Abstract
Introduction
We performed a systematic review of comorbidities and symptoms of adult patients with coronavirus disease 2019 (COVID-19) to evaluate comorbidities, symptoms, and severity.
Material and methods
We searched databases and extracted comorbidities and symptoms from the included studies. We stratified the similar signs and symptoms in groups and on the basis of severity and compared them with stratified analysis. Individual case reports and case series with < 5 patients were excluded.
Results
A total of 163 studies with 43,187 patients were included. Mean age was 54.6 years. There were significantly fewer women in the study (43.9% vs. 56.1%, p < 0.0001). Prevalent cardiovascular comorbidities were hypertension (31.9%), obesity (27.9%), hyperlipidemia (26.4%), smoking (18.9%), diabetes mellitus (17.2%), atherosclerotic disease (9.2%) and arrhythmia (5.0%). The most frequently reported constitutional symptoms of COVID-19 were fever (73.9%), fatigue (33.4%), malaise (29.9%), myalgia and/or arthralgia (19.2%), generalized weakness (19.0%), and chills (11.3%). For the cardiovascular system, chest pain and/or tightness were most often reported (19.6%), followed by palpitations (5.2%). Hypertension and diabetes were common in severe disease. Obesity and congestive heart failure were not observed in any non-severe cases. Severe cases compared to non-severe cases more frequently had fever (87.8% vs. 58.5%, p < 0.001), shortness of breath (47.4% vs. 20.6%, p < 0.001), cough (66.8% vs. 62.9%, p < 0.001), sputum production (35.4% vs. 26.5%, p < 0.001) and rhinorrhea (32.2% vs. 7.3%, p < 0.001).
Conclusions
Hypertension, diabetes, and atherosclerotic diseases are common comorbidities across the world, with obesity as the second most common in the US and more common in men.
Keywords: symptoms, comorbidities, severity, COVID-19, SARS-CoV-2
Introduction
Coronavirus disease 2019 (COVID-19) is now a global pandemic caused by a novel coronavirus. The first case of COVID-19 was reported in December 2019 in Wuhan, China. Since then, it has affected over 138,010,168 people and caused over 2,970,000 deaths across the world [1]. Similar to other coronaviruses, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) primarily affects the pulmonary system. However, multi-system involvement, including cardiac, vascular, and neurological complications, has been reported [2]. The clinical manifestations range from asymptomatic infection or mild disease with fever, myalgias, and cough to severe disease characterized by shortness of breath, hypoxemia, acute respiratory distress syndrome requiring mechanical ventilation, multi-organ failure, and death [3]. However, due to this disease’s novelty, within the first year of the initial description, the prevalence of various symptoms and comorbidities associated with the disease remains unclear.
Several studies have evaluated the prevalence of various symptoms. A systematic review of 3600 patients reported fever, cough, and fatigue as most common [4]. Similarly, another meta-analysis of 78 studies found the prevalence of gastrointestinal symptoms to be 1 out of every 5 COVID-19 patients [5]. Another systematic review described the prevalence of acute myocardial injury in COVID-19 infection and found a pooled prevalence of nearly 20% [6]. Given the variable presentations and unclear prevalence of comorbidities and the accrual of interim experience, we performed a systematic review to assess the contemporary prevalence of comorbidities and symptoms from all the published studies.
Material and methods
We performed a systematic review following the Cochrane Handbook for Systematic Reviews and Intervention statement in health care interventions [7].
Selection criteria
We included observational studies, case series (retrospective, prospective, descriptive), randomized controlled trials, and survey studies that included adults’ comorbidities or symptoms with confirmed COVID-19 infection. Individual case reports and case series with < 5 patients were excluded.
Data Sources and Search Strategy
A comprehensive literature search was done on Ovid MEDLINE(R) and Epub Ahead of Print, In-Process; Other Non-Indexed Citations and Daily, Ovid Embase, Ovid Cochrane Central Register of Controlled Trials, Ovid Cochrane Database of Systematic Reviews, and Scopus from March 2019 to June 18, 2020. The main keywords used in the search were: (Corona virinae or corona virus or Coronavirinae or coronavirus or COVID or nCoV or 2019; or novel or new) or (Corona virinae or & corona virus; or Coronavirinae or coronavirus or COVID or nCoV) and wuhan) or Corona virinae19; or ;Corona virinae 2019 or "corona virus19 or &;corona virus2019; or Coronavirinae19 or Coronavirinae2019 or coronavirus19 or coronavirus2019 or COVID19 or COVID2019 or nCOV19 or nCOV2019 or;2019-nCOV or 2019nCOV or SARS Corona virus or SARS Coronavirus or SARS-COV-2. Two investigators (D.R. and R.P.) reviewed the titles and abstracts of the identified studies independently and screened them as per the selection criteria mentioned above. Any conflict was resolved with the consensus of a third investigator (R.T.).
Data abstraction
Data from included studies were independently abstracted by two investigators (D.R. and M.W.T.). The abstracted data included study design and setting, month and year of publication, duration of the study period, gender, comorbidities, symptoms and severity, mortality, survival, and discharge data. Data extraction excluded studies with pediatric patients. All comorbidities were initially abstracted separately, then grouped based on system involvement for data analysis. Similarly, all symptoms were extracted separately, then subsequently grouped for analysis.
Statistical analysis
The frequency of variable occurrence was calculated using percentages. For comorbidity analysis, studies with fewer than 3 reported comorbidities were excluded. Primary analysis involved the calculation of the presence of comorbidities and symptoms in the pooled data. Comorbidities and symptoms were compared based on the severity of the patients studied. For this stratification, we included studies reporting symptoms or comorbidities exclusively for severe or non-severe cases. Studies with severe and non-severe cases with inseparable comorbidity or severity data were excluded. A χ2 test was performed with α set at 0.05. All analyses were performed using SPSS version 25.
Results
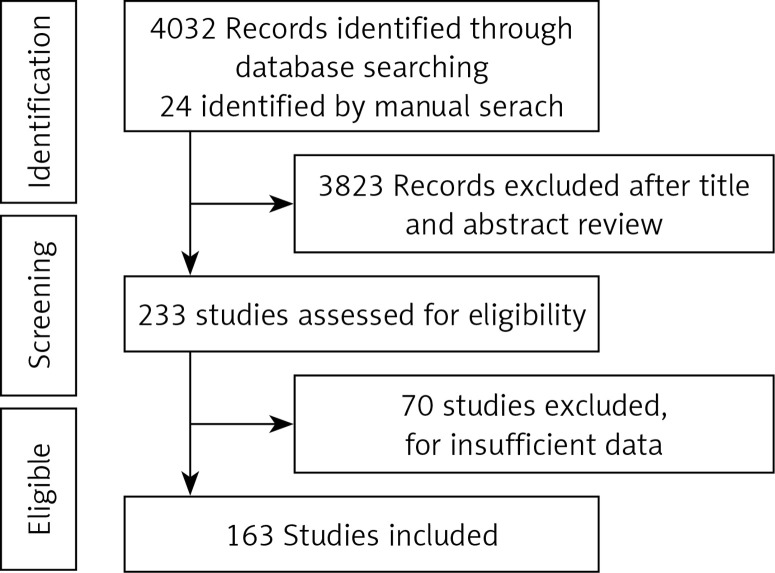
The preliminary database search resulted in 4032 studies; 24 other studies were identified from other sources; after the titles’ preliminary screening, 233 full-text studies were reviewed. Of these, 163 studies were included in the systematic reviews and in the primary analysis of symptoms [8–170]. For comorbidity analysis, 41 of 163 studies were excluded based on fewer than three reported comorbidities criteria, as described above, yielding 122 studies. A flow chart of the study selection is shown in Figure 1. The details of the included studies are provided in Table I.
Figure 1.
Flow chart low study
Table I.
