Abstract
Stress associated with diabetes makes managing diabetes harder. We investigated whether mindfulness-based stress reduction (MBSR) could reduce diabetes distress and improve management. We recruited 38 participants to complete an MBSR program. Surveys and lab values were completed at baseline and post-intervention. Participants showed significant improvement in diabetes-related distress (Cohen’s d, −.71, p<.002), psychosocial self-efficacy (Cohen’s d .80, p<.001), and glucose control (Cohen’s d −.79, p<.001). Significant improvements in depression, anxiety, stress, coping, self-compassion, and social support were also found. These results suggest that MBSR may offer an effective method for helping people better self-manage their diabetes and improve mental health.
Keywords: diabetes distress, mindfulness, stress reduction, diabetes management, MBSR
Type 2 diabetes mellitus (DM) is a chronic, progressive condition affecting 29.1 million adults in the United States, about 9.3% of the adult population, with prevalence expected to increase dramatically in the coming decade (Centers for Disease Control and Prevention, 2014). DM is a serious metabolic disorder characterized by high levels of blood glucose due to improper production or use of insulin related to both genetic and environmental factors. It reduces life expectancy by more than 6 years, quality of life by 20–30%, and substantially increases costs of medical care (Tan, Lindquist, Rush, & O'Connor, 2002). Diabetes also disproportionately affects minority communities (Kanaya et al., 2011; Karter et al., 2013; Mayeda et al., 2013; Naranjo, Hessler, Deol, & Chesla, 2012). Optimal care for DM is achieved through good self-management that includes glucose monitoring, medication management, healthy eating, and regular physical activity which reduces the risks of serious complications (Clinical Evidence, 2001; Gaede, Lund-Andersen, Parving, & Pedersen, 2008). The rigorous daily self- management needs however, can also result in chronic stress including diabetes-related distress from the significant changes required in diet and lifestyle that affect self-perception, self-esteem and relationships with family and friends (Browne, Ventura, Mosely, & Speight, 2013; Stoop et al., 2014).
Chronic stress is associated with numerous deleterious effects on health and well-being, including poorer physical health, compromised immune function, increased mortality, social isolation, depression, anxiety and poor quality of life (R. J. Anderson, Freedland, Clouse, & Lustman, 2001; Nomura et al., 2000; Sapolsky, 2004). It sets off a cascade of physical effects including increases in hormones such as adrenaline, cortisol, and epinephrine leading to increased glucose and blood pressure as the body’s flight or fight system is activated (Faulenbach et al., 2012; Nomura et al., 2000; Peyrot, McMurry, & Kruger, 1999; Sapolsky, 2004; Weijman et al., 2005). In this way, chronic stress not only increases the risk of poor quality of life, depression, and anxiety but also increases blood glucose and blood pressure levels making self-management and optimal diabetes care far more difficult and less likely.
Chronic stress directly associated with diabetes includes what has been termed diabetes-related distress. Diabetes-related distress has been defined as including diabetes regimen distress, emotional distress, physician-related distress, and interpersonal distress (Wardian & Sun, 2014). It has been linked to poor glycemic control and treatment adherence and is associated with an increased risk of mental health disorders such as depression (Fisher, Glasgow, & Strycker, 2010; Gonzalez, Shreck, Psaros, & Safren, 2014). Interventions to help people manage diabetes-related distress have focused primarily on stress management techniques, including relaxation and biofeedback (Esch, Fricchione, & Stefano, 2003; McGinnis, McGrady, Cox, & Grower-Dowling, 2005; McGrady & Horner, 1999; Surwit et al., 2002). Stress reduction techniques however, have shown mixed results, with biofeedback demonstrating better effects in short-term improvement in glucose control (measured as HemoglobinA1c level).
Increasingly people with diabetes are exploring complementary and integrative practices, as defined by the National Center for Complementary and Integrative Health, for addressing diabetes-related distress including: yoga (Yang et al., 2011), Qigong and T’ai chi (Gates & Mick, 2010; Liu, Miller, Burton, Chang, & Brown, 2011; Song, Ahn, Roberts, Lee, & Ahn, 2009), meditation (Callaghan, 2008; Teixeira, 2010), guided imagery (Wichowski & Kubsch, 1999), Acceptance and Commitment Therapy (ACT) (Gregg, Callaghan, Hayes, & Glenn-Lawson, 2007), and Mindfulness-Based Stress Reduction (Rosenzweig et al., 2007; Whitebird, Kreitzer, & O'Connor, 2009). Research on these complementary practices ranges from uncontrolled exploratory studies (Rosenzweig et al., 2007; Wichowski & Kubsch, 1999) to controlled randomized controlled trials (Gregg et al., 2007; Liu et al., 2011).
Mindfulness-based stress reduction (MBSR) is a stress-reduction technique that includes elements of these integrative approaches. Developed by Jon Kabat-Zinn in the late 1980’s at the University of Massachusetts Medical Center for patients with chronic pain, it is a standardized group-based program that is 8-weeks long and focuses on reducing stress and managing difficult emotions through training in mindfulness (Kabat-Zinn, 1990). The practice of MBSR focuses on present moment mindfulness, nonjudgmental awareness and acceptance of experience, both internal and external, with a stance of openness and curiosity (Bishop, 2002; Chambers, Gullone, & Allen, 2009). Chambers et al. (2009) note that mindfulness may facilitate the development of metacognitive insight, where thoughts are perceived to be insubstantial and transient events rather than accurate representations of reality, a process known as decentering. MBSR training teaches participants to become more aware of their thoughts and feelings so they can change their relationship to them. This is accomplished through accepting thoughts and feelings as they arise without judgement and letting go them, then refocusing attention to an object of focus, most commonly the breath (Bishop, 2002). MBSR includes a formal meditation practice done though sitting or standing meditation and mindful movement, it also includes guided meditations such as scanning of the body. Daily practice of MBSR includes incorporating mindfulness into one’s everyday life (Cullen, 2011).
The use of MBSR has been studied for decreasing symptoms in a wide range of medical conditions and improving quality of life. It has been used with cancer patients and for managing symptoms, and improving quality of life following solid organ transplant (Gross et al., 2004; Gross et al., 2010; Kreitzer, Gross, Ye, Russas, & Treesak, 2005; Ledesma & Kumano, 2008; Lengacher et al., 2008). It has also been studied in patients with pain, rheumatoid arthritis and fibromyalgia (Grossman, Tiefenthaler-Gilmer, Raysz, & Kesper, 2007; McCracken, Gauntlett-Gilbert, & Vowles, 2007; Pradhan et al., 2007; Rosenzweig et al., 2010). We studied its use for decreasing stress and burden in caregivers of people with dementia (Whitebird et al., 2012; Whitebird et al., 2011). In aggregate, studies of MBSR have found decreases in medically related symptoms and improved functioning including reduced stress, anxiety and depression (Astin, Shapiro, Eisenberg, & Forys, 2003; Fjorback, Arendt, Ørnbøl, Fink, & Walach, 2011; Grossman, Niemann, Schmidt, & Walach, 2004; Hofmann, Sawyer, Witt, & Oh, 2010).
