Objective:
This study aimed to characterize changes in firearm injuries at 5 level 1 trauma centers in Northern California in the 12 months following the start of the COVID-19 pandemic compared with the preceding 4 years, accounting for regional variations and seasonal trends.
Summary and Background Data:
Increased firearm injuries have been reported during the early peaks of the COVID-19 pandemic despite shelter-in-place restrictions. However, these data are overwhelmingly from singlecenter studies, during the initial phase of the pandemic prior to lifting of shelter-in-place restrictions, or do not account for seasonal trends.
Methods:
An interrupted time-series analysis (ITSA) of all firearm injuries presenting to 5 adult level 1 trauma centers in Northern California was performed (January 2016to February 2021). ITSA modeled the association of the onset of the COVID-19 pandemic (March 2020) with monthly firearm injuries using the ordinary least-squares method, included month indicators to adjust for seasonality, and specified lags of up to 12 months to account for autocorrelation.
Results:
Prior to the start of COVID-19, firearm injuries averaged (±SD) of 86 (±16) and were decreasing by 0.5/month (P < 0.01). The start of COVID- 19 (March 2020) was associated with an alarming increase of 39 firearm injuries/month (P < 0.01) followed by an ongoing rise of 3.5/mo (P < 0.01). This resulted in an average of 130 (±26) firearm injuries/month during the COVID-19 period and included 8 of the 10 highest monthly firearm injury rates in the past 5 years.
Conclusions:
These data highlight an alarming escalation in firearm injuries in the 12 months following the onset of the COVID-19 pandemic in Northern California. Additional studies and resources are needed to better understand and address this parallel public health crisis.
Keywords: trauma, COVID-19, Interrupted Time Series Analysis, Gun Violence, pandemics
Escalations in firearm injuries have been reported since the start of the coronavirus disease 2019 (COVID-19) pandemic, concurrent with shelter-in-place restrictions.1–3 Possible contributing and mediating factors include increased economic stress, social isolation, and increased firearm purchases during the pandemic.4–6 However, knowledge of regional variation and appropriate accounting for seasonal trends in firearm injury rates is needed to better contextualize the observed firearm injury increases. Additionally, it is not known whether the increase in firearm injuries has subsided with the lifting of shelter-in-place restrictions or with the decrease in COVID- 19 cases after the summer and winter surges in mid- and late-2020. We conducted an interrupted time-series analysis (ITSA) of all firearm injuries at 5 level 1 trauma centers in Northern California through the summer and winter peaks of the COVID-19 pandemic to highlight ongoing and future demands for injury prevention efforts during the pandemic.
METHODS
A multicenter retrospective study of all firearm injuries included in the trauma registries at 5 American College of Surgeons verified level-1 trauma centers in Northern California (CA) (January 2016 to February 2021) was performed (Zuckerberg San Francisco General Hospital [UCSF], San Francisco, CA; Highland Hospital [Highland], Oakland, CA; Stanford Health Care Medical Center [Stanford], Palo Alto, CA; University of California at Davis Medical Center [UC-Davis], Sacramento, CA; Community Regional Medical Center [CRMC], Fresno, CA). ITSA modeled the association of the COVID-19 pandemic onset (March 2020) with firearm injuries using the ordinary least-squares method.7 Temporal autocorrelation, or the tendency of data points close in time to be similar in value, is common in time-series data and can lead to underestimation of standard errors if not addressed. Correlated measurements of the outcome may occur across multiple consecutive months due to numerous factors including seasonality. We identified that statistically significant autocorrelation was present in the monthly firearm injury time series at a lag of 12 months, based on the Cumby- Huizinga test for autocorrelation.7 To account for temporal autocorrelation, our ITSA model included the following features: 1) NeweyWest standard errors allowing for temporal autocorrelation up to 12 lags, and 2) month indicator terms to account for seasonality. To examine regional variation, we additionally performed ITSA for each site individually. Total COVID-19 hospitalizations in the 5 counties (San Francisco, Santa Clara, Alameda, Sacramento, and Fresno) included in the catchment areas of the trauma centers were aggregated by month from publicly available California Department of Public Health data.8
RESULTS
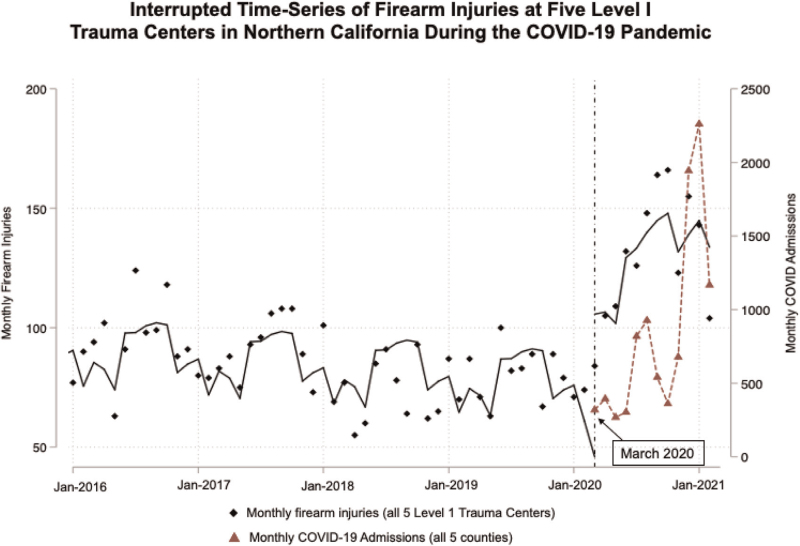
