Abstract
Background:
Rerupture of the reconstructed ulnar collateral ligament (UCL) is becoming more frequent at the professional level of baseball. However, there is no literature describing outcomes after UCL graft repair.
Purpose:
To evaluate rerupture rate, return to play, performance upon return, and patient-reported outcomes after a novel UCL graft repair technique.
Study Design:
Case series; Level of evidence, 4.
Methods:
All included patients underwent UCL graft repair after a previous UCL reconstruction, pitched in at least 1 professional baseball game before repair, and were at least 2 years postprocedure within the same 10-year time period. The authors evaluated patient characteristics and performance metrics, including wins, losses, win percentage, earned run average, innings pitched, walks and hits per inning pitched, for the 2 seasons before and after the procedure. Patients were contacted to assess UCL rerupture, timing of return to sport, current level of competition, Conway score, and Kerlan-Jobe Orthopaedic Clinic (KJOC) Shoulder and Elbow Score.
Results:
Six players met the inclusion criteria. All had proximal UCL graft ruptures and underwent flexor-pronator tendon repair in combination with graft repair. At a mean (±SD) follow-up of 56.7 ± 37.8 months, no reruptures were encountered, and the mean KJOC score was 87.9 ± 14.6. Of the 6 pitchers who underwent UCL graft repair, 4 (67%) returned to professional pitching at a mean of 17 ± 6 months. Three of the 6 (50%) achieved an excellent Conway score, signifying a return to prior level of sport. There was no significant difference in demographic or preoperative pitching performance metrics between players who did and did not return to pitching. For those players who returned to professional pitching, there was no significant difference between preprocedure and postprocedure performance statistics.
Conclusion:
Repair of the UCL graft appears to yield comparable rates of return to play and performance with revision UCL reconstruction. This technique serves as a viable alternative for proximal avulsion ruptures of the UCL graft.
Keywords: ulnar collateral ligament, Tommy John surgery, pitching, return to play
Medial ulnar collateral ligament (UCL) injuries of the elbow are common among overhead-throwing athletes. While first described among javelin athletes, UCL injury is synonymous with baseball pitchers, and the frequency of this injury has seen a meteoric rise in the United States. 6,17,25 Hodgins et al 12 demonstrated a yearly increase in the number of UCL reconstructions (UCLRs) performed from 2002 to 2011. There has been an increasing incidence of primary UCLR among players in Major League Baseball (MLB) and Minor League Baseball. 4 Perhaps most concerning is the rising trend of UCLR among youth throwers aged 15 to 19 years, which accounted for more than twice as many procedures as the 20- to 24-year-old cohort in a single-payer database. 10 Mahure et al 17 again demonstrated this finding while also forecasting further increases in UCLR among this same demographic through 2025. However, outcomes after UCLR are excellent, with most series reporting an 80% to 95% return-to-pitching rate, with 67% to 78% at the same level of competition. 11,15,18,20,23 Return-to-sport outcomes support UCLR as the gold standard of treatment for patients with UCL injuries.
Outcomes after revision reconstruction are much less successful. 5,13,19 In the largest series on revision UCLRs, Camp et al 4 showed that while 77% of players return to competitive baseball, only 55% return at the same level. Andrews et al 1 showed near-identical findings in a series of 40 baseball players undergoing revision UCLR via the modified Jobe technique, with only 50% able to return to the same level of competition. Previous smaller cohorts demonstrated similar rates of return to play and level of return. 14,19 These tempered results should be viewed with greater clinical concern given the rising trend in revision UCLRs combined with the lack of surgical alternatives for recurrent UCL graft rupture.
There are currently no studies describing alternatives to revision reconstruction in the setting of UCL graft rupture and none discussing outcomes based on UCL graft rupture pattern. The purpose of this study was to evaluate rerupture rates, patient-reported outcome measures, and return-to-play rate of professional pitchers undergoing a novel UCL graft repair. Our hypothesis was that UCL graft repair would lead to similar rates of return to play and patient-reported outcomes compared with revision reconstruction, as has been described in the literature among professional pitchers.
