Abstract
Background:
Advances in computed tomography (CT) have facilitated widespread use of medical imaging while increasing patient lifetime exposure to ionizing radiation.
Purpose:
To describe dose optimization strategies used by health care organizations to optimize radiation dose – and image quality
Materials and Methods:
A qualitative study of semi-structured interviews conducted with 26 leaders from 19 health care systems in the United States, Europe, and Japan. Interviews focused on strategies that were used to optimize radiation dose at the organizational level. A directed content analysis approach was used in data analysis.
Results:
Analysis identified seven organizational strategies used by these leaders for optimizing CT dose: (1) engaging radiologists and technologists, (2) establishing a CT dose committee, (3) managing organizational change, (4) providing leadership and support, (5) monitoring and benchmarking, (6) modifying CT protocols, and (7) changes in equipment and work rules.
Conclusions:
Leaders in these health systems engaged in specific strategies to optimize CT dose in within their organizations. The strategies address challenges health systems encounter in optimizing CT dose at the organizational level and offer an evolving framework for consideration in dose optimization efforts for enhancing safety and use of medical imaging.
Keywords: computed tomography, health resources, radiation dosage, organizational culture
Summary Sentence:
This study describes strategies used by healthcare organizations in the U.S., Europe and Japan to optimize CT dose imaging.
Introduction
Advances in medical imaging with computed tomography (CT) have led to widespread availability and use of CT imaging to improve health care1. Concurrent with this are heightened concerns regarding potential health and safety risks related to increasing lifetime exposure for patients to ionizing radiation.2–6 While there is agreement that imaging doses should be as low as reasonably achievable, there remains widespread variation in clinical practice across facilities for similar procedures.7,8 There is little agreement on the best approaches to addressing this issue at the health system or organizational level.
Strategies to improve dose optimization have been implemented, including standardizing protocols, use of dose tracking, dose auditing, and implementation of best practices.9–14 A recent study comparing the effectiveness of a single strategy, audit feedback, to a multicomponent intervention indicates that dose optimization strategies combining interventions such as detailed audit and feedback with actionable suggestions and quality improvement interventions can significantly reduce radiation dose within health systems.15,16 Multiple component interventions however, require significant effort and there are a wide variety of organizational barriers that can hamper successful CT dose optimization efforts at the organizational level.2,17–19
To better understand the strategies health care leaders are using to optimize radiation dose at the organizational level we conducted interviews with a diverse set of leaders in healthcare organizations in the United States and abroad regarding the strategies they have successfully employed to implement change and optimizing CT dose within their organizations.
Materials and Methods
The data for this qualitative study are from semi-structured interviews conducted for the Partnership for Dose Study, a multisite randomized controlled trial of quality improvement interventionsto optimize CT dose funded by the NIH. The study included 19 healthcare organizations, including 100 imaging facilities in the United States, Europe, and Japan with diverse organizational structures including community hospitals, academic teaching systems, and standalone radiology imaging facilities. Primary study results showed significant improvement in improving CT dose.15 This study was conducted in 2018, approved/monitored by the local Institutional Review Board (IRB) and IRBs of participating health systems.
Study Population and Recruitment
The institutions participating in the study were diverse in size, were academic and private practices, provided different types of services, and were diverse in whether they had full-time medical physicists on staff or shared best practices.7,11 The study recruited 26 participants identified by principal site-investigators from the 19 healthcare organizations as leaders in their dose optimization. This purposive sampling strategy was used to identify participants with detailed information about dose optimization activities within their organizations. 20 Recruitment included an introductory email from the study principal investigator, follow-up to answer questions, and obtaining informed consent.
Data Collection
We conducted 21 semi-structured telephone interviews focusing on CT dose optimization efforts; five interviews included 2 participants each. An interview guide containing 13 open-ended questions asked about the approaches/strategies they had used for dose optimization and facilitators/barriers encountered. A single interviewer conducted interviews over 6 months. Interviews were audio-recorded and professionally transcribed, averaging 30 minutes (range, 19–40).