Baseline characteristics of included studies
| Author name, year | Study period | Type of study | Patients N | Female patients (N) | Hospitalization status | Severity |
|---|---|---|---|---|---|---|
| Akalin et al., 2020 | Mar 16–Apr 1 | Retrospective single-center case series | 36 | 10 | 3 | B |
| An Ping et al., 2020 | Jan 17–Jan 24 | Retrospective single-center case series | 9 | 5 | 1 | |
| Bangalore et al., 2020 | Retrospective single-center case series | 18 | 3 | |||
| Beigel JH et al., 2020 | Feb 21–Apr 19 | RCT double blinded | 1063 | 377 | 1 | B |
| Bhatraju PK et al., 2020 | Feb 24–Mar 9 | Retrospective multi-center case series | 24 | 9 | 1 | S |
| Borba MGS et al., 2020 | Mar 23–Apr 5 | Parallel, double-masked, randomized, phase IIb clinical trial | 81 | 20 | 1 | S |
| Cai Qingxian et al., 2020 | Jan 30–Feb 14 | Open labelled non-randomized control study | 80 | 45 | 1 | B |
| Cai Qingxian et al., 2020 | Jan 11–Feb 6 | Retrospective single-center case series | 298 | 153 | 1 | B |
| Cao Jianlei et al., 2020 | Jan 3–Feb 1 | Retrospective single-center case series | 102 | 49 | 1 | B |
| Chan Fuk-Woo J et al., 2020 | Retrospective single-center case series | 6 | 3 | 1 | ||
| Chang De et al., 2020 | Jan 16–Jan 29 | Retrospective multi-center case series | 13 | 3 | 1 | |
| Chen J et al., 2020 | Jan 20–Feb 7 | Retrospective single-center case series | 249 | 123 | 1 | B |
| Chen L et al., 2020 | Dec 8–Mar 20 | Retrospective multi-center case series | 118 | B | ||
| Chen Nanshan et al., 2020 | Jan 1–Jan 20 | Retrospective single-center case series | 99 | 32 | 1 | B |
| Chen Qing et al., 2020 | Retrospective single-center case series | 9 | 4 | 1 | NS | |
| Chen Qingqing et al., 2020 | Jan 1–Mar 11 | Retrospective multi-center case series | 145 | 66 | 1 | B |
| Chen Tao et al., 2020 | Jan 13–Feb 12 | Retrospective single-center case series | 274 | 103 | S | |
| Chen TL et al., 2020 | Jan 1–Feb 10 | Retrospective single-center case series | 203 | 95 | B | |
| Cholankeril George et al., 2020 | Mar 4–Mar 24 | Retrospective single-center case series | 116 | 54 | 1 | B |
| Chu J et al., 2020 | Jan 7–Feb 11 | Retrospective single-center case series | 54 | 18 | 1 | B |
| COVID-19 National Emergency Response Center, Epidemiology and Case Management Team, Korea Centers for Disease Control and Prevention | Before 2/14/2020 | Retrospective multi-center case series | 28 | 13 | 3 | B |
| COVID-19 National Incident Room Surveillance Team | Retrospective single-center case series | 295 | 3 | B | ||
| Dai H et al., 2020 | Jan 10–Feb 7 | Retrospective multi-center case series | 234 | 98 | ||
| Deng Qing et al., 2020 | Jan 6–Feb 20 | Retrospective single-center case series | 112 | 55 | 1 | B |
| Dong X et al., 2020 | Retrospective multi-center case series | 11 | 6 | 1 | ||
| Du Rong-Hui et al., 2020 | Dec 25–Feb 7 | Prospective single center cohort | 179 | 82 | 1 | B |
| Du Y et al., 2020 | Jan 9–Feb 15 | Retrospective single-center case series | 85 | 23 | 1 | S |
| Escalera-Antezana JP et al., 2020 | Mar 2–Mar 15 | Retrospective multi-center case series | 12 | 6 | 2 | NS |
| Hua Fan et al., 2020 | Dec 30–Feb 16 | Retrospective single-center case series | 101 | 37 | 1 | S |
| Fei Xiao et al., 2020 | Feb 1–Feb 14 | Retrospective single-center case series | 73 | 32 | 1 | B |
| Feng Pan et al., 2020 | Jan 12–Feb 6 | Retrospective single-center case series | 21 | 15 | 1 | NS |
| Feng Yun et al., 2020 | Jan 1–Feb 15 | Retrospective multi-center case series | 476 | 205 | 1 | B |
| Fernández-Ruiz Mario et al., 2020 | March 5–March 23 | Retrospective single-center case series | 18 | 4 | 1 | B |
| Gautret Philippe et al., 2020 | Feb–March | Prospective single center cohort | 80 | 37 | 1 | B |
| Geleris et al., 2020 | Mar 7–Apr 8 | Cross-sectional Multi-center case series | 1376 | 595 | 1 | B |
| Giacomelli A et al., 2020 | Cross-sectional single-center case series | 59 | 19 | 1 | ||
| Goyal et al., 2020 | Mar 3–mar 27 | Retrospective single-center case series | 393 | 155 | 1 | B |
| Griiti Giuseppe et al., 2020 | Retrospective single-center cohort | 21 | 3 | 1 | B | |
| Guan W et al., 2020 | Dec 11–Jan 29 | Retrospective multi-center case series | 1099 | 459 | 3 | B |
| Guo Tao et al., 2020 | Jan 23–Feb 25 | Retrospective single-center case series | 187 | 96 | 1 | B |
| Hajifathalian K et al., 2020 | Mar 4–Apt 9 | Retrospective multi-center case series | 1059 | 448 | 3 | B |
| Han Chaoqun et al., 2020 | Feb 13–Feb 29 | Retrospective single-center case series | 206 | 115 | 1 | NS |
| Hong Kyung Soo et al., 2020 | Mar–20 | Retrospective single-center case series | 98 | 60 | 1 | B |
| Horby P et al., 2020 | Early 2020–June 8 | Randomized controlled open labelled trial | 6425 | 2337 | 1 | B |
| Huang Chaolin et al., 2020 | Dec 16–Jan 2 | Prospective single center cohort | 41 | 11 | 1 | B |
| Huang Yihui et al., 2020 | Dec–Jan | Retrospective single-center case series | 34 | 14 | 3 | B |
| Israelsen S B et al., 2020 | Mar 10–April 23 | Retrospective single-center case series | 175 | 90 | 1 | B |
| Javanian M, et al. 2020 | Feb 25–Mar 12 | Retrospective multi-center case series | 110 | 49 | 1 | |
| Jin Xi et al., 2020 | Jan 17–Feb 8 | Retrospective multi-center case series | 651 | 320 | 1 | B |
| Kaye et al., 2020 | Mar 25–Apr 3 | Retrospective multi-center case series | 237 | 129 | ||
| Kim ES et al., 2020 (Korea National Committee for Clinical Management of COVID-19 (KNCCMC)) | Feb | Prospective multi-center case series | 28 | 13 | 1 | B |
| Klopfenstein T et al., 2020 | Mar 1–Mar 17 | Retrospective single-center case series | 114 | 1 | B | |
| Kluytmans-van den Bergh M et al., 2020 | Mar 7–Mar 12 | Cross-sectional multi-center case series | 86 | 71 | 3 | NS |
| Kuang Y et al., 2020 | Jan 1–Feb 10 | Retrospective multi-center cohort | 944 | 476 | B | |
| Kujawski Stephanie et al., 2020 | Jan 20–Feb 5 | Retrospective multi-center case series | 12 | 4 | 3 | B |
| Lechien JR et al., 2020 | Retrospective multi-center case series | 417 | 263 | 1 | NS | |
| Lei H et al., 2020 | Jan 25–Jan 27 | Retrospective multi-center case series | 8 | 2 | 1 | |
| Lei S et al., 2020 | Jan 1–Feb 5 | Retrospective multi-center case series | 34 | 20 | 1 | B |
| Lei Wang et al., 2020 | Jan 21–Feb 5 | Retrospective single-center case series | 18 | 8 | 1 | |
| Lei Z et al., 2020 | Jan 22–Feb 12 | Retrospective single-center case series | 20 | 10 | ||
| Li Kunhua et al., 2020 | Jan–Feb | Retrospective multi-center case series | 83 | 39 | 1 | B |
| Li X et al., 2020 | Jan 14–Feb 13 | Retrospective single-center case series | 25 | 15 | 1 | S |
| Li Xiaochen et al., 2020 | Jan 26–Feb 5 | Retrospective single-center cohort | 548 | 269 | 1 | B |
| Lian J et al., 2020 | Jan 17–Jan 31 | Retrospective single-center case series | 465 | 222 | B | |
| Lian J et al., 2020 | Jan 17–Feb 12 | Retrospective multi-center case series | 788 | 381 | ||
| Liang WH, et al., 2020 | Nov 21–Jan 31 | Retrospective multi-center case series | 1590 | 674 | B | |
| Lin Lu et al., 2020 | Jan 17–Feb 15 | Retrospective single-center case series | 95 | 50 | 1 | B |
| Liu Jui-Yao et al., 2020 | Jan 21–Apr 6 | Retrospective multi-center case series | 321 | 170 | NS | |
| Liu Kai et al., 2020 | Jan 15–Feb 18 | Retrospective single-center case series | 56 | 25 | 1 | B |
| Liu Kiu et al., 2020 | Dec 30 –Jan 24 | Retrospective multi-center case series | 137 | 76 | 1 | B |
| Liu Yingxia et al., 2020 | December 26–January | Retrospective single-center case series | 12 | 4 | 1 | B |
| Liu Zhe et al., 2020 | Jan 16–Feb 13 | Retrospective multi-center case series | 72 | 33 | 1 | B |
| Lo LI et al., 2020 | Jan 21–Feb 16 | Prospective single center case series | 10 | 7 | 1 | B |
| Luo Shihua et al., 2020 | Jan 1–Feb 20 | Retrospective single-center case series | 183 | 81 | 1 | B |
| Lu-Xiaofan et al., 2020 | Jan 25–Feb 25 | Retrospective single-center case series | 244 | 116 | 1 | S |
| Ma J et al., 2020 | Jan 1–Mar 30 | Retrospective single-center case series | 37 | 20 | 1 | B |
| Mahevas M et al., 2020 | Mar 12–Mar 31 | Retrospective multi-center case series | 173 | 101 | 1 | B |
| Mathian A et al., 2020 | Mar 29–Apr 6 | Cross-sectional single-center case series | 17 | 13 | 3 | B |
| Meng Yifan et al., 2020 | Jan 16–Feb 4 | Retrospective single-center case series | 168 | 82 | 1 | S |
| Mi Bobib et al., 2020 | Jan 1–Feb 27 | Retrospective multi-center case series | 10 | 8 | 1 | B |
| Million M et al., 2020 | Mar 3–Mar 31 | Retrospective multi-center cohort | 1061 | 569 | 3 | B |
| Mo P et al., 2020 | Jan 1 –Feb 5 | Retrospective single-center case series | 155 | 69 | 1 | B |
| Moein S et al., 2020 | Mar 21–Apr 5 | Prospective single center case series | 60 | 20 | 1 | B |
| Morena V et al., 2020 | Mar 10–Mar 23 | Prospective single center open label study | 51 | 11 | S | |
| Nobel Yael et al., 2020 | Mar 10–Mar 21 | Retrospective single-center cohort | 278 | 133 | B | |
| Pan Lei et al., 2020 | Jan 18–Feb 28 | Cross-sectional multicenter case series | 103 | 48 | 1 | B |
| Pung Rachel et al., 2020 | Jan–Feb | Retrospective multi-center case series | 17 | 10 | 2 | NS |
| Qi X et al., 2020 | Jan 23–Feb 18 | Retrospective multi-center case series | 70 | 1 | B | |
| Qian GQ et al., 2020 | Jan 20–Feb 11 | Retrospective multi-center case series | 91 | 54 | 1 | B |
| Redd WD et al., 2020 | Feb 11–Feb 29 | Randomized, parallel, open label trial | 150 | 68 | 1 | B |