Methods
This study was approved by our institutional review board. All elbow UCL procedures performed over a 10-year period (2010-2019) by the senior author (N.S.E.) were reviewed. Criteria for inclusion were a UCL injury in a patient who had a prior UCLR and at least 1 game of professional pitching experience before UCL graft repair with a minimum clinical follow-up of 2 years. The indication for this procedure is medial ulnar collateral graft avulsion resulting in medial elbow insufficiency in a player who desires to return to professional pitching. Players with a concurrent diagnosis of flexor-pronator injury, ulnar neuritis or nerve instability, and/or posteromedial impingement were also included. Professional pitchers with less than 2 years’ follow-up from the procedure, professional position players, amateur baseball players, and other overhead athletes were excluded from this cohort.
Pertinent clinical records were reviewed to obtain player information, advanced imaging, injury characteristics, operative details, and level of sport. Players were then contacted via telephone to ascertain the status of the UCL repair, time to return to sport, and Conway score. The Kerlan-Jobe Orthopaedic Clinic (KJOC) Shoulder and Elbow questionnaire was administered over the telephone as well. Pitching performance metrics including wins, losses, win percentage, earned run average (ERA), innings pitched, and walks and hits per inning pitched (WHIP) for the 2 years before and after surgery were also collected from publicly available data and reported as an average. Subgroup analysis was performed using paired t tests for continuous data with the level of significance set at P < .5 and is reported as mean ± SD. A power analysis was not performed, given that this is a descriptive series of a novel procedure.
Operative Technique
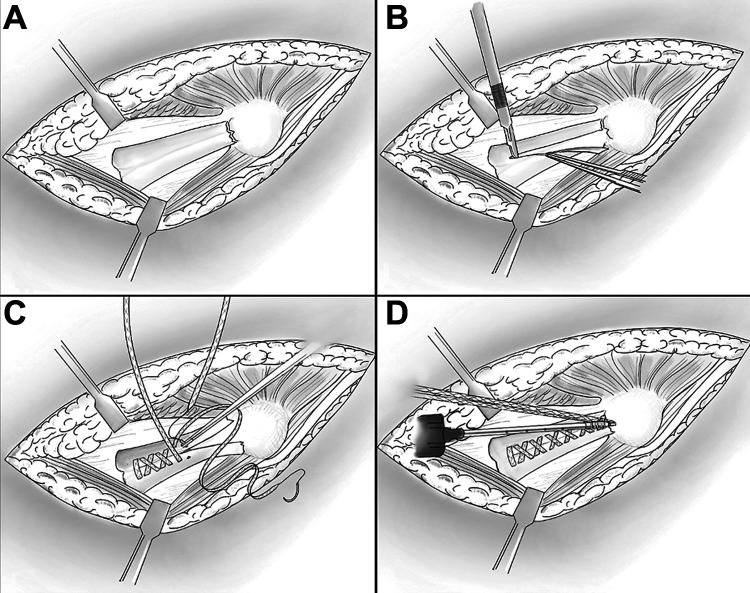
The patient was placed in the supine position with the operative extremity placed on a hand table attachment. A tourniquet was used to assist with hemostasis. The incision was dictated based on the previous scar, and care was taken during dissection to identify and spare the remaining branches of the medial antebrachial cutaneous nerve. The fascia overlying the flexor muscle mass was then incised longitudinally, and the muscle was split in-line with its fibers. The muscle and scar tissue were elevated to expose the entire graft, including the humeral and ulnar attachments (Figure 1A). The graft was then split longitudinally in its midportion, and the deep surface was inspected to confirm no areas of attenuation (Figure 1B). The avulsed end of the ligament and its bony attachment site were then debrided to create a healing surface on either the epicondyle or the sublime tubercle.
