Abstract
Introduction:
Men who have sex with men (MSM) account for two-thirds of new HIV diagnoses. Pre-exposure prophylaxis (PrEP), a highly efficacious HIV preventive medication, is underutilized. Identifying correlates of PrEP awareness and attitudes may help increase PrEP use. Thus, we evaluated (1) PrEP awareness; (2) differences in awareness related to substance use and sociodemographics; (3) initial PrEP information sources; and (4) possible associations between information sources and PrEP-related attitudes.
Methods:
Young adult (ages 18–30) HIV-negative MSM from Southern U.S. undertook a web survey including questions about substance use, sexual behaviors, perceived HIV risk, and PrEP. Participants were recruited using in-person and online approaches between January 2018 - January 2020.
Results:
Of 506 participants, 89% were aware of PrEP. Participants with high alcohol consumption and greater perceived HIV risk had higher odds of PrEP unawareness with a trend for minority race/ethnicity. PrEP-aware participants reported high overall perceived safety, confidence in PrEP’s efficacy, and low perceived difficulties with adherence though those with higher perceived HIV risk and individuals who used tobacco had less favorable attitudes. Most participants first heard about PrEP from the internet. There were no statistically significant differences in PrEP-related attitudes across initial information sources.
Discussion:
Associations between substance use and racial/ethnic minority status and lack of PrEP awareness suggest priority subgroups for educational campaigns. Future campaigns may tailor outreach materials to the respective audience (e.g., Spanish materials for Hispanic people) and disseminate where individuals who use substances may be more likely to see them (e.g., liquor and convenience stores).
Keywords: HIV, internet, MSM, PrEP beliefs, Southeastern U.S.
Introduction
National HIV infection rates have decreased in recent years (Centers for Disease Control and Prevention [CDC], 2020), but remain a serious public health concern. Men who have sex with men (MSM) account for two-thirds of new HIV cases, with highest incidence among Black and Latino MSM (CDC, 2020). Young adults are also disproportionately affected. By the end of 2018, people aged 25–29 years had the highest rate (32.6%) of HIV infections, immediately followed by those aged 20–24 years (27.9%; CDC, 2020). HIV rates vary geographically, with the Southern U.S. accounting for 52% of new cases while only accounting for 37% of the population (CDC, 2020). Thus, HIV prevention strategies for young MSM in the Southern U.S. are needed.
PrEP is a class of oral medications that is currently available in pill form and is highly efficacious in preventing HIV (CDC, 2020). When taken daily, PrEP prevents the spread of HIV among at-risk groups such as MSM, with up to 99% efficacy (Desai et al., 2017; McCormack et al., 2016). However, despite concerted efforts to increase uptake, PrEP remains underutilized among MSM (Finlayson et al., 2019), with only 10% (Chan et al., 2020) to 25% (CDC, 2020) of eligible individuals taking the medication.
According to the PrEP care continuum (Nunn et al., 2017; Sullivan et al., 2020), increasing awareness is essential. In a study among MSM recently diagnosed with HIV, Marcus and colleagues (2019) reported the most common barrier to PrEP use was lack of awareness. Similarly, in a qualitative study, Rice and colleagues (2019) reported that lack of awareness was a considerable barrier to PrEP use among current and potential PrEP candidates in a Southern U.S. state (Alabama). Some evidence suggests nearly one-third of MSM are unaware of PrEP (Behler et al., 2018; Strauss et al., 2017). Encouragingly, Finlayson and colleagues’ (2019) more recent large study (N = 7,873 MSM) reported PrEP awareness increased from 60% to 90% between 2014 and 2017 among young MSM in 20 urban areas.
Among those who are aware, barriers to PrEP uptake include unfavorable attitudes (Bauermeister et al., 2013; King et al., 2014), despite evidence that PrEP is safe and efficacious (CDC, 2020). Empirically supported theories (e.g., Theory of Planned Behavior) support the importance of attitudes in health-related decision making (Ajzen, 1991; Conner et al., 2017; McEachan et al. 2016). Indeed, concerns about side-effects (i.e., PrEP safety) (Bauermeister et al., 2013, Smith et al., 2012); confidence in effectiveness (i.e., PrEP confidence); and perceived difficulty of adhering to a regimen (i.e., PrEP difficulty) are all associated with low uptake (Koechlin et al., 2017; Sidebottom et al., 2018; Smith et al., 2012). Thus, in addition to increasing awareness, education and prevention efforts must also address misconceptions about PrEP.
Efforts to increase PrEP awareness include mass media and health education campaigns, and public service announcements (French et al., 2014; Sophus & Mitchell, 2019). These efforts have had varying efficacy and are influenced by characteristics of the message and messenger, including information source, perceived credibility, and modality of delivery (Ahn et al., 2019). Thus, as awareness increases, the ways at-risk individuals learn about PrEP and whether information sources are associated with differences in related attitudes become important issues. Evidence indicates that initial sources of information may inordinately influence resulting attitudes, a phenomenon known as the primacy effect (Buda & Zhang, 2000; Holbert et al., 2007; Murphy et al., 2006). According to the primacy effect, people pay disproportionate attention to initial information and may view later messages more critically (Holbert et al., 2007). Therefore, knowledge of relationships between initial PrEP information sources and associated attitudes may inform future education and prevention efforts.
Similar to HIV rates, PrEP-related awareness and attitudes vary across sociodemographic factors (Golub et al., 2017; Strauss et al., 2017), including age, income and race/ethnicity. White, non-Hispanic MSM are more aware than individuals from other races/ethnicities (Sullivan et al., 2020). Older MSM have been found to be more aware than younger MSM (Bauermeister et al., 2013; Sullivan et al., 2020). More education and household income of $20,000 or more have also been related to PrEP awareness (Bauermeister et al., 2013; Fallon et al., 2017; Roth et al., 2019). Concerns about PrEP side effects may be especially pronounced among Black MSM (Thomann et al., 2018). Similarly, individuals of color endorsed barriers to PrEP as being significantly more important than White individuals (Golub et al., 2013).
Across the PrEP care continuum, awareness is generally lower among those who use substances (McFarland et al., 2020; Roth et al., 2019; Sherman et al., 2019; Walters et al., 2020). However, the relationship between PrEP awareness and specific substance use is less clear. Some studies report marijuana use (Torres et al., 2019) and increased alcohol use (Garnett et al., 2018) are associated with low PrEP awareness, whereas other research reports null results (Sullivan & Eaton, 2020). Physicians report low willingness to discuss or prescribe PrEP to people who use substances (Edelman et al., 2017; Karris et al., 2014), which may be associated with low awareness in this population. Notably, substance use is common among young adults and MSM. Young adults (ages 18–30) have the highest rates of alcohol use compared to other age groups (Center for Behavioral Health Statistics and Quality, 2020). Alcohol is also one of the most commonly used substances among MSM (Allen et al., 2015; Pollock et al., 2012). MSM have higher rates of illicit substance use than the general population as well (Mackesy-Amiti et al., 2008; Reback et al., 2013; Solomon et al., 2012). These findings add to the importance of relating substance use/misuse to PrEP awareness and attitudes.
Sexual behaviors and perceived risk have also been associated with PrEP use and awareness, with mixed findings. Across studies of young adult MSM, rates of higher-risk behaviors – including recent engagement in group sex (Kuhns et al., 2017) – were positively and significantly associated with PrEP use. Strauss and colleagues (2017) found that PrEP aware participants reported less condomless anal sex than PrEP unaware participants. In addition, lower perceived HIV risk has been associated with lack of interest in taking PrEP (Liu et al., 2018). Similarly, in their study assessing the effect of providing objective and subjective risk scores on PrEP uptake, Blumenthal and colleagues (2019) reported that low risk perception was the most common reason for not starting PrEP. Others have similarly found that higher perceived risk of HIV infection is associated with increased PrEP uptake (Golub et al., 2019). These results suggest that sexual behaviors and HIV risk perceptions are important considerations, but equivocal prior findings call for further research.
While awareness has improved, key subgroups (e.g., those who use/misuse substances) may continue to lag behind. Relatedly, unfavorable attitudes toward PrEP may also be hindering uptake among these same groups. In addition to substance use and sociodemographic factors, initial source of information may be a correlate of PrEP-related attitudes. As such, we examined these factors using data from a recent, web-based survey among MSM in the Southern U.S.
Methods
Participants
Participants were young adult (ages 18–30), HIV-negative MSM in the Southeastern U.S. Data were collected between January 2018 – January 2020, to inform a parent intervention study to address alcohol misuse and HIV prevention including PrEP. Individuals reporting male assignment at birth; ages 18–30; no lifetime PrEP use; at least 1 instance of sexual activity of any kind (oral and/or anal) with another man in the previous 3 months; and self-reported HIV-negative status were eligible. Recruitment was localized to the Southern U.S. The majority of participants came from Florida, but participants also came from Alabama, Arkansas, Georgia, Kentucky, Louisiana, Mississippi, North Carolina, South Carolina, Tennessee, Texas, and Virginia. Participants were compensated with a $25 electronic gift card. The study was approved by the University of Florida’s institutional review board (IRB201701367; Advancing New Computer-based Health Outreach Regarding Sexual behavior [ANCHORS] Study: UH2 Project).
Measures
Demographics.
