Abstract
There is evidence that the more frequent, severe, and chronic posttraumatic stress disorder (PTSD) symptomatology experienced by Black compared to White individuals cannot be explained by disparities in socioeconomic status or trauma exposure. One factor that may be important to consider is racial discrimination, which is associated with numerous negative mental health outcomes yet has not been studied in the context of interpersonal traumas for Black women. This study aims to fill this gap by examining the independent and interactive roles of racial discrimination and interpersonal trauma in predicting PTSD symptoms in a community sample of trauma-exposed, Black women (n = 292). Consistent with the previous literature, we found that more frequent experiences of racial discrimination were associated with more severe PTSD symptoms overall (r = .34) and by symptom cluster. Furthermore, we found a significant interaction between experiences of racial discrimination and experiences of interpersonal trauma (b = .46, 95%CI[.04, .88], SE = .28; ΔR2 = .01, p = .03) such that the association between PTSD symptoms and interpersonal trauma was stronger at higher (+1 SD above the mean) levels of racial discrimination. This pattern was replicated for most PTSD symptom clusters. These results suggest that racial discrimination experiences exacerbate the association between interpersonal traumatic experiences and PTSD symptoms among Black women.
Keywords: racial discrimination, interpersonal trauma, posttraumatic stress, moderation, Black women
Growing evidence that Black Americans experience more frequent, severe, and chronic posttraumatic stress disorder (PTSD) symptomatology compared to Whites (Himle et al., 2009; Roberts et al., 2011; Sibrava et al., 2019) has led to the identification of potential culprits of this inequity (e.g., socioeconomic status, disparities in trauma exposure). Although low-income Black individuals have high lifetime rates of PTSD and are exposed to relatively more traumatic events, these racial disparities persist even when controlling for trauma exposure and socioeconomic status (Alim et al., 2006; Davis et al., 2008; Goldmann et al., 2011). One possibility is that factors specific to the Black American experience in the U.S., such as racial discrimination, may be at play (Brooks et al., 2018; Pieterse et al., 2010; Williams et al., 2018).
Racial discrimination, defined as experiences of injustice perpetrated on the basis of race (Williams et al., 2003), is experienced by Black individuals across gender, age, and socioeconomic status (Lewis et al., 2012; Mays et al., 2007). Racial discrimination has been theorized to set in motion a process of negative emotional states that influence both cognitive and biological heightened stress responses that, in turn, contribute to an individual’s increased vulnerability to developing mental health difficulties (Williams et al., 2003). For example, racial discrimination has consistently been shown to have detrimental effects on a multitude of mental health outcomes for Black Americans, including depression, anxiety, and substance abuse (Pascoe & Smart Richman, 2009; Williams & Mohammed, 2009). Particularly relevant to PTSD symptoms, frequent experiences of racial discrimination may be particularly harmful because racial discrimination exposure is often chronic, unpredictable, and occurs in myriad settings. This conceptualization aligns with the prolonged activation of stress model (Utsey et al., 2000; 2012) which indicates that the chronic physiological and cognitive appraisal of stress from racial discrimination over an extended time, above and beyond the timing of the actual stressor, significantly influences the mental health disparities seen in Black populations.
A small but growing body of literature has explored the association between racial discrimination and PTSD in Black individuals (Brooks et al., 2018; Carter & Forsyth, 2010; Kirkinis et al., 2018; Sibrava et al., 2019). In a study examining racial discrimination and PTSD symptoms in a representative sample of racially or ethnically marginalized groups, Black Americans reported higher rates of racial discrimination than Asian American and Latinx American groups and were more likely to endorse experiencing lifetime PTSD than Asian Americans (Chou et al., 2012). Specifically focusing on Black populations, Brooks and colleagues (2018) found that racial discrimination was significantly associated with PTSD symptoms in a community sample of low-income Black adults even after controlling for psychological distress, perceived safety, and neighborhood crime. Recently, Sibrava et al. (2019) examined the influence of racial discrimination on the clinical course of PTSD in a longitudinal clinical sample of Black and Latinx American adults and found that, over five years, racial discrimination significantly predicted PTSD diagnostic status. Thus, there is evidence that more frequent experiences of racial discrimination are associated with worse PTSD symptomology.
Within the racial discrimination literature, researchers have theorized about how to interpret experiences of racial discrimination within the conceptualization of trauma and trauma-related symptoms (Carter, 2007). The term “race-based traumatic stress” was driven by these theoretical considerations and formulates that exposure to racial discrimination produces race-based traumatic stress reactions (i.e., hyperarousal, intrusion or re-experiencing, avoidance or numbing, and negative self-concept) that coincide with symptoms of PTSD (Carter, 2007; Kirkinis et al., 2018; Williams et al., 2018). In support of this conceptualization, Carter and Forsyth (2010) found that racially marginalized adults who reported direct and interpersonal experiences of racial discrimination reported higher levels of race-related anxiety, guilt/shame, avoidance, and hypervigilance compared to individuals who did not. Thus, there is evidence that the experience of racial discrimination can function as a traumatic stressor, as evidenced by similar subsequent symptom pattern responses.
Although there is sufficient evidence that Black Americans experience disproportionately high PTSD symptoms and that racial discrimination is associated with general and race-specific PTSD symptoms, there are noteworthy gaps in the research literature that warrant further investigation. First, most research exclusively examines either race-based or non-race-based stressors, precluding the contextual consideration that marginalized communities often experience both the stress of racial discrimination and non-race-based trauma exposure throughout their life and that these potentially interconnected experiences may impact the course of PTSD development. This bifurcation precludes the development of an integrated understanding of how race-based and non-race-based experiences may interact to predict PTSD symptoms. Second, when studying the etiology and development of PTSD and trauma symptomatology, studies often do not consider the place that racial discrimination and interpersonal trauma experiences hold in social power structures in our society. Consistent with the theory of intersectionality (Cho et al., 2013; Cole, 2009; Crenshaw, 1989), Black women are at risk for double oppression through experiences of gender-based violence/interpersonal violence and racial discrimination. Thus, examining the intersection of these experiences is needed to gain further insight into the ways in which multiple forms of oppression may lead to poor outcomes (Hampton et al., 2003; Watson et al., 2016). Doing so may expand our understanding of the multifaceted experiences of Black women who may have experienced racial discrimination as well as chronic interpersonal trauma exposure in their lifetime. Finally, the generalizability of previous work is concerning, given that much of it has been conducted among college students, despite stronger associations existing in populations more likely to be chronically exposed to trauma and who may not actively seek clinical treatment (e.g., low-income and urban populations; Alim et al., 2006; Norris & Slone, 2007).
