Abstract
Background
Findings and limitations of previous studies on persistent organic pollutants (POPs) and pancreatic cancer risk support conducting further research in prospective cohorts.
Methods
We conducted a prospective case-control study nested within the European Prospective Investigation into Cancer and Nutrition (EPIC) cohort. Participants were 513 pancreatic cancer cases and 1020 matched controls. Concentrations of 22 POPs were measured in plasma collected at baseline.
Results
Some associations were observed at higher concentrations of p, p’-DDT, trans-nonachlor, β-hexachlorocyclohexane and the sum of six organochlorine pesticides and of 16 POPs. The odds ratio (OR) for the upper quartile of trans-nonachlor was 1.55 (95% confidence interval 1.06-2.26; P for trend = 0.025). Associations were stronger in the groups predefined as most valid (participants having fasted >6 h, with microscopic diagnostic confirmation, normal weight, and never smokers), and as most relevant (follow-up ≥10 years). Among participants having fasted >6 h, the ORs were relevant for 10 of 11 exposures. Higher ORs were also observed among cases with microscopic confirmation than in cases with a clinical diagnosis, and among normal-weight participants than in the rest of participants. Among participants with a follow-up ≥10 years, estimates were higher than in participants with a shorter follow-up (for trans-nonachlor: OR = 2.14, 1.01 to 4.53, P for trend = 0.035). Overall, trans-nonachlor, three PCBs and the two sums of POPs were the exposures most clearly associated with pancreatic cancer risk.
Conclusions
Individually or in combination, most of the 22 POPs analysed did not or only moderately increased the risk of pancreatic cancer.
Keywords: Pancreatic cancer, persistent organic pollutants, biomarkers, environmental health, methods
Key Messages.
This is the first study that measured persistent organic pollutants (POPs) long before pancreatic cancer occurred.
Several of the 22 POPs analysed did not increase the risk of pancreatic cancer, but others did, some in a dose-dependent manner.
Associations were stronger in the groups predefined as most valid and relevant.
Whereas the null associations are reassuring, results also suggest that policies controlling POPs contribute to prevent pancreatic cancer.
Introduction
Knowledge on modifiable causes of exocrine pancreatic cancer, including environmental causes, is scant.1–8 The methodological characteristics and findings of previous studies on persistent organic pollutants (POPs)9,10 and pancreatic cancer risk1,11 support as well the conduct of further research. Notably, all four previous studies1,4 measured POP concentrations in blood samples drawn at the time of diagnosis of pancreatic cancer, thus being prone to disease progression bias, a form of reverse causation through which the pathophysiological progression of the disease before diagnosis alters concentrations of the lipophilic contaminants in biological samples; as a consequence, disease-altered exposure estimates lack aetiological significance. All four studies found some POPs associated with pancreatic cancer risk;1,4 together with the other relevant studies,1–8,11 their findings were of reference in designing the present study.
Therefore, the main objective of the present study was to investigate in a prospective cohort associations between baseline plasma concentrations of selected POPs and the subsequent risk of exocrine pancreatic cancer, based on previously defined methodological options.1
Methods
Study design and participants
The EPIC study was approved by the Ethical Review Board of the International Agency for Research on Cancer (IARC, Lyon) and by the local ethical committees. Participants signed an informed consent before completing questionnaires at baseline.
The study design has been described in detail.1,12 Briefly, we performed a case-control study nested within the European Prospective Investigation into Cancer and Nutrition (EPIC). The EPIC cohort recruited 521 457 participants aged 35 to 70 years between 1992 and 2000 in 23 centres from 10 European countries. Three bio-repositories from EPIC contributed samples for the present study: the repositories in Denmark and in Sweden (Västerbotten county, including Umeå), and the IARC central repository, which stored the biospecimens of Germany, the UK, The Netherlands, Italy, Spain, Greece, France and Norway.
At recruitment, participants had blood drawn and a questionnaire collected baseline information about sociodemographic characteristics, lifestyles (such as usual diet, lifetime history of alcohol and tobacco consumption) and medical history. Participants were followed until cancer diagnosis, death, migration or the end of the follow-up period (2007, 2010 and 2014 for Denmark, IARC and Sweden, respectively), whichever occurred first. The median length of follow-up of participants was 11.6 years.1
A total of 513 pancreatic cancer cases were included in the present study: 135 from Denmark, 79 from Sweden and 299 from the other mentioned countries.1 Exclusion criteria were: (i) cases of endocrine pancreatic cancer; (ii) occurrence of other malignant tumours preceding the diagnosis of pancreatic cancer, except for non-melanoma skin cancer; (iii) participants diagnosed with pancreatic cancer during the first 2 years after blood draw (5 years for cases from Denmark); and (iv) cases with less than two straws of plasma remaining available.1 Cases were diagnosed from 1995 to 2014. For each case, two control participants alive and free of cancer at the time of diagnosis of the index case were selected using an incidence density sampling procedure13; only six cases had just one control. Thus, a total of 1020 matched controls were included. Matching factors were study centre, sex, age at blood collection, date and time of the day of blood collection, fasting status and, for women, use of exogenous hormones.1
Characteristics of participants were also previously published.1 At study entry, a higher proportion of cases than controls were current smokers (33% vs 23%, respectively), and had diabetes mellitus (6% of cases vs 3% of controls); no differences between cases and controls were observed for body mass index (BMI), total lipids and its components, alcohol consumption or physical activity. Smoking was barely associated with POP concentrations (Spearman’s rho from −0.16 to 0.15), very similarly in cases and controls.
Chemical analyses of plasma concentrations of persistent organic pollutants and lipids
Laboratory methods have also previously been described.1,14 Concentrations of 22 compounds were measured by gas chromatography–triple quadrupole mass spectrometry (GC-MS/MS) in 200 µL plasma samples at the National Institute for Health and Welfare (THL), Finland. Measured POPs were: three polybrominated diphenyl ethers (PBDEs 47, 99, 153), eight non-dioxin-like polychlorinated biphenyls (PCB congeners 74, 99, 138, 153, 170, 180, 183 and 187), two dioxin-like PCBs (congeners 118 and 156), and nine organochlorine (OC) pesticides or their metabolites: dichlorodiphenyltrichloroethane (p, p’-DDT), dichlorodiphenyldichloroethene (p, p’-DDE), α-hexachlorocyclohexane (α-HCH), β-HCH, γ-HCH, pentachlorobenzene (PeCB), hexachlorobenzene (HCB), trans-nonachlor and oxychlordane.
The instrument used was an Agilent 7010 GC-MS/MS system (Wilmington, DE, USA), GC column DB-5MS UI (J&W Scientific, 20 m, ID 0.18 mm, 0.18 μm). Limits of detection and quantification for POPs were 2 to 16 pg/mL and 5 to 40 pg/mL, respectively.1 When a sample had a concentration of a compound below the detection threshold, it was assigned the mid-value of this limit; when a compound was detected but under the quantification threshold, the mid-value between detection and quantification limits was used. We focused the main statistical analyses on the 16 compounds that were detected in ≥90% of participants: p, p’-DDT, p, p’-DDE, oxychlordane, trans-nonachlor, HCB, β-HCH and all 10 PCB congeners.1
Measurements of total cholesterol and triglycerides were carried out enzymatically by Abbott Architect reagents (Abbott Laboratories, Abbott Park, IL, USA). Total lipids (TL) were calculated by the standard formula 2.15 POP concentrations were individually converted to lipid-based concentrations (i.e. corrected for TL) by dividing the crude plasma POP concentration by TL.15
Statistical analyses
Univariate statistics were computed as customary.13 To assess differences in POP concentrations by case-control status, a Mann–Whitney U test was used. To estimate the magnitude of the associations between plasma concentrations of POPs and pancreatic cancer risk, odds ratios (ORs) and their corresponding 95% confidence intervals (CIs) were calculated by conditional logistic regression.13 When the ORs showed no linear trend, the P-value was derived from Wald’s test. When a linear trend was apparent, the test for such trend was the multivariate analogue of Mantel’s extension test.13 Models were built based on four causal scenarios, two of which (A and B) were a priori deemed more relevant for the present study; they both suggested that more valid estimates are obtained when crude POP concentrations are analysed.1 In addition, we also present results from models using lipid-corrected POPs and adjusting for BMI and smoking.
