
| Binge per week | 0.00 (0.50) | 1.00 (1.50) | 2.00 (2.00) | 2.00 (2.50) |
| Acute Problems α = .46 | 0.00 (0.00) | 1.00 (1.00) | 1.00 (1.00) | 2.00 (1.00) |
| Drug Use α = .96 | −0.39 (0.00) | −0.31 (0.24) | −0.19 (0.60) | 0.04 (2.38) |
| Impulsivity α = .82 | 4.00 (6.00) | 8.00 (7.00) | 10.00 (6.00) | 12.00 (5.00) |
| Experience Seeking α = .62 | 5.00 (3.00) | 6.00 (3.00) | 5.00 (4.00) | 5.00 (5.00) |
| Conduct Symptoms α = .75 | 0.00 (1.00) | 1.00 (3.00) | 2.00 (3.00) | 3.00 (5.00) |
| Trait Anxiety α = .90 | 37.00 (12.00) | 37.00 (11.00) | 42.00 (12.00) | 48.00 (11.00) |
| Depression α = .89 n = 492 | 1.00 (7.00) | 9.00 (10.00) | 9.00 (12.75) | 14.50 (15.00) |
| Borderline Traits α = .83 n = 860 | 1.00 (3.00) | 3.00 (4.75) | 4.00 (5.00) | 7.00 (4.50) |
Can. = cannabis, Sx. = # of symptoms endorsed, Dx. = % with DSM-V diagnosis, SD = standard deviation. Cells depict the median with the interquartile range (IQR) in parentheses. All descriptive statistics included the full sample (n = 1390), besides depression and borderline traits that have their respective sample sizes listed. α = Cronbach’s alpha.
Table 4.
Univariable multinomial regression results (odd ratios)
| Measure | Low Problems | Heavy Consumption | Consumption and Harm | Consumption, Harm, and Dysfunction |
|---|---|---|---|---|
|
| ||||
| Sex (female) | 1.37 [1.04, 1.81] p = .024 | - | .89 [.68, 1.18] p = .435 | .82 [ .54, 1.24] p = .353 |
| Can. Dx. | .11 [.07, .16] p < .001 | - | 1.57 [1.20, 2.10] p = .001 | 2.52 [1.63, 3.91] p < .001 |
| Drug Dx. | .13 [.07, .25] p < .001 | - | 2.07 [1.45, 2.92] p < .001 | 4.75 [3.02, 7.45] p < .001 |
| % Talk to Professional | .02 [.01, .18] p < .001 | - | 2.37 [1.51, 3.74] p < .001 | 8.72 [ 5.18, 14.68] p < .001 |
| Age | 1.03 [.97, 1.09] p = .397 | - | 1.07 [1.01, 1.13] p = .043 | 1.33 [1.23, 1.43] p < .001 |
| Quantity per week | .84 [.82, .86] p < .001 | - | 1.04 [1.03, 1.05] p < .001 | 1.04 [1.03, 1.06] p < .001 |
| Frequency per week | .45 [.40, .52] p < .001 | - | 1.41 [1.28, 1.55] p < .001 | 1.49 [1.30, 1.71] p < .001 |
| Binges per week | .21 [.16, .26] p < .001 | - | 1.7 [1.51, 1.92] p < .001 | 1.68 [1.43, 1.97] p < .001 |
| Acute Problems | .12 [.09, .17] p < .001 | - | 1.62 [1.35, 1.95] p < .001 | 3.06 [2.37, 3.97] p < .001 |
| Drug Use | .11 [.06, .2] p < .001 | - | 1.55 [1.26, 1.92] p < .001 | 2.57 [2.04, 3.23] p < .001 |
| Impulsivity | .84 [.81, .87] p < .001 | - | 1.06 [1.03, 1.09] p < .001 | 1.16 [1.10, 1.21] p < .001 |
| Experience Seeking | .82 [.78, .87] p < .001 | - | .80 [.75, .85] p < .001 | .82 [.76, .90] p < .001 |
| Conduct Symptoms | .51 [.45, .57] p < .001 | - | 1.1 [1.03, 1.18] p = .003 | 1.33 [1.22, 1.45] p < .001 |
| Trait Anxiety | 1.01 [.99, 1.02] p =.496 | - | 1.05 [1.03, 1.06] p < .001 | 1.11 [1.08, 1.13] p < .001 |
| Depression n = 492 | .89 [.85, .93] p < .001 | - | 1.00 [.97, 1.04] p = .954 | 1.05 [1.01, 1.09] p = .045 |
| Borderline Traits n = 860 | .82 [.77, .88] p < .001 | - | 1.11 [1.05, 1.17] p < .001 | 1.35 [1.25, 1.46] p < .001 |