The Current Study
The current study addresses limitations in the literature in three important ways. First, very limited research has examined the role of racial discrimination in experiences of trauma symptomatology. The current study will examine the degree to which racial discrimination is associated with PTSD symptoms. Second, there is a gap in the literature specifically considering intersectionality frameworks and examining interlocking systems of oppression in marginalized communities (i.e., sexism and racism). Therefore, the current study will address this gap by examining the degree to which racial discrimination influences the association between interpersonal trauma exposure and PTSD symptoms. Finally, given that the effects of racial discrimination have been mostly studied among college students, this study extends the generalizability of these findings by examining a community sample of low-income, urban, Black women. We had two main hypotheses: (a) consistent with previous literature, we predicted that experiences of racial discrimination and interpersonal violence will be positively associated with PTSD symptom severity, and (b) experiences of racial discrimination will moderate the association between experiences of interpersonal violence and overall PTSD symptom severity, whereby this relationship will be strongest among individuals who report more frequent experiences of racial discrimination. Given the limited research on the interaction between racial discrimination and interpersonal violence to predict PTSD symptoms, we did not make specific predictions about differential moderating effects for the symptom clusters. We thus consider these analyses to be exploratory.
Method
Procedure
Participants were drawn from an ongoing study of PTSD risk factors in a low-income, primarily Black, urban population. Only those participants who completed key measures (i.e., racial discrimination, PTSD assessment) were included in our analyses. Participants were Black women recruited from waiting rooms in a publicly funded hospital in the South. All participants were approached at random. Eligible participants were required to be at least 18 years old, not actively psychotic, and able to give informed consent. If eligible and willing to participate, individuals signed informed consent. An initial 30-to-75 minute interview was then administered by trained research assistants in private areas using questionnaires about trauma history, general demographic information, and other psychological factors. All participants were compensated $15 for their time. Select participants were recruited to complete a follow-up clinical interview by trained graduate and post-graduate level trainees as part of other ongoing research studies. Follow-up interviews averaged 2 to 3 hours to complete and participants were compensated an additional $60 for their time. Only participants with complete data on all study variables were included in these analyses. All study procedures were approved by the university and hospital ethical review boards.
Participants
The analytic sample consisted of 292 women, aged 18 to 65 (M = 40.90, SD = 11.91), who self-identified as Black or African American. The majority of participants were single/never married (55.5%), unemployed (61.6%), not supported by disability (79.1%), and had a household monthly income of $1,999 or less (78.4%). Regarding education level, 19.9% of participants had completed less than 12th grade, 32.9% completed high school or equivalent, 26.0% had some college or technical school, 17.8% graduate from college or technical school, and 3.4% completed graduate school.Approximately 92.1% of participants reported experiencing at least one type of interpersonal trauma (e.g., experiencing violence, witnessing violence, experiencing sexual assault) and 66.4% of participants reported experiencing at least one type of racial discrimination.
Measures
Demographics.
General demographic information was collected, which included sex, race/ethnicity, relationship status, education level, employment status, and household income.
Experiences of Discrimination (EOD; Krieger et al., 2005).
The EOD is a psychometrically validated measure of experiences of discrimination originally developed in the context of a large, public health study that utilized a racially diverse community sample of adults. Participants were first asked, “Have you ever experienced discrimination, been prevented from doing something, or been hassled or made to feel inferior in any of the following situations because of your race, ethnicity, or color?” and then instructed to respond regarding nine different situations (e.g., school, work) using a scale of 0 (never) or 1 (happened at least once). Scores were summed to create a total score.
Clinician-Administered PTSD Scale (CAPS-5; Weathers et al., 2013).
The CAPS-5 is an interviewer-administered diagnostic instrument for current PTSD based on criteria from the DSM-5. The CAPS-5 includes items that rate social and occupational functioning, global PTSD symptom severity, and the validity of the participant’s responses. Interrater reliability in this sample has been previously reported and has shown good reliability for current diagnosis of PTSD (k=0.83; Powers et al., 2017). In these analyses, we used the severity ratings for each criterion.
Traumatic Events Inventory (TEI; Gillespie et al., 2009).
The TEI is a 19-item screening measure that examines the presence vs. absence of different types of trauma exposure and frequency of trauma occurrence. For the current study, we focused on endorsement of 13 events that represent a variety of interpersonal traumas, such as witnessing the murder of a close family member/friend, being attacked with or without a weapon by a spouse/romantic partner or stranger, witnessing a close family member/friend being attacked with or without a weapon, and experiencing a sexual assault.
Data Analytic Plan
We first conducted preliminary analyses to determine basic descriptive data and examine the correlations among the main study variables: interpersonal trauma experiences, racial discrimination, and PTSD. For our moderation analyses, we used the PROCESS SPSS Macro (Hayes et al., 2017) which utilized ordinary least squares regression to determine whether the association between interpersonal trauma experiences and PTSD symptoms is contingent on experiences of racial discrimination. We ran five models predicting the following outcomes for symptom severity: PTSD overall, re-experiencing, avoidance, negative alterations in mood and cognition, and arousal. Based on a sample size of 290, an effect size of .20 and two predictors, a priori power analyses indicated we had sufficient statistical power (.80) to reject an incorrect null hypothesis (Faul, Erdfelder, Lang, & Buchner, 2007). We used a bootstrapping methodology which increases power by not relying on distributional assumptions (Hayes et al., 2017). More specifically, bootstrapping was completed with 10,000 random samples to determine the 95% confidence intervals for each effect. Confidence interval values that did not contain “0” were interpreted to indicate statistical significance for each effect. To probe statistically significant interaction effects, we first examined the ΔR2 value and then calculated the conditional effects at different levels of the moderator (−1 SD, mean, +1 SD).