Participants reported their age (i.e., “In what year were you born?”), race (i.e., “What race do you consider yourself?” [options: American Indian/Alaska Native, Asian, Native Hawaiian or Other Pacific Islander, Black or African American, White, more than one race, or Other]), and ethnicity (i.e., “What ethnicity do you consider yourself?” [options: Hispanic/Latino or Not Hispanic/Latino]). Participants were also asked about their education level (i.e., “What is the highest grade or year of school you have completed?” [options: elementary school or below; some high school; high school graduate or GED; some college or technical/trade school/college or trade school graduate; or graduate or professional degree]) and relationship status (i.e., “What is your current relationship status?” [options: married, divorced, widower, separated, never married/single, and not married, but in a long-term relationship]). Personal (i.e., “During the last 12 months, what was your total personal income?” and household income (i.e., “During the last 12 months, what was the total income from all people living in your household”) and were assessed separately and asked participants to report income from all sources. Participants were asked to “report income from all jobs before taxes. Include any tips, bonuses, overtime pay and commissions, as well as any income from pensions, dividends, interest, Social Security, alimony, child support, workman’s compensation or any public assistance or welfare payments and any other money income received by you from any other source. Response options for each question included $9,999 or less; $10,000 to $19,999; $20,000 - $39,999; $40,000 - $59,999; $60,000 - $79,999; $80,000 - $99,999. Options for personal income also included $100,000 or more; whereas options for household income included $100,000 - $149,999; $150,000 - $199,999; $200,000 or more.
Substance Use.
Past-month alcohol use was assessed using the National Institute on Alcohol Use and Alcoholism (2003) recommended alcohol use questions, modified to allow a greater range of response options. Participants reported frequency of any alcohol use (response options: 0–30 days), heavy drinking (i.e., five or more drinks in a day; options: 0–30 days), drinks per drinking day (options: 0–25 or more drinks), and maximum number of drinks within a 24-hour period (options: 0–36 or more drinks). Responses to the frequency and drinks per drinking day items were used to create a drinks per week variable.
Participants were asked, on average, how many cigarettes they smoked per day in the past 12 months (7 response options ranged from I have not smoked in the past 12 months to 40 cigarettes a day). Using single-item measures, participants were also asked to select the option that best described their use of marijuana and their use of other drugs besides marijuana. Response options ranged from no use to daily use.
Alcohol Misuse.
The 10-item Alcohol Use Disorders Identification Test (AUDIT; Saunders, 1993) assessed frequency and magnitude of alcohol use, and symptoms of DSM-IV alcohol dependence (alpha for current study =.90). Responses were on Likert-type scales, with scoring from 0 to 4. Scores from 8–15 suggest hazardous use. Scores of 16 or more suggest possible alcohol dependence (Babor et al., 2001).
Sexual behaviors.
The 9-item sexual risk subscale of the Risk Assessment Battery (RAB; Metzger et al., 1993) captures frequency of engagement in these behaviors (e.g., exchange of sex for drugs or money and frequency of condom use) over the past 6 months. There are four response options (e.g., 0 = “Never” to 3 = “Once or more each week”). Participants were also asked how many men and women they had had sex with in the past 6 months, where sex was defined to include oral, anal, and vaginal sex. Participants were given the following options: 0 men (women); 1 man (woman); 2 or 3 men (women); and 4 or more men (women). Scores were summed with higher numbers indicating greater sexual risk. The original authors reported strong discriminant and predictive validity and test-retest reliability but weaker internal consistency reliability, confirmed in the present study (alpha for current study=.41). Participants also reported their frequency of consuming alcohol before or during oral, anal or vaginal sex during the past month (options: 0 to 50 or more times).
Perceived HIV risk.
The reliable and valid, 8-item Perceived Risk of HIV Scale (PRHS; Napper et al., 2012) captured individuals’ perceived likelihood of HIV infection, with higher scores indicating higher perceived risk (alpha for current study=.85).
PrEP awareness.
Participants reported whether they had heard of PrEP before the present study.
PrEP information source.
Participants who reported having heard of PrEP before the survey reported where they first heard about PrEP from a list of sources: news, internet, HIV support group, public health organization, doctor, spouse/partner, friends/family, and other. Participants who indicated “other” were asked to specify their information source (Algarin et al., 2020).
PrEP-related attitudes.
On 5-point Likert-type scales, participants who had heard of PrEP rated perceived safety (i.e., “In your opinion, how safe do you think PrEP is?” anchored by “Not safe” and “Safe”), confidence in its efficacy (i.e., “How confident are you that taking PrEP every day would reduce the transmission of HIV?” anchored by “Not confident” and “Confident”), and anticipated difficulty with adherence (i.e., “How difficult do you think it would be to take PrEP every day?” – anchored by “Not difficult” and “Difficult”).
Procedures
Participants were recruited online (e.g., Craigslist, Grindr, Facebook, mTurk). In person recruitment also took place at community events and clinics in and around Gainesville, FL, where the parent study is based. Prospective participants were directed to a brief, online pre-screening survey before the main web survey to ensure eligibility. Data presented here are from the main web-based survey, which was hosted on REDCap (Harris et al., 2009, 2019).
Statistical analyses
Fraudulent responses (e.g., non-existent mailing addresses, repeat attempts at completing survey from the same IP address) were removed prior to analyses following published fraud detection procedures (Ballard et al., 2019).
For analytic purposes and parsimony, PrEP information source was grouped into 4 categories: internet, friends/family, news, and public health organizations/doctors. HIV support groups were grouped together with public health organizations and doctors, whereas spouse/partners were grouped together with friends/family. Participants’ answers to the “other” option (n = 16) were added to the most appropriate category.
SPSS software version 27 was used to conduct the analyses. Descriptive statistics were conducted to characterize the sample. Race and ethnicity were crossed to create a reduced race/ethnicity variable for analytic purposes: White, non-Hispanic; Black, non-Hispanic; Hispanic/Latin; and Other. Past 12-month cigarette, marijuana, and non-marijuana drug use variables were dichotomized (i.e., any vs none). Those not reporting past-month drinking had zero entered for drinks per drinking day. Continuous variables were transformed to reduce skewness and kurtosis as needed. Drinking days per week, maximum number of drinks in 24 hours, AUDIT score, and PRHS score were square-root transformed. Drinks per drinking day, drinks per week, number of times alcohol was used before or during sex, and RAB scores were log transformed. Number of sex partners and condomless sex were winsorized and log transformed. Heavy drinking days and number of times alcohol was used before or during sex were winsorized and inverse transformed. When results are reported for inverse transformed variables, signs were reversed to be in line with raw versions of the variables.
To account for multiple comparisons and the exploratory nature of these analyses, p ≤ .01 was used as a threshold for statistical significance. Chi-square, t-tests, one-way ANOVAs and correlation coefficients were used to evaluate bivariate relationships with PrEP awareness and related attitudes. Variables with statistically significant or trend-level bivariate relationships (p < .05) were entered into regression models to determine the strongest correlates of PrEP awareness and related attitudes. For parsimony in the regression models, race was also converted into a binary variable (i.e., White vs non-White).
Results
Sample descriptives
Among survey participants (N=673), 506 provided responses about PrEP and made up the sample for this study. Table 1 provides full demographic characteristics. Mean age was 24.83 (SD=3.27) years. The sample was 55% White, non-Hispanic and 13% Black, non-Hispanic, with approximately 24% of the sample indicating Hispanic/Latin ethnicity. Most were educated, with approximately 85% reporting some college education or above and about half reporting having graduated from college or trade school. There were no statistically significant differences between those who did and did not (n=167) answer (i.e., skipped) PrEP-related questions. Among participants for whom geographic data were available (n = 543), a large majority were from Florida (75%, n = 404). Georgia (7%, n = 36), North Carolina (4%, n = 23), followed by South Carolina (2%, n = 12) and Alabama (2%, n = 12) rounded out the five most represented states. Others included Texas (2%, n = 11), Tennessee (2%, n = 10), Virginia (1%, n = 6) and Kentucky (1%, n = 5).
Table 1.
Sociodemographic and Substance Use Differences between PrEP Aware and Unaware Participants (N=506).
| Full sample (N = 506) | Aware of PrEP (n = 451) | Not aware of PrEP (n = 55) | X 2 | ||||
|---|---|---|---|---|---|---|---|
| n | % | n | % | n | % | ||
| Race/ethnicity | 34.5** | ||||||
| White, Non-Hispanic | 273 | 54.9 | 261 | 58.9 | 12 | 22.2 | |
| Black, Non-Hispanic | 64 | 12.9 | 57 | 12.9 | 7 | 13 | |
| Hispanic | 118 | 23.7 | 95 | 21.4 | 23 | 42.6 | |
| Other | 42 | 8.5 | 30 | 6.8 | 12 | 22.2 | |
| Education level | 5.4 | ||||||
| High school diploma or less | 77 | 15.2 | 68 | 15.1 | 9 | 16.4 | |
| Some college or trade school | 174 | 34.5 | 148 | 32.9 | 26 | 47.3 | |
| College graduate or above | 254 | 50.3 | 234 | 52. | 20 | 36.4 | |
| Marital status | 5.8 | ||||||
| Married/long-term relationship | 140 | 27.7 | 132 | 29.3 | 8 | 14.5 | |
| Single | 352 | 69.6 | 306 | 67.8 | 46 | 83.6 | |
| Other (e.g., divorced) | 14 | 2.8 | 13 | 2.9 | 1 | 1.8 | |
| Annual personal income | .63 | ||||||
| $19,999 or less | 182 | 38.4 | 161 | 38.1 | 21 | 41.2 | |
| $20,000 to $59,999 | 225 | 47.5 | 202 | 47.8 | 23 | 45.1 | |
| $60,000 to $79,000 | 40 | 8.4 | 35 | 8.3 | 5 | 9.8 | |
| $80,000 or more | 27 | 5.7 | 25 | 5.9 | 2 | 3.9 | |
| Annual household income | 1.9 | ||||||
| $19,999 or less | 80 | 17.2 | 69 | 16.7 | 11 | 21.2 | |
| $20,000 to $59,999 | 195 | 42 | 172 | 41.7 | 23 | 44.2 | |
| $60,000 to $99,999 | 106 | 22.8 | 94 | 22.8 | 12 | 23.1 | |
| $100,000 or more | 83 | 17.9 | 77 | 18.7 | 6 | 11.5 | |
| Cigarette use (past 12 months) | 9.4* | ||||||
| No cigarette use | 320 | 64.1 | 295 | 66.4 | 25 | 45.5 | |
| Used cigarette | 179 | 35.9 | 149 | 33.6 | 30 | 54.5 | |
| Marijuana use (past 12 months) | 5.5 | ||||||
| No marijuana use | 255 | 51.3 | 235 | 53.2 | 20 | 36.4 | |
| Used marijuana | 242 | 48.7 | 207 | 46.8 | 35 | 63.6 | |
| Other drug use (past 12 months) | 13.3** | ||||||
| No drug use | 373 | 75.7 | 343 | 78.1 | 30 | 55.6 | |
| Used drugs | 120 | 24.3 | 96 | 21.9 | 24 | 44.4 | |
p < 0.001;
p < 0.01
Regarding use of alcohol in the past month (past 30 days): the sample reported, on average, 2.11 drinking days per week (SD = 1.89) and 3.78 drinks per drinking day (3.45). Participants also reported, on average, 3.82 (SD = 6.18) heavy drinking days and 11.09 total drinks per week (SD = 19.21).