We also analysed associations in the most valid stratum1 of four variables: fasting (>6 h), diagnostic basis (microscopic confirmation), BMI (normal weight) and smoking (never smokers). Similarly, we analysed associations in the most relevant stratum of the interval between blood extraction and date of cancer diagnosis of the index case (index date) (≥10 years). When models were restricted to a stratum (e.g. normal weight, never smokers) of a non-matching factor (e.g. BMI, smoking), ORs and CIs were calculated by unconditional logistic regression adjusting for all matching factors. The rationale for other analyses by sex, age at diagnosis and birth cohort (1919–38, 1939–45, 1946–64) has also been explained.1
POP concentrations were entered in the models either as crude concentrations (pg/mL) or individually corrected by TL (ng/g of lipid),15 using quartile categories. Cut-off points for the quartiles were based on the distribution of controls’ concentrations (Table 1).1 In models for POPs detected in <90% of participants (PBDEs 47, 99, 153, α-HCH, γ-HCH and PeCB), concentrations were categorized as ‘non-detected’, ‘detected, non-quantified’ and ‘detected and quantified’.
Table 1.
Plasma concentrations of persistent organic pollutants (POPs) in cases and controlsa
| Persistent organic pollutants | Cases (n = 513) | Controls (n = 1020) | P-valueb | ||
|---|---|---|---|---|---|
| Organochlorine (OC) pesticides | |||||
| Dichlorodiphenyltrichloroethane (p, p’-DDT) | 90.9 | (49.7–160.5) | 82.2 | (46.5–170.2) | 0.219 |
| Dichlorodiphenyldichloroethene (p, p’-DDE) | 3590.3 | (1870.2–6914.2) | 3255.6 | (1695.9–6623.6) | 0.126 |
| Oxychlordane | 55.7 | (38.9–85.2) | 55.0 | (36.8–81.4) | 0.199 |
| Trans-nonachlor | 77.0 | (50.1–125.2) | 72.1 | (46.6–118.9) | 0.080 |
| Hexachlorobenze | 405.2 | (263.5–746.3) | 389.1 | (247.5–807.1) | 0.535 |
| β-hexachlorocyclohexane | 373.7 | (200.7–689.3) | 332.9 | (200.5–658.6) | 0.361 |
| Polychlorinated biphenyls (PCBs) | |||||
| PCB 118 | 149.3 | (97.0–230.1) | 152.7 | (98.1–235.0) | 0.718 |
| PCB 156 | 126.5 | (83.3–169.8) | 121.7 | (83.3–169.8) | 0.723 |
| PCB 138 | 641.8 | (438.3–945.0) | 632.3 | (424.5–924.9) | 0.450 |
| PCB 153 | 1036.0 | (713.1–1459.9) | 1017.0 | (707.0–1445.6) | 0.657 |
| PCB 180 | 795.9 | (579.6–1122.6) | 819.1 | (573.5–1133.2) | 0.881 |
| PCB 74 | 65.8 | (44.6–97.9) | 66.6 | (44.7–97.3) | 0.852 |
| PCB 99 | 73.7 | (46.0–110.9) | 69.6 | (45.9–105.8) | 0.387 |
| PCB 170 | 368.2 | (258.0–509.6) | 370.1 | (256.2–520.3) | 0.970 |
| PCB 183 | 77.5 | (51.4–115.8) | 75.1 | (48.7–111.9) | 0.424 |
| PCB 187 | 194.8 | (131.8–277.5) | 190.0 | (124.8–278.3) | 0.718 |
| Sum of all 10 PCBsc | 3631.6 | (2485.2–5011.5) | 3571.0 | (2496.6–4946.1) | 0.711 |
| Sum of 4 PCBsd | 2676.5 | (1851.0–3720.1) | 2645.0 | (1835.1–3698.1) | 0.709 |
| Sum of orders, 6 OC pesticidese | 16.0 | (12–19) | 15.0 | (11–19) | 0.105 |
| Sum of orders, 16 POPsf | 41.0 | (31–51) | 40.0 | (29–51) | 0.380 |
| Number of POPs at high concentrations (nPhc) | 3.0 | (0–7) | 2.0 | (0–7) | 0.363 |
Crude concentrations expressed in median (and percentile 25–percentile 75), pg/mL (parts per trillion, ppt). The individual compounds are the 16 persistent organic pollutants (POPs) detected in ≥90% of participants.1
P-value for Mann-Whitney U test (two-tailed).
Sum of the individual concentrations of eight non-dioxin-like polychlorinated biphenyls (PCBs) (congeners 74, 99, 138, 153, 170, 180, 183 and 187), and two dioxin-like PCBs (congeners 118 and 156).
Sum of the individual concentrations of PCB congeners 118, 138, 153 and 180.
p, p’-DDT, p, p’-DDE, oxychlordane, trans-nonachlor, hexachlorobenze, and β-hexachlorocyclohexane, the 6 organochlorine (OC) pesticides detected at higher concentrations. For these 6 OC pesticides, the sum of orders was computed by categorizing each pesticide in quartiles, and then adding the category number, thus producing a value ranging between 6 and 24.
For the 16 POPs quantified in ≥90% of participants, the sum of orders was computed by categorizing each POP in quartiles, and then adding the category number, thus producing a value ranging between 16 and 64.1
To assess exposure to multiple compounds, we computed: (i) the sum of all 10 PCBs; (ii) the sum of four PCBs; (iii) the sum of orders of the six OC pesticides quantified in ≥90% of participants; and (iv) the sum of orders of the 16 POPs quantified in ≥90% of participants (Table 1).1,16 We computed the number of POPs detected in each person at high concentrations (nPhc) by adding the number of POPs (out of the 16 POPs quantified in ≥90% of participants) whose plasma concentrations were equal to or greater than a selected cut-off point, as percentile 75.17
A relatively large number of associations were tested without changing the level of statistical significance; both the latter, the precision of the estimates and the magnitude of the associations were assessed.13,18 Analyses were conducted using SPSS version 22 and R version 3.5.2.
Results
Crude (unadjusted) concentrations of the 22 POPs analysed were similar in cases and controls. Thus, median concentrations were only slightly higher in cases than controls (P-values ranged from 0.080 to 0.970); this was so for both lipid-uncorrected (Table 1) and lipid-corrected concentrations.
The risk of pancreatic cancer increased slightly with increasing concentrations of certain POPs, sometimes in a dose-dependent manner. Relevant ORs were observed for p, p′-DDT, trans-nonachlor, β-HCH and for the sum of orders of the six organochlorine pesticides and of the 16 POPs (lipid-uncorrected POP concentrations, Table 2, Model 1). The OR for the upper quartile of trans-nonachlor was 1.55 (95% CI 1.06-2.26, P for trend = 0.025). In models adjusted for BMI, such ORs became slightly weaker (Table 2, Model 2). When Models 2 were further adjusted for tobacco smoking, the estimates were unchanged; the OR for the upper quartile β-HCH went from 1.23 to 1.20 (95% CI 0.72-1.99, P = 0.016). No relevant associations were observed when analysing lipid-corrected concentrations of POPs adjusted for BMI and smoking (Table 2, Model 3). Further adjusting for alcohol, physical activity, diabetes or education did not materially change the effect estimates shown in Table 2.