Results
Preliminary Analyses
A summary of the means, standard deviations, ranges, and intercorrelations among main study variables is depicted in Table 1. Higher frequency of interpersonal traumas was associated with greater PTSD symptom severity overall (r = .37, p < .01) as well as with all symptom clusters (r’s = .28 to .36; p’s < .01). Similarly, higher endorsement of racial discrimination experiences was associated with greater PTSD symptom severity overall (r = .34, p < .01) as well as with symptom clusters (r’s = .25 to .32; p’s < .01). We found a small association between traumatic experiences and racial discrimination (r = .13, p < .01). We compared the magnitude of the correlations for interpersonal traumas and racial discrimination predicting PTSD using Lee and Preacher’s (2013) z-score formula and found no significant differences for overall PTSD and symptom clusters. This suggests that the magnitude of associations between interpersonal trauma and PTSD symptoms did not differ from the magnitude of associations between racial discrimination and PTSD symptoms.
Table 1.
Means, standard deviations, and correlations among main study variables
| Range | M | SD | 1 | 2 | 3 | 4 | 5 | 6 | |
|---|---|---|---|---|---|---|---|---|---|
|
|
|||||||||
| 1. Traumatic Experiences | 0–8 | 2.35 | 1.47 | - | |||||
| 2. Racial Discrimination | 0–9 | 2.41 | 2.44 | .13* | |||||
| 3. PTSD Overall Severity | 0–62 | 18.22 | 13.13 | .37* | .34* | - | |||
| 4. Re-Experiencing (B) Symptoms | 0–17 | 4.14 | 3.91 | .31* | .32* | .87* | - | ||
| 5. Avoidance (C) Symptoms | 0–8 | 2.38 | 1.96 | .28* | .25* | .81* | .72* | - | |
| 6. Mood/Cognition (D) Symptoms | 0–24 | 6.42 | 5.27 | .36* | .30* | .91* | .68* | .67* | - |
| 7. Arousal (E) Symptoms | 0–17 | 5.73 | 3.93 | .32* | .32* | .88* | .68* | .64* | .73* |
Note. The maximum severity scores for the CAPS-5 are as follows: overall = 80, B = 20, C = 8, D = 28, E = 24
Moderation Analyses
PTSD overall severity.
The first moderation analysis tested the main and interactive effects of interpersonal trauma and racial discrimination on overall PTSD symptom severity (see Table 2 and Figure 1). The model accounted for 23.5% of the variance in PTSD symptom severity, F(3, 288) = 29.34, MSE = 133.51, p <.01. As expected, interpersonal trauma (b = 3.18, 95%CI[2.24, 4.12], SE = .48), racial discrimination (b = 1.57, 95%CI[1.01, 2.12], SE = .28) and their interaction (b = .46, 95%CI[.04, .88], SE = .28; ΔR2 = .01, p = .03) predicted PTSD symptom severity. Follow-up analyses examining conditional effects at different levels of the moderator (racial discrimination) revealed the association between interpersonal trauma was strongest at +1 SD above the mean of racial discrimination (θx→y = 4.31, 95%CI [2.78, 5.85]), though the effect was still significant at the mean (θx→y = 3.18, 95%CI [2.24, 4.12]) and −1 SD below the mean (θx→y = 2.07, 95%CI [.85, 3.29]). This suggests that the association between interpersonal trauma and PTSD symptoms was stronger at relatively higher levels of racial discrimination.
Table 2.
Summary of regression results and conditional effects at different levels of the moderator
| b | 95% CI | SE | t | p | Conditional Effects Based on RD | ||||
|---|---|---|---|---|---|---|---|---|---|
| PTSD Overall Symptom Severity | RD | Effect | 95% CI | p | |||||
|
| |||||||||
| Traumatic Experiences | 3.18 | [2.24, 4.12] | .68 | 6.65 | <.01 | − 1 SD | 2.07 | [.85, 3.29] | <.01 |
| Racial Discrimination | 1.57 | [1.01, 2.12] | .28 | 5.59 | <.01 | Mean | 3.18 | [2.24, 4.12] | <.01 |
| RD x TE | .46 | [.04, .88] | .21 | 2.16 | .03 | +1 SD | 4.31 | [2.78, 5.85] | <.01 |
|
| |||||||||
| Re-Experiencing Symptoms | RD | Effect | 95% CI | p | |||||
|
| |||||||||
| Traumatic Experiences | .80 | [.51, 1.08] | .15 | 5.43 | <.01 | − 1 SD | .44 | [.06, .81] | .02 |
| Racial Discrimination | .45 | [.28, .62] | .09 | 5.26 | <.01 | Mean | .80 | [.51, 1.08] | <.01 |
| RD x TE | .15 | [.02, .28] | .07 | 2.28 | .02 | +1 SD | 1.16 | [.69, 1.63] | <.01 |
|
| |||||||||
| Avoidance Symptoms | |||||||||
|
| |||||||||
| Traumatic Experiences | .35 | [.20, .50] | .08 | 4.61 | <.01 | ||||
| Racial Discrimination | .17 | [.08, .26] | .05 | 3.82 | <.01 | ||||
| RD x TE | .03 | [−.04, .10] | .03 | .84 | .40 | ||||
|
| |||||||||
| Mood/Cognition Symptoms | RD | Effect | 95% CI | p | |||||
|
| |||||||||
| Traumatic Experiences | 1.24 | [.86, 1.63] | .20 | 6.35 | <.01 | − 1 SD | .88 | [.38, 1.38] | <.01 |
| Racial Discrimination | .55 | [.32, .77] | .12 | 4.77 | <.01 | Mean | 1.24 | [.86, 1.63] | <.01 |
| RD x TE | .15 | [−.02, .32] | .09 | 1.72 | .09 | +1 SD | 1.61 | [.98, 2.24] | <.01 |
|
| |||||||||
| Arousal Symptoms | RD | Effect | 95% CI | p | |||||
|
| |||||||||
| Traumatic Experiences | .83 | [.54, 1.12] | .15 | 5.66 | <.01 | − 1 SD | .49 | [.11, .86] | .01 |
| Racial Discrimination | .45 | [.28, .61] | .09 | 5.18 | <.01 | Mean | .83 | [.54, 1.12] | <.01 |
| RD x TE | .14 | [.01, .27] | .07 | 2.18 | .03 | +1 SD | 1.18 | [.71, 1.65] | <.01 |
Note. RD = Racial Discrimination; TE = Traumatic Experiences; Racial discrimination and traumatic experiences were mean-centered prior to analysis.
