Abstract
Head injuries are the most common type of birth injuries. Among them, most of the injuries is limited to the scalp. and the prognosis is good enough to be unnoticed in some cases. Intracranial injuries caused by excessive forces during delivery are rare. However, since some of them can be fatal, it is necessary to suspect it at an early stage and evaluate thoroughly if there are abnormal findings in the patient.
Keywords: Birth injuries, Birth trauma, Intracranial hemorrhages, Scalp injuries, Skull fractures
INTRODUCTION
Birth injury is defined as a condition that affects neonate’s structure and function caused by an adverse event at birth. It is often used interchangeably with “birth trauma”. However, it is also used as a more comprehensive term because it includes effects other than trauma, for example, hypoxic insult. In this article, the term “birth injury” was limited to the same meaning as birth trauma.
The incidence of birth injury is known to be about 2% for normal vaginal delivery and 1% for cesarean delivery [1,11]. According to the latest statistics in the USA, it is known that birth injury occurs in about 25.3 to 31.1 cases per 1000 hospital births [15]. Since the head is the first part to enter the birth canal during delivery, it is one of the most vulnerable area to birth injury. The frequency of cranial birth injury is gradually increasing, but this is due to an increase in minor scalp injuries, and rather, major injuries are on a decreasing trend. Although most cranial birth injuries are self-limiting and have a good prognosis, major birth injuries increase the health care burden. Risk factors for cranial birth injuries include large for gestational age neonate, precipitous labor, vaginal delivery using instruments such as force or vacuum extraction and malpresentation at delivery [5,9,21,31].
Cranial birth injuries dealt with in the field of neurosurgery range from minor scalp injuries to major injuries such as skull fractures or intracranial hemorrhages. In this review paper, we would like to summarize these injuries.
SCALP INJURIES
Scalp injuries are the most common birth injuries and account for about 80% of all birth injuries [15]. Males have higher odds of scalp injuries than females, and Asians have higher odds of scalp injuries than Caucasians. In most cases of scalp injuries, conservative management is sufficient because they usually heal spontaneously without any intervention. These soft tissue injuries of the scalp are classified according to the layer of scalp involved.
Caput succedaneum
It is a type of scalp injury commonly observed in vaginal delivery. Margin is not clearly defined because the injury occurs in the subcutaneous layer. Since it is an extraperiosteal lesion, it can be observed beyond the suture lines and midline. It is self-limited and is absorbed within a few days and requires no treatment.
Subgaleal hematoma
Subgaleal hematoma refers to the occurrence of hematoma in the space between galea aponeurosis and periosteum caused by emissary vein injury during delivery. For this space is a potential space of loose connective tissue, the hematoma could spatially spread beyond suture lines, and its amount could gradually increase over time.
The occurrence of subgaleal hematoma is rare, about 1.5 to four cases per 10000 cases in normal vaginal delivery [10,28]. However, it greatly increases to 59 cases per 100000 cases when vacuum is used during labor. According to a study in the 1990s [6], 90% of cases with subgaleal hematoma were associated with intrument-assisted deliveries, and in 40% of patients, other kinds of head injury was accopanied such as intracranial hemorrhage, skull fracture, or cerebral edema. Recent domestic studies showed similar data [20]. Seventy percent of patients received vacuum-assisted vaginal delivery, and 20% of patients received vacuum-assisted cesarean section, thus 90% of patients were delivered with the assistance of the instruments. Among them, comorbid intracranial injury presents in 75% of cases, and the morbidity rate was 41.2%.
A diagnosis is made based on inspection and palpation of the diffuse, soft, and fluctuant mass is sufficient for the diagnosis of the subgaleal hematoma. As a large amount of bleeding can be life-threatening, early detection and careful monitoring is important in those cases. During monitoring, changes in vital signs and increase in head circumference should be checked. Required laboratory tests includes hemoglobin or hematocrit levels in the blood and the coagulation tests. Cranial ultrasonography is helpful to evaluate the extent and to screen for associated intracranial lesions. Computed tomography (CT) and magnetic resonance imaging (MRI) is useful for the evaluation of intracranial lesions, however, it should be performed in consideration of the patient’s clinical conditions and necessities.
