Abstract
Background
Oil and gas extraction produces air pollutants that are associated with increased risks of hypertension. To date, no study has examined residential proximity to oil and gas extraction and hypertensive conditions during pregnancy. This study quantifies associations between residential proximity to oil and gas development on gestational hypertension and eclampsia.
Methods
We utilized a population-based retrospective birth cohort in Texas (1996–2009), where mothers reside <10 km from an active or future drilling site (n = 2 845 144.) Using full-address data, we linked each maternal residence at delivery to assign exposure and evaluate this exposure with respect to gestational hypertension and eclampsia. In a difference-in-differences framework, we model the interaction between maternal health before (unexposed) or after (exposed) the start of drilling activity (exposed) and residential proximity near (0–1, >1–2 or >2–3 km) or far (≥3–10 km) from an active or future drilling site.
Results
Among pregnant women residing 0–1 km from an active oil or gas extraction site, we estimate 5% increased odds of gestational hypertension [95% confidence interval (CI): 1.00, 1.10] and 26% increased odds of eclampsia (95% CI: 1.05, 1.51) in adjusted models. This association dissipates in the 1- to 3-km buffer zones. In restricted models, we find elevated odds ratios among maternal ages ≤35 years at delivery, maternal non-Hispanic White race, ≥30 lbs gained during pregnancy, nulliparous mothers and maternal educational attainment beyond high school.
Conclusions
Living within 1 km of an oil or gas extraction site during pregnancy is associated with increased odds of hypertensive conditions during pregnancy.
Keywords: Gestational hypertension, eclampsia, oil drilling, gas drilling, resource extraction, difference-in-differences
Key Messages.
Among pregnant women who reside within 1 km of at least one oil or gas drilling site, we find 5% increased odds of gestational hypertension and 26% increased odds of eclampsia.
We find no evidence of this association for pregnant women who reside in within 1–2 km or 2–3 km of at least one oil or gas drilling site.
Restricted models show that women who were most sensitive to drilling exposures were under age 35 years, were nulliparous, were non-Hispanic White mothers and had greater than a high-school education.
However, we also find an unexpected reduced association among Hispanic women and women with less than a high-school education.
Given that hypertensive conditions during pregnancy carry serious risks for pregnant women and their infants, these findings warrant further examination.
Background
Gestational hypertension, pre-eclampsia and eclampsia are hypertensive conditions in pregnancy that threaten maternal health. Up to 8% of all pregnancies are impacted by hypertensive conditions and 16% of maternal deaths are attributed to complications arising from high blood pressure.1 Gestational hypertension, which is defined as incident blood pressure of >140/90 at two time points after 20 weeks of pregnancy, is the most common condition. Pre-eclampsia and eclampsia, though less common, are more serious complications.2 These hypertensive conditions have significant public health consequences and cost the healthcare system over 1 billion dollars for mothers within 12 months of delivery.3
Over the past 15 years, incidence of hypertensive conditions during pregnancy have increased.4,5 Known risk factors such as obesity, nulliparity and history of hypertension explain some of these cases,4–6 but the complex mechanisms causing this increase are largely unknown.7 Environmental contamination, particularly air pollution, is emerging as a contributor towards high blood pressure during pregnancy.8–12 A recent expert review by the National Toxicology Program concludes that components of traffic-related air pollution may be causally linked to gestational hypertension, pre-eclampsia and eclampsia.13 However, few other sources of air pollution have been assessed with respect to maternal hypertensive conditions.
We hypothesized that air-pollution exposures from oil and gas resource extraction may pose risks for hypertensive conditions during pregnancy similarly to traffic-related air pollution. Additional sources of pollution released from the oil and gas industry such as water contamination and increased noise and light pollution may also negatively impact maternal-health conditions.14–17 Environmental monitoring studies show higher concentrations of air pollution and water contamination near oil and gas development sites compared with background levels15,18–21 and a recent pair of biomonitoring studies shows differences in exposures to heavy metals and volatile organic compounds among pregnant women residing in close proximity to gas extraction compared with people living in the general population.22,23 Therefore, we hypothesize that there may be an increased odds of gestational hypertension and eclampsia associated with increasing residential proximity to oil and gas drilling sites.
Globally, estimates indicate that 300 million people across six continents reside on viable oil and gas reservoirs that may be drilled in the future.24 The oil and gas industry has rapidly expanded over the last 20 years, with an estimated 17.6 million Americans now living within 1.6 km (1 mile) of an active oil or gas drilling site.25 Within this industry, there are many potential sources of air pollution including site construction, borehole drilling, hydraulic fracturing, industry traffic and gas flaring.15 Air pollution from oil and gas drilling has some similar components to traffic-related air pollution such as particulate matter [diesel particulate matter (PM), PM10 (particulate matter <10 micrometers)], volatile organic compounds (benzene, toluene, ethylbenzene and xylene) and polycyclic aromatic hydrocarbons (naphthalene, chlorobenzene, phenol).15 These pollutants are expected to be concentrated within 1 km of drilling sites and mostly dissipating to background levels beyond 3 km.25
Whereas oil and gas extraction increases air pollution, this industry may also produce positive community impacts, including increased employment and income, enhanced community resources and reduced oil and gas costs.26–29 New employment prospects may also rapidly shift the socio-demographic composition of a community.30,31 These socio-demographic and economic changes provide an important, but often overlooked, source of confounding that needs to be taken into account to determine the population health impacts of pollution from this industry. Despite extensive community concerns about the public health implications of oil and gas development, the population health implications of this industry are unclear. Residing near oil and gas development has been associated with a number of conditions such as asthma exacerbations,32–34 anxiety or depression,35,36 sleep disturbances37 and adverse birth outcomes.38–47 A pilot study that examined markers of cardiovascular disease observed increased systolic blood pressure for participants who lived closer to drilling sites than those who lived farther away.48 To date, no studies have specifically examined associations between oil and gas development and hypertensive conditions during pregnancy.
Locations of oil and gas drilling sites and who chooses to live near them is not entirely random, so conventional epidemiological approaches may not adequately account for the socio-economic and structural factors that lead to living near an oil and gas site, independently of pollution effects. To overcome this problem, we implement a difference-in-differences analysis to evaluate associations between drilling exposures and hypertensive conditions during pregnancy. This technique allows us to compare before and after drilling changes in hypertension outcome risk to a nearby temporal control group where drilling has not directly occurred49 and to disaggregate the socio-economic impacts of an industrial boom from the simultaneous introduction of new environmental pollution. In this study design, we aim to overcome the confounding that may be induced from changes in maternal stress or anxiety during pregnancy,35,50 variation in healthcare usage51,52 or other external non-environmental factors that may be related to an industrial boom. Using geocoded vital-statistics records from 1996 to 2009 in Texas, the state with the highest oil and gas production during a period of rapid industry growth,53 we conduct a population-based retrospective cohort study in a difference-in-differences analytical framework to assess associations between exposure to oil and gas drilling and hypertensive conditions during pregnancy.