Data Analysis
A directed content analysis approach was used employing the Practice Improvement Model (PIM) as a framework for the analysis.21 The PIM assesses use of systems/workflow-level strategies for modifying/improving care processes and the organization’s change process capability (Figure 1).22 The PIM, developed as a framework for primary care improvement, was used since no specific model exists for radiology improvement.
Figure 1:
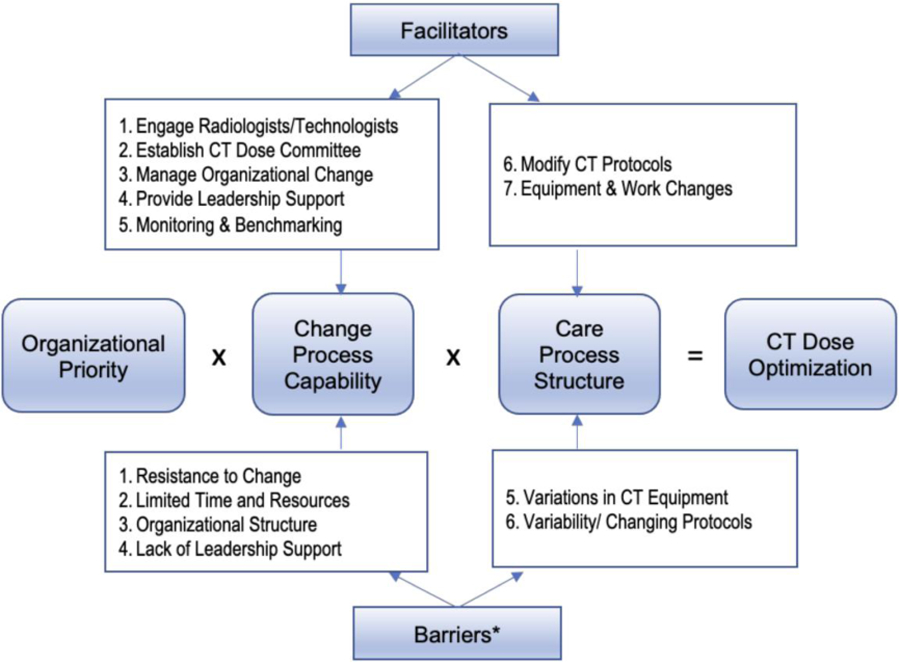
Practice Improvement Model for Computed Tomography (CT) Dose Optimization *Barriers have previously been assessed.
NVivo qualitative data analysis software (version 11.4.3 for Mac) was used to code and structure the data. Data were independently reviewed by investigators experienced in qualitative analysis who met regularly to systematically identify, analyze, and code emerging patterns, categories, and themes/strategies present in the data. A constant comparative method starting with open-coding and using an iterative process was applied in the analysis. Emerging categories and themes/strategies were identified and discussed until consensus was reached on the final coding structure, which was then applied to all data.23 Inductive thematic saturation reached in the analysis with no new codes or themes emerging in the final analysis.24 A study codebook including audit trail, decision points and coding structure enhanced analytic rigor. 25