Prior to the COVID-19 pandemic, there was an average (±SD) of 86 (±16) firearm injuries/mo across all centers which was gradually declining by 0.5 firearm injuries/month (P < 0.01, Fig. 1 and Table 1). In March 2020, there was a large stepwise increase of 39 monthly firearm injuries (P < 0.01), followed by an ongoing increase of 3.5 additional firearm injuries/mo from March 2020 to February 2021 (P < 0.01, Fig. 1 and Table 1). The average rate of firearm injuries was 130 (±26)/mo during the pandemic which included 8 of the 10 highest monthly firearm injury rates in the past 5 years (Fig. 1). The trends were not uniform across sites, although no site experienced a decline in firearm injuries: UC-Davis, Highland, and CRMC had initial increases in March 2020 of 7.5, 11.1, and 17.1 more firearm injuries respectively (all P < 0.01), followed by stable (for UC-Davis and CRMC) or rising trends (Highland) (Supplemental Table 1); UCSF and Stanford had no significant initial change, but did have gradual and significant increases over the study period by 1.2 and 0.4 firearm injuries/mo respectively (both P < 0.01).
FIGURE 1.
Interrupted time-series analysis of firearm injuries at five level I trauma centers in Northern California during the COVID- 19 Pandemic. Black diamonds are values for number of monthly firearm injuries across all 5 sites, solid black line represents the modeled trend for monthly firearm injuries based on the interrupted time series model. Red triangles (connected by dotted red line) = monthly cumulative COVID-19 hospital admissions across all 5 Northern California counties in which trauma centers are located. Pre-pandemic, there were 86 (±16) firearm injuries/mo with a slight downtrend over time (by 0.5/mo, P < 0.01) and expected seasonal fluctuation. This was followed by a significant level-shift up in firearm injuries in March 2020 associated with the regional onset of the COVID-19 pandemic (by 39.4/mo, P < 0.01), followed by continued significant uptrend of 3.5 more firearm injuries/ mo (P < 0.01), with an overall average of 130 (±26) firearm injuries/mo during the pandemic.
TABLE 1.
Interrupted Time-Series Analysis of Firearm Injuries—All Sites in aggregate
| Coefficient | NW Std. Error | CI-Low | CI-High | P-Value | |
| Pre-COVID-19 trend (Jan 2016–Feb 2020) | –0.47 | 0.09 | <0.01 | –0.65 | –0.28 |
| Level shift at start of COVID-19 (Mar 2020) | 39.37 | 9.51 | <0.01 | 20.24 | 58.50 |
| Post-COVID-19 trend (Mar 2020–February 2021) | 3.48 | 1.30 | 0.01 | 0.87 | 6.09 |
Coefficients represent estimates for change in number of firearm injuries per month.
CI indicates 95% confidence interval; NW Std Error, Newey West Standard Errors.
All estimates adjusted for month of the year (not shown) to account for seasonal trends and lags of up to 12 months.
DISCUSSION
These data highlight an alarming rise in firearm injuries in Northern California since the start of the COVID-19 pandemic to levels not seen in the prior 4 years. Although we included all firearm injuries at each center, the vast majority were related to assaults, suggesting these trends are driven by interpersonal violence rather than accidental firearm discharges or self-harm. The widespread increases in economic and psychological stress due to job loss and social isolation during COVID-19 may contribute to increased interpersonal and domestic violence.5 This is congruent with a large survey among Californians in July 2020 that identified significant increases in self-reported concerns regarding interpersonal and domestic violence, as well as increased firearm acquisitions during the pandemic.4 Firearm purchases significantly increased across the United States above historical averages based on an analysis of data through July of 2020.6 However, this was not clearly linked to increases in firearm violence at the state level, and California firearm purchases increased only modestly compared to other states.6
Data from prior periods of increased economic hardship such as the Great Recession have also been linked to increased interpersonal violence and violent crime.9,10 However, more work is needed to better understand the complex socio-political and economic factors that may contribute to the observed trends in firearm injuries during the COVID-19 pandemic. In addition to the stressors associated with the pandemic, 2020 was also marked by large-scale social and political unrest, particularly in the wake of the death of George Floyd in May of 2020. However, the spike in firearm injuries in Northern California reported here preceded these events by several months (March of 2020) and is consistent with data from other single-center studies.2,3 Better understanding of which subgroups are most affected by persistent interpersonal violence and the circumstances driving violent incidents during the pandemic would help inform violence prevention efforts during future waves of the pandemic. The leveling-off of firearm injuries in the last 3 months (December 2020 to February 2021; Fig. 1) of the study period may be an early sign of improvement, and correspond with a decline in COVID-19 hospitalizations, but firearm injury rates remain far above corresponding winter months during the pre-pandemic years.