Methods
Data sources
This cohort study evaluates birth-certificate data obtained from the Vital Statistics Program in the Texas Department of State Health Services for the period of 1 January 1996 to 31 December 2009. The restricted-access data contain maternal residential location at delivery geocoded to the full-address level. We received academic access to a propriety database of oil and gas drilling sites from Enverus Drillinginfo.54 This study has been approved by the Institutional Review Boards at Oregon State University (#6692) and the Texas Department of State Health Services (#15–063). We used the Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) reporting guidelines.55
Study population
We acquired birth-certificate data for all births in Texas from 1 January 1996 to 31 December 2009, which contain the residences at delivery geocoded to the full-address level (N = 4 569 428). We exclude non-singleton births (n = 131 880) and remove implausible observations (n = 12 577) based on maternal age (≤10 and ≥65 years old), gestational age (<22 and ≥45 weeks) and birthweight (≤500 and ≥5000 g). In addition, we remove observations with missing continuous covariates (n = 414 816), which is primarily due to the weight-gain-during-pregnancy variable. To reduce potential for community-level confounding, our study population further excluded mothers living outside 10 km of an active or permitted drilling site between 1 January 1985 and 30 June 2019 (n = 1 165 011). Our study population contains mothers who gave birth at 22–44 weeks’ gestation with a reported residence at delivery within 10 km of an active or future drilling site (n = 2 845 144 mothers.)
Exposure assessment
We evaluate exposure to oil and gas extraction via maternal residential proximity at delivery to at least one active drilling site on the date of delivery. All drilling sites with oil or gas as the primary resource with a first date of drilling of between 1 January 1985 and 30 June 2019 were included in our database. Including drilling-site activity prior to our study period that were active during pregnancy allows for better understanding of the full extent of oil and gas extraction in a community, whereas drilling activity after our study period provides a reasonable counterfactual for places where oil and gas extraction will eventually occur but has not started yet. Any drilling site with an end date for its activity prior to the delivery date was excluded from this exposure metric.
A recent review on environmental exposures from oil and gas activity concludes that pollution directly from drilling should dissipate to background levels at 3 km from the drilling site, with the highest concentrations within 1 km.25 To examine potential exposure–response gradients, we split our sample into four distinct zones: 0 to <1, 1 to <2, 2 to <3 and 3–10 km. The 3- to 10-km group represents the sample that is unlikely to be exposed to air pollution from oil and gas drilling, thus the participants in this zone act as the counterfactual in the difference-in-differences framework.
Outcome assessment
Data in birth certificates were used to assign a hypertension condition during pregnancy. This certificate has checkboxes for risk factors during pregnancy including gestational hypertension and eclampsia (yes if indicated, otherwise no). There was no question specific to pre-eclampsia for the study period, thus we were unable to examine this outcome. We treated both outcomes as a binary (reported diagnosis vs no reported diagnosis) in all models.
Statistical analysis
We compared trends in population demographics and socio-economic status before and after drilling began in our near and far groups using means in each subset of our sample. Because our analysis was predicated on drilling-related pollution as the potential cause of hypertension, we then examined trends in maternal hypertensive conditions before drilling began in our near and far groups. We also examined distance gradients in risk by implementing unadjusted local regressions of distance to the nearest active drilling site and our outcomes.
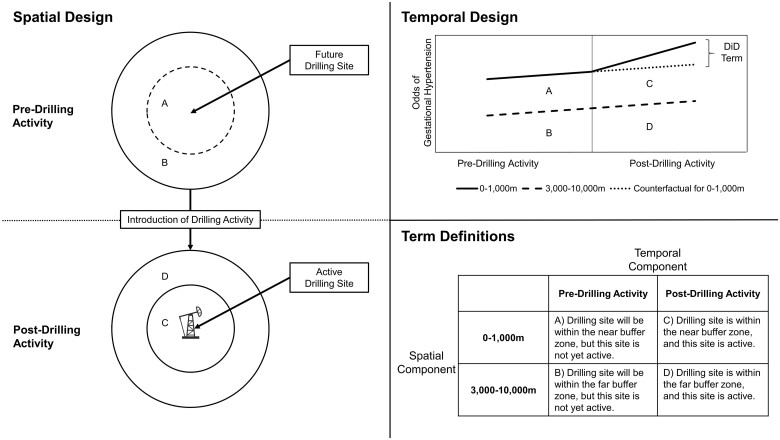
We subsequently implemented logistic-regression models with robust standard errors on our sample using a difference-in-differences framework in which the coefficient of interest was the interaction between an indicator for residential location within a buffer (0–1, 1–2 and 2–3 km) of one or more drilling sites and an indicator for delivery date after drilling began (Figure 1). In this model, we compared pregnant people who reside near drilling before and after drilling begins to a temporal control group in similar communities.49 By leveraging a difference-in-differences design, we were able to parse the impacts of drilling-related pollution on maternal health from secular trends in hypertension treatment that may be changing over time. This study design takes into account unmeasured confounding factors that may influence the magnitude of our associations. Minimally adjusted models are adjusted for birth year (categorical). Fully adjusted models contained a priori selected covariates via literature review that were potential confounders or risk factors: birth year (categorical), infant sex (male, female), gestational age (continuous), maternal age (continuous), maternal race and ethnicity (White non-Hispanic, Black non-Hispanic, Hispanic, other/unknown/missing),56 maternal educational attainment (less than high school, high-school graduate, some college education, bachelor’s degree, postgraduate education, missing), nulliparous (yes, no), prenatal care received (yes, no, missing), smoking during pregnancy (yes, no, missing), maternal weight gain during pregnancy (continuous) and distance to major roads (continuous in metres). We implemented separate models for each buffer zone of the residences. To test the sensitivity of our results, we present several variations on our adjusted model as follows: (i) adding neighbourhood covariates at the census tract level (unemployment percentage, White-population percentage, median household income in US dollars); (ii) adding a month covariate to account for seasonal variability; (iii) removing the covariates related to race, ethnicity and educational attainment to check for confounding by socio-demographic variation; (iv) excluding any records with missing data indicators to examine the role of missing data (e.g. conduct a complete case analysis); and (v) excluding births in 2008–2009 to assess the impact of the Great Recession.
Figure 1.
Conceptual diagram of spatial and temporal components for the difference-in-differences study design to examine the association between residential proximity to oil and gas drilling activity and hypertensive disorders during pregnancy. DiD, difference-in-differences.