| Richardson Safiya et al., 2020 | Before April 2 | Retrospective multicenter cohort | 318 | 144 | 1 | B |
| Rodríguez-Cola M et al., 2020 | Mar 1–Apr 4 | Retrospective multi-center case series | 5700 | 2263 | 1 | B |
| Ronald LT et al., 2020 | Mar 20 –Apr 4 | Prospective single center case series | 7 | 2 | 1 | B |
| Rosenberg ES et al., 2020 | Mar 31–Apr 10 | Electronic survey | 145 | 94 | ||
| Sciascia S et al., 2020 | Mar 15–Mar 28 | Retrospective multi-center cohort | 1438 | 580 | 1 | B |
| Shaobo Shi et al., 2020 | Double-blind, placebo-controlled, multicenter trial | 63 | 7 | 1 | S | |
| Shi Heshui et al., 2020 | Jan 1–Feb 23 | Retrospective single-center case series | 671 | 349 | 1 | B |
| Shi Shaobo et al., 2020 | Dec 20–Jan 23 | Retrospective single-center case series | 81 | 39 | 1 | NS |
| Shu Lei et al., 2020 | Jan 20–Feb 10 | Retrospective single-center case series | 416 | 211 | 1 | B |
| Song F et al., 2020 | Feb 13–Feb 29 | Retrospective single-center case series | 545 | 281 | 1 | NS |
| Spiteri Gianfranco 2020 | Jan 20–Jan 27 | Retrospective single-center case series | 51 | 26 | 1 | NS |
| Tabata Sakiko et al., 2020 | Jan 24 –Feb 21 | Retrospective multi-center case series | 38 | 13 | 3 | NS |
| Tang Wei et al., 2020 | Feb 11–Feb 25 | Retrospective single-center case series | 104 | 50 | 1 | B |
| Tian S et al., 2020 | Jan 20–Feb 10 | Retrospective multi-center case series | 262 | 135 | B | |
| Toniati Paola et al., 2020 | Mar 9–Mar 20 | Multicenter prospective non-randomized study | 100 | 12 | 1 | S |
| Tu Wen-Jun et al. 2020 | Jan 3–Feb 24 | Retrospective single-center case series | 174 | 95 | 1 | B |
| Wan S et al., 2020 | Jan 23–Feb 8 | Retrospective single-center case series | 135 | 63 | 3 | |
| Wan Yunle et al., 2020 | Jan 19–Mar 6 | Retrospective multi-center case series | 232 | 101 | 1 | B |
| Wang Dawei et al., 2020 | Jan 1–Jan 28 | Retrospective single-center case series | 138 | 63 | 1 | B |
| Wang J et al., 2020 | Jan–Feb | Prospective multicenter case series | 93 | 36 | ||
| Wang L et al., 2020 | Jan 1–Feb 6 | Retrospective single-center case series | 339 | 173 | 1 | B |
| Wang Lizhen et al., 2020 | Jan 31–Feb 12 | Retrospective single-center case series | 26 | 15 | 1 | |
| Wang Luwen et al., 2020 | Jan 14–Feb 13 | Prospective single center cohort | 116 | 49 | 1 | B |
| Wang Min et al., 2020 | Jan 21–Feb 2 | Retrospective multi-center case series | 66 | 23 | 1 | |
| Wang Ruirui et al., 2020 | Jan 20–Feb 9 | Retrospective single-center case series | 125 | 71 | 1 | B |
| Yang Wenjie et al., 2020 | Jan 17–Feb 10 | Retrospective multi-center cohort | 149 | 68 | 1 | NS |
| Wang X et al., 2020 | Feb 7–Feb 12 | Retrospective single-center case series | 1012 | 488 | 1 | NS |
| Wang X et al., 2020 | Jan 10–Feb 24 | Retrospective multi-center case series | 80 | 49 | 1 | |
| Wang Yang et al., 2020 | Jan 25–Feb 25 | Retrospective single-center case series | 344 | 165 | 1 | S |
| Wang Yanrong et al., 2020 | Jan 11–Fbe 29 | Retrospective single-center case series | 55 | 22 | 1 | NS |
| Wang Yeming et al., 2020 | Feb 6–Mar 12 | Randomized, double-blind, placebo-controlled, multicenter trial | 236 | 96 | 1 | B |
| Wang Z et al., 2020 | Jan 16–Jan 29 | Retrospective single-center case series | 69 | 1 | ||
| Wei XS et al., 2020 | Jan 19–Feb 7 | Retrospective single-center case series | 84 | 56 | 1 | |
| Wei Jia-Fu et al., 2020 | Jan 16–Mar 10 | Prospective multicenter cohort | 101 | 47 | 1 | B |
| Wentao Ni et al., 2020 | Retrospective single-center case series | 179 | 1 | B | ||
| Wolfel Roman et al., 2020 | Jan 23–Jan 26 | Retrospective single-center case series | 9 | 1 | NS | |
| Wu Chaomin et al., 2020 | Dec 25–Jan 26 | Retrospective single-center case series | 201 | 73 | S | |
| Wu J et al., 2020 | Jan 22–Feb 14 | Retrospective multi-center case series | 80 | 41 | 1 | B |
| Wu Jiong et al., 2020 | Jan –Feb | Retrospective multi-center case series | 80 | 38 | 1 | B |
| Wu Yongjian et al., 2020 | Jan 16–Mar 15 | Prospective single center case series | 74 | 35 | 1 | B |
| Xia Xiao-ying et al., 2020 | Jan 23–Feb 18 | Retrospective single-center case series | 10 | 4 | 1 | B |
| Xie Hansheng et al., 2020 | Feb 2–Feb 23 | Retrospective single-center case series | 79 | 35 | 1 | NS |
| Xiong Fei et al., 2020 | Jan 1–Mar 10 | Retrospective multi-center cohort | 131 | 56 | 1 | B |
| Xiong Ying et al., 2020 | Jan 11–Feb 5 | Retrospective single-center case series | 42 | 17 | 1 | B |
| Xu T et al., 2020 | Jan 23–Feb 18 | Retrospective single-center case series | 51 | 26 | 1 | |
| Xu Xi et al., 2020 | Jan 23–Feb 4 | Retrospective single-center case series | 90 | 51 | 1 | B |
| Xu Xiaoling et al., 2020 | Feb 5–Feb 14 | Prospective single center case series | 21 | 3 | 1 | S |
| Xu XW et al., 2020 | Jan 10–Jan 26 | Retrospective single-center case series | 62 | 27 | 1 | NS |
| Xun Ding 2020 | Feb–March | Retrospective single-center case series | 112 | 61 | ||
| Yan CH et al., 2020 | Mar 3–mar 29 | Cross-sectional single-center case series | 59 | 29 | 3 | |
| Yan Yongli et al., 2020 | Jan 10–Feb 24 | Retrospective single-center case series | 193 | 79 | 1 | S |
| Yang Fan et al., 2020 | Jan 1 –April15 | Retrospective single-center case series | 52 | 24 | 1 | B |
| Yang X 2020 | Dec 24–Jan 26 | Retrospective single-center case series | 52 | 17 | 1 | S |
| Young BE el al., 2020 | Jan 23–Feb 3 | Retrospective multi-center case series | 18 | 9 | 1 | NS |
| Yu Yuan et al., 2020 | 27–Feb | Prospective multicenter case series | 226 | 87 | 1 | S |
| Zha Lei et al., 2020 | Jan 24–Feb 24 | Retrospective multi-center case series | 31 | 11 | 1 | NS |
| Zhang Guqin et al., 2020 | Jan 2–Feb 10 | Retrospective multi-center case series | 221 | 113 | 1 | B |
| Zhang JingCheng et al., 2020 | Jan 27–Feb 10 | Retrospective single-center case series | 14 | 7 | 1 | NS |
| Zhang Jin-Jin et al., 2020 | Jan 16–Feb 3 | Retrospective single-center case series | 140 | 69 | 1 | B |
| Zhang Jun et al., 2020 | Jan 28–Feb 24 | Retrospective single-center case series | 13 | 1 | B | |
| Zhang L et al., 2020 | Jan 13–Feb 26 | Retrospective multi-center case series | 28 | 11 | 1 | B |
| Zhang Xiaoli et al., 2020 | Jan 17–Feb 8 | Retrospective multi-center case series | 645 | 317 | 1 | B |
| Zhao Xin-Ying et al., 2020 | Jan 16–Feb 10 | Retrospective single-center case series | 91 | 42 | 1 | B |
| Zhao D et al., 2020 | Jan 23–Feb 5 | Retrospective multi-center case series | 19 | 8 | 1 | |
| Zhao Wei et al., 2020 | Retrospective single-center case series | 101 | 45 | 1 | ||
| Zheng F et al., 2020 | Jan 17–Feb 7 | Retrospective single-center case series | 161 | 81 | 1 | B |
| Zheng Y et al., 2020 | Jan 16–Feb 20 | Retrospective single-center case series | 99 | 48 | 1 | B |
| Zhou Fei et al., 2020 | Dec 29–Jan 31 | Retrospective multi-center cohort | 191 | 119 | 1 | S |
| Zhou Shuchang et al., 2020 | Jan 16–Feb 12 | Retrospective single-center case series | 100 | 46 | 1 | NS |
| Zhou Shuchang et al., 2020 | Jan 16–Jan 30 | Retrospective single-center case series | 62 | 23 | 1 | B |
| Zhou Y et al., 2020 | Jan 28–Mar 2 | Prospective single center case series | 21 | 8 | 1 | S |
| Zhou Zili et al., 2020 | Dec 20–Feb 9 | Retrospective single-center case series | 254 | 139 | 1 | |
| Zou Lirong et al., 2020 | Jan 7–Jan 26 | Retrospective single-center case series | 18 | 9 |
Hospitalization: 1: inpatient, 2: outpatient, 3: combined inpatient, and outpatient. S – severe, NS – non-severe, B – Both, N – number, RCT – randomized controlled trial, COVID-19: coronavirus disease 2019.
Study characteristics
A total of 163 studies with 43,187 patients were included. Of these, 117 were from China, 19 from the European region, 14 from the US, 2 from other countries, and the remaining 11 were from Australia, Brazil, Iran, Japan, S Korea, Singapore, and Taiwan. The earliest study recruitment started on December 11, 2019 and ended on April 19, 2020. There were 80 retrospective single-center case series; 43 retrospective multicenter case series, 7 retrospective multicenter cohorts, 3 retrospective single-center cohorts, 6 prospective single-center series, 3 prospective single-center series, 4 prospective single-center cohort studies, 1 prospective multicenter cohort study, 7 randomized controlled trials of various design, 1 open-label non-randomized control study, 1 descriptive case series, and 1 prospective single-center open-label study (Table I). A total of 128 studies included only hospitalized patients, 13 included both hospitalized and non-hospitalized patients, 2 included only non-hospitalized patients, and 20 studies did not list hospitalization status.
Patient baseline characteristics and outcomes
For a total of 40,632 patients, the mean age was 54.6 years, with a range of 18–98 years. A total of 8 studies, including adult patients with 2,325 patients, did not provide age data. Data regarding gender were not available in 8 studies. There were significantly fewer women in the study (43.9% vs. 56.1%, p < 0.0001). Hospitalization outcomes were reported in 116 studies for 37,349 patients; 48.5% (28,779) were discharged, 29% (18,810) remained in the hospital, and 12.1% (4284) died at the end of the study period for these studies. The details regarding invasive mechanical ventilation (IMV) were reported in 61 studies with 30,190 patients, of whom 9.89% (3,359) underwent IMV.
