Abstract
Background/Aims
Rapid percutaneous coronary intervention (PCI) is the cornerstone of treatment for ST-elevation myocardial infarction (STEMI). However, there have been conflicting results regarding the differences in clinical outcomes between on-hours and off-hours presentation in STEMI patients. We aimed to examine the difference in long-term outcomes between off-hours and on-hours PCI in patients with STEMI.
Methods
The characteristics and clinical outcomes of 5,364 STEMI patients between November 2011 and June 2015 from the Korea Acute Myocardial Infarction Registry-National Institutes of Health (KAMIR-NIH) registry were analyzed. Patients were divided into two groups: the off-hours group (weekdays from 6:01 PM to 7:59 AM, weekends, and legal holidays) and the on-hours group (weekdays from 8:00 AM to 6:00 PM). Major adverse cardiac and cerebrovascular events (MACCEs) were defined as a composite of all-cause mortality, non-fatal myocardial infarction, any revascularization, cerebrovascular accident, and stent thrombosis. The primary endpoint was the occurrence of MACCEs, and all other clinical outcomes were analyzed.
Results
A total of 3,119 patients (58.1%) underwent primary PCI due to STEMI during off-hours and 2,245 patients (41.9%) during on-hours. At 36 months, the clinical outcomes of the off-hours group were similar to those of the on-hours group in both the unadjusted and propensity score weighting-adjusted analyses.
Conclusions
Our analysis revealed that the long-term outcomes in STEMI patients admitted to hospitals during off-hours were similar to outcomes of those admitted during on-hours.
Keywords: Percutaneous coronary intervention, ST elevation myocardial infarction, Treatment outcome, Republic of Korea
Graphical abstract
INTRODUCTION
The prevalence of acute myocardial infarction (AMI) is gradually increasing, which contributes to a high proportion of socioeconomic problems. This condition is recognized as an emergent medical situation. In particular, ST-elevation myocardial infarction (STEMI) is an emergency requiring primary percutaneous coronary intervention (PCI) of the infarct-related arteries [1]. Moreover, timely PCI is considered to be the cornerstone of the treatment strategy for AMI, including STEMI.
It is important to determine whether the efficacy of PCI in AMI during off-hours is comparable to that during on-hours. In a literature review, we found articles on the difference between on and off-duty PCI. Some studies reported that AMI had worse clinical outcomes when it occurred during off than on-hours [2,3]. In contrast, other reports showed no significant differences in the clinical outcomes between on-hours and off-hours [4–6]. In addition to clinical studies on the overall AMI population, controversial results have been reported in comparative studies among STEMI patients [7–10]. Hence, it is still contentious whether off-hours presentation is indeed different from on-hours presentation in terms of clinical outcomes among STEMI patients. Furthermore, there is a paucity of clinical studies concerning the outcomes in patients with STEMI undergoing primary PCI in relation to the time of visit to the hospital in the Republic of Korea.
Therefore, in this study, we aimed to investigate the relation between time of hospital visit and clinical outcomes in patients with STEMI undergoing primary PCI from the Republic of Korea.
METHODS
Study population
The clinical information on study population was extracted from the Korea Acute Myocardial Infarction Registry-National Institutes of Health (KAMIR-NIH) registry, a nationwide, multicenter, and online-based observational cohort study. The KAMIR-NIH is also a prospective registry that gradually enrolled AMI patients from about 20 major cardiovascular centers eligible for primary PCI from 2011 to 2015. The registry contains data on characteristics and clinical outcomes of Korean patients with AMI, reflecting the prognostic and surveillance indexes. These data were collected by an attending physician and trained clinical research coordinators using an online-based case report form in a clinical data management system. The study protocol for the KAMIR-NIH was previously published and approved by the ethics committee of each participating institution [11].
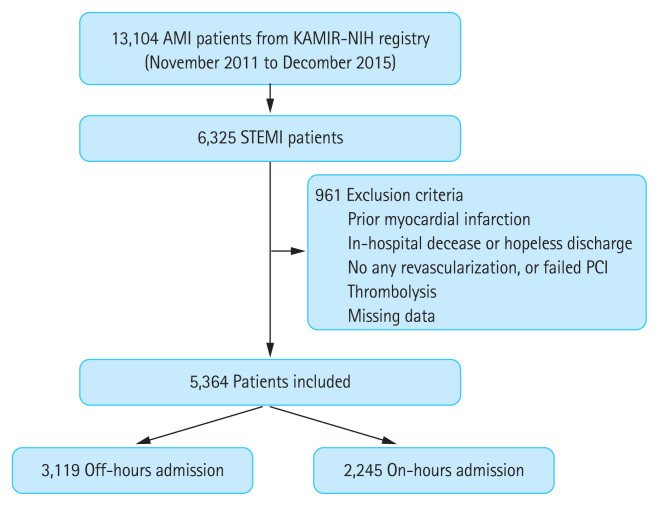
In this large-scale registry, 13,104 AMI patients were initially screened. Among them, 6,325 patients presenting with a final diagnosis of STEMI were selected and their data were extracted. We excluded the following patients: (1) those who had previous myocardial infarction; (2) those who died during the index hospitalization or were hopelessly discharged; (3) those who received no revascularization strategy or a failed PCI; (4) those who were treated by thrombolysis; and (5) those with missing data. Finally, a total of 5,364 patients constituted the study population. These patients were divided into two groups according to the timing of hospital visit for PCI of the infarct-related artery (namely, the off-hours group versus the on-hours group). They were followed up by outpatient visits at regular intervals. The study design is summarized in Fig. 1.
Figure 1.
Study population flow chart. Patients with ST-elevation myocardial infarction (STEMI) were enrolled and divided into two groups (an off-hours group and an on-hours group) in accordance with the time of hospital visit. AMI, acute myocardial infarction; KAMIR-NIH, Korea Acute Myocardial Infarction Registry-National Institute of Health; PCI, percutaneous coronary intervention.
This study was conducted in accordance with the ethical standards of the World Medical Association’s Declaration of Helsinki (revised in 2013) [12]. The study protocol of the KAMIR-NIH registry was also approved by the ethics committee of each participating center (IRB No. CNUH-2021-372). Written informed consent was obtained from all the enrolled patients.
Definition and clinical endpoints
STEMI was diagnosed and treated according to the most contemporary guidelines [1] and was defined as a new-onset ST-segment elevation in at least two continuous leads, measuring > 0.2 mV in precordial leads V1–3 or 0.1 mV in all other leads on 12-lead electrocardiography, with a concomitant rise or fall in cardiac biomarker levels (namely, troponin-I). First medical contact (FMC) was defined as the time at which the medical personnel arrived to support the AMI patient [1,13]. During FMC, there were two cases in which emergency medical service (EMS) was used and two in which it was not used. The patients with no EMS use were divided into two groups (first immediate visit to a PCI-capable center or to a PCI-incapable center). Total ischemic time (TIT) was defined as the time from the onset of angina to the first balloon inflation during the primary PCI.