Regarding use of marijuana in any form: 33% (n=165) reported never using marijuana; 18% (n=90) reported using marijuana but not in the past 12 months; 18% (n=90) reported using marijuana less than once a month over the past 12 months; 11% (n=57) reported using 1–3 times a month over the past 12 months; 7% (n=34) reported using 1–3 times a week over the past 12 months; 6% (n=29) reported using 4–6 times a week over the past 12 months, 6% (n=32) reported using every day over the past 12 months; 2% (n=9) had missing data.
Regarding use of any drugs besides marijuana: 60% (n=305) reported never using illegal drugs in any form; 13% (n=68) reported using illegal drugs but not in the past 12 months; 13% (n=63) reported using drugs less than once a month over the past 12 months; 5% (n=25) reported using 1–3 times a month over the past 12 months; 3% (n=16) reported using 1–3 times a week over the past 12 months; 1% (n=7) reported using 4–6 times a week over the past 12 months, 2% (n=9) reported using every day over the past 12 months; 3% (n=13) had missing data.
Marijuana use was more common than cigarette use and much more common than other drug use. The majority of participants were non-users of each of the three. Given the relatively small number of participants endorsing use, and given the distribution among the trend of use, comparisons were made between any use versus no use in the past 12 months.
PrEP awareness
A total of 451 (89%) reported having heard about PrEP prior to this study. There were significant associations between PrEP awareness and race/ethnicity (Table 1). Pairwise post-hoc comparisons revealed White, non-Hispanic participants were significantly more likely to be aware than Hispanic participants, X2(1, n=391)=23.04, p< 0.001, and those with “Other” race/ethnicity, X2(1, n=315)=30.23, p < 0.001. White, non-Hispanic participants were also more likely than Black, non-Hispanic participants to be aware at a near-significant level, X2(1, n=337)=4.17, p=.04. Remaining race/ethnicity pairwise comparisons revealed no significant associations. There were no statistically significant associations between PrEP awareness and other demographics (Tables 1 and 2).
Table 2.
Differences in Age, Alcohol Use, Sexual Risk Behavior and Perceived Risk of HIV between PrEP Aware and PrEP Unaware Participants.
| Full sample (N = 506) | Aware of PrEP (n = 451) | Not aware of PrEP (n = 55) | t | df | p | Cohen’s d | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| M | SD | M | SD | M | SD | |||||
| Age | 24.83 | 3.27 | 24.87 | 3.32 | 24.51 | 2.80 | −0.89 | 74 | .37 | .11 |
| Alcohol use (past month) | ||||||||||
| Drinking days per week | 2.11 | 1.89 | 1.97 | 1.83 | 3.26 | 1.98 | 4.69 | 503 | <.001** | .67 |
| Drinks per drinking day | 3.78 | 3.45 | 3.57 | 3.14 | 5.47 | 5.08 | 4.63 | 75 | <.001** | .57 |
| Heavy drinking days | 3.82 | 6.18 | 3.21 | 5.41 | 8.84 | 9.15 | 4.57 | 71 | <.001** | .60 |
| Maximum number of drinks in 24 hours | 6.48 | 5.94 | 5.95 | 5.47 | 10.83 | 7.66 | 5.36 | 495 | <.001** | .77 |
| Drinks per week | 11.09 | 19.21 | 9.62 | 14.81 | 23.13 | 38.11 | 5.15 | 503 | <.001** | .74 |
| Number of times alcohol used before or during sex | 2.92 | 5.21 | 2.47 | 4.23 | 6.53 | 9.39 | 5.88 | 73 | <.001** | .74 |
| AUDIT score | 9.50 | 8.14 | 8.65 | 7.50 | 16.29 | 9.84 | 5.85 | 497 | <.001** | .84 |
| RAB score | 7.94 | 2.40 | 7.82 | 2.24 | 8.47 | 2.57 | 1.22 | 61 | .226 | .21 |
| PRHS score | 23.99 | 6.44 | 23.59 | 6.03 | 27.30 | 8.53 | 3.41 | 60 | .001** | .68 |
Note. AUDIT = Alcohol Use Disorders Identification Test; PRHS = Perceived Risk of HIV Scale; RAB = Risk Assessment Battery.
Those not reporting past-month drinking had zero entered for drinks per drinking day. Data were transformed for analyses to reduce skewness. Raw results are reported here for ease of interpretation. Drinking days per week, maximum number of drinks in 24 hours, AUDIT score, and PRHS score were square-root transformed. Drinks per drinking day, drinks per week, number of times alcohol used before or during sex, and RAB scores were log transformed. Number of sex partners and condomless sex were winsorized and log transformed. Heavy drinking days and number of times alcohol use before or during sex were winsorized and inverse transformed. Signs were reversed to be in line with raw versions of the variables for inverse transformed variables.
p < 0.001;
p < 0.01
Participants who reported past-12-month cigarette use and use of drugs other than marijuana were significantly less likely to be PrEP aware compared to those who reported no use. There was a similar relationship with past-12-month marijuana use (Table 1) that did not reach statistical significance (p = .02).
Similarly, PrEP unaware participants reported significantly higher alcohol use, including past-month any and heavy drinking days, drinks per drinking day, maximum number of drinks in a 24-hour period, and overall drinks per week (Table 2). Further, PrEP-unaware participants had a mean AUDIT score nearly twice the level of PrEP-aware participants. PrEP-unaware participants also reported significantly higher frequency of alcohol use before or during sex, though Risk Assessment Battery score did not differ significantly between those aware and unaware of PrEP. However, perceived risk of HIV was significantly higher among those not aware of PrEP.
Variables with trend-level (p < .05) or statistically significant bivariate correlations with PrEP awareness were included in exploratory logistic regressions to statistically predict lack of PrEP awareness (see Table 3 for correlations among PrEP awareness and all predictor variables). In examining relations between alcohol use and HIV sexual risk, previous research has used drinks per week as a global measure of alcohol use (e.g., Arasteh et al., 2008), thus drinks per week was selected as a representative indicator of overall alcohol exposure. Given high correlations among drinks per week, AUDIT scores, and frequency of alcohol use before/during sexual activity (rs .65–.82, ps<. 001), to avoid multicollinearity, three separate regression models were tested, resulting in a similar pattern of findings: the respective alcohol use variable and greater perceived risk of HIV were the only significant statistical predictors. There was a non-significant trend in the direction of non-white participants having lower odds of PrEP awareness (Table 4; Supplemental Tables 1 and 2).
Table 3.
Correlations among PrEP Unawareness, Sociodemographics, Alcohol and Other Substance Use, Sexual Risk Behavior and Perceived Risk of HIV (N=506)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PrEP | Age | Educ. | Race | Cig | MJ | Drugs | DD | DDD | HDD | Max | DW | AS | AUDIT | RAB | PRHS | |
| 1 | -- | .04 | .07 | −.08 | .14* | .11 | .16* | .21* | .17* | .18* | .23* | .22* | .23* | .25* | .07 | .21* |
| 2 | -- | .31 | −.08 | .02 | −.13* | −.02 | .1 | .01 | .01 | .02 | .07 | .09 | .02 | .11* | −.03 | |
| 3 | -- | −.18* | −.07 | .04 | −.05 | .1 | .05 | .08 | .12* | .04 | .03 | .07 | −.02 | .06 | ||
| 4 | -- | −.05 | −.08 | −.04 | −.12* | −.01 | −.05 | −.11* | −.07 | −.05 | −.08 | .06 | −.03 | |||
| 5 | -- | .39* | .36* | .26* | .18* | .32* | .25* | .27* | .20* | .34* | .23* | .19* | ||||
| 6 | -- | .42* | .28* | .24* | .31* | .30* | .28* | .23* | .35* | .16* | .19* | |||||
| 7 | -- | .22* | .20* | .26* | .24* | .24* | .18* | .30* | .35* | .25* | ||||||
| 8 | -- | .67* | .70* | .76* | .91* | .63* | .76* | .21* | .17* | |||||||
| 9 | -- | .71* | .85* | .86* | .53* | .75* | .21* | .21* | ||||||||
| 10 | -- | −.78* | −.80* | .53* | −.77* | .22* | .22* | |||||||||
| 11 | -- | .85* | .56* | .78* | .25* | .24* | ||||||||||
| 12 | -- | .65* | .82* | .24* | .21* | |||||||||||
| 13 | -- | −.62* | .28* | .19* | ||||||||||||
| 14 | -- | .29* | .32* | |||||||||||||
| 15 | -- | .37* | ||||||||||||||
| 16 | -- |
Note. AS = Number of times alcohol was used before or during sex; AUDIT = Alcohol Use Disorders Identification Test; Cig. = Cigarette use; DD = drinking days; DDD = Drinks per drinking days; Drugs = Other drugs use; Educ. = Education level; HDD = Heavy drinking days; Max = Maximum number of drinks in 24 hours; MJ = Marijuana use; PrEP = PrEP unawareness; PRHS = Perceived Risk of HIV Scale; RAB = Risk Assessment Battery. Those not reporting past-month drinking had zero entered for drinks per drinking day. Data were transformed for analyses to reduce skewness. Drinking days per week, maximum number of drinks in 24 hours, AUDIT score, and PRHS score were square-root transformed. Drinks per drinking day, drinks per week, number of times alcohol used before or during sex, and RAB scores were log transformed. Number of sex partners and condomless sex were winsorized and log transformed. Heavy drinking days and number of times alcohol use before or during sex were winsorized and inverse transformed. Signs were reversed to be in line with raw versions of the variables for inverse transformed variables.
p < 0.01
Table 4.