Comorbidities and symptoms for all patients
Prevalent cardiovascular comorbidities were hypertension (31.9%), obesity (27.9%), hyperlipidemia (26.4%), smoking (18.9%), diabetes mellitus (17.2%), atherosclerotic disease (9.2%) and arrhythmia (5.0%). Asthma (7.8%), followed by chronic obstructive lung disease (COPD) or chronic lung disease (CLD) (6.2%), were the most common respiratory comorbidities. The gastrointestinal comorbidities of hepatitis, liver disease and fatty liver disease had a prevalence of 2.4%. Chronic kidney disease and/or end-stage renal disease were reported in 6.2% of patients. Cerebrovascular disease or cerebrovascular accidents were reported in 3.5% of patients. Cancer and/or malignancy were reported in 4.4%, and HIV and/or immunodeficiency were observed in 1.6% of patients.
The most often reported constitutional symptoms of COVID-19 were fever (73.9%), fatigue (33.4%), malaise (29.9%), myalgia and/or arthralgia (19.2%), generalized weakness (19.0%), and chills (11.3%). For the cardiovascular system, chest pain and/or tightness were most often reported (19.6%), followed by palpitations (5.2%). Cough (60.3%), sputum production (29.7%), shortness of breath (27.3%), loss of smell and/or taste (25.1%), rhinorrhea (12.9%), and sore throat (12.3%) were the most often reported respiratory symptoms. The most common gastrointestinal symptoms were anorexia or loss of appetite (29.4%), followed by diarrhea (14.8%), nausea and/or vomiting (13.2%), and abdominal pain (7.4%). Commonly reported neurological symptoms were headache (12.8%), confusion (9.4%), and dizziness (8.2%). The details of the prevalence of constitutional, cardiovascular, respiratory, and gastrointestinal symptoms, and their related comorbidities, along with the number of studies, are shown in Tables II and III, respectively.
Table II.
Symptoms based on systems involved overall in patients with coronavirus disease 2019
| Symptom | %Age | Number of patients (N) | Total patients | Number of studies |
|---|---|---|---|---|
| Constitutional: | ||||
| Fever | 73.9.0 | 16999 | 22987 | 134 |
| Myalgia/arthralgia | 19.20 | 3657 | 19064 | 96 |
| Fatigue | 33.40 | 4266 | 12785 | 69 |
| Chills | 11.30 | 546 | 4816 | 19 |
| Generalized weakness | 19.00 | 434 | 2286 | 9 |
| Malaise | 29.90 | 272 | 909 | 8 |
| Respiratory/upper respiratory infection: | ||||
| Cough | 60.30 | 13739 | 22778 | 134 |
| Dyspnea | 27.30 | 5440 | 19926 | 111 |
| Sore throat | 12.30 | 1877 | 15302 | 78 |
| Sputum production | 29.70 | 3789 | 12730 | 64 |
| Nasal congestion | 6.60 | 507 | 7658 | 19 |
| Hemoptysis | 1.90 | 134 | 7191 | 22 |
| Rhinorrhea | 12.90 | 529 | 4089 | 34 |
| Loss of smell or taste | 25.10 | 740 | 2952 | 13 |
| Conjunctival congestion | 0.90 | 26 | 2927 | 4 |
| Cardiovascular: | ||||
| Chest pain/tightness | 19.60 | 1251 | 6394 | 47 |
| Palpitations | 5.20 | 22 | 422 | 4 |
| Gastrointestinal: | ||||
| Diarrhea | 14.80 | 2903 | 19544 | 112 |
| Nausea/vomiting | 13.20 | 1992 | 15081 | 76 |
| Abdominal pain | 7.40 | 504 | 6783 | 34 |
| Anorexia | 29.40 | 1857 | 6319 | 37 |
| Neurologic: | ||||
| Headache | 12.80 | 2005 | 15704 | 75 |
| Confusion | 9.40 | 191 | 2025 | 6 |
| Dizziness | 8.20 | 293 | 3564 | 22 |
Table III.
Prevalence of comorbidities overall in patients with coronavirus disease 2019
| Comorbidity | % | N | Total | Count |
|---|---|---|---|---|
| Cardiovascular: | ||||
| Hypertension | 31.90 | 9818 | 30792 | 105 |
| Diabetes mellitus | 17.20 | 5122 | 29796 | 107 |
| Atherosclerotic disease | 9.20 | 2642 | 28806 | 102 |
| Smoking | 18.90 | 2980 | 15728 | 31 |
| Obesity | 27.90 | 2758 | 9870 | 9 |
| Heart failure | 5.90 | 554 | 9403 | 9 |
| Arrythmia | 5.01 | 65 | 1297 | 5 |
| Hyperlipidemia | 26.40 | 199 | 753 | 9 |
| Respiratory: | ||||
| COPD/CLD | 6.20 | 1643 | 26570 | 83 |
| Asthma | 7.80 | 555 | 7136 | 11 |
| Gastrointestinal: | ||||
| Hepatitis/liver disease/fatty liver | 2.40 | 459 | 19310 | 60 |
| Renal: | ||||
| CKD/ESRD | 6.20 | 1445 | 23149 | 58 |
| Neurologic: | ||||
| CVA/cerebrovascular disease | 3.50 | 320 | 9152 | 40 |
| Other: | ||||
| Cancer/malignancy | 4.40 | 1062 | 23962 | 66 |
| HIV/immunodeficiency | 1.60 | 216 | 13506 | 23 |
COPD – chronic obstructive pulmonary disease, CLD – chronic lung disease, CKD – chronic kidney disease, ESRD – end-stage renal disease, CVA – cerebrovascular accident, HIV – human immunodeficiency virus.
Subgroup analysis by severity
For stratification based on severity for comorbidities and symptoms, only 30 studies met the inclusion criteria, with a total of 5,819 cases. Table IV shows the prevalence of comorbidities and symptoms in both groups.
Table IV.
Comorbidities and symptoms by severity vs. non-severity in patients with coronavirus disease 2019
| Parameter | Non- severe | Severe | P-value |
|---|---|---|---|
| Comorbidity: | |||
| Hypertension | 8.1% | 45.2% | < 0.001 |
| Diabetes mellitus | 3.5% | 19.5% | < 0.001 |
| Atherosclerotic disease | 5.2% | 10.9% | < 0.001 |
| Smoking | 13.5% | 3.8% | < 0.001 |
| Obesity | 0.0% | 30.5% | – |
| Heart failure | 0.0% | 5.2% | – |
| COPD/CLD | 9.2% | 12.0% | 0.083 |
| Liver disease | 2.8% | 3.0% | 0.814 |
| CKD/ESRD | 0.8% | 8.7% | < 0.001 |
| Malignancy | 3.8% | 3.7% | 0.899 |
| Symptom: | |||
| Fever | 58.5% | 87.8% | < 0.001 |
| Myalgia/Arthralgia | 25.8% | 19.0% | < 0.001 |
| Fatigue | 40.4% | 45.1% | 0.091 |
| Cough | 62.9% | 66.8% | 0.03 |
| Shortness of breath | 20.6% | 47.4% | < 0.001 |
| Sore throat | 12.6% | 14.0% | 0.279 |
| Sputum production | 26.5% | 35.4% | < 0.001 |
| Nasal congestion | 4.8% | 4.8% | 0.998 |
| Rhinorrhea | 7.3% | 32.2% | < 0.001 |
| Loss of smell/taste | 71.5% | 18.6% | < 0.001 |
| Chest pain/tightness | 19.3% | 21.1% | 0.34 |
| Diarrhea | 19.4% | 20.2% | 0.515 |
| Nausea/vomiting | 8.4% | 8.8% | 0.643 |
| Abdominal pain | 10.3% | 4.2% | < 0.001 |
| Anorexia | 41.0% | 27.1% | < 0.001 |
| Headache | 20.4% | 10.6% | < 0.001 |
| Hemoptysis | 3.2% | 2.5% | 0.725 |
| Chills | 15.9% | 6.9% | 0.001 |
COPD – chronic obstructive pulmonary disease, CLD – chronic lung disease, CKD – chronic kidney disease, ESRD – end-stage renal disease.
Comorbidities
Hypertension was the most commonly observed comorbidity among severe cases (45.2% vs. 8.1%, p < 0.001). Diabetes mellitus was also more common in severe disease (19.5% vs. 3.5%, p < 0.001). Obesity and congestive heart failure (CHF) were not observed in any non-severe cases among the studies included for this analysis but were present in severe cases (30.5% and 5.2%, respectively). Smoking was more commonly observed in non-severe cases than severe cases (13.5% vs. 3.8%, p < 0.001). COPD was similar in non-severe and severe cases (9.2% vs. 12.0%, p = 0.083).
Symptoms
Among all the symptoms compared, non-respiratory symptoms were more commonly observed among non-severe cases (headaches, anorexia, abdominal pain, loss of smell/taste). Severe compared to non-severe cases more frequently had fever (87.8% vs. 58.5%, p < 0.001), shortness of breath (47.4% vs. 20.6%, p < 0.001), cough (66.8% vs. 62.9%, p < 0.001), sputum production (35.4% vs. 26.5%, p < 0.001) and rhinorrhea (32.2% vs. 7.3%, p < 0.001). Both groups had a similar prevalence of chest pain (21.1% severe vs. 19.3% non-severe, p = 0.34), diarrhea (20.2% severe vs. 19.4% non-severe, p = 0.515), and nausea/vomiting (8.8% severe vs. 8.4% non-severe, p = 0.643).
Discussion
Since the emergence of SARS-CoV-2 infection in China and its spread worldwide, the knowledge regarding disease course, clinical characteristics, and treatment options has continued to evolve. We performed a comprehensive systematic review of published studies with COVID-19 patients. This systematic review summarized the prevalence of clinical symptoms and comorbidities in COVID-19 patients, stratified by the severity of symptoms [164–170].
This analysis found that the prevalence of COVID-19 was higher in men compared to women. Hypertension, obesity, hyperlipidemia, smoking, diabetes mellitus, and atherosclerotic diseases are the most common comorbidities overall. Fever, cough, fatigue, malaise, sputum production, shortness of breath, and anosmia are the most common symptoms overall. After stratification of patients on the basis of severity, hypertension, diabetes, obesity, and CHF were the most common comorbidities in severe illness. In contrast, smoking is more common in non-severe illnesses. Fever, shortness of breath, cough, sputum production, and rhinorrhea are more commonly reported in patients with severe illness, whereas headache, anorexia, abdominal pain, and loss of smell/taste are reported more often in patients with non-severe illness.
We report a higher prevalence of COVID-19 in men compared to women. An analysis of 14,712 patients revealed men to have significantly higher mortality than women even after adjusting for comorbidities [171]. Gender differences have been reported in the prior influenza pandemic, suggesting that men are more susceptible to viral respiratory illness; this is attributed to females generating stronger innate and adaptive immune responses [172, 173]. Thus, it could be why SARS-CoV-2, being a respiratory virus, was noted to have a higher prevalence in men in our study. One study evaluating 524 SARS-CoV-2 patients ages 51 to 70 found that males were significantly more likely to be hospitalized and had increased mortality regardless of age [174]. It could be hypothesized that women have a robust immune response to viruses as seen with the influenza virus as well; hence that could be the reason for the protection of females against SARS-CoV 2 infection.