Results
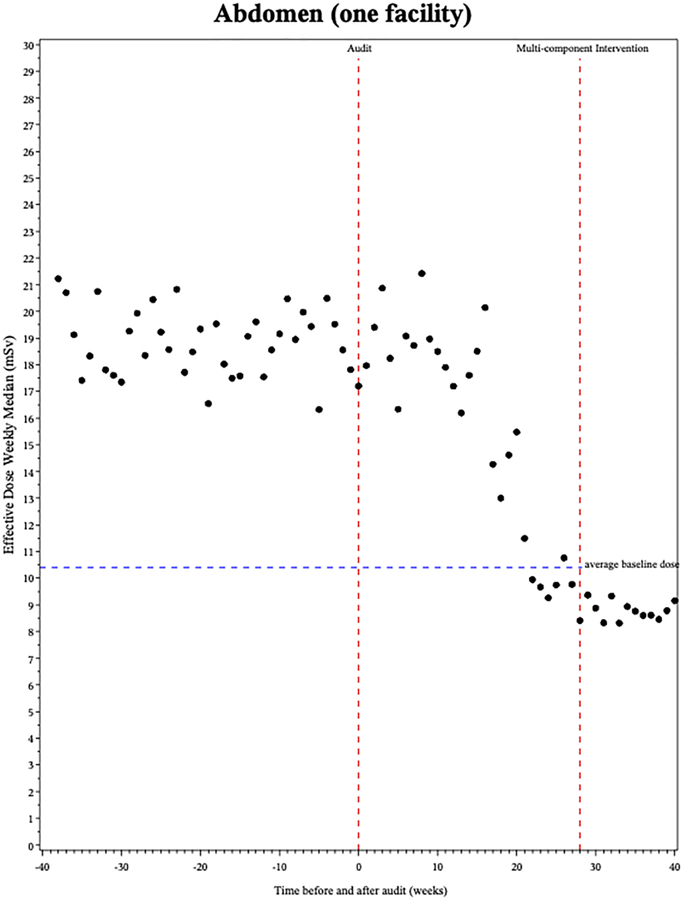
The 26 participants interviewed included 11 radiologists, 8 medical physicists, 5 CT technologists, and 2 operational managers/directors from the 19 participating health care organizations who had responsibility/oversight for radiology services in their organization. Participants were predominately male (n=17, 65%), Caucasian (n=20, 77%) and had been employed for an average of 9.8 years (range 11 months-25 years). The pragmatic trial showed an overall reduction in radiation doses, as illustrated by a drop in weekly average abdomen effective dose across all trial sites (Figure 2), as well as greater than the average decrease in dose by some exemplar institutions (Figure 3). 15
Figure 2.
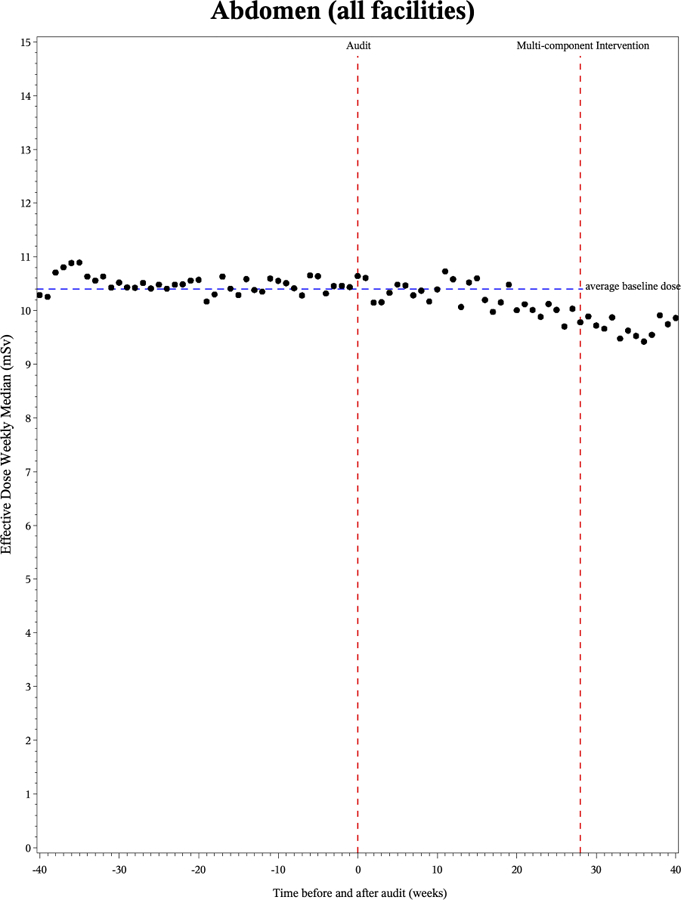
Figure 3.
Analysis identified seven organizational strategies for dose optimization: 1) engaging radiologists/technologists, 2) establishing a CT dose committee, 3) managing organizational change, 4) providing leadership, 5) monitoring/benchmarking, 6) modifying CT protocols, and 7) equipment/work rule changes. Five of these strategies were related to change process capability in the PIM and two to care process structure (Table 1).