Can. = cannabis Dx. = DSM-V diagnosis. Odds ratio (OR) from univariable multinomial regression (i.e., not adjusted for other covariates) with 95% confidence intervals in brackets presented in the 1st row of each cell. P-values are presented in the second row of each cell. All analyses included the full sample (n = 1390), besides depression and borderline traits that have their respective sample sizes listed. Alcohol use disorder (AUD) diagnoses could not be tested because several classes had 100% of individuals with AUD leading to issues with perfect prediction in the model.
Figure 2.
Odd ratios from univariable multinomial regression using standardized variables
Figure shows the odds ratio from univariable multinomial regression using standardized variables with the “Heavy Consumption” class as the reference category represented by the dotted line. Error bars depict the 95% confidence intervals. Odds ratios were plotted on a logarithmic scale for ease of interpretation. On a log scale, odd ratios are symmetrical. E.g., an OR of 1 is halfway between a ratio of .5 (half the risk) and a ratio of 2 (twice the risk).
DISCUSSION
Although the identified latent classes are consistent with an overall spectrum of increasing severity, the classes also showed differential patterns related to the symptom clusters of consumption, loss of control, and withdrawal. The “Low Problems” class consisted of individuals without AUD or significant AUD problems. The “Heavy Consumption” class consisted of individuals with predominantly mild (60%) and then moderate (33%) AUD diagnoses. Interestingly, this group was defined by predominantly endorsing items related to consumption such as tolerance or drinking more than intended (see Figure 1) and then showing low to moderate probability of only select loss of control items, specifically, difficulty cutting down (item 2a and 2b), mixing alcohol with medication (item 8a), and drinking in dangerous situations (item 8c). The “Heavy Consumption” class had very low probabilities of endorsing withdrawal symptoms or of endorsing significant social/obligation related issues and therefore do not necessarily wish to cut down due to significant global impairment, but perhaps other lower severity concerns (e.g., negative experiences while drinking). The “Consumption and Loss of Control” group was the first class to show significant levels of loss of control symptomology, however, they also had low endorsement of withdrawal symptoms. The last class labeled “Consumption, Loss of Control, & Withdrawal” was the only class to show moderate to high probabilities of symptoms across all symptom clusters. Importantly, the classes showed an additive pattern of increasing severity, where consumption symptoms are present at lower severity, followed by loss of control symptoms (with increasing endorsement of consumption symptoms), and then finally withdrawal symptoms (with increasing loss of control and consumption symptoms). Taken together, the current results partially support the DSM-V AUD formulation as results are consistent with a general spectrum of severity. However, this spectrum is not characterized by a simple linear increase in the probability of all criteria, but, in fact, qualitatively different presentations at increasing severity levels. Supplementary Figure 5 uses simulated data to provide a visual example of a simple linearly increasing spectrum of severity, where the probability of every criterion increases in unison across severity levels.