Figure 1.
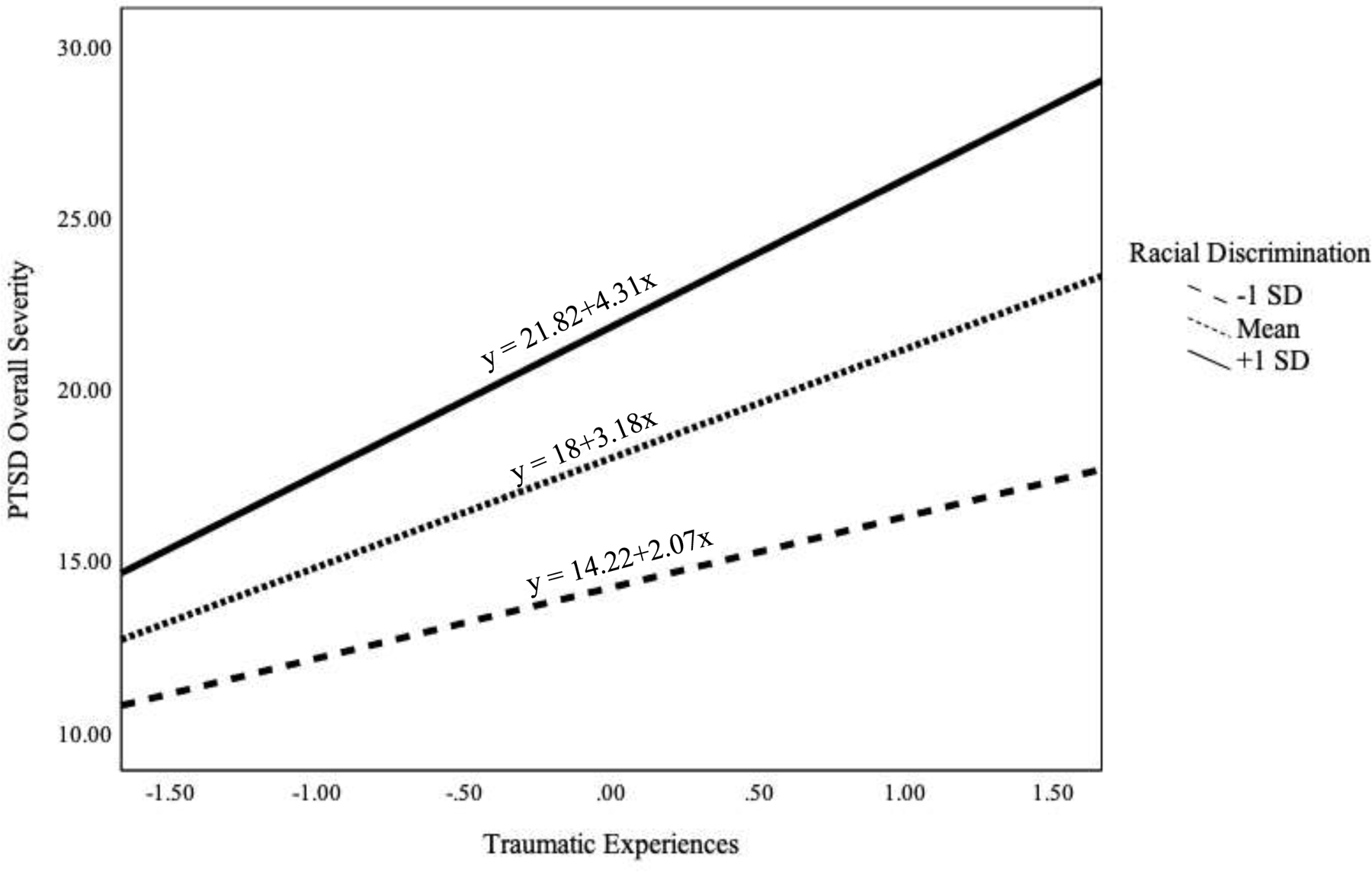
A visual representation of the conditional effects of traumatic experiences on PTSD symptom severity among those at low (-SD), mean, and high (+1 SD) levels of exposure to racial discrimination.
Re-experiencing symptom severity.
The second moderation analysis tested the main and interactive effects of interpersonal trauma and racial discrimination on re-experiencing symptoms. The model accounted for 19% of the variance in symptom severity, F(3, 288) = 22.52, MSE = 12.54, p <.01. Consistent with the overall symptom results, interpersonal trauma (b = .80, 95%CI[.51, 1.08], SE = .15), racial discrimination (b = .46, 95%CI[.28, .62], SE = .09) and their interaction (b = .15, 95%CI[.02, .28], SE = .07; ΔR2 = .02, p = .02) predicted severity of re-experiencing symptoms. Follow-up analyses examining the conditional effects revealed the association between interpersonal trauma and re-experiencing symptoms was strongest at +1 SD above the mean of racial discrimination (θx→y = 1.16, 95%CI [.69, 1.63]), though the effect was still significant at the mean (θx→y = .80, 95%CI [.51, 1.08]) and −1 SD below the mean (θx→y = .44, 95%CI [.06, .81]). This suggests that the association between interpersonal trauma and re-experiencing symptoms was strongest at relatively higher levels of racial discrimination.
