Abstract
Background:
Internal bracing of anterior cruciate ligament (ACL) surgery is a newer concept gaining popularity.
Purpose/Hypothesis:
To assess the biomechanical performance of soft tissue ACL reconstruction allografts reinforced with suture tape. It was hypothesized that load to failure would increase and cyclic displacement would decrease at time zero in the constructs reinforced with internal brace suture tape compared with those without suture tape augmentation.
Study Design:
Controlled laboratory study.
Methods:
We performed ACL reconstruction on porcine knees using bovine extensor tendon soft tissue allografts: 10 knees without (control) and 10 knees with (reinforced) suture tape reinforcement. An all-inside reconstruction technique was utilized with retrograde tunnel creation. An adjustable-loop device was used for femoral and tibial fixation of all grafts. The suture tape was placed through the tension loop in the femoral fixation construct and independently fixed in the tibia with an interference screw anchor. For each specimen, the authors recorded ultimate load, yield load, stiffness, cyclic displacement, and mode of failure. Outcomes between groups were compared using the Student t test.
Results:
There was a 33% decrease in mean cyclic displacement in the specimens with reinforced grafts (reinforced vs control: 3.9 ± 0.7 vs 5.8 ± 1.5 mm; P = .001). The reinforced grafts also had a 22% higher mean ultimate load (921 ± 180 vs 717 ± 122 N; P = .008) and a 25% higher mean yield load (808 ± 201 vs 602 ± 155 N; P = .020). There was no significant difference in stiffness between the reinforced versus nonreinforced grafts (136 ± 16 vs 132 ± 18 N/mm; P = .617). Three of the 10 control specimens failed at the graft, compared with 1 of 10 reinforced grafts. All other constructs in both groups failed at the tibial fixation site.
Conclusion:
Suture tape reinforcement of soft tissue grafts significantly decreased cyclic displacement while significantly increasing ultimate and yield loads without increasing graft construct stiffness during biomechanical testing at time zero in a porcine animal model.
Clinical Relevance:
The improved biomechanical performance of suture tape–reinforced graft constructs could allow patients to participate in earlier advancement of aggressive rehabilitation and potentially reduce failure rates as graft remodeling progresses.
Keywords: anterior cruciate ligament, ACL reconstruction, soft tissue, internal brace, biomechanics
Anterior cruciate ligament (ACL) reconstructions have historically utilized autologous and allograft tissues as well as synthetic materials. 14,18,26,39 Various techniques, graft configurations, sizes, and composition have been used, but failure rates have ranged from 8% to 17%. 19,25 Currently, all tendon soft tissue and middle-third patellar bone-tendon-bone (BTB) grafts are most commonly used in ACL reconstruction. 40
Clinical and animal studies have revealed increased incorporation and maturation times for soft tissue grafts in comparison with BTB grafts. 3,7 Longer revascularization and remodeling maturation times of soft tissue grafts present a challenge during rehabilitation. 3,31 An increased interest in accelerated rehabilitation and return to sporting activities provides a challenge of protecting the graft from elongation and overt failure until maturity of the graft is achieved. Stemming from these concerns is a renewed focus on the application of synthetic graft augmentation with suture tape internal bracing techniques. 33,34,37
ACL surgery reinforcement with suture bracing has emerged as a newer technique. Repairs of ACL tears reinforced with suture tape have been previously described by Mackay et al; 22 internal bracing with suture of pediatric ACL reconstructions was described by Smith et al. 32 Smith et al 33,34 have provided techniques for internal brace suture reinforcement of soft tissue allograft ACL reconstructions and biomechanical data for BTB reconstructions with internal brace augmentation. These techniques have provided further methods and data, suggesting protection of the ACL reconstruction graft from early elongation and failure. This could allow early accelerated physical therapy and possibly reinjury after return to higher-level activities.
The purpose of this study was to assess the biomechanical performance of soft tissue allografts reinforced with suture tape for ACL reconstruction. The hypothesis was that load to failure would increase and that cyclic displacement would decrease in the suture tape–reinforced constructs compared with the soft tissue constructs without suture tape augmentation.