Multinomial regression indicated that the “Heavy Consumption” class (used as reference category in Figure 2) drank significantly more than the “Low Problems” class, but significantly less than the two higher severity classes. Measures of drinking behavior including quantity, frequency, and number of binges per week did not appear to vary between the two highest severity classes, perhaps indicating a ceiling effect. Measures of illicit drug use, conduct problems, and impulsive personality increased additively across the classes. Interestingly, the “Heavy Consumption” class was the highest in the experience-seeking personality trait, a result consistent with previous studies examining excitement-seeking and alcohol use (9, 12, 13). This may indicate that individuals with heavy use without severe problems see these behaviors as integrated into a broader and positive personality pattern of experience-seeking, whereas more impaired individuals may define themselves using more maladaptive traits (e.g., impulsive)(50). Internalizing measures did not discriminate as strongly between latent classes, in particular depression, which was only significantly lower in the “Low Problems” class. For trait anxiety, the “Low Problems” and “Heavy Consumption” classes were very similar, followed by the higher severity classes. BPD symptoms strongly discriminated between all groups, which is consistent with previous literature as borderline traits have demonstrated a strong statistical and theoretical relationship with externalizing problems (51, 52). Furthermore, a recent study demonstrated that BPD symptoms mediated the association between internalizing and substance use problems (53).
LCA provided important insights into assessing and modeling AUD symptoms. When examining the predicted probabilities across latent classes (Figure 1), we can consider conceptualizing AUD symptoms as having three subscales related to consumption, loss of control, and withdrawal. Firstly, our results are consistent with previous findings (4, 5) that many of the AUD symptoms can be satisfied by very different criteria in terms of content, but also severity. When examining the items related to AUD symptom six (i.e., continued alcohol use despite persistent or recurrent social problems), losing friends (item 6b) is exceptionally rare in all classes, except the highest severity class, whereas having problems with family/friends due to drinking (item 6a) is already moderately endorsed in the “Loss of Control” class. This highlights the importance of considering what items are present in different AUD assessments that are eventually aggregated into AUD symptoms (54). More broadly, it appears that the consumption symptoms provide significant information in discriminating between individuals with no symptoms and individuals with symptoms. However, as severity increases, especially in the two highest severity classes, consumption items provide minimal information. This is consistent with results examining measures of drinking behavior in multinomial regression. Loss of control symptoms showed an overall linear increase across classes. Lastly, the withdrawal symptoms distinguished the highest severity group from the lower classes but did not vary much among other classes.
These endorsement patterns may provide insights into the differential predictive validity of different AUD clusters reported in previous studies. Previous studies have demonstrated that consumption symptoms have lower predictive ability than the other symptom clusters (7, 10) and provide limited additional predictive power when other symptom clusters are included in the model (4). These results may be driven by the previously reviewed measurement considerations, specifically that moderate endorsement of consumption items is ubiquitous in individuals with AUD problems and therefore are of limited value in stratifying risk in higher severity samples, especially when other symptoms are available. Similarly, Wakefield & Schmitz (11) “harmful dysfunction” criteria requiring symptoms of both “harm” (similar to loss of control) and “dysfunction” (similar to withdrawal) clusters would essentially identify the highest severity class presented in the current study. This AUD presentation, consistent with their results, is certainly the most severe, while also being less common compared to lower severity presentations (9% of current sample). These individuals also, consistent with Wakefield & Schmitz (10), showed the highest endorsement of speaking to a professional about their drinking. Furthermore, similar to the “transient drinkers” identified in Wakefield & Schmitz (10) or the “Heavy Drinkers” identified in Lynskey et al., (18) there does appear a substantial minority of lower severity individuals with AUD who are characterized predominantly by symptoms related to excessive consumption. Importantly, these individuals showed significantly elevated levels of other externalizing psychopathology (i.e., drug use, conduct problems, acute alcohol problems) compared to controls, indicating that although these individuals are certainly less impaired than individuals with other AUD presentations, they still are a highly relevant population from a public health point-of-view. For example, although these individuals may be less likely to require hospitalization due to AUD, they are likely still at elevated risk for drinking related health problems or more acute issues like drunk-driving.