Figure 1.
(A) Wide exposure via the muscle-splitting approach showing the proximal avulsion of the ulnar collateral ligament (UCL) in a right elbow. (B) The graft was split longitudinally but sparing the origin of the intact distal attachment. The UCL graft was examined for any areas of attenuation of calcifications that would preclude a repair. (C) The UCL graft was sutured in a running fashion starting at the nonruptured end, tensioning the suture after each throw. The final pass of each suture limb ended with the tails exiting superficially to the graft. (D) Both free ends of the suture were secured to the anatomic bony footprint with a knotless suture anchor.
A nonabsorbable SutureTape (Arthrex) suture was then stitched in a running fashion from the nondiseased end of the graft toward the avulsed end (Figure 1C). With each throw, the suture was tensioned to draw any slack from the construct. These suture tails were then placed through the eyelit of a 3.5-mm SwiveLock anchor (Arthrex) and seated into the location on the footprint that would allow the anchor the best purchase, which was seated without undue tension (Figure 1D). Alternatively, if the epicondyle bone stock was unsuitable to hold an anchor, a 2.6-mm cortical button (Arthrex) was passed through the previous bone tunnel to the superior dorsal surface and the sutures were tied. The elbow was then ranged and stressed to confirm that stability was achieved. The flexor pronator tendon was then repaired using a separate suture anchor unless the epicondyle bone was severely compromised. The fascia and skin were then closed in a layered fashion.
Postoperative Rehabilitation
Our rehabilitation protocol called for the elbow to be placed in a splint and sling for 1 to 2 weeks after the procedure with isometric wrist and forearm strengthening permitted. The elbow was transitioned into a hinged brace at this time and elbow range of motion was begun. Once the incision healed, a total body conditioning program emphasizing shoulder and core exercises was begun. When full elbow range of motion was achieved, progressive resistance strengthening was incorporated with the total body conditioning program. An interval throwing program was begun typically around 4 months postoperatively, lasting approximately 6 months.
Results
Of the 7 professional pitchers undergoing this procedure, 6 met criteria and were included in this study; 1 pitcher was excluded because the location of the UCL tear was midsubstance, not proximal. Of the included pitchers, 4 were right-handed while 2 were left-handed. The mean age was 27.5 ± 3.1 years. The mean number of professional seasons pitched before surgery was 6.67 ± 3.0. The mean number of prior UCL procedures was 1.5 ± 0.8 (range, 1-3), and the mean time from most recent UCL procedure to UCL graft repair was 4.0 ± 2.96 years. Ulnar nerve transposition was performed in 5 of the 6 (83%) players, and arthroscopic posterior compartment decompression in 1 (17%) player (Table 1). All players had proximal avulsion graft tears on preoperative imaging and underwent concomitant flexor-pronator tendon repair as described above.
Table 1.
Patient Characteristics and Concomitant Procedures a
| Player | Position | Starter or Reliever | Age at Surgery, y | Prior Professional Experience, y | Previous UCL Surgeries, n | Time Between Previous Surgery and UCL Graft Repair, y | Concomitant Procedures |
|---|---|---|---|---|---|---|---|
| 1 | RHP | Reliever | 26 | 4 | 1 | 7 | None |
| 2 | RHP | Starter | 29 | 8 | 2 | 1 | UNT |
| 3 | LHP | Reliever | 31 | 8 | 3 | 1 | UNT |
| 4 | RHP | Reliever | 22 | 2 | 1 | 2 | UNT |
| 5 | LHP | Starter | 28 | 10 | 1 | 7 | UNT |
| 6 | RHP | Reliever | 29 | 8 | 1 | 6 | UNT, arthroscopic PCD |
| Mean ± SD | — | — | 27.5 ± 3.1 | 6.67 ± 3.0 | 1.5 ± 0.84 | 4.0 ± 2.96 | — |
a LHP, left-handed pitcher; PCD, posterior compartment decompression; RHP, right-handed pitcher; UCL, ulnar collateral ligament; UNT, ulnar nerve transposition. Dashes indicate no value.