Methods
Six-month-old porcine femurs and tibias with all soft tissue removed (Advanced Tissue Concepts) were potted in fiberglass resin (Bondo; 3M). Twenty (16 right, 4 left) total porcine knees were split into 2 groups of 10. Each group had an equal number of right- and left-sided specimens. The number of specimens and initial preparation were guided by research from Walsh et al 38 and equaled those of Smith et al. 34
A sample size of 20 knees was used to obtain significance given the differences in the means for the biomechanical study. This was verified using a sample-size calculator. 16 The number of samples coincides with similar biomechanical studies involving ligament repair and reconstruction with augmentation. 4,9,12,13,34
Graft Preparation
Quadrupled bovine extensor tendon allografts were utilized as the ACL reconstruction grafts. The graft sizes used had diameters of 10 mm (n = 6), 10.5 mm (n = 12), and 11 mm (n = 2). The larger grafts were used in larger knees. The grafts were prepared by whipstitching the free ends with a looped suture. Each graft was quadrupled and sutured with 2-0 polyblend high-strength suture at 10 and 20 mm from the graft ends to secure all the graft limbs together. Adjustable-loop suspensory-fixation devices (TightRope RT and ABS; Arthrex) were positioned at each end of the graft before the cerclage suture placement at 10 and 20 mm from the graft ends. The femoral adjustable-loop device construct incorporated a suspensory button, and the tibial side allowed for a suspensory button attachment.
A 2-mm suture tape was looped through the suspensory-loop suture portion of the femur-sided fixation, providing a loop-to-loop configuration (Figure 1). This configuration was chosen by the surgeon because it allows easier passage of the femoral button through the cortex and less potential to interfere with suspensory-loop tightening. The suture tape was then passed deep to the graft cerclage sutures with a Keith needle. This arrangement allows for less suture between the graft and bone socket interface in an attempt to have less interference of graft-to-bone healing. The suture tape internal brace was kept independent of the graft and was passed freely under all cerclage sutures, exiting the tibial side of the graft (Figure 2). Tensioning of the graft with 20 N of longitudinal force using a spring-loaded tensioning device was applied to reduce creep from the tissue.
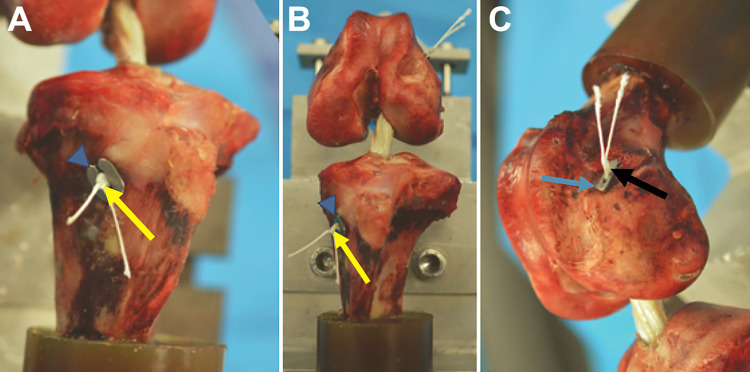
Figure 1.

Suture tape internal brace (white arrows) placed through the femoral suspensory-fixation suture loop (black arrows). Shown without the graft to illustrate the loop-to-loop configuration (A) in a graft preparation station and (B) freestanding.
Figure 2.
Quadrupled soft tissue graft showing the passage of the suture tape augmentation (white arrows) deep to the cerclage stitches and out through the tibial end of the graft separated to each side of the graft. The femoral suspensory-fixation suture loop (black arrows) and the tibial suspensory loop (yellow arrows) are shown exiting the graft and secured in the prep station.
The cured resin ends of the tibial and femoral shafts were then secured in a custom rig with an intra-articular distance of 30 mm between the ACL femoral and tibial footprints at 90° of knee flexion.
ACL Reconstruction
The knee specimens were split into 2 groups of 10. The 2 largest specimens were prepared with 11-mm grafts. Twelve knees were reconstructed by 10.5-mm grafts, and a 10-mm graft was utilized in the 6 smallest specimens.
Retrograde femoral and tibial tunnels were created using a pin with a deployable blade. Femoral and tibial ACL aiming guides were placed at the center of the ACL footprints. The guide angles were set to allow for 20- to 25-mm tunnels with a cortical bridge of 7 mm. Tunnel diameters were reamed according to the allograft diameter of 10 mm, 10.5 mm, or 11 mm of the graft chosen for the specimen. After the retrograde cutting device was removed, a passing suture was introduced through the guide, delivering a loop into the joint for later graft passage.
An all-inside technique described by Lubowitz et al 20 was used for the reconstructions. The prepared graft was first drawn into the femoral tunnel by the passing suture loop and then the suspensory button was flipped on the lateral cortex. The sutures passing through the adjustable-loop device button were alternately tensioned until the graft construct was fully seated in the femoral socket.
The sutures of the tibial side of the graft were delivered through the tibial tunnel by the loop of the passing suture. The ends of the graft sutures were placed through a suspensory button. The knee was then placed at full extension, and the graft suture ends were alternately tensioned and tightened on the tibial and femoral sides to remove slack from the graft with at least 20 mm of graft in each socket. The femoral-side sutures were tied over the button with a surgeon’s knot and 4 alternating half hitches in all specimens. The tibial sutures of all specimens were tied over the button in the same fashion. This technique was chosen in an attempt to avoid any elongation of the initial adjustable-loop construct, as found by Noonan et al 28 (Figure 3).