Logistic Regression Statistically Predicting PrEP Unawareness Using AUDIT Score as the Alcohol Variable (n=477).
| Variables | Odds Ratio | β | P |
|---|---|---|---|
| Race/ethnicitya | 2.07 | 1.16 – 4.49 | .027 |
| Cigarette useb | 1.19 | .59 – 2.40 | .63 |
| Marijuana usec | 1.06 | .52 – 2.20 | .87 |
| Other drug used | 1.40 | .68 – 2.87 | .36 |
| PRHS scoree | 1.001 | 1.000 – 1.002 | .005 |
| AUDITf | 1.59 | 1.23 – 2.06 | <.001 |
Note. PrEP unawareness was coded as 1. Awareness is coded as 0. AUDIT = Alcohol Use Disorder Identification Test; PRHS = Perceived Risk of HIV Scale; RAB = Risk Assessment Battery.
0 = White, 1 = Non-white.
0 = No cigarette use in past 12 months, 1 = Cigarette used in past 12 months.
0 = No marijuana use in past 12 months, 1 = Marijuana used in past 12 months.
0 = No other drug use in past 12 months, 1 = Drug used in past 12 months.
PRHS score was square root transformed.
AUDIT score was square root transformed.
Initial PrEP information sources and relationships to attitudes
The most common source of initial PrEP information was the internet, with a majority (n = 235, 53%) of the sample indicating they first heard of PrEP that way, followed by friends and family (n = 75, 17%), the news (n = 68, 15%) and public health organizations/doctors (n = 66, 15%). There were statistically significant correlations among the three PrEP-related attitudes, such that perceived PrEP safety was positively correlated with PrEP confidence. Perceived difficulty with PrEP adherence had small but statistically significant inverse correlations with perceived safety and confidence in efficacy (Table 5).
Table 5.
Correlations among PrEP-Related Attitudes, Age, Alcohol Use, Sexual Risk Behavior and Perceived Risk of HIV in Young Adult MSM Who Were Aware of PrEP (n=451)
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| PrEP Diff | PrEP Saf | PrEP Conf | Age | DD | DDD | HDD | Max | DW | AS | AUDIT | RAB | PRHS | |
| 1 | -- | −.18* | −.15* | .01 | .11 | .12 | .11 | .08 | .12 | .08 | .14* | .07 | .16* |
| 2 | -- | .54* | −.09 | −.04 | −.05 | −.03 | −.03 | −.06 | −.09 | −.07 | −.13* | −.14* | |
| 3 | -- | −.08 | −.02 | −.05 | −.06 | −.03 | −.07 | −.03 | −.06 | −.13* | −.14* | ||
| 4 | -- | .09 | .01 | .02 | .03 | .07 | .08 | .02 | .14* | −.03 | |||
| 5 | -- | .67* | .69* | .75* | .90* | .60* | .75* | .17* | .08 | ||||
| 6 | -- | .72* | .86* | .86* | .53* | .76* | .21* | .19* | |||||
| 7 | -- | −.77* | −.80* | .50* | −.75* | .17* | .14* | ||||||
| 8 | -- | .84* | .53* | .76* | .19* | .16* | |||||||
| 9 | -- | .63* | .82* | .22* | .14* | ||||||||
| 10 | -- | −.59* | .25* | .11 | |||||||||
| 11 | -- | .28* | .24* | ||||||||||
| 12 | -- | .35* | |||||||||||
| 13 | -- |
Note AS = Number of times alcohol was used before or during sex; AUDIT = Alcohol Use Disorders Identification Test; DD = drinking days; DDD = Drinks per drinking days; HDD = Heavy drinking days; Max = Maximum number of drinks in 24 hours; PrEP Conf = perceived confidence in PrEP efficacy; PrEP Diff = perceived difficulty with PrEP adherence; PrEP Saf = perceived PrEP safety; PRHS = Perceived Risk of HIV Scale; RAB = Risk Assessment Battery. Those not reporting past-month drinking had zero entered for drinks per drinking day. Data were transformed for analyses to reduce skewness. Drinking days per week, maximum number of drinks in 24 hours, AUDIT score, and PRHS score were square-root transformed. Perceived PrEP safety and confidence in efficacy were squared transformed. Perceived difficulty adhering to PrEP, drinks per drinking day, drinks per week, number of times alcohol used before or during sex, and RAB scores were log transformed. Number of sex partners and condomless sex were winsorized and log transformed. Heavy drinking days and number of times alcohol use before or during sex were winsorized and inverse transformed. Signs were reversed to be in line with raw versions of the variables for inverse transformed variables.
p < 0.01
Among those who had heard of PrEP, perceived safety (M=4.32 on a 1–5 scale, SD = 0.84) and confidence in efficacy were high (M=4.22, SD=0.91) and perceived difficulties with adherence were low (M=2.04, SD=1.15). There were no statistically significant differences in attitudes regarding PrEP safety, F(3, 437)=0.38, p=0.77, perceived PrEP efficacy, F(3, 437) = 0.24, p=0.87, or perceived PrEP difficulty across the four initial PrEP information source categories, F(3,436)=0.69, p=0.56.
Other correlates of PrEP-related attitudes
Given the statistically significant bivariate relationship between race/ethnicity and PrEP awareness, analyses were conducted to examine if PrEP-related attitudes varied by race/ethnicity. There were no statistically significant differences in perceived safety, F(3,429)=1.14, p=0.33, confidence in efficacy, F(3,429)=1.58, p=0.19, or perceived difficulty with adherence, F(3,428)=1.15, p=0.33) based on race. Further, there were no significant differences in PrEP-related attitudes by education level: PrEP safety, F(2,437)=.15, p=0.86, confidence in efficacy, F(2,437)=1.78, p=0.17, and perceived difficulty with adherence, F(2,436)=2.19, p=0.11.
Regarding relationships between substance use and PrEP-related attitudes (Table 5), there was a small but significant correlation between perceived difficulty adhering to PrEP and AUDIT score and a trend-level correlation between perceived difficulty and drinks per week (p=.011). Analyses relating other substance use to PrEP-related attitudes revealed that there were largely similar PrEP-related attitudes between those who reported using and not using substances. However, t-tests revealed that those who reported past 12-month cigarette use reported significantly lower confidence in PrEP’s efficacy (M=3.97, SD=1.02) than those who did not use cigarettes (M=4.33, SD=.82), t(432)=−3.76, p< .001). There was a trend in which participants who reported past 12-month other (non-marijuana) drug use had lower confidence in efficacy (M=4.03, SD=.98) than those who did not report using other drugs (M=4.26, SD=.88), t(428)=−2.13, p=.03. There were no other significant or trend-level differences in PrEP-related attitudes based on substance use.
Regarding sexual risk behavior, there were small but significant correlations between Risk Assessment Battery score and lower perceived safety and lower confidence in efficacy, but no significant correlation with perceived difficulty adhering to PrEP. There were small but significant correlations between perceived risk of HIV and greater perceived difficulty, lower perceived safety and perceived confidence in PrEP’s efficacy (Table 5).
Significant and trend-level correlates were included in linear regressions to statistically predict each PrEP-related attitude (Table 6). Perceived difficulty adhering to PrEP was correlated with both drinks per week and AUDIT score (Table 5), which were tested further in separate regressions. Perceived risk of HIV was a significant statistical predictor of perceived difficulty in both regression models while drinks per week and AUDIT score were trend-level statistical predictors. Neither sexual risk behavior nor perceived risk of HIV predicted perceived safety. Past-12-month cigarette use was the only significant statistical predictor of perceived efficacy.
Table 6.
