Abstract
Due to its excellent diagnostic performance, CT is the mainstay of diagnostic test in adults with suspected acute appendicitis in many countries. Although debatable, extensive epidemiological studies have suggested that CT radiation is carcinogenic, at least in children and adolescents. Setting aside the debate over the carcinogenic risk of CT radiation, the value of judicious use of CT radiation cannot be overstated for the diagnosis of appendicitis, considering that appendicitis is a very common disease, and that the vast majority of patients with suspected acute appendicitis are adolescents and young adults with average life expectancies. Given the accumulated evidence justifying the use of low-dose CT (LDCT) of only 2 mSv, there is no reasonable basis to insist on using radiation dose of multi-purpose abdominal CT for the diagnosis of appendicitis, particularly in adolescents and young adults. Published data strongly suggest that LDCT is comparable to conventional dose CT in terms of clinical outcomes and diagnostic performance. In this narrative review, we will discuss such evidence for reducing CT radiation in adolescents and young adults with suspected appendicitis.
Keywords: Appendicitis, Evidence-based practice, Multidetector computed tomography, Radiation dosage
INTRODUCTION
CT radiation is arguably carcinogenic [1,2,3,4,5]. Concerns about carcinogenic risk have prompted attempts to reduce CT radiation exposure used for the diagnosis of appendicitis. Some researchers have concluded that low-dose appendiceal CT (LDCT) should be implemented in all emergency departments and clinical trials [6,7]. However, the adoption of LDCT is disappointingly slow. A survey [8] in 2016 showed that care providers were still concerned that the low image quality with LDCT may lead to incorrect diagnoses. It is disappointing that some care providers are still unaware of or disregard previous study results showing that LDCT is comparable to conventional dose CT (CDCT). The discrepancy between science and practice is attributable to care providers’ defensive natures, preferring cleaner CT images to noisy LDCT images. Once medical treatments become universally accepted in clinical practice, their use becomes very difficult to modify, even if proven ineffective or even harmful [9].
To bridge this discrepancy, this narrative review aims to provide care providers with a neutral and critical assessment of evidence for reducing CT radiation in adolescents and young adults with suspected appendicitis.
Current CT Utilization
Patients with appendicitis typically present with right lower quadrant tenderness, pain, abdominal rigidity, and pain migration to the right lower quadrant. However, diagnosis using only clinical features and laboratory tests is often limited [10,11] because most patients with appendicitis do not have typical presentations, while other diseases can mimic appendicitis clinically. Therefore, the use of preoperative imaging tests in patients with suspected appendicitis is now accepted as standard practice in many developed countries [12,13]. Although there have been historical debates [14], ample evidence suggests that utilization of preoperative imaging, particularly CT, prevents unnecessary appendectomy (i.e., unnecessary removal of the uninflamed appendix) without increasing appendiceal perforation [15].
In many countries, CT is the mainstay of diagnostic imaging in adults with suspected appendicitis. Previous meta-analyses [16,17,18] drew consistent conclusions that CT outperforms ultrasonography in the diagnosis of appendicitis. Due to its excellent diagnostic performance, CT is utilized 10–15 times more frequently than ultrasonography in the United States [19] and South Korea [20,21]. In contrast, in some European regions [22,23,24], ultrasonography is widely used, while CT is reserved for patients with inconclusive ultrasonography results. Recently, magnetic resonance imaging has been introduced for the diagnosis of appendicitis, showing high reported diagnostic sensitivities and specificities often exceeding 95% [25]. However, it is yet to be determined whether these promising results can be generalized to most hospitals and different healthcare systems due to the variability of magnetic resonance imaging availability, accuracy, and feasibility in acute care settings.
CT Radiation Dose
The term diagnostic reference levels (DRLs) have been used to refer to the “representative” dose of a given CT application in a population. DRL is typically defined as the third quartile of doses collected across CT machines and hospitals [26]. The unit of radiation dose used in this study is the effective dose (in mSv), which is a general measure of the detrimental effect of ionizing radiation often used for comparing imaging studies or justifying the use of an imaging study [27]. Hereafter, we use “conventional dose” to refer a radiation dose near the DRL which is typically 7 mSv or higher [28,29,30,31,32], and “low dose” to refer a dose considerably lower than the DRL.
There have been only limited data on the DRL of CT examinations dedicated to the diagnosis of appendicitis. However, some large-scale data are available regarding DRLs used for multi-purpose abdominal CT examination in adults, which is presumably the same scanning protocol used for adults with suspected appendicitis in many hospitals. The reported DRLs from various countries in 2000–2020 range from 460 mGy·cm to 880 mGy·cm in dose-length product [28,29,30,31,32], which corresponds to effective doses of 7–13 mSv with a conversion factor of 0.015 mSv/mGy·cm [33].
Reported CT radiation doses used for the evaluation of suspected appendicitis vary widely depending on the region, hospitals, and CT machines. In a survey involving 14 US hospitals in 2004–2005 [34], most of the hospitals used fixed tube-current time products ranging from 160 mAs to 380 mAs with a peak tube potential of 120 kVp or 140 kVp, while few hospitals used automatic exposure control techniques. A survey [20] involving 22 CT machines in 11 South Korean hospitals in 2011 found a surprisingly wide variation in dose, ranging from 2 mSv to over 20 mSv. The variation was partly attributable to the use of multi-phase scanning in some hospitals, despite the lack of a rationale for using multi-phase scans for the diagnosis of appendicitis. A European survey [35] involving 19 hospitals in 14 countries in 2018–2019 also reported considerable inter- and within-hospital variations in radiation dose, which was again attributable to multi-phase scanning in a substantial portion of patients. In the European survey, the DRL was 874 mGy·cm in the dose-length product (corresponding to an effective dose of 13 mSv) for a CT examination and 498 mGy·cm (corresponding to 7 mSv) for a contrast-enhancement phase.
In 2004, Keyzer et al. [36] first reported the use of LDCT (approximately 2 mSv) for the diagnosis of appendicitis in adults. In subsequent studies comparing LDCT and CDCT [37,38,39,40,41,42,43], the tested low dose ranged from 1 mSv to 4 mSv, while the tested conventional dose ranged from 5 mSv to 10 mSv, with a 2–6 fold difference between the low and conventional doses within each of the studies. In recent comparative studies [41,42,43,44], the tested low dose ranged from 1 to 2 mSv, which was similar to the radiation level tested by Keyzer et al. [36]. In non-comparative studies that explored the usefulness of LDCT in the diagnosis of appendicitis [45,46], the tested low dose also ranged from 1 to 2 mSv, which is close to the worldwide average annual exposure to natural radiation sources [47] or dose of three conventional abdominal radiographs [27]. Park et al. [48] tested even lower doses (i.e., sub-mSv levels) for appendiceal CT using an iterative reconstruction technique.
Carcinogenic Risk of CT Radiation
Even if the carcinogenic risk for an individual patient is assumed to be very small, the risk projected to a very large population may render a real risk of cancer [49]. This concern is based on the following epidemiological knowledge. First, a vast number of patients undergo appendiceal CT worldwide due to the high incidence of appendicitis and the popularity of CT. Second, among those exposed to CT radiation, patients who turn out to have a normal appendix heavily outnumber patients confirmed to have appendicitis, particularly in the regions where appendiceal CT is popular [50]. Third, a substantial portion of the patients suspected of having appendicitis are adolescents and young adults with average life expectancies, and are intrinsically more vulnerable to the carcinogenic risk of radiation compared to older patients.