All STEMI patients enrolled in our clinical study were divided into the on-hours group and the off-hours group according to the day and time of visit to the hospital. Based on the conventional working schedules of many hospitals in the Republic of Korea, regular hours (on-hours) were defined as weekdays from 8:00 AM to 6:00 PM. Off-hours were defined as weekdays from 6:01 PM to 7:59 AM, all weekends (Saturday and Sunday), and all public holidays in the Republic of Korea.
All the demographic and clinical characteristics of the patients with STEMI were recorded. Left ventricular ejection fraction (LVEF) was evaluated using two-dimensional echocardiography. Creatinine clearance (CrCl) was calculated using the Cockcroft-Gault formula [14]. Body mass index was measured using the patient’s weight and height. Angiographic and procedural characteristics were also recorded.
Image-guided PCI was defined as the use of optical coherence tomography or intravascular ultrasound during the primary PCI. Infarct-related artery referred to an epicardial coronary vessel that was blocked or stenosed by an atheromatous or thrombotic pathologic process and was directly responsible for acute coronary syndrome. The degree of coronary flow was quantitatively classified according to Thrombolysis in Myocardial Infarction (TIMI) flow grade [15].
Clinical follow-up was performed for 36 months after the commencement of the study. The primary outcome was the occurrence of major adverse cardiac and cerebrovascular events (MACCEs). MACCEs refer to a collection of all-cause mortality (cardiac and non-cardiac death), non-fatal myocardial infarction (NFMI), any revascularization (any re-do PCI or coronary artery bypass graft), cerebrovascular accident (CVA), and stent thrombosis (ST). The secondary outcomes were the occurrence of net adverse clinical events (NACEs), all-cause mortality, cardiac and non-cardiac death, NFMI, any revascularization, CVA, and ST. NACEs refer to a composite of cardiac death, NFMI, and any revascularization.
Statistical analysis
Statistical analysis was performed to evaluate the differences in clinical outcomes between the two groups according to the time and date of hospital visit. Continuous variables are expressed as mean ± standard deviation and were analyzed using Student’s t test. Discrete (categorical) variables are described as percentages with numbers and were analyzed using Pearson’s chi-square test or Fisher’s two-by-two exact test. All results were statistically significant at a p value < 0.05.
To reduce the effect of selection bias in this analysis of observational data, a propensity score weighting method known as the inverse probability of treatment weighting (IPTW) was used. The propensity score was constructed by a multiple logistic regression model using a total of 35 covariates (sex, age ≥ 65 years, FMC [EMS, PCI-capable center, and PCI-incapable center], TIT ≥ 12 hours, onset-to-door time [O2DT] ≥ 4 hours, door-to-balloon time [D2BT] ≥ 90 minutes, pulse pressure ≥ 40 mmHg), previous history (hypertension, diabetes mellitus, dyslipidemia, prior angina, prior heart failure, prior CVA), smoking (current smoker or ex-smoker, and non-smoker), family history of CAD, CrCl < 60 mL/min/1.73 m2, LVEF < 40%, discharge medications (aspirin, P2Y12 inhibitor, calcium channel blocker, beta-blocker, angiotensin converting enzyme inhibitor or angiotensin receptor blocker, and statin), and angiographic characteristics (use of transfemoral approach, glycoprotein IIb/IIIa inhibitor, thrombus aspiration, image-guided PCI [use of intravascular ultrasound or optical coherence tomography], anatomical site of the infarct-related artery [culprit vessel], and preprocedural TIMI flow grade). Patients who had any missing data in these covariates or those with a follow-up period after hospital discharge of 0 days were excluded from the analysis with IPTW adjustment.
The analysis of cumulative events was performed using time-to-event data with the Kaplan-Meier method. Survival curves were compared using the log-rank test. Patients were censored at the time of the event or at the final follow-up. Kaplan-Meier curves were plotted for the time of occurrence of clinical outcomes. All analyses were performed using SPSS version 25.0 (IBM Co., Armonk, NY, USA).
RESULTS
Baseline clinical and procedural characteristics
In our study, 5,364 consecutive patients with confirmed STEMI diagnosis were included in the analysis. Among them, 2,245 patients (41.9%) were admitted during on-hours, and 3,119 (58.1%) during off-hours (Fig. 1). In terms of baseline clinical characteristics (Table 1), the off-hours group had a higher proportion of male patients (79.5% [2,480] vs. 77.3% [1,735], p = 0.050), a lower proportion of older patients (40.6% [1,266] vs. 47.3% [1,063], p < 0.001) and a higher proportion of EMS use (21.8% [681] vs. 15.3% [343], p < 0.001) than the on-hours group. The off-hours group presented earlier with a lower proportion of TIT ≥ 12 hours (13.4% [418] vs. 22.5% [505], p < 0.001) and O2DT ≥ 4 hours (28.7% [895] vs. 39.6% [888], p < 0.001) than the on-hours group. The proportion of pulse pressure ≥ 40 mmHg was higher in the on-hours group (81.1% [2,498] vs. 83.3% [1,842], p = 0.037), and it showed worse kidney function with higher proportion of CrCl < 60 mL/min/1.73 m2 than the off-hours group (25.6% [777] vs. 30.3% [666], p < 0.001). In terms of procedural characteristics (Table 2), no significant differences were observed between the two groups. After IPTW adjustment, some differences in baseline clinical and procedural characteristics were well balanced between two groups (Tables 1 and 2).
Table 1.