Table 1.
Organizational Strategies for Dose Optimization
| Strategy | % (N=26) Respondents Reporting | Strategy Description |
|---|---|---|
| Engaging Radiologists & Technologists | 81% (21) | Involving radiology groups or individual radiologists to approve and/or champion efforts. Also involving Lead Technologists to disseminate efforts to staff |
| Establishing a CT Dose Committee | 73% (19 | Establishing a formal CT Dose Committee to meet regularly and assess and direct dose optimization efforts. Often multidisciplinary |
| Managing Organizational Change | 65% (17) | Providing clear communication and staff education. Engaging in culture change to facilitate behaviors and interactions supportive of dose optimization efforts |
| Providing Leadership Support | 50% (13) | Providing department and organizational leadership who bring support and authority to dose optimization efforts |
| Monitoring & Benchmarking | 38% (10) | Data driven strategy to monitor and assess dose levels across time and compare efforts to other organizations and/or registries |
| Modifying CT Protocols | 88% (23) | Standardization of protocols within or across departments. Locking protocols |
| Facilitating Equipment & Work Rule Changes | 31% (8) | Investing in new CT scanners. Setting specific work rules and staff requirements for education and/or certification |
CT, computed tomography
Change Process Capability Strategies
Engaging Radiologists/ Technologists
Engaging radiologists and technologists, cited by 81% of respondents, was a primary strategy. The work of radiologists is impacted by dose optimization and engaging radiologists was viewed as a critical element for successful change. As one respondent noted, “I would say to take the time to work with the radiologists, and, I mean, make it a priority.” Respondents discussed engaging either all radiologists or identifying a primary radiologist. Involving all radiologists included having the radiology group signoff on proposed changes. Involving a primary radiologist, a more frequent strategy, involved identifying a radiologist to lead/champion the effort, “Probably, number one thing to do would be get a radiologist involved who’s interested and wants to take an active role in that, because without them you can’t really make a lot of changes.”
Engaging technologists was also viewed as important, with respondents noting the expertise/experience technologists bring to the effort, “our lead tech is heavily involved. We use their experience… [and] benefit a lot from their feedback.” Within some organizations technologists led optimization efforts, “Get a champion, or two … lead technologists in the leadership roles who have good experience in CT.” Technologists were also critical to spreading optimization efforts with departments, “by bringing in the lead techs … they would be able to then disseminate it to their staff under them.” Respondents also noted the importance of communication between technologists and radiologists for successful change efforts, “there was a lot of communication between the lead tech and radiologist … [they] decided how they were going to trial it or any changes that they were going to make.”
Establishing a CT Dose Committee
Establishing a CT dose committee, discussed by 73% of respondents, was an important strategy with many noting their efforts were “driven by our committee.” Respondents discussed the importance of a structured group effort for successful change, “forming a committee where it’s not left to one person, or unclear who’s doing what”, noting that, “it takes a committee or a group of people or a team to make it really happen and keep it going.” Respondents focused on the committee’s importance to organizational change, “the committee that we formed is the most important part. I think that was our big organizational change.” The composition of committees varied from small multidisciplinary groups to large endeavors organized to be “as inclusive as possible” with some committees having up to 30 representatives from multiple departments/divisions “who have expertise and can speak the language of each section.” Committees met regularly setting goals, reviewing protocols, and assessing progress.
Managing Organizational Change
Managing organizational change was discussed by 65% of respondent and involved clear communication, education, and engaging in culture change. Respondents said enhancing communication “established a communication route” between individuals and departments, laying an important foundation, “It’s really important we have a constant interaction between the different professional groups”. Clear, effective communication builds relationships and enhances staff involvement in change efforts, highlighting the importance of “getting everybody on board and getting everybody to cooperate and being on the same page.” Staff education efforts were also important, especially for technologists, “we have formal training and some continuing education” and when changing protocols “we had to do quite a bit of education.”