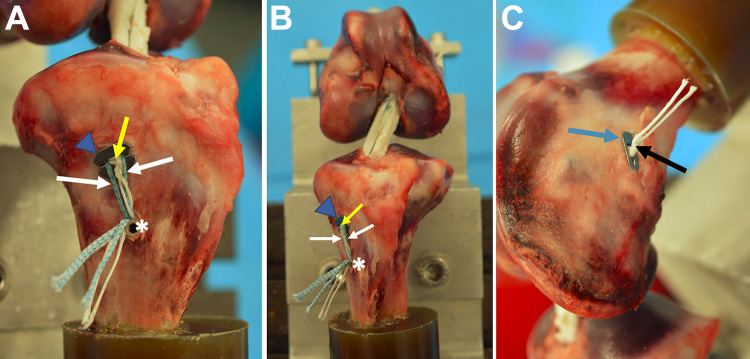
Figure 3.
(A and B) Left knee specimen demonstrating anterior cruciate ligament reconstruction soft tissue graft with tibial suspensory-fixation button (blue triangles) and tibial suspensory-fixation loop suture (yellow arrows) without suture tape augmentation. (C) Femoral suspensory-fixation button (blue arrow) and femoral suspensory-fixation loop suture (black arrow).
Test specimens with augmentation had the suture tape internal brace ends passed through the tibial socket independent of the suspensory button sutures. These suture ends were placed through the tibial button but peripherally to the suspensory sutures in an attempt to not trap the sutures between the button and the tibia. The suture tape ends and the suspensory button sutures were passed through a 4.75-mm biocomposite anchor (SwiveLock; Arthrex). An awl was used 15 mm distal to the tibial exit of the sutures to create a pilot hole that was then tapped for delivery of the anchor. The suture tape was tensioned independently of the suspensory button system sutures with a hemostat under the suture tape ends during the delivery of the anchor into the tibia to avoid overtightening to allow for a small amount of slack compared with the graft tension (Figure 4).
Figure 4.
(A and B) Left knee specimen demonstrating anterior cruciate ligament reconstruction soft tissue graft with tibial suspensory-fixation button (blue triangle) and tibial suspensory-fixation loop suture (yellow arrows) with suture tape augmentation (white arrows) and suspensory-loop sutures independently secured to the tibia with biocomposite suture anchor (asterisk). (C) Femoral suspensory-fixation button (blue arrow) and femoral suspensory-fixation loop suture (black arrow).
Biomechanical Testing
Tensile mechanical testing was performed using an E10000 Instron ElectroPuls Testing Machine (Instron), with a 10-kN load cell attached to the crosshead. The specimens were positioned in the testing machine with 30° of knee flexion, with an initial preload of 5 N applied by the actuator to avoid initiating mechanical testing in a slack condition (Figure 5). The testing protocols were performed as previously demonstrated by Walsh et al. 38 Specimens were preconditioned for 10 sinusoidal cycles at 1 Hz, between 10 and 50 N. Preconditioning was followed by a single-cycle loading to 250 N. Sinusoidal cyclic loading of the specimens was then conducted for 500 cycles, between 50 and 250 N, at 1 Hz. This was followed by a single-cycle final load to failure at 20 mm/min. The full testing protocols were modeled after Smith et al 35 and Chang et al. 8
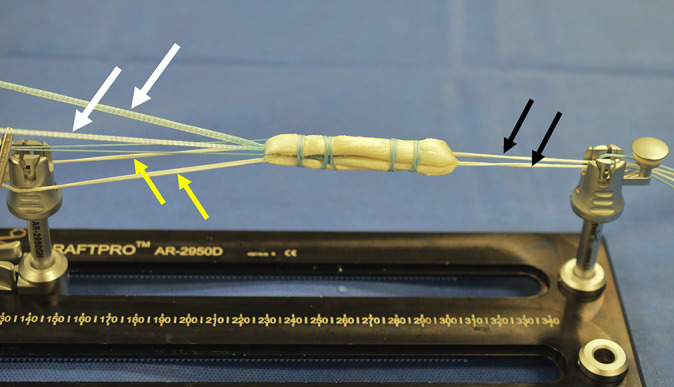
Figure 5.

Testing rig setup with suture tape–augmented left knee specimen shown.