Epidemiological Studies
There has been only one epidemiological study [5] on the carcinogenic risk of CT radiation specifically used for the diagnosis of appendicitis. This was a nationwide population-based cohort study in South Korea that included more than eight hundred thousand children and adults who underwent appendectomy. The study concluded that exposure to CT radiation was associated with a higher incidence of hematologic malignancies (incidence rate ratio between CT-exposed versus CT-unexposed group, 1.26). The increase in incidence was more pronounced in children (incidence rate ratio, 2.14) than in adults. Unlike previous epidemiologic studies [1,2], the Korean cohort study was designed to account for reverse causation and confounding by specifying the indication for CT examination (i.e., diagnosing appendicitis).
In terms of CT examinations not confined to the diagnosis of appendicitis, extensive epidemiological studies [1,2,3,4] have suggested that radiation is carcinogenic, particularly in children and adolescents. A United Kingdom cohort study [1] reported that cumulative organ doses of 50–60 mGy triple the risk of leukemia and brain cancer. An Australian cohort study [2] showed that CT radiation exposure is associated with an increase of 20% or more in cancer risk. Unlike the Korean cohort study [5], these studies did not specify the indications for CT examinations. The reported carcinogenic risk may have been overestimated, as some of the CT examinations may have been performed in patients with preexisting but yet undetectable cancer (reverse causation), or in patients with conditions that confer the risk of cancer (confounding by indication) [51]. A French cohort study [52] claimed that adjustment for confounders (i.e., cancer-predisposing factors) may mitigate the overestimation of carcinogenic risk. The upcoming study—Epidemiological study to quantify risks for paediatric computerized tomography and to optimise doses (EPI-CT) [53]—will offer an opportunity for a better understanding of the potential risk of CT radiation.
Modeling Studies
Sex- and organ-specific lifetime excess incidence of radiation-induced cancer can be estimated using risk models, such as the biological effects of the ionizing radiation VII model [54]. A similar simulation method has been used in landmark studies to estimate the carcinogenic risk associated with CT radiation [49]. However, it should be noted that risk projection involves unverified assumptions and that the methods of estimating carcinogenic risk are still evolving. Using the risk projection model, Kim et al. [41] estimated that exposure to 2-mSv CT at the age of 30 years would result in a lifetime excess risk of 14 and 16 cancers per 100000 male and female patients, respectively, while exposure to 8-mSv CT would result in 63 and 72 cancers, respectively. These estimates imply that using 2 mSv instead of 8 mSv in an estimated 2000 male or 1800 female patients aged 30 years would eventually prevent one case of cancer.
In contrast, a decision analysis study [55] suggested that the choice of imaging modality between CT and others (combined ultrasonography and CT, or magnetic resonance imaging) for the diagnosis of appendicitis would affect life expectancy only minimally. For example, a 20-year-old male would have a life-expectancy loss of 5.8, 6.8, and 8.2 days by using magnetic resonance imaging, combined ultrasonography and CT, and CT, respectively. The small differences in the life-expectancy loss among different imaging modalities could be attributed to the very low incidence of radiation-induced cancer. If the fatality is diluted in a large base of the population, the average individual loss in life expectancy would be small.
Diagnostic Effectiveness and Efficacy: LDCT vs. CDCT
Critical Appraisal of Previous Studies
Previous studies investigating the diagnostic effectiveness or efficacy of LDCT should be critically appraised with three important viewpoints that have not been sufficiently addressed in previous reviews [56,57,58,59]. First, most of the studies were prone to potential biases intrinsic to their retrospective nature. Therefore, the biases must have affected the meta-analyses [56,57,58,59] regarding the diagnostic performance. Except for two prospective randomized controlled trials [41,43], the remaining studies mostly featured multi-reader multi-case designs for intra-patient pair-wise comparisons of two serial CT scans [36,38,39,42,60] or dose simulations [37]. One study [40] retrospectively analyzed official CT reports using a before-and-after design.
Second, all but one study were single-center studies conducted by a small number of expert radiologists motivated toward the use of LDCT, which raises concerns about the generalizability of the study results. In a pragmatic clinical trial [43,61], 20 hospitals with little prior experience in LDCT successfully delivered 2-mSv CT practice to over 1500 adolescents and young adults. Even for the trial, the generalizability of the study results is still uncertain from a strict viewpoint, since all the participating sites were teaching hospitals, only a third of the eligible patients were randomly assigned, and the catchment area was limited to South Korea.
Third, clinical outcomes were assessed in only two randomized controlled trials [41,43]. Other studies were limited to the assessment of diagnostic performance or inter-observer agreement, which are all intermediate outcomes that may be decoupled from more ultimate outcomes [62].
Clinical Outcomes and Diagnostic Performance
The primary clinical outcomes measured in the two trials [41,43] were negative appendectomy rate (i.e., the percentage of uninflamed appendices out of all non-incidental appendectomies) and appendiceal perforation rate (i.e., the percentage of perforated appendicitis out of all cases of confirmed appendicitis). Negative appendectomy indicates the clinical consequence of a false-positive diagnosis of appendicitis, whereas appendiceal perforation is associated with a delayed (or false-negative) diagnosis. The two reciprocal endpoints have been commonly used as quality indices in the management of patients with suspected appendicitis [63,64,65], and in the overall patient access to emergency medical care [66].
In one of the two trials, which was a single-center study [41], the 2-mSv group was non-inferior to the 8-mSv group in terms of negative appendectomy rate (3.5% vs. 3.2%), while the appendiceal perforation rate was comparable between the two groups (26.5% vs. 23.3%). To test the generalizability of the single-center trial results, Korean researchers conducted another multi-center pragmatic trial [43,67,68] involving 20 hospitals with little prior experience with LDCT [69]. A total of 3074 adolescents and young adults were randomized to undergo 2-mSv CT or CDCT (≤ 8 mSv). Again, the two groups were comparable in terms of negative appendectomy rate (3.9% vs. 2.7%), appendiceal perforation rate (34.7% vs. 31.2%), the need for additional imaging tests, or delay in patient disposition. An example LDCT protocol used in the Korean multicenter trial is detailed in the Supplementary Table 1.
Several studies have directly compared the diagnostic performance of LDCT and CDCT as the first line imaging test in adolescents and young adults with suspected appendicitis (Table 1). The studies were conducted mainly in South Korea [38,40,41,42,43] and Europe [36,37,39,60]. Importantly, the studies consistently reported that LDCT is comparable to CDCT with respect to the area under the receiver operating characteristic curve, sensitivity, and specificity. Recent meta-analyses [56,57,58,59] of randomized [41] and non-randomized [36,37,38,39,40,42] studies that used different CT imaging protocols have also shown similar results.