The long-term prognosis is usually good. Management involves watchful observation and correction of hypovolemia and anemia. Thereafter, monitoring and correction for developing hyperbilirubinemia and other combined medical conditions such as metabolic acidosis is required in some cases. Although it is rarely required, surgical evacuation is performed when massive subgaleal hematomas produce neurological deteriorations with the evidence of increased intracranial pressure on images [2].
Cephalhematoma
Cephalhematoma is an accumulation of hematoma in the subperiosteal space. It is known to occur in 0.4–3% of all deliveries [14,18]. It often occurs in the parietal bone. As with other scalp injuries described above, it occurs more frequently in neonates delivered with the assitance of instruments [22].
Unlike subgaleal hematoma, cephahematoma does not cross suture lines. Therefore, cephalhematoma is more self-limited than subgaleal hematoma, and its clinical course is usually favorable. Treatment is usually conservative observation until absorption. Aspiration and drain are generally ineffective for clotted blood and not recommended due to the potential risk of infection. In the case of large amounts of hematoma, there are reports of experiences with aspiration or surgical evacuation for better esthetic outcomes [4,13]. Most cephalhematoma resolves spontaneously within a few days, but in some cases, it may take several weeks [22]. In those cases, calcification may also occur from collected blood. If disfiguration is severe, surgical treatment could be considered [8,33,34]. Rarely, cephalhematoma becomes infected even without laceration or abrasion (Fig. 1) [7]. The major causative organism is Escherichia coli. It could be accompanied by osteomyelitis, meningitis, or sepsis. When infected cephalhematoma is suspected, diagnostic aspiration should be performed [19].
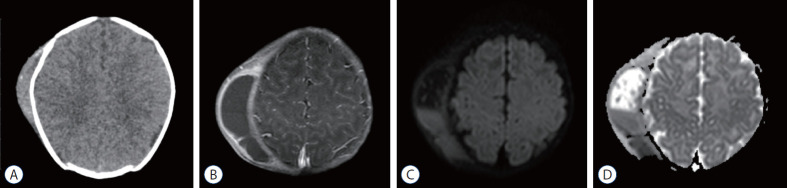
Fig. 1.
A : A brain computed tomography image of 26-day-old girl who presented with swelling of her head not crossing suture lines. Additional magnetic resonance imaging (MRI) (B-D) were obtained due to progression of swelling with fever. MRI demonstrates thickening of the wall with septation (B) and fluid-fluid level with diffusion restriction (C and D) which suggests combined infection. Further aspiration with culture study revealed that infected cephalhematoma caused by Escherichia coli.
SKULL FRACTURES
Skull of the newborn can be molded during delivery and is resistant to fracture because it is separated into several bones [24]. However, although it is rare, skull fracture could occur at birth if there are difficulties during delivery. The overall fracture incidence was 2–3.7 per 100000 live births [12,17]. Some insists on that this data is underestimated because of undetected clinically silent simple linear fractures [3,17,25].
As with scalp birth injury, it can be observed more frequently in instrument-assisted delivery. About 46% of birth-related skull fractures are associated with vaccum-assisted vaginal delivery [17]. Most cases are diagnosed on the date of birth or within a few days after birth. Most of birth-related skull fractures are linear fractures in the parietal bone. Sometimes, in the setting of a forceps delivery, depressed fractures (also known as ping-pong fractures) can also occur which is not common in uncomplicated vaginal deliveries (Fig. 2) [30].