Table 2.
Risk of pancreatic cancer according to quartiles of concentrations of persistent organic pollutants (POPs)a
| Persistent organic pollutants | Model 1 |
Model 2 |
Model 3 |
||||||
|---|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | P b | OR | (95% CI) | P b | OR | (95% CI) | P b | |
| p, p’-DDT | |||||||||
| 1st quartile | 1.00 | 0.029 | 1.00 | 0.037 | 1.00 | 0.909 | |||
| 2nd quartile | 1.11 | (0.80–1.53) | 1.06 | (0.77–1.48) | 1.09 | (0.79–1.52) | |||
| 3rd quartile | 1.57 | (1.12–2.19) | 1.46 | (1.04–2.06) | 1.14 | (0.80–1.62) | |||
| 4th quartile | 1.12 | (0.74–1.70) | 0.97 | (0.62–1.50) | 1.09 | (0.69–1.73) | |||
| p, p’-DDE | |||||||||
| 1st quartile | 1.00 | 0.129c | 1.00 | 0.313c | 1.00 | 0.391c | |||
| 2nd quartile | 1.05 | (0.77–1.45) | 1.03 | (0.75–1.42) | 1.10 | (0.80–1.53) | |||
| 3rd quartile | 1.22 | (0.88–1.69) | 1.15 | (0.83–1.61) | 1.18 | (0.84–1.66) | |||
| 4th quartile | 1.29 | (0.88–1.88) | 1.18 | (0.80–1.74) | 1.16 | (0.78–1.73) | |||
| Oxychlordane | |||||||||
| 1st quartile | 1.00 | 0.135 | 1.00 | 0.257 | 1.00 | 0.397c | |||
| 2nd quartile | 1.40 | (1.02–1.93) | 1.36 | (0.98–1.88) | 1.14 | (0.82–1.59) | |||
| 3rd quartile | 1.19 | (0.84–1.69) | 1.18 | (0.83–1.68) | 1.17 | (0.82–1.66) | |||
| 4th quartile | 1.42 | (0.98–2.06) | 1.35 | (0.92–1.97) | 1.19 | (0.81–1.76) | |||
| Trans-nonachlor | |||||||||
| 1st quartile | 1.00 | 0.025c | 1.00 | 0.038c | 1.00 | 0.110c | |||
| 2nd quartile | 1.27 | (0.91–1.76) | 1.32 | (0.94–1.85) | 1.12 | (0.80–1.58) | |||
| 3rd quartile | 1.38 | (0.98–1.96) | 1.39 | (0.97–1.98) | 1.25 | (0.87–1.79) | |||
| 4th quartile | 1.55 | (1.06–2.26) | 1.54 | (1.04–2.27) | 1.36 | (0.92–2.00) | |||
| β-hexachlorocyclohexane | |||||||||
| 1st quartile | 1.00 | 0.008 | 1.00 | 0.014 | 1.00 | 0.395 | |||
| 2nd quartile | 0.78 | (0.55–1.09) | 0.74 | (0.52–1.04) | 0.79 | (0.54–1.15) | |||
| 3rd quartile | 1.41 | (0.96–2.05) | 1.30 | (0.88–1.93) | 1.04 | (0.69–1.58) | |||
| 4th quartile | 1.37 | (0.86–2.17) | 1.23 | (0.75–2.01) | 1.01 | (0.59–1.72) | |||
| Sum of orders, 6 OC pesticides | |||||||||
| 1st quartile | 1.00 | 0.045c | 1.00 | 0.110c | 1.00 | 0.680 | |||
| 2nd quartile | 1.29 | (0.92–1.79) | 1.21 | (0.86–1.70) | 1.19 | (0.87–1.64) | |||
| 3rd quartile | 1.56 | (1.08–2.27) | 1.47 | (1.00–2.16) | 1.09 | (0.75–1.58) | |||
| 4th quartile | 1.48 | (1.00–2.20) | 1.37 | (0.91–2.07) | 1.20 | (0.81–1.78) | |||
| Sum of orders, 16 POPs | |||||||||
| 1st quartile | 1.00 | 0.034 | 1.00 | 0.031 | 1.00 | 0.254 | |||
| 2nd quartile | 1.49 | (1.06–2.09) | 1.49 | (1.05–2.11) | 1.38 | (0.98–1.93) | |||
| 3rd quartile | 1.67 | (1.17–2.39) | 1.68 | (1.17–2.41) | 1.15 | (0.78–1.68) | |||
| 4th quartile | 1.38 | (0.94–2.02) | 1.34 | (0.90–1.97) | 1.14 | (0.77–1.70) | |||
OR, odds ratio, an OR = 1 indicates the reference category; CI, confidence interval; p, p’-DDT, dichlorodiphenyltrichloroethane; p, p’-DDE, dichlorodiphenyldichloroethene.
Quartile cut-off points based on the distribution of plasma concentrations in controls, see Table 1; e.g. for p, p’-DDT (Models 1 and 2), the highest concentration for the first quartile is 46.5 pg/mL, the highest concentration for the second quartile is 82.2 pg/mL and the highest concentration for the third quartile is 170.2 pg/mL. All models from conditional (matched) logistic regression. Matching factors: centre, sex, age at blood collection, date and time at blood collection, fasting status and, for women, use of exogenous hormones. Model 1: crude POP concentrations. n = 1533 (513 cases and 1020 controls). Model 2: crude POP concentrations; model further adjusted for body mass index. n = 1493 (501 cases and 992 controls). Model 3: POP concentrations individually corrected by total lipids; model further adjusted for body mass index and tobacco smoking (never, former, and current). n = 1464 (493 cases and 971 controls).
Unless otherwise specified, P-value derived from Wald’s test, which was applied when no linear trend was apparent.
Test for linear trend (multivariate analogue of Mantel’s extension test).
No associations were observed for hexachlorobenzene and PCBs (Supplementary Table S1, available as Supplementary data at IJE online), nor for PBDEs and the other less detected POPs (Supplementary Table S2, available as Supplementary data at IJE online). Highly similar risks were observed for all compounds between women and men.