We found the most common comorbidities to be hypertension and diabetes; these results are consistent with prior studies with a similar prevalence of hypertension and diabetes ranging from 13% to 27% and 7% to 12%, respectively [4, 175]. The slightly higher prevalence of hypertension and diabetes in this study could be attributed to the inclusion of studies worldwide. In contrast, prior studies included only studies from China. The prevalence of obesity was 27.9% from 9 studies; interestingly, all these studies were from the US. Obesity has also been postulated to be a risk factor for COVID-19 by the dysregulation of the immune system due to excess adiposity and decreased diaphragm contractility [176]. Smoking was more common in non-severe patients; the “smoker’s paradox” has been proposed as a possible mechanism suggesting smoking to have a protective effect, although this hypothesis continues to remain controversial [177].
Hypertension, hyperlipidemia, smoking, diabetes mellitus, and obesity are well-known cardiovascular risk factors [178]. Heart disease, stroke, and diabetes are known risk factors for influenza and its complications. SARS-CoV-2, being a respiratory virus, could also be hypothesized to have a similar risk factor [179]. Several hypotheses have been proposed for the cardiovascular complications of SARS-CoV-2, including angiotensin-converting enzyme-2 mediated cardiac damage, direct viral injury to myocardium, and hypoxemia mediated damage. However, none of these hypotheses have been proven yet [6, 180, 181]. Our findings suggest a higher prevalence of cardiovascular comorbidities in severe cases, which could be likely because of myocardial injury in these patients. The presence of comorbidities, including hypertension, diabetes mellitus, and atherosclerotic disease, was noted to be significantly higher in the severely ill patient population, which is corroborated by prior studies [19, 24, 35, 182].
Our study is in concordance with a prior meta-analysis of 43 studies with 3600 patients reporting fever, cough, and fatigue to be the most common clinical symptoms, suggesting COVID-19 to have primary respiratory system involvement [4]. In our study, fever was the most common presenting symptom as well [4, 35, 54, 109]. Respiratory symptoms of shortness of breath, cough, sputum production, and rhinorrhea were more common in severe illnesses, whereas non-respiratory symptoms are more common in non-severe disease. This could be because dyspnea and the need for supplemental oxygen are the criteria for severe illness. Initial studies were suggestive of COVID-19 being primarily a respiratory illness; however, recent studies suggest COVID-19 to be a multi-system disorder with the involvement of cardiovascular, gastrointestinal, musculoskeletal, and nervous systems. We report the involvement of respiratory, cardiovascular, gastrointestinal, musculoskeletal, and nervous systems, suggesting that COVID-19 is a multi-system disease with primary respiratory system involvement.
Our study reports a low prevalence (25.1% in 7952 from 13 studies) of loss of smell or taste; this is likely because of the inclusion of outpatient and survey studies in our review. A review focusing on olfactory dysfunction reported that up to 80% of patients with COVID-19 might develop subjective olfactory dysfunction in the disease’s initial stages [183]. The lower prevalence in our study can be attributed to the inclusion of more inpatient studies in our analysis, as loss of smell tends to be an early-onset symptom and not recognized in inpatients. A review focusing on musculoskeletal symptoms of 12,046 patients reported occurrence of fatigue in 25.6% and arthralgia and/or myalgia in 15.5% of patients. Our study also showed a similar prevalence of these symptoms, although they seem to be nonspecific and represent viral prodromal symptoms for most of the respiratory viruses [184].
Our study’s strength lies in its large patient population of more than 40,000 cases, including inpatients and outpatients, severe and non-severe cases, and spread over multiple continents. Our study has certain limitations as the majority of studies included in our study are observational. Even though our study included patients across the world, the majority of studies originate from China. Of concern, many of the studies were incomplete and did not include a comprehensive picture of the patients such as outcomes on discharge. Additionally, most of the studies were in inpatient settings, thus under-representing cases within the community. Lastly, the literature evolving around COVID-19 is very dynamic and rapidly evolving, especially in terms of outcomes.
In conclusion, the prevalence of COVID-19 was found to be higher in men. Hypertension, diabetes, and atherosclerotic diseases are common comorbidities globally, and obesity is the second most common in the US. There is a higher prevalence of comorbid hypertension and diabetes amongst severely ill patients and a higher prevalence of fever, myalgia/arthralgia, shortness of breath, and cough symptoms in severely ill patients. We believe that further high-quality prospective studies are needed to identify the demographics and regional differences and ascertain characteristics of outpatient COVID-19 individuals.
Conflict of interest
The authors declare no conflict of interest.
References
- 1.University, J.H. Coronavirus Resource Center. July 1, 2020; Available from: https://coronavirus.jhu.edu/data.
- 2.Gupta A, Madhavan MV, Sehgal K, et al. Extrapulmonary manifestations of COVID-19. Nat Med 2020; 26: 1017-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Organization W.H . Clinical management of COVID-19. July 1, 2020; Available from: https://www.who.int/publications/i/item/clinical-management-of-covid-19.
- 4.Fu L, Wang B, Yuan T, et al. Clinical characteristics of coronavirus disease 2019 (COVID-19) in China: a systematic review and meta-analysis. J Infect 2020; 80: 656-65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Tariq R, Saha S, Furqan F, et al. , Prevalence and mortality of COVID-19 patients with gastrointestinal symptoms: a systematic review and meta-analysis. Mayo Clinic Proc 2020; 95: 1632-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bavishi C, Bonow RO, Trivedi V, et al. Acute myocardial injury in patients hospitalized with COVID-19 infection: a review. Prog Cardiovasc Dis 2020; 63: 682-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. J Clin Epidemiol 2009; 62: 1006-12. [DOI] [PubMed] [Google Scholar]
- 8.Ni W, Yang X, Liu J, et al. Acute myocardial injury at hospital admission is associated with all-cause mortality in COVID-19. J Am Coll Cardiol 2020; 76: 124-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wei JF, Huang FY, Xiong TY, et al. , Acute myocardial injury is common in patients with covid-19 and impairs their prognosis. Heart 2020; 106: 1154-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lu X, Chen T, Wang Y, et al. Adjuvant corticosteroid therapy for critically ill patients with COVID-19. Crit Care 2020; 24: 241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lian J, Jin X, Hao S, et al. , Analysis of epidemiological and clinical features in older patients with coronavirus disease 2019 (COVID-19) outside Wuhan. Clin Infect Dis 2020; 71: 740-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liu JY, Chen TJ, Hwang SJ. Analysis of imported cases of covid-19 in Taiwan: a nationwide study. Int J Environ Res Public Health 2020; 17: 3311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Liu Z, Jin C, Wu CC, et al. Association between initial chest CT or clinical features and clinical course in patients with coronavirus disease 2019 Pneumonia. Korean J Radiol 2020; 21: 736-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shi S, Qin M, Shen B, et al. Association of cardiac injury with mortality in hospitalized patients with COVID-19 in Wuhan, China. JAMA Cardiol 2020; 5: 802-10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Yan CH, Faraji F, Prajapati DP, et al. Association of chemosensory dysfunction and Covid-19 in patients presenting with influenza-like symptoms. Int Forum Allergy Rhinol 2020; 10: 806-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Rosenberg ES, Dufort EM, Udo T, et al. Association of treatment with hydroxychloroquine or azithromycin with in-hospital mortality in patients with COVID-19 in New York State. JAMA 2020; 323: 2493-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Goyal P, C or r e sp ondence Clinical Characteristics of Covid-19 in China. N Eng J Med 2020; 382: 2372-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Guo T, Fan Y, Chen M, et al. Cardiovascular implications of fatal outcomes of patients with coronavirus disease 2019 (COVID-19). JAMA Cardiol 2020; 5: 811-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Shi S, Qin M, Cai Y, et al. Characteristics and clinical significance of myocardial injury in patients with severe coronavirus disease 2019. Eur Heart J 2020; 41: 2070-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Mi B, Chen L, Xiong Y, et al. Characteristics and early prognosis of covid-19 infection in fracture patients. J Bone Joint Surg Am 2020; 102: 750-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Tian S, Hu N, Lou J, et al. Characteristics of COVID-19 infection in Beijing. J Infect 2020; 80: 401-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Israelsen SB, Kristiansen KT, Hindsberger B, et al. Characteristics of patients with COVID-19 pneumonia at Hvidovre Hospital, March-April 2020. Danish Med J 2020; 67: 28-31. [PubMed] [Google Scholar]
- 23.Wu J, Wu X, Zeng W, et al. Chest CT findings in patients with coronavirus disease 2019 and its relationship with clinical features. Investig Radiol 2020; 55: 257-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zhou Y, Han T, Chen J, et al. Clinical and autoimmune characteristics of severe and critical cases with COVID-19. Clin Transl Sci 2020; 13: 1077-86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Liu Y, Yang Y, Zhang C, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked. Sci China Life Sci 2020; 63: 364-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Li K, Wu J, Wu F, et al. The clinical and chest CT features associated with severe and critical COVID-19 pneumonia. Investig Radiol 2020; 55: 327-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Xiong Y, Sun D, Liu Y, et al. Clinical and high-resolution CT Features of the COVID-19 infection: comparison of the initial and follow-up changes. Investig Radiol 2020; 55: 332-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Javanian M, Bayani M, Shokri M, et al. Clinical and laboratory findings from patients with COVID-19 pneumonia in Babol North of Iran: a retrospective cohort study. Rom J Intern Med 2020; 58: 161-7. [DOI] [PubMed] [Google Scholar]
- 29.COVID-19 Investigation Team . Clinical and virologic characteristics of the first 12 patients with coronavirus disease 2019 (COVID-19) in the United States. Nat Med 2020; 26: 861-8. [DOI] [PubMed] [Google Scholar]