Perhaps the most complex component of managing organizational change was addressing the culture change that comes with it, respondents noted “optimizing dose is quite a bit of a cultural change process” and “you have to create a culture … to work to optimize dose. If you don’t have a culture, you always have barriers.” The culture of an organization, i.e., its unique values, behaviors, and ways of interacting, are deeply embedded and resistant to change. These organizations approached culture change though involving/engaging staff, as a respondent noted, “I think they felt more engaged in the process … they felt like their job was important and an important part of this.” Policy changes and the use of monetary incentives were also used to change long-standing practices, “when things are tied to dollars, they’re more likely to get done.”
Providing Leadership Support
Providing leadership support, discussed by 50% of respondents, addressed the importance of leadership to change efforts, “if the organizational leadership … is not convinced about this topic, that you should work on dose optimization, then I think it’s very hard to successfully implement change.” Respondents noted that efforts that have “lukewarm leadership buy-in” are not likely to work. Leadership support includes not only clearly stated expressions of support, but “resources where necessary” and “man-hours” to do the work. Respondents noted the importance of leadership that comes from both the department/division and overall organization, “get on the same page as the leadership because without the leadership support … you can’t get anything done.” Leadership support denotes both responsibility and authority for a project and provides a clear message about the importance of the effort, “I think it starts with leadership.”
Monitoring/Benchmarking
Monitoring/benchmarking were strategies discussed by 38% of respondents. They highlight using data to drive change, as one respondent noted, “providing data, and having data integrity so that they believe the data. I mean, you know that saying, In God we trust. All others bring data!” Monitoring data internally and then comparing that data to other organizations as a benchmark can provide new perspective on dose optimization, “I would recommend that someone compares what they’re doing to what everybody else is doing … the overall sense before we started all this was that we were doing just fine and this wasn’t a big priority, and it wasn’t, until we started comparing to other benchmarks.” Using data and metrics to guide optimization efforts can provide a clearer picture of where to focus change efforts. For many organizations the comparison also provides friendly competition to drive organizational change
Care Process Strategies
Modifying CT Protocols
Modifying CT protocols, cited by 88% of respondents, was a key strategy for optimizing dose. Respondents discussed “harmonizing” or “synchronizing” protocols, leading to increased standardization and less variation. This was particularly true in organizations with large variation in the number/type of protocols used and in multi-site organizations where protocols vary greatly, “the goal was to have a network sort of standardization that we would have one protocol that we would do at all sites. Locking protocols was also used to decrease variation, “the first thing we ever did, was to lock the protocols and not allow anybody to modify unless we all agree that it needs to be modified.” In some organizations, protocols varied significantly by site and radiologist and were modified continually. As one respondent noted, “figuring out why people had access to protocols, and why they were changing them when they really shouldn’t be … was pretty easy to solve just by locking down the protocols.” Reviewing protocols on an ongoing basis was seen as a foundational effort in dose optimization. One organization evolved an innovative approach deemed Protocol of the Week, “every week we have one focus protocol that is sent out for all the sites to check their scanners to see if … it’s the same or make changes if they need to.”
Equipment/Work Rule Changes
Investing in new equipment/changing work rules were strategies cited by 31% of respondents. New scanning equipment is expensive and hence a less used strategy but can enhance dose optimization though standardizing technology. As respondents noted, “two different vendors and then four or five different platforms, every protocol is different” and “I would have all the exact same scanners so that I knew … and completely understood how every one of those… worked.” Newer scanners provide increased opportunities for optimization, “the biggest thing without sacrificing image quality, would be newer scanners.” Changes in work rules was a strategy focusing on developing procedures via manuals, registries, or certifications for employees, “We’ve also created a CT manual that requires everyone who comes to work for our hospital to go to take the CT registry and they also have to be registered technologists.”.
Discussion
This study describes strategies used by healthcare organizations in the U.S., Europe and Japan to optimize CT dose imaging. Five of the strategies are related to the change process capability of an organization, including engaging radiologists/technologists, establishing a CT dose committee, managing organizational change, providing leadership, and monitoring/benchmarking. Two strategies focused on care process structures within the organization, including modify CT protocols and facilitating equipment/work rule changes. Taken together these seven strategies present a potential framework for healthcare organizations to consider as they navigate the complex challenge of optimizing CT dose and make meaningful and sustained improvement in the care and safety of patients receiving medical imaging.