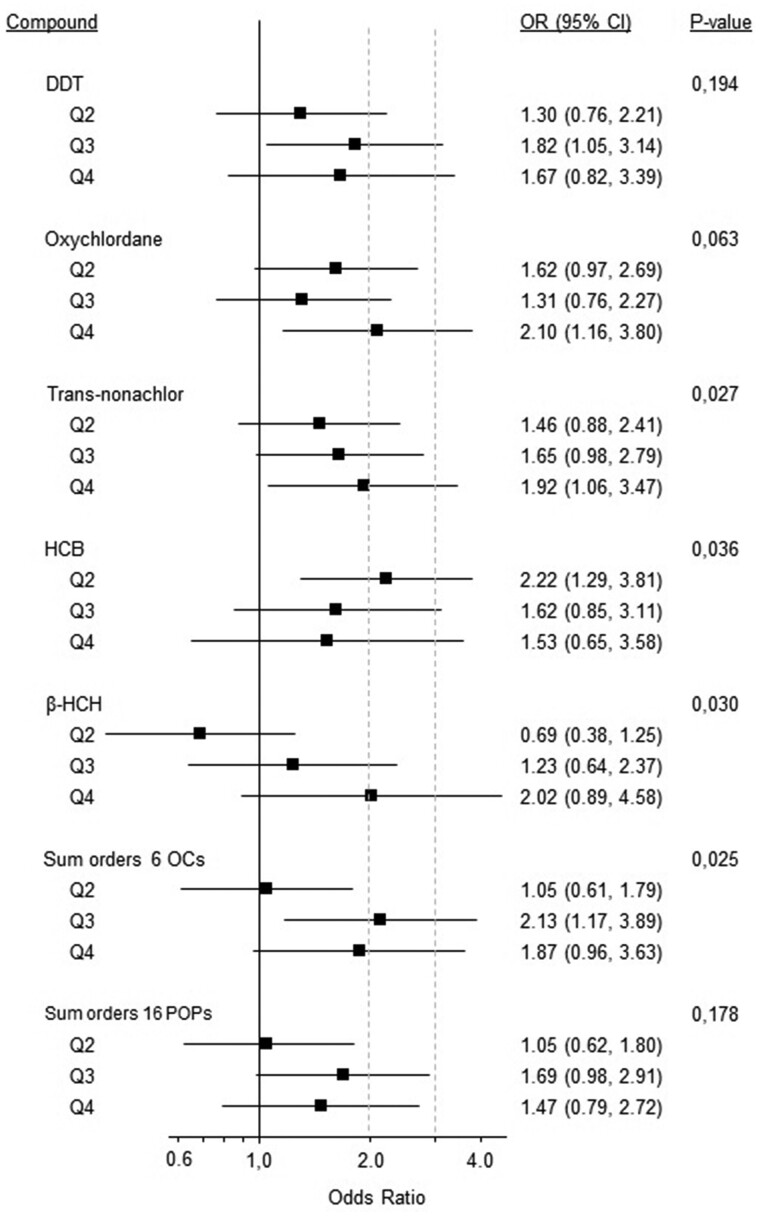
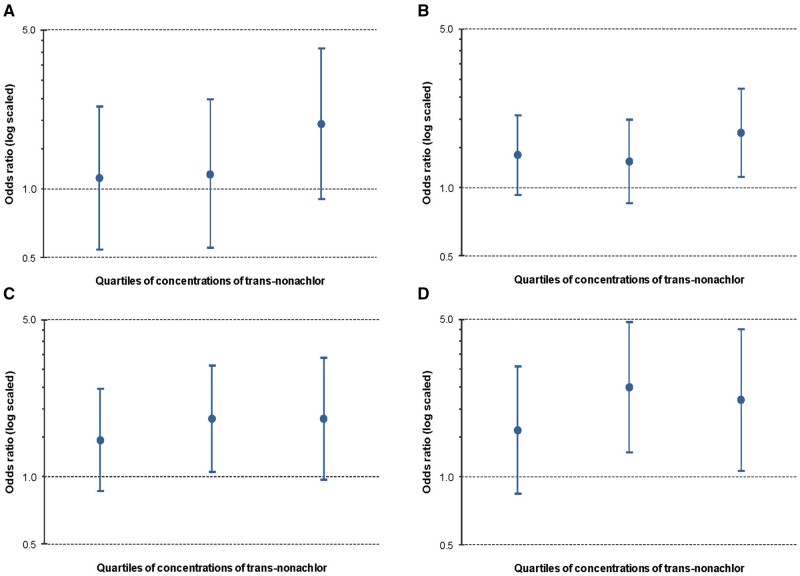
As compared with estimates for the entire study population, virtually all ORs were higher in the strata a priori defined as most valid or relevant (Table 3 and Figures 1 and 2; Supplementary Table S3, available as Supplementary data at IJE online), although precision was sometimes lower due to lower numbers. Among participants having fasted >6 h at blood collection, the ORs were ≥1.5 for 10 of the 11 exposure categories shown in Table 3; the OR for the fourth quartile of p, p′-DDE was 2.23 (95% CI 1.02-4.88, P for trend = 0.012). Higher ORs were also observed among cases with microscopic confirmation than in cases with a clinical diagnosis, with relevant estimates for p, p′-DDT, oxychlordane, trans-nonachlor, β-HCH and the two sums of orders (Table 3). Higher ORs were also observed among normal-weight participants than in the rest of participants, with relevant estimates for all 11 exposure categories and particularly for the three PCBs and the sum of orders of the six OC pesticides (ORs above 2 and P <0.05) (Table 3). Results were essentially unchanged when correcting for total lipids. Among participants with a time from blood extraction to the index date ≥10 years, estimates were also higher than in participants with a shorter follow-up, with relevant estimates for 10 exposure categories, particularly for trans-nonachlor, three PCBs and the sum of orders of the 16 POPs (ORs above 2 and some near 3, P <0.05) (Table 3). When models were further adjusted by tobacco smoking, the ORs were materially unchanged; for example, among participants with a follow-up ≥10 years, the OR for the upper quartile of trans-nonachlor was 2.14 (95% CI 1.01-4.53, P for trend = 0.035). Among never smokers, the ORs were relevant (≥1.5 and all P-values ≤0.194) for p, p′-DDT, oxychlordane, trans-nonachlor, hexachlorobenzene, β-HCH, two PCBs and the two sums of orders (Figure 1). Overall, trans-nonachlor (Figure 2), three PCBs and the two sums of orders were the exposures most clearly associated with pancreatic cancer risk.
Table 3.