Studies of MBSR have also begun to look at its potential for people with diabetes (Whitebird et al., 2009). Hartmann and colleagues (2012) looked at the use of an adapted version of MBSR using an acceptance and mindfulness-based group intervention to reduce psychosocial distress and decrease the progression of nephropathy in people at high risk for diabetes complications. Results showed a reduction in psychosocial distress, although no significant differences in nephropathy. Rosenzweig et al. (2007) in small study of MBSR at an academic medical center in 14 patients with diabetes, looked at glycemic control in addition to stress-related psychological symptoms, weight and blood-pressure at one month follow-up. While the study found decreases in HbA1c, blood pressure and stress related psychological symptoms, only 11 of the 14 people completed the study and participant’s initial HbA1c were restricted to being within >6.5 and <8.5, indicating relatively well-controlled diabetes at the start of the study. Considering the few studies of MBSR in people with diabetes, and the improvements that MBSR has shown for people with other chronic conditions, we were interested in the potential of a community-based MBSR program to improve diabetes management and reduce stress related specifically to diabetes, especially for those with poor diabetes control. The purpose of the present study was to examine whether a community-based MBSR program can improve diabetes management by improving HbA1c values and decrease diabetes related-distress and improve anxiety and depression in people with Type 2 diabetes.
Methods
Participants
The study Managing Diabetes Mindfully, was a one-arm pilot study that was conducted from 2012 to 2013 in the upper Midwest at a nonprofit research center affiliated with a mixed-model health plan. Participants were members of the health plan and were eligible to participate in the study if they had Type 2 diabetes and had two Hemoglobin (Hb)A1c values of ≥ 8.0% in the prior 16 months, with the most recent HbA1c > 8% in the prior 3 months. Eligibility criteria also included the ability to speak and read English (for course participation and to read the course materials), no history of mental illness or major depression and the ability to attend weekly classes. Potential participants were excluded if they had completed formal training in other mind body practices such as meditation, yoga, or tai chi within the prior year.
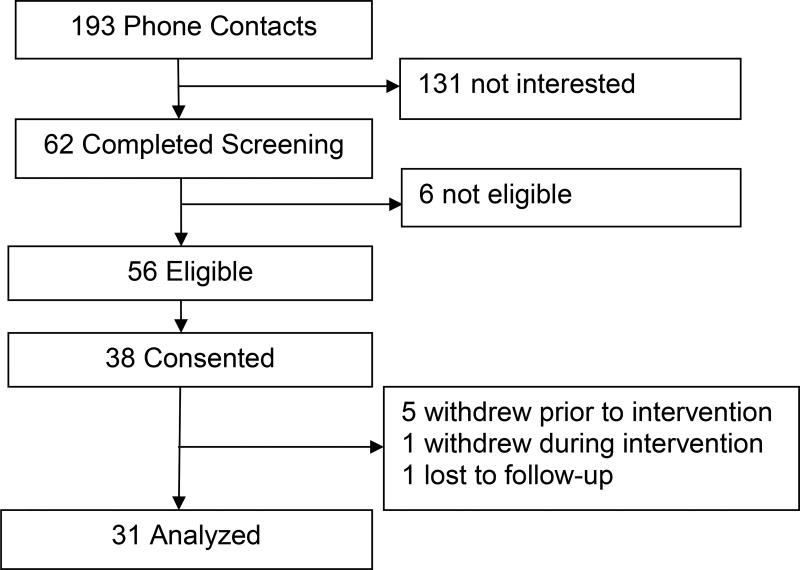
The study screened 193 people for potential participation, 56 of whom were eligible, and 38 who agreed to participate, were enrolled and consented to participate in the study (Figure 1). Our target recruitment goal was 30 participants; we over-recruited to address potential dropouts and loss to follow-up. Of the 38 participants, 6 withdrew prior to completing the intervention and 1 withdrew during the intervention; we had 1 loss to follow-up. Reasons for withdrawal included time conflicts, health, and anxiety. The study was reviewed and approved by the local Institutional Review Board.
Figure 1.
Participant Flow though the study.
Materials and Procedure
Participants were recruited to participate in the study through letter and telephone contact, they completed eligibility screening for participation at that time. Those interested in study participation met with the study coordinator where they received additional study information, completed their consent form, and received a yoga mat and blood pressure cuff. Participants also received a daily log to track their time in home practice course activities which included meditation and yoga, and their daily morning blood pressure. Participants filled out surveys prior to the start of the intervention and following completion, they also participated in an open-ended qualitative interview about their perceptions of their course participation.
Intervention
The study included participation in a community-based MBSR course that was offered through a Center affiliated with a state university program. Participants were enrolled in an MBSR course offered at a variety of locations in a metropolitan area. Course facilitators were trained using Jon Kabat-Zinn’s MBSR program and the course was conducted as described in his book Full Catastrophe Living (Kabat-Zinn, 1990). Participants received 8-weeks of program instruction in MBSR that included four forms of meditation (sitting, standing, walking and supine) and gentle Hatha yoga. Participants learned the skills of meditation from the instructor, guided and reinforced by an audio series (CD/MP3) for home practice. The eight sessions were 2.5 hours each week and included a one-day retreat was held between weeks 6 and 7 of the course. Participants were encouraged to do at least one meditation practice 5–6 days per week for 20 minutes throughout course and to track their home practice in a daily log.
Measures
A study survey was used to collect information on participant demographics, stress, mental health, social support and diabetes-related distress and self-management. Lab values measuring Hemoglobin A1c and self-reported blood pressure were also collected.
Mental health
General mental health was measured using the Short-Form-12 Health Survey (SF-12) which provides composite scores of mental health (MCS-12). It has been used widely and demonstrates good reliability and validity (McDowell, 2006). Symptoms of depression were measured using the Patient Health Questionnaire (PHQ9), a widely-used clinical measure of depression demonstrating good validity and reliability. (Kroenke, Spitzer, & Williams, 2001; Kroenke, Spitzer, Williams, & Lowe, 2010). Anxiety was measured with the State-Trait Anxiety Inventory (STAI) - State Version Y subscale. The STAI is widely used clinical practice and research demonstrating internal consistency and validity (Spelberger, 1983).
Stress and coping
Stress was measured using the Perceived Stress Scale (PSS) 10-item version. This is a self-reported measure looking at previous month and the degree to which situations were considered stressful (S. Cohen, & Williamson, G., 1988; Cohen, Kamarck, & Mermelstein, 1983). Coping was measured the short-form version of the Coping Strategies Inventory (CPI-SF) which measures engaged and disengaged coping styles. The CSI-SF has been studied and found to have adequate validity and reliability for all scales (Addison et al., 2007).