Risks of gestational hypertension and eclampsia vary by demographic characteristics, socio-economic conditions and pregnancy attributes.4,7,57 We examined variations in associations by key risk factors in restricted models: maternal age (≤35 years, >35 years), maternal weight gain during pregnancy (<30 lbs, ≥30 lbs), parity (nulliparous, multiparous), maternal race and ethnicity (White non-Hispanic, Black non-Hispanic, Hispanic) and maternal educational attainment (high-school diploma or less, more education than high-school diploma). These cut-off points were selected based on risk factors for both conditions, as well as the study characteristics in this sample. Due to concerns about incorporating an additional interaction term into our difference-in-differences models, we implement restricted models for each subgroup by buffer zone of the residences: 0–1, 1–2 and 2–3 km.
Results
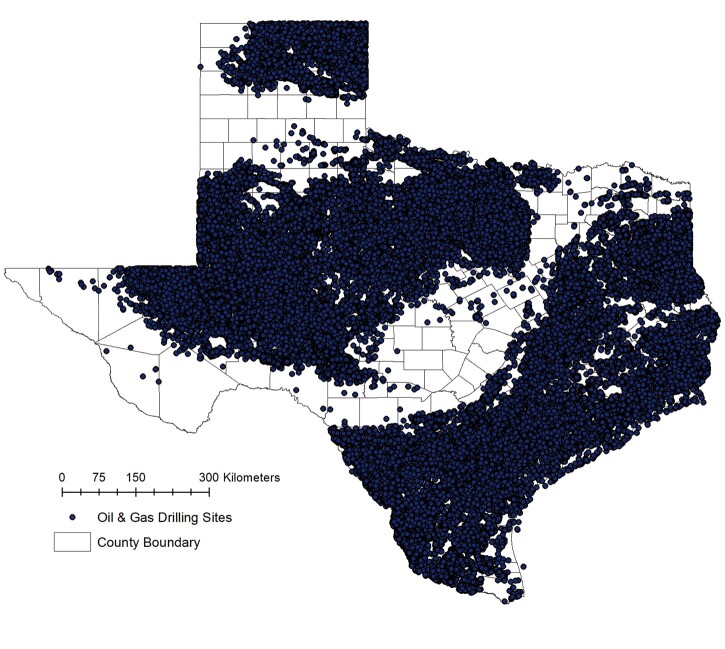
The spatial distributions of drilling activity by resource and type across the state are displayed in Figure 2. After accounting for secular trends using the difference-in-differences framework, descriptive statistics showed that the percentage of women reporting a gestational hypertension diagnosis increases by 0.3% and the percentage of women reporting an eclampsia diagnosis decreases by −0.1% for women residing within 1 km vs women residing 3–10 km from at least one drilling site (Table 1). Maternal characteristics were largely similar in the difference-in-differences terms, except for proportions of Black non-Hispanic women (−7.8%) and Hispanic women (7.9%). Characteristics for the 1- to 2- and 2- to 3-km groups showed similar patterns (Supplementary Tables S1 and S2, available as Supplementary data at IJE online). Gestational hypertension and eclampsia diagnoses over time appear to be similar among our groups, though there is annual variation (Supplementary Figure S1, available as Supplementary data at IJE online).
Figure 2.
Spatial distribution of oil and gas drilling in Texas, 1985–2019. Data displayed include all oil and gas drilling sites spudded in Texas between 1 January 1985 and 30 June 2019.
Table 1.
Demographic information for the Texas birth cohort (1996–2009) for maternal residences <1 and 3–10 km away before and after drilling began
| Characteristic | Near, 0–1 km |
Far, 3–10 km |
Differences between groups |
||||
|---|---|---|---|---|---|---|---|
| Pre-drilling activity | Post-drilling activity | Pre-drilling activity | Post-drilling activity | B–Aa | D–Ca | DiD termb | |
| A | B | C | D | ||||
| Total births | 86 893 | 158 644 | 438 370 | 1 746 922 | — | — | — |
| Gestational hypertension (%) | 4.2 | 4.4 | 4.2 | 4.1 | 0.2 | −0.1 | 0.3 |
| Eclampsia (%) | 0.3 | 0.2 | 0.2 | 0.2 | −0.1 | 0.0 | −0.1 |
| Female sex (%) | 49.1 | 48.9 | 48.9 | 48.9 | −0.2 | 0.0 | −0.2 |
| Gestational age (mean) | 38.7 | 38.6 | 38.7 | 38.6 | −0.1 | −0.1 | 0.0 |
| Maternal age (mean) | 26.1 | 26.0 | 26.2 | 26.1 | −0.1 | −0.1 | 0.0 |
| Maternal race and ethnicity | |||||||
| White non-Hispanic (%) | 46.1 | 47.1 | 35.9 | 35.3 | 1.0 | −0.6 | 1.6 |
| Black non-Hispanic (%) | 14.9 | 9.7 | 9.8 | 12.4 | −5.2 | 2.6 | −7.8 |
| Hispanic (%) | 34.2 | 40.2 | 50.2 | 48.3 | 6.0 | −1.9 | 7.9 |
| Other (%) | 4.7 | 3.0 | 4.3 | 4.1 | −1.7 | −0.2 | −1.5 |
| Maternal educational attainment | |||||||
| Did not complete high school (%) | 35.5 | 28.3 | 34.3 | 31.7 | −7.2 | −2.6 | −4.6 |
| Completed high school (%) | 32.7 | 30.3 | 28.3 | 29.9 | −2.4 | 1.6 | −4.0 |
| Some college (%) | 18.7 | 23.6 | 17.5 | 20.3 | 4.9 | 2.8 | 2.1 |
| Bachelor’s degree (%) | 11.4 | 12.2 | 11.4 | 11.0 | 0.8 | −0.4 | 1.2 |
| Postgraduate (%) | 6.1 | 5.2 | 7.3 | 6.4 | −0.9 | −0.9 | 0.0 |
| Weight gain during pregnancy (lbs) | 30.4 | 31.0 | 29.9 | 30.2 | 0.6 | 0.3 | 0.3 |
| Nulliparous (%) | 41.1 | 40.0 | 41.7 | 40.3 | −1.1 | −1.4 | 0.3 |
| No prenatal care (%) | 1.6 | 2.0 | 1.9 | 2.2 | 0.4 | 0.3 | 0.1 |
| Smoking during pregnancy | 8.4 | 10.3 | 6.6 | 7.6 | 1.9 | 1.0 | 0.9 |
| Neighbourhood characteristicsc | |||||||
| Nearest highway (m)d | 1482 | 1700 | 1247 | 1501 | 218 | 254 | −36 |
| Median household income (USD) | 44 452 | 47 282 | 41 258 | 44 004 | 2830 | 2746 | 84 |
| Unemployment (%) | 4.0 | 6.1 | 5.3 | 6.0 | 2.1 | 0.7 | 1.4 |
| White population (%) | 64.9 | 72.8 | 66.5 | 66.3 | 7.9 | −0.2 | 8.1 |
DiD, difference-in-differences.