Avoidance symptom severity.
The third moderation analysis tested the main and interactive effects of interpersonal trauma and racial discrimination on avoidance symptoms. The model accounted for 12.6% of the variance in symptom severity, F(3, 288) = 13.8, MSE = 3.40, p <.01. Interpersonal trauma (b = .35, 95%CI [.20, .50], SE = .08) and racial discrimination (b = .17, 95%CI [08, .26], SE = .05) predicted severity of symptoms, but their interaction did not reach statistical significance (ΔR2 = .00, p = .40). These results suggest that although both interpersonal trauma and racial discrimination predicted worse avoidance symptoms, the effect of interpersonal trauma was not conditional on the level of racial discrimination.
Mood and cognition symptom severity.
The fourth moderation analysis tested the main and interactive effects of interpersonal trauma and racial discrimination on negative alterations in mood and cognition symptoms. The model accounted for 20.2% of the variance in symptom severity, F(3, 288) = 22.36, MSE = 24.33, p <.01. Both trauma (b = 1.24, 95%CI[.86, 1.63], SE = .20) and racial discrimination (b = .55, 95%CI[.32, .77], SE = .12) predicted symptom severity. Although the trauma by discrimination interaction did not quite reach statistical significance (ΔR2 = .01; p = .09), we nevertheless completed follow-up analyses given our a priori hypotheses. Those analyses revealed that the association between traumatic experiences and mood and cognition symptoms was strongest at +1 SD above the mean of racial discrimination (θx→y = 1.61, 95%CI [.98, 2.24]), though the effect was significant at the mean (θx→y = 1.24, 95%CI [.86, 1.63]) and −1 SD below the mean (θx→y = .88, 95%CI [.11, 86]). This suggests that the association between interpersonal trauma and mood and cognition symptom severity was somewhat stronger at relatively higher levels of racial discrimination.
Arousal symptom severity.
Finally, the model for the fifth moderation analysis predicting arousal symptoms accounted for 19.4% of the variance in arousal symptom severity, F(3, 288) = 23.07, MSE = 12.55, p <.01. Trauma (b = .83, 95%CI[.54, 1.12], SE = .15), racial discrimination (b = .45, 95%CI[.28, .61], SE = .09) and their interaction (b = .14, 95%CI[.01, .27], SE = .07; ΔR2 = .01, p = .03) predicted severity of arousal symptoms. Consistent with the previously-noted pattern, follow-up analyses on the conditional effects revealed the association between trauma and arousal symptoms was strongest at +1 SD above the mean of racial discrimination (θx→y = 1.18, 95%CI [.71, 1.65]), though the effect was still significant at the mean (θx→y = .83, 95%CI [.54, 1.12]) and −1 SD below the mean (θx→y = .49 95%CI [.11, .86]). This suggests that the association between interpersonal trauma and arousal symptoms was stronger at relatively higher levels of racial discrimination.
Moderation analysis summary.
Our results suggested that the magnitude of the association between traumatic experiences and overall PTSD symptom severity, as well as re-experiencing and arousal symptoms, was contingent on exposure to racial discrimination; such that the association was considerably stronger among participants who experienced relatively greater exposure to different types of racial discrimination. This pattern was also observed for the mood and cognition symptoms, but the interaction effect did not reach statistical significance. For completeness, we also ran these analyses with SES as a moderator and found that this inclusion did not alter the significance of the results.
Discussion
Little is known about the interplay of interpersonal trauma and racial discrimination’s effects on PTSD symptoms in Black women because research examining the effects of interpersonal trauma typically fails to incorporate race-specific stressors and research on race-specific stressors typically excludes non-race-based stressors. Our findings contribute to the growing body of literature on race and non-race based stressors in Black women by a) replicating the finding that interpersonal trauma and racial discrimination account for unique variance in PTSD symptoms, and b) identifying the exacerbating effect of racial discrimination on the association between interpersonal trauma and PTSD symptoms. The moderating effect of racial discrimination, though present for overall, re-experiencing, and arousal symptoms, was not statistically significant for symptoms related to avoidance or negative alterations in mood and cognition. This pattern of results is generally in line with the prolonged activation of stress model (Utsey et al., 2012).
Prolonged activation of the stress response, which has been theorized to explain why racial discrimination is associated with negative mental health outcomes (Utsey et al., 2012), may also explain why racial discrimination may worsen the association between interpersonal trauma and PTSD symptoms. One component of this model, perseverative cognition, refers to repetitive and negative past-oriented thoughts. Indeed, there is evidence that experiencing both interpersonal traumas and racial discrimination are associated with more frequent perseverative cognition (Borders & Liang, 2011; Hatzenbuehler et al., 2009; Kubota & Nixon, 2017). Given that perseverative cognition is conceptualized as a maladaptive coping response to stressors that are particularly uncontrollable or unpredictable, it is possible that the ubiquity of racial discrimination, the diversity of contexts in which it can occur (e.g., work, eating at a restaurant), and its range of ambiguity (e.g., ranging from subtle racial microaggressions to blatant racism) make it particularly conducive to repetitive, intrusive thoughts.
In addition to prolonging the activation of the stress response through the repeated cueing of previous experiences, racial discrimination may also prolong the stress response through the activation of future threat-oriented thoughts. Indeed, another component of the prolonged activation of stress response model for Black Americans is the notion of race-related anticipatory stress, which refers to the psychological (e.g., worry) and physiological (e.g., bodily alarm response) state of hypervigilance regarding experiences of injustice and racism (Lewis et al., 2015; Utsey et al., 2000). Similar to the theorized function of hypervigilance in relation to non-raced based trauma, race-related anticipatory anxiety may function as a way to cope with the uncertainty of possible race-related threat. Particularly for participants in our sample – who, in addition to racism, likely experience sexism and classism – this hypervigilance may be reinforced by legitimate concerns regarding safety. Although a police encounter while driving, for example, could be threatening for all individuals, low-income Black women must contend with concern for additional threat beyond legal repercussions (e.g., sexual assault, use of a lethal firearm; Smith & Alpert, 2007). For individuals who experience both interpersonal trauma and racial discrimination, this adaptive concern for safety may escalate to maladaptive states of sustained, heightened physiological arousal (Lewis et al., 2015).