Cyclic displacement, yield, and ultimate loads were measured directly from the load-displacement curves generated using OriginPro Version 9.1 software (OriginLab). Cyclic displacement was measured as the change in position from the end of the precycling at 50 N to the valley of the 500th cycle at 250 N. The 500 cycles are more than adequate to test the specimens, as Ahmad et al 2 and later Kleweno et al 17 showed that the largest displacement of grafts is found within the first 100 cycles. Stiffness was measured from the slope of the linear portion of the load-displacement curve immediately after cyclic loading. The mode of graft failure was also recorded for each specimen.
Statistical Analysis
Suture tape reinforcement was noted to be the independent variable. The Shapiro-Wilk test was utilized to demonstrate that the data were normally distributed. Equal variance of the groups was determined by the Brown-Forsythe test. Differences in the means of the outcome measures were the dependent variables of the 2 study groups and were compared using the Student t test, with a significance level of P < .05.
Results
All results are summarized in Table 1. The testing showed a statistically significant increase in ultimate load by 22% in the reinforced specimens (P = .008). The mean ± SD ultimate loads were 921 ± 180 N for augmented specimens and 717 ± 122 N for those without suture tape. The largest ultimate load in an augmented specimen was 1134 N in a 10.5-mm augmented graft. The largest ultimate load in a nonaugmented specimen was 907 N, also in a 10.5-mm graft.
Table 1.
Results of Biomechanical Graft Testing a
| Specimen | Side | Graft Size, mm | Ultimate Load, N | Yield Load, N | Stiffness, N/mm | Cyclic Disp, mm | Mode of Failure |
|---|---|---|---|---|---|---|---|
| Graft Alone | |||||||
| 1 | R | 10.5 | 907 | 830 | 132 | 5.1 | Suture failure at tibial button |
| 2 | R | 11.0 | 597 | 534 | 122 | 5.3 | Button pulled through tibia |
| 3 | R | 10.0 | 520 | 520 | 125 | 7.8 | Graft tore at cerclage sutures |
| 4 | L | 10.0 | 721 | 314 | 146 | 5.1 | Suture failure at tibial button |
| 5 | R | 10.0 | 653 | 653 | 137 | 7.3 | Button pulled through tibia |
| 6 | R | 10.5 | 752 | 752 | 86 | 7.9 | Graft tore at cerclage sutures |
| 7 | R | 10.5 | 844 | 781 | 148 | 3.9 | Graft tore at cerclage sutures |
| 8 | R | 10.5 | 806 | 531 | 139 | 4.1 | Suture failure at tibial button |
| 9 | R | 10.5 | 761 | 600 | 144 | 5.1 | Button pulled through tibia |
| 10 | L | 10.5 | 604 | 507 | 144 | 6.3 | Button pulled through tibia |
| Mean ± SD | — | 10.4 ± 0.3 | 717 ± 122 | 602 ± 155 | 132 ± 18 | 5.8 ± 1.5 | |
| Graft With Suture Tape Internal Brace Augmentation | |||||||
| 1 | R | 10.5 | 572 | 572 | 134 | 4.6 | Button pulled through tibia |
| 2 | R | 11.0 | 870 | 643 | 156 | 3.3 | Button pulled through tibia |
| 3 | R | 10.0 | 1124 | 1103 | 150 | 3.4 | Button broke at tibia |
| 4 | L | 10.0 | 890 | 835 | 133 | 3.8 | Button pulled through tibia |
| 5 | R | 10.0 | 1042 | 1022 | 143 | 4.8 | Graft tore at cerclage sutures |
| 6 | R | 10.5 | 788 | 495 | 123 | 3.6 | Button pulled through tibia |
| 7 | R | 10.5 | 1134 | 744 | 121 | 4.0 | Button broke at tibia |
| 8 | R | 10.5 | 1105 | 1015 | 110 | 4.9 | Button broke at tibia |
| 9 | R | 10.5 | 860 | 860 | 134 | 3.1 | Button pulled through tibia |
| 10 | L | 10.5 | 822 | 789 | 158 | 3.4 | Button pulled through tibia |
| Mean ± SD | — | 10.4 ± 0.3 | 921 ± 180 | 808 ± 201 | 136 ± 16 | 3.9 ± 0.7 | |
| P value, t test | — | — | .008 | .020 | .617 | .001 | |
a Bolding indicates statistically significant difference between graft alone and graft with suture tape augmentation (P < .05). Disp, displacement; L, left; R, right. Dashes indicate no numerical value relevant for the outcome measurement.
Yield loads were significantly increased by 25% in the augmented internal brace group (P = .020). The mean yield load was 808 ± 201 N for augmented grafts and 602 ± 155 N for those without suture tape augmentation. The largest yield load of 1103 N was recorded in a 10-mm augmented graft. The largest yield load in a standard graft was found in a 10-mm graft specimen at 830 N.