Strategies focused on changing practices in healthcare often start with engaging those most affected to encourage participation in change. In CT dose optimization, radiologists are a principal focus given the impact this has on their day-to-day work. Involving a radiology group/individual radiologist to be involved in change is an important strategy.15,26 Designating a champion or lead for change is an important component in QI practices. Establishing a CT dose committee also engages the organization and has broad implications. Committees provide structure, focus, set targets and direction for ongoing change efforts. Committees provide a multidisciplinary perspective and formal process for review and decision-making to reach consensus and implement solutions. Siegelman et al. 26 studied the effectiveness of a CT dose optimization committee in a hospital finding it improved the quality of patient care and fostered a culture of safety and quality improvement. This committee can also assist with another important strategy, managing organizational change.
Managing organizational change encompasses a broad strategy including providing clear communication, education, and engaging in culture change to encourage new behaviors/interactions regarding the importance of dose optimization. It provides a foundation to ground successful change efforts yet is one of the more complex strategies to implement. Communication and behavior within organizations are deeply embedded and resistant to change. Providing clear consistent communication, ongoing education, and staff engagement are key to implement this strategy. Providing leadership support in tandem is also critical for setting a strong foundation for dose optimization as an organizational priority. Solberg et al.16 in studying organizational factors and QI strategies in CT examination found that having radiology leadership support dose optimization efforts was a critical factor in reducing high dose examinations. Organizational leadership can provide both focus and authority to move an organization in the direction of change efforts.
Currently most dose optimization efforts place greater focus on technical issues.27,28 One of the most used strategies in dose optimization is changing CT protocols.9,10,27,28 Harmonizing protocols across an organization can set standards for dose levels meeting the needs for diagnostic accuracy and safety. This can assist organizations in better tracking and managing CT dose across an array of scanner types and departments in large health systems. Monitoring/benchmarking, a less discussed but no less important strategy, is a data-driven strategy that is perhaps best represented in audit/review interventions where dose levels are monitored across time, compared with others, and reviewed for optimization efforts.12 Demb et al.11 in a study of audit and best practices found the use of institutional audit reports combined with engaging in best practices lowered radiation dose for chest and abdominal CT. Using data and metrics to guide optimization efforts can help direct where to focus improvement efforts and track progress across time. Facilitating equipment/work rule changes, a less discussed and used strategy, is limited by the costs associated with investing in new CT equipment and efforts required to institute changes on work rules/requirements.
Optimizing CT dose within healthcare organizations is a complex effort requiring a variety of strategies to reach optimal goals. Strategies employed depend on many organizational factors and barriers that exist to optimization efforts.19 This study adds to the literature by presenting the perspectives of leaders who have engaged in successful change efforts, demonstrated by the results of the successful randomized clinical trial they participated in to lower CT dose associated with this study.15,16 There are limitations to this study however, including its qualitative exploratory nature and small sample size. Other physicians such as cardiologists and urologists may be involved in dose optimization but were not included in our study. However, the study does represent geographic diversity, both national and international, and brings to the fore the voices of leaders in health systems responsible for optimizing CT dose in their organizations.
Conclusions
There is an ongoing interest in the need to address the significant variation in CT dose patients receive within and across healthcare organizations. However, there has been limited focus on how to successfully approach these change efforts at the organizational level. This study adds to the literature by clarifying strategies for change that taken together form a framework through which to consider the complex issues involved in the organizational change needed to achieve CT dose optimization. Framing these strategies is a further step along the pathway of optimizing CT dose and sustained improvement to enhance the care and safety of patients receiving medical imaging.
Take Home Points.
There are seven specific strategies health care leaders have used to successfully address issues of organizational change needed to improve dose optimization at the health system level.
Five strategies identified focus on the change process capability of an organization including engaging radiologists and technologists, establishing a CT dose committee, managing organizational change, providing leadership and support, and monitoring/ benchmarking.