Social support and self-compassion
Social support was measured using the Medical Outcomes Study (MOS) Social Support Survey. The scale covers four categories of support: emotional or informational support, positive social interaction, tangible support and affectionate support. The MOS social support survey has been extensively studied demonstrating good validity and reliability (McDowell, 2006). Self-compassion, which is associated with psychological well-being, was measured using the short-form of the Self-Compassion Scaled (SCS-SF) which has been shown in factorial validation to have good validity and reliability (Raes, Pommier, Neff, & Van Gucht, 2011).
Diabetes-related distress
Diabetes-related distress was measured using the Problem Areas In Diabetes Questionnaire (PAID). The PAID is a measure of diabetes distress developed by the Joslin Diabetes Center (Polonsky et al., 1995). It has been shown to have high internal reliability and to correlate with general theoretical constructs such as diabetes distress, diabetes self-care behaviors, diabetes coping, and health beliefs (Reddy, Wilhelm, & Campbell, 2013; Snoek, Pouwer, Welch, & Polonsky, 2000; Van Der Ven et al., 2003; Welch, Weinger, Anderson, & Polonsky, 2003).
Diabetes self-management and self-efficacy
Diabetes self-management and psychosocial self-efficacy was measured using the Diabetes Empowerment Scale (DES). The DES is a psychosocial measure that has been predictive of self-management and self-efficacy in diabetes health interventions (Lorig et al., 2001). The DES is a valid and reliable measure of overall diabetes-related psychosocial self-efficacy and self-management (R. M. Anderson, Fitzgerald, Gruppen, Funnell, & Oh, 2003; R. M. Anderson, Funnell, Fitzgerald, & Marrero, 2000). The DES is conceptually related to sense of control, a construct found to be enhanced by MBSR (Astin, 1997; Astin, Shapiro, Lee, & Shapiro, 1999).
Hemoglobin A1c (HbA1c)
HbA1c refers to glycated hemoglobin and provides a clinical picture of blood sugar levels over the prior 10–12 weeks. It is a standard clinical measure used to monitor glucose levels in the blood. Baseline HbA1c lab values were collected from medical records tied to in-person visits and follow-up HbA1c labs were also collected from in-person clinic visits between weeks 13–16 following intervention completion. This latter HbA1c test centered the test result (an average of the prior 3 months) at the end of course participation and in the first weeks following the course completion.
Statistical Analysis
Baseline characteristics and outcomes were descriptively analyzed including mean values ± standard deviation, or frequency distribution. Outcome measures were analyzed for departure of normality. Pre-post changes of outcome measures were evaluated using pair-wise t-test. Cohen-D Statistic (pre-post change divided by pre outcome measure standard deviation) were calculated to evaluate the size of the effect (J. Cohen, 1988; Kotrlik, 2003).
Results
Participants (n=31) in the study were 31 to 78 years of age with a mean age of 56 years. They were predominately non-Hispanic White (70%) women (67%), the majority of whom were married (62%) with some post-secondary education (Table 1). Adherence to the intervention included attendance at the eight weekly group meetings and the one-day retreat; group sessions had a mean adherence of 7.5 and the retreat .94, with a combined attendance of 8.0 sessions (Table 2). Participants did an average of 4.9 home practice sessions per week for an average of 35 minutes per session.
Table 1.
Characteristics of Study Participants
| Demographics | N=31 |
|---|---|
| Age M (SD) | 56.6(12.6) |
| Female N (%) | 21 (67.4) |
| Race N (%) | |
| White | 22 (71.0) |
| African American | 7 (22.6) |
| Other | 2 (6.5) |
| Hispanic N (%) | 2 (6.5) |
| Non-Hispanic white N (%) | 29 (93.5) |
| Marital status N (%) | |
| Married | 19 (62.3) |
| Never married | 7 (22.6) |
| Widowed, divorced, separated | 5 (16.1) |
| Education N (%) | |
| High school graduate | 3 (9.7) |
| Some post-secondary | 12 (38.7) |
| College graduate | 9 (29.0) |
| Graduate school | 7 (22.6) |
| Employment N (%) | |
| Employed | 17 (54.8) |
| Out of work/unable to work | 5 (16.1) |
| Student | 2 (6.5) |
| Retired/homemaker | 7 (22.6) |
Table 2.
Adherence to the Study Intervention
| Intervention Adherence | Mean ±-SD |
|---|---|
| Number of weekly sessions | 7.6± 0.72 |
| Attendance at Retreat/Wellness Day | 0.94±0.25 |
| Number of total sessions attended | 8.0 ±1.9 |
| Sessions per week of MBSR home practice, M (SD) | 5.0±2.6 |
| Minutes per session per week of MBSR home practice, M (SD) | 35.5 ±22.5 |
There were two patterns of outcomes that indicated support for the efficacy of MBSR in improving diabetes self-management and mental health. The first was observed for measures of diabetes-related distress and self-management, with participants showing significant improvements in pre-post measures (Table 3). There was a significant decrease in diabetes-related distress as measured by the PAID (Cohen’s d −.71, p<.002), and significant improvement in diabetes self-management as measured by HbA1c levels (Absolute change: −.79, Cohen’s d −.67, p<.001), and psycho-social self-efficacy as measured by the DES (Cohen’s d .80, p<.001).
Table 3.
Observed pre, post mean (SD) and Cohen-D of Hemoglobin A1C and Measures of Diabetes Management
| DM Management Outcome | PRE | POST | Cohen-D | P |
|---|---|---|---|---|
| Hemoglobin A1C | 9.2 (1.2) | 8.4 (1.3) | Absolute diff −.79 Cohen-D −0.67 | .0004 |
| Problem areas in diabetes scale (PAID) | 30.3 (2.7) | 18.3 (0.14) | −.71 | .002 |
| Diabetes engagement scale | 3.4 (0.14) | 4.1 (0.11) | .80 | <.001 |
The second pattern of support can be seen in measures of mental health (Table 4). Participants showed significant improvement in measures of pre-post change in perceived stress as measured by the PSS (Cohen’s d −.76, p<.001), decreases in depressive symptoms as measured by the PHQ9 (Cohen’s d −.62, p<.001), improvement in anxiety as measured by the STAI (Cohen’s d −.66, p<.001), and improvement in overall mental health as measured by the SF12 (Cohen’s d .69, p<.001). Improvement was also seen in measures of coping engagement as measured by the CSI (Cohen’s d .52, p<.001), social support as measured by the MOSS (Cohen’s d .38, p<.02) and self-compassion as measured by the SCS (Cohen’s d .33, p<.04).
Table 4.