Testing revealed a 33% decrease in cyclic displacement in the suture tape internal brace group compared with the group without suture tape. The mean ± SD elongation was 3.9 ± 0.7 mm with suture tape and 5.8 ± 1.5 mm without augmentation, providing a P = .001 value of significance. The 10.5-mm grafts experienced the least and most displacement, with a range of 3.9 to 7.9 mm in the control specimens versus 3.1 to 4.9 mm in the reinforced group.
There was no statistically significant difference in stiffness between the 2 groups. The mean ± SD augmented graft stiffness was 136 ± 16 N/mm, compared with 132 ± 18 N/mm for the group with only graft reconstruction (P = .617).
Graft Failure
While not measured as significant, there were 3 midsubstance graft failures in the group without augmentation and only 1 in the suture tape augmentation group. All other grafts failed at the tibia, and breakage of the suspensory button on the tibia was only seen in the augmented group. This type of failure was seen in 3 of the 9 remaining grafts. Tibia-sided graft construct failures also were noted by the button pulling through the cortex and into the tibial tunnel (6/10 augmented, 4/10 nonaugmented) or the sutures cutting through and tearing at the tibial button, resulting in a loss of fixation (0/10 augmented, 3/10 nonaugmented).
Discussion
The major findings from this study showed a significant increase in yield (25%; P = .020) and ultimate failure (22%; P = .008) loads in augmented ligament reconstructions compared with those without. Cyclic displacement significantly decreased by 33% (P = .001) in the group with suture tape compared with the group without suture tape. Similar results of significantly increased ultimate failure loads and decreased elongation of soft tissue and patellar BTB grafts with independent suture tape reinforcement have been demonstrated in other biomechanical studies. 4,24,34
A concern when using a synthetic suture tape augmentation technique with ACL reconstruction is the risk of overconstraining the joint and stress shielding the graft. This could lead to loss of knee motion or catastrophic failure if the graft does not experience loads to facilitate revascularization and remodeling under stresses the knee would normally experience. The graft was secured with the knee in full extension, and suture tape was secured to the tibia separately from the primary graft fixation to avoid these potential complications. The suture tape was also secured with the tip of a hemostat under it, allowing for a small amount of slack compared with the final graft tension. 33,34
Cyclic displacement was significantly decreased in the suture tape–reinforced grafts in this study. It was noted that the mean ± SD displacement was 3.9 ± 0.7 mm with suture tape, compared with 5.8 ± 1.5 mm without suture tape. This is greater than the 3.0-mm displacement accepted as the limit for graft failure based on KT-1000 testing. 10 It should be noted that KT-1000 testing is performed on knees with intact soft tissues, ligaments, tendons, and menisci, which can provide secondary restraint to displacement. The adjustable-loop devices were not retightened after the preconditioning of 10 sinusoidal cycles at 1 Hz, between 10 and 50 N. These preconditioning cycles simulate cycling of the knee during surgery. Multiple authors have shown initial loosening of adjustable-loop suspensory devices occurring in the stresses and cycling of the knee. This can be combatted by retightening of the devices after the initial cycling. 6,28,30,36 This may have been the cause for the displacement above 3.0 mm for all graft constructs. Since all the graft constructs were treated the same, the amount of displacement can still be analyzed for any significance between the 2 groups. Cyclic displacement was significantly decreased by 33% in the suture tape group. Smith et al 34 revealed similar findings of 31% decreased cyclic displacement when adding suture tape as an independent reinforcement of patellar BTB grafts. The tibia- and femur-sided fixation was the same in all of their specimens. The only variable was the addition of the suture tape to the construct and resulted in the 31% decreased elongation. 34
Suture tape reinforcement is proposed for accelerated rehabilitative programs to facilitate earlier return to activity by protecting the ligament reconstruction during the maturation period. 29 Surgical techniques are now well described for suture tape augmentation of acromioclavicular joint ligament reconstruction, 15 ulnar collateral ligament repairs, 12 and spring ligament 1 as well as modified Broström ankle ligament repair procedures. 22,23,43 Suture tape augmentation of extra-articular knee ligaments has been employed and met with clinical success. Such reinforcement of posteromedial corner, 21 medial collateral ligament, 13,21 medial patellofemoral ligament, 42 and ACL 22,32 repairs and reconstructions has been presented in the literature. Suture tape reinforcement has shown promising results in early return to activity in Broström ankle ligament repair procedures. 41
Bachmaier et al 4 provided biomechanical data of soft tissue ACL reconstruction grafts with independent suture tape reinforcement. A comparison was made between 8-mm and 9-mm grafts with suture tape reinforcement showing a synergistic load-sharing configuration. The suture tape acts as a secondary stabilizer to protect the soft tissue graft during elongation without overconstraining the graft construct. Smith et al 34 provided biomechanical evidence of maintained stiffness of ACL patellar BTB reconstructions. The results of the current study also did not show a statistically significant difference in stiffness (P = .617) between the augmented specimens and those without suture tape augmentation.