Two of the strategies address workflow issues in the organization including modifying CT protocols and changes in equipment and work rules.
Funding:
Research reported in this publication was supported by the National Cancer Institute of the National Institutes of Health under Award Number R01CA181191 and Patient-Centered Outcomes Research Institute® (PCORI®) Award (CD‐1304‐7043). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or PCORI.
Footnotes
Leadership Roles:
Dr. Smith-Bindman is the Director of the Radiology Outcomes Research Laboratory.
Dr. Leif Solberg is a Senior Advisor to Health Partners Medical Group.
Data Statement: The authors declare that they had full access to all of the data in this study and the authors take complete responsibility for the integrity of the data and accuracy of the data analysis.
Conflict of Interest: Dr. Smith-Bindman is a founder of Alara Imaging, a company focused on collecting and reporting radiation dose information associated with CT.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Smith-Bindman R, Miglioretti DL, Larson EB. Rising use of diagnostic medical imaging in a large integrated health system. Health Aff (Millwood) Nov-Dec 2008;27(6):1491–502. doi: 10.1377/hlthaff.27.6.1491 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Brenner DJ, Hricak H. Radiation exposure from medical imaging: time to regulate? JAMA Jul 14 2010;304(2):208–9. doi: 10.1001/jama.2010.973 [DOI] [PubMed] [Google Scholar]
- 3.Fazel R, Krumholz HM, Wang Y, et al. Exposure to low-dose ionizing radiation from medical imaging procedures. N Engl J Med Aug 27 2009;361(9):849–57. doi: 10.1056/NEJMoa0901249 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Rehani MM, Heil J, Baliyan V. Multicentric study of patients receiving 50 or 100 mSv in a single day through CT imaging-frequency determination and imaging protocols involved. Eur Radiol Mar 8 2021;doi: 10.1007/s00330-021-07734-y [DOI] [PubMed]
- 5.Rehani MM, Yang K, Melick ER, et al. Patients undergoing recurrent CT scans: assessing the magnitude. Eur Radiol Apr 2020;30(4):1828–1836. doi: 10.1007/s00330-019-06523-y [DOI] [PubMed] [Google Scholar]
- 6.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med Dec 14 2009;169(22):2078–86. doi: 10.1001/archinternmed.2009.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Smith-Bindman R, Wang Y, Chu P, et al. International variation in radiation dose for computed tomography examinations: prospective cohort study. BMJ Jan 2 2019;364:k4931. doi: 10.1136/bmj.k4931 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Smith-Bindman R, Lipson J, Marcus R, et al. Radiation dose associated with common computed tomography examinations and the associated lifetime attributable risk of cancer. Arch Intern Med Dec 14 2009;169(22):2078–86. doi: 10.1001/archinternmed.2009.427 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Venkataraman V, Browning T, Pedrosa I, et al. Implementing Shared, Standardized Imaging Protocols to Improve Cross-Enterprise Workflow and Quality. J Digit Imaging Oct 2019;32(5):880–887. doi: 10.1007/s10278-019-00185-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Sachs PB, Hunt K, Mansoubi F, Borgstede J. CT and MR Protocol Standardization Across a Large Health System: Providing a Consistent Radiologist, Patient, and Referring Provider Experience. J Digit Imaging Feb 2017;30(1):11–16. doi: 10.1007/s10278-016-9895-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Demb J, Chu P, Nelson T, et al. Optimizing Radiation Doses for Computed Tomography Across Institutions: Dose Auditing and Best Practices. JAMA Intern Med Jun 1 2017;177(6):810–817. doi: 10.1001/jamainternmed.2017.0445 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Duong PA, Little BP. Dose tracking and dose auditing in a comprehensive computed tomography dose-reduction program. Semin Ultrasound CT MR Aug 2014;35(4):322–30. doi: 10.1053/j.sult.2014.05.004 [DOI] [PubMed] [Google Scholar]