The current study should be interpreted in light of its limitations. Firstly, the sample was predominantly college-students and White and therefore results should be further investigated in more diverse samples. Relatedly, the young-adult sample may limit generalizability to more chronic and severe AUD presentations. Furthermore, research has shown that severity estimates of different AUD criteria can vary significantly between different AUD measures and diagnostic interviews (54), therefore, although the reported results are overall consistent with previous literature, results using different AUD measures should continue to be compared closely. Moreover, although we judged the four-class LCA solution as the most parsimonious and theoretically meaningful solution, the fit indices did not equivocally support retaining this model. Furthermore, the “Acute Alc. Problems” scale had below adequate internal reliability (α=.46) indicating these problems may be best examined separately in future studies. Additionally, the multinomial regressions did not include correction for classification error, which may lead to down-biased associations between class-membership and covariates (55). However, it is unlikely this has a large effect given the strong separation of the presented classes (55). Also, the performed multinomial regressions also did not control for the simultaneous effects of validating variables, therefore it might be possible that an unmeasured, third variable can explain the relationships between the validating variables and class memberships. Lastly, given the cross-sectional nature of the current study it is not possible to comment on the trajectories represented in these classes. It is possible, for example, that the “Heavy Consumption” pattern is an earlier developmental stage for some individuals before progressing into more severe manifestations.
We believe the current results, in conjunction with previous findings, support the importance of several meaningful symptom clusters within AUD. Interestingly, although the identified symptom clusters were consistent with an increasing spectrum of severity, there appeared to be qualitatively different presentations of AUD at varying severity levels. This has significant clinical implications. For example, clinicians should be aware that individuals with lower severity AUD may benefit most from harm-reduction interventions (56) that target common problems associated with heavy consumption compared to an anti-craving intervention given that it is unlikely to be a common symptom in that sample. Moreover, the current results provide some useful insights into the etiology of AUD. It is possible that the loss of control and withdrawal symptom clusters are somewhat dependent on the existence of consumption symptoms. For example, the interaction of heavy/habitual alcohol consumption and other risk factors may lead to the introduction of other clusters of symptoms (e.g., physiological dependence) and the solidification of a more severe form of AUD. Therefore, individuals identified as “just” heavy drinkers, may be of particular value for early prevention efforts. Furthermore, given that previous research on these symptom clusters have identified disparate genetic risk, differential associations with personality, and now qualitatively different AUD presentation, it is possible that more severe AUD is best characterized as the intersection of two separate, but correlated, liabilities. It is possible that all individuals with AUD can be characterized by having strong approach tendencies leading to heavy consumption, but perhaps only some have additional liabilities that lead to loss control and a more impairing presentation. We believe, consistent with Watts et al., (4), that researchers should recognize the mounting evidence supporting the importance of these symptom clusters to understanding and assessing AUD. Lastly, as researchers continue to embrace dimensional approaches to psychopathology, it will be necessary to rigorously examine and describe these spectra.
Supplementary Material
Financial Support:
This research was supported by National Institutes of Alcohol Abuse and Alcoholism grant [R01AA13650] to Peter Finn, National Institutes of Drug Abuse (NIDA) grant [T32 DA24628] Lindy Howe and Allen Bailey, National Institutes of Health grant [T32 MH103213] to Allen Bailey, and National Institutes of Alcohol Abuse and Alcoholism [T32 AA07462] grant to Polly Ingram.