Limitations
This study has limitations common to biomechanical studies on cadaveric tissue. This was a time-zero biomechanical study performed using longitudinal force tension loads, which do not completely represent in vivo loads with rotational forces on grafts used for ACL reconstruction. Human tissues were not utilized, but porcine knees provided a bone density similar to human bone for the study. 5,27 Bovine extensor tendons were used instead of human semitendinosus tissue, but stiffness and failure loads have not shown statistically significant differences compared with the human tendons. 11 Some of the graft sizes utilized in this study may be larger than those most commonly used in soft tissue ACL reconstruction.
The specimens were also devoid of other soft tissues, such as joint capsule, ligaments, menisci, muscles, and tendons. This did not permit the simulation of specimens to react as they would with in vivo tissue, although it did remove structures that may have acted as secondary restraints, allowing us to provide testing data on only the reconstructive tissue, fixation, and augmentation when present.
The cyclic loading applied may have been nonphysiologic, as it was in a single direction without rotational forces, which may also lead to graft failure. The grafts were tested in a nonbiological milieu, which also does not have the ability to simulate ACL graft-to-bone healing. The adjustable-loop suspensory device may also perform differently than other graft fixation constructs.
Conclusion
The study results demonstrated that suture tape reinforcement of soft tissue grafts for ACL reconstruction significantly decreased cyclic displacement by 33% (1.9 mm; P = .001) while significantly increasing ultimate and yield loads by 22% (204 N; P = .008) and 25% (206 N; P = .020), respectively, without increasing graft construct stiffness during biomechanical testing.
Acknowledgment
The authors acknowledge Josh Karnes and John Konicek, MS, of Arthrex.
Footnotes
Final revision submitted November 12, 2021; accepted January 10, 2022.
One or more of the authors has declared the following potential conflict of interest or source of funding: E.D.W. has received education payments from Arthrex, MVP Orthopedics, and Smith & Nephew and hospitality payments from Medical Device Business Services. J.S. has received education payments from Arthrex and hospitality payments from Corin USA and Stryker. N.R. has received education payments from Arthrex and Fones Marketing Management and hospitality payments from Stryker. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was waived by the Orlando Regional Medical Center Institutional Review Board (reference No. 1052065 -1).
References
- 1. Acevedo JI, Vora A. Anatomic reconstruction of the spring ligament complex. Tech Foot Ankle Surg. 2014;13:89–93. [Google Scholar]
- 2. Ahmad CS, Gardner TR, Groh M, Arnouk J, Levine WN. Mechanical properties of soft tissue femoral fixation devices for anterior cruciate ligament reconstruction. Am J Sports Med. 2004;32:635–640. [DOI] [PubMed] [Google Scholar]
- 3. Arnoczky SP, Tarvin GB, Marshall JL. Anterior cruciate ligament replacement using patellar tendon. An evaluation of graft revascularization in the dog. J Bone Joint Surg Am. 1982;64:217–224. [PubMed] [Google Scholar]
- 4. Bachmaier S, Smith PA, Bley J, Wijdicks CA. Independent suture tape reinforcement of small and standard diameter grafts for anterior cruciate ligament reconstruction: a biomechanical full construct model. Arthroscopy. 2018;34:490–499. [DOI] [PubMed] [Google Scholar]
- 5. Barfield WR, Calandra JJ, Hayes M, et al. Comparison of immature porcine and human bone mineral density about the knee. Curr Orthop Pract. 2014;25:147–151. [Google Scholar]
- 6. Bedi A, Kovacevic D, Fox AJ, et al. Effect of early and delayed mechanical loading on tendon-to-bone healing after anterior cruciate ligament reconstruction. J Bone Joint Surg Am. 2010;92:2387–2401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bhatia S, Bell R, Frank RM, et al. Bony incorporation of soft tissue anterior cruciate ligament grafts in an animal model: autograft versus allograft with low-dose gamma irradiation. Am J Sports Med. 2012;40:1789–1798. [DOI] [PubMed] [Google Scholar]