Linear Regressions Predicting PrEP-Related Attitudes from Alcohol and Other Substance Use, Sexual Risk Behavior and Perceived Risk of HIV
| PrEP Difficulty (n=433/439) | PrEP Safety (n=439) | PrEP Confidence (n=428) | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE B | β | p | B | SE B | β | p | B | SE B | β | p | |
| Model 1 | ||||||||||||
| AUDIT | .02 | .01 | .11 | .03 | ||||||||
| PRHS | .001 | .001 | .13 | .009 | ||||||||
| Model 2 | ||||||||||||
| Drinks per week | .05 | .02 | .10 | .03 | ||||||||
| PRHS | .001 | .001 | .14 | .003 | ||||||||
| Model 3 | ||||||||||||
| RAB | −4.26 | 2.57 | −.08 | .10 | ||||||||
| PRHS | −.002 | .001 | −.11 | .03 | ||||||||
| Model 4 | ||||||||||||
| RAB | −3.77 | 2.91 | −.07 | .20 | ||||||||
| PRHS | −.002 | .001 | −.10 | .06 | ||||||||
| Cigarette use | −2.19 | .73 | −.15 | .003 | ||||||||
| Drug use | −.14 | .87 | −.01 | .87 | ||||||||
Note AUDIT = Alcohol Use Disorders Identification Test; PRHS = Perceived Risk of HIV Scale; RAB = Risk Assessment Battery. Data were transformed for analyses to reduce skewness. Perceived difficulty adhering to PrEP, drinks per week and RAB scores were log transformed. Perceived PrEP safety and confidence in efficacy were squared transformed. AUDIT score and PRHS score were square-root transformed.
Discussion
Given the continued HIV incidence rate, there have been efforts to increase PrEP awareness in the past decade (CDC, 2020) using varied approaches (Sophus & Mitchell, 2019). It is essential to learn more about characteristics of those who are aware versus unaware of PrEP, along with correlates of more and less favorable attitudes toward PrEP, particularly among young adult MSM: a subgroup at particular risk of HIV (CDC, 2020) and in the South: the region of the U.S. most heavily affected by HIV (CDC, 2020).
Among this sample of young adult MSM in the Southern U.S., PrEP awareness was 89%, which is higher than in earlier studies (Strauss et al., 2017), but comparable to more recent research (around 90%; Finlayson et al., 2019). The trend is promising, yet several significant differences between those who were aware and unaware in this study are concerning. Young adult MSM of Hispanic and “other” race/ethnicity; those who drink alcohol heavily; engage in frequent sexual risk behavior (i.e., alcohol use before or during sexual activity); with higher perceived risk of HIV were less likely to be aware of PrEP. A finding where White participants were more likely than Black participants to be aware of PrEP was at trend level. These findings are in line with prior studies indicating that non-Hispanic Whites were more likely than members of underrepresented racial/ethnic groups to have heard of PrEP (Raifman et al., 2019; Sullivan et al., 2020). These disparities in PrEP awareness parallel broader racial/ethnic health disparities, including across the HIV care continuum (CDC, 2020). Research also indicates that Black and Hispanic MSM are less likely to discuss PrEP with a health care provider and less likely to take PrEP, compared to White MSM (Kanny et al., 2019). Unequal access to PrEP is due to several individual and systemic factors (Kanny et al., 2019). To address racial/ethnic health disparities, future efforts must acknowledge and address systemic factors, including racism and the scientific community’s history of unfair treatment of Black people that continues to drive mistrust of HIV preventive efforts, including PrEP (Ball et al., 2013; Hoyt et al., 2012; Kalichman et al., 2016).
Race/ethnicity related to PrEP unawareness at a bivariate but not a multivariable level in the regression models with a similar pattern of results for cigarette and non-marijuana drug use. However, alcohol use strongly related to PrEP unawareness in bivariate analyses and regression models. Notably, PrEP unaware individuals had an AUDIT score almost double that of aware individuals. These findings align with the larger literature noting inordinately high substance use/misuse in young adult MSM (Allen et al., 2015). Further, given substantial evidence demonstrating the role of alcohol and other substance use in HIV incidence (CDC, 2020), the present findings support the need to concurrently target substance misuse in HIV prevention efforts.
In the present sample, only 15% heard about PrEP initially from public health organizations or their doctors. Physicians have reported low willingness to prescribe PrEP to those who use/misuse substances (Edelman et al., 2017). Barriers to PrEP access are present across structural (including stigma; Calabrese et al., 2019) and individual levels (including concerns that individuals who use substances will have low adherence; Adams & Balderson, 2016). Our results indicate that MSM who use substances tend to have positive attitudes toward PrEP. Thus, more work could be done to encourage physicians and health care providers to engage MSM who use substances in conversations regarding HIV and PrEP. Health care providers may have greater confidence in holding these conversations if they avail themselves of training resources (e.g., webinars provided by the Southeast AIDS Education and Training Center [SE AETC]).
In addition to racial/ethnic differences and relationships to alcohol and other substance use/misuse, the current findings linked sexual risk behavior to PrEP awareness. PrEP unaware participants reported consuming alcohol before or during sex about 2.5 times more often than PrEP aware participants. In parallel, PrEP unaware participants reported significantly higher perceived risk of HIV than PrEP aware participants. These results are in line with other research reporting lower sexual risk behaviors among PrEP aware individuals (Strauss et al., 2017).
In addition to extending the reach of information about PrEP, the effect of this information on related attitudes is critical. Overall, participants reported high perceived safety, confidence in efficacy and low perceived difficulty with adherence, suggesting optimism that young adult MSM may take and remain on PrEP if given access, based on theory and empirical evidence (Ajzen, 1991; Conner et al., 2017; McEachan et al. 2016). However, PrEP uptake remains low (Finalyson et al., 2019) and is affected by several factors (Bauermeister et al., 2013; CDC, 2020; Liu et al., 2018), thus future work could examine other potential barriers to uptake (e.g., perceptions of PrEP’s effect on sexual behaviors) in relation to information sources.
Prior research suggests characteristics of educational approaches, including information source, may be associated with PrEP-related attitudes (Ahn et al., 2019). To our knowledge, this is the first study to examine the association between initial PrEP information sources and PrEP-related attitudes. Results revealed a lack of statistically significant differences in PrEP-related attitudes across information sources. Thus, public health efforts may utilize varied dissemination tools with confidence that each can elicit favorable attitudes. Though varied approaches may have utility, it is critical to reach potential PrEP candidates where they are. Over half of PrEP-aware participants in this study first heard about PrEP via the internet. These results are comparable to prior findings (Garcia & Harris, 2017). The internet is a cost-effective, accessible platform to disseminate PrEP-related information. Social media- and other internet-based dissemination enables users to access PrEP information while maintaining anonymity, which may be particularly important to MSM given potential stigma (Hannaford et al., 2018).
Fortunately, there were also no significant differences in PrEP-related attitudes based on race/ethnicity and education levels. Though attitudes were favorable overall, it is concerning that perceived HIV risk and cigarette use were associated with less favorable attitudes. These findings support prior results linking substance use to barriers to PrEP uptake and adherence (Oldenburg et al., 2016). Tailored educational strategies may be needed for users of different substances to yield more favorable attitudes towards PrEP.
The current study had several strengths including a large, relatively diverse sample. Data were collected from Southern U.S., the region most heavily affected by HIV, and from young MSM, who are at disproportionate HIV risk (CDC, 2020). Examination of PrEP awareness and attitudes is needed in this at-risk population. Further, our study included established measures, measured alcohol use in several ways and related alcohol, marijuana, and other substance use to PrEP awareness and attitudes. This represents a novel contribution to the literature on substance use, PrEP awareness and related attitudes which has focused mainly on people who use injection drugs (Allen et al., 2020; Bazzi et al., 2018; Jo et al., 2020; McFarland et al., 2020; Roth et al., 2019; Schneider et al., 2020; Sherman et al., 2019; Walters et al., 2020; see Mistler et al., 2020; Shoptaw et al., 2013 for a review).
The study also had limitations. First, this was a web-based study, thus there is a possibility that resulting data may have been affected by fraud (e.g., individuals completing the survey multiple times). However, a fraud detection protocol that has been previously used with MSM in web-based studies (Ballard et al., 2019) was implemented. Further, research has demonstrated that web-based research, including via mTurk, yields valid data (Strickland & Stoops, 2018), including among MSM and for sexual behavior data (Beymer et al., 2018; Herrmann et al., 2015), increasing confidence in the integrity of our data. Second, although the internet was listed as the source of PrEP information by many, we did not disaggregate between specific sources (e.g., social media mobile applications). Third, although we were interested in where participants first heard about PrEP that does not imply that they acquired all information and knowledge from that source. However, considerable research suggests that initial sources of information influence resulting attitudes disproportionately (Holbert et al. 2007). In addition, given the relative recency of PrEP awareness campaigns, most participants likely learned of PrEP within recent years, further increasing the continued impact of initial knowledge sources. Though other favorable psychometric data have been reported for the Risk Assessment Battery (Metzger et al., 1993) and it has the advantage of assessing multiple risk behaviors (e.g., number of partners, condom use/non-use), its internal consistency reliability was not high. Data were collected over a period of two years, thus PrEP awareness and attitudes may have changed during the data collection period, which we could not capture in this cross-sectional survey. Another limitation is that use of other drugs besides alcohol, tobacco, and marijuana was assessed blanketly using a single item. Future research will assess associations between study variables and use of specific substances (e.g., stimulants). Lastly, the present study used a combination of recruitment methods (online and local) to reach the sample size goal, thus the sample may not be fully representative of the young adult MSM population in the Southern U.S. However, use of online recruitment, including online dating applications (e.g., Grindr) along with offline approaches, has been shown to be an effective way to recruit a diverse sample from this population (Iott et al., 2018). This study focused on the Southern U.S. because it is the region most heavily affected by HIV. However, there may also be differences across States within the South. Hence, future studies can use representative samples from each State to compare outcomes and to determine the generalizability of findings to other locations.