Baseline characteristics of the patients
| Characteristic | Before propensity score weighting | After propensity score weighting | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Off-hours group (n = 3,119) | On-hours group (n = 2,245) | p value | Off-hours group (n = 4,758) | On-hours group (n = 4,773) | p value | |
| Male patients | 2,480 (79.5) | 1,735 (77.3) | 0.050 | 3,726 (78.3) | 3,733 (78.2) | 0.943 |
|
| ||||||
| Age, yr | 61.41 ± 12.64 | 63.19 ± 12.66 | < 0.001 | 61.94 ± 12.70 | 62.12 ± 12.59 | 0.626 |
|
| ||||||
| Age ≥ 65 years | 1,266 (40.6) | 1,063 (47.3) | < 0.001 | 2,039 (42.9) | 2,048 (42.9) | 0.974 |
|
| ||||||
| First medical contact | < 0.001 | 0.975 | ||||
|
| ||||||
| Emergency medical service | 681 (21.8) | 343 (15.3) | 889 (18.7) | 885 (18.6) | ||
|
| ||||||
| No emergency medical service | 2,438 (78.2) | 1,902 (84.7) | 3,869 (81.3) | 3,888 (81.4) | ||
|
| ||||||
| PCI-capable center | 900 (28.9) | 598 (29.6) | 1,310 (27.5) | 1,329 (27.8) | ||
|
| ||||||
| PCI-incapable center | 1,538 (49.3) | 1,304 (58.1) | 2,559 (53.8) | 2,559 (53.6) | ||
|
| ||||||
| Total ischemic time ≥ 12 hr | 418 (13.4) | 505 (22.5) | < 0.001 | 799 (16.8) | 802 (16.8) | 0.983 |
|
| ||||||
| Total ischemic time, hr | 9.56 ± 32.70 | 16.50 ± 53.98 | < 0.001 | 10.59 ± 31.68 | 13.06 ± 48.29 | 0.036 |
|
| ||||||
| Onset-to-door time, min | 444.79 ± 1,723.64 | 835.97 ± 2,554.58 | < 0.001 | 506.80 ± 1,648.81 | 638.12 ± 2,166.64 | 0.017 |
|
| ||||||
| Onset-to-door time ≥ 4 hr | 895 (28.7) | 888 (39.6 ) | < 0.001 | 1,566 (32.9) | 1,569 (32.9) | 0.978 |
|
| ||||||
| Door-to-balloon time, min | 158.23 ± 752.62 | 182.89 ± 1709.53 | 0.522 | 157.66 ± 764.92 | 174.12 ± 1,655.81 | 0.658 |
|
| ||||||
| Door-to-balloon time ≥ 90 min | 375 (12.0) | 238 (10.6) | 0.106 | 525 (11.0) | 530 (11.1) | 0.941 |
|
| ||||||
| Pulse pressure, mmHg | 49.70 ± 16.10 | 49.88 ± 16.39 | 0.688 | 49.67 ± 15.78 | 49.58 ± 16.41 | 0.848 |
|
| ||||||
| Pulse pressure ≥ 40 mmHg | 2,498 (81.1) | 1,842 (83.3) | 0.037 | 3,920 (82.4) | 3,935 (82.4) | 0.959 |
|
| ||||||
| Killip functional classification | 0.341 | 0.732 | ||||
|
| ||||||
| Killip functional class I | 2,491 (79.9) | 1,795 (80.0) | 3,850 (80.9) | 3,843 (80.5) | ||
|
| ||||||
| Killip functional class II | 230 (7.4) | 189 (8.4) | 374 (7.9) | 391 (8.2) | ||
|
| ||||||
| Killip functional class III | 174 (5.6) | 110 (4.9) | 278 (5.8) | 254 (5.3) | ||
|
| ||||||
| Killip functional class IV | 224 (7.2) | 151 (6.7) | 256 (5.4) | 284 (6.0) | ||
|
| ||||||
| Killip functional class III–IV | 398 (12.8) | 261 (11.6) | 0.212 | 534 (11.2) | 538 (11.3) | 0.953 |
|
| ||||||
| BMI, kg/m2 | 24.18 ± 3.20 | 24.04 ± 3.28 | 0.117 | 24.09 ± 3.22 | 24.12 ± 3.30 | 0.783 |
|
| ||||||
| BMI ≥ 25 kg/m2 | 1,108 (36.5) | 745 (34.0) | 0.054 | 1,680 (35.3) | 1,681 (35.2) | 0.948 |
|
| ||||||
| Previous history | ||||||
|
| ||||||
| Hypertension | 1,411 (45.2) | 1,034 (46.1) | 0.552 | 2,165 (45.5) | 2,180 (45.7) | 0.906 |
|
| ||||||
| Diabetes mellitus | 706 (22.6) | 552 (24.6) | 0.096 | 1,106 (23.2) | 1,106 (23.2) | 0.958 |
|
| ||||||
| Dyslipidemia | 336 (10.8) | 209 (9.3) | 0.080 | 484 (10.2) | 484 (10.1) | 0.970 |
|
| ||||||
| Prior angina | 200 (6.4) | 108 (4.8) | 0.013 | 273 (5.7) | 276 (5.8) | 0.963 |
|
| ||||||
| Prior heart failure | 19 (0.6) | 17 (0.8) | 0.514 | 33 (0.7) | 32 (0.7) | 0.948 |
|
| ||||||
| Prior CVA | 151 (4.9) | 108 (4.8) | 0.954 | 228 (4.8) | 229 (4.8) | 0.990 |
|
| ||||||
| Smoking | 1,989 (65.6) | 1,380 (63.0) | 0.047 | 3,056 (64.2) | 3,066 (64.2) | 0.994 |
|
| ||||||
| Family history of CAD | 212 (7.0) | 124 (5.7) | 0.054 | 306 (6.4) | 308 (6.5) | 0.987 |
|
| ||||||
| CrCl, mL/min/1.73 m2 | 82.79 ± 38.03 | 79.38 ± 39.61 | 0.002 | 81.86 ± 38.17 | 81.19 ± 39.15 | 0.558 |
|
| ||||||
| CrCl < 60 mL/min/1.73 m2 | 777 (25.6) | 666 (30.3) | < 0.001 | 1,297 (27.3) | 1,301 (27.3) | 0.995 |
|
| ||||||
| LVEF, % | 50.88 ± 9.94 | 50.43 ± 10.22 | 0.109 | 50.87 ± 9.93 | 50.77 ± 10.11 | 0.733 |
|
| ||||||
| LVEF < 40% | 357 (11.7) | 278 (12.7) | 0.304 | 559 (11.8) | 558 (11.7) | 0.953 |
|
| ||||||
| Discharge medications | ||||||
|
| ||||||
| Aspirin | 3,117 (99.9) | 2,245 (100.0) | 0.513 | 4,758 (100.0) | 4,773 (100.0) | - |
|
| ||||||
| P2Y12 inhibitor | 3,111 (99.7) | 2,243 (99.9) | 0.209 | 4,749 (99.8) | 4,763 (99.8) | 0.965 |
|
| ||||||
| Calcium channel blocker | 112 (3.6) | 72 (3.2) | 0.446 | 158 (3.3) | 161 (3.4) | 0.941 |
|
| ||||||
| Beta-blocker | 2,748 (88.1) | 1,971 (87.8) | 0.731 | 4,191 (88.1) | 4,200 (88.0) | 0.921 |
|
| ||||||
| ACE inhibitor or ARB | 2,542 (81.5) | 1,848 (82.3) | 0.445 | 3,931 (82.6) | 3,946 (82.7) | 0.969 |
|
| ||||||
| Statin | 2,969 (95.2) | 2,151 (95.8) | 0.281 | 4,550 (95.6) | 4,563 (95.6) | 0.976 |
Values are presented as number (%) or mean ± standard deviation.