Risk of pancreatic cancer according to quartiles of concentrations of persistent organic pollutants (POPs) in groups predefined as most valid of fasting (>6 h), diagnostic basis (microscopic confirmation) and weight (normal), and as most relevant (follow-up ≥10 years)a
| Persistent organic pollutants | Fasting >6 hb,c |
Microscopic confirmationb,d |
Normal weighte,f |
Follow-up ≥10 yearsb,g |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | (95% CI) | P h | OR | (95% CI) | P h | OR | (95% CI) | P h | OR | (95% CI) | P h | |
| p, p′-DDT | ||||||||||||
| 1st quartile | 1.00 | 0.204 | 1.00 | 0.074 | 1.00 | 0.180 | 1.00 | 0.026 | ||||
| 2nd quartile | 1.06 | (0.55–2.03) | 1.15 | (0.80–1.67) | 1.45 | (0.91–2.32) | 1.22 | (0.70–2.14) | ||||
| 3rd quartile | 1.81 | (0.93–3.53) | 1.57 | (1.06–2.33) | 1.57 | (0.94–2.61) | 1.94 | (1.10–3.42) | ||||
| 4th quartile | 1.23 | (0.52–2.91) | 1.04 | (0.62–1.73) | 0.98 | (0.46–2.11) | 0.93 | (0.44–1.99) | ||||
| p, p’-DDE | ||||||||||||
| 1st quartile | 1.00 | 0.012i | 1.00 | 0.177i | 1.00 | 0.012i | 1.00 | 0.088i | ||||
| 2nd quartile | 0.98 | (0.46–2.07) | 1.05 | (0.73–1.51) | 1.32 | (0.81–2.14) | 1.23 | (0.70–2.15) | ||||
| 3rd quartile | 1.85 | (0.94–3.63) | 1.22 | (0.84–1.79) | 2.04 | (1.23–3.39) | 1.44 | (0.81–2.56) | ||||
| 4th quartile | 2.23 | (1.02–4.88) | 1.31 | (0.84–2.03) | 1.79 | (0.95–3.37) | 1.71 | (0.90–3.26) | ||||
| Oxychlordane | ||||||||||||
| 1st quartile | 1.00 | 0.072 | 1.00 | 0.192 | 1.00 | 0.111i | 1.00 | 0.242 | ||||
| 2nd quartile | 1.51 | (0.77–2.94) | 1.37 | (0.94–1.99) | 1.04 | (0.63–1.74) | 1.52 | (0.84–2.73) | ||||
| 3rd quartile | 0.88 | (0.41–1.87) | 1.14 | (0.76–1.71) | 1.31 | (0.76–2.24) | 1.81 | (0.99–3.31) | ||||
| 4th quartile | 1.78 | (0.84–3.81) | 1.50 | (0.97–2.31) | 1.58 | (0.85–2.94) | 1.34 | (0.69–2.63) | ||||
| Trans-nonachlor | ||||||||||||
| 1st quartile | 1.00 | 0.058i | 1.00 | 0.032i | 1.00 | 0.041i | 1.00 | 0.026i | ||||
| 2nd quartile | 1.12 | (0.54–2.30) | 1.39 | (0.93–2.08) | 1.45 | (0.86–2.46) | 1.61 | (0.84–3.09) | ||||
| 3rd quartile | 1.16 | (0.55–2.47) | 1.30 | (0.85–1.99) | 1.81 | (1.05–3.11) | 2.49 | (1.28–4.85) | ||||
| 4th quartile | 1.93 | (0.90–4.14) | 1.74 | (1.11–2.73) | 1.81 | (0.97–3.37) | 2.19 | (1.06–4.51) | ||||
| β-hexachlorocyclohexane | ||||||||||||
| 1st quartile | 1.00 | 0.573 | 1.00 | 0.024 | 1.00 | 0.049 | 1.00 | 0.225 | ||||
| 2nd quartile | 0.74 | (0.37–1.45) | 0.73 | (0.50–1.06) | 0.68 | (0.40–1.16) | 0.78 | (0.43–1.41) | ||||
| 3rd quartile | 0.88 | (0.39–1.97) | 1.34 | (0.86–2.07) | 1.40 | (0.78–2.54) | 1.48 | (0.77–2.84) | ||||
| 4th quartile | 1.32 | (0.46–3.76) | 1.31 | (0.74–2.33) | 1.42 | (0.64–3.16) | 1.32 | (0.55–3.16) | ||||
| PCB 99 | ||||||||||||
| 1st quartile | 1.00 | 0.071 | 1.00 | 0.223 | 1.00 | 0.007i | 1.00 | 0.008i | ||||
| 2nd quartile | 0.71 | (0.34–1.46) | 0.75 | (0.50–1.11) | 1.05 | (0.62–1.80) | 1.14 | (0.61–2.14) | ||||
| 3rd quartile | 1.15 | (0.57–2.31) | 1.05 | (0.72–1.53) | 1.45 | (0.86–2.44) | 2.20 | (1.19–4.07) | ||||
| 4th quartile | 1.62 | (0.80–3.30) | 1.04 | (0.69–1.56) | 2.01 | (1.14–3.54) | 2.04 | (1.06–3.94) | ||||
| PCB 138 | ||||||||||||
| 1st quartile | 1.00 | 0.319 | 1.00 | 0.749 | 1.00 | 0.035i | 1.00 | 0.024i | ||||
| 2nd quartile | 0.87 | (0.41–1.82) | 0.95 | (0.63–1.43) | 1.97 | (1.13–3.41) | 1.30 | (0.65–2.61) | ||||
| 3rd quartile | 1.20 | (0.56–2.59) | 0.96 | (0.63–1.47) | 1.64 | (0.90–3.00) | 1.85 | (0.90–3.79) | ||||
| 4th quartile | 1.56 | (0.70–3.44) | 1.13 | (0.73–1.76) | 2.32 | (1.23–4.36) | 2.13 | (1.01–4.51) | ||||
| PCB 183 | ||||||||||||
| 1st quartile | 1.00 | 0.072i | 1.00 | 0.369i | 1.00 | 0.027i | 1.00 | 0.023i | ||||
| 2nd quartile | 1.38 | (0.57–3.33) | 1.10 | (0.74–1.64) | 1.55 | (0.90–2.65) | 2.21 | (1.15–4.25) | ||||
| 3rd quartile | 1.41 | (0.59–3.38) | 1.15 | (0.76–1.75) | 1.57 | (0.90–2.73) | 2.46 | (1.20–5.05) | ||||
| 4th quartile | 2.12 | (0.86–5.21) | 1.22 | (0.79–1.90) | 2.10 | (1.14–3.88) | 2.76 | (1.31–5.80) | ||||
| Sum of orders, 16 POPs | ||||||||||||
| 1st quartile | 1.00 | 0.080i | 1.00 | 0.053 | 1.00 | 0.047i | 1.00 | 0.016i | ||||
| 2nd quartile | 1.77 | (0.79–3.97) | 1.41 | (0.95–2.10) | 1.57 | (0.92–2.67) | 2.41 | (1.20–4.83) | ||||
| 3rd quartile | 2.17 | (0.98–4.78) | 1.80 | (1.18–2.73) | 1.75 | (1.03–3.00) | 3.02 | (1.45–6.29) | ||||
| 4th quartile | 2.19 | (0.97–4.92) | 1.42 | (0.92–2.20) | 1.83 | (1.00–3.35) | 3.00 | (1.39–6.46) | ||||
| Sum of orders, 6 OC pesticides | ||||||||||||
| 1st quartile | 1.00 | 0.211i | 1.00 | 0.047i | 1.00 | 0.014i | 1.00 | 0.149i | ||||
| 2nd quartile | 1.19 | (0.61–2.32) | 1.07 | (0.73–1.56) | 1.41 | (0.87–2.27) | 1.45 | (0.81–2.60) | ||||
| 3rd quartile | 1.75 | (0.85–3.58) | 1.53 | (1.00–2.35) | 1.71 | (0.97–3.04) | 1.88 | (0.97–3.66) | ||||
| 4th quartile | 1.56 | (0.71–3.41) | 1.46 | (0.92–2.31) | 2.22 | (1.15–4.26) | 1.71 | (0.84–3.46) | ||||
| Number of POPs at high concentrations (nPhc) | ||||||||||||
| 0 | 1.00 | 0.048i | 1.00 | 0.181i | 1.00 | 0.050i | 1.00 | 0.061 | ||||
| 1–5 | 1.78 | (0.95–3.35) | 1.13 | (0.80–1.61) | 1.64 | (1.05–2.55) | 1.78 | (1.09–2.93) | ||||
| >5 | 2.01 | (1.05–3.84) | 1.28 | (0.89–1.84) | 1.61 | (0.97–2.69) | 1.71 | (0.99–2.97) | ||||
OR, odds ratio, an OR = 1 indicates the reference category; CI, onfidence interval; p, p’-DDT, dichlorodiphenyltrichloroethane; p, p’-DDE, dichlorodiphenyldichloroethene.
All four models are based on crude concentrations of persistent organic pollutants (POPs). Columns show results for the predefined1 most valid stratum of three variables: fasting (>6 h), diagnostic basis (microscopic confirmation) and normal weight, and for the most relevant stratum of the interval between blood extraction and date of cancer diagnosis of the index case (index date) (follow-up ≥10 years). Results for the most valid stratum of smoking (never smokers) are shown in Figure 1.
Conditional logistic regression, model further adjusted for body mass index.
n = 430 (150 cases and 280 controls).
n = 1110 (372 cases and 738 controls).