- 30.Yang W, Cao Q, Qin L, et al. Clinical characteristics and imaging manifestations of the 2019 novel coronavirus disease (COVID-19): a multi-center study in Wenzhou city, Zhejiang, China. J Infection 2020; 80: 388-93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Yang F, Shi S, Zhu J, et al. Clinical characteristics and outcomes of cancer patients with COVID-19. J Med Virol 2020; 92: 2067-73. [DOI] [PubMed] [Google Scholar]
- 32.Liang WH, Guan WJ, Li CC, et al. Clinical characteristics and outcomes of hospitalised patients with COVID-19 treated in Hubei (epicenter) and outside Hubei (non-epicenter): a nationwide analysis of China. Eur Respir J 2020; 55: 2000562. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Chen TL, Dai Z, Mo P, et al. Clinical characteristics and outcomes of older patients with coronavirus disease 2019 (COVID-19) in Wuhan, China (2019): a single-centered, retrospective study. J Gerontol A Biol Sci Med Sci 2020; 75: 1788-95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Lei S, Jiang F, Su W, et al. Clinical characteristics and outcomes of patients undergoing surgeries during the incubation period of COVID-19 infection. EClinicalMedicine 2020; 21: 100331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Yan Y, Yang Y, Wang F, et al. Clinical characteristics and outcomes of patients with severe covid-19 with diabetes. BMJ Open Diabetes Res Care 2020; 8: 1-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ma J, Yin J, Qian Y, et al. Clinical characteristics and prognosis in cancer patients with COVID-19: a single center’s retrospective study. J Infect 2020; 81: 318-56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Li X, Wang L, Yan S, et al., Clinical characteristics of 25 death cases infected with COVID-19 pneumonia: a retrospective review of medical records in a single medical center, Wuhan, China. medRxiv 2020. DOI: 2020.02.19.20025239. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chu J, Yang N, Wei Y, et al. Clinical characteristics of 54 medical staff with COVID-19: a retrospective study in a single center in Wuhan, China. J Med Virol 2020; 92: 807-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wang X, Liu W, Zhao J, et al. Clinical characteristics of 80 hospitalized frontline medical workers infected with COVID-19 in Wuhan, China. J Hospital Infect 2020; 105: 399-403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Chen T, Wu DI, Chen H, et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: retrospective study. BMJ 2020; 368: m1091. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wang D, Hu B, Hu C, et al. Clinical characteristics of 138 hospitalized patients with 2019 novel coronavirus-infected pneumonia in Wuhan, China. JAMA 2020; 323: 1061-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Zhang J, Dong X, Cao Y, et al. Clinical characteristics of 140 patients infected with SARS-CoV-2 in Wuhan, China. Allergy 2020; 75; 1730-41. [DOI] [PubMed] [Google Scholar]
- 43.Chen Q, Zheng Z, Zhang C, et al. Clinical characteristics of 145 patients with corona virus disease 2019 (COVID-19) in Taizhou, Zhejiang, China. Infection 2020; 48: 543-51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Zheng F, Tang W, Li H, et al. Clinical characteristics of 161 cases of corona virus disease 2019 (COVID-19) in Changsha. Eur Rev Med Pharmacol Sci 2020; 24: 3404-10. [DOI] [PubMed] [Google Scholar]
- 45.Shu L, Wang X, Li M, et al. Clinical characteristics of 545 cases confirmed COVID-19 in Wuhan Stadium Cabin Hospital. SSRN 2020. doi: 10.2139/ssrn.3552844. [DOI] [Google Scholar]
- 46.Xiong F, Tang H, Liu L, et al. Clinical characteristics of and medical interventions for COVID-19 in hemodialysis patients in Wuhan, China. J Am Soc Nephrol 2020; 31: 1387-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Guan W, Ni Z, Hu Y, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med 2020; 382: 1708-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pan L, Mu M, Yang P, et al. Clinical characteristics of COVID-19 patients with digestive symptoms in Hubei, China: a descriptive, cross-sectional, multicenter study. Am J Gastroenterol 2020; 115: 766-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Zhang L, Zhu F, Xie L, et al. Clinical characteristics of COVID-19-infected cancer patients: a retrospective case study in three hospitals within Wuhan, China. Ann Oncol 2020; 31: 894-901. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tabata S, Imai K, Kawano S, et al. The clinical characteristics of COVID-19: a retrospective analysis of 104 patients from the outbreak on board the Diamond Princess cruise ship in Japan. medRxiv 2020. doi: 10.1101/2020.03.18.20038125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Wu J, Liu J, Zhao X, et al. Clinical characteristics of imported cases of COVID-19 in Jiangsu Province: a multicenter descriptive study. Clin Infect Dis 2020; 71: 706-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Wang X, Fang J, Zhu Y, et al. Clinical characteristics of non-critically ill patients with novel coronavirus infection (COVID-19) in a Fangcang Hospital. Clin Microbiol Infect 2020; 26: 1063-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Xie H, Zhao J, Lian N, et al. Clinical characteristics of non-ICU hospitalized patients with coronavirus disease 2019 and liver injury: a retrospective study. Liver Int 2020; 40: 1321-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Liu K, Fang YY, Deng Y, et al. Clinical characteristics of novel coronavirus cases in tertiary hospitals in Hubei Province. Chin Med J 2020; 133: 1025-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Zhao XY, Xu XX, Yin HS, et al. Clinical characteristics of patients with 2019 coronavirus disease in a non-Wuhan area of Hubei Province, China: a retrospective study. BMC Infect Dis 2020; 20: 311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Chen L, Li Q, Zheng D, et al. Clinical characteristics of pregnant women with covid-19 in Wuhan, China. N Engl J Med 2020; 382: e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mo P, Xing Y, Xiao Y, et al. Clinical characteristics of refractory COVID-19 pneumonia in Wuhan, China. Clin Infect Dis 2020. doi: 10.1093/cid/ciaa270. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Wang Y, Lu X, Li Y, et al. Clinical course and outcomes of 344 intensive care patients with COVID-19. Am J Respir Crit Care Med 2020; 201: 1430-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Yang X, Yu Y, Xu J, et al. Clinical course and outcomes of critically ill patients with SARS-CoV-2 pneumonia in Wuhan, China: a single-centered, retrospective, observational study. Lancet Respir Med 2020; 8: 475-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Zhou F, Yu T, Du R, et al. Clinical course and risk factors for mortality of adult inpatients with COVID-19 in Wuhan, China: a retrospective cohort study. Lancet 2020; 395: 1054-62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Mathian A, Mahevas M, Rohmer J, et al. Clinical course of coronavirus disease 2019 (COVID-19) in a series of 17 patients with systemic lupus erythematosus under long-term treatment with hydroxychloroquine. Ann Rheum Dis 2020; 79: 2019-21. [DOI] [PubMed] [Google Scholar]
- 62.Wang L, Gao YH, Lou LL, et al. The clinical dynamics of 18 cases of COVID-19 outside of Wuhan, China. Eur Respir J 2020; 55: 10-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Mahévas M, Tran VT, Roumier M, et al. Clinical efficacy of hydroxychloroquine in patients with covid-19 pneumonia who require oxygen: observational comparative study using routine care data. BMJ 2020; 369: m1844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Xu T, Chen C, Zhu Z, et al. Clinical features and dynamics of viral load in imported and non-imported patients with COVID-19. Int J Infect Dis 2020; 94: 68-71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Hong KS, Lee KH, Chung JH, et al. Clinical features and outcomes of 98 patients hospitalized with sars-cov-2 infection in Daegu, South Korea: a brief descriptive study. Yonsei Med J 2020; 61: 431-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Cao J, Tu WJ, Cheng W, et al. Clinical features and short-term outcomes of 102 patients with corona virus disease 2019 in Wuhan, China 2. Institute of Radiation Medicine, China Academy of Medical Science & Peking Union Medical College, Tianjin, China 3. Department of Infectious. 2019(238). [Google Scholar]
- 67.Zhang G, Hu C, Luo L, et al. Clinical features and short-term outcomes of 221 patients with COVID-19 in Wuhan, China. J Clin Virol 2020; 127: 104364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Wan S, Xiang Y, Fang W, et al. Clinical features and treatment of COVID-19 patients in northeast Chongqing. J Med Virol 2020; 92: 797-806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wang Z, Yang B, Li Q, et al. Clinical features of 69 cases with coronavirus disease 2019 in Wuhan, China. Clin Infect Dis 2020; 71: 769-77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Du Y, Tu L, Zhu P, et al. Clinical features of 85 fatal cases of COVID-19 from Wuhan. A retrospective observational study. Am J Respir Crit Care Med 2020; 201: 1372-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.An P, Chen H, Jiang X, et al. Clinical features of 2019 novel coronavirus pneumonia presented gastrointestinal symptoms but without fever onset. SSRN; 2020. 10.2139/ssrn.3532530. [DOI] [Google Scholar]
- 72.Rodríguez-Cola M, Jiménez-Velasco I, Gutiérrez-Henares F, et al. Clinical features of coronavirus disease 2019 (COVID-19) in a cohort of patients with disability due to spinal cord injury. Spinal Cord Series Cases 2020; 6: 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Huang C, Wang Y, Li X, et al. Clinical features of patients infected with 2019 novel coronavirus in Wuhan, China. Lancet 2020; 395: 497-506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Escalera-Antezana JP, Lizon-Ferrufino NF, Maldonado-Alanoca A, et al. Clinical features of the first cases and a cluster of Coronavirus Disease 2019 (COVID-19) in Bolivia imported from Italy and Spain. Travel Med Infect Dis 2020; 35: 101653. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Xu XW, Wu XX, Jiang XG, et al. Clinical findings in a group of patients infected with the 2019 novel coronavirus (SARS-Cov-2) outside of Wuhan, China: retrospective case series. BMJ 2020; 368: m606. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Zhang J, Liu ZH, Luo XH, et al. Clinical hallmarks of 13 COVID-19 patients revealing SAA biomarker. SSRN; 2020. 3546066. [Google Scholar]