PCI, percutaneous coronary intervention; BMI, body-mass index; CVA, cerebrovascular accident; CAD, coronary artery disease; CrCl, creatinine clearance; LVEF, left ventricular ejection fraction; ACE, angiotensin-converting enzyme; ARB, angiotensin receptor blocker.
Table 2.
Procedural characteristics
| Characteristic | Before propensity score weighting | After propensity score weighting | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Off-hours group (n = 3,119) | On-hours group (n = 2,245) | p value | Off-hours group (n = 4,758) | On-hours group (n = 4,773) | p value | |
| Transfemoral approach | 2,280 (73.1) | 1,684 (75.0) | 0.116 | 3,565 (74.9) | 3,577 (75.0) | 0.978 |
|
| ||||||
| Use of GPIIb/IIIa inhibitor | 645 (20.7) | 511 (22.8) | 0.067 | 1,021 (21.5) | 1,019 (21.4) | 0.930 |
|
| ||||||
| Use of thrombus aspiration | 1157 (37.1) | 831 (37.0) | 0.952 | 1,768 (37.2) | 1,776 (37.2) | 0.971 |
|
| ||||||
| Image-guided PCI (OCT or IVUS) | 611 (19.6) | 454 (20.2) | 0.566 | 947 (19.9) | 947 (19.8) | 0.958 |
|
| ||||||
| Preprocedural TIMI flow grade 0–I | 2,326 (74.6) | 1,662 (74.0) | 0.653 | 3,544 (74.5) | 3,557 (74.5) | 0.975 |
|
| ||||||
| Infarct-related artery (culprit vessel) | 0.078 | 0.356 | ||||
|
| ||||||
| LMCA | 28 (0.9) | 29 (1.3) | 42 (0.9) | 68 (1.4) | ||
|
| ||||||
| LAD | 1,640 (52.6) | 1,120 (49.9) | 2,503 (52.6) | 2,464 (51.6) | ||
|
| ||||||
| LCX | 298 (9.6) | 203 (9.0) | 428 (9.0) | 435 (9.1) | ||
|
| ||||||
| RCA | 1,153 (37.0) | 893 (39.8) | 1,786 (37.5) | 1,806 (37.8) | ||
Values are presented as number (%).
GPIIb/IIIa, glycoprotein IIb/IIIa; PCI, percutaneous coronary intervention; OCT, optical coherence tomography; IVUS, intravascular ultrasound; TIMI, Thrombolysis in Myocardial Infarction; LMCA, left main coronary artery; LAD, left anterior descending coronary artery; LCX, left circumflex coronary artery; RCA, right coronary artery.
Long-term follow-up clinical outcomes
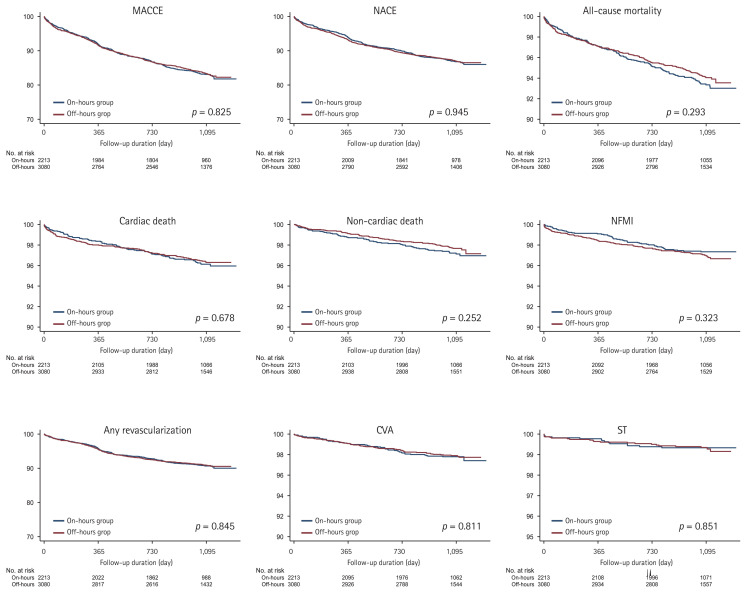
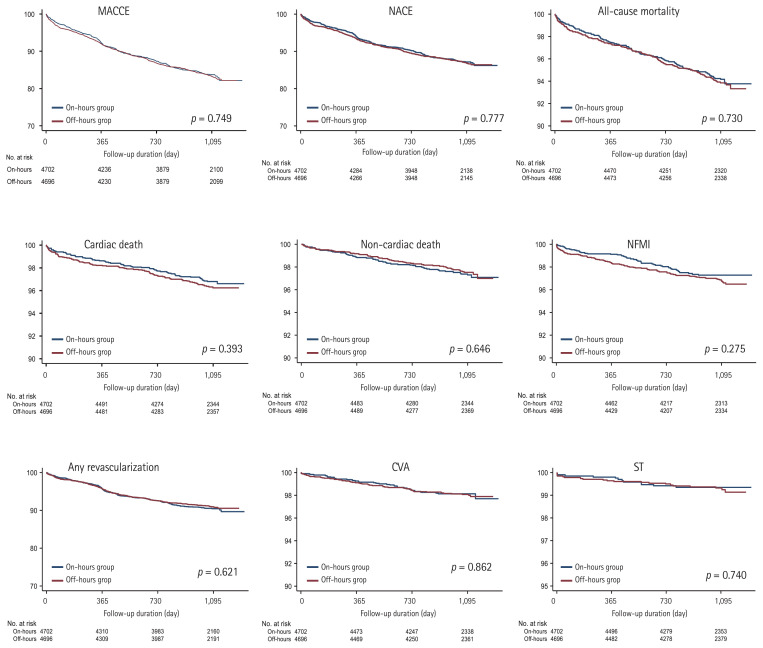
The median follow-up period in the overall study population was 1,092 days, and the median follow-up periods were 1,091 days in the off-hours group and 1,093 days in the on-hours group. We summarized the clinical outcomes during the 3-year follow-up. The clinical outcomes were determined, including MACCE, NACE, all-cause mortality, cardiac and non-cardiac death, NFMI, any revascularization, CVA, and ST (Table 3). Kaplan-Meier analysis was used to depict the unadjusted and IPTW-adjusted survival curves (Figs. 2 and 3). Before and after IPTW adjustment, there were no significant differences in any clinical outcomes between the on- and off-hours groups.