A vs B and C vs D columns are the result of the differences for binary and continuous characteristics to compare demographic characteristics before and after drilling began, where categorical covariates are reassigned as dummy indicator variables.
The DiD term is the difference of the near (0–1 km) before and after to the far (3–10 km) groups between near and exposed on the demographic characteristic.
Derived from the US Census at the tract level. Births before 2005 were joined to the 2000 Census data and births in 2005 and after were joined to the 2010 Census data.
Derived from the 2010 Census road file for Texas.
Minimally adjusted and fully adjusted results show largely similar results (Table 2). Our fully adjusted difference-in-differences models for all women in our sample showed an increased odds of reporting gestational hypertension [1.05; 95% confidence interval (CI): 1.00, 1.09) and eclampsia (1.26; 95% CI: 1.05, 1.51) among women who resided within 1 km of at least one active drilling site at delivery compared with other women living within 1 km of a drilling site before active drilling and women living within 3–10 km of a drilling site before or after active drilling. These effects dissipated for gestational hypertension at 1–2 km (0.99; 95% CI: 0.95, 1.04) and 2–3 km (1.00; 95% CI: 0.94, 1.05). Although the point estimates were still elevated at 1–2 km for eclampsia, the association becomes statistically null at 1–2 km (1.10; 95% CI: 0.92, 1.32) and 2–3 km (0.97; 95% CI: 0.78, 1.21).
Table 2.
Difference-in-differences estimates (95% confidence intervals) between maternal residential distances of at least one active drilling site and markers of hypertensive conditions during pregnancy by key risk factors
| Minimally adjusted model | n | Gestational hypertension | Eclampsia |
|---|---|---|---|
| 0–1 km | 2 430 829 | 1.04 (0.99, 1.08) | 1.25 (1.04, 1.49) |
| 1–2 km | 2 429 660 | 0.97 (0.93, 1.02) | 1.16 (0.97, 1.39) |
| 2–3 km | 2 355 239 | 0.98 (0.93, 1.04) | 1.03 (0.83, 1.28) |
|
Fully adjusted model |
n |
Gestational hypertension |
Eclampsia |
| 0–1 km | 2 430 829 | 1.05 (1.00, 1.10) | 1.26 (1.05, 1.51) |
| 1–2 km | 2 429 660 | 0.99 (0.95, 1.04) | 1.10 (0.92, 1.32) |
| 2–3 km | 2 355 239 | 1.00 (0.94, 1.05) | 0.97 (0.78, 1.21) |
Reported coefficient is the interaction term for residence in that distance bin of drilling and after drilling has started. Minimally adjusted model is a logistic regression with adjustment for birth year (categorical for each year from 1996 to 2009). Fully adjusted model is a logistic regression with adjustment for birth year (categorical), infant sex (male, female), gestational age (continuous), maternal age (continuous), maternal race and ethnicity (White non-Hispanic, Black non-Hispanic, Hispanic, other/unknown/missing), maternal educational attainment (less than high school, high-school graduate, some college education, bachelor’s degree, postgraduate education, missing), nulliparous (yes, no), prenatal care received (yes, no, missing), smoking during pregnancy (yes, no, missing), maternal weight gain during pregnancy (continuous) and distance to major roads (continuous in metres). All models include robust standard errors.
We then proceeded to examine restricted models (Table 3). We found elevated odds of gestational hypertension at 1 km in restricted models among women <35 years old at delivery (1.05; 95% CI: 1.00, 1.10), weight gain during pregnancy of >30 lbs (1.08; 95% CI: 1.02, 1.15), nulliparous women (1.13; 95% CI: 1.06, 1.20), White non-Hispanic women (1.27; 95% CI: 1.19, 1.35) and women with more education than a high-school diploma (1.29; 95% CI: 1.20, 1.40) (Table 2.) These effects persisted to 1–2 km for nulliparous women, White non-Hispanic women and women with more education than a high-school diploma. Protective effects out to 2 km were also noted for Hispanic women and women with less than or equivalent to a high-school diploma.
Table 3.
Difference-in-differences estimates (95% confidence intervals) between maternal residential distances of at least one active drilling site and markers of hypertensive conditions during pregnancy by key maternal characteristics
| Maternal characteristic | n | Gestational hypertension | Eclampsia |
|---|---|---|---|
| Maternal age ≤35 years | |||
| 0–1 km | 2 243 504 | 1.05 (1.00, 1.10) | 1.25 (1.04, 1.51) |
| 1–2 km | 2 240 795 | 1.00 (0.95, 1.05) | 1.14 (0.95, 1.38) |
| 2–3 km | 2 172 076 | 0.99 (0.94, 1.05) | 0.96 (0.76, 1.20) |
| Maternal age >35 years | |||
| 0–1 km | 187 325 | 1.01 (0.86, 1.18) | 1.27 (0.65, 2.50) |
| 1–2 km | 188 819 | 0.96 (0.83, 1.12) | 0.67 (0.35, 1.28) |
| 2–3 km | 183 122 | 1.02 (0.84, 1.22) | 1.18 (0.50, 2.80) |
| Weight gain <30 lbs | |||
| 0–1 km | 1 177 727 | 1.00 (0.93, 1.07) | 1.32 (1.01, 1.72) |
| 1–2 km | 1 179 012 | 0.93 (0.87, 1.00) | 0.86 (0.64, 1.14) |
| 2–3 km | 1 145 161 | 0.98 (0.90, 1.06) | 1.03 (0.73, 1.45) |
| Weight gain ≥30 lbs | |||
| 0–1 km | 1 253 102 | 1.08 (1.02, 1.15) | 1.21 (0.95, 1.55) |
| 1–2 km | 1 250 648 | 1.04 (0.98, 1.10) | 1.30 (1.02, 1.64) |
| 2–3 km | 1 210 078 | 1.01 (0.93, 1.08) | 0.93 (0.70, 1.25) |
| Nulliparous | |||
| 0–1 km | 986 253 | 1.13 (1.06, 1.20) | 1.62 (1.28, 2.06) |
| 1–2 km | 985 917 | 1.07 (1.00, 1.14) | 1.45 (1.14, 1.86) |
| 2–3 km | 955 430 | 0.99 (0.92, 1.07) | 0.93 (0.70, 1.23) |
| Multiparous | |||
| 0–1 km | 1 444 576 | 0.95 (0.89, 1.02) | 0.87 (0.65, 1.15) |
| 1–2 km | 1 443 743 | 0.91 (0.85, 0.97) | 0.74 (0.56, 0.98) |
| 2–3 km | 1 399 809 | 1.01 (0.93, 1.10) | 1.03 (0.73, 1.47) |
| White non-Hispanic | |||
| 0–1 km | 888 367 | 1.27 (1.19, 1.35) | 1.18 (0.89, 1.55) |
| 1–2 km | 880 919 | 1.17 (1.10, 1.26) | 1.26 (0.96, 1.67) |
| 2–3 km | 840 026 | 1.08 (0.99, 1.17) | 1.16 (0.81, 1.65) |
| Black non-Hispanic | |||
| 0–1 km | 287 093 | 0.90 (0.80, 1.01) | 1.69 (1.06, 2.68) |
| 1–2 km | 287 801 | 0.86 (0.76, 0.98) | 0.89 (0.61, 1.58) |
| 2–3 km | 278 214 | 0.87 (0.74, 1.03) | 0.80 (0.43, 1.52) |
| Hispanic or Latina | |||
| 0–1 km | 1 156 530 | 0.80 (0.74, 0.87) | 1.13 (0.84, 1.52) |
| 1–2 km | 1 161 190 | 0.79 (0.73, 0.86) | 0.96 (0.72, 1.28) |
| 2–3 km | 1 140 524 | 0.95 (0.86, 1.03) | 0.86 (0.62, 1.18) |
| ≤High school | |||
| 0–1 km | 1 499 065 | 0.92 (0.86, 0.97) | 1.14 (0.92, 1.42) |