The mean length of clinical follow-up was 56.7 ± 37.8 months. Four (67%) players were able to return to professional pitching at an average of 17 ± 6 months (range, 12-24 months). Of these 4 players, 3 (75%) had a Conway score of excellent, denoting return to the same level of professional baseball, and 1 player had a Conway score of good, denoting a return to professional baseball but at a lower level. Of the 2 players who did not return to professional baseball, both were still actively seeking professional pitching opportunities at the time of final follow-up. No reruptures were encountered for the entire cohort, and the mean KJOC score was 87.9 ± 14.6 (Table 2).
Table 2.
Patient Outcomes After UCL Graft Repair a
| Level of Competition | |||||||
|---|---|---|---|---|---|---|---|
| Player | Before Surgery | After Surgery | Conway Score | Time to Return to Competition, mo | Length of Follow-up, mo | KJOC Score | Graft Rupture |
| 1 | MLB | MLB | Excellent | 12 | 129 | 95 | No |
| 2 | MLB | AAA b | Good | 24 | 58 | 85 | No |
| 3 | MLB | MLB | Excellent | 20 | 58 | 90 | No |
| 4 | A | — | Fair | — | 36 | 97.2 | No |
| 5 | MLB | — | Fair | — | 35 | 60.25 | No |
| 6 | AAA | AAA | Excellent | 12 | 24 | 100 | No |
| Mean ± SD | 17 ± 6 | 56.7 ± 37.8 | 87.9 ± 14.6 | ||||
a MLB, Major League Baseball; UCL, ulnar collateral ligament. Dashes indicate no value.
b A, Single A; AAA, Triple A.
No reruptures occurred at a mean follow-up length of 56.7 ± 37.8 months. The mean KJOC score was 87.9 ± 14.6. When comparing the cohort of players who returned to professional baseball and those who did not, there were no significant differences in age, seasons of prior professional experience, number of prior UCL procedures, time between previous UCL procedure and UCL graft repair, KJOC score, or preoperative wins, losses, win percentage, ERA, innings pitched, and WHIP (Table 3). There was no difference in preoperative and postoperative wins, losses, win percentage, ERA, innings pitched, or WHIP for those players who returned to pitching (Table 4).
Table 3.
Comparison Between Pitchers Who Did Versus Did Not Return to Play a
| Returners, n = 4; 67% | Nonreturners, n = 2; 33% | P | |
|---|---|---|---|
| Age, y | 28.8 ± 2.1 | 25.0 ± 4.2 | .19 |
| Prior professional experience, y | 7 ± 2 | 6 ± 5.7 | .75 |
| Number of previous UCL surgeries | 1.75 ± 0.9 | 1 ± 0 | .36 |
| Time between previous surgery and UCL graft repair, y | 3.75 ± 3.2 | 4.5 ± 3.5 | .81 |
| KJOC score | 92.5 ± 6.5 | 78.73 ± 26.1 | .32 |
| Yearly pitching statistics in 2 y before surgery | |||
| Wins | 2.67 ± 1.7 | 5.5 ± 3.5 | .42 |
| Losses | 2.83 ± 1.24 | 4.5 ± 0.5 | .17 |
| Win percentage | 0.52 ± 0.03 | 0.49 ± 0.15 | .81 |
| ERA | 3.15 ± 1.27 | 5.15 ± 0.79 | .22 |
| Innings pitched | 45.3 ± 2.74 | 69.1 ± 36.1 | .44 |
| WHIP | 2.59 ± 1.93 | 1.58 ± 0.13 | .61 |
a Data are reported as mean ± SD. ERA, earned run average; KJOC, Kerlan-Jobe Orthopaedic Clinic; UCL, ulnar collateral ligament; WHIP, walks and hits per inning pitched.