Table 1. Studies that Directly Compared Low- and Conventional-Dose CTs as First-Line Imaging Test for Diagnosing Appendicitis.
| Study | Comparison | Study Type* | Population/Sample | Results | ||||
|---|---|---|---|---|---|---|---|---|
| Low-Dose CT/Contrast Material | Conventional-Dose CT/Contrast Material | Age (Years) | Clinical Presentation†‡ | Sample Size§ | Outcome | Low-Dose CT vs. Conventional-Dose CT | ||
| Keyzer et al. 2004 [36] Radiology | 1–2 mSv | 5–7 mSv | Retrospectiveǁ | 16–74 | NS | 29/95¶ | AUC | 0.92–0.93 vs. 0.91–0.93 |
| None | None | Scan each patient twice | Sensitivity, % | 97–100 vs. 97–100 | ||||
| MRMC (2 readers) | Specificity, % | 80–94 vs. 82–94 | ||||||
| Keyzer et al. 2009 [37] AJR Am J Roentgenol | 30 mAs eff and 120 kVp (simulated**) | 100 mAseff and 120 kVp | Retrospectiveǁ | 18–87 | NS | 33/131 †† | With IV contrast | |
| With or without oral†† | With or without oral†† | Dose simulation | Sensitivity, % | 76–88 vs. 91 | ||||
| MRMC (2 readers) | Specificity, % | 98–99 vs. 97–99 | ||||||
| Without IV contrast | ||||||||
| Sensitivity, % | 82–91 vs. 79–82 | |||||||
| Specificity, % | 90–95 vs. 95 | |||||||
| Seo et al. 2009 [38] AJR Am J Roentgenol | 4 mSv | 8 mSv | Retrospective | 15–83 | Typical and atypical | 78/207¶ | AUC | 0.98–0.99 vs. 0.97–0.98 |
| None | IV | Scan each patient twice | Sensitivity, % | 98.7–100 vs. 100 | ||||
| MRMC (2 readers) | Specificity, % | 95.3–96.9 vs. 93–96.9 | ||||||
| Platon et al. 2009 [39] Eur Radiol | 1–2 mSv | 7–10 mSv | Retrospectiveǁ | 18–96 | NS | 37/86¶ | Sensitivity, % | 95 vs. 100 |
| Oral | Oral and IV | Scan each patient twice | Specificity, % | 96 vs. 96 | ||||
| MRMC (2 readers) | ||||||||
| Kim et al. 2011 [40] Radiology | 2 mSv | 8 mSv | Retrospective | 15–40 | Typical and atypical | 95/257‡‡ | NAR, % | 4.5 vs. 1.9 |
| IV | IV | Prospective image interpretation | APR, % | 33 vs. 13 | ||||
| Before-and-after design | AUC | 0.96 vs. 0.97 | ||||||
| Sensitivity, % | 90 vs. 89 | |||||||
| Specificity, % | 92 vs. 94 | |||||||
| Kim et al. 2012 [41] N Engl J Med | 2 mSv | 8 mSv | Prospective | 15–44§§ | Typical and atypical | 346/891‡‡ | NAR, % | 3.5 vs. 3.2 |
| IV | IV | RCT | APR, % | 26.5 vs. 23.3 | ||||
| AUC | 0.97 vs. 0.98 | |||||||
| Sensitivity, % | 94.5 vs. 95.0 | |||||||
| Specificity, % | 93.3 vs. 93.8 | |||||||
| Kim et al. 2015 [42] Acta Radiol | 2 mSv | 4 mSv | Retrospectiveǁ | 15–82 | NS | 58/102¶ | AUC | 0.96–0.97 vs. 0.93–0.97 |
| IV (portal phase) | IV (arterial phase) | Scan each patient twice | ||||||
| IR | FBP | MRMC (2 readers) | ||||||
| LOCAT Group 2017 [43] Lancet Gastroenterol Hepatol | 2 mSv | 8 mSv | Prospective | 15–44§§ | Typical and atypical | 1088/3074‡‡ | NAR, % | 3.9 vs. 2.7 |
| IV | IV | RCT | APR, % | 34.7 vs. 31.2 | ||||
| AUC | 0.983 vs. 0.986 | |||||||
| Sensitivity, % | 97.1 vs. 98.0 | |||||||
| Specificity, % | 95.8 vs. 94.0 | |||||||
| Sippola et al. 2020 [60] Ann Surg | 3 mSv | 4 mSv | Prospective | 18–60 | NS | 49/57¶ | Accuracy, % | 79 vs. 80 |
| IV | IV | Scan each patient twice | ||||||
| MRMC (2 readers) | ||||||||
*All studies except for that by the LOCAT Group were single-institutional studies, †In all studies, clinical presentation was described as suspected appendicitis, ‡If patients with typical presentation and/or patients with atypical presentation of appendicitis were included, §Number of confirmed appendicitis/number of patients undergoing CT, ∥Patients were included prospectively, but images were reviewed retrospectively, ¶Each patient underwent low- and then conventional-dose CTs, **Low-dose CT was simulated by adding noise to original scans, ††Patients were randomized into oral-contrast or no-oral-contrast group. Each patient underwent conventional-dose CT before and after IV contrast enhancement, ‡‡Each patient underwent either low- or conventional-dose, §§Inclusion criteria. APR = appendiceal perforation rate, AUC = area under the receiver operating characteristic curve, FBP = filtered back-projection, IR = iterative reconstruction, IV = intravenous, mAseff = effective mAs, MRMC = multireader multicase, NAR = negative appendectomy rate, NS = not specified, RCT = randomized controlled trial
However, the reported diagnostic performance may have been inflated due to verification biases, because in all the studies, histopathologic confirmation of appendicitis was selectively obtained in patients with positive CT results [41,43]. Furthermore, the bias may have occurred differently in the LDCT and CDCT groups, even in the randomized controlled trials, due to the imbalance in the number of appendectomies [43].
Complicated vs. Uncomplicated Appendicitis
Recent clinical trials [70,71,72,73,74] have shown the potential of non-surgical antibiotic treatment as an alternative to surgery for appendicitis in patients presumed to have uncomplicated appendicitis. The ongoing shift of surgical threshold from appendicitis vs. non-appendicitis to complicated vs. uncomplicated appendicitis poses a new diagnostic challenge of differentiating complicated from uncomplicated appendicitis [75]. The motivation is to triage patients, thereby applying the option of non-surgical treatment selectively to patients with uncomplicated appendicitis while performing emergency appendectomy in patients with complicated appendicitis [76].
The data from several previous studies [38,40,41] indirectly suggest that LDCT is comparable to CDCT for the diagnosis of perforated appendicitis, although few studies have directly addressed this issue. A post hoc analysis [77] of the Korean multicenter trial data [43] suggested that 2-mSv CT and CDCT (≤ 8 mSv) were comparable for correct detection and false detection of perforated appendicitis. A Finnish study [60] also reported comparable diagnostic accuracy of a LDCT protocol (3 mSv) to a standard CT protocol (4 mSv) in differentiating between uncomplicated and complicated appendicitis.
However, regardless of the radiation dose, CT has limited sensitivity in differentiating complicated appendicitis from uncomplicated appendicitis [78]. Based on data from the Korean multi-center trial [43] comparing 2-mSv CT and CDCT (≤ 8 mSv), the sensitivity was limited to 43% in both groups despite a high specificity (89.2% vs. 91.2%) for the differentiation of perforated appendicitis from unperforated appendicitis [77]. This corroborates the results of a recent systematic review [75], which concluded that many individual CT findings indicative of complicated appendicitis (e.g., appendiceal wall defect) are highly specific but not sensitive (Fig. 1). For successful non-surgical treatment, sensitivity is more important than specificity in diagnosing complicated appendicitis, because false-negative diagnosis may result in serious abdominal infection complicating unsuccessful non-surgical treatment [79]. Retrospective studies have shown the potential for improving sensitivity over 90% by refining the diagnostic criteria for CT findings [80] or by incorporating clinical and laboratory findings as well as image findings, but at the cost of specificity [81,82]. There seems to be much room for improvement to optimally select patients for non-surgical treatment. To achieve generalizability and global standardization of treatment, international scientific collaboration is needed by combining prospective patient databases [83].