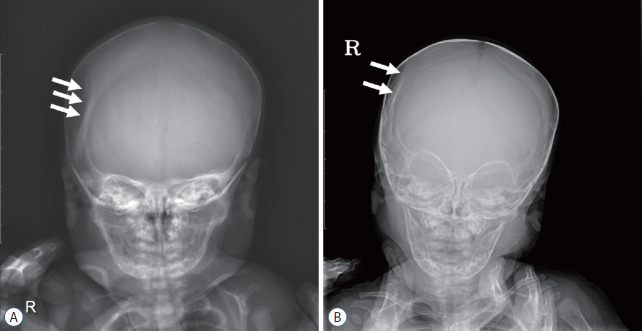
Fig. 2.
A : A simple skull radiograph of 2-day-old girl shows depressed skull fractures (arrows). B : On follow up images at 6-month-old age demonstrates quite improvements (arrows).
Simple linear fractures can be identified by skull radiographs. However, for physicians who are less experienced in pediatric patients, it can be difficult to detect fractures on plain skull radiographs. This is because neonate skulls are less mineralized and have wide sutures. It is reported that 23% of birth-related fracture cases that required hospitalization were hard to detect their fractures on simple radiographs [24]. Nevertheless, considering favorable clinical course of simple linear fractures and to avoid unnecessary additional radiation exposures, further imaging such as CT has not been recommended [26,29]. Meanwhile, depressed skull fractures usually require additinoal imaging studies. With low-dose CT and 3D reconstruction, the detection of fractures could be made much easier without further increase in radiation exposure [23,27].
Extracranial scalp injury especially cephalhematoma is frequently observed together in birth-related skull fractures, however, intracranial hemorrhage is rare. When intracranial hemorrhage is present, seizures, apneic events, or neurological abnormalities are often found together on clinical examination. If these abnormalities are present, further imaging study such as CT scans should be considered to exclude the presence of intracranial lesions, although there is a little consensus or recommendation for image modality and follow up intervals [24].
If there is fracture without other intracranial injuries, it can be managed conservatively. Even in the cases of depressed skull fracture, most of them can be resolved spontaneously. Surgical reduction could be considered depending on its severity.
INTRACRANIAL HEMORRHAGE
Intracranial hemorrhage during delivery is rare but can cause brain injuries in the neonate. Severity of perinatal traumatic brain injury ranges from clinically silent to fatal. Diagnosing intracranial injury in neonate is sometimes difficult. First, open fontanelles and unfused sutures allows intracranial compliance buffering mass effect caused by hematoma. Second, early detection of neurological symptoms and signs of neonate is not easy. For example, seizures in neonates appear very subtle and brief, and this makes them hard to be recognized. Finally, if the patient’s condition is unstable, there may be a delay in intracranial imaging.
Data on the incidence of intracranial hemorrhage are lacking, but according to the results of one study, the regional incidence of symptomatic intracranil hemorrhage in full-term infants is known to be 2.7 per 100000 live births [16]. Instrumental delivery, macrosomia, and abrupt labor are known risk factors for neonatal intracranial injury [32]. When forces from the maternal pelvic outlet or external environment applied to infant’s head during delivery and they exceed beyond compensation by molding of infant’s head, they might act as shearing forces to intracranial vessels such as meiningeal vessels (epidural hemorrhage), bridging veins (subdural hemorrhage) or leptomeningeal vessels (subarachnoid hemorrhages).
When the amount of intracranial bleeding is small, it is often clinically silent. Seizures can be observed. As the bleeding volume increases, symptoms and signs of increased intracranial pressure caused by mass effect may occur. In neonate, this includes systemic signs such as irritability, lethargy, bradycardia or apnea as well as physical signs like bulging fontanelle or sutural diastases. Ultrasonography is a good imaging tool for screening and early diagnosis of intracranial hemorrhages in neonate. If the patient’s condition is available, MRI is the modality of choice for clear assessment. CT can be also considered for faster scan time. If necessary, test for coagulopathy should be performed.