| 1–2 km | 1 493 873 | 0.91 (0.85, 0.96) | 1.04 (0.83, 1.30) |
| 2–3 km | 1 451 265 | 0.96 (0.89, 1.04) | 1.04 (0.80, 1.36) |
| >High school | |||
| 0–1 km | 913 573 | 1.29 (1.20, 1.40) | 1.58 (1.13, 2.22) |
| 1–2 km | 917 335 | 1.11 (1.03, 1.20) | 1.21 (0.89, 1.65) |
| 2–3 km | 885 749 | 1.04 (0.96, 1.14) | 0.88 (0.59, 1.31) |
Reported coefficient is the interaction term for residence in that distance bin of drilling and after drilling has started. Model is a logistic regression with adjustment for birth year (categorical), infant sex (male, female), gestational age (continuous), maternal age (continuous), maternal race and ethnicity (White non-Hispanic, Black non-Hispanic, Hispanic, other/unknown/missing), maternal educational attainment (less than high school, high-school graduate, some college education, bachelor’s degree, postgraduate education, missing), nulliparous (yes, no), prenatal care received (yes, no, missing), smoking during pregnancy (yes, no, missing), maternal weight gain during pregnancy (continuous) and distance to major roads (continuous in metres). All models include robust standard errors.
We also observed evidence for elevated odds of eclampsia in restricted models among women <35 years old at delivery (1.25; 95% CI: 1.04, 1.51), nulliparous women (1.62; 95% CI: 1.28, 2.06) and women with more education than a high-school diploma (1.58; 95% CI: 1.13, 2.22) (Table 3). Restricted models for weight gain yielded odds ratios of similar magnitude for <30 lbs of weight gain (1.32; 95% CI: 1.01, 1.72) and >30 lbs of weight gain (1.21; 95% CI: 0.95, 1.55). These effects persisted out to 2 km for nulliparous women and weight gain during pregnancy of >30 lbs.
Sensitivity analyses of these results generally show consistent elevated point estimates, but many of these results contain less statistical precision than the primary adjusted model (Supplementary Table S3, available as Supplementary data at IJE online). The largest attenuation of model estimates occurred when neighbourhood covariates (census tract unemployment percentage, White-population percentage and median household income) were added to the model for gestational hypertension (1.03; 95% CI: 0.98, 1.07) and eclampsia (1.17; 95% CI: 0.97, 1.40). Adding a covariate for birth month yielded similar results to the primary models. Removing socio-demographic variables and observations with missing data from the model did not change model results, respectively. Removing birth years for 2008–2009 (corresponding to the Great Recession) increased model estimates for gestational hypertension (1.08; 95% CI: 1.03, 1.14) and eclampsia (1.34; 95% CI: 1.11, 1.61) among women who resided within 1 km of at least one active drilling site at delivery compared with other women living within 1 km of a drilling site before active drilling.
Discussion
This study represents the first analysis to examine the impacts of oil and gas drilling on hypertension conditions during pregnancy. By applying a difference-in-differences design, we attempted to disaggregate the socio-economic changes associated with an industrial boom from the impacts of residing near drilling-related pollution on maternal health. Specifically, our study found that women who resided within 1 km of at least one active drilling site at delivery had a 5% increased odds of reporting gestational hypertension and a 26% increased odds of reporting eclampsia. Women who were most sensitive to oil and gas drilling exposures were <35 years old, gained >30 lbs during pregnancy, were nulliparous, were non-Hispanic White mothers and had greater than a high-school education. These findings indicate that close residential proximity to oil and gas drilling may pose a substantial hazard for pregnant women.
Our results contribute to the growing body of literature on the population health impacts of the oil and gas extraction industry. Much of the focus to date has been on adverse birth outcomes, including preterm birth, birthweight, small for gestational age, congenital anomalies and infant mortality.38–45 Existing analyses on drilling and infant health generally find elevated risks that persist much further than the 1 km that we see in our risk estimates for pregnancy-related hypertensive conditions. This smaller distance suggests that there may be distinct exposure pathways for drilling-related pollution to influence infant health outcomes compared with maternal hypertension conditions. Components of pollution from oil and gas extraction sites are estimated to dissipate to background levels within 3 km of the extraction location, where the bulk of the dispersion is within 1 km for air pollution25 and 2 km for water contamination.18 This combination of evidence provides additional support for our results indicating that drilling activity is associated with hypertensive conditions during pregnancy.
We observed different socio-demographic characteristics of mothers that substantially altered the risk estimates for residing near at least one active drilling site and pregnancy-related hypertension. Surprisingly, these were opposite to the factors typically observed in environmental injustice cases in which higher exposure and risk are observed among minority and lower socio-economic-status populations.58–61 In our analysis restricted to Hispanic women, we find a protective association between residential proximity to oil and gas drilling and odds of gestational hypertension. This result contrasts with some recent work on drilling-related exposures and population health outcomes.34,45 Existing work has documented that Hispanic women show a decreased odds of a gestational hypertension diagnosis relative to White non-Hispanic women,62 but we do not expect that this difference could explain our results. These protective results may be due to dissimilar residential patterns among Hispanic women living near oil and gas drilling sites or simply residual confounding in our analyses. Considering the severe health consequences of gestational hypertension and eclampsia, future research is necessary to fully understand which subpopulations may be disproportionately burdened by health impacts from exposure to oil and gas drilling.