Table 3.
Three-year clinical outcomes in propensity score matched patients
| Outcome | Off-hours group (n = 3,119) | On-hours group (n = 2,245) | Unadjusted analysis | IPTW-adjusted analysis | ||
|---|---|---|---|---|---|---|
| HR (95% CI)a | p value | HR (95% CI)b | p value | |||
| MACCEc | 503 (16.1) | 365 (16.3) | 0.985 (0.861–1.127) | 0.825 | 1.024 (0.884–1.187) | 0.749 |
| NACE | 389 (12.5) | 280 (12.5) | 0.995 (0.853–1.160) | 0.945 | 1.025 (0.866–1.212) | 0.777 |
| All-cause mortality | 117 (5.7) | 142 (6.3) | 0.888 (0.712–1.108) | 0.293 | 1.044 (0.818–1.333) | 0.730 |
| Cardiac death | 108 (3.5) | 82 (3.7) | 0.941 (0.706–1.254) | 0.678 | 1.151 (0.834–1.589) | 0.393 |
| Non-cardiac death | 69 (2.2) | 60 (2.7) | 0.817 (0.578–1.155) | 0.252 | 0.916 (0.630–1.332) | 0.646 |
| NFMI | 91 (2.9) | 55 (2.4) | 1.184 (0.847–1.655) | 0.323 | 1.221 (0.853–1.748) | 0.275 |
| Any revascularization | 268 (8.6) | 195 (8.7) | 0.982 (0.816–1.181) | 0.845 | 0.951 (0.779–1.161) | 0.621 |
| CVA | 63 (2.0) | 47 (2.1) | 0.955 (0.655–1.393) | 0.811 | 1.038 (0.678–1.592) | 0.862 |
| ST | 21 (0.7) | 14 (0.6) | 1.067 (0.542–2.098) | 0.851 | 1.130 (0.549–2.327) | 0.740 |
Values are presented as number (%).
IPTW, inverse probability of treatment weighting; HR, hazard ratio; CI, confidence interval; MACCE, major adverse cardiac and cerebrovascular event; NACE, net adverse clinical event; NFMI, non-fatal myocardial infarction; CVA, cerebrovascular accident; ST, stent thrombosis.
HR corresponds to the off-hours percutaneous coronary intervention (PCI) group compared with the on-hours PCI group.
Adjusted Cox hazard regression analysis included a variety of clinical variables, including age, sex, first medical contact, total ischemic time, body-mass index, prior medical history, smoking history, family history, creatinine clearance, discharge medications, transfemoral route, image-guided PCI, culprit lesion, preprocedural Thrombolysis In Myocardial Infarction flow grade, and left ventricular ejection fraction.
MACCE is defined as a composite of all-cause mortality, non-fatal myocardial infarction, any revascularization, cerebrovascular accident, and stent thrombosis.
Figure 2.
Event rates of primary and secondary outcomes for all the patients after a 3-year follow-up (before inverse probability of treatment weighting-adjusted analysis). The figure shows the Kaplan-Meier curves for cumulative event rates according to the timing of primary percutaneous revascularization. MACCE, major adverse cardiac and cerebrovascular event; NACE, net adverse clinical event; NFMI, non-fatal myocardial infarction; CVA, cerebrovascular accidents; ST, stent thrombosis.
Figure 3.
Event rates of primary and secondary outcomes for all the patients after a 3-year follow-up (after inverse probability of treatment weighting-adjusted analysis). The figure shows the Kaplan-Meier curves for cumulative event rates according to the timing of primary percutaneous revascularization. MACCE, major adverse cardiac and cerebrovascular event; NACE, net adverse clinical event; NFMI, non-fatal myocardial infarction; CVA, cerebrovascular accidents; ST, stent thrombosis.
DISCUSSION
We conducted a comparative analysis of clinical outcomes among patients with STEMI depending on the time and date of hospital visit. We analyzed the data of 5,364 patients with STEMI, derived from the KAMIR-NIH registry. Our results showed that long-term outcomes of STEMI patients admitted to hospitals during off-hours were similar to those in patients admitted during on-hours. The off-hours group had a higher proportion of male patients and EMS utilization, but a lower proportion of those aged ≥ 65 years than the on-hours group did.
Although a longer revascularization time could be expected in the off-hours group, the patients admitted during off-hours had a significantly shorter TIT. This difference was mainly driven by O2DT, rather than D2BT, given that D2BT was similar in both groups, although the off-hours group had a lower proportion of patients with O2DT ≥ 4 hours. The similarity of proportions of D2BT ≥ 90 minutes in both groups indicated that each PCI-capable cardiovascular center had a comparable performance during off- and on-hours. On the contrary, the difference in O2DT can be explained through some mechanisms. First, women often complain of atypical chest pain or anginal equivalents such as dyspnea, fatigue, general weakness, and indigestion [16]. For this reason, female STEMI patients are found to have significant pre-hospital delay with greater TIT and O2DT according to some published articles [17–20]. This trend may contribute to higher TIT in the on-hours group with higher proportion of female patients. Second, higher proportion of elderly patients in the on-hours group accounts for the increase in TIT and O2DT. Although chest pain is the most common presentation in AMI, elderly patients present with atypical chest pain or without chest pain [21], which may interfere with early diagnosis then contribute to facilitate pre-hospital delay. Third, this finding seems to be related to the difference in the utilization rate of EMS and transfer rates via other PCI-incapable centers. From a clinical study based on the KAMIR-NIH registry, Lee et al. [20] elucidated that EMS utilization was shown to be a factor that reduces O2DT. They also highlighted that female sex and old age (age ≥ 65 years) were risk factors for delayed O2DT. In addition to that, female sex was shown to be one of predictors for EMS non-utilization. Thus, the on-hours group having higher proportion of patients aged ≥ 65 years and female patients demonstrated a lower EMS use with relatively higher rates of first immediate visit to PCI-incapable centers, thereby resulting in greater TIT and O2DT. Similar trends regarding these disparities have been observed in some comparative studies from foreign countries. In a national cohort study in England, STEMI patients admitted during off-hours were younger and had higher proportion of male patients than those admitted during on-hours [22]. In a substudy from the Japanese Registry of Acute Myocardial Infarction Diagnosed by Universal Definition (J-MINUET) registry, patients in the AMI group admitted during off-hours tended to be younger, included more male patients, used more frequent EMS and showed lower O2DT but similar D2DT compared with those in the AMI group treated during on-hours [6], which was consistent with the respective findings in our study.