The final component of Utsey et al.’s (2012) adapted model refers to secondary appraisal or beliefs about one’s ability to cope with stressors. Relevant to symptoms of negative mood and cognition, narratives regarding experiences of interpersonal trauma (e.g., rape myths) may be internalized in such a way that increases women’s likelihood of blaming themselves for sexual assault or abuse (Suarez & Gadalla, 2010). Similarly, those who have experienced racial discrimination may also internalize negative societal beliefs and stereotypes about the causes of traumatic experiences, which may have implications for persistent states of negative affect. Further, these stressors may be compounded by experiences that occur at the intersection of racism and sexism, referred to as gendered racism (Lewis & Neville, 2015), such as being confronted with racism related to the endorsement of stereotypes about Black women in particular (e.g., Jezebel stereotype). Thus, the moderation may have been smaller for negative mood and cognition symptoms because it only captured additive effects of interpersonal trauma and racial discrimination, rather than experiences of gendered racism.
Both interpersonal traumas and racial discrimination predicted avoidance symptom severity, however, the interaction between these variables was not statistically significant. It is possible that internalization of the Strong Black Woman schema (e.g., coping styles that involve avoiding expression and experience of negative emotions in favor of unyielding strength; Watson & Hunter, 2015) is already heightened for women who have experienced interpersonal trauma, and that racial discrimination, therefore, does not necessarily worsen this effect. The ubiquity of racist experiences may also be an important consideration, such that it precludes the possibility of successful avoidance. Thus, the unfeasibility of avoidance related to racial discrimination may explain why racial discrimination may not worsen the association between interpersonal trauma and avoidance symptoms.
Clinical Implications
The results from our study have implications for understanding the impact of racial discrimination on PTSD symptomatology in marginalized groups. Specifically, this study provides evidence that racial discrimination and interpersonal trauma are similarly associated with and interact to predict PTSD symptom severity even when the effect of socioeconomic status is considered, which has implications for providing psychotherapy to trauma-exposed Black women. By identifying and processing experiences with racial discrimination, clinicians can provide treatment to decrease self-blame, perseveration, and negative cognitive schemas while providing trauma-informed psychotherapy (Carter, 2007; Carter et al., 2017). For example, it may be important to challenge notions of distorted self-blame regarding sexual assault, while also identifying and validating the role of social narratives that may reinforce the internalizations of such belief (e.g., stereotypes about sexual promiscuity of Black women). Similarly, it may be important to reduce hypervigilance by examining potential distortions in the estimation of threat, while also recognizing and taking into consideration the realistic risk of threat Black women encounter as a result of racism and sexism. Future work is needed to identify the ways in which such culturally informed approaches to trauma treatment may improve the effectiveness of treatment for Black women.
Limitations and Future Directions
Although the current study has several strengths, including increased generalizability due to recruitment of a community sample and increased validity due to the use of a clinician-administered measure of PTSD, there are several limitations. First, our assessment of racial discrimination experiences was dichotomous, which precluded the assessment of important considerations such as frequency and stress appraisal. Future research should include more comprehensive assessments of discrimination which also take into consideration experiences occurring at the intersection of multiple systems of oppression (e.g., race, gender, socioeconomic status). Second, we did not examine the moderating role of discrimination in relation to other forms of trauma exposure (e.g., combat trauma, natural disasters) which could evidence different relationships and therefore should be considered in future research. Third, the measures we used assumed that instances of interpersonal trauma occurred independently of racial discrimination which may not be the case. For example, the perpetration of an interpersonal trauma may have occurred in a racial context (e.g., hate crime), which would not have been captured by either measure. Additionally, accruing research utilizing the cultural betrayal trauma theory framework (Gómez & Freyd, 2018) has started to indicate that interpersonal violence perpetration is importantly linked with societal trauma (e.g., oppression, discrimination); such that within-group interpersonal violence in marginalized communities have a strong impact on mental health symptoms. Thus, in addition to examining the interaction between experiences of interpersonal trauma and racial discrimination, future work should examine experiences that occur at the intersection of interpersonal trauma and racial discrimination. Lastly, the cross-sectional design of our study precluded temporal conclusions regarding the impact of racial discrimination on interpersonal trauma experiences and PTSD. Future work should survey the progression of PTSD symptoms to provide a more robust assessment of how chronic experiences of interpersonal trauma and racial discrimination are associated with symptomatology over time.
Conclusions
Our findings provide evidence that racial discrimination exacerbates the association between experiences of interpersonal trauma and the severity of PTSD symptoms. These results highlight the importance of taking these heterogeneous stressors into consideration when conceptualizing PTSD in Black women, rather than assuming that the presence of one type obviates the need to consider another. Given the prevalence of racial discrimination in marginalized groups, our findings inform the literature on the consequences of interpersonal trauma and racial discrimination and may provide insight into the etiology of PTSD in Black women. Continued empirical work in this domain is necessary to reduce the onset, course, and severity of PTSD symptoms among Black women.
Acknowledgements
This work was supported by the National Institute of Mental Health (MH071537; MH100122; MH102890; MH101380, MH115174), the National Institute of Child Health and Human Development (HD071982), the National Institute of Aging (AG062334) and the National Center for Complementary & Integrative Health (K23AT009713).
The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health.
We thank the entire Grady Trauma Project team for their assistance in data collection and management of this project and our participants for their willingness to be a part of our study.
Contributor Information
Yara Mekawi, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 69 Jesse Hill Dr., Atlanta, GA, 30303.
Sierra Carter, Department of Psychology, Georgia State University, 140 Decatur St SE, Atlanta, GA 30303.
Brittney Brown, College of Health Professions, Mercer University, 3001 Mercer University Dr, Atlanta, GA 30341.
Ana Martinez de Andino, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 69 Jesse Hill Dr., Atlanta, GA, 30303.