This study has several strengths worth noting. First, we used a large population-based retrospective birth cohort to obtain our maternal-health information, yielding a sample size (n = 2 845 144) that is much larger than existing work on drilling activity and population health. This feature of our data allows us to examine smaller distances between drilling and residences without forfeiting the power to detect associations. Second, our study setting is Texas, the state with the most oil and gas production in the country,53 and our study period covers multiple oil and gas booms.63 Third, we apply a difference-in-differences analytical framework to our study population.49 This feature of our study design reduces the potential for residual confounding by controlling for temporal trends at the population level. Fourth, we include both oil and gas drilling as well as historical drilling (active wells pre-1996) in our analysis to account for the range of exposures that may occur near a residence. Despite their similar potential for air pollution,64 exposures beyond unconventional gas drilling have rarely been included in health analyses to date.15 This set of strengths in our analysis allows our results to considerably expand on existing literature and provide new data on key concerns for local communities.
Although our study has substantial strengths, there are limitations to consider. First, our study is observational in nature and, as such, we cannot interpret our present findings as a causal relationship. Rather, this analysis contributes to the growing body of evidence which suggests that exposures related to oil and gas drilling are associated with adverse health outcomes. Second, our difference-in-differences framework shows some signs of measured population changes that are occurring dissimilarly among our groups such as the proportion of unemployed people and the proportion of Hispanic mothers. This may be due to unmeasured spatial confounding that we do not assess in this study. Although this implementation is not perfect, the difference-in-differences framework still shows that it reduced confounding by demographic changes and socio-economic status compared with a pre vs post or near vs far study design. Third, we obtained information on hypertensive conditions during pregnancy from birth certificates that are abstracted from the mother’s medical record at delivery. This method of outcome ascertainment likely yields an under-reporting of the true incidence of these conditions, particularly for gestational hypertension.65 We also do not have access to data on pre-eclampsia and it is unclear how those cases may be classified on birth certificates. In this data source, we anticipate that outcome misclassification trends towards under-reporting the diagnoses, which would bias our results towards the null. Fourth, birth-certificate data are unable to provide residential information beyond reported maternal address at delivery. Existing literature estimates that 9–32% of women change residences during pregnancy,66 but the distances moved may not meaningfully impact environmental exposure assessment.67 Fifth, we did not account for external sources of air pollution that could confound our analysis such as industrial emissions. Whereas we account for proximity to major roads, more refined co-exposure metrics would improve this analysis. Sixth, drilling activity and infrastructure are inherently more complicated than the coordinates of site locations. Additional components of this infrastructure include pipelines, compressor stations and retention ponds,25 and other activities that may be occurring at a drilling site include gas flaring, hydraulic fracturing and fluid spills.15 Although these components could produce local pollution that may increase the risks of hypertension, evaluating each of these exposures is beyond the scope of our present analysis. Seventh, we also note that ancillary exposure sources such as diesel-truck traffic and construction activities likely occur prior to the date that drilling began on the site, which may create some exposure misclassification in our analysis. Finally, we cannot rule out the role that residual confounding may be playing in our results, as with all observational research. We overcome some concerns about residual confounding via the difference-in-differences study design, but it is very possible that other sources of confounding could be infiltrating our results. Our restricted analyses by population characteristics are largely exploratory, thus they should be interpreted with caution. With these limitations in mind, our analysis still provides a novel contribution to the existing literature on how the oil and gas industry may affect population health. Additional work is necessary to confirm our findings in other populations, as this analysis is the first one to our knowledge to specifically examine the association between oil and gas development exposures and hypertensive conditions during pregnancy.
Conclusions
Using a population-based retrospective birth cohort with a large sample size, our study provides the first evidence to date that exposure to oil and gas drilling increases the risks of gestational hypertension and eclampsia. These effects are concentrated among maternal residences at delivery within 1 km of at least one drilling site. Given the substantial burden of hypertension conditions on pregnant women, their families and healthcare systems,2 associations between oil and gas drilling and elevated risks of gestational hypertension and eclampsia require more research from the scientific community and careful consideration by policymakers.
Supplementary data
Supplementary data are available at IJE online.
Ethics approval
This research has been approved by the Texas State Department of Health and Human Services (#15-063) and the Oregon State University Institutional Review Board (#6692).
Funding
This work is partially funded by the National Institute of Environmental Health Sciences, National Institutes of Health [Award Number: F31 ES029801], the National Center for Advancing Translational Sciences, National Institutes of Health [Award Number: TL1 TR002371] and Office of the Director, National Institutes of Health [Award Number: DP5 OD021338]. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
Data availability
Data are available by request from the Vital Statistics Unit in the Texas Department of State Health Services.
Supplementary Material
Acknowledgements
We thank Dr Andrew Boslett (University of Rochester) for insightful comments on an earlier version of this manuscript.
Author contributions
M.D.W. conducted the analysis and prepared the first draft of the manuscript. E.L.H. and M.L.K. provided input on the analytical strategy and helped interpret the results. S.C. facilitated access to the health data and helped interpret the results. P.H. supervised the study, provided input on study design and helped interpret the results. All co-authors reviewed and contributed to the writing of the manuscript.
Conflict of interest
None declared.
Contributor Information
Mary D Willis, School of Biological and Population Health Sciences, College of Public Health and Human Sciences, Oregon State University, Corvallis, OR, USA; Department of Epidemiology, School of Public Health, Boston University, Boston, MA, USA.
Elaine L Hill, Department of Public Health Sciences, School of Medicine and Dentistry, University of Rochester, Rochester, NY, USA.
Molly L Kile, School of Biological and Population Health Sciences, College of Public Health and Human Sciences, Oregon State University, Corvallis, OR, USA.
Susan Carozza, School of Biological and Population Health Sciences, College of Public Health and Human Sciences, Oregon State University, Corvallis, OR, USA.
Perry Hystad, School of Biological and Population Health Sciences, College of Public Health and Human Sciences, Oregon State University, Corvallis, OR, USA.