Observed Mean (SD) of Mental and Behavioral Health Measures at PRE-POST, Cohen’s d for PRE-POST Difference, Significance of Simple Effects Test
| Mental Health/ Behavioral Measures |
PRE M (SD) |
POST M (SD) |
Range | d | P |
|---|---|---|---|---|---|
| Perceived stress (PSS) | 16.5 (1.0) | 11.7 (1.3) | (0–40) | −0.76 | .001 |
| Depression (PHQ9) | 7.7 (1.0) | 3.9 (0.9) | (0–27) | −0.62 | .001 |
| Anxiety (STAI) | 40.4 (2.2) | 31.4 (2.0) | (20–80) | −0.66 | .001 |
| Mental Health (MCS-12) | 46.1 (1.4) | 51.8 (1.1) | (0–100) | 0.69 | .001 |
| Social Support (MOSS) | 64.9 (4.3) | 74.91 (3.83) | (0–100) | 0.38 | .02 |
| Coping (CSI-engagement) | 25.3 (0.9) | 28.1 (0.8) | (8–40) | 0.52 | <.001 |
| Coping (CSI – disengagement) | 24.8 (0.8) | 23.5 (0.8) | (8–40) | −0.27 | .18 |
| Self-compassion (SCS) | 3.2 (0.1) | 3.4 (0.1) | (12–60) | 0.33 | .04 |
Discussion
There has been little study to date on the use of a community-based MBSR programs to improve diabetes-related distress, self-management and mental health in people with diabetes, especially for those with poorly-controlled diabetes. Participants in our study showed significant improvements in pre-post measures of diabetes-related distress, psychosocial self-efficacy and glucose control, all measures related to good diabetes self-management. Participants also showed significant improvement in measures of mental health including depression, anxiety, stress, coping, self-compassion and social support. The pre-post changes observed in this pilot study were large and significant and add to the literature on the benefits of community-based MBSR programs for people with diabetes. While the study design precludes causal inference, these results suggest that community-based MBSR programs may offer an effective method for helping people reduce diabetes-related distress, better self-manage their diabetes and improve their mental health.
How the practice of MBSR specifically affects diabetes self-management and mental health is not yet unclear. Prior research of MBSR with other chronic conditions has found improvements in medically-related symptoms and functioning, and decreases in stress, anxiety, and depression (Astin et al., 2003; Fjorback et al., 2011; Grossman et al., 2004; Hofmann et al., 2010). Certainly, improving the management of stress can have significant benefits to both physical and mental. Chronic stress can elevate blood glucose and blood pressure levels and interfere with diabetes self-management through both its physiological effects and psychosocial consequences such as anxiety and depression, which are known to be correlated with diabetes (R. J. Anderson et al., 2001; Faulenbach et al., 2012; Surwit & Schneider, 1993; Surwit, Schneider, & Feinglos, 1992; Surwit et al., 2002).
People with diabetes also experience psychosocial issues that are unique to their condition. Browne and colleagues (2013) for example, in their qualitative study of people with diabetes found that people experienced diabetes-related social stigma. They note that blame, shame and guilt are often associated with the condition due to its relationship to poor dietary habits and being overweight. In their study, people with diabetes described feeling judged and blamed by others for bringing the condition on themselves. Here the foundational features of MBSR, present-moment mindfulness and nonjudgmental awareness, may be significant factors in the beneficial effects on diabetes management.
Present-moment mindfulness has been found to have moderating and potentially protective effects against the harmful aspects of stress (Haenen, Nyklicek, van Son, Pop, & Pouwer, 2016; van Son et al., 2015; Whitebird et al., 2012). The practice of nonjudgmental awareness, especially where one is feeling judged and stigmatized, may also have significant mediating effects on mental health. Nidich and colleagues (2009) in a study of the effects of meditation on hypertension using TM meditations which also focuses on present moment mindfulness, found that it decreased psychological distress and increased coping, similar to our findings of improved coping in our study participants. It may be that improved coping skills enhance resilience in people’s capacity to respond to difficult situations.
We also found improvement in self-compassion among our study participants, as did Robins et al (2012) in their study of MBSR on emotional experience and expression. Self-compassion is an important component of mental health and they posited that because MBSR emphasizes not judging experiences as intrinsically good or bad, it would increase self-compassion and emotion regulation, which was consistent with their findings. Improvements in mental health though management of stress and decreases in worry and rumination have all been associated with MBSR (Raes, 2010; Raes, Dewulf, Van Heeringen, & Williams, 2009).
Currently diabetes education and self-management programs, which are the cornerstone of diabetes care, focus primarily on decreasing the risk of the serious complications associated with diabetes through increasing knowledge and improving self-management skills such as medication management, glucose monitoring, and self-care behaviors including checking eyes and feet. While these skills are important, prior RCTs of education and self-management programs have shown mixed results in the short and long-term success for improving people’s ability to self-manage their diabetes (Chodosh et al., 2005; RAND, 2003). This may be in part because they do not address the significant psychosocial issues including the many facets of diabetes-related distress that underlie having this long-term chronic condition (Dahl, 2004; O'Connor, Crabtree, & Yanoshik, 1997; Sperl-Hillen et al., 2011; Surwit et al., 2002; Tillotson & Smith, 1996). Until psychosocial issues resulting from the significant lifestyle changes required by the condition are addressed, good diabetes self-management may prove challenging for many.
There are limitations to this study. As a single-arm pilot study the design precludes causal inference and thus only provides preliminary data to address the question of effectiveness of MBSR with diabetes-related distress and self-management. Our sample size was small and predominately female with limited representation of minorities. This population profile however, fits what we know about the overall interest in the population regarding this type of health intervention. The study does however, provide encouraging results to support for the potential efficacy of MBSR as an integrative intervention to improve diabetes-related distress and self-management.
Implications for future research include larger randomized controlled trials of community-based MBSR programs for people with diabetes, especially those with uncontrolled diabetes. Research should also investigate adaptations of community-based MBSR programs that may be specifically relevant and important in meeting the needs of people with diabetes. Other areas of potential research include development of programs that combine both diabetes education and MBSR in a new and innovative ways, and finally studying the experiences of people with diabetes and what causal mechanisms support continuation of good diabetes self-management over time.
Implications for Social Work
Social workers are an integral part of the provision of health care (Golden, 2011). From providing mental health services to individuals and families, to working on interdisciplinary teams in acute and chronic care settings (Moore et al., 2016), social workers are often on the front lines of serving people with chronic conditions such as diabetes (Claiborne & Vandenburgh, 2001; DeCoster, 2001). They are far more likely than many other health care professionals in health care settings to be called on to address psychosocial issues associated with chronic conditions, such as diabetes-related distress or mental health concerns, guiding individuals and families to interventions and services that will meet their needs (Wardian & Sun, 2015). The physical and mental health consequences of poorly-managed diabetes are significant, for both people with diabetes and their families (Wardian & Sun, 2014). MBSR is an intervention that is readily available in many communities and could provide a valuable tool for many people with diabetes to help reduce diabetes-related distress and improve their self-management over the long-term.