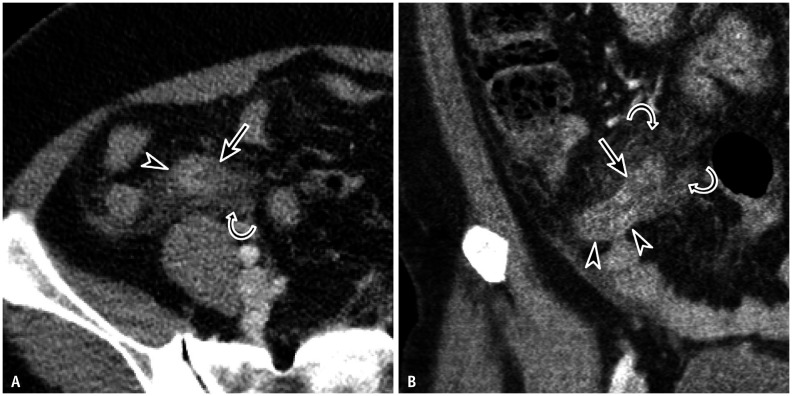
Fig. 1. A 38-year-old female with right lower quadrant pain.
A, B. Contrast-enhanced transverse (A) and coronal (B) low-dose CT images show an appendiceal wall defect (arrows) at the inflamed appendix (arrowheads) and periappendiceal fat infiltration (curved arrows). Perforation was confirmed both surgically and pathologically.
Alternative Diagnoses
A post hoc analysis [84] of the Korean multi-center trial data [43] suggested that 2-mSv CT is comparable to CDCT (≤ 8 mSv) for the diagnosis of right colonic diverticulitis, which is the most common specific alternative diagnosis in South Korea [41,43], and probably in Eastern Asia. Other data also indirectly support the idea that LDCT also works well for alternative diagnoses. In a Korean multicenter trial [43], final diagnoses other than appendicitis were adjudicated in 673 (43.8%) patients in the 2-mSv CT group and 687 (44.6%) patients in the CDCT (≤ 8 mSv) group with a similar distribution of alternative diagnoses. In other smaller retrospective studies [38,39,40,42], the reported diagnostic sensitivity for alternative diagnosis was similar between the two groups.
Unfortunately, all these data had inevitable limitations, including a small number of patients in each disease category, incompleteness of reference standards, and subjectivity in adjudicating final diagnoses. Specifically, final diagnosis often had to be adjudicated based on the CT results, as CT was practically the most accurate test for diagnosis (e.g., ureteral stone) [41,43]. Importantly, the three largest [40,41,43] of the studies discussed above included only patients aged 15–44 years. Thus, the optimism that LDCT is comparable to CDCT for alternative diagnoses may not apply to an older population with a higher prevalence of serious chronic or malignant diseases that can mimic appendicitis or cause secondary appendicitis [85].
Stepwise Multimodal Diagnostic Approach Incorporating LDCT
Patient Subgroups Less Benefited From LDCT
Given its radiation-free nature, it is unclear whether ultrasonography is the preferred imaging test for children and pregnant women with suspected appendicitis [13]. For pediatric patients under 15 years of age, ultrasonography should be preferred over CT, as supported by many guidelines. The radiation-saving advantage is less likely to be useful in patients with shorter life expectancies due to old age or serious comorbidities. CDCT may be more appropriate in such patients, because they have a higher prevalence of critical intra-abdominal abnormalities as alternative diagnoses or incidental findings on CT [85].
The subgroups of the Korean multicenter trial [43] were stratified by sex, body size, clinical risk scores for appendicitis [86,87], time of CT examination (working hours vs. after hours), CT machine, radiologist’s experience, site practice volume, and site experience with LDCT. Overall, the subgroup analyses showed consistent results of important clinical outcomes [43] and diagnostic performance [88] across various subgroups, implying that LDCT can replace CDCT in diverse populations. Nevertheless, the researchers pointed out that further studies are needed to confirm their conclusion in patients with extreme body sizes, as their data included a limited number of patients.
We recognize the practitioners’ concern that the diagnostic accuracy of LDCT may be compromised in patients with large body sizes. Unfortunately, no previous studies have included enough obese patients to answer this question. Importantly, the physical principle that image noise increases with increasing body size does not directly project to modern CT machines equipped with automatic exposure control that can maintain consistent image quality across different body sizes. Patients with obesity tend to have more intra-abdominal fat, which helps visualize the appendix on CT images (Fig. 2) [89].
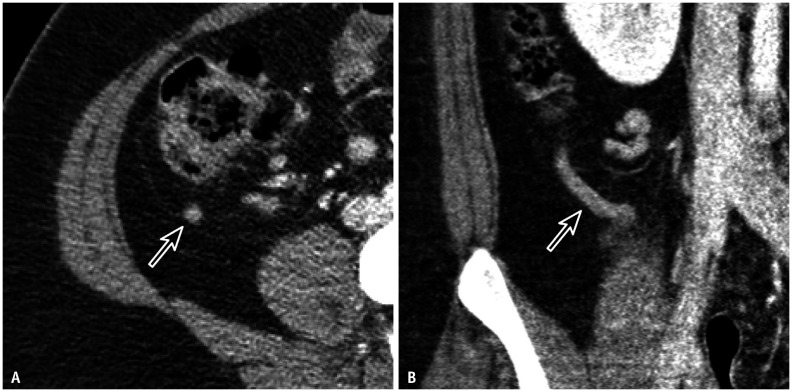
Fig. 2. A 21-year-old female with right lower quadrant pain.
A, B. Contrast-enhanced transverse (A) and coronal (B) low-dose CT images clearly show the normal appendix (arrows) in the abundant periappendiceal fat. The effective dose of the CT scan was 3 mSv, which was adjusted to the body size (body-mass index, 33.5 kg/m2) through automatic exposure control.
A smaller body size can limit the performance of LDCT. Two small studies [39,45] have suggested that 1–2-mSv CT may have limited diagnostic sensitivity in patients with small body sizes or sparse pericecal fat. However, many other studies [36,38,40,41,43,45] including the two Korean trials did not find notable effects of body-mass index or pericecal fat [90] on the diagnosis of appendicitis at 1–4 mSv CT. Regardless of these data, ultrasonography instead of CT should be preferred to CT for slender patients who generally have a good sonic window.
Selective Utilization of CT
Several studies that did not specifically address low-dose techniques have attempted to use selective CT in patients with suspected appendicitis. The study results [91,92,93] regarding the usefulness of clinical scoring systems for selective CT were conflicting. A meta-analysis [94] regarding selective CT following ultrasonography reported a pooled sensitivity of 89.9% and specificity of 93.6%. Evidence on the use of selective LDCT is limited. Further efforts are needed to incorporate LDCT into radiation-efficient diagnostic algorithms [93]. Importantly, for the patient subset of clinically equivocal cases in the Korean multicenter trial, 2-mSv CT was comparable to CDCT (≤ 8 mSv) in terms of clinical outcomes [43] and diagnostic performance [88].
CONCLUSION
Compelling evidence has accumulated for the use of an LDCT dose of only 2 mSv instead of CDCT in adolescents and adults with suspected appendicitis. The diagnosis of appendicitis is one of the few CT applications for which LDCT has been found by large pragmatic trials and systematic reviews as comparable to CDCT. We encourage radiologists, emergency room physicians, and surgeons to implement LD appendiceal CT in everyday clinical practice.
Acknowledgments
The authors thank to Yousun Ko, Hae Young Kim, Jungheum Cho, Ji Ye Sim, and Seungjae Lee for help in preparing the manuscript.