Since the model is restricted to a stratum (normal weight) of a non-matching factor (body mass index), ORs and CIs were calculated by unconditional logistic regression adjusting for all matching factors.
n = 611 (197 cases and 414 controls).
n = 532 (179 cases and 353 controls).
Unless otherwise specified, P-value derived from Wald’s test.
Test for linear trend (multivariate analogue of Mantel’s extension test).
Figure 1.
Risk of pancreatic cancer according to quartiles of concentrations of persistent organic pollutants (POPs) in never smokers. Models based on crude POP concentrations. Since each model is restricted to a stratum (never smokers) of a non-matching factor (smoking), odds ratios (ORs) and confidence intervals (CIs) were calculated by unconditional logistic regression adjusting for all matching factors, as well as for body mass index (BMI); thus, results from the model can be compared with results from Model 2 in Table 2. n = 638 (202 cases and 436 controls)
Figure 2.
Risk of pancreatic cancer according to quartiles of trans-nonachlor in the most valid or relevant stratum of fasting (>6 h) (A), diagnostic basis (microscopic confirmation) (B), weight (normal weight) (C), and interval between blood extraction and index date (≥10 years) (D). From left to right: Q2, Q3 and Q4. Models based on crude concentrations. (A, B, D) Conditional logistic regression, model further adjusted for body mass index. (C) Unconditional logistic regression adjusting for all matching factors. (A) n = 430 (150 cases and 280 controls). (B) n = 1110 (372 cases and 738 controls). (C) n = 611 (197 cases and 414 controls). (D) n = 532 (179 cases and 353 controls). Q, quartile
There were also associations with hexachlorobenzene, the two sums of PCBs, BDE 47 and BDE 99 among normal-weight participants, as well as with hexachlorobenzene and some measures of PCB exposure among participants with a follow-up ≥10 years (Supplementary Table S3).
Among the three birth cohorts, the only clearly different risk pattern was observed for PCB 99 in the younger cohort (1946–64): the OR for the upper quartile was 5.08 (95% CI 1.13-22.88) (conditional model with lipid-corrected POPs and further adjusted for BMI and smoking, with consistent estimates in the other models). Analyses by age at diagnosis of pancreatic cancer did not reveal consistent differences.
Although analyses by study centre were not a primary objective,1 we did note increased ORs in Sweden; for example, the OR for the upper quartile of trans-nonachlor was 3.92 (Supplementary Table S4, Model 2, available as Supplementary data at IJE online); the corresponding figure for PCBs 99, 138 and 183 was always >3.4; for the sum of 10 PCBs, 9.79, and for the sum of orders of the 16 POPs, 3.30 (all P <0.02). When further adjusted for smoking, the ORs remained similar or slightly weaker; for example, the OR for the upper quartile of trans-nonachlor was 3.75 (95% CI 1.00-14.12, P for trend = 0.016). When lipid-corrected POPs were adjusted for BMI and smoking, most ORs for the pesticides decreased again, whereas the ORs for the PCBs remained unchanged (Supplementary Table S4, Model 3).
Discussion
A few moderately increased risks of pancreatic cancer were apparent for the highest crude concentrations of certain POPs, sometimes with a dose-response relationship.19,20 Risks were weaker or not consistently increased when analysing lipid-corrected concentrations. Overall, trans-nonachlor, some PCBs and the two sums of orders were the exposures most clearly associated with pancreatic cancer risk. These compounds have been found to increase pancreatic cancer risk in some but not all four previous studies:1,4 more clearly, trans-nonachlor in the San Francisco Bay Area Study and in the Örebro study, and PCBs in San Francisco.
Based on the a priori defined causal scenarios A and B,1 we built conditional logistic regression models (i.e., adjusting for matching factors), essentially using crude concentrations of POPs. Therefore, precedence should be given to Models 1 and 2 of Table 2, and to models in Table 3. There were no differences between cases and controls in total lipids and its components—as in scenario A in Supplemental Figure 1 in Gasull et al.1—nor in BMI. Smoking was more frequent among cases than controls, but it was not associated with POPs. These observations argue against the need to condition on total lipids, BMI or smoking.16,21 Nevertheless, to explore alternative scenarios, in some instances we also used lipid-corrected POPs or further conditioned on BMI or smoking.
As compared with estimates for all participants, associations were stronger in the groups predefined as most valid or relevant.1 Thus, higher ORs were observed among normal-weight participants than in the rest of participants, with ORs above 2 for three PCBs and the sum of orders of the six OC pesticides. Among participants who had fasted >6 h at blood collection, the ORs were remarkable for 10 exposure categories. Whereas matching factors included age, date and time of the day of blood collection, and fasting status, results are coherent with the notion that exposure misclassification is lower and the comparison of POP measures between cases and controls more accurate among participants who fast longer or have normal weight.1,9,13,15,16
Higher ORs were also observed among cases with microscopic confirmation than in cases with a clinical diagnosis; disease misclassification is less likely among cases with microscopic confirmation.1,11 Among never smokers—a stratum where residual confounding was likely lower—the ORs were also increased for several compounds.
Among participants with a follow-up ≥10 years, estimates were also higher than in participants with a shorter follow-up, with relevant estimates for 10 exposure categories.
Analyses by birth cohort and by age at diagnosis of pancreatic cancer did not reveal consistent differences. Cases were between 30 and 75 years old at study entry, they were diagnosed from 1995 to 2014, their median length of follow-up was 12 years and the median age at diagnosis was 66 years.1 Demographic characteristics were thus quite diverse, but a longer follow-up would be desirable.
Although POPs have long half-lives, one single measure of POP concentrations in adulthood is obviously more limited than two or more measures to assess the intensity and duration of POP body burden (e.g., in youth and adulthood).19–21 In cohorts as large as EPIC, repeated measurements of biomarkers are not common.
Given the available knowledge on adverse pancreatic effects of other contaminants,2–9,11,16,22,23 the number of compounds analysed was small. Although the associations were generally weak, their population impact might be relevant since low-dose exposure is widespread,19,20,22 and some populations worldwide have POP concentrations similar to the concentrations where we observed associations.10 Whereas the null and moderate associations are reassuring, the positive findings are in line with policies that aim to prevent human exposure to POPs.
By study centre, POP estimates were only consistently increased in Sweden. Compared with participants from the other countries, more participants from Sweden had been fasting for more than 6 h, were younger at blood collection and had a lower BMI, longer follow-up and higher concentrations of total lipids.1 These factors did not explain the stronger associations in Sweden. We can only speculate why; for example, perhaps in Sweden but not in the other countries, the compounds that appeared more strongly associated with an increased risk of pancreatic cancer were also associated with other, unmeasured contaminants also associated with an increased risk.
Our planned analyses include assessing: the joint and separate impact of POPs, dietary patterns and anthropometric factors on pancreatic cancer risk; the possible mediating role of type 2 diabetes in the association between POPs and that risk; and the possible mediating role of POPs in the association between type 2 diabetes and such risk. In this report, we did not adjust the associations between plasma concentrations of POPs and pancreatic cancer risk by dietary factors24 because diet is a common source of POPs.13 The influence of diet and other lifestyle and personal factors on POP concentrations in cases and controls will also be undertaken soon.16,22 Future studies with even larger sizes might analyse differences in risks among countries.