- 8. Chang HC, Nyland J, Nawab A, Burden R, Caborn DN. Biomechanical comparison of the bioabsorbable RetroScrew system, BioScrew XtraLok with stress equalization tensioner, and 35-mm Delta Screws for tibialis anterior graft-tibial tunnel fixation in porcine tibiae. Am J Sports Med. 2005;33:1057–1064. [DOI] [PubMed] [Google Scholar]
- 9. Cook JL, Smith P, Stannard JP, et al. A canine arthroscopic anterior cruciate ligament reconstruction model for study of synthetic augmentation of tendon allografts. J Knee Surg. 2017;30:704–711. [DOI] [PubMed] [Google Scholar]
- 10. Daniel DM, Stone ML, Dobson BE, et al. Fate of the ACL-injured patient: a prospective outcome study. Am J Sports Med. 1994;22:632–644. [DOI] [PubMed] [Google Scholar]
- 11. Domnick C, Wieskotter B, Raschke MJ, et al. Evaluation of biomechanical properties: are porcine flexor tendons and bovine extensor tendons eligible surrogates for human tendons in in vitro studies? Arch Orthop Trauma Surg. 2016;136:1465–1471. [DOI] [PubMed] [Google Scholar]
- 12. Dugas JR, Walters BL, Beason DP, Fleisig GS, Chronister JE. Biomechanical comparison of ulnar collateral ligament repair with internal bracing versus modified Jobe reconstruction. Am J Sports Med. 2016;44:735–741. [DOI] [PubMed] [Google Scholar]
- 13. Gilmer BB, Crall T, DeLong J, et al. Biomechanical analysis of internal bracing for treatment of medial knee injuries. Orthopedics. 2016;39:e532–e537. [DOI] [PubMed] [Google Scholar]
- 14. Hussein M, van Eck CF, Cretnik A, Dinevski D, Fu FH. Prospective randomized clinical evaluation of conventional single-bundle, anatomic single-bundle, and anatomic double-bundle anterior cruciate ligament reconstruction: 281 cases with 3- to 5-year follow-up. Am J Sports Med. 2012;40:512–520. [DOI] [PubMed] [Google Scholar]
- 15. Izadpanah K, Jaeger M, Ogon P, Sudkamp NP, Maier D. Arthroscopically assisted reconstruction of acute acromioclavicular joint dislocations: anatomic AC ligament reconstruction with protective internal bracing—the “AC-RecoBridge” technique. Arthrosc Tech. 2015;4:e153–e161. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Kane S. Sample size calculator. Updated July 24, 2019. Accessed April 3, 2022. https://clincalc.com/Stats/SampleSize.aspx
- 17. Kleweno CP, Jacir AM, Gardner TR, Ahmad CS, Levine WN. Biomechanical evaluation of anterior cruciate ligament femoral fixation techniques. Am J Sports Med. 2009;37:339–345. [DOI] [PubMed] [Google Scholar]
- 18. Lawhorn KW, Howell SM. Scientific justification and technique for anterior cruciate ligament reconstruction using autogenous and allogeneic soft-tissue grafts. Orthop Clin North Am. 2003;34:19–30. [DOI] [PubMed] [Google Scholar]
- 19. Leys T, Salmon L, Waller A, Linklater J, Pinczewski L. Clinical results and risk factors for reinjury 15 years after anterior cruciate ligament reconstruction: a prospective study of hamstring and patellar tendon grafts. Am J Sports Med. 2012;40:595–605. [DOI] [PubMed] [Google Scholar]
- 20. Lubowitz JH, Amhad CH, Anderson K. All-inside anterior cruciate ligament graft-link technique: second-generation, no-incision anterior cruciate ligament reconstruction. Arthroscopy. 2011;27:717. [DOI] [PubMed] [Google Scholar]
- 21. Lubowitz JH, MacKay G, Gilmer B. Knee medial collateral ligament and posteromedial corner anatomic repair with internal bracing. Arthrosc Tech. 2014;3:e505–e508. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mackay GM, Blyth MJ, Anthony I, Hopper GP, Ribbans WJ. A review of ligament augmentation with the InternalBrace: the surgical principle is described for the lateral ankle ligament and ACL repair in particular, and a comprehensive review of other surgical applications and techniques is presented. Surg Technol Int. 2015;26:239–255. [PubMed] [Google Scholar]
- 23. Mackay GM, Ribbans WJ. The addition of an “internal brace” to augment the Broström technique for lateral ankle ligament instability. Tech Foot Ankle Surg. 2016;15(1):47–56. [Google Scholar]
- 24. Matava MJ, Koscso J, Melara L, Bogunovic L. Suture tape augmentation improves the biomechanical performance of bone-patellar tendon-bone grafts used for anterior cruciate ligament reconstruction. Arthroscopy. 2021;37:3335–3343. [DOI] [PubMed] [Google Scholar]
- 25. Mohtadi NG, Chan DS. A randomized clinical trial comparing patellar tendon, hamstring tendon, and double-bundle ACL reconstructions: patient-reported and clinical outcomes at 5-year follow-up. J Bone Joint Surg Am. 2019;101:949–960. [DOI] [PubMed] [Google Scholar]