Footnotes
Conflicts of Interest: Paulina Salminen reports personal fees for lectures from Merck and Orion Pharma, outside the submitted work. Kyoung Ho Lee received a research grant from the National Research Foundation of Korea. Other authors declare there is no conflict of interest.
- Conceptualization: Ji Hoon Park, Kyoung Ho Lee.
- Data curation: all authors.
- Funding acquisition: Kyoung Ho Lee.
- Investigation: all authors.
- Methodology: Ji Hoon Park, Kyoung Ho Lee.
- Project administration: Ji Hoon Park, Kyoung Ho Lee.
- Supervision: Ji Hoon Park, Kyoung Ho Lee.
- Writing—original draft: all authors.
- Writing—review & editing: all authors.
Funding Statement: This research was supported by the National Research Foundation of Korea (NRF) grant funded by the Korea government (MSIT) (NRF-2019R1A2C1002118).
Availability of Data and Material
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.
Supplement
The Supplement is available with this article at https://doi.org/10.3348/kjr.2021.0596.
References
- 1.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mathews JD, Forsythe AV, Brady Z, Butler MW, Goergen SK, Byrnes GB, et al. Cancer risk in 680,000 people exposed to computed tomography scans in childhood or adolescence: data linkage study of 11 million Australians. BMJ. 2013;346:f2360. doi: 10.1136/bmj.f2360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Krille L, Dreger S, Schindel R, Albrecht T, Asmussen M, Barkhausen J, et al. Risk of cancer incidence before the age of 15 years after exposure to ionising radiation from computed tomography: results from a German cohort study. Radiat Environ Biophys. 2015;54:1–12. doi: 10.1007/s00411-014-0580-3. [DOI] [PubMed] [Google Scholar]
- 4.Huang WY, Muo CH, Lin CY, Jen YM, Yang MH, Lin JC, et al. Paediatric head CT scan and subsequent risk of malignancy and benign brain tumour: a nation-wide population-based cohort study. Br J Cancer. 2014;110:2354–2360. doi: 10.1038/bjc.2014.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee KH, Lee S, Park JH, Lee SS, Kim HY, Lee WJ, et al. Risk of hematologic malignant neoplasms from abdominopelvic computed tomographic radiation in patients who underwent appendectomy. JAMA Surg. 2021;156:343–351. doi: 10.1001/jamasurg.2020.6357. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Haijanen J, Sula S, Salminen P. Optimizing the gold standard—low-dose computed tomography modalities as a part of clinical practice in acute appendicitis imaging. JAMA Surg. 2021;156:351–352. doi: 10.1001/jamasurg.2020.6358. [DOI] [PubMed] [Google Scholar]
- 7.Woo JH, Jeon JJ, Choi SJ, Choi JY, Jang YS, Lim YS, et al. Low-dose (2-mSv) computed tomography for suspected appendicitis: applicability in an emergency department. Am J Emerg Med. 2018;36:2139–2143. doi: 10.1016/j.ajem.2018.03.031. [DOI] [PubMed] [Google Scholar]
- 8.Kim HJ, Lee KH, Kim MJ, Park SB, Ko Y LOCAT Group. Using 2-mSv appendiceal CT in usual practice for adolescents and young adults: willingness survey of 579 radiologists, emergency physicians, and surgeons from 20 hospitals. Korean J Radiol. 2020;21:68–76. doi: 10.3348/kjr.2019.0010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Prasad VK, Cifu AS. Ending medical reversal: improving outcomes, saving lives. Baltimore: Johns Hopkins University Press; 2019. [Google Scholar]
- 10.Lietzén E, Ilves I, Salminen P, Paajanen H, Rautio T, Nordström P, et al. Clinical and laboratory findings in the diagnosis of right lower quadrant abdominal pain: outcome analysis of the APPAC trial. Clin Chem Lab Med. 2016;54:1691–1697. doi: 10.1515/cclm-2015-0981. [DOI] [PubMed] [Google Scholar]
- 11.Lietzén E, Mällinen J, Grönroos JM, Rautio T, Paajanen H, Nordström P, et al. Is preoperative distinction between complicated and uncomplicated acute appendicitis feasible without imaging? Surgery. 2016;160:789–795. doi: 10.1016/j.surg.2016.04.021. [DOI] [PubMed] [Google Scholar]
- 12.Lahaye MJ, Lambregts DM, Mutsaers E, Essers BA, Breukink S, Cappendijk VC, et al. Mandatory imaging cuts costs and reduces the rate of unnecessary surgeries in the diagnostic work-up of patients suspected of having appendicitis. Eur Radiol. 2015;25:1464–1470. doi: 10.1007/s00330-014-3531-0. [DOI] [PubMed] [Google Scholar]
- 13.Garcia EM, Camacho MA, Karolyi DR, Kim DH, Cash BD, Chang KJ, et al. ACR Appropriateness Criteria® right lower quadrant pain-suspected appendicitis. J Am Coll Radiol. 2018;15:S373–S387. doi: 10.1016/j.jacr.2018.09.033. [DOI] [PubMed] [Google Scholar]
- 14.Flum DR, Morris A, Koepsell T, Dellinger EP. Has misdiagnosis of appendicitis decreased over time? A population-based analysis. JAMA. 2001;286:1748–1753. doi: 10.1001/jama.286.14.1748. [DOI] [PubMed] [Google Scholar]
- 15.Paulson EK, Kalady MF, Pappas TN. Clinical practice. Suspected appendicitis. N Engl J Med. 2003;348:236–242. doi: 10.1056/NEJMcp013351. [DOI] [PubMed] [Google Scholar]
- 16.Doria AS, Moineddin R, Kellenberger CJ, Epelman M, Beyene J, Schuh S, et al. US or CT for diagnosis of appendicitis in children and adults? A meta-analysis. Radiology. 2006;241:83–94. doi: 10.1148/radiol.2411050913. [DOI] [PubMed] [Google Scholar]
- 17.Terasawa T, Blackmore CC, Bent S, Kohlwes RJ. Systematic review: computed tomography and ultrasonography to detect acute appendicitis in adults and adolescents. Ann Intern Med. 2004;141:537–546. doi: 10.7326/0003-4819-141-7-200410050-00011. [DOI] [PubMed] [Google Scholar]
- 18.van Randen A, Bipat S, Zwinderman AH, Ubbink DT, Stoker J, Boermeester MA. Acute appendicitis: meta-analysis of diagnostic performance of CT and graded compression US related to prevalence of disease. Radiology. 2008;249:97–106. doi: 10.1148/radiol.2483071652. [DOI] [PubMed] [Google Scholar]
- 19.Cuschieri J, Florence M, Flum DR, Jurkovich GJ, Lin P, Steele SR, et al. Negative appendectomy and imaging accuracy in the Washington state surgical care and outcomes assessment program. Ann Surg. 2008;248:557–563. doi: 10.1097/SLA.0b013e318187aeca. [DOI] [PubMed] [Google Scholar]
- 20.Park JH LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: multi-center experience. J Korean Med Sci. 2014;29:1308–1316. doi: 10.3346/jkms.2014.29.9.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lee J, Ko Y, Ahn S, Park JH, Kim HJ, Hwang SS, et al. Comparison of US and CT on the effect on negative appendectomy and appendiceal perforation in adolescents and adults: a post-hoc analysis using propensity-score methods. J Clin Ultrasound. 2016;44:401–410. doi: 10.1002/jcu.22351. [DOI] [PubMed] [Google Scholar]
- 22.Toorenvliet BR, Wiersma F, Bakker RF, Merkus JW, Breslau PJ, Hamming JF. Routine ultrasound and limited computed tomography for the diagnosis of acute appendicitis. World J Surg. 2010;34:2278–2285. doi: 10.1007/s00268-010-0694-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Surgical Research Collaborative. Multicentre observational study of performance variation in provision and outcome of emergency appendicectomy. Br J Surg. 2013;100:1240–1252. doi: 10.1002/bjs.9201. [DOI] [PubMed] [Google Scholar]
- 24.Jaunoo SS, Hale AL, Masters JP, Jaunoo SR. An international survey of opinion regarding investigation of possible appendicitis and laparoscopic management of a macroscopically normal appendix. Ann R Coll Surg Engl. 2012;94:476–480. doi: 10.1308/003588412X13373405385377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Duke E, Kalb B, Arif-Tiwari H, Daye ZJ, Gilbertson-Dahdal D, Keim SM, et al. A systematic review and meta-analysis of diagnostic performance of MRI for evaluation of acute appendicitis. AJR Am J Roentgenol. 2016;206:508–517. doi: 10.2214/AJR.15.14544. [DOI] [PubMed] [Google Scholar]
- 26.International Commission on Radiological Protection. Diagnostic reference levels in medical imaging: review and additional advice. Ann ICRP. 2001;31:33–52. [PubMed] [Google Scholar]
- 27.Mettler FA, Jr, Huda W, Yoshizumi TT, Mahesh M. Effective doses in radiology and diagnostic nuclear medicine: a catalog. Radiology. 2008;248:254–263. doi: 10.1148/radiol.2481071451. [DOI] [PubMed] [Google Scholar]
- 28.American College of Radiology. ACR-AAPM-SPR practice parameter for diagnostic reference levels and achievable doses in medical X-ray imaging. ACR.org Web site. [Accessed Oct 8, 2021]. https://www.acr.org/-/media/ACR/Files/Practice-Parameters/diag-ref-levels.pdf .