Footnotes
Conflict of interest declaration: None
REFERENCES
- 1.Hasin DS, Auriacombe M, Borges G, Bucholz K, Budney A, Crowley T, et al. The DSM5 field trials and reliability of Alcohol Use Disorder. The American journal of psychiatry. 2013;170(4):442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mewton L, Slade T, McBride O, Grove R, Teesson M. An evaluation of the proposed DSM-5 alcohol use disorder criteria using Australian national data. Addiction. 2011;106(5):941–50. [DOI] [PubMed] [Google Scholar]
- 3.Gelhorn H, Hartman C, Sakai J, Stallings M, Young S, Rhee SH, et al. Toward DSM-V: an item response theory analysis of the diagnostic process for DSM-IV alcohol abuse and dependence in adolescents. Journal of the American Academy of Child & Adolescent Psychiatry. 2008;47(11):1329–39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Watts AL, Boness CL, Loeffelman JE, Steinley D, Sher KJ. Does crude measurement contribute to observed unidimensionality of psychological constructs? An example with DSM-5 alcohol use disorder. 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lane SP, Sher KJ. Limits of current approaches to diagnosis severity based on criterion counts: An example with DSM-5 alcohol use disorder. Clinical Psychological Science. 2015;3(6):819–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Hyman SE. The diagnosis of mental disorders: the problem of reification. Annual review of clinical psychology. 2010;6:155–79. [DOI] [PubMed] [Google Scholar]
- 7.Kendler K, Aggen S, Prescott C, Crabbe J, Neale M. Evidence for multiple genetic factors underlying the DSM-IV criteria for alcohol dependence. Molecular psychiatry. 2012;17(12):1306–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Muthen BO, Grant B, Hasin D. The dimensionality of alcohol abuse and dependence: factor analysis of DSM-III-R and proposed DSM-IV criteria in the 1988 National Health Interview Survey. Addiction. 1993;88(8):1079–90. [DOI] [PubMed] [Google Scholar]
- 9.Mustanski BS, Viken RJ, Kaprio J, Rose RJ. Genetic influences on the association between personality risk factors and alcohol use and abuse. Journal of Abnormal Psychology. 2003;112(2):282. [DOI] [PubMed] [Google Scholar]
- 10.Wakefield JC, Schmitz MF. The harmful dysfunction model of alcohol use disorder: revised criteria to improve the validity of diagnosis and prevalence estimates. Addiction. 2015;110(6):931–42. [DOI] [PubMed] [Google Scholar]
- 11.Wakefield JC, Schmitz MF. How many people have alcohol use disorders? Using the harmful dysfunction analysis to reconcile prevalence estimates in two community surveys. Frontiers in Psychiatry. 2014;5:10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Finn PR. Motivation, working memory, and decision making: A cognitive-motivational theory of personality vulnerability to alcoholism. Behavioral and cognitive neuroscience reviews. 2002;1(3):183–205. [DOI] [PubMed] [Google Scholar]
- 13.Gunn RL, Finn PR, Endres MJ, Gerst KR, Spinola S. Dimensions of disinhibited personality and their relation with alcohol use and problems. Addictive behaviors. 2013;38(7):2352–60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Müller M, Ajdacic-Gross V, Vetrella AB, Preisig M, Castelao E, Lasserre A, et al. Subtypes of alcohol use disorder in the general population: A latent class analysis. Psychiatry research. 2020;285:112712. [DOI] [PubMed] [Google Scholar]
- 15.Babor TF, Hofmann M, DelBoca FK, Hesselbrock V, Meyer RE, Dolinsky ZS, et al. Types of alcoholics, I: Evidence for an empirically derived typology based on indicators of vulnerability and severity. Archives of general psychiatry. 1992;49(8):599–608. [DOI] [PubMed] [Google Scholar]
- 16.Cloninger CR, Bohman M, Sigvardsson S. Inheritance of alcohol abuse: Cross-fostering analysis of adopted men. Archives of general psychiatry. 1981;38(8):861–8. [DOI] [PubMed] [Google Scholar]