Conclusion
People with diabetes often struggle to address the significant lifestyle changes that are required for living with a chronic condition such as diabetes. Practices such as MBSR that decrease stress and improve mental health may provide the ongoing support that many need While current diabetes education and self-management programs address the knowledge needed for the life-style changes that are required, they don’t provide the necessary tools to help weather the stressful emotional toll that diabetes can have on relationships, self-identity and self-esteem. It is likely that diabetes-related distress also negatively impacts the ability to maintain good diabetes self-management over time. Until we tackle the thorny problems of stress and mental health in diabetes care, good diabetes self-management may prove an elusive reality for the many people living with diabetes.
Acknowledgments
This research was supported by the National Center for Complementary and Integrative Health of the National Institutes of Health under Award Number K23AT003919. NCT01796834, ClinicalTrials.gov
Contributor Information
Robin R. Whitebird, School of Social Work, University of St Thomas, 2115 Summit Ave SCB #106, St Paul, MN 55105, 651-962-5867.
Mary Jo Kreitzer, Center for Spiritualty & Healing, University of Minnesota, C510 Mayo Memorial Bldg., MMC 505, 420 Delaware Street SE, Minneapolis, MN 55455, 612-625-3977, Kreit003@umn.edu.
Gabriela Vazquez-Benitez, HealthPartners Institute, PO Box 1524, MS 21111R, Minneapolis, MN 55440-1524, 952-967-5354, Gabriela.X.VazquezBenitez@healthpartners.com.
Chris J. Enstad, HealthPartners Institute, PO Box 1524, MS 21111R, Minneapolis, MN 55440-1524, 952-967-5007, Chris.j.enstad@healthpartners.com.
References
- Addison CC, Campbell-Jenkins BW, Sarpong DF, Kibler J, Singh M, Dubbert P, Taylor H. Psychometric evaluation of a Coping Strategies Inventory Short-Form (CSI-SF) in the Jackson Heart Study cohort. Int J Environ Res Public Health. 2007;4(4):289–295. doi: 10.3390/ijerph200704040004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Anderson RJ, Freedland KE, Clouse RE, Lustman PJ. The prevalence of comorbid depression in adults with diabetes: a meta-analysis. Diabetes Care. 2001;24(6):1069–1078. doi: 10.2337/diacare.24.6.1069. [DOI] [PubMed] [Google Scholar]
- Anderson RM, Fitzgerald JT, Gruppen LD, Funnell MM, Oh MS. The Diabetes Empowerment Scale-Short Form (DES-SF) Diabetes Care. 2003;26(5):1641–1642. doi: 10.2337/diacare.26.5.1641-a. [DOI] [PubMed] [Google Scholar]
- Anderson RM, Funnell MM, Fitzgerald JT, Marrero DG. The Diabetes Empowerment Scale: a measure of psychosocial self-efficacy. Diabetes Care. 2000;23(6):739–743. doi: 10.2337/diacare.23.6.739. [DOI] [PubMed] [Google Scholar]
- Astin JA. Stress reduction through mindfulness meditation. Effects on psychological symptomatology, sense of control, and spiritual experiences. Psychotherapy and Psychosomatics. 1997;66(2):97–106. doi: 10.1159/000289116. [DOI] [PubMed] [Google Scholar]
- Astin JA, Shapiro SL, Eisenberg DM, Forys KL. Mind-body medicine: state of the science, implications for practice. Journal of the American Board of Family Practice. 2003;16(2):131–147. doi: 10.3122/jabfm.16.2.131. [DOI] [PubMed] [Google Scholar]
- Astin JA, Shapiro SL, Lee RA, Shapiro DH., Jr The construct of control in mind-body medicine: implications for healthcare. Alternative Therapies in Health and Medicine. 1999;5(2):42–47. [PubMed] [Google Scholar]
- Bishop SR. What do we really know about mindfulness-based stress reduction? Psychosomatic Medicine. 2002;64(1):71–83. doi: 10.1097/00006842-200201000-00010. [DOI] [PubMed] [Google Scholar]
- Browne JL, Ventura A, Mosely K, Speight J. 'I call it the blame and shame disease': a qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ Open. 2013;3(11):e003384. doi: 10.1136/bmjopen-2013-003384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Callaghan GM. Taking a Zen approach to diabetes. Diabetes Self Manag. 2008;25(5):66–68. 71. [PubMed] [Google Scholar]
- Centers for Disease Control and Prevention. National Diabetes Statistics Report: Estimates of Diabetes and Its Burden in the United States, 2014. Atlanta, GA: 2014. Retrieved from https://www.cdc.gov/diabetes/pubs/statsreport14/national-diabetes-report-web.pdf. [Google Scholar]
- Chambers R, Gullone E, Allen NB. Mindful emotion regulation: An integrative review. Clinical Psychology Review. 2009;29(6):560–572. doi: 10.1016/j.cpr.2009.06.005. [DOI] [PubMed] [Google Scholar]
- Chodosh J, Morton SC, Mojica W, Maglione M, Suttorp MJ, Hilton L, Shekelle P. Meta-analysis: chronic disease self-management programs for older adults. Ann Intern Med. 2005;143(6):427–438. doi: 10.7326/0003-4819-143-6-200509200-00007. [DOI] [PubMed] [Google Scholar]
- Claiborne N, Vandenburgh H. Social workers' role in disease managment. Health and Social Work. 2001;26(4):217–228. doi: 10.1093/hsw/26.4.217. [DOI] [PubMed] [Google Scholar]
- Clinical Evidence. London: BMJ Publishing Group; 2001. [Google Scholar]
- Cohen J. Statistical Power Analysis for the Behavioral Sciences. Hillsdale, NJ: Lawrence Erlbaum; 1988. [Google Scholar]
- Cohen S, Williamson G. Percieved stress in a probability sample of the United States. In: Sapcapam S, Oskamp S, editors. The social psychology of health: Claremont Symposium on applied social psychology. Newbury Park, CA: Sage; 1988. [Google Scholar]
- Cohen S, Kamarck T, Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24(4):385–396. [PubMed] [Google Scholar]
- Cullen M. Mindfulness-based interventions: An emerging phenomenon. Mindfulness. 2011;2:186–193. doi: 10.1007/s12671-011-0058-1. [DOI] [Google Scholar]
- Dahl J, Wilson KG, Nilsson A. Acceptance and commitment therapy and the treatment of persons at risk for long-term disability resulting from stress and pain symptoms: A preliminary randomized trial. Behavior therapy. 2004;35:785–801. [Google Scholar]
- DeCoster VA. Challenges of type 2 diabetes and rold of health care social work: A Neglected area of practice. Health and Social Work. 2001;26(1):26–37. doi: 10.1093/hsw/26.1.26. [DOI] [PubMed] [Google Scholar]