A clinical study published in 2001 highlighted that patients presenting on weekends had worse clinical outcomes than those presenting on weekdays with respect to some serious medical disorders [23], drawing attention to the clinical impact of the timing of visit in case of acute medical conditions such as AMI. Since then, some studies on the clinical impact of off-hours presentation in AMI have been conducted [4–6]. Several studies have underlined that the off-hours presentation of AMI patients was associated with high rates of in-hospital [2,24] and 1-month mortality [2,22]. This finding has also been supported by several proposed assumptions, including lower possibility of timely revascularization [25,26], variations in the healthcare delivery system between off-hours and on-hours [27,28], reduced hospital staff performance during off-hours [29,30], and unbalanced proportion of severe conditions, including cardiac arrest or cardiogenic shock [2,25,31]. Especially, STEMI patients showed a longer D2BT, resulting in a low likelihood of timely performed PCI strategy (within 90 minutes after hospital admission) [2,22]. Nonetheless, because some studies on this subject have found opposite results [5,7], it has remained a contentious issue.
Traditionally, it has been believed that off-hours presentation may be associated with worse long-term results in AMI patients [29,31]. Nonetheless, recent studies found similar long-term outcomes in the off- and on-hours groups. Likewise, 1- or 2-year mortality rates have been reported to be similar in STEMI patients presenting during on-hours and off-hours [6–8]. Suwa et al. [6] reported that patients with STEMI presenting during off-hours had similar 3-year clinical outcomes compared with those presenting during regular hours. Furthermore, according to one meta-analysis, STEMI patients presenting during off-hours had similar short-, intermediate-, and long-term (at 3 to 4 years) outcomes as those who presented during regular hours [7].
Similar to the results of the aforementioned studies, our results implicate that STEMI patients admitted off-hours showed similar long-term outcomes to those admitted on-hours. These clinical outcomes are presumably explained by multi-directional innovations in public healthcare practices. After numerous studies have demonstrated the effectiveness of PCI for reducing mortality in AMI patients [32], primary PCI has become the standard strategy for AMI, including STEMI. The estimated PCI rate and the number of PCI-capable medical centers have increased in the last years in the Republic of Korea [33], with a marked increase in the proportion of centers capable of a PCI volume ≥ 500/year [34]. The PCI procedure has gradually evolved from only balloon angioplasty through bare-metal stents to the use of drug-eluting stents, reducing the rate of cardiovascular death [35]. Meanwhile, many randomized clinical trials have focused on optimization of the selection, dosage, and duration of antithrombotic agents. After dual antiplatelet therapy (DAPT) with aspirin and P2Y12 inhibitors became the mainstream option for the use of antithrombotic agents [36], ≥ 12 months of DAPT involving aspirin and clopidogrel was shown to be beneficial in the secondary prevention of ischemic events [37]. Later on, new-generation P2Y12 inhibitors such as ticagrelor and prasugrel were introduced, and novel contributions were made, including the development of risk-benefit scoring systems and the investigation of ethnic differences in terms of the safety and efficacy of these antithrombotic agents [38,39]. Additionally, the continuous implementation of veno-arterial extracorporeal membrane oxygenation has contributed to increase in the survival rate in STEMI patients [40]. These evolutionary changes may well explain the results of our study.
Besides our study focus on the long-term outcomes of STEMI patients admitted during on-hours versus off-hours, short-term outcomes containing in-hospital decease, hopeless discharge, no any revascularization or failed PCI, thrombolysis, in-hospital complications, and supportive treatment are additionally investigated, which are summarized in Supplementary Table 1 (unlike all analyzes about long-term outcomes, this investigation contains all STEMI patients [n = 6,325] including patients excluded by the exclusion criteria). The proportion of patients who underwent thrombolysis therapy was higher in the off-hours group (3.06% [114] vs. 0.58% [15], p < 0.001). The off-hours group experienced higher rates of cardiogenic shock (13.74% [512] vs. 11.96% [311], p = 0.038), ventricular tachycardia or fibrillation (8.27% [308] vs. 6.85% [178], p = 0.037), while the on-hours group had higher proportion of bleeding complications (hemoglobin decrease by 5 g/dL or hematocrit decrease by 15 %) (1.29% [48] vs. 1.96% [51], p = 0.034). In terms of supportive treatment, cardiopulmonary resuscitation was more frequent in the off-hours group (9.72% [362] vs. 7.81% [203], p = 0.009), whereas implantable cardiac defibrillator was more implanted in the on-hours group (0.02% [1] vs. 0.19% [5], p = 0.046). Nonetheless, there was no significant difference in terms of in-hospital decease or hopeless discharge, and no any revascularization or failed PCI.
We examined the long-term effect of hospital presentation (off-hours vs. on-hours presentation) among STEMI patients from the KAMIR-NIH registry. As this is a well-known nationwide Korean prospective multicenter data collection registry, we were able to represent, for the first time, the clinical characteristics and outcomes in STEMI patients in the Korean population with respect to the time of hospital visit. Our results demonstrated that the time and date of hospital visit did not affect the long-term clinical course of STEMI.
However, our study has several limitations. First, the KAMIR-NIH registry mainly included tertiary medical centers that treat high volumes of STEMI patients. Therefore, it is difficult to generalize the clinical outcomes including mortality rates and the treatment practice patterns with respect to all medical institutions with STEMI patients. Second, although this study was based only on a prospective, observational registry, it was a non-randomized study. Moreover, STEMI is an emergent situation that requires a rapid revascularization strategy, and hence it is difficult to conduct a randomized clinical study based on the time of hospital visit in STEMI. For this reason, although the propensity score weighing method was conducted to minimize the selection bias, a multicenter randomized controlled trial is needed in the future.
Despite the well-known fact that timely and rapid reperfusion is the key point of STEMI management and the belief that on-hour hospital presentation ensures more favorable clinical outcomes for acute medical diseases such as STEMI, our results showed that there were no significant differences in the long-term outcomes in STEMI patients regardless of the time of presentation.
KEY MESSAGE
1. We found no significant differences in the long-term outcomes of ST-elevation myocardial infarction (STEMI) patients undergoing percutaneous coronary intervention (PCI) regardless of the time of presentation.
2. Although the off- and on-hours groups showed different total ischemic time and onset-to-door time, door-to-balloon time was similar in both two groups, indicating that PCI-capable cardiovascular center had a comparable performance during off- and on-hours.
3. Similar long-term outcomes of STEMI patients admitted off-hours to those admitted on-hours are presumably explained by multi-directional innovations in public healthcare practice.
4. We represent, for the first time, the clinical characteristics and outcomes in STEMI patients in Korean population with respect to the time of hospital visit.