To summarize, PrEP is highly efficacious but underutilized, including by young adult MSM, especially those from underrepresented racial/ethnic groups. Though awareness is increasing, the current findings are concerning in that those who were unaware in the current study represented several at-risk subgroups: Hispanic and those from “other” racial/ethnic groups; individuals who use alcohol and other substances; those engaging in frequent sexual risk behaviors; and with high perceived HIV risk. Future research should explore ways to address these barriers, including by tailoring education/outreach materials to the respective audience (e.g., materials for Hispanic people could be presented in Spanish with references to Spanish culture). Future campaigns could also be disseminated where individuals who use alcohol or other substances may be more likely to see and engage with them (e.g., at liquor and convenience stores). PrEP-related attitudes were favorable overall, but those at high perceived HIV risk and cigarette smokers had somewhat less favorable attitudes. Thus, targeted outreach and educational efforts are needed for these subgroups of young adult MSM. Though the internet was the most common PrEP information source, attitudes did not differ significantly based on information source. Thus, optimistically, public health organizations have myriad options for reaching potential PrEP candidates. Future research should examine if PrEP attitudes vary for forthcoming HIV prevention tools (e.g., injectable PrEP), the utility of such novel efforts in helping address the disparities in PrEP awareness, and in turn, uptake and adherence.
Supplementary Material
Fig 1.
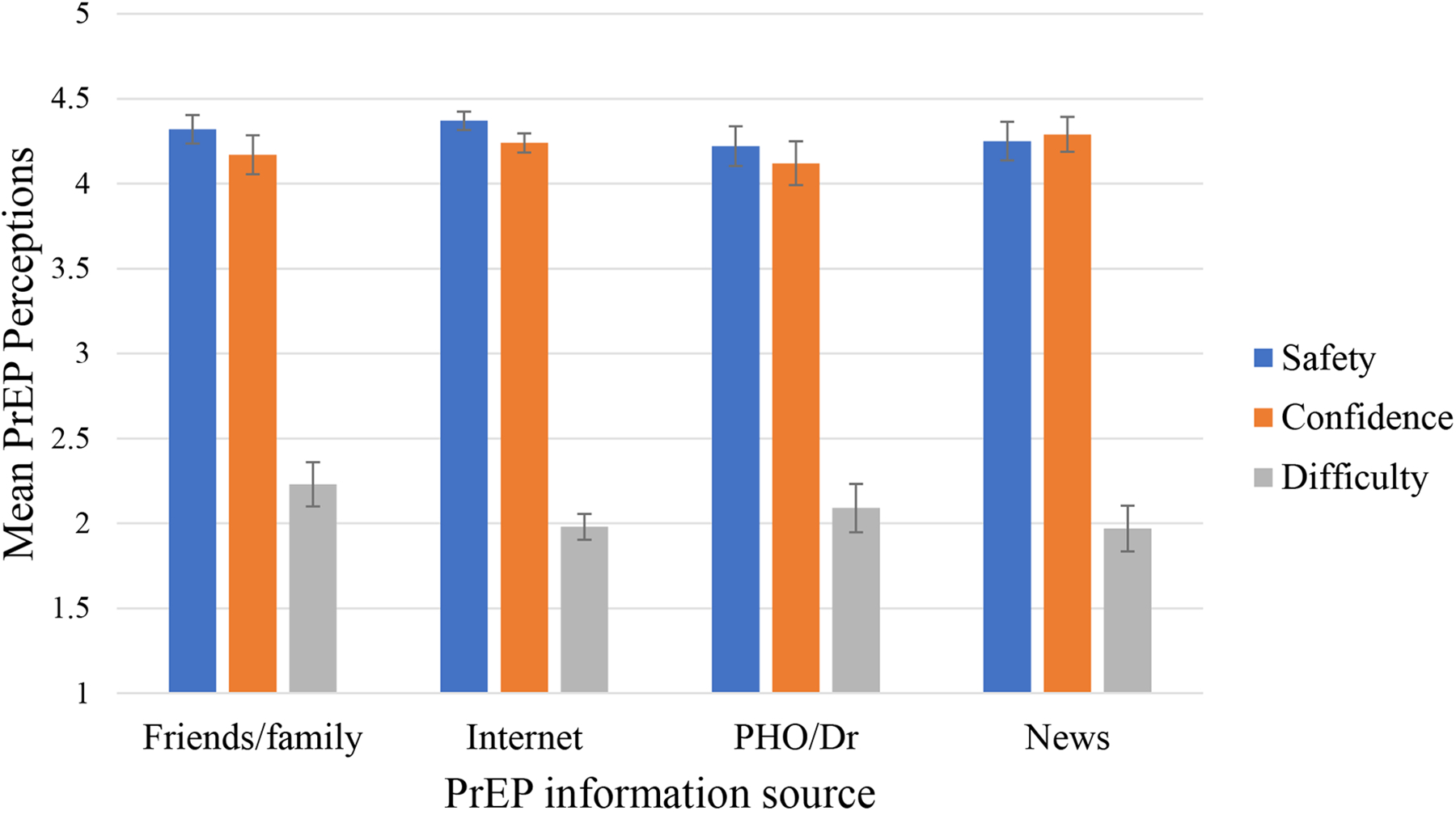
PrEP perceptions by PrEP information source
Note: Dr: Doctor. PHO: Public health organization.
References
- Adams LM, & Balderson BH (2016). HIV providers’ likelihood to prescribe pre-exposure prophylaxis (PrEP) for HIV prevention differs by patient type: A short report. AIDS Care, 28(9), 1154–1158. 10.1080/09540121.2016.1153595 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahn H-Y, Paek H-J, & Tinkham S (2019). The role of source characteristics and message appeals in public service advertising (PSA) Messages: An application of Fishbein’s expectancy-value model and the match-up hypothesis for anti-binge-drinking campaigns targeting college students. Journal of Current Issues & Research in Advertising, 40(2), 147–170. 10.1080/10641734.2018.1503112 [DOI] [Google Scholar]
- Ajzen I (1991). The theory of planned behavior. Organizational Behavior and Human Decision Processes, 50(2), 179–211. 10.1016/0749-5978(91)90020-T [DOI] [Google Scholar]
- Algarin AB, Zhou Z, Canidate S, Gebru NM, Krieger JL, Neil JM, Cook RL, & Ibañez GE (2020). PrEP awareness among people living with HIV in Florida: Florida Cohort study. AIDS Care, 428–433. 10.1080/09540121.2020.1717421 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen VC, Myers HF, & Ray L (2015). The association between alcohol consumption and condom use: Considering correlates of HIV risk among black men who have sex with men. AIDS and Behavior, 19(9), 1689–1700. 10.1007/s10461-015-1075-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Allen ST, O’Rourke A, White RH, Smith KC, Weir B, Lucas GM, Sherman SG, & Grieb SM (2020). Barriers and Facilitators to PrEP Use Among People Who Inject Drugs in Rural Appalachia: A Qualitative Study. AIDS and Behavior, 24(6), 1942–1950. 10.1007/s10461-019-02767-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arasteh K, Jarlais DCD, & Perlis TE (2008). Alcohol and HIV sexual risk behaviors among injection drug users. Drug and Alcohol Dependence, 95(1), 54–61. 10.1016/j.drugalcdep.2007.12.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, & Monteiro MG (2001). AUDIT: The Alcohol Use Disorders Identification Test: Guidelines for use in primary health care. https://apps.who.int/iris/handle/10665/67205
- Ball K, Lawson W, & Alim T (2013). Medical mistrust, conspiracy beliefs & HIV-related behavior among African Americans. Journal of Psychology and Behavioral Science, 1(1), 1–7. [Google Scholar]
- Ballard AM, Cardwell T, & Young AM (2019). Fraud detection protocol for web-based research among men who have sex with men: Development and descriptive evaluation. JMIR Public Health and Surveillance, 5(1):e12344. 10.2196/12344 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bauermeister JA, Meanley S, Pingel E, Soler JJ, & Harper GW (2013). PrEP awareness and perceived barriers among single young men who have sex with men. Current HIV Research, 11(7), 520–527. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bazzi AR, Biancarelli DL, Childs E, Drainoni M-L, Edeza A, Salhaney P, Mimiaga MJ, & Biello KB (2018). Limited knowledge and mixed interest in Pre-Exposure Prophylaxis for HIV prevention among people who inject drugs. AIDS Patient Care and STDs, 32(12), 529–537. 10.1089/apc.2018.0126 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Behler RL, Cornwell BT, & Schneider JA (2018). Patterns of social affiliations and healthcare engagement among young, black, men who have sex with men. AIDS and Behavior, 22(3), 806–818. 10.1007/s10461-016-1668-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beymer MR, Holloway IW, & Grov C (2018). Comparing self-reported demographic and sexual behavioral factors among men who have sex with men recruited through mechanical Turk, Qualtrics, and a HIV/STI clinic-based sample: Implications for researchers and providers. Archives of Sexual Behavior, 47(1), 133–142. 10.1007/s10508-016-0932-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blumenthal J, Jain S, Mulvihill E, Sun S, Hanashiro M, Ellorin E, Graber S, Haubrich R, & Morris S (2019). Perceived versus calculated HIV risk: Implications for Pre-exposure prophylaxis uptake in a randomized trial of men who have sex with men. Journal of Acquired Immune Deficiency Syndromes, 80(2), e23–e29. 10.1097/QAI.0000000000001888 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Buda R, & Zhang Y (2000). Consumer product evaluation: The interactive effect of message framing, presentation order, and source credibility. Journal of Product & Brand Management, 9(4), 229–242. 10.1108/10610420010344022 [DOI] [Google Scholar]
- Calabrese SK, Tekeste M, Mayer KH, Magnus M, Krakower DS, Kershaw TS, Eldahan AI, Gaston Hawkins LA, Underhill K, Hansen NB, Betancourt JR, & Dovidio JF (2019). Considering stigma in the provision of HIV pre-exposure prophylaxis: Reflections from current prescribers. AIDS Patient Care and STDs, 33(2), 79–88. 10.1089/apc.2018.0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Center for Behavioral Health Statistics and Quality. (2020). Results from the 2019 National Survey on Drug Use and Health: Detailed tables. Rockville, MD: Substance Abuse and Mental Health Services Administration. https://www.samhsa.gov/data/ [Google Scholar]
- Centers for Disease Control and Prevention (CDC). (2020). HIV Basics | HIV/AIDS | CDC. https://www.cdc.gov/hiv/basics/index.html
- Chan SS, Chappel AR, Maddox KEJ, Hoover KW, Huang YA, Zhu W, Cohen SM, Klein PW, & Lew ND (2020). Pre-exposure prophylaxis for preventing acquisition of HIV: A cross-sectional study of patients, prescribers, uptake, and spending in the United States, 2015–2016. PLOS Medicine, 17(4), e1003072. 10.1371/journal.pmed.1003072 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Conner M, McEachan R, Lawton R, & Gardner P (2017). Applying the reasoned action approach to understanding health protection and health risk behaviors. Social Science & Medicine, 195, 140–148. 10.1016/j.socscimed.2017.10.022 [DOI] [PubMed] [Google Scholar]
- Desai M, Field N, Grant R, & McCormack S (2017). Recent advances in pre-exposure prophylaxis for HIV. BMJ, 359. 10.1136/bmj.j5011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Edelman EJ, Moore BA, Calabrese SK, Berkenblit G, Cunningham C, Patel V, Phillips K, Tetrault JM, Shah M, Fiellin DA, & Blackstock O (2017). Primary care physicians’ willingness to prescribe HIV Pre-exposure Prophylaxis for people who inject drugs versus other risk groups. AIDS and Behavior, 21(4), 1025–1033. 10.1007/s10461-016-1612-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fallon SA, Park JN, Ogbue CP, Flynn C, & German D (2017). Awareness and acceptability of Pre-exposure HIV Prophylaxis among men who have sex with men in Baltimore. AIDS and Behavior, 21(5), 1268–1277. 10.1007/s10461-016-1619-z [DOI] [PubMed] [Google Scholar]