References
- 1. Report of the National High Blood Pressure Education Program Working Group on high blood pressure in pregnancy. Am J Obstet Gynecol 2000;183:s1–22. [PubMed] [Google Scholar]
- 2.American College of Obstetrics and Gynecologists. ACOG Practice Bulletin No. 202: gestational hypertension and preeclampsia. Obstet Gynecol 2019;133:1. [DOI] [PubMed] [Google Scholar]
- 3. Stevens W, Shih T, Incerti D et al. Short-term costs of preeclampsia to the United States health care system. Am J Obstet Gynecol 2017;217:237–48.e16. [DOI] [PubMed] [Google Scholar]
- 4. Fingar KR, Mabry-Hernandez I, Ngo-Metzger Q, Wolff T, Steiner CA, Elixhauser A. Delivery Hospitalizations Involving Preeclampsia and Eclampsia, 2005-2014 Statistical Brief #222. Rockville, MD: Healthcare Cost and Utilization Project (HCUP) Statistical Briefs, 2006. [PubMed]
- 5. Wallis AB, Saftlas AF, Hsia J, Atrash HK. Secular trends in the rates of preeclampsia, eclampsia, and gestational hypertension, United States, 1987–2004. Am J Hypertens 2008;21:521–26. [DOI] [PubMed] [Google Scholar]
- 6. Shen M, Smith GN, Rodger M, White RR, Walker MC, Wen SW. Comparison of risk factors and outcomes of gestational hypertension and pre-eclampsia. PLoS One 2017;12:e0175914. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Brown CM, Garovic VD. Mechanisms and management of hypertension in pregnant women. Curr Hypertens Rep 2011;13:338–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Leaños-Miranda A, Méndez-Aguilar F, Ramírez-Valenzuela KL et al. Circulating angiogenic factors are related to the severity of gestational hypertension and preeclampsia, and their adverse outcomes. Medicine (Baltimore) 2017;96:e6005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Wu J, Wilhelm M, Chung J, Ritz B. Comparing exposure assessment methods for traffic-related air pollution in an adverse pregnancy outcome study. Environ Res 2011;111:685–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Assibey-Mensah V, Glantz JC, Hopke PK et al. Ambient wintertime particulate air pollution and hypertensive disorders of pregnancy in Monroe County, New York. Environ Res 2019;168:25–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Rudra CB, Williams MA, Sheppard L, Koenig JQ, Schiff MA. Ambient carbon monoxide and fine particulate matter in relation to preeclampsia and preterm delivery in Western Washington State. Environ Health Perspect 2011;119:886–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Savitz DA, Elston B, Bobb JF et al. Ambient fine particulate matter, nitrogen dioxide, and hypertensive disorders of pregnancy in New York City. Epidemiology 2015;26:748–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.National Toxicology Program. NTP Monograph on the Systematic Review of Traffic-Related Air Pollution and Hypertensive Disorders of Pregnancy. National Institute of Environmental Health Sciences, National Institutes of Health, Research Triangle Park, NC 2019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. McKenzie LM, Witter RZ, Newman LS, Adgate JL. Human health risk assessment of air emissions from development of unconventional natural gas resources. Sci Total Environ 2012;424:79–87. [DOI] [PubMed] [Google Scholar]
- 15.HEI Energy Research Committee. Human Exposure to Unconventional Oil and Gas Development: A Literature Survey for Research Planning. Health Effects Institute – Energy, 2019. https://hei-energy.org/publication/human-exposure-unconventional-oil-and-gas-development-literature-survey-research (June 2020, date last accessed). [Google Scholar]
- 16. Korfmacher KS, Jones WA, Malone SL, Vinci LF. Public health and high volume hydraulic fracturing. New Solut J Solut 2013;23:13–31. [DOI] [PubMed] [Google Scholar]
- 17. Adgate JL, Goldstein BD, McKenzie LM. Potential public health hazards, exposures and health effects from unconventional natural gas development. Environ Sci Technol 2014;48:8307–20. [DOI] [PubMed] [Google Scholar]
- 18. Hill E, Ma L. Shale gas development and drinking water quality. Am Econ Rev 2017;107:522–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Bonetti P, Leuz C, Michelon G. Large-sample evidence on the impact of unconventional oil and gas development on surface waters. Science 2021;373:896–902. [DOI] [PubMed] [Google Scholar]
- 20. Allen DT. Emissions from oil and gas operations in the United States and their air quality implications. J Air Waste Manag Assoc 2016;66:549–75. [DOI] [PubMed] [Google Scholar]
- 21. Eapi GR, Sabnis MS, Sattler ML. Mobile measurement of methane and hydrogen sulfide at natural gas production site fence lines in the Texas Barnett Shale. J Air Waste Manag Assoc 2014;64:927–44. [DOI] [PubMed] [Google Scholar]
- 22. Caron-Beaudoin É, Valter N, Chevrier J, Ayotte P, Frohlich K, Verner M-A. Gestational exposure to volatile organic compounds (VOCs) in Northeastern British Columbia, Canada: a pilot study. Environ Int 2018;110:131–38. [DOI] [PubMed] [Google Scholar]
- 23. Caron-Beaudoin É, Bouchard M, Wendling G et al. Urinary and hair concentrations of trace metals in pregnant women from Northeastern British Columbia, Canada: a pilot study. J Expo Sci Environ Epidemiol 2019;29:613–23. [DOI] [PubMed] [Google Scholar]
- 24. Measham TG, Fleming DA. Assess benefits and costs of shale energy. Nature 2014;510:473. [DOI] [PubMed] [Google Scholar]
- 25. Czolowski E, Santoro R, Srebotnjak T, Shonkoff S. Toward consistent methodology to quantify populations in proximity to oil and gas development: a national spatial analysis and review. Environ Health Perspect 2017;125:086004–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Brown JP, Fitzgerald T, Weber JG. Does resource ownership matter? Oil and gas royalties and the income effect of extraction. J Assoc Environ Resour Econ 2019;6:1039–64. [Google Scholar]
- 27. Weber JG. The effects of a natural gas boom on employment and income in Colorado, Texas, and Wyoming. Energy Econ 2012;34:1580–88. [Google Scholar]
- 28. Feyrer J, Mansur ET, Sacerdote B. Geographic dispersion of economic shocks: evidence from the fracking revolution. Am Econ Rev 2017;107:1313–34. [Google Scholar]
- 29. Maniloff P, Mastromonaco R. The local employment impacts of fracking: a national study. Resour Energy Econ 2017;49:62–85. [Google Scholar]
- 30. Silva TLS, Morales-Torres S, Castro-Silva S, Figueiredo JL, Silva AMT. An overview on exploration and environmental impact of unconventional gas sources and treatment options for produced water. J Environ Manage 2017;200:511–29. [DOI] [PubMed] [Google Scholar]
- 31. Zwickl K. The demographics of fracking: a spatial analysis for four U.S. states. Ecol Econ 2019;161:202–15. [Google Scholar]