Acknowledgments
This study was supported by grants from the Korean Health Technology R&D Project, Ministry of Health & Welfare (HI13C1527) and the Research of Korea Centers for Disease Control and Prevention (2016-ER6304-01), Republic of Korea.
Footnotes
No potential conflict of interest relevant to this article was reported.
Supplementary Information
Short-term outcomes during index hospitalization, from 6,325 patients with a final diagnosis of ST-elevation myocardial infarction
REFERENCES
- 1.Ibanez B, James S, Agewall S, et al. 2017 ESC guidelines for the management of acute myocardial infarction in patients presenting with ST-segment elevation: the task force for the management of acute myocardial infarction in patients presenting with ST-segment elevation of the European Society of Cardiology (ESC) Eur Heart J. 2018;39:119–177. doi: 10.1093/eurheartj/ehx393. [DOI] [PubMed] [Google Scholar]
- 2.Sorita A, Ahmed A, Starr SR, et al. Off-hour presentation and outcomes in patients with acute myocardial infarction: systematic review and meta-analysis. BMJ. 2014;348:f7393. doi: 10.1136/bmj.f7393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Henriques JP, Haasdijk AP, Zijlstra F Zwolle Myocardial Infarction Study Group. Outcome of primary angioplasty for acute myocardial infarction during routine duty hours versus during off-hours. J Am Coll Cardiol. 2003;41:2138–2142. doi: 10.1016/s0735-1097(03)00461-3. [DOI] [PubMed] [Google Scholar]
- 4.Marume K, Nagatomo K, Yamamoto N, et al. Prognostic impact of the presence of on-duty cardiologist on patients with acute myocardial infarction admitted during off-hours. J Cardiol. 2020;76:184–190. doi: 10.1016/j.jjcc.2020.02.016. [DOI] [PubMed] [Google Scholar]
- 5.Ogita M, Suwa S, Ebina H, et al. Off-hours presentation does not affect in-hospital mortality of Japanese patients with acute myocardial infarction: J-MINUET substudy. J Cardiol. 2017;70:553–558. doi: 10.1016/j.jjcc.2017.05.006. [DOI] [PubMed] [Google Scholar]
- 6.Suwa S, Ogita M, Ebina H, et al. Admission during off-hours does not affect long-term clinical outcomes of Japanese patients with acute myocardial infarction. Int Heart J. 2020;61:215–222. doi: 10.1536/ihj.19-434. [DOI] [PubMed] [Google Scholar]
- 7.Enezate TH, Omran J, Al-Dadah AS, et al. Comparison of outcomes of ST-elevation myocardial infarction treated by percutaneous coronary intervention during off-hours versus on-hours. Am J Cardiol. 2017;120:1742–1754. doi: 10.1016/j.amjcard.2017.07.082. [DOI] [PubMed] [Google Scholar]
- 8.Lattuca B, Kerneis M, Saib A, et al. On- versus off-hours presentation and mortality of ST-segment elevation myocardial infarction patients treated with primary percutaneous coronary intervention. JACC Cardiovasc Interv. 2019;12:2260–2268. doi: 10.1016/j.jcin.2019.07.017. [DOI] [PubMed] [Google Scholar]
- 9.Reinstadler SJ, Stiermaier T, Eitel C, et al. Impact of off-hours versus on-hours primary percutaneous coronary intervention on myocardial damage and clinical outcomes in ST-segment elevation myocardial infarction. JACC Cardiovasc Interv. 2018;11:915–917. doi: 10.1016/j.jcin.2018.02.026. [DOI] [PubMed] [Google Scholar]
- 10.Tokarek T, Dziewierz A, Plens K, et al. Percutaneous coronary intervention during on- and off-hours in patients with ST-segment elevation myocardial infarction. Hellenic J Cardiol. 2021;62:212–218. doi: 10.1016/j.hjc.2021.01.011. [DOI] [PubMed] [Google Scholar]
- 11.Kim JH, Chae SC, Oh DJ, et al. Multicenter cohort study of acute myocardial infarction in Korea: interim analysis of the Korea Acute Myocardial Infarction Registry. National Institutes of Health Registry. Circ J. 2016;80:1427–1436. doi: 10.1253/circj.CJ-16-0061. [DOI] [PubMed] [Google Scholar]
- 12.World Medical Association. World Medical Association Declaration of Helsinki: ethical principles for medical research involving human subjects. JAMA. 2013;310:2191–2194. doi: 10.1001/jama.2013.281053. [DOI] [PubMed] [Google Scholar]
- 13.Neumann FJ, Sousa-Uva M, Ahlsson A, et al. 2018 ESC/EACTS guidelines on myocardial revascularization. Eur Heart J. 2019;40:87–165. doi: 10.1093/eurheartj/ehy855. [DOI] [PubMed] [Google Scholar]
- 14.Cockcroft DW, Gault MH. Prediction of creatinine clearance from serum creatinine. Nephron. 1976;16:31–41. doi: 10.1159/000180580. [DOI] [PubMed] [Google Scholar]
- 15.Stone GW, Brodie BR, Griffin JJ, et al. Prospective, multicenter study of the safety and feasibility of primary stenting in acute myocardial infarction: in-hospital and 30-day results of the PAMI stent pilot trial. Primary Angioplasty in Myocardial Infarction Stent Pilot Trial Investigators. J Am Coll Cardiol. 1998;31:23–30. doi: 10.1016/s0735-1097(97)00439-7. [DOI] [PubMed] [Google Scholar]
- 16.Wenger NK. Angina in women. Curr Cardiol Rep. 2010;12:307–314. doi: 10.1007/s11886-010-0111-z. [DOI] [PubMed] [Google Scholar]
- 17.Park JS, Kim YJ, Shin DG, et al. Gender differences in clinical features and in-hospital outcomes in ST-segment elevation acute myocardial infarction: from the Korean Acute Myocardial Infarction Registry (KAMIR) study. Clin Cardiol. 2010;33:E1–E6. doi: 10.1002/clc.20557. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Stehli J, Martin C, Brennan A, Dinh DT, Lefkovits J, Zaman S. Sex differences persist in time to presentation, revascularization, and mortality in myocardial infarction treated with percutaneous coronary intervention. J Am Heart Assoc. 2019;8:e012161. doi: 10.1161/JAHA.119.012161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Meyer MR, Bernheim AM, Kurz DJ, et al. Gender differences in patient and system delay for primary percutaneous coronary intervention: current trends in a Swiss ST-segment elevation myocardial infarction population. Eur Heart J Acute Cardiovasc Care. 2019;8:283–290. doi: 10.1177/2048872618810410. [DOI] [PubMed] [Google Scholar]