- Finlayson T, Cha S, Xia M, Trujillo L, Denson D, Prejean J, Kanny D, Wejnert C, & National HIV Behavioral Surveillance Study Group. (2019). Changes in HIV Preexposure Prophylaxis awareness and use among men who have sex with men—20 Urban Areas, 2014 and 2017. Morbidity and Mortality Weekly Report, 68(27), 597–603. 10.15585/mmwr.mm6827a1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- French RS, Bonell C, Wellings K, & Weatherburn P (2014). An exploratory review of HIV prevention mass media campaigns targeting men who have sex with men. BMC Public Health, 14(1), 616. 10.1186/1471-2458-14-616 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garcia M, & Harris AL (2017). PrEP awareness and decision-making for Latino MSM in San Antonio, Texas. PLOS ONE, 12(9), e0184014. 10.1371/journal.pone.0184014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garnett M, Hirsch-Moverman Y, Franks J, Hayes-Larson E, El-Sadr WM, & Mannheimer S (2018). Limited awareness of Pre-exposure Prophylaxis among black men who have sex with men and transgender women in New York city. AIDS Care, 30(1), 9–17. 10.1080/09540121.2017.1363364 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub SA, Gamarel KE, Rendina HJ, Surace A, & Lelutiu-Weinberger CL (2013). From efficacy to effectiveness: Facilitators and barriers to PrEP acceptability and motivations for adherence among MSM and transgender women in New York City. AIDS Patient Care and STDs, 27(4), 248–254. 10.1089/apc.2012.0419 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub SA, Gamarel KE, & Surace A (2017). Demographic differences in PrEP-related stereotypes: Implications for implementation. AIDS and Behavior, 21(5), 1229–1235. 10.1007/s10461-015-1129-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golub SA, Fikslin RA, Goldberg MH, Peña SM, & Radix A (2019). Predictors of PrEP uptake among patients with equivalent access. AIDS and Behavior, 23(7), 1917–1924. 10.1007/s10461-018-2376-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hannaford A, Lipshie-Williams M, Starrels JL, Arnsten JH, Rizzuto J, Cohen P, Jacobs D, & Patel VV (2018). The use of online posts to identify barriers to and facilit ators of HIV Pre-exposure Prophylaxis (PrEP) among men who have sex with men: A comparison to a systematic review of the peer-reviewed literature. AIDS and Behavior, 22(4), 1080–1095. 10.1007/s10461-017-2011-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Minor BL, Elliott V, Fernandez M, O’Neal L, McLeod L, Delacqua G, Delacqua F, Kirby J, & Duda SN (2019). The REDCap consortium: Building an international community of software platform partners. Journal of Biomedical Informatics, 95, 103208. 10.1016/j.jbi.2019.103208 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)—A metadata-driven methodology and workflow process for providing translational research informatics support. Journal of Biomedical Informatics, 42(2), 377–381. 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Herrmann ES, Johnson PS, & Johnson MW (2015). Examining delay discounting of condom-protected sex among men who have sex with men using crowdsourcing technology. AIDS and Behavior, 19(9), 1655–1665. 10.1007/s10461-015-1107-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Holbert RL, Lambe JL, Dudo AD, & Carlton KA (2007). Primacy effects of the daily show and national TV news viewing: Young viewers, political gratifications, and internal political self-efficacy. Journal of Broadcasting & Electronic Media, 51(1), 20–38. 10.1080/08838150701308002 [DOI] [Google Scholar]
- Hoyt MA, Rubin LR, Nemeroff CJ, Lee J, Huebner DM, & Proeschold-Bell RJ (2012). HIV/AIDS-related institutional mistrust among multiethnic men who have sex with men: Effects on HIV testing and risk behaviors. Health Psychology, 31(3), 269–277. 10.1037/a0025953 [DOI] [PubMed] [Google Scholar]
- Iott BE, Veinot TC, Loveluck J, Kahle E, Golson L, & Benton A (2018). Comparative analysis of recruitment strategies in a study of men who have sex with men (MSM) in Metropolitan Detroit. AIDS and Behavior, 22(7), 2296–2311. [DOI] [PubMed] [Google Scholar]
- Jo Y, Bartholomew TS, Doblecki-Lewis S, Rodriguez A, Forrest DW, Tomita-Barber J, Oves J, & Tookes HE (2020). Interest in linkage to PrEP among people who inject drugs accessing syringe services; Miami, Florida. PLOS ONE, 15(4), e0231424. 10.1371/journal.pone.0231424 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalichman SC, Eaton L, Kalichman MO, Grebler T, Merely C, & Welles B (2016). Race-based medical mistrust, medication beliefs and HIV treatment adherence: Test of a mediation model in people living with HIV/AIDS. Journal of Behavioral Medicine, 39(6), 1056–1064. 10.1007/s10865-016-9767-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanny D, Jeffries IV, W. L, Chapin-Bardales J, Denning P, Cha S, Finlayson T, & Wejnert C (2019). Racial/Ethnic disparities in HIV Preexposure Prophylaxis among men who have sex with men — 23 urban areas, 2017. Morbidity and Mortality Weekly Report, 68(37), 801–806. 10.15585/mmwr.mm6837a2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karris MY, Beekmann SE, Mehta SR, Anderson CM, & Polgreen PM (2014). Are we prepped for Preexposure Prophylaxis (PrEP)? Provider opinions on the real-world use of PrEP in the United States and Canada. Clinical Infectious Diseases, 58(5), 704–712. 10.1093/cid/cit796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- King HL, Keller SB, Giancola MA, Rodriguez DA, Chau JJ, Young JA, Little SJ, & Smith DM (2014). Pre-Exposure Prophylaxis accessibility research and evaluation (PrEPARE Study). AIDS and Behavior, 18(9), 1722–1725. 10.1007/s10461-014-0845-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koechlin FM, Fonner VA, Dalglish SL, O’Reilly KR, Baggaley R, Grant RM, Rodolph M, Hodges-Mameletzis I, & Kennedy CE (2017). Values and preferences on the use of oral Pre-exposure Prophylaxis (PrEP) for HIV prevention among multiple populations: A systematic review of the literature. AIDS and Behavior, 21(5), 1325–1335. 10.1007/s10461-016-1627-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuhns LM, Hotton AL, Schneider J, Garofalo R, & Fujimoto K (2017). Use of pre-exposure prophylaxis (PrEP) in young men who have sex with men is associated with race, sexual risk behavior and peer network size. AIDS and Behavior, 21(5), 1376–1382. 10.1007/s10461-017-1739-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu C, Ding Y, Ning Z, Gao M, Liu X, Wong FY, & He N (2018). Factors influencing uptake of pre-exposure prophylaxis: Some qualitative insights from an intervention study of men who have sex with men in China. Sexual Health, 15(1), 39–45. 10.1071/SH17075 [DOI] [PubMed] [Google Scholar]
- Mackesy-Amiti ME, Fendrich M, & Johnson TP (2008). Prevalence of recent illicit substance use and reporting bias among MSM and other urban males. Addictive Behaviors, 33(8), 1055–1060. 10.1016/j.addbeh.2008.03.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marcus JL, Hurley LB, Dentoni-Lasofsky D, Ellis CG, Silverberg MJ, Slome S, Snowden JM, & Volk JE (2019). Barriers to preexposure prophylaxis use among individuals with recently acquired HIV infection in Northern California. AIDS Care, 31(5), 536–544. 10.1080/09540121.2018.1533238 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCormack S, Dunn DT, Desai M, Dolling DI, Gafos M, Gilson R, Sullivan AK, Clarke A, Reeves I, Schembri G, Mackie N, Bowman C, Lacey CJ, Apea V, Brady M, Fox J, Taylor S, Antonucci S, Khoo SH, … Gill ON (2016). Pre-exposure prophylaxis to prevent the acquisition of HIV-1 infection (PROUD): Effectiveness results from the pilot phase of a pragmatic open-label randomised trial. The Lancet, 387(10013), 53–60. 10.1016/S0140-6736(15)00056-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McEachan R, Taylor N, Harrison R, Lawton R, Gardner P, & Conner M (2016). Meta-analysis of the reasoned action approach (RAA) to understanding health behaviors. Annals of Behavioral Medicine, 50(4), 592–612. 10.1007/s12160-016-9798-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- McFarland W, Lin J, Santos G-M, Arayasirikul S, Raymond HF, & Wilson E (2020). Low PrEP awareness and use among people who inject drugs, San Francisco, 2018. AIDS and Behavior, 24(5), 1290–1293. 10.1007/s10461-019-02682-7 [DOI] [PubMed] [Google Scholar]