- 77.Wang Y, Liu Y, Liu L, et al. Clinical outcomes in 55 patients with severe acute respiratory syndrome coronavirus 2 who were asymptomatic at hospital admission in Shenzhen, China. J Infect Dis 2020; 221: 1770-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Chen J, Qi T, Liu L, et al. Clinical progression of patients with COVID-19 in Shanghai, China. J Infect 2020; 80: e1-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Tu WJ, Cao J, Yu L, et al. Clinicolaboratory study of 25 fatal cases of COVID-19 in Wuhan. Intensive Care Medicine 2020; 46: 1117-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Zhao D, Yao F, Wang L, et al. A comparative study on the clinical features of COVID-19 pneumonia to other pneumonias. Clin Infect Dis 2020; 71: 756-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Wang L, Li X, Chen H, et al. Coronavirus disease 19 infection does not result in acute kidney injury: an analysis of 116 hospitalized patients from Wuhan, China. Am J Nephrol 2020; 51: 343-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Wang L, He W, Yu X, et al. Coronavirus disease 2019 in elderly patients: characteristics and prognostic factors based on 4-week follow-up. J Infect 2020; 80: 639-45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Zha L, Li S, Pan L, et al. Corticosteroid treatment of patients with coronavirus disease 2019 (COVID-19). Med J Australia 2020; 212: 416-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Akalin E, Azzi Y, Bartash R, et al. Covid-19 and kidney transplantation. N Engl J Med 2020; 382: 2475-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Kaye R, Chang CWD, Kazahaya K, et al. COVID-19 anosmia reporting tool: initial findings. Otolaryngol Head Neck Surg 2020; 163: 132-4. [DOI] [PubMed] [Google Scholar]
- 86.Cai Q, Huang D, Ou P, et al. COVID-19 in a designated infectious diseases hospital outside Hubei Province, China. Allergy 2020; 75: 1742-52. [DOI] [PubMed] [Google Scholar]
- 87.Bhatraju PK, Ghassemieh BJ, Nichols M, et al. COVID-19 in critically ill patients in the Seattle region – case series. N Engl J Med 2020; 382: 2012-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Fernández-Ruiz M, Andrés A, Loinaz C, et al. COVID-19 in solid organ transplant recipients: a single-center case series from Spain. Am J Transplant 2020; 20: 1849-58. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Feng Y, Ling Y, Bai T, et al. COVID-19 with different severities: a multicenter study of clinical features. Am J Respir Crit Care Med 2020; 201: 1380-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 90.COVID-19, Australia: Epidemiology Report 8 (Reporting period from 19:00 AEDT 14 March to 23:59 AEDT 22 March 2020). Commun Dis Intell (2018), 2020; 44. [DOI] [PubMed] [Google Scholar]
- 91.Lei Z, Cao H, Jie Y, et al. A cross-sectional comparison of epidemiological and clinical features of patients with coronavirus disease (COVID-19) in Wuhan and outside Wuhan, China. Travel Med Infect Dis 2020; 35: 101664. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wang J, Xu Z, Wang J, et al. , CT characteristics of patients infected with 2019 novel coronavirus: association with clinical type. Clin Radiol 2020; 75: 408-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Zhou S, Wang Y, Zhu T, et al. CT features of coronavirus disease 2019 (COVID-19) pneumonia in 62 patients in Wuhan, China. Am J Roentgenol 2020; 214: 1287-94. [DOI] [PubMed] [Google Scholar]
- 94.Klopfenstein T, Kadiane-Oussou NDJ, Royer PY, et al. Diarrhea: an underestimated symptom in Coronavirus disease 2019. Clin Res Hepatol Gastroenterol 2020; 44: 282-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 95.Han C, Duan C, Zhang S, et al. Digestive symptoms in COVID-19 patients with mild disease severity: clinical presentation, stool viral RNA testing, and outcomes. Am J Gastroenterol 2020; 115: 916-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 96.Luo S, Zhang X, Xu H. Don’t overlook digestive symptoms in patients with 2019 novel coronavirus disease (COVID-19). Clin Gastroenterol Hepatol 2020; 18: 1636-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Early Epidemiological and Clinical Characteristics of 28 cases of coronavirus Disease in South Korea. Osong Public Health Res Perspect 2020; 11: 8-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Horby P, Lim WS, Emberson J, et al. Effect of dexamethasone in hospitalized patients with COVID-19: preliminary report. medRxiv 2020; doi: 10.1101/2020.06.22.20137273. [DOI] [Google Scholar]
- 99.Zhou Z, Zhao N, Shu Y, et al. Effect of gastrointestinal symptoms on patients infected with COVID-19. Gastroenterology 2020; 158: 2294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Borba MGS, Val FFA, Sampaio VS, et al. Effect of high vs low doses of chloroquine diphosphate as adjunctive therapy for patients hospitalized with severe acute respiratory syndrome Coronavirus 2 (SARS-CoV-2) infection: a randomized clinical trial. JAMA Network Open 2020; 3: e208857. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 101.Xu X, M Han, T Li, et al. Effective treatment of severe COVID-19 patients with tocilizumab. Proc Natl Acad Sci USA 2020; 117: 10970-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102.Dong X, Cao YY, Lu XX, et al. Eleven faces of coronavirus disease 2019. Allergy 2020; 75: 1699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Song F, Shi N, Shan F, et al. , Emerging 2019 novel coronavirus (2019-NCoV) pneumonia. Radiology 2020; 295: 210-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 104.Wan Y, Li J, Shen L, et al. Enteric involvement in hospitalised patients with COVID-19 outside Wuhan. Lancet Gastroenterol Hepatol 2020; 5: 534-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Wang L, Duan Y, Zhang W, et al. Epidemiologic and clinical characteristics of 26 cases of covid-19 arising from patient-to-patient transmission in Liaocheng, China. Clin Epidemiol 2020; 12: 387-91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Qian GQ, Yang NB, Ding F, et al. Epidemiologic and Clinical characteristics of 91 hospitalized patients with COVID-19 in Zhejiang, China: a retrospective, multi-centre case series. QJM 2020; 113: 474-81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Chang D, Lin M, Wei L, et al. Epidemiologic and clinical characteristics of novel coronavirus infections involving 13 patients outside Wuhan, China. JAMA 2020; 323: 1092-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Young BE, Ong SWX, Kalimuddin S, et al. Epidemiologic features and clinical course of patients infected with SARS-CoV-2 in Singapore. JAMA 2020; 323: 1488-94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 109.Chen N, Zhou M, Dong X, et al. Epidemiological and clinical characteristics of 99 cases of 2019 novel coronavirus pneumonia in Wuhan, China: a descriptive study. Lancet 2020; 395: 507-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110.Kuang Y, Zhang H, Zhou R, et al. Epidemiological and clinical characteristics of 944 cases of 2019 novel coronavirus infection of non-COVID-19 Exporting City, Zhejiang, China. SSRN Electronic Journal 2020. 10.2139/ssrn.3543604. [DOI] [Google Scholar]
- 111.Wang R, Pan M, Zhang X, et al. Epidemiological and clinical features of 125 hospitalized patients with COVID-19 in Fuyang, Anhui, China. Int J Infect Dis 2020; 95: 421-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Xia XY, Wu J, Liu H, et al. Epidemiological and initial clinical characteristics of patients with family aggregation of COVID-19. J Clin Virol 2020; 127: 104360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 113.Zheng Y, Xu H, Yang M, et al. Epidemiological characteristics and clinical features of 32 critical and 67 noncritical cases of COVID-19 in Chengdu. J Clin Virol 2020; 127: 104366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 114.Jin X, Lian JS, Hu JH, et al. Epidemiological, clinical and virological characteristics of 74 cases of coronavirus-infected disease 2019 (COVID-19) with gastrointestinal symptoms. Gut 2020; 69: 1002-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Zhang X, Cai H, Hu J, et al. Epidemiological, clinical characteristics of cases of SARS-CoV-2 infection with abnormal imaging findings. Int J Infect Dis 2020; 94: 81-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Lian J, Jin X, Hao S, et al. Epidemiological, clinical, and virological characteristics of 465 hospitalized cases of coronavirus disease 2019 (COVID-19) from Zhejiang province in China. Influenza Other Respir Viruses 2020; 14: 564-74. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Lo IL, Lio CF, Cheong HH, et al. Evaluation of sars-cov-2 rna shedding in clinical specimens and clinical characteristics of 10 patients with COVID-19 in Macau. Int J Biol Sci 2020; 16: 1698-707. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.Xiao F, Tang M, Zheng X, et al. Evidence for gastrointestinal infection of SARS-CoV-2. Gastroenterology 2020; 158: 1831-3.e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Cai Q, Yang M, Liu D, et al. Experimental treatment with favipiravir for COVID-19: an open-label control study. Engineering 2020; 6: 1192-98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 120.Chan JFW, Yuan S, Kok KH, et al. A familial cluster of pneumonia associated with the 2019 novel coronavirus indicating person-to-person transmission: a study of a family cluster. Lancet 2020; 395: 514-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Zhang JC, Wang SB, Xue YD. Fecal specimen diagnosis 2019 novel coronavirus-infected pneumonia. J Med Virol 2020; 92: 680-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Spiteri G, Fielding J, Diercke M, et al. First cases of coronavirus disease 2019 (COVID-19) in the WHO European Region, 24 January to 21 February 2020. Euro Surveillance 2020; 25: 2000178. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 123.Million M, Lagier JC, Gautret P, et al. Early treatment of COVID-19 patients with hydroxychloroquine and azithromycin: a retrospective analysis of 1061 cases in Marseille, France. Travel Med Infect Dis 2020; 35: 101738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Hajifathalian K, Krisko T, Mehta A, et al. Gastrointestinal and hepatic manifestations of 2019 novel coronavirus disease in a large cohort of infected patients from New York: clinical implications. Gastroenterology 2020; 159: 1137-40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Nobel YR, Phipps M, Zucker J, et al. Gastrointestinal symptoms and COVID-19: case-control study from the United States. Gastroenterology 2020; 159: 373-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Lin L, Jiang X, Zhang Z, et al. Gastrointestinal symptoms of 95 cases with SARS-CoV-2 infection. Gut 2020; 159: 373-5. [DOI] [PubMed] [Google Scholar]
- 127.Cholankeril G, Podboy A, Aivaliotis VI, et al. High prevalence of concurrent gastrointestinal manifestations in patients with SARS-CoV-2: early experience from California. Gastroenterology 2020; 159: 775-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Dai H, Zhang X, Xia J, et al. High-resolution chest CT features and clinical characteristics of patients infected with COVID-19 in Jiangsu, China. Int J Infect Dis 2020; 95: 106-12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Tang W, Cao Z, Han M, et al. , Hydroxychloroquine in patients with mainly mild to moderate coronavirus disease 2019: open label, randomised controlled trial. BMJ 2020; 369: m1849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Gritti G, Raimondi F, Ripamonti D, et al. IL-6 signalling pathway inactivation with siltuximab in patients with COVID-19 respiratory failure: an observational cohort study. medRxiv 2020. doi: 10.1101/2020.04.01.20048561. [DOI] [Google Scholar]