- 20.Lee SH, Kim HK, Jeong MH, et al. Pre-hospital delay and emergency medical services in acute myocardial infarction. Korean J Intern Med. 2020;35:119–132. doi: 10.3904/kjim.2019.123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Brieger D, Eagle KA, Goodman SG, et al. Acute coronary syndromes without chest pain, an underdiagnosed and undertreated high-risk group: insights from the Global Registry of Acute Coronary Events. Chest. 2004;126:461–469. doi: 10.1378/chest.126.2.461. [DOI] [PubMed] [Google Scholar]
- 22.Jayawardana S, Salas-Vega S, Cornehl F, Krumholz HM, Mossialos E. The relationship between off-hours admissions for primary percutaneous coronary intervention, door-to-balloon time and mortality for patients with ST-elevation myocardial infarction in England: a registry-based prospective national cohort study. BMJ Qual Saf. 2020;29:541–549. doi: 10.1136/bmjqs-2019-010067. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bell CM, Redelmeier DA. Mortality among patients admitted to hospitals on weekends as compared with weekdays. N Engl J Med. 2001;345:663–668. doi: 10.1056/NEJMsa003376. [DOI] [PubMed] [Google Scholar]
- 24.Wang B, Zhang Y, Wang X, Hu T, Li J, Geng J. Off-hours presentation is associated with short-term mortality but not with long-term mortality in patients with ST-segment elevation myocardial infarction: a meta-analysis. PLoS One. 2017;12:e0189572. doi: 10.1371/journal.pone.0189572. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Glaser R, Naidu SS, Selzer F, et al. Factors associated with poorer prognosis for patients undergoing primary percutaneous coronary intervention during off-hours: biology or systems failure? JACC Cardiovasc Interv. 2008;1:681–688. doi: 10.1016/j.jcin.2008.08.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Ryan JW, Peterson ED, Chen AY, et al. Optimal timing of intervention in non-ST-segment elevation acute coronary syndromes: insights from the CRUSADE (Can Rapid risk stratification of Unstable angina patients Suppress ADverse outcomes with Early implementation of the ACC/AHA guidelines) Registry. Circulation. 2005;112:3049–3057. doi: 10.1161/CIRCULATIONAHA.105.582346. [DOI] [PubMed] [Google Scholar]
- 27.Shah AP, French WJ. Physicians ..wake up! JACC Cardiovasc Interv. 2008;1:689–691. doi: 10.1016/j.jcin.2008.08.019. [DOI] [PubMed] [Google Scholar]
- 28.Redelmeier DA, Bell CM. Weekend worriers. N Engl J Med. 2007;356:1164–1165. doi: 10.1056/NEJMe068310. [DOI] [PubMed] [Google Scholar]
- 29.Kostis WJ, Demissie K, Marcella SW, et al. Weekend versus weekday admission and mortality from myocardial infarction. N Engl J Med. 2007;356:1099–1109. doi: 10.1056/NEJMoa063355. [DOI] [PubMed] [Google Scholar]
- 30.Gyenes GT, Yan AT, Tan M, et al. Use and timing of coronary angiography and associated in-hospital outcomes in Canadian non-ST-segment elevation myocardial infarction patients: insights from the Canadian Global Registry of Acute Coronary Events. Can J Cardiol. 2013;29:1429–1435. doi: 10.1016/j.cjca.2013.04.035. [DOI] [PubMed] [Google Scholar]
- 31.Berger A, Meier JM, Wasserfallen JB, et al. Out of hours percutaneous coronary interventions in acute coronary syndromes: long-term outcome. Heart. 2006;92:1157–1158. doi: 10.1136/hrt.2005.081281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Zijlstra F, Patel A, Jones M, et al. Clinical characteristics and outcome of patients with early (<2 h), intermediate (2–4 h) and late (>4 h) presentation treated by primary coronary angioplasty or thrombolytic therapy for acute myocardial infarction. Eur Heart J. 2002;23:550–557. doi: 10.1053/euhj.2001.2901. [DOI] [PubMed] [Google Scholar]
- 33.Sung J, Hong KP. Descriptive study on the Korean status of percutaneous coronary intervention using National Health Insurance Service-National Sample Cohort (NHIS-NSC) database: focused on temporal trend. Korean Circ J. 2019;49:1155–1163. doi: 10.4070/kcj.2019.0080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Shin DH, Kang HJ, Jang JS, et al. The current status of percutaneous coronary intervention in Korea: based on year 2014 & 2016 cohort of Korean Percutaneous Coronary Intervention (K-PCI) Registry. Korean Circ J. 2019;49:1136–1151. doi: 10.4070/kcj.2018.0413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Benjamin EJ, Muntner P, Alonso A, et al. Heart disease and stroke statistics: 2019 update. A report from the American Heart Association. Circulation. 2019;139:e56–e528. doi: 10.1161/CIR.0000000000000659. [DOI] [PubMed] [Google Scholar]
- 36.Schomig A, Neumann FJ, Kastrati A, et al. A randomized comparison of antiplatelet and anticoagulant therapy after the placement of coronary-artery stents. N Engl J Med. 1996;334:1084–1089. doi: 10.1056/NEJM199604253341702. [DOI] [PubMed] [Google Scholar]
- 37.Bhatt DL, Fox KA, Hacke W, et al. Clopidogrel and aspirin versus aspirin alone for the prevention of atherothrombotic events. N Engl J Med. 2006;354:1706–1717. doi: 10.1056/NEJMoa060989. [DOI] [PubMed] [Google Scholar]
- 38.Kang J, Kim HS. The evolving concept of dual antiplatelet therapy after percutaneous coronary intervention: focus on unique feature of East Asian and “Asian Paradox”. Korean Circ J. 2018;48:537–551. doi: 10.4070/kcj.2018.0166. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Costa F, van Klaveren D, James S, et al. Derivation and validation of the predicting bleeding complications in patients undergoing stent implantation and subsequent dual antiplatelet therapy (PRECISE-DAPT) score: a pooled analysis of individual-patient datasets from clinical trials. Lancet. 2017;389:1025–1034. doi: 10.1016/S0140-6736(17)30397-5. [DOI] [PubMed] [Google Scholar]
- 40.van den Brink FS, Magan AD, Noordzij PG, et al. Veno-arterial extracorporeal membrane oxygenation in addition to primary PCI in patients presenting with ST-elevation myocardial infarction. Neth Heart J. 2018;26:76–84. doi: 10.1007/s12471-017-1068-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Short-term outcomes during index hospitalization, from 6,325 patients with a final diagnosis of ST-elevation myocardial infarction