If there is a large amount of bleeding and a mass effect exists, craniotomy may be considered. However, if craniotomy is difficult depending on the patient’s condition, it may have to be solved with a limited approach (Fig. 3). If hydrocephalus follows bleeding, surgical treatment for hydrocephalus is also required.
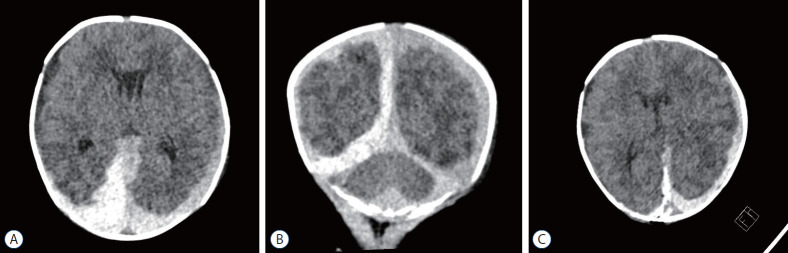
Fig. 3.
An axial (A) and a coronal (B) computed tomography (CT) images of 2-day-old girl who presented with lethargy and intermittent apnea. Images show subdural hemorrhages on bilateral convexities and along the falx and the tentorium. The physical examination revealed a tense and bulging anterior fontanelle. The patient was treated by burr holetrephination and drainage of subdural hemorrhage. A postoperative CT image (C) reveals improvement of mass effect. Courtesy of Dr. Youngbeom Seo; Department of Neurosurgery, Yeungnam University Hospital.
CONCLUSIONS
Head injury is common birth-related injury and usually has good prognosis. In rare cases of intracranial injury, surgical treatment is required. Early diagnosis and prompt treatment are necessary, although there might be limitations because patients are too young or have accompanying morbidities.
Footnotes
Conflicts of interest
No potential conflict of interest relevant to this article was reported.
Informed consent
This type of study does not require informed consent.
Author contributions
Conceptualization : SC; Data curation : SC; Visualization : SC; Writing - original draft : SC; Writing - review & editing : SC
Data sharing
None
Preprint
None
References
- 1.Alexander JM, Leveno KJ, Hauth J, Landon MB, Thom E, Spong CY, et al. Fetal injury associated with cesarean delivery. Obstet Gynecol. 2006;90:885–890. doi: 10.1097/01.AOG.0000237116.72011.f3. [DOI] [PubMed] [Google Scholar]
- 2.Amar AP, Aryan HE, Meltzer HS, Levy ML. Neonatal subgaleal hematoma causing brain compression: report of two cases and review of the literature. Neurosurgery. 2003;4:1470–1474. doi: 10.1227/01.neu.0000065180.07961.54. [DOI] [PubMed] [Google Scholar]
- 3.Ami O, Maran JC, Gabor P, Whitacre EB, Musset D, Dubray C, et al. Three-dimensional magnetic resonance imaging of fetal head molding and brain shape changes during the second stage of labor. PLoS One. 2003;14:e0215721. doi: 10.1371/journal.pone.0215721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Blanc F, Bigorre M, Lamouroux A, Captier G. Early needle aspiration of large infant cephalohematoma: a safe procedure to avoid esthetic complications. Eur J Pediatr. 2020;179:265–269. doi: 10.1007/s00431-019-03487-5. [DOI] [PubMed] [Google Scholar]
- 5.Boulet SL, Alexander GR, Salihu HM, Pass M. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol. 2003;188:1372–1378. doi: 10.1067/mob.2003.302. [DOI] [PubMed] [Google Scholar]
- 6.Chadwick LM, Pemberton PJ, Kurinczuk JJ. Neonatal subgaleal haematoma: associated risk factors, complications and outcome. J Paediatr Child Health. 1996;32:228–232. doi: 10.1111/j.1440-1754.1996.tb01559.x. [DOI] [PubMed] [Google Scholar]