The validity of this study nested within the half-million people EPIC cohort is substantially higher than previous studies.1,4,11 Notably, this is the first time that POPs were measured long before pancreatic cancer occurred; this lag time yielded similar concentrations of lipids and BMI among cases and controls, and it practically ruled out disease progression bias.1 The study also included a higher number of participants and contaminants than previous studies, and precision was good even for associations of modest magnitude. More complex studies would be warranted to measure at several points during the life course and with different latency periods the possible effects on pancreatic cancer risk of a higher variety of chemical mixtures, as well as their interactions with other biological, clinical and environmental factors, including interactions with changes in BMI and with endocrine, metabolic and inflammatory disorders.1,9,11,21,25
Individually or in combination, most of the 22 POPs analysed did not or only moderately increased the risk of pancreatic cancer.
Supplementary Data
Supplementary data are available at IJE online.
Data availability
The data underlying this article belong to the European Prospective Investigation into Cancer and Nutrition (EPIC). Reasonable requests may be addressed to the corresponding author.
Funding
This work was supported in part by research grants from: Government of Catalonia [2014 SGR 1012, 2017 SGR 439]; Instituto de Salud Carlos III—FEDER [FIS PI13/00020, FIS PI17/00088 and CIBER de Epidemiología y Salud Pública—CIBERESP], Government of Spain; Fundació La Marató de TV3 [20132910]; CRUE-Santander Fondo Supera Covid-19 [15072020]; and the Hellenic Health Foundation. Swedish investigators acknowledge the contribution from Biobank Sweden, supported by the Swedish Research Council [VR 2017–00650].
Supplementary Material
Acknowledgements
The authors gratefully acknowledge technical and scientific assistance provided by Natàlia Pallarès, Marc Domínguez, Yolanda Rovira and Meri Corominas. The work of Tuula Rissanen, Arja Moilanen and Eija Mehtonen in analysing POPs in plasma samples is also gratefully acknowledged. Swedish investigators thank the County Council of Västerbotten for providing data and samples.
Conflict of Interest
None declared.
Contributor Information
Miquel Porta, Hospital del Mar Institute of Medical Research (IMIM PSMar), Barcelona, Catalonia, Spain; Universitat Autònoma de Barcelona, Barcelona, Catalonia, Spain; Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain.
Magda Gasull, Hospital del Mar Institute of Medical Research (IMIM PSMar), Barcelona, Catalonia, Spain; Universitat Autònoma de Barcelona, Barcelona, Catalonia, Spain; Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain.
José Pumarega, Hospital del Mar Institute of Medical Research (IMIM PSMar), Barcelona, Catalonia, Spain; Universitat Autònoma de Barcelona, Barcelona, Catalonia, Spain; Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain.
Hannu Kiviranta, Department of Health Security, National Institute for Health and Welfare, Kuopio, Finland.
Panu Rantakokko, Department of Health Security, National Institute for Health and Welfare, Kuopio, Finland.
Ole Raaschou-Nielsen, Danish Cancer Society Research Center, Copenhagen, Denmark.
Ingvar A Bergdahl, Department of Biobank Research, Umeå University, Umeå, Sweden; Occupational and Environmental Medicine, Department of Public Health and Clinical Medicine, Umeå University, Umeå, Sweden.
Torkjel Manning Sandanger, Department of Community Medicine, UiT-The Arctic University of Norway, Tromsø, Norway.
Antoni Agudo, Unit of Nutrition and Cancer, Catalan Institute of Oncology (ICO-IDIBELL), Barcelona, Spain.
Charlotta Rylander, Department of Community Medicine, UiT-The Arctic University of Norway, Tromsø, Norway.
Therese Haugdahl Nøst, Department of Community Medicine, UiT-The Arctic University of Norway, Tromsø, Norway.
Carolina Donat-Vargas, Cardiovascular and Nutritional Epidemiology, Institute of Environmental Medicine, Karolinska Institutet, Stockholm, Sweden; Department of Preventive Medicine and Public Health, School of Medicine, Universidad Autónoma de Madrid, CEI UAM+CSIC, Madrid, Spain.
Dagfinn Aune, Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, UK.
Alicia K Heath, Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, UK.
Lluís Cirera, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; Department of Epidemiology, Murcia Regional Health Council, IMIB—Arrixaca, Murcia, Spain; Department of Health and Social Sciences, University of Murcia, Murcia, Spain.
Fernando Goñi-Irigoyen, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; Health Department of Basque Government, Public Health Laboratory in Gipuzkoa, San Sebastian, Spain; Health Research Institute Biodonostia, San Sebastian, Spain.
Juan Alguacil, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; University of Huelva, Huelva, Spain.
Àlex Giménez-Robert, Hospital del Mar Institute of Medical Research (IMIM PSMar), Barcelona, Catalonia, Spain; Universitat Autònoma de Barcelona, Barcelona, Catalonia, Spain.
Anne Tjønneland, Danish Cancer Society Research Center, Copenhagen, Denmark.
Malin Sund, Department of Surgical and Perioperative Sciences, Umeå University, Umeå, Sweden.
Kim Overvad, Department of Public Health, Aarhus University, Aarhus, Denmark.
Francesca Romana Mancini, CESP, Faculté de médecine (USVQ), Université Paris-Sud, INSERM, Université Paris-Saclay, Villejuif, France; Inserm UMR1018, Institut Gustave Roussy, Villejuif, France.
Vinciane Rebours, Pancreatology Department, Beaujon Hospital, AP-HP, Clichy, France; Inserm UMR1149, DHU Unit, Paris-Diderot University, Paris, France.
Marie-Christine Boutron-Ruault, CESP, Faculté de médecine (USVQ), Université Paris-Sud, INSERM, Université Paris-Saclay, Villejuif, France; Inserm UMR1018, Institut Gustave Roussy, Villejuif, France.
Rudolf Kaaks, Division of Cancer Epidemiology, German Cancer Research Center (DKFZ), Heidelberg, Germany.
Matthias B Schulze, Department of Molecular Epidemiology, German Institute of Human Nutrition Potsdam, Rehbruecke, Nuthetal, Germany; Institute of Nutrition Science, University of Potsdam, Nuthetal, Germany.
Antonia Trichopoulou, Hellenic Health Foundation, Athens, Greece.
Domenico Palli, Cancer Risk Factors and Life-Style Epidemiology Unit, Institute for Cancer Research, Prevention and Clinical Network—ISPRO, Florence, Italy.
Sara Grioni, Epidemiology and Prevention Unit, Fondazione IRCCS Istituto Nazionale dei Tumori di Milano, Milan, Italy.
Rosario Tumino, Cancer Registry and Histopathology Department, “Civic—M.P. Arezzo” Hospital, ASP Ragusa, Ragusa, Italy.
Alessio Naccarati, Molecular and Genetic Epidemiology Unit, Italian Institute for Genomic Medicine (IIGM), Turin, Italy.
Salvatore Panico, Dipartimento di Medicina Clinica e Chirurgia, Federico II University, Naples, Italy.
Roel Vermeulen, Institute for Risk Assessment Sciences (IRAS), Utrecht University, Utrecht, The Netherlands.
J Ramón Quirós, Public Health Directorate, Asturias, Spain.
Miguel Rodríguez-Barranco, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; Escuela Andaluza de Salud Pública (EASP), Instituto de Investigación Biosanitaria ibs.GRANADA, Granada, Spain.
Sandra M Colorado-Yohar, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; Department of Epidemiology, Murcia Regional Health Council, IMIB—Arrixaca, Murcia, Spain; National Faculty of Public Health, University of Antioquia, Medellín, Colombia.
María-Dolores Chirlaque, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; Department of Epidemiology, Murcia Regional Health Council, IMIB—Arrixaca, Murcia, Spain; Department of Health and Social Sciences, University of Murcia, Murcia, Spain.