Table 4.
Pitching Performance Before and After UCL Graft Repair a
| 2 y Before Surgery | 2 y After Surgery | P | |
|---|---|---|---|
| Wins | 2.6 ± 1.52 | 3.14 ± 3.24 | .74 |
| Losses | 1.00 ± 1.73 | 2.14 ± 2.54 | .92 |
| Win percentage | 0.60 ± 0.11 | 0.54 ± 0.33 | .74 |
| ERA | 2.92 ± 1.25 | 1.82 ± 1.14 | .88 |
| Innings pitched | 50.6 ± 8.1 | 41.6 ± 29.8 | .53 |
| WHIP | 2.07 ± 1.81 | 1.18 ± 0.11 | .22 |
a Data are reported as mean ± SD. ERA, earned run average; UCL, ulnar collateral ligament; WHIP, walks and hits per inning pitched.
Subgroup analysis comparing pitchers who returned to play with those who did not return to play showed no statistically significant difference in demographic or pitching performance metrics. No significant statistical difference was found in pitching performance in the 2 years before and after UCL graft repair.
Discussion
Refinement of UCLR techniques combined with diligent rehabilitation has largely shifted a UCL rupture diagnosis from a career-ending injury to merely an occupational hazard. The same cannot be said after reruptures of the previously reconstructed graft. Andrews et al 1 reported that of a series of 40 pitchers from various levels in an institutional database, 80% were able to return to baseball, but only 47% returned to the same level of competition (reported as a Conway score of excellent). Of the 10 MLB pitchers included in that study, 80% reported excellent Conway scores. In a review of the MLB Health and Injury Tracking System database, Camp et al 5 identified 69 pitchers undergoing revision UCLR over a 7-year period. Of these, 76% returned to pitching, but only 55% at their same level of competition. Camp et al 4 reviewed the outcomes of all professional pitchers from 1974 to 2016 undergoing revision UCLR, finding that 80% returned to pitching, but only 63.5% at their previous level of competition. While all 3 of these studies do show slightly superior rates of return to play, all mirror the trend of a lower return to level of competition. Additionally, there is likely significant crossover of individuals included among these studies.
Our cohort of pitchers returned to professional competition at a mean of 17.0 ± 6 months, consistent with other similar reported series. Andrews et al 1 reported pitchers of all levels returning to competition at a mean of 12.8 ± 3.7 months, while the MLB pitchers took 14.5 months (range, 10-21 months). Camp et al 5 reported that their cohort of professional pitchers returned to the same level of competition at 16.1 ± 3.9 months.
Our study showed no significant change in pitching performance statistics in the 2 years before and 2 years after UCL graft repair. This is in contrast to the findings of Liu et al, 16 who, in a series of 35 MLB pitchers, showed a significant drop in innings pitched and total pitches after revision UCLR. However, there were no significant changes in ERA, batting average against pitcher, strikeouts per 9 innings, percentage of pitches thrown in the strike zone, WHIP, or average fastball velocity. In a series of 43 MLB pitchers undergoing revision UCLR, Marshall et al 19 also showed significant decreases in innings pitched, in addition to wins, losses, and walks per 9 innings. They failed to show a significant change in ERA, WHIP, or win percentage. It should be noted that their control cohort pitched a mean of 75 innings per year, which is demonstrably higher than the innings pitched before surgery for our series. In terms of patient-reported outcomes, our cohort showed mean KJOC score of 87.9 ± 14.6. There was no significant difference in KJOC score among those players who returned to pitching and those who did not. The only other series recording patient-reported outcomes is that of Andrews et al, 1 who showed a mean KJOC score of 74 ± 21 for pitchers of all levels. It has been demonstrated that the KJOC score is the most sensitive way to detect subtle variations in pitching performance after UCLR. 7 Thus, the KJOC score may provide more accurate insight into pitching performance and ability than performance metrics alone.