- 29.Australian Radiation Protection and Nuclear Safety Agency. Current Australian national diagnostic reference levels for multi detector computed tomography. Arpansa.gov.au Web site. [Accessed Oct 8, 2021]. https://www.arpansa.gov.au/research-and-expertise/surveys/national-diagnostic-reference-level-service/current-australian-drls/mdct .
- 30.Kim JS, Lee SK, Kim SK, Yoo SM, Kim JM, Yoon SW. National diagnostic reference levels and achievable doses for 13 adult CT protocols and a paediatric head CT protocol: national survey of Korean hospitals. Radiat Prot Dosimetry. 2019;187:220–229. doi: 10.1093/rpd/ncz156. [DOI] [PubMed] [Google Scholar]
- 31.European Commission. European guidelines on quality criteria for computed tomography. EUR 1626. Luxembourg: European Commission; 2000. [Google Scholar]
- 32.Kanda R, Akahane M, Koba Y, Chang W, Akahane K, Okuda Y, et al. Developing diagnostic reference levels in Japan. Jpn J Radiol. 2020;39:307–314. doi: 10.1007/s11604-020-01066-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Deak PD, Smal Y, Kalender WA. Multisection CT protocols: sex- and age-specific conversion factors used to determine effective dose from dose-length product. Radiology. 2010;257:158–166. doi: 10.1148/radiol.10100047. [DOI] [PubMed] [Google Scholar]
- 34.Johnson PT, Horton KM, Mahesh M, Fishman EK. Multidetector computed tomography for suspected appendicitis: multi-institutional survey of 16-MDCT data acquisition protocols and review of pertinent literature. J Comput Assist Tomogr. 2006;30:758–764. doi: 10.1097/01.rct.0000228156.65904.b4. [DOI] [PubMed] [Google Scholar]
- 35.Tsapaki V, Damilakis J, Paulo G, Schegerer AA, Repussard J, Jaschke W, et al. CT diagnostic reference levels based on clinical indications: results of a large-scale European survey. Eur Radiol. 2021;31:4459–4469. doi: 10.1007/s00330-020-07652-5. [DOI] [PubMed] [Google Scholar]
- 36.Keyzer C, Tack D, de Maertelaer V, Bohy P, Gevenois PA, Van Gansbeke D. Acute appendicitis: comparison of low-dose and standard-dose unenhanced multi-detector row CT. Radiology. 2004;232:164–172. doi: 10.1148/radiol.2321031115. [DOI] [PubMed] [Google Scholar]
- 37.Keyzer C, Cullus P, Tack D, De Maertelaer V, Bohy P, Gevenois PA. MDCT for suspected acute appendicitis in adults: impact of oral and IV contrast media at standard-dose and simulated low-dose techniques. AJR Am J Roentgenol. 2009;193:1272–1281. doi: 10.2214/AJR.08.1959. [DOI] [PubMed] [Google Scholar]
- 38.Seo H, Lee KH, Kim HJ, Kim K, Kang SB, Kim SY, et al. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose i.v. contrast-enhanced CT scans. AJR Am J Roentgenol. 2009;193:96–105. doi: 10.2214/AJR.08.1237. [DOI] [PubMed] [Google Scholar]
- 39.Platon A, Jlassi H, Rutschmann OT, Becker CD, Verdun FR, Gervaz P, et al. Evaluation of a low-dose CT protocol with oral contrast for assessment of acute appendicitis. Eur Radiol. 2009;19:446–454. doi: 10.1007/s00330-008-1164-x. [DOI] [PubMed] [Google Scholar]
- 40.Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, et al. Acute appendicitis in young adults: low-versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology. 2011;260:437–445. doi: 10.1148/radiol.11102247. [DOI] [PubMed] [Google Scholar]
- 41.Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012;366:1596–1605. doi: 10.1056/NEJMoa1110734. [DOI] [PubMed] [Google Scholar]
- 42.Kim SH, Yoon JH, Lee JH, Lim YJ, Kim OH, Ryu JH, et al. Low-dose CT for patients with clinically suspected acute appendicitis: optimal strength of sinogram affirmed iterative reconstruction for image quality and diagnostic performance. Acta Radiol. 2015;56:899–907. doi: 10.1177/0284185114542297. [DOI] [PubMed] [Google Scholar]
- 43.LOCAT Group. Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): a pragmatic, multicentre, randomised controlled non-inferiority trial. Lancet Gastroenterol Hepatol. 2017;2:793–804. doi: 10.1016/S2468-1253(17)30247-9. [DOI] [PubMed] [Google Scholar]
- 44.Park JH, Kim B, Kim MS, Kim HJ, Ko Y, Ahn S, et al. Comparison of filtered back projection and iterative reconstruction in diagnosing appendicitis at 2-mSv CT. Abdom Radiol (NY) 2016;41:1227–1236. doi: 10.1007/s00261-015-0632-4. [DOI] [PubMed] [Google Scholar]
- 45.Karabulut N, Kiroglu Y, Herek D, Kocak TB, Erdur B. Feasibility of low-dose unenhanced multi-detector CT in patients with suspected acute appendicitis: comparison with sonography. Clin Imaging. 2014;38:296–301. doi: 10.1016/j.clinimag.2013.12.014. [DOI] [PubMed] [Google Scholar]
- 46.Poletti PA, Platon A, De Perrot T, Sarasin F, Andereggen E, Rutschmann O, et al. Acute appendicitis: prospective evaluation of a diagnostic algorithm integrating ultrasound and low-dose CT to reduce the need of standard CT. Eur Radiol. 2011;21:2558–2566. doi: 10.1007/s00330-011-2212-5. [DOI] [PubMed] [Google Scholar]
- 47.UNSCEAR. Sources and effects of ionizing radiation. New York: United Nations; 2008. Volume I: sources. Report to the general assembly, scientific annexes A and B. [Google Scholar]
- 48.Park JH, Jeon JJ, Lee SS, Dhanantwari AC, Sim JY, Kim HY, et al. Can we perform CT of the appendix with less than 1 mSv? A de-escalating dose-simulation study. Eur Radiol. 2018;28:1826–1834. doi: 10.1007/s00330-017-5159-3. [DOI] [PubMed] [Google Scholar]
- 49.Brenner DJ, Hall EJ. Computed tomography--an increasing source of radiation exposure. N Engl J Med. 2007;357:2277–2284. doi: 10.1056/NEJMra072149. [DOI] [PubMed] [Google Scholar]
- 50.Pickhardt PJ, Lawrence EM, Pooler BD, Bruce RJ. Diagnostic performance of multidetector computed tomography for suspected acute appendicitis. Ann Intern Med. 2011;154:789–796. doi: 10.7326/0003-4819-154-12-201106210-00006. [DOI] [PubMed] [Google Scholar]
- 51.National Council on Radiation Protection and Measurements. Implications of recent epidemiologic studies for the linear nonthreshold model and radiation protection. NCRP Commentary 27. Bethesda: National Council on Radiation Protection and Measurements; 2018. [Google Scholar]