- 7.Chang HY, Chiu NC, Huang FY, Kao HA, Hsu CH, Hung HY. Infected cephalohematoma of newborns: experience in a medical center in Taiwan. Pediatr Int. 2005;47:274–277. doi: 10.1111/j.1442-200x.2005.02062.x. [DOI] [PubMed] [Google Scholar]
- 8.Chung HY, Chung JY, Lee DG, Yang JD, Baik BS, Hwang SG, et al. Surgical treatment of ossified cephalhematoma. J Craniofac Surg. 2004;15:774–779. doi: 10.1097/00001665-200409000-00015. [DOI] [PubMed] [Google Scholar]
- 9.Cieplinski JAM, Bhutani VK. Lactational and neonatal morbidities associated with operative vaginal deliveries. 1191. Pediatric Research. 1996;39:201. [Google Scholar]
- 10.Davis DJ. Neonatal subgaleal hemorrhage: diagnosis and management. CMAJ. 2001;164:1452–1453. [PMC free article] [PubMed] [Google Scholar]
- 11.Demissie K, Rhoads GG, Smulian JC, Balasubramanian BA, Gandhi K, Joseph KS, et al. Operative vaginal delivery and neonatal and infant adverse outcomes: population based retrospective analysis. BMJ. 2004;329:24–29. doi: 10.1136/bmj.329.7456.24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dupuis O, Silveira R, Dupont C, Mottolese C, Kahn P, Dittmar A, et al. Comparison of “instrument-associated” and “spontaneous” obstetric depressed skull fractures in a cohort of 68 neonates. Am J Obstet Gynecol. 2005;192:165–170. doi: 10.1016/j.ajog.2004.06.035. [DOI] [PubMed] [Google Scholar]
- 13.Eseonu CI, Sacino AN, Ahn ES. Early surgical intervention for a large newborn cephalohematoma. Pediatr Neurosurg. 2016;51:210–213. doi: 10.1159/000444195. [DOI] [PubMed] [Google Scholar]
- 14.Firlik KS, Adelson PD. Large chronic cephalohematoma without calcification. Pediatr Neurosurg. 1999;30:39–42. doi: 10.1159/000028759. [DOI] [PubMed] [Google Scholar]
- 15.Gupta R, Cabacungan ET. Neonatal birth trauma: analysis of yearly trends, tisk factors, and outcomes. J Pediatr. 2021;238:174–180. doi: 10.1016/j.jpeds.2021.06.080. [DOI] [PubMed] [Google Scholar]
- 16.Hanigan WC, Powell FC, Miller TC, Wright RM. Symptomatic intracranial hemorrhage in full-term infants. Childs Nerv Syst. 1995;11:698–707. doi: 10.1007/BF00262235. [DOI] [PubMed] [Google Scholar]
- 17.Högberg U, Fellman V, Thiblin I, Karlsson R, Wester K. Difficult birth is the main contributor to birth-related fracture and accidents to other neonatal fractures. Acta Paediatr. 2020;109:2040–2048. doi: 10.1111/apa.15217. [DOI] [PubMed] [Google Scholar]
- 18.Kendall N, Woloshin H. Cephalhematoma associated with fracture of the skull. J Pediatr. 1952;41:125–132. doi: 10.1016/s0022-3476(52)80047-2. [DOI] [PubMed] [Google Scholar]
- 19.LeBlanc CM, Allen UD, Ventureyra E. Cephalhematomas revisited. when should a diagnostic tap be performed? Clin Pediatr (Phila) 1995;34:86–89. doi: 10.1177/000992289503400204. [DOI] [PubMed] [Google Scholar]
- 20.Lee SJ, Kim JK, Kim SJ. The clinical characteristics and prognosis of subgaleal hemorrhage in newborn. Korean J Pediatr. 2018;61:387–391. doi: 10.3345/kjp.2018.06800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Levine MG, Holroyde J, Woods JR, Jr, Siddiqi TA, Scott M, Miodovnik M. Birth trauma: incidence and predisposing factors. Obstet Gynecol. 1984;63:792–795. [PubMed] [Google Scholar]