- Metzger D (1993). Risk Assessment Battery (RAB). Alcohol and Drug Abuse Institute, University of Washington. https://openscholarship.wustl.edu/bsltests/24 [Google Scholar]
- Mistler CB, Copenhaver MM, & Shrestha R (2020). The Pre-exposure Prophylaxis (PrEP) care cascade in people who inject drugs: A systematic review. AIDS and Behavior, 25, 1490–1506. 10.1007/s10461-020-02988-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Murphy J, Hofacker C, & Mizerski R (2006). Primacy and recency effects on clicking behavior. Journal of Computer-Mediated Communication, 11(2), 522–535. 10.1111/j.1083-6101.2006.00025.x [DOI] [Google Scholar]
- Napper LE, Fisher DG, & Reynolds GL (2012). Development of the perceived risk of HIV scale. AIDS and Behavior, 16(4), 1075–1083. 10.1007/s10461-011-0003-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute on Alcohol Abuse and Alcoholism (NIAAA). Helping Patients With Alcohol Problems: A Health Practitioner’s Guide. Bethesda, MD: NIAAA; (2003). NIH Pub. No. 03–3769. https://pubs.niaaa.nih.gov/publications/practitioner/cliniciansguide2005/guide.pdf [Google Scholar]
- Nunn AS, Brinkley-Rubinstein L, Oldenburg CE, Mayer KH, Mimiaga M, Patel R, & Chan PA (2017). Defining the HIV pre-exposure prophylaxis care continuum. AIDS (London, England), 31(5), 731–734. 10.1097/QAD.0000000000001385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oldenburg CE, Mitty JA, Biello KB, Closson EF, Safren SA, Mayer KH, & Mimiaga MJ (2016). Differences in attitudes about HIV Pre-Exposure Prophylaxis use among stimulant versus alcohol using men who have sex with men. AIDS and Behavior, 20(7), 1451–1460. 10.1007/s10461-015-1226-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pollock JA, Halkitis PN, Moeller RW, Solomon TM, Barton SC, Blachman-Forshay J, Siconolfi DE, & Love HT (2012). Alcohol use among young men who have sex with men. Substance Use & Misuse, 47(1), 12–21. 10.3109/10826084.2011.618963 [DOI] [PubMed] [Google Scholar]
- Raifman J, Dean LT, Montgomery MC, Almonte A, Arrington-Sanders R, Stein MD, Nunn AS, Sosnowy CD, & Chan PA (2019). Racial and ethnic disparities in HIV pre-exposure prophylaxis awareness among men who have sex with men. AIDS and Behavior, 23(10), 2706–2709. 10.1007/s10461-019-02462-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Reback CJ, Fletcher JB, Shoptaw S, & Grella CE (2013). Methamphetamine and other substance use trends among street-recruited men who have sex with men, from 2008 to 2011. Drug and Alcohol Dependence, 133(1), 262–265. 10.1016/j.drugalcdep.2013.06.007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rice WS, Stringer KL, Sohail M, Crockett KB, Atkins GC, Kudroff K, Batey DS, Hicks J, Turan JM, Mugavero MJ, & Turan B (2019). Accessing Pre-exposure Prophylaxis (PrEP): Perceptions of current and potential PrEP users in Birmingham, Alabama. AIDS and Behavior, 23(11), 2966–2979. 10.1007/s10461-019-02591-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roth A, Tran N, Piecara B, Welles S, Shinefeld J, & Brady K (2019). Factors associated with awareness of Pre-exposure Prophylaxis for HIV among persons who inject drugs in Philadelphia: National HIV behavioral surveillance, 2015. AIDS and Behavior, 23(7), 1833–1840. 10.1007/s10461-018-2293-0 [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, De La Fuente JR, & Grant M (1993). Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction, 88(6), 791–804. 10.1111/j.1360-0443.1993.tb02093.x [DOI] [PubMed] [Google Scholar]
- Schneider KE, White RH, Musci RJ, O’Rourke A, Kilkenny ME, Sherman SG, & Allen ST (2020). The relationship between polysubstance injection drug use, HIV risk behaviors, and interest in Pre-Exposure Prophylaxis (PrEP) among people who inject drugs in rural West Virginia. Journal of Studies on Alcohol and Drugs, 81(6), 740–749. 10.15288/jsad.2020.81.740 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherman SG, Schneider KE, Park JN, Allen ST, Hunt D, Chaulk CP, & Weir BW (2019). PrEP awareness, eligibility, and interest among people who inject drugs in Baltimore, Maryland. Drug and Alcohol Dependence, 195, 148–155. 10.1016/j.drugalcdep.2018.08.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shoptaw S, Montgomery B, Williams CT, El-Bassel N, Aramrattana A, Metzger DS, Kuo I, Bastos FI, & Strathdee SA (2013). Not just the needle: The state of HIV prevention science among substance users and future directions. Journal of Acquired Immune Deficiency Syndromes. 63, S174–S178. 10.1097/QAI.0b013e3182987028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sidebottom D, Ekström AM, & Strömdahl S (2018). A systematic review of adherence to oral Pre-exposure Prophylaxis for HIV - How can we improve uptake and adherence? BMC Infectious Diseases, 18(1), 581. 10.1186/s12879-018-3463-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith DK, Toledo L, Smith DJ, Adams MA, & Rothenberg R (2012). Attitudes and program preferences of African-American urban young adults about Pre-Exposure Prophylaxis (PrEP). AIDS Education and Prevention, 24(5), 408–421. 10.1521/aeap.2012.24.5.408 [DOI] [PubMed] [Google Scholar]
- Solomon TM, Halkitis PN, Moeller RW, & Pappas MK (2012). Levels of methamphetamine use and addiction among gay, bisexual, and other men who have sex with men. Addiction Research & Theory, 20(1), 21–29. 10.3109/16066359.2011.552816 [DOI] [Google Scholar]
- Sophus AI, & Mitchell JW (2019). A review of approaches used to increase awareness of Pre-exposure Prophylaxis (PrEP) in the United States. AIDS and Behavior, 23(7), 1749–1770. 10.1007/s10461-018-2305-0 [DOI] [PubMed] [Google Scholar]
- Strauss BB, Greene GJ, Phillips G, Bhatia R, Madkins K, Parsons JT, & Mustanski B (2017). Exploring patterns of awareness and use of HIV Pre-Exposure Prophylaxis among young men who have sex with men. AIDS and Behavior, 21(5), 1288–1298. 10.1007/s10461-016-1480-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Strickland JC, & Stoops WW (2018). Feasibility, acceptability, and validity of crowdsourcing for collecting longitudinal alcohol use data. Journal of the Experimental Analysis of Behavior, 110(1), 136–153. 10.1002/jeab.445 [DOI] [PubMed] [Google Scholar]
- Sullivan MC, & Eaton LA (2020). Intersecting barriers to PrEP awareness and uptake in black men who have sex with men in Atlanta, GA: A syndemic perspective. International Journal of Behavioral Medicine. 1–11. 10.1007/s12529-020-09925-1 [DOI] [PubMed] [Google Scholar]
- Sullivan PS, Sanchez TH, Zlotorzynska M, Chandler CJ, Sineath R, Kahle E, & Tregear S (2020). National trends in HIV pre‐exposure prophylaxis awareness, willingness and use among United States men who have sex with men recruited online, 2013 through 2017. Journal of the International AIDS Society, 23(3). 10.1002/jia2.25461 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomann M, Grosso A, Zapata R, & Chiasson MA (2018). “WTF is PrEP?”: Attitudes towards pre-exposure prophylaxis among men who have sex with men and transgender women in New York City. Culture, Health & Sexuality, 20(7), 772–786. 10.1080/13691058.2017.1380230 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Torres TS, Luz PM, Boni RBD, Vasconcellos M. T. L. de, Hoagland B, Garner A, Moreira RI, Veloso VG, & Grinsztejn B (2019). Factors associated with PrEP awareness according to age and willingness to use HIV prevention technologies: The 2017 online survey among MSM in Brazil. AIDS Care, 31(10), 1193–1202. 10.1080/09540121.2019.1619665 [DOI] [PubMed] [Google Scholar]
- Walters SM, Kral AH, Simpson KA, Wenger L, & Bluthenthal RN (2020). HIV Pre-Exposure Prophylaxis prevention awareness, willingness, and perceived barriers among people who inject drugs in Los Angeles and San Francisco, CA, 2016–2018. Substance Use & Misuse, 55(14), 2409–2419. 10.1080/10826084.2020.1823419 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