- 131.Xu X, Yu C, Qu J, et al. Imaging and clinical features of patients with 2019 novel coronavirus SARS-CoV-2. Eur J Nucl Med Mol Imaging 2020; 47: 1275-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Zhou S, Zhu T, Wang Y, et al. Imaging features and evolution on CT in 100 COVID-19 pneumonia patients in Wuhan, China. Eur Radiol 2020; 30: 5446-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Pung R, Chiew CJ, Young BE, et al. Investigation of three clusters of COVID-19 in Singapore: implications for surveillance and response measures. Lancet 2020; 395: 1039-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Kim ES, Chin BS, Kang CK, et al. Clinical course and outcomes of patients with severe acute respiratory syndrome coronavirus 2 infection: a preliminary report of the first 28 patients from the Korean Cohort Study on COVID-19. J Korean Med Sci 2020; 35: e142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Wei XS, Wang X, Peng WB, et al. Clinical characteristics of SARS-CoV-2 infected pneumonia with diarrhea. Lancet Respir Med 2019. 10.2139/ssrn.3546120. [DOI] [Google Scholar]
- 136.Qi X, Liu C, Jiang Z, et al. Multicenter analysis of clinical characteristics and outcomes in patients with COVID-19 who develop liver injury. J Hepatol 2020; 73: 455-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Geleris J, Sun Y, Platt J, et al. Observational study of hydroxychloroquine in hospitalized patients with Covid-19. N Engl J Med 2020; 73: 2411-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138.Morena V, Milazzo L, Oreni L, et al. Off-label use of tocilizumab for the treatment of SARS-CoV-2 pneumonia in Milan, Italy. Eur J Intern Med 2020; 76: 36-42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 139.Lechien JR, Chiesa-Estomba C, De Siati DR, et al. Olfactory and gustatory dysfunctions as a clinical presentation of mild-to-moderate forms of the coronavirus disease (COVID-19): a multicenter European study. Eur Arch Otorhinolaryngol 2020; 277: 2251-61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140.Yu Y, Xu D, Fu S, et al. Patients with COVID-19 in 19 ICUs in Wuhan, China: a cross-sectional study. Critical Care 2020; 24: 219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 141.Sciascia S, Aprà F, Baffa A, et al. Pilot prospective open, single-arm multicentre study on off-label use of tocilizumab in patients with severe COVID-19. Clin Exp Rheumatol 2020; 38: 529-32. [PubMed] [Google Scholar]
- 142.Du RH, Liang LR, Yang CQ, et al. Predictors of mortality for patients with COVID-19 pneumonia caused by SARSCoV- 2: a prospective cohort study. Eur Respir J 2020; 55: 2000524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143.Richardson S, Hirsch JS, Narasimhan M, et al. Presenting characteristics, comorbidities, and outcomes among 5700 patients hospitalized with COVID-19 in the New York City Area. JAMA 2020; 323: 2052-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144.Redd WD, Zhou JC, Hathorn KE, et al. Prevalence and characteristics of gastrointestinal symptoms in patients with SARS-CoV-2 infection in the United States: a multicenter cohort study. Gastroenterology 2020; 159: 765-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145.Wu Y, Guo C, Tang L, et al. Prolonged presence of SARS-CoV-2 viral RNA in faecal samples. Lancet Gastroenterol Hepatol 2020; 5: 434-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146.Shi H, Han X, Jiang N, et al. Radiological findings from 81 patients with COVID-19 pneumonia in Wuhan, China: a descriptive study. Lancet Infect Dis 2020; 20: 425-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147.Huang L, Zhang X, Zhang X, et al. Rapid asymptomatic transmission of COVID-19 during the incubation period demonstrating strong infectivity in a cluster of youngsters aged 16-23 years outside Wuhan and characteristics of young patients with COVID-19: a prospective contact-tracing study. J Infect 2020; 80: e1-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 148.Zhao W, Zhong Z, Xie X, et al. Relation between chest CT findings and clinical conditions of coronavirus disease (covid-19) pneumonia: a multicenter study. Am J Roentgenol 2020; 214: 1072-7. [DOI] [PubMed] [Google Scholar]
- 149.Beigel JH, Tomashek KM, Dodd LE, et al. Remdesivir for the treatment of Covid-19 – preliminary report. N Engl J Med 2020; 383: 1813-26. [DOI] [PubMed] [Google Scholar]
- 150.Wang Y, Zhang D, Du G, et al. Remdesivir in adults with severe COVID-19: a randomised, double-blind, placebo-controlled, multicentre trial. Lancet 2020; 395: 1569-78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 151.Chen Q, Quan B, Li X, et al. A report of clinical diagnosis and treatment of nine cases of coronavirus disease 2019. J Med Virol 2020; 92: 683-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 152.Fan H, Zhang L, Huang B, et al. Retrospective analysis of clinical features in 101 death cases with COVID-19. medRxiv 2020, [Google Scholar]
- 153.Wu C, Chen X, Cai Y, et al. Risk factors associated with acute respiratory distress syndrome and death in patients with Coronavirus disease 2019 pneumonia in Wuhan, China. JAMA Int Med 2020; 180: 934-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 154.Kluytmans M, Buiting A, Pas S, et al. SARS-CoV-2 infection in 86 healthcare workers in two Dutch hospitals in March 2020. medRxiv 2020. doi: 10.1101/2020.03.23.20041913. [DOI] [Google Scholar]
- 155.Zou L, Ruan F, Huang M, et al. , SARS-CoV-2 viral load in upper respiratory specimens of infected patients. N Engl J Med 2020; 382: 1177-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 156.Giacomelli A, Pezzati L, Conti F, et al. Self-reported olfactory and taste disorders in SARS-CoV-2 patients: a cross-sectional study. Clin Infect Dis 2020; (Xx Xxxx): p. 2-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 157.Meng Y, Wu P, Lu W, et al. Sex-specific clinical characteristics and prognosis of coronavirus disease-19 infection in Wuhan, China: a retrospective study of 168 severe patients. PLoS Pathog 2020; 16: e1008520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 158.Ding X, Xu J, Zhou J, et al. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information. 2020. (January). [Google Scholar]
- 159.Gautret P, Lagier JC, Parola P, et al. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information. 2020. (January). [Google Scholar]
- 160.Huang Y, Tu M, Wang S, et al. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information. 2020. (January). [Google Scholar]
- 161.Li X, Xu S, Yu M, et al. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect , the company’s public news and information. 2020. (January). [Google Scholar]
- 162.Liu K, Chen Y, Lin R, et al. Since January 2020 Elsevier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information. 2020. (January). [Google Scholar]
- 163.Roland LT, Gurrola JG, Loftus 2nd PA, et al. Smell and taste symptom-based predictive model for COVID-19 diagnosis. Int Forum Allergy Rhinol 2020; 10: 832-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 164.Moein ST, Hashemian SMR, Mansourafshar B, et al. Smell dysfunction: a biomarker for COVID-19. Int Forum Allergy Rhinol 2020; 10: 944-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 165.Bangalore S, Sharma A, Slotwiner A, et al. ST-segment elevation in patients with Covid-19 – a case series. N Engl J Med 2020; 2: 17-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 166.Pan F, Ye T, Sun P, et al. Time course of lung changes at chest CT during recovery from coronavirus disease 2019 (COVID-19). Radiology 2020; 295: 715-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 167.Toniati P, Piva S, Cattalini M, et al. Tocilizumab for the treatment of severe COVID-19 pneumonia with hyperinflammatory syndrome and acute respiratory failure: a single center study of 100 patients in Brescia, Italy. Autoimmun Rev 2020; 19: 102568. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 168.Wang M, Guo L, Chen Q, et al. Typical radiological progression and clinical features of patients with coronavirus disease 2019. Aging 2020; 12: 7652-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 169.Deng Q, Hu B, Zhang Y, et al. vier has created a COVID-19 resource centre with free information in English and Mandarin on the novel coronavirus COVID-19. The COVID-19 resource centre is hosted on Elsevier Connect, the company’s public news and information. 2020. (January). [Google Scholar]
- 170.Wölfel R, Corman VM, Guggemos W, et al. Virological assessment of hospitalized patients with COVID-2019. Nature 2020; 581: 465-9. [DOI] [PubMed] [Google Scholar]
- 171.Alkhouli M, Nanjundappa A, Annie F, et al. Sex differences in case fatality rate of COVID-19: insights from a multinational registry. Mayo Clinic Proc 2020; 95: 1613-20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 172.Klein SL, Hodgson A, Robinson DP. Mechanisms of sex disparities in influenza pathogenesis. J Leukocyte Biol 2012; 92: 67-73. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 173.Avitsur R, Mays JW, Sheridan JF. Sex differences in the response to influenza virus infection: modulation by stress. Hormones Behavior 2011; 59: 257-64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 174.Jin JM, Bai P, He W, et al. Gender differences in patients with COVID-19: focus on severity and mortality. Front Public Health 2020; 8: 152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 175.Yang J, Zheng, Gou X, et al. Prevalence of comorbidities and its effects in patients infected with SARS-CoV-2: a systematic review and meta-analysis. Int J Infect Dis 2020; 94: 91-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 176.Sattar N, McInnes IB, McMurray JJV. Obesity is a risk factor for severe COVID-19 infection: multiple potential mechanisms. Circulation 2020; 142: 4-6. [DOI] [PubMed] [Google Scholar]
- 177.Usman MS, Siddiqi TJ, Khan MS, et al. Is there a smoker’s paradox in COVID-19? BMJ Evid Based Med 2021; 26: 279-84. [DOI] [PubMed] [Google Scholar]
- 178.O’Donnell CJ, Elosua R. Cardiovascular risk factors. Insights from Framingham Heart Study. Rev Esp Cardiol 2008; 61: 299-310. [PubMed] [Google Scholar]
- 179.Prevention, C.f.D.C.a . People at High Risk For Flu Complications. 2020. July 14, 2020. Available from: https://www.cdc.gov/flu/highrisk/index.htm.
- 180.Bandyopadhyay D, Akhtar T, Hajra A, et al. COVID-19 pandemic: cardiovascular complications and future implications. Am J Cardiovasc Drugs 2020; 20: 311-24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 181.Fang L, Karakiulakis G, Roth M. Are patients with hypertension and diabetes mellitus at increased risk for COVID-19 infection? Lancet Respir Med 2020; 8: e21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 182.Wang X, Fang X, Cai Z, et al. Comorbid chronic diseases and acute organ injuries are strongly correlated with disease severity and mortality among COVID-19 patients: a systemic review and meta-analysis. Research 2020; 2020: 2402961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 183.Sedaghat AR, Gengler I, Speth MM. Olfactory dysfunction: a highly prevalent symptom of COVID-19 with public health significance. Otolaryngol Head Neck Surg 2020; 163: 12-5. [DOI] [PubMed] [Google Scholar]
- 184.Cipollaro L, Giordano L, Padulo J, et al. Musculoskeletal symptoms in SARS-CoV-2 (COVID-19) patients. J Orthop Surg Res 2020; 15: 178. [DOI] [PMC free article] [PubMed] [Google Scholar]