- 17.Hesselbrock VM, Hesselbrock MN. Are there empirically supported and clinically useful subtypes of alcohol dependence? Addiction. 2006;101:97–103. [DOI] [PubMed] [Google Scholar]
- 18.Lynskey MT, Nelson EC, Neuman RJ, Bucholz KK, Madden PA, Knopik VS, et al. Limitations of DSM-IV operationalizations of alcohol abuse and dependence in a sample of Australian twins. Twin Research and Human Genetics. 2005;8(6):574–84. [DOI] [PubMed] [Google Scholar]
- 19.Finn PR, Gunn RL, Gerst KR. The Effects of a Working Memory Load on Delay Discounting in Those with Externalizing Psychopathology. Clin Psychol Sci. 2015;3(2):202–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Connor JP, Gullo MJ, White A, Kelly AB. Polysubstance use: diagnostic challenges, patterns of use and health. Current opinion in psychiatry. 2014;27(4):269–75. [DOI] [PubMed] [Google Scholar]
- 21.Bucholz KK, Cadoret R, Cloninger CR, Dinwiddie SH, Hesselbrock V, Nurnberger J Jr, et al. A new, semi-structured psychiatric interview for use in genetic linkage studies: a report on the reliability of the SSAGA. Journal of studies on alcohol. 1994;55(2):149–58. [DOI] [PubMed] [Google Scholar]
- 22.White AM, Hingson RW, Pan I-J, Yi H-Y. Hospitalizations for alcohol and drug overdoses in young adults ages 18–24 in the United States, 1999–2008: results from the Nationwide Inpatient Sample. Journal of studies on alcohol and drugs. 2011;72(5):774–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.White AM, Jamieson-Drake DW, Swartzwelder HS. Prevalence and correlates of alcohol-induced blackouts among college students: Results of an e-mail survey. Journal of American College Health. 2002;51(3):117–31. [DOI] [PubMed] [Google Scholar]
- 24.Beck KH, Kasperski SJ, Caldeira KM, Vincent KB, O’Grady KE, Arria AM. Trends in alcohol-related traffic risk behaviors among college students. Alcoholism: Clinical and Experimental Research. 2010;34(8):1472–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Palk G, Davey J, Freeman J. Prevalence and characteristics of alcohol-related incidents requiring police attendance. Journal of Studies on Alcohol and Drugs. 2007;68(4):575–81. [DOI] [PubMed] [Google Scholar]
- 26.Bailey AJ, Finn PR. Examining the Utility of a General Substance Use Spectrum Using Latent Trait Modeling. Drug and alcohol dependence. 2020;212:107998. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bailey AJ, Farmer EJ, Finn PR. Patterns of polysubstance use and simultaneous co-use in high risk young adults. Drug and alcohol dependence. 2019;205:107656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Browne MW, Arminger G. Specification and estimation of mean-and covariance-structure models. Handbook of statistical modeling for the social and behavioral sciences: Springer; 1995. p. 185–249. [Google Scholar]
- 29.Rosseel Y lavaan: an R package for structural equation modeling and more Version 0.4–9 (BETA). Retrieved from. 2011.
- 30.Browne MW, Cudeck R. Alternative ways of assessing model fit. Sociological methods & research. 1992;21(2):230–58. [Google Scholar]
- 31.Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological bulletin. 1980;88(3):588. [Google Scholar]
- 32.Skrondal A, Rabe-Hesketh S. Generalized latent variable modeling: Multilevel, longitudinal, and structural equation models: Crc Press; 2004. [Google Scholar]
- 33.Eysenck SB, Pearson PR, Easting G, Allsopp JF. Age norms for impulsiveness, venturesomeness and empathy in adults. Personality and individual differences. 1985;6(5):613–9. [Google Scholar]
- 34.Zuckerman M Beyond the optimal level of arousal. Hillsdale, NJ: Lawrence Erlbraum Associates. 1979. [Google Scholar]
- 35.Spielberger CD. Manual for the State-Trait Anxiety Inventory STAI (form Y)(“ self-evaluation questionnaire”). 1983.