While this UCL repair is novel in its application for revision surgery, it is well described in the primary setting. Savoie et al 22 described the first series showing successful native UCL ligament repair in proximal and distal avulsion tear patterns with an otherwise intact ligament. This laid the groundwork for further advancement by Walters et al 24 with their addition of a high-strength suture to act as a brace to support the ligament. This procedure has great promise, with short-term results showing high rates of return to play and performance among pitchers. 8 Additionally, native UCL repair with suture augmentation with an InternalBrace (Arthrex) has been shown to have equivalent time-zero biomechanical properties to the native ligament and reconstructed ligament using the docking and modified Jobe techniques. 2,9,13,21 Our technique also utilizes a high-strength suture acting as a biologic internal brace to allow partial shielding of valgus stress during the early repair phases of ligament healing. It is not beyond reason to assume that the biomechanical properties of native UCL repair extend to repairs of the UCL graft.
Our described technique has several technical benefits, the first being the avoidance of graft harvest morbidity associated with reconstructions. It also avoids the need to allow the newly reconstructed tendon to mature into ligamentous tissue, theoretically accelerating the rehabilitation progress. By anchoring the suture through the ligament on one side and into an anchor on the other, there is no concern for overconstraint of the construct, a common criticism of independent fixation. Overconstraint has been sparsely reported in the literature and has not been reported with native UCL repair combined with InternalBrace, and it remains unclear if this construct has a role with UCL graft. The disadvantages of this technique are the same as those with repair of the native UCL ligament. Preoperative magnetic resonance imaging may not fully detail ligament integrity and could conceal areas of attenuation. Thus, intraoperative evaluation of the entire ligament is necessary. As with all UCL surgery, secure fixation is dependent on adequate bone stock of the ulna and/or epicondyle. 3 In the revision setting, this may be compromised from previous procedures, will dictate fixation method, and may preclude repair.
The limitations of this study are multiple. This study was retrospective in nature and consisted of only 6 players, making this a small series despite case series being the most common study design regarding UCL surgery. Additionally, this is a single-surgeon series, which may not be reproducible or generalizable to other institutions or patient populations. Another limitation is that this technique only applies to proximal UCL graft tears/avulsions and not UCL re-repairs. The reporting of KJOC scores for all individuals is certainly of merit for this study, as they have been shown to be a highly valid measure of function and performance after UCL surgery. Perhaps more advantageous would be the collection of preprocedure KJOC scores, allowing one to better quantify the amount of improvement gained after this procedure.
Conclusion
Outcomes after UCL graft repair yield comparable rates of return to sport and level of competition with revision UCLR. For those who do return to professional baseball, pitching statistics will remain similar to their preprocedure performance. Overall satisfaction with the elbow based on KJOC score does not appear to be affected by ability to return to competitive baseball. This procedure may be a viable alternative to revision reconstruction of proximal avulsion tears with an otherwise intact graft.
Acknowledgment
The authors acknowledge Ali Noorzad, MD, for the illustrations.
Footnotes
Final revision submitted January 11, 2022; accepted February 8, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: M.J.S. has received grant support from Arthrex and Stryker and education payments from Micromed and Smith & Nephew. B.M.H. has received grant support from Arthrex and education payments from Micromed and Smith & Nephew. N.S.E. has received education payments from Arthrex and Micromed and speaking fees and royalties from Arthrex. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from Cedars-Sinai Medical Center (reference No. STUDY00000978).