Eva Ardanaz, Spanish Consortium for Research on Epidemiology and Public Health (CIBERESP), Madrid, Spain; Navarra Public Health Institute, Pamplona, Spain; IdiSNA, Navarra Institute for Health Research, Pamplona, Spain.
Nick Wareham, MRC Epidemiology Unit, Institute of Metabolic Science, University of Cambridge, Cambridge, UK.
Tim Key, Cancer Epidemiology Unit, Nuffield Department of Population Health, University of Oxford, Oxford, UK.
Mattias Johansson, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Neil Murphy, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Pietro Ferrari, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Inge Huybrechts, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Veronique Chajes, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Carlos Alberto Gonzalez, Unit of Nutrition and Cancer, Catalan Institute of Oncology (ICO-IDIBELL), Barcelona, Spain.
Bas Bueno-de-Mesquita, Department for Determinants of Chronic Diseases (DCD), National Institute for Public Health and the Environment (RIVM), Bilthoven, The Netherlands.
Marc Gunter, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Elisabete Weiderpass, International Agency for Research on Cancer (IARC), World Health Organization, Lyon, France.
Elio Riboli, Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, UK.
Eric J Duell, Oncology Data Analytics Program, Catalan Institute of Oncology (ICO-IDIBELL), Barcelona, Spain.
Verena Katzke, Division of Cancer Epidemiology, German Cancer Research Center (DKFZ), Heidelberg, Germany.
Paolo Vineis, Department of Epidemiology and Biostatistics, School of Public Health, Imperial College London, London, UK; Molecular and Genetic Epidemiology Unit, Italian Institute for Genomic Medicine (IIGM), Turin, Italy.
References
- 1. Gasull M, Pumarega J, Kiviranta H et al. Methodological issues in a prospective study on plasma concentrations of persistent organic pollutants and pancreatic cancer risk within the EPIC cohort. Environ Res 2019;169:417–33. [DOI] [PubMed] [Google Scholar]
- 2. Amaral AFS, Porta M, Silverman DT et al. Pancreatic cancer risk and levels of trace elements. Gut 2012;61:1583–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Antwi SO, Eckert EC, Sabaque CV et al. Exposure to environmental chemicals and heavy metals, and risk of pancreatic cancer. Cancer Causes Control 2015;26:1583–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Hardell L, Carlberg M, Hardell K et al. Decreased survival in pancreatic cancer patients with high concentrations of organochlorines in adipose tissue. Biomed Pharmacother 2007;61:659–64. [DOI] [PubMed] [Google Scholar]
- 5. Barone E, Corrado A, Gemignani F, Landi S. Environmental risk factors for pancreatic cancer: an update. Arch Toxicol 2016;90:2617–42. [DOI] [PubMed] [Google Scholar]
- 6. Djordjevic VR, Wallace DR, Schweitzer A et al. Environmental cadmium exposure and pancreatic cancer: evidence from case control, animal and in vitro studies. Environ Int 2019;128:353–61. [DOI] [PubMed] [Google Scholar]
- 7. Eriksen KT, Sørensen M, McLaughlin JK et al. Perfluorooctanoate and perfluorooctanesulfonate plasma levels and risk of cancer in the general Danish population. J Natl Cancer Inst 2009;101:605–09. [DOI] [PubMed] [Google Scholar]
- 8. Landman A, Feetham L, Stuckey D. Working together to reduce the burden of pancreatic cancer. Lancet Oncol 2020;21:334–35. [DOI] [PubMed] [Google Scholar]
- 9. Gore AC, Chappell VA, Fenton SE et al. EDC-2: the Endocrine Society's second scientific statement on endocrine-disrupting chemicals. Endocr Rev 2015;36:E1–E150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Porta M, Puigdomènech E, Ballester F et al. Monitoring concentrations of persistent organic pollutants in the general population: the international experience. Environ Int 2008;34:546–61. [DOI] [PubMed] [Google Scholar]
- 11. Porta M. Role of organochlorine compounds in the etiology of pancreatic cancer: a proposal to develop methodological standards. Epidemiology 2001;12:272–76. [DOI] [PubMed] [Google Scholar]
- 12. Riboli E, Hunt KJ, Slimani N et al. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr 2002;5:1113–24. [DOI] [PubMed] [Google Scholar]
- 13. Rothman KJ, Greenland S, Lash TL (eds). Modern Epidemiology. 3rd edn. Philadelphia, PA: Lippincott-Raven, 2008. [Google Scholar]
- 14. Koponen J, Rantakokko P, Airaksinen R, Kiviranta H. Determination of selected perfluorinated alkyl acids and persistent organic pollutants from a small volume human serum sample relevant for epidemiological studies. J Chromatogr A 2013;1309:48–55. [DOI] [PubMed] [Google Scholar]
- 15. Porta M, Jariod M, López T et al. Correcting serum concentrations of organochlorine compounds by lipids: alternatives to the organochlorine/total lipids ratio. Environ Int 2009;35:1080–85. [DOI] [PubMed] [Google Scholar]
- 16. Gasull M, Castell C, Pallarès N et al. Blood concentrations of persistent organic pollutants and unhealthy metabolic phenotypes in normal-weight, overweight and obese individuals. Am J Epidemiol 2018;187:494–506. [DOI] [PubMed] [Google Scholar]
- 17. Pumarega J, Gasull M, Lee DH, López T, Porta M. Number of persistent organic pollutants detected at high concentrations in blood samples of the United States population. PLoS One 2016;11:e0160432. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Amrhein V, Greenland S, McShane B. Scientists rise up against statistical significance. Nature 2019;567:305–07. [DOI] [PubMed] [Google Scholar]
- 19. Lee DH, Porta M, Jacobs DR, Vandenberg LN. Chlorinated persistent organic pollutants, obesity, and type 2 diabetes. Endocr Rev 2014;35:557–601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Vandenberg LN, Colborn T, Hayes TB et al. Hormones and endocrine-disrupting chemicals: low-dose effects and nonmonotonic dose responses. Endocr Rev 2012;33:378–455. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Suarez-Lopez JR, Clemesha CG, Porta M, Gross MD, Lee DH. Organochlorine pesticides and polychlorinated biphenyls (PCBs) in early adulthood and blood lipids over a 23-year follow-up. Environ Toxicol Pharmacol 2019;66:24–35. [DOI] [PubMed] [Google Scholar]
- 22. Zong G, Valvi D, Coull B et al. Persistent organic pollutants and risk of type 2 diabetes: a prospective investigation among middle-aged women in Nurses' Health Study II. Environ Int 2018;114:334–42. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.National Toxicology Program (NTP). NTP Technical Report on the Toxicology and Carcinogenesis Studies of Perfluorooctanoic Acid (CAS No. 335–67-1) Administered in Feed to Sprague Dawley (Hsd: Sprague Dawley® SD®) Rats. Technical Report 598. Research Triangle Park, NC: National Toxicology Program, 2019. [DOI] [PMC free article] [PubMed]
- 24. Park JY, Bueno-de-Mesquita HB, Ferrari P et al. Dietary folate intake and pancreatic cancer risk: Results from the European prospective investigation into cancer and nutrition. Int J Cancer 2019;144:1511–21. [DOI] [PubMed] [Google Scholar]
- 25. Wood SA, Xu F, Armitage JM, Wania F. Unravelling the relationship between body mass index and polychlorinated biphenyl concentrations using a mechanistic model. Environ Sci Technol 2016;50:10055–64. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data underlying this article belong to the European Prospective Investigation into Cancer and Nutrition (EPIC). Reasonable requests may be addressed to the corresponding author.