This analysis has several important limitations, including that the findings may not reflect trends in other geographic regions, and inability to distinguish between the impacts of the pandemic itself versus pandemic responses, such as shelter-in-place policies and economic downturns. The ITSA model provides linear estimates which can only approximate the nonlinear real-world trends in firearm injuries. Further, our data only include patients presenting to trauma centers included in this study, though this accounts for 5 out of 6 level 1 trauma centers in Northern California. In summary, we identified a concerning and persistent rise in firearm injuries in the 12months following the onset of the COVID-19 pandemic in Northern California, underscoring an escalating parallel public health crisis. Future studies are needed to better understand the mechanisms driving this observed escalation in firearm violence to guide mitigation efforts.
ACKNOWLEDGMENTS
The authors thank the UCSF Clinical and Translational Science Institute for supporting this work through the COVID-19 Rapid Response Pilot Grant, Lilian Li RHIT, and Sue Peterson RN MSN.
Supplementary Material
Footnotes
Dr. L.Z.K. is supported by NIH 1K23GM13O892-O1 and UL1 TR001872; Drs. A.M.K. and Z.A.M. are supported by UL1 TR001872. Dr. E.C.M. is supported by K99AA028256.
Northern California Research Consortium for Trauma and Acute Care Surgery Study Group: Carl A Beyer, MD (Department of Surgery, Penn Presbyterian Medical Center, Philadelphia, PA), Shannon L. Castle, MD (Department of Surgery, Valley Children's Healthcare, Madera, CA), Rachel C. Dirks, PhD (Department of Surgery, University of California San Francisco Fresno, Fresno, CA), Jessica Dzubnar, MD (Department of Surgery, University of California San Francisco-East Bay, Oakland, CA), Joseph M. Galante, MD (Department of Surgery, University of California Davis Medical Center, Sacramento, CA), Aaron E. Kornblith, MD (Department of Emergency Medicine, University of California, San Francisco; San Francisco, CA), Ellicott C. Matthay, PhD (Center for Health and Community, University of California, San Francisco; San Francisco, CA), Jung Gi Min, MD (Department of Surgery, Stanford University, Stanford, CA), Christopher Newton, MD, FACS (Department of Surgery, University of California San Francisco Benioff Children's Hospital Oakland, Oakland, CA), Brenda Nunez Garcia, BA (Department of Surgery, Zuckerberg San Francisco General Hospital and the University of California, San Francisco; San Francisco, California), David A. Spain, MD (Department of Surgery, Stanford University, Stanford, CA), Lakshika Tennakoon, MSc, MPhil (Department of Surgery, Stanford University, Stanford, CA).
The authors report no conflicts of interest.
Supplemental digital content is available for this article.
Contributor Information
Collaborators: Northern California Research Consortium for Trauma & Acute Care Surgery Study Group
REFERENCES
- 1.Hatchimonji JS, Swendiman RA, Seamon MJ, et al. Trauma does not quarantine: violence during the COVID-19 Pandemic. Ann Surg 2020; 272:e53–e54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Sutherland M, McKenney M, Elkbuli A. Gun violence during COVID-19 pandemic: paradoxical trends in New York City, Chicago, Los Angeles and Baltimore. Am J Emerg Med 2021; 39:225–226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Beard JH, Jacoby SF, Maher Z, et al. Changes in Shooting Incidence in Philadelphia, Pennsylvania, Between March and November 2020. JAMA 2021; 325:1327–1328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kravitz-Wirtz N, Aubel A, Schleimer J, et al. Public concern about violence, firearms, and the COVID-19 Pandemic in California. JAMA Netw Open 2021; 4:e2033484. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Boserup B, McKenney M, Elkbuli A. Alarming trends in US domestic violence during the COVID-19 pandemic. Am J Emerg Med 2020; 38:2753–2755. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Schleimer JP, McCort CD, Shev AB, et al. Firearm purchasing and firearm violence during the coronavirus pandemic in the United States: a crosssectional study. Inj Epidemiol 2021; 8:43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Linden A. Conducting interrupted time-series analysis for single and multiple group comparisons. Stata J 2015; 15:480–500. [Google Scholar]
- 8.COVID-19 State Dashboard; 2020. Available at: https://covid19.ca.gov/state-dashboard/. Accessed June 1, 2021. [Google Scholar]
- 9.Schneider D, Harknett K, McLanahan S. Intimate partner violence in the Great Recession. Demography 2016; 53:471–505. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Janet L, Lauritsen KH. Violent victimization among males and economic conditions. Criminal Public Policy 2010; 9:665–692. [Google Scholar]