- Esch T, Fricchione GL, Stefano GB. The therapeutic use of the relaxation response in stress-related diseases. Med Sci Monit. 2003;9(2):RA23–34. doi:3454. [PubMed] [Google Scholar]
- Faulenbach M, Uthoff H, Schwegler K, Spinas GA, Schmid C, Wiesli P. Effect of psychological stress on glucose control in patients with Type 2 diabetes. Diabetic Medicine. 2012;29(1):128–131. doi: 10.1111/j.1464-5491.2011.03431.x. [DOI] [PubMed] [Google Scholar]
- Fisher L, Glasgow RE, Strycker LA. The relationship between diabetes distress and clinical depression with glycemic control among patients with type 2 diabetes. Diabetes Care. 2010;33(5):1034–1036. doi: 10.2337/dc09-2175. doi:dc09-2175. 10.2337/dc09-2175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fjorback LO, Arendt M, Ørnbøl E, Fink P, Walach H. Mindfulness-based stress reduction and mindfulness-based cognitive therapy: a systematic review of randomized controlled trials. Acta Psychiatrica Scandinavica. 2011;124(2):102–119. doi: 10.1111/j.1600-0447.2011.01704.x. [DOI] [PubMed] [Google Scholar]
- Gaede P, Lund-Andersen H, Parving HH, Pedersen O. Effect of a multifactorial intervention on mortality in type 2 diabetes. New England Journal of Medicine. 2008;358(6):580–591. doi: 10.1056/NEJMoa0706245. [DOI] [PubMed] [Google Scholar]
- Gates DJ, Mick D. Qigong: an innovative intervention for rural women at risk for type 2 diabetes. Holistic Nursing Practice. 2010;24(6):345–354. doi: 10.1097/HNP.0b013e3181fbb832. [DOI] [PubMed] [Google Scholar]
- Golden RL. Coordination, integration, and collaboration: A clear path for social work in health care reform. Health and Social Work. 2011;36(3) doi: 10.1093/hsw/36.3.227. [DOI] [PubMed] [Google Scholar]
- Gonzalez JS, Shreck E, Psaros C, Safren SA. Distress and Type 2 Diabetes-Treatment Adherence: A Mediating Role for Perceived Control. Health Psychology. 2014 doi: 10.1037/hea0000131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gregg JA, Callaghan GM, Hayes SC, Glenn-Lawson JL. Improving diabetes self-management through acceptance, mindfulness, and values: a randomized controlled trial. Journal of Consulting and Clinical Psychology. 2007;75(2):336–343. doi: 10.1037/0022-006X.75.2.336. [DOI] [PubMed] [Google Scholar]
- Gross CR, Kreitzer MJ, Russas V, Treesak C, Frazier PA, Hertz MI. Mindfulness meditation to reduce symptoms after organ transplant: a pilot study. Alternative Therapies in Health and Medicine. 2004;10(3):58–66. [PubMed] [Google Scholar]
- Gross CR, Kreitzer MJ, Thomas W, Reilly-Spong M, Cramer-Bornemann M, Nyman JA, Ibrahim HN. Mindfulness-based stress reduction for solid organ transplant recipients: a randomized controlled trial. Alternative Therapies in Health and Medicine. 2010;16(5):30–38. [PMC free article] [PubMed] [Google Scholar]
- Grossman P, Niemann L, Schmidt S, Walach H. Mindfulness-based stress reduction and health benefits. A meta-analysis. Journal of Psychosomatic Research. 2004;57(1):35–43. doi: 10.1016/S0022-3999(03)00573-7. [DOI] [PubMed] [Google Scholar]
- Grossman P, Tiefenthaler-Gilmer U, Raysz A, Kesper U. Mindfulness training as an intervention for fibromyalgia: evidence of postintervention and 3-year follow-up benefits in well-being. Psychotherapy and Psychosomatics. 2007;76(4):226–233. doi: 10.1159/000101501. [DOI] [PubMed] [Google Scholar]
- Haenen S, Nyklicek I, van Son J, Pop V, Pouwer F. Mindfulness facets as differential mediators of short and long-term effects of Mindfulness-Based Cognitive Therapy in diabetes outpatients: Findings from the DiaMind randomized trial. Journal of Psychosomatic Research. 2016;85:44–50. doi: 10.1016/j.jpsychores.2016.04.006. [DOI] [PubMed] [Google Scholar]
- Hartmann M, Kopf S, Kircher C, Faude-Lang V, Djuric Z, Augstein F, Nawroth PP. Sustained effects of a mindfulness-based stress-reduction intervention in type 2 diabetic patients: design and first results of a randomized controlled trial (the Heidelberger Diabetes and Stress-study) Diabetes Care. 2012;35(5):945–947. doi: 10.2337/dc11-1343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hofmann SG, Sawyer AT, Witt AA, Oh D. The effect of mindfulness-based therapy on anxiety and depression: A meta-analytic review. Journal of Consulting and Clinical Psychology. 2010;78(2):169–183. doi: 10.1037/a0018555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kabat-Zinn J. Full Catastrophe Living: Using the wisdom of your body and mind to face stress, pain, and illness. New York: Dell Publishing; 1990. [Google Scholar]
- Kanaya AM, Adler N, Moffet HH, Liu J, Schillinger D, Adams A, Karter AJ. Heterogeneity of diabetes outcomes among asians and pacific islanders in the US: the diabetes study of northern california (DISTANCE) Diabetes Care. 2011;34(4):930–937. doi: 10.2337/dc10-1964. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karter AJ, Schillinger D, Adams AS, Moffet HH, Liu J, Adler NE, Kanaya AM. Elevated rates of diabetes in Pacific Islanders and Asian subgroups: The Diabetes Study of Northern California (DISTANCE) Diabetes Care. 2013;36(3):574–579. doi: 10.2337/dc12-0722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kotrlik JWW, H A. The Incorporation of Effect Size in Information Technology, Learning and Performance Research. Information Technology, Learning and Performance Journal. 2003;21(1):1–7. [Google Scholar]
- Kreitzer MJ, Gross CR, Ye X, Russas V, Treesak C. Longitudinal impact of mindfulness meditation on illness burden in solid-organ transplant recipients. Progress in Transplantation. 2005;15(2):166–172. doi: 10.1177/152692480501500210. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. Journal of General Internal Medicine. 2001;16(9):606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JB, Lowe B. The Patient Health Questionnaire Somatic, Anxiety, and Depressive Symptom Scales: a systematic review. General Hospital Psychiatry. 2010;32(4):345–359. doi: 10.1016/j.genhosppsych.2010.03.006. [DOI] [PubMed] [Google Scholar]