- 52.Journy N, Rehel JL, Ducou Le Pointe H, Lee C, Brisse H, Chateil JF, et al. Are the studies on cancer risk from CT scans biased by indication? Elements of answer from a large-scale cohort study in France. Br J Cancer. 2015;112:185–193. doi: 10.1038/bjc.2014.526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Bosch de Basea M, Pearce MS, Kesminiene A, Bernier MO, Dabin J, Engels H, et al. EPI-CT: design, challenges and epidemiological methods of an international study on cancer risk after paediatric and young adult CT. J Radiol Prot. 2015;35:611–628. doi: 10.1088/0952-4746/35/3/611. [DOI] [PubMed] [Google Scholar]
- 54.National Research Council. Health risks from exposure to low levels of ionizing radiation: BEIR VII phase 2. Washington DC: The National Academies Press; 2006. p. 422. [PubMed] [Google Scholar]
- 55.Kiatpongsan S, Meng L, Eisenberg JD, Herring M, Avery LL, Kong CY, et al. Imaging for appendicitis: should radiation-induced cancer risks affect modality selection? Radiology. 2014;273:472–482. doi: 10.1148/radiol.14132629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Aly NE, McAteer D, Aly EH. Low vs. standard dose computed tomography in suspected acute appendicitis: is it time for a change? Int J Surg. 2016;31:71–79. doi: 10.1016/j.ijsu.2016.05.060. [DOI] [PubMed] [Google Scholar]
- 57.Yoon HM, Suh CH, Cho YA, Kim JR, Lee JS, Jung AY, et al. The diagnostic performance of reduced-dose CT for suspected appendicitis in paediatric and adult patients: a systematic review and diagnostic meta-analysis. Eur Radiol. 2018;28:2537–2548. doi: 10.1007/s00330-017-5231-z. [DOI] [PubMed] [Google Scholar]
- 58.Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY, Yang DM. Comparison of low-and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. AJR Am J Roentgenol. 2017;208:W198–W207. doi: 10.2214/AJR.16.17274. [DOI] [PubMed] [Google Scholar]
- 59.Rud B, Vejborg TS, Rappeport ED, Reitsma JB, Wille-Jørgensen P. Computed tomography for diagnosis of acute appendicitis in adults. Cochrane Database Syst Rev. 2019;2019:CD009977. doi: 10.1002/14651858.CD009977.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sippola S, Virtanen J, Tammilehto V, Grönroos J, Hurme S, Niiniviita H, et al. The accuracy of low-dose computed tomography protocol in patients with suspected acute appendicitis: the OPTICAP study. Ann Surg. 2020;271:332–338. doi: 10.1097/SLA.0000000000002976. [DOI] [PubMed] [Google Scholar]
- 61.Ahn S LOCAT group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: study protocol for a randomized controlled trial. Trials. 2014;15:28. doi: 10.1186/1745-6215-15-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Douglas PS. The theory and practice of imaging outcomes research. Lancet. 2015;385:2334–2335. doi: 10.1016/S0140-6736(15)60463-9. [DOI] [PubMed] [Google Scholar]
- 63.Velanovich V, Satava R. Balancing the normal appendectomy rate with the perforated appendicitis rate: implications for quality assurance. Am Surg. 1992;58:264–269. [PubMed] [Google Scholar]
- 64.Scott JW, Loehrer AP. The utility of perforated appendix rate as a proxy for timely access to care. JAMA Surg. 2020;155:1081–1082. doi: 10.1001/jamasurg.2020.2504. [DOI] [PubMed] [Google Scholar]
- 65.Kim HJ, Kim MS, Park JH, Ahn S, Ko Y, Song SY, et al. Meaningful standard of reference for appendiceal perforation: pathology, surgery, or both? Ann Surg Treat Res. 2017;93:88–97. doi: 10.4174/astr.2017.93.2.88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Braveman P, Schaaf VM, Egerter S, Bennett T, Schecter W. Insurance-related differences in the risk of ruptured appendix. N Engl J Med. 1994;331:444–449. doi: 10.1056/NEJM199408183310706. [DOI] [PubMed] [Google Scholar]
- 67.Ko Y, Choi JW, Kim DH, Lee KJ, Shin SS, Woo JY, et al. Central image archiving and management system for multicenter clinical studies: lessons from low-dose CT for appendicitis trial. J Korean Soc Radiol. 2017;76:165–172. [Google Scholar]
- 68.Cho J, Lee S, Min HD, Kim HY, Ko Y, Park JH, et al. Final diagnosis and patient disposition following equivocal results on 2-mSv CT vs. conventional-dose CT in adolescents and young adults with suspected appendicitis: a post hoc analysis of large pragmatic randomized trial data. Eur Radiol. 2021;31:9176–9187. doi: 10.1007/s00330-021-08020-7. [DOI] [PubMed] [Google Scholar]
- 69.Yang HK, Ko Y, Lee MH, Woo H, Ahn S, Kim B, et al. Initial performance of radiologists and radiology residents in interpreting low-dose (2-mSv) appendiceal CT. AJR Am J Roentgenol. 2015;205:W594–W611. doi: 10.2214/AJR.15.14513. [DOI] [PubMed] [Google Scholar]
- 70.Varadhan KK, Neal KR, Lobo DN. Safety and efficacy of antibiotics compared with appendicectomy for treatment of uncomplicated acute appendicitis: meta-analysis of randomised controlled trials. BMJ. 2012;344:e2156. doi: 10.1136/bmj.e2156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Salminen P, Paajanen H, Rautio T, Nordström P, Aarnio M, Rantanen T, et al. Antibiotic therapy vs appendectomy for treatment of uncomplicated acute appendicitis: the APPAC randomized clinical trial. JAMA. 2015;313:2340–2348. doi: 10.1001/jama.2015.6154. [DOI] [PubMed] [Google Scholar]
- 72.Flum DR, Davidson GH, Monsell SE, Shapiro NI, Odom SR, Sanchez SE, et al. A randomized trial comparing antibiotics with appendectomy for appendicitis. N Engl J Med. 2020;383:1907–1919. doi: 10.1056/NEJMoa2014320. [DOI] [PubMed] [Google Scholar]