References
- 1. Andrews JR, Venkateswaran V, Christensen KD, et al. Outcomes after ulnar collateral ligament revision reconstruction in baseball players. Am J Sports Med. 2020;48(13):3359–3364. doi:10.1177/0363546520951529 [DOI] [PubMed] [Google Scholar]
- 2. Bodendorfer BM, Looney AM, Lipkin SL, et al. Biomechanical comparison of ulnar collateral ligament reconstruction with the docking technique versus repair with internal bracing. Am J Sports Med. 2018;46(14):3495–3501. doi:10.1177/0363546518803771 [DOI] [PubMed] [Google Scholar]
- 3. Bruce JR, ElAttrache NS, Andrews JR. Revision ulnar collateral ligament reconstruction. J Am Acad Orthop Surg. 2018;26(11):377–385. doi:10.5435/JAAOS-D-16-00341 [DOI] [PubMed] [Google Scholar]
- 4. Camp CL, Conte S, D’Angelo J, Fealy SA. Epidemiology of ulnar collateral ligament reconstruction in Major and Minor League Baseball pitchers: comprehensive report of 1429 cases. J Shoulder Elbow Surg. 2018;27(5):871–878. doi:10.1016/j.jse.2018.01.024 [DOI] [PubMed] [Google Scholar]
- 5. Camp CL, Desai V, Conte S, et al. Revision ulnar collateral ligament reconstruction in professional baseball: current trends, surgical techniques, and outcomes. Orthop J Sports Med. 2019;7(8):232596711986410. doi:10.1177/2325967119864104 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. DeFroda SF, Goodman AD, Gil JA, Owens BD. Epidemiology of elbow ulnar collateral ligament injuries among baseball players: National Collegiate Athletic Association Injury Surveillance Program, 2009-2010 through 2013-2014. Am J Sports Med. 2018;46(9):2142–2147. doi:10.1177/0363546518773314 [DOI] [PubMed] [Google Scholar]
- 7. Domb BG, Davis JT, Alberta FG, et al. Clinical follow-up of professional baseball players undergoing ulnar collateral ligament reconstruction using the new Kerlan-Jobe Orthopaedic Clinic Overhead Athlete Shoulder and Elbow Score (KJOC Score). Am J Sports Med. 2010;38(8):1558–1563. doi:10.1177/0363546509359060 [DOI] [PubMed] [Google Scholar]
- 8. Dugas JR, Looze CA, Capogna B, et al. Ulnar collateral ligament repair with collagen-dipped FiberTape augmentation in overhead-throwing athletes. Am J Sports Med. 2019;47(5):1096–1102. doi:10.1177/0363546519833684 [DOI] [PubMed] [Google Scholar]
- 9. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44(3):735–741. doi:10.1177/0363546515620390 [DOI] [PubMed] [Google Scholar]
- 10. Erickson BJ, Nwachukwu BU, Rosas S, et al. Trends in medial ulnar collateral ligament reconstruction in the United States: a retrospective review of a large private-payer database from 2007 to 2011. Am J Sports Med. 2015;43(7):1770–1774. doi:10.1177/0363546515580304 [DOI] [PubMed] [Google Scholar]
- 11. Ford GM, Genuario J, Kinkartz J, Githens T, Noonan T. Return-to-play outcomes in professional baseball players after medial ulnar collateral ligament injuries: comparison of operative versus nonoperative treatment based on magnetic resonance imaging findings. Am J Sports Med. 2016;44(3):723–728. doi:10.1177/0363546515621756 [DOI] [PubMed] [Google Scholar]
- 12. Hodgins JL, Vitale M, Arons RR, Ahmad CS. Epidemiology of medial ulnar collateral ligament reconstruction: a 10-year study in New York State. Am J Sports Med. 2016;44(3):729–734. doi:10.1177/0363546515622407 [DOI] [PubMed] [Google Scholar]