- 32. Rasmussen S, Ogburn E, McCormack M et al. Association between unconventional natural gas development in the Marcellus Shale and asthma exacerbations. JAMA Intern Med 2016;176:1334–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Willis MD, Jusko TA, Halterman JS, Hill EL. Unconventional natural gas development and pediatric asthma hospitalizations in Pennsylvania. Environ Res 2018;166:402–08. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Willis M, Hystad P, Denham A, Hill E. Natural gas development, flaring practices and paediatric asthma hospitalizations in Texas. Int J Epidemiol 2020;49:1883–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Casey JA, Wilcox HC, Hirsch AG, Pollak J, Schwartz BS. Associations of unconventional natural gas development with depression symptoms and disordered sleep in Pennsylvania. Sci Rep 2018;8:11375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Casey JA, Goin DE, Rudolph KE et al. Unconventional natural gas development and adverse birth outcomes in Pennsylvania: the potential mediating role of antenatal anxiety and depression. Environ Res 2019;177:108598. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Boslett A, Hill E, Ma L, Zhang L. Rural light pollution from shale gas development and associated sleep and subjective well-being. Resour Energy Econ. 2021;64:101220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38. Casey JA, Savitz DA, Rasmussen SG et al. Unconventional natural gas development and birth outcomes in Pennsylvania, USA. Epidemiology 2016;27:163–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39. McKenzie LM, Guo R, Witter RZ, Savitz DA, Newman LS, Adgate JL. Birth outcomes and maternal residential proximity to natural gas development in rural Colorado. Environ Health Perspect 2014;122:412–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40. Hill EL. Shale gas development and infant health: evidence from Pennsylvania. J Health Econ 2018;61:134–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Currie J, Greenstone M, Meckel K. Hydraulic fracturing and infant health: new evidence from Pennsylvania. Sci Adv 2017;3:e1603021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Whitworth K, Marshall A, Symanski E. Maternal residential proximity to unconventional gas development and perinatal outcomes among a diverse urban population in Texas. PLoS One 2017;12:e0180966. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43. Gonzalez DJX, Sherris AR, Yang W et al. Oil and gas production and spontaneous preterm birth in the San Joaquin Valley, CA: a case–control study. Environ Epidemiol 2020;4:e099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Tran K, Casey J, Cushing L, Morello-Frosch R. Residential proximity to oil and gas development and birth outcomes in California: a retrospective cohort study of 2006–2015 births. Environ Health Perspect 2020;128:67001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Cushing L, Vavra-Musser K, Chau K, Franklin M, Johnston J. Flaring from unconventional oil and gas development and birth outcomes in the Eagle Ford Shale in South Texas. Environ Health Perspect 2020;128:77003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46. Caron-Beaudoin É, Whitworth KW, Bosson-Rieutort D, Wendling G, Liu S, Verner M-A. Density and proximity to hydraulic fracturing wells and birth outcomes in Northeastern British Columbia, Canada. J Expo Sci Environ Epidemiol 2021;31:53–59. [DOI] [PubMed] [Google Scholar]
- 47. Willis MD, Hill EL, Boslett A, Kile ML, Carozza SE, Hystad P. Associations between residential proximity to oil and gas drilling and term birth weight and small for gestational age infants in Texas: a difference-in-differences analysis. Environ Health Perspect 2021;129:077002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. McKenzie LM, Crooks J, Peel JL et al. Relationships between indicators of cardiovascular disease and intensity of oil and natural gas activity in Northeastern Colorado. Environ Res 2019;170:56–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Abadie A. Semiparametric difference-in-differences estimators. Rev Econ Stud 2005;72:1–19. [Google Scholar]
- 50. Zhang S, Ding Z, Liu H et al. Association between mental stress and gestational hypertension/preeclampsia: a meta-analysis. Obstet Gynecol Surv 2013;68:825–34. [DOI] [PubMed] [Google Scholar]
- 51. Denham A, Willis M, Zavez A, Hill E. Unconventional natural gas development and hospitalizations: evidence from Pennsylvania, United States, 2003-2014. Public Health 2019;168:17–25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Gearhart R, Michieka N. Natural resource abundance and healthcare efficiency in Appalachia: a robust conditional approach. Energy Policy 2019;129:985–996. [Google Scholar]
- 53.U.S. Energy Information Administration. Natural Gas Explained: Where Our Natural Gas Comes From. 2017. (29 November 2021, date last accessed).
- 54.Enverus Drillinginfo. https://www.enverus.com.
- 55. Vandenbroucke JP, von Elm E, Altman DG et al. ; for the STROBE Initiative. Strengthening the Reporting of Observational Studies in Epidemiology (STROBE): explanation and elaboration. PLoS Med 2007;4:e297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Texas Department of State Health Services. Vital Statistics Annual Report, Table 44. 2015. https://www.dshs.texas.gov/chs/vstat/vs08/t44.shtm (17 March 2021, date last accessed).
- 57. Noris M, Perico N, Remuzzi G. Mechanisms of disease: pre-eclampsia. Nat Clin Pract Nephrol 2005;1:98–114. [DOI] [PubMed] [Google Scholar]
- 58.Department of Energy. What Is Environmental Justice? 2016. https://www.energy.gov/lm/services/environmental-justice/what-environmental-justice (29 June 2018, date last accessed).
- 59. Lee C. Environmental justice: building a unified vision of health and the environment. Environ Health Perspect 2002;110:141–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Clark LP, Millet DB, Marshall JD. National patterns in environmental injustice and inequality: outdoor NO2 air pollution in the United States. PLoS One 2014;9:e94431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61. Johnston JE, Werder E, Sebastian D. Wastewater disposal wells, fracking, and environmental injustice in Southern Texas. Am J Public Health 2016;106:550–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62. Ghosh G, Grewal J, Männistö T et al. Racial/ethnic differences in pregnancy-related hypertensive disease in nulliparous women. Ethn Dis 2014;24:283–89. [PMC free article] [PubMed] [Google Scholar]
- 63. Rahm D. Regulating hydraulic fracturing in shale gas plays: the case of Texas. Energy Policy 2011;39:2974–81. [Google Scholar]
- 64.U.S. Department of Energy. Modern Shale Gas Development in the United States: A Primer. 2009. https://energy.gov/fe/downloads/modern-shale-gas-development-united-states-primer (19 January 2018, date last accessed).
- 65. Roberts CL, Bell JC, Ford JB, Hadfield RM, Algert CS, Morris JM. The accuracy of reporting of the hypertensive disorders of pregnancy in population health data. Hypertens Pregnancy 2008;27:285–97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66. Bell ML, Belanger K. Review of research on residential mobility during pregnancy: consequences for assessment of prenatal environmental exposures. J Expo Sci Environ Epidemiol 2012;22:429–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67. Lupo P, Symanski E, Chan W et al. Differences in exposure assignment between conception and delivery: the impact of maternal mobility. Paediatr Perinat Epidemiol 2010;24:200–08. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
Data are available by request from the Vital Statistics Unit in the Texas Department of State Health Services.