- 73.Salminen P, Tuominen R, Paajanen H, Rautio T, Nordström P, Aarnio M, et al. Five-year follow-up of antibiotic therapy for uncomplicated acute appendicitis in the APPAC randomized clinical trial. JAMA. 2018;320:1259–1265. doi: 10.1001/jama.2018.13201. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Sippola S, Haijanen J, Viinikainen L, Grönroos J, Paajanen H, Rautio T, et al. Quality of life and patient satisfaction at 7-year follow-up of antibiotic therapy vs appendectomy for uncomplicated acute appendicitis: a secondary analysis of a randomized clinical trial. JAMA Surg. 2020;155:283–289. doi: 10.1001/jamasurg.2019.6028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kim HY, Park JH, Lee YJ, Lee SS, Jeon JJ, Lee KH. Systematic review and meta-analysis of CT features for differentiating complicated and uncomplicated appendicitis. Radiology. 2018;287:104–115. doi: 10.1148/radiol.2017171260. [DOI] [PubMed] [Google Scholar]
- 76.Sippola S, Grönroos J, Sallinen V, Rautio T, Nordström P, Rantanen T, et al. A randomised placebo-controlled double-blind multicentre trial comparing antibiotic therapy with placebo in the treatment of uncomplicated acute appendicitis: APPAC III trial study protocol. BMJ Open. 2018;8:e023623. doi: 10.1136/bmjopen-2018-023623. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Kim HY, Ko Y, Park JH, Lee KH LOCAT Group. Detection and false-referral rates of 2-mSv CT relative to standard-dose CT for appendiceal perforation: pragmatic multicenter randomized controlled trial. AJR Am J Roentgenol. 2020;215:874–884. doi: 10.2214/AJR.19.22632. [DOI] [PubMed] [Google Scholar]
- 78.Bom WJ, Bolmers MD, Gans SL, van Rossem CC, van Geloven AAW, Bossuyt PMM, et al. Discriminating complicated from uncomplicated appendicitis by ultrasound imaging, computed tomography or magnetic resonance imaging: systematic review and meta-analysis of diagnostic accuracy. BJS Open. 2021;5:zraa030. doi: 10.1093/bjsopen/zraa030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Foley WD. CT features for complicated versus uncomplicated appendicitis: what is the evidence? Radiology. 2018;287:116–118. doi: 10.1148/radiol.2018180022. [DOI] [PubMed] [Google Scholar]
- 80.Kim HY, Park JH, Lee SS, Lee WJ, Ko Y, Andersson RE, et al. CT in differentiating complicated from uncomplicated appendicitis: presence of any of 10 CT features versus radiologists’ gestalt assessment. AJR Am J Roentgenol. 2019;213:W218–W227. doi: 10.2214/AJR.19.21331. [DOI] [PubMed] [Google Scholar]
- 81.Kim HY, Park JH, Lee SS, Jeon JJ, Yoon CJ, Lee KH. Differentiation between complicated and uncomplicated appendicitis: diagnostic model development and validation study. Abdom Radiol (NY) 2020;46:948–959. doi: 10.1007/s00261-020-02737-7. [DOI] [PubMed] [Google Scholar]
- 82.Atema JJ, van Rossem CC, Leeuwenburgh MM, Stoker J, Boermeester MA. Scoring system to distinguish uncomplicated from complicated acute appendicitis. Br J Surg. 2015;102:979–990. doi: 10.1002/bjs.9835. [DOI] [PubMed] [Google Scholar]
- 83.Bom WJ, Scheijmans JCG, Salminen P, Boermeester MA. Diagnosis of uncomplicated and complicated appendicitis in adults. Scand J Surg. 2021;110:170–179. doi: 10.1177/14574969211008330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Kim HY, Lee S, Kim DH, Ko Y, Park JH, Ko A, et al. Conventional-dose CT versus 2-mSv CT for right colonic diverticulitis as an alternate diagnosis of appendicitis: secondary analysis of large pragmatic randomized trial data. AJR Am J Roentgenol. 2021;217:1113–1121. doi: 10.2214/AJR.21.25584. [DOI] [PubMed] [Google Scholar]
- 85.Pooler BD, Lawrence EM, Pickhardt PJ. Alternative diagnoses to suspected appendicitis at CT. Radiology. 2012;265:733–742. doi: 10.1148/radiol.12120614. [DOI] [PubMed] [Google Scholar]
- 86.Alvarado A. A practical score for the early diagnosis of acute appendicitis. Ann Emerg Med. 1986;15:557–564. doi: 10.1016/s0196-0644(86)80993-3. [DOI] [PubMed] [Google Scholar]
- 87.Andersson M, Andersson RE. The appendicitis inflammatory response score: a tool for the diagnosis of acute appendicitis that outperforms the Alvarado score. World J Surg. 2008;32:1843–1849. doi: 10.1007/s00268-008-9649-y. [DOI] [PubMed] [Google Scholar]
- 88.Ko Y, Lee WJ, Park JH, Kim HY, Sim JY, Tannaphai P, et al. Diagnostic sensitivity and specificity of 2-mSv CT vs. conventional-dose CT in adolescents and young adults with suspected appendicitis: post hoc subgroup analysis of the LOCAT data. Eur Radiol. 2020;30:4573–4585. doi: 10.1007/s00330-020-06811-y. [DOI] [PubMed] [Google Scholar]
- 89.Benjaminov O, Atri M, Hamilton P, Rappaport D. Frequency of visualization and thickness of normal appendix at nonenhanced helical CT. Radiology. 2002;225:400–406. doi: 10.1148/radiol.2252011551. [DOI] [PubMed] [Google Scholar]
- 90.Karabulut N, Boyaci N, Yagci B, Herek D, Kiroglu Y. Computed tomography evaluation of the normal appendix: comparison of low-dose and standard-dose unenhanced helical computed tomography. J Comput Assist Tomogr. 2007;31:732–740. doi: 10.1097/RCT.0b013e318033c7de. [DOI] [PubMed] [Google Scholar]
- 91.Lee CC, Golub R, Singer AJ, Cantu R, Jr, Levinson H. Routine versus selective abdominal computed tomography scan in the evaluation of right lower quadrant pain: a randomized controlled trial. Acad Emerg Med. 2007;14:117–122. doi: 10.1197/j.aem.2006.08.007. [DOI] [PubMed] [Google Scholar]
- 92.Andersson M, Kolodziej B, Andersson RE. Randomized clinical trial of appendicitis inflammatory response score-based management of patients with suspected appendicitis. Br J Surg. 2017;104:1451–1461. doi: 10.1002/bjs.10637. [DOI] [PubMed] [Google Scholar]
- 93.Song H, Lee S, Park JH, Kim HY, Min HD, Jeon JJ, et al. Can patient triaging with clinical scoring systems reduce CT use in adolescents and young adults suspected of having appendicitis? Radiology. 2021;300:350–358. doi: 10.1148/radiol.2021203884. [DOI] [PubMed] [Google Scholar]
- 94.Eng KA, Abadeh A, Ligocki C, Lee YK, Moineddin R, Adams-Webber T, et al. Acute appendicitis: a meta-analysis of the diagnostic accuracy of US, CT, and MRI as second-line imaging tests after an initial US. Radiology. 2018;288:717–727. doi: 10.1148/radiol.2018180318. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data sharing does not apply to this article as no datasets were generated or analyzed during the current study.