Negar Fani, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 49 Jesse Hill Dr., Atlanta, GA.
Vas Michopoulos, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 69 Jesse Hill Dr., Atlanta, GA, 30303.
Abigail Powers, Department of Psychiatry and Behavioral Sciences, Emory University School of Medicine, 49 Jesse Hill Dr., Atlanta, GA, 30303.
References
- Alim TN, Graves E, Mellman TA, Lawson W, & Charney DS (2006). Trauma exposure, posttraumatic stress disorder and depression in an African-American primary care population. Journal of the National Medical Association, 98(10), 1630–1636. [PMC free article] [PubMed] [Google Scholar]
- Borders A, & Liang CT (2011). Rumination partially mediates the associations between perceived ethnic discrimination, emotional distress, and aggression. Cultural Diversity and Ethnic Minority Psychology, 17(2), 125–133. 10.1177/1368430219875214 [DOI] [PubMed] [Google Scholar]
- Brooks S, Dubowitz T, Haas A, Ghosh-Dastidar B, DeSantis A, & Troxel WM (2018). The association between discrimination and PTSD in African Americans: Exploring the role of gender. Ethnicity & Health, 1–15. 10.1080/13557858.2018.1444150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carter RT (2007). Racism and psychological and emotional injury: Recognizing and assessing race-based traumatic stress. The Counseling Psychologist, 35(1), 13–105. 10.1177/0011000006292033 [DOI] [Google Scholar]
- Carter RT, & Forsyth J (2010). Reactions to racial discrimination: Emotional stress and help-seeking behaviors. Psychological Trauma: Theory, Research, Practice, and Policy, 2(3), 183–191. 10.1037/a0020102 [DOI] [Google Scholar]
- Carter RT, Johnson VE, Roberson K, Mazzula SL, Kirkinis K, & Sant-Barket S (2017). Race-based traumatic stress, racial identity statuses, and psychological functioning: An exploratory investigation. Professional Psychology: Research and Practice, 48(1), 30–37. 10.1037/pro0000116 [DOI] [Google Scholar]
- Cho S, Crenshaw KW, & McCall L (2013). Toward a field of intersectionality studies: Theory, applications, and praxis. Signs, 38(4), 785–810. 10.1086/669608 [DOI] [Google Scholar]
- Chou T, Asnaani A, & Hofmann SG (2012). Perception of racial discrimination and psychopathology across three US ethnic minority groups. Cultural Diversity and Ethnic Minority Psychology, 18(1), 74–81. 10.1037/a0025432 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cole ER (2009). Intersectionality and research in psychology. American Psychologist, 64(3), 170–180. 10.1037/a0014564 [DOI] [PubMed] [Google Scholar]
- Crenshaw K (1989). Demarginalizing the intersection of race and sex: A Black Feminist critique of antidiscrimination doctrine, feminist theory and antiracist politics. University of Chicago Legal Forum, 1989(8). https://chicagounbound.uchicago.edu/uclf/vol1989/iss1/8 [Google Scholar]
- Davis RG, Ressler KJ, Schwartz AC, Stephens KJ, & Bradley RG (2008). Treatment barriers for low‐income, urban African Americans with undiagnosed Posttraumatic Stress Disorder. Journal of Traumatic Stress, 21(2), 218–222. 10.1002/jts.20313 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Faul F, Erdfelder E, Lang A-G, & Buchner A (2007). G*Power 3: A flexible statistical power analysis program for the social, behavioral, and biomedical sciences. Behavior Research Methods, 39(2), 175–191. 10.3758/bf03193146 [DOI] [PubMed] [Google Scholar]
- Gillespie CF, Bradley B, Mercer K, Smith AK, Conneely K, Gapen M, … Ressler KJ (2009). Trauma exposure and stress-related disorders in inner city primary care patients. General Hospital Psychiatry, 31(6), 505–514. doi: 10.1016/j.genhosppsych.2009.05.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldmann E, Aiello A, Uddin M, Delva J, Koenen K, Gant LM, & Galea S (2011). Pervasive exposure to violence and Posttraumatic Stress Disorder in a predominantly African American Urban Community: The Detroit Neighborhood Health Study. Journal of Traumatic Stress, 24(6), 747–751. 10.1002/jts.20705 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gómez JM, & Freyd JJ (2018). Psychological outcomes of within-group sexual violence: Evidence of cultural betrayal. Journal of Immigrant and Minority Health, 20(6), 1458–1467. 10.1007/s10903-017-0687-0 [DOI] [PubMed] [Google Scholar]
- Hampton R, Oliver W, & Magarian L (2003). Domestic violence in the African American community: An analysis of social and structural factors. Violence Against Women, 9(5), 533–557. 10.1177/1077801202250450 [DOI] [Google Scholar]
- Hatzenbuehler ML, Nolen-Hoeksema S, & Dovidio J (2009). How does stigma “get under the skin”?: The mediating role of emotion regulation. Psychological Science, 20, 1282–1289. 10.1111/j.1467-9280.2009.02441.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AF, Montoya AK, & Rockwood NJ (2017). The analysis of mechanisms and their contingencies: PROCESS versus structural equation modeling. Australasian Marketing Journal (AMJ), 25(1), 76–81. 10.1016/j.ausmj.2017.02.001 [DOI] [Google Scholar]
- Himle JA, Baser RE, Taylor RJ, Campbell RD, & Jackson JS (2009). Anxiety disorders among African Americans, Blacks of Caribbean descent, and non-Hispanic whites in the United States. Journal of Anxiety Disorders, 23(5), 578–590. 10.1016/j.janxdis.2009.01.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirkinis K, Pieterse AL, Martin C, Agiliga A, & Brownell A (2018). Racism, racial discrimination, and trauma: a systematic review of the social science literature. Ethnicity & Health, 1–21. 10.1080/13557858.2018.1514453 [DOI] [PubMed] [Google Scholar]
- Krieger N, Smith K, Naishadham D, Hartman C, & Barbeau EM (2005). Experiences of discrimination: Validity and reliability of a self-report measure for population health research on racism and health. Social Science & Medicine, 61(7), 1576–1596. 10.1016/j.socscimed.2005.03.006 [DOI] [PubMed] [Google Scholar]