- 22.Mangurten H, Puppala B. Birth injuries. Fanaroff and Martin’s Neonatal Perinatal Medicine-Diseases of the Fetus and Newborn. ed 8. Philadelphia: Mosby Elsevier; 2006. pp. 529–559. [Google Scholar]
- 23.Martin A, Paddock M, Johns CS, Smith J, Raghavan A, Connolly DJA, et al. Avoiding skull radiographs in infants with suspected inflicted injury who also undergo head CT: “a no-brainer?”. Eur Radiol. 2020;30:1480–1487. doi: 10.1007/s00330-019-06579-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Merhar SL, Kline-Fath BM, Nathan AT, Melton KR, Bierbrauer KS. Identification and management of neonatal skull fractures. J Perinatol. 2016;36:640–642. doi: 10.1038/jp.2016.53. [DOI] [PubMed] [Google Scholar]
- 25.Nachtergaele P, Van Calenbergh F, Lagae L. Craniocerebral birth injuries in term newborn infants: a retrospective series. Childs Nerv Syst. 2017;33:1927–1935. doi: 10.1007/s00381-017-3539-2. [DOI] [PubMed] [Google Scholar]
- 26.Nakahara K, Shimizu S, Kitahara T, Oka H, Utsuki S, Soma K, et al. Linear fractures invisible on routine axial computed tomography: a pitfall at radiological screening for minor head injury. Neurol Med Chir (Tokyo) 2011;51:272–274. doi: 10.2176/nmc.51.272. [DOI] [PubMed] [Google Scholar]
- 27.Orman G, Wagner MW, Seeburg D, Zamora CA, Oshmyansky A, Tekes A, et al. Pediatric skull fracture diagnosis: should 3D CT reconstructions be added as routine imaging? J Neurosurg Pediatr. 2015;16:426–431. doi: 10.3171/2015.3.PEDS1553. [DOI] [PubMed] [Google Scholar]
- 28.Plauché WC. Subgaleal hematoma. a complication of instrumental delivery. JAMA. 1980;244:1597–1598. [PubMed] [Google Scholar]
- 29.Quayle KS, Jaffe DM, Kuppermann N, Kaufman BA, Lee BC, Park TS, et al. Diagnostic testing for acute head injury in children: when are head computed tomography and skull radiographs indicated? Pediatrics. 1997;99:E11. doi: 10.1542/peds.99.5.e11. [DOI] [PubMed] [Google Scholar]
- 30.Reichard R. Birth injury of the cranium and central nervous system. Brain Pathol. 2008;18:565–570. doi: 10.1111/j.1750-3639.2008.00205.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Robinson S. Neonatal posthemorrhagic hydrocephalus from prematurity: pathophysiology and current treatment concepts. J Neurosurg Pediatr. 2012;9:242–258. doi: 10.3171/2011.12.PEDS11136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Towner D, Castro MA, Eby-Wilkens E, Gilbert WM. Effect of mode of delivery in nulliparous women on neonatal intracranial injury. N Engl J Med. 1999;341:1709–1714. doi: 10.1056/NEJM199912023412301. [DOI] [PubMed] [Google Scholar]
- 33.Ulma RM, Sacks G, Rodoni BM, Duncan A, Buchman AT, Buchman BC, et al. Management of calcified cephalohematoma of infancy: the University of Michigan 25-year experience. Plast Reconstr Surg. 2021;148:409–417. doi: 10.1097/PRS.0000000000008199. [DOI] [PubMed] [Google Scholar]
- 34.Wong CH, Foo CL, Seow WT. Calcified cephalohematoma: classification, indications for surgery and techniques. J Craniofac Surg. 2006;17:970–979. doi: 10.1097/01.scs.0000229552.82081.de. [DOI] [PubMed] [Google Scholar]