- 13. Jones CM, Beason DP, Dugas JR. Ulnar collateral ligament reconstruction versus repair with internal bracing: comparison of cyclic fatigue mechanics. Orthop J Sports Med. 2018;6(2):232596711875599. doi:10.1177/2325967118755991 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Jones KJ, Conte S, Patterson N, ElAttrache NS, Dines JS. Functional outcomes following revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. J Shoulder Elbow Surg. 2013;22(5):642–646. doi:10.1016/j.jse.2013.01.031 [DOI] [PubMed] [Google Scholar]
- 15. Keller RA, Steffes MJ, Zhuo D, Bey MJ, Moutzouros V. The effects of medial ulnar collateral ligament reconstruction on Major League pitching performance. J Shoulder Elbow Surg. 2014;23(11):1591–1598. doi:10.1016/j.jse.2014.06.033 [DOI] [PubMed] [Google Scholar]
- 16. Liu JN, Garcia GH, Conte S, ElAttrache N, Altchek DW, Dines JS. Outcomes in revision Tommy John surgery in Major League Baseball pitchers. J Shoulder Elbow Surg. 2016;25(1):90–97. doi:10.1016/j.jse.2015.08.040 [DOI] [PubMed] [Google Scholar]
- 17. Mahure SA, Mollon B, Shamah SD, Kwon YW, Rokito AS. Disproportionate trends in ulnar collateral ligament reconstruction: projections through 2025 and a literature review. J Shoulder Elbow Surg. 2016;25(6):1005–1012. doi:10.1016/j.jse.2016.02.036 [DOI] [PubMed] [Google Scholar]
- 18. Marshall NE, Keller RA, Limpisvasti O, ElAttrache NS. Pitching performance after ulnar collateral ligament reconstruction at a single institution in Major League Baseball pitchers. Am J Sports Med. 2018;46(13):3245–3253. doi:10.1177/0363546518795670 [DOI] [PubMed] [Google Scholar]
- 19. Marshall NE, Keller RA, Lynch JR, Bey MJ, Moutzouros V. Pitching performance and longevity after revision ulnar collateral ligament reconstruction in Major League Baseball pitchers. Am J Sports Med. 2015;43(5):1051–1056. doi:10.1177/0363546515579636 [DOI] [PubMed] [Google Scholar]
- 20. Osbahr DC, Cain EL, Raines BT, Fortenbaugh D, Dugas JR, Andrews JR. Long-term outcomes after ulnar collateral ligament reconstruction in competitive baseball players: minimum 10-year follow-up. Am J Sports Med. 2014;42(6):1333–1342. doi:10.1177/0363546514528870 [DOI] [PubMed] [Google Scholar]
- 21. Roth TS, Beason DP, Clay TB, Cain EL, Dugas JR. The effect of ulnar collateral ligament repair with internal brace augmentation on articular contact mechanics: a cadaveric study. Orthop J Sports Med. 2021;9(4):232596712110010. doi:10.1177/23259671211001069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Savoie FH, Trenhaile SW, Roberts J, Field LD, Ramsey JR. Primary repair of ulnar collateral ligament injuries of the elbow in young athletes: a case series of injuries to the proximal and distal ends of the ligament. Am J Sports Med. 2008;36(6):1066–1072. doi:10.1177/0363546508315201 [DOI] [PubMed] [Google Scholar]
- 23. Walker CM, Genuario JW, Houck DA, Murayama S, Mendez H, Noonan TJ. Return-to-play outcomes in professional baseball players after nonoperative treatment of incomplete medial ulnar collateral ligament injuries: a long-term follow-up study. Am J Sports Med. 2021;49(5):1137–1144. doi:10.1177/0363546521996706 [DOI] [PubMed] [Google Scholar]
- 24. Walters BL, Cain EL, Emblom BA, Frantz JT, Dugas JR. Ulnar collateral ligament repair with internal brace augmentation: a novel UCL repair technique in the young adolescent athlete. Orthop J Sports Med. 2016;4(3)(suppl 3):2325967116S0007. doi:10.1177/2325967116S00071 [Google Scholar]
- 25. Waris W. Elbow injuries of javelin-throwers. Acta Chir Scand. 1946;93(6):563–575. [PubMed] [Google Scholar]