- Kubota R, & Nixon RDV (2017). An analogue investigation into the effect of trauma-related rumination on trauma intrusions and the moderating role of trait rumination and depression. Journal of Experimental Psychopathology, 8(4), 413–442. 10.5127/jep.058516 [DOI] [Google Scholar]
- Lee IA, & Preacher KJ (2013, September). Calculation for the test of the difference between two dependent correlations with one variable in common [Computer software] [Google Scholar]
- Lewis JA, & Neville HA (2015). Construction and initial validation of the Gendered Racial Microaggressions Scale for Black women. Journal of Counseling Psychology, 62(2), 289–302. 10.1037/cou0000062 [DOI] [PubMed] [Google Scholar]
- Lewis TT, Cogburn CD, & Williams DR (2015). Self-reported experiences of discrimination and health: scientific advances, ongoing controversies, and emerging issues. Annual Review of Clinical Psychology, 11, 407–440. 10.1146/annurev-clinpsy-032814-112728 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lewis TT, Yang FM, Jacobs EA, & Fitchett G (2012). Racial/ethnic differences in responses to the everyday discrimination scale: A differential item functioning analysis. American Journal of Epidemiology, 175(5), 391–401. 10.1093/aje/kwr287 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mays VM, Cochran SD, & Barnes NW (2007). Race, race-based discrimination, and health outcomes among African Americans. Annual Review of Psychology, 58, 201–225. 10.1146/annurev.psych.57.102904.190212 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norris FH, & Slone LB (2007). The epidemiology of trauma and PTSD. In Friedman MJ, Keane TM, & Resick PA (Eds.), Handbook of PTSD: Science and practice (p. 78–98). The Guilford Press. [Google Scholar]
- Pascoe EA, & Smart Richman L (2009). Perceived discrimination and health: A meta-analytic review. Psychological Bulletin, 135(4), 531–554. 10.1037/a0016059 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pieterse AL, Carter RT, Evans SA, & Walter R (2010). An exploratory examination of the associations among racial and ethnic discrimination, racial climate, and trauma-related symptoms in a college student population. Journal of Counseling Psychology 57, 255–263. 10.1037/a0020040 [DOI] [PubMed] [Google Scholar]
- Powers A, Fani N, Carter S, Cross D, Cloitre M, & Bradley B (2017). Differential predictors of DSM-5 PTSD and ICD-11 complex PTSD among African American women. European Journal of Psychotraumatology, 8(1), 1338914. 10.1080/20008198.2017.1338914 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts AL, Gilman SE, Breslau J, Breslau N, & Koenen KC (2011). Race/ethnic differences in exposure to traumatic events, development of post-traumatic stress disorder, and treatment-seeking for post-traumatic stress disorder in the United States. Psychological Medicine, 41(1), 71–83. 10.1017/s0033291710000401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sibrava NJ, Bjornsson AS, Pérez Benítez ACI, Moitra E, Weisberg RB, & Keller MB (2019). Posttraumatic stress disorder in African American and Latinx adults: Clinical course and the role of racial and ethnic discrimination. American Psychologist, 74(1), 101–116. 10.1037/amp0000339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Smith MR, & Alpert GP (2007). Explaining police bias: A theory of social conditioning and illusory correlation. Criminal Justice and Behavior, 34(10), 1262–1283. 10.1177/0093854807304484 [DOI] [Google Scholar]
- Suarez E, & Gadalla TM (2010). Stop Blaming the Victim: A Meta-Analysis on Rape Myths. Journal of Interpersonal Violence, 25(11), 2010–2035. 10.1177/0886260509354503 [DOI] [PubMed] [Google Scholar]
- Utsey SO, Belvet B, Hubbard RR, Fischer NL, Opare-Henaku A, & Gladney LL (2012). Development and validation of the Prolonged Activation and Anticipatory Race-Related Stress Scale. Journal of Black Psychology, 39(6), 532–559. 10.1037/t27626-000 [DOI] [Google Scholar]
- Utsey SO, Ponterotto JG, Reynolds AL, & Cancelli AA (2000). Racial discrimination, coping, life satisfaction, and self-esteem among African Americans. Journal of Counseling & Development, 78(1), 72–80. 10.1002/j.1556-6676.2000.tb02562.x [DOI] [Google Scholar]
- Watson LB, DeBlaere C, Langrehr KJ, Zelaya DG, & Flores MJ (2016). The influence of multiple oppressions on women of color’s experiences with insidious trauma. Journal of Counseling Psychology, 63(6), 656–667. 10.1037/cou0000165 [DOI] [PubMed] [Google Scholar]
- Watson NN, & Hunter CD (2015). Anxiety and depression among African American women: The costs of strength and negative attitudes toward psychological help-seeking. Cultural Diversity and Ethnic Minority Psychology, 21(4), 604–612. 10.1037/cdp0000015 [DOI] [PubMed] [Google Scholar]
- Weathers FW, Bovin MJ, Lee DJ, Sloan DM, Schnurr PP, Kaloupek DG, Keane TM, & Marx BP (2017). Clinician-Administered PTSD Scale for DSM-5 (CAPS-5) [Database record]. APA PsycTests 10.1037/t71324-000 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, & Mohammed SA (2009). Discrimination and racial disparities in health: Evidence and needed research. Journal of Behavioral Medicine, 32(1), 20–47. 10.1007/s10865-008-9185-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams DR, Neighbors HW, & Jackson JS (2003). Racial/ethnic discrimination and health: Findings from community studies. American Journal of Public Health, 93(2), 200–208. 10.2105/ajph.93.2.200 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MT, Metzger IW, Leins C, & DeLapp C (2018). Assessing racial trauma within a DSM–5 framework: The UConn Racial/Ethnic Stress & Trauma Survey. Practice Innovations, 3(4), 242–260. 10.1037/pri0000076 [DOI] [Google Scholar]