- 13.Seuri R, Rehani MM, Kortesniemi M. How tracking radiologic procedures and dose helps: experience from Finland. AJR Am J Roentgenol Apr 2013;200(4):771–5. doi: 10.2214/ajr.12.10112 [DOI] [PubMed] [Google Scholar]
- 14.Little BP, Duong PA, Knighton J, et al. A Comprehensive CT Dose Reduction Program Using the ACR Dose Index Registry. J Am Coll Radiol Dec 2015;12(12 Pt A):1257–65. doi: 10.1016/j.jacr.2015.07.020 [DOI] [PubMed] [Google Scholar]
- 15.Smith-Bindman R, Chu P, Wang Y, et al. Comparison of the Effectiveness of Single- Component and Multicomponent Interventions for Reducing Radiation Doses in Patients Undergoing Computed Tomography: A Randomized Clinical Trial. JAMA Intern Med May 1 2020;180(5):666–675. doi: 10.1001/jamainternmed.2020.0064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Solberg LI, Wang Y, Whitebird R, Lopez-Solano N, Smith-Bindman R. Organizational Factors and Quality Improvement Strategies Associated With Lower Radiation Dose From CT Examinations. J Am Coll Radiol Jul 2020;17(7):951–959. doi: 10.1016/j.jacr.2020.01.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Hendee WR, Becker GJ, Borgstede JP, et al. Addressing overutilization in medical imaging. Radiology Oct 2010;257(1):240–5. doi: 10.1148/radiol.10100063 [DOI] [PubMed] [Google Scholar]
- 18.Lee JH, Kim K, Lee KH, et al. Perception of radiation dose and potential risks of computed tomography in emergency department medical personnel. Clin Exp Emerg Med Jun 2015;2(2):123–129. doi: 10.15441/ceem.14.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Whitebird RR, Solberg LI, Bergdall AR, López-Solano N, Smith-Bindman R. Barriers to CT Dose Optimization: The Challenge of Organizational Change. Acad Radiol Apr 8 2020;doi: 10.1016/j.acra.2020.02.016 [DOI] [PMC free article] [PubMed]
- 20.Luborsky MR, Rubinstein RL. Sampling in Qualitative Research: Rationale, Issues, and Methods. Res Aging Mar 1 1995;17(1):89–113. doi: 10.1177/0164027595171005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hsieh HF, Shannon SE. Three approaches to qualitative content analysis. Qual Health Res Nov 2005;15(9):1277–88. doi: 10.1177/1049732305276687 [DOI] [PubMed] [Google Scholar]
- 22.Solberg LI. Improving medical practice: A conceptual framework. Annals of Family Medicine 2007;5(3):251–256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Saldana J The Coding Manual for Qualitative Researchers 2nd ed. Sage Publications Ltd; 2013. [Google Scholar]
- 24.Saunders B, Sim J, Kingstone T, et al. Saturation in qualitative research: exploring its conceptualization and operationalization. Qual Quant 2018;52(4):1893–1907. doi: 10.1007/s11135-017-0574-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Patton MQ. Qualitative Research and Evaluation Methods 3rd ed. Sage Publications; 2002. [Google Scholar]
- 26.Siegelman JR, Gress DA. Radiology stewardship and quality improvement: the process and costs of implementing a CT radiation dose optimization committee in a medium-sized community hospital system. J Am Coll Radiol Jun 2013;10(6):416–22. doi: 10.1016/j.jacr.2012.12.008 [DOI] [PubMed] [Google Scholar]
- 27.Tamm EP, Szklaruk J, Puthooran L, Stone D, Stevens BL, Modaro C. Quality initiatives: planning, setting up, and carrying out radiology process improvement projects. Radiographics Sep-Oct 2012;32(5):1529–42. doi: 10.1148/rg.325125013 [DOI] [PubMed] [Google Scholar]
- 28.McCollough CH, Chen GH, Kalender W, et al. Achieving routine submillisievert CT scanning: report from the summit on management of radiation dose in CT. Radiology Aug 2012;264(2):567–80. doi: 10.1148/radiol.12112265 [DOI] [PMC free article] [PubMed] [Google Scholar]