- 36.Beck AT, Steer RA, Brown G. Beck depression inventory–II. Psychological Assessment. 1996. [Google Scholar]
- 37.First MB, Spitzer RL, Gibbon M, Williams JB, Davies M, Borus J, et al. The structured clinical interview for DSM-III-R personality disorders (SCID-II). Part II: Multi-site test-retest reliability study. Journal of personality disorders. 1995;9(2):92–104. [Google Scholar]
- 38.Team RC. R: A language and environment for statistical computing. 2013. [Google Scholar]
- 39.Linzer DA, Lewis JB. poLCA: An R package for polytomous variable latent class analysis. Journal of statistical software. 2011;42(10):1–29. [Google Scholar]
- 40.Yee TW. Vector generalized linear and additive models: with an implementation in R: Springer; 2015. [Google Scholar]
- 41.Stekhoven DJ, Bühlmann P. MissForest—non-parametric missing value imputation for mixed-type data. Bioinformatics. 2012;28(1):112–8. [DOI] [PubMed] [Google Scholar]
- 42.Wickham H Elegant graphics for data analysis (ggplot2). Appl Spatial Data Anal R. 2009. [Google Scholar]
- 43.Waljee AK, Mukherjee A, Singal AG, Zhang Y, Warren J, Balis U, et al. Comparison of imputation methods for missing laboratory data in medicine. BMJ open. 2013;3(8). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Dempster AP, Laird NM, Rubin DB. Maximum likelihood from incomplete data via the EM algorithm. Journal of the Royal Statistical Society: Series B (Methodological). 1977;39(1):1–22. [Google Scholar]
- 45.Sclove SL. Application of model-selection criteria to some problems in multivariate analysis. Psychometrika. 1987;52(3):333–43. [Google Scholar]
- 46.Celeux G, Soromenho G. An entropy criterion for assessing the number of clusters in a mixture model. Journal of classification. 1996;13(2):195–212. [Google Scholar]
- 47.Lo Y, Mendell NR, Rubin DB. Testing the number of components in a normal mixture. Biometrika. 2001;88(3):767–78. [Google Scholar]
- 48.Westreich D, Greenland S. The table 2 fallacy: presenting and interpreting confounder and modifier coefficients. American journal of epidemiology. 2013;177(4):292–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Shireman EM, Steinley D, Sher K. Sex differences in the latent class structure of alcohol use disorder: Does (dis) aggregation of indicators matter? Experimental and clinical psychopharmacology. 2015;23(4):291. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Pettersson E, Mendle J, Turkheimer E, Horn EE, Ford DC, Simms LJ, et al. Do maladaptive behaviors exist at one or both ends of personality traits? Psychological assessment. 2014;26(2):433. [DOI] [PubMed] [Google Scholar]
- 51.James LM, Taylor J. Revisiting the structure of mental disorders: Borderline personality disorder and the internalizing/externalizing spectra. British Journal of Clinical Psychology. 2008;47(4):361–80. [DOI] [PubMed] [Google Scholar]
- 52.Bailey AJ, Finn PR. Borderline personality disorder symptom comorbidity within a high externalizing sample: Relationship to the internalizing-externalizing dimensional structure of psychopathology. Journal of personality disorders. 2020;34(6):814–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Howe LK, Fisher LR, Atkinson EA, Finn PR. Symptoms of anxiety, depression, and borderline personality in alcohol use disorder with and without comorbid substance use disorder. Alcohol. 2021;90:19–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lane S, Steinley D, Sher K. Meta-analysis of DSM alcohol use disorder criteria severities: structural consistency is only ‘skin deep’. Psychological medicine. 2016;46(8):1769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Vermunt JK. Latent class modeling with covariates: Two improved three-step approaches. Political analysis. 2010;18(4):450–69. [Google Scholar]
- 56.Ritter A, Cameron J. A review of the efficacy and effectiveness of harm reduction strategies for alcohol, tobacco and illicit drugs. Drug and alcohol review. 2006;25(6):611–24. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.