- Ledesma D, Kumano H. Mindfulness-based stress reduction and cancer: a meta-analysis. Psycho-Oncology. 2008;18(6):571–579. doi: 10.1002/pon.1400. [DOI] [PubMed] [Google Scholar]
- Lengacher CA, Bennett MP, Gonzalez L, Gilvary D, Cox CE, Cantor A, Djeu J. Immune responses to guided imagery during breast cancer treatment. Biol Res Nurs. 2008;9(3):205–214. doi: 10.1177/1099800407309374. [DOI] [PubMed] [Google Scholar]
- Liu X, Miller YD, Burton NW, Chang JH, Brown WJ. Qi-gong mind-body therapy and diabetes control a randomized controlled trial. American Journal of Preventive Medicine. 2011;41(2):152–158. doi: 10.1016/j.amepre.2011.04.007. doi:S0749-3797(11)00264-9. 10.1016/j.amepre.2011.04.007. [DOI] [PubMed] [Google Scholar]
- Lorig KR, Ritter P, Stewart AL, Sobel DS, Brown BW, Jr, Bandura A, Holman HR. Chronic disease self-management program: 2-year health status and health care utilization outcomes. Medical Care. 2001;39(11):1217–1223. doi: 10.1097/00005650-200111000-00008. [DOI] [PubMed] [Google Scholar]
- Mayeda ER, Karter AJ, Huang ES, Moffet HH, Haan MN, Whitmer RA. Racial/ethnic differences in dementia risk among older type 2 diabetes patients: The Diabetes and Aging Study. Diabetes Care. 2013 doi: 10.2337/dc13-0215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCracken LM, Gauntlett-Gilbert J, Vowles KE. The role of mindfulness in a contextual cognitive-behavioral analysis of chronic pain-related suffering and disability. Pain. 2007;131(1–2):63–69. doi: 10.1016/j.pain.2006.12.013. [DOI] [PubMed] [Google Scholar]
- McDowell I, Newell C. Measuring Health: A Guide to Rating Scales and Questionnaires. 3. New York: Oxford University Press; 2006. [Google Scholar]
- McGinnis RA, McGrady A, Cox SA, Grower-Dowling KA. Biofeedback-assisted relaxation in type 2 diabetes. Diabetes Care. 2005;28(9):2145–2149. doi: 10.2337/diacare.28.9.2145. [DOI] [PubMed] [Google Scholar]
- McGrady A, Horner J. Role of mood in outcome of biofeedback assisted relaxation therapy in insulin dependent diabetes mellitus. Applied Psychophysiology and Biofeedback. 1999;24(1):79–88. doi: 10.1023/a:1022851232058. [DOI] [PubMed] [Google Scholar]
- Moore M, Whiteside LK, Dotolo D, Wang J, Ho L, Conley B, Zatzick DF. The Role of Social Work in Providing Mental Health Services and Care Coordination in an Urban Trauma Center Emergency Department. Psychiatric Services. 2016;67(12):1348–1354. doi: 10.1176/appi.ps.201500469. [DOI] [PubMed] [Google Scholar]
- Naranjo D, Hessler DM, Deol R, Chesla CA. Health and psychosocial outcomes in U.S. adult patients with diabetes from diverse ethnicities. Curr Diab Rep. 2012;12(6):729–738. doi: 10.1007/s11892-012-0319-y. [DOI] [PubMed] [Google Scholar]
- Nidich SI, Rainforth MV, Haaga DA, Hagelin J, Salerno JW, Travis F, Schneider RH. A randomized controlled trial on effects of the Transcendental Meditation program on blood pressure, psychological distress, and coping in young adults. American Journal of Hypertension. 2009;22(12):1326–1331. doi: 10.1038/ajh.2009.184. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nomura M, Fujimoto K, Higashino A, Denzumi M, Miyagawa M, Miyajima H, Nakaya Y. Stress and coping behavior in patients with diabetes mellitus. Acta Diabetologica. 2000;37(2):61–64. doi: 10.1007/s005920070020. [DOI] [PubMed] [Google Scholar]
- O'Connor PJ, Crabtree BF, Yanoshik MK. Differences between diabetic patients who do and do not respond to a diabetes care intervention: a qualitative analysis. Fam Med. 1997;29(6):424–428. [PubMed] [Google Scholar]
- Peyrot M, McMurry JF, Jr, Kruger DF. A biopsychosocial model of glycemic control in diabetes: stress, coping and regimen adherence. Journal of Health and Social Behavior. 1999;40(2):141–158. [PubMed] [Google Scholar]
- Polonsky WH, Anderson BJ, Lohrer PA, Welch G, Jacobson AM, Aponte JE, Schwartz CE. Assessment of diabetes-related distress. Diabetes Care. 1995;18(6):754–760. doi: 10.2337/diacare.18.6.754. [DOI] [PubMed] [Google Scholar]
- Pradhan EK, Baumgarten M, Langenberg P, Handwerger B, Gilpin AK, Magyari T, Berman BM. Effect of Mindfulness-Based Stress Reduction in rheumatoid arthritis patients. Arthritis and Rheumatism. 2007;57(7):1134–1142. doi: 10.1002/art.23010. [DOI] [PubMed] [Google Scholar]
- Raes F. Rumination and worry as mediators of the relationship between self-compassion and depression and anxiety. Personality and individual Differences. 2010;48:757–761. doi: 10.1016/j.paid.2010.01.023. doi: [DOI] [Google Scholar]
- Raes F, Dewulf D, Van Heeringen C, Williams JM. Mindfulness and reduced cognitive reactivity to sad mood: evidence from a correlational study and a non-randomized waiting list controlled study. Behaviour Research and Therapy. 2009;47(7):623–627. doi: 10.1016/j.brat.2009.03.007. [DOI] [PubMed] [Google Scholar]
- Raes F, Pommier E, Neff KD, Van Gucht D. Construction and factorial validation of a short form of the Self-Compassion Scale. Clin Psychol Psychother. 2011;18(3):250–255. doi: 10.1002/cpp.702. [DOI] [PubMed] [Google Scholar]
- RAND. Chronic Disease Self Management for Diabetes, Osteoarthritis, Post-Myocardial Infarction Care, and Hypertension (500-98-0281) 2003. Retrieved from http://www.rand.org/
- Reddy J, Wilhelm K, Campbell L. Putting PAID to diabetes-related distress: the potential utility of the problem areas in diabetes (PAID) scale in patients with diabetes. Psychosomatics. 2013;54(1):44–51. doi: 10.1016/j.psym.2012.08.004. [DOI] [PubMed] [Google Scholar]
- Robins CJ, Keng SL, Ekblad AG, Brantley JG. Effects of mindfulness-based stress reduction on emotional experience and expression: a randomized controlled trial. Journal of Clinical Psychology. 2012;68(1):117–131. doi: 10.1002/jclp.20857. [DOI] [PubMed] [Google Scholar]
- Rosenzweig S, Greeson JM, Reibel DK, Green JS, Jasser SA, Beasley D. Mindfulness-based stress reduction for chronic pain conditions: variation in treatment outcomes and role of home meditation practice. Journal of Psychosomatic Research. 2010;68(1):29–36. doi: 10.1016/j.jpsychores.2009.03.010. [DOI] [PubMed] [Google Scholar]