- 26. Mohtadi NG, Chan DS, Dainty KN, Whelan DB. Patellar tendon versus hamstring tendon autograft for anterior cruciate ligament rupture in adults. Cochrane Database Syst Rev. 2011;9(9):CD005960. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Nagarkatti DG, McKeon BP, Donahue BS, Fulkerson JP. Mechanical evaluation of a soft tissue interference screw in free tendon anterior cruciate ligament graft fixation. Am J Sports Med. 2001;29:67–71. [DOI] [PubMed] [Google Scholar]
- 28. Noonan BC, Dines JS, Allen AA, Altchek DW, Bedi A. Biomechanical evaluation of an adjustable loop suspensory anterior cruciate ligament reconstruction fixation device: the value of retensioning and knot tying. Arthroscopy. 2016;32:2050–2059. [DOI] [PubMed] [Google Scholar]
- 29. Parkes CW, Leland DP, Levy BA, et al. Hamstring autograft anterior cruciate ligament reconstruction using an all-inside technique with and without independent suture tape reinforcement. Arthroscopy. 2021;37:609–616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Petre BM, Smith SD, Jansson KS, et al. Femoral cortical suspension devices for soft tissue anterior cruciate ligament reconstruction: a comparative biomechanical study. Am J Sports Med. 2013;41:416–422. [DOI] [PubMed] [Google Scholar]
- 31. Shino K, Inoue M, Horibe S, Nagano J, Ono K. Maturation of allograft tendons transplanted into the knee. An arthroscopic and histological study. J Bone Joint Surg Br. 1988;70:556–560. [DOI] [PubMed] [Google Scholar]
- 32. Smith JO, Yasen SK, Palmer HC, et al. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surg Sports Traumatol Arthrosc. 2016;24:1845–1851. [DOI] [PubMed] [Google Scholar]
- 33. Smith PA, Bley JA. Allograft anterior cruciate ligament reconstruction utilizing internal brace augmentation. Arthrosc Tech. 2016;5:e1143–e1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Smith PA, Bradley JP, Konicek J, Bley JA, Wijdicks CA. Independent suture tape internal brace reinforcement of bone--patellar tendon—bone allografts: biomechanical assessment in a full-ACL reconstruction laboratory model. J Knee Surg. 2020,33:1047–1054. [DOI] [PubMed] [Google Scholar]
- 35. Smith PA, DeBerardino TM. Tibial fixation properties of a continuous-loop ACL hamstring graft construct with suspensory fixation in porcine bone. J Knee Surg. 2015;28:506–512. [DOI] [PubMed] [Google Scholar]
- 36. Smith PA, Piepenbrink M, Smith SK, et al. Adjustable- versus fixed-loop devices for femoral fixation in ACL reconstruction: an in vitro full-construct biomechanical study of surgical technique-based tibial fixation and graft preparation. Orthop J Sports Med. 2018;6:2325967118768743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. van Eck CF, Limpisvasti O, ElAttrache NS. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. Am J Sports Med. 2018;46:2291–2298. [DOI] [PubMed] [Google Scholar]
- 38. Walsh MP, Wijdicks CA, Parker JB, Hapa O, LaPrade RF. A comparison between a retrograde interference screw, suture button, and combined fixation on the tibial side in an all-inside anterior cruciate ligament reconstruction: a biomechanical study in a porcine model. Am J Sports Med. 2009;37:160–167. [DOI] [PubMed] [Google Scholar]
- 39. West RV, Harner CD. Graft selection in anterior cruciate ligament reconstruction. J Am Acad Orthop Surg. 2005;13:197–207. [DOI] [PubMed] [Google Scholar]
- 40. Widner M, Dunleavy M, Lynch S. Outcomes following ACL reconstruction based on graft type: are all grafts equivalent? Curr Rev Musculoskel Med. 2019;12:460–465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Wittig U, Hohenberger G, Ornig M, et al. Improved outcome and earlier return to activity after suture tape augmentation versus Broström repair for chronic lateral ankle instability? A systematic review. Arthroscopy. 2021;38:597–608. [DOI] [PubMed] [Google Scholar]
- 42. Xie G, Zhao J, Huangfu X, He Y. Medial patellofemoral ligament reconstruction using semitendinosus tendons: polyester suture augmentation versus nonaugmentation. Am J Sports Med. 2012;40:1365–1374. [DOI] [PubMed] [Google Scholar]
- 43. Yoo JS, Yang EA. Clinical results of an arthroscopic modified Broström operation with and without an internal brace. J Orthop Traumatol. 2016;17:353–360. [DOI] [PMC free article] [PubMed] [Google Scholar]