- Rosenzweig S, Reibel DK, Greeson JM, Edman JS, Jasser SA, McMearty KD, Goldstein BJ. Mindfulness-based stress reduction is associated with improved glycemic control in type 2 diabetes mellitus: a pilot study. Alternative Therapies in Health and Medicine. 2007;13(5):36–38. [PubMed] [Google Scholar]
- Sapolsky RM. Why zebras don't get ulcers. 3. New York, NY: Henry Holt and Co; 2004. [Google Scholar]
- Snoek FJ, Pouwer F, Welch GW, Polonsky WH. Diabetes-related emotional distress in Dutch and U.S. diabetic patients: cross-cultural validity of the problem areas in diabetes scale. Diabetes Care. 2000;23(9):1305–1309. doi: 10.2337/diacare.23.9.1305. [DOI] [PubMed] [Google Scholar]
- Song R, Ahn S, Roberts BL, Lee EO, Ahn YH. Adhering to a t'ai chi program to improve glucose control and quality of life for individuals with type 2 diabetes. Journal of Alternative and Complementary Medicine. 2009;15(6):627–632. doi: 10.1089/acm.2008.0330. [DOI] [PubMed] [Google Scholar]
- Spelberger CD. Manual for the State-Trait Anxiety Inventory for Adults. Palo Alto CA: Consulting Psychologists Press, Mind Garden Inc; 1983. [Google Scholar]
- Sperl-Hillen J, Beaton S, Fernandes O, Von Worley A, Vazquez-Benitez G, Parker E, Spain CV. Comparative effectiveness of patient education methods for type 2 diabetes: a randomized controlled trial. Archives of Internal Medicine. 2011;171(22):2001–2010. doi: 10.1001/archinternmed.2011.507. [DOI] [PubMed] [Google Scholar]
- Stoop CH, Nefs G, Pop VJ, Wijnands-van Gent CJ, Tack CJ, Geelhoed-Duijvestijn PH, Pouwer F. Diabetes-specific emotional distress in people with Type 2 diabetes: a comparison between primary and secondary care. Diabetic Medicine. 2014 doi: 10.1111/dme.12472. [DOI] [PubMed] [Google Scholar]
- Surwit RS, Schneider MS. Role of stress in the etiology and treatment of diabetes mellitus. Psychosomatic Medicine. 1993;55(4):380–393. doi: 10.1097/00006842-199307000-00005. [DOI] [PubMed] [Google Scholar]
- Surwit RS, Schneider MS, Feinglos MN. Stress and diabetes mellitus. Diabetes Care. 1992;15(10):1413–1422. doi: 10.2337/diacare.15.10.1413. [DOI] [PubMed] [Google Scholar]
- Surwit RS, van Tilburg MA, Zucker N, McCaskill CC, Parekh P, Feinglos MN, Lane JD. Stress management improves long-term glycemic control in type 2 diabetes. Diabetes Care. 2002;25(1):30–34. doi: 10.2337/diacare.25.1.30. [DOI] [PubMed] [Google Scholar]
- Tan AW, Lindquist T, Rush WA, O'Connor PJ. Direct costs of various microvascular and macrovascular complications in 6,958 adults with diabetes; Paper presented at the American Diabetes Association's 62nd Scientific Sessions; San Francisco, CA. 2002. Jun 14–18, [Google Scholar]
- Teixeira E. The effect of mindfulness meditation on painful diabetic peripheral neuropathy in adults older than 50 years. Holistic Nursing Practice. 2010;24(5):277–283. doi: 10.1097/HNP.0b013e3181f1add2. [DOI] [PubMed] [Google Scholar]
- Tillotson LM, Smith MS. Locus of control, social support, and adherence to the diabetes regimen. Diabetes Educator. 1996;22(2):133–139. doi: 10.1177/014572179602200206. [DOI] [PubMed] [Google Scholar]
- Van Der Ven NC, Weinger K, Yi J, Pouwer F, Ader H, Van Der Ploeg HM, Snoek FJ. The confidence in diabetes self-care scale: psychometric properties of a new measure of diabetes-specific self-efficacy in Dutch and US patients with type 1 diabetes. Diabetes Care. 2003;26(3):713–718. doi: 10.2337/diacare.26.3.713. [DOI] [PMC free article] [PubMed] [Google Scholar]
- van Son J, Nyklicek I, Nefs G, Speight J, Pop VJ, Pouwer F. The association between mindfulness and emotional distress in adults with diabetes: could mindfulness serve as a buffer? Results from Diabetes MILES: The Netherlands. Journal of Behavioral Medicine. 2015;38(2):251–260. doi: 10.1007/s10865-014-9592-3. [DOI] [PubMed] [Google Scholar]
- Wardian J, Sun F. Factors associated with diabetes-related distress: implications for diabetes self-management. Social Work in Health Care. 2014;53(4):364–381. doi: 10.1080/00981389.2014.884038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wardian J, Sun F. Removing barriers to promote more positive thinking for people with diabetes: Implications for social work. Social Work. 2015;60(2):175–182. doi: 10.1093/sw/swv001. [DOI] [PubMed] [Google Scholar]
- Weijman I, Ros WJ, Rutten GE, Schaufeli WB, Schabracq MJ, Winnubst JA. The role of work-related and personal factors in diabetes self-management. Patient Educ Couns. 2005;59(1):87–96. doi: 10.1016/j.pec.2004.10.004. [DOI] [PubMed] [Google Scholar]
- Welch G, Weinger K, Anderson B, Polonsky WH. Responsiveness of the Problem Areas In Diabetes (PAID) questionnaire. Diabetic Medicine. 2003;20(1):69–72. doi: 10.1046/j.1464-5491.2003.00832.x. doi:832. [DOI] [PubMed] [Google Scholar]
- Whitebird RR, Kreitzer M, Crain AL, Lewis BA, Hanson LR, Enstad CJ. Mindfulness-Based Stress Reduction for Family Caregivers: A Randomized Controlled Trial. Gerontologist. 2012;53(4):676–686. doi: 10.1093/geront/gns126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitebird RR, Kreitzer MJ, Lewis BA, Hanson LR, Crain AL, Enstad CJ, Mehta A. Recruiting and retaining family caregivers to a randomized controlled trial on mindfulness-based stress reduction. Contemporary Clinical Trials. 2011;32(5):654–661. doi: 10.1016/j.cct.2011.05.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitebird RR, Kreitzer MJ, O'Connor PJ. Mindfulness-based stress reduction and diabetes. Diabetes Spectrum. 2009;22(4):226–230. doi: 10.2337/diaspect.22.4.226. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wichowski HC, Kubsch SM. Increasing diabetic self-care through guided imagery. Complementary Therapies in Nursing and Midwifery. 1999;5(6):159–163. doi: 10.1016/s1353-6117(99)80079-1. [DOI] [PubMed] [Google Scholar]
- Yang K, Bernardo LM, Sereika SM, Conroy MB, Balk J, Burke LE. Utilization of 3-month yoga program for adults at high risk for type 2 diabetes: a pilot study. Evid Based Complement Alternat Med 2011. 2011:257891. doi: 10.1093/ecam/nep117. [DOI] [PMC free article] [PubMed] [Google Scholar]