Abstract
OBJECTIVES:
Chronic infection with hepatitis C virus (HCV) was previously the leading indication for liver transplant (LT) in the United States. However, since 2014 the use of direct-acting antivirals (DAAs) has decreased the chronic HCV burden, while the prevalence of nonalcoholic steatohepatitis (NASH) has risen substantially through the last decade. Both gender and ethnic disparities in indications for LT have been shown in the past but no data on this have been reported since the implementation of DAAs.
METHODS:
We assessed changes in etiologies for LT listing and in gender and ethnic differences in those listed for LT. Adult patients registered for LT in the United Network for Organ Sharing/Organ Procurement and Transplantation Network database between January 1, 2004 and December 31, 2016 were included. Multinomial logistic regression modeling was used to test for changes in waitlist or liver transplant rates.
RESULTS:
The study included 127,164 adult patients registered for LT. By 2016, alcoholic liver disease (ALD) was the leading etiology for waitlisting and LT; NASH was second; hepatocellular carcinoma (HCC) due to chronic HCV and chronic HCV alone were 3rd and 4th. NASH was the leading cause for LT for women and the 2nd leading cause for men (following ALD). NASH increased as the cause in all ethnic subgroups and was the leading cause in 2016 among Asian, Hispanic, and non-Hispanic white females. We also found that although the indication for liver transplant for hepatocellular carcinoma (HCC) due to HCV has increased over the years, this indication decreased for the first time between 2015 and 2016 in both males and females.
CONCLUSIONS:
NASH is currently the second leading cause for LT waitlist registration/liver transplantation overall, and in females, the leading cause. Given the rate of increase, NASH will likely rise to become the leading indication for LT in males as well.
IntroductIon
Chronic infection with hepatitis C virus (HCV) was previously the leading etiology of chronic liver disease among patients registered for liver transplant (LT) in the United States (U.S.) [1, 2].However, since the advent of direct-acting antivirals (DAAs) in 2014, the burden of chronic HCV has decreased [3, 4]. Over the course of the last decade, nonalcoholic steatohepatitis (NASH) has risen to be the second leading etiology of chronic liver disease among new LT registrants in the U.S. [4–7]. The leading cause of LT in the U.S. in 2013 was chronic HCV followed by NASH, but more recent data from 2015 showed that alcoholic liver disease (ALD) was the leading cause followed by NASH [4, 5]. It is currently thought that NASH will be the leading cause of LT by 2020 [8]. The previous reports from Wong et al and Goldberg et al. [4, 5] investigated LT etiologies one year prior to and one year post-implementation of DAAs. However, gender and race differences on the LT list have not been assessed since DAAs became the standard treatment for chronic HCV.
When gender disparities in LT were studied in the past, it was shown that compared to men women had increased LT waiting-list mortality and lower transplantation rates, pointing to the need for further research to understand these disparities and close the gap between males and females [9, 10]. Ethnic disparities have also been shown to exist throughout the process of LT, from disease recognition to treatment to registration [11, 12]. African Americans are disproportionately affected by chronic HCV, and have been shown to have more severe liver disease at the time of waitlist registration compared to non-Hispanic whites [13, 14]. Prior to the adoption of the Model for End-Stage Liver Disease (MELD)-based liver allocation system, African Americans were noted to have significantly lower transplant rates which subsequently improved in the MELD era [15–17]. NASH and ALD have been largely associated with minority populations in the U.S. and the incidence of subsequent chronic liver disease and HCC is growing fastest among Hispanics [12, 18, 19]. However, studies have shown significantly lower transplant rates among minorities, particularly Hispanics and Asians, when compared to non-Hispanic whites [12]. Given the shifting demographics of the U.S., the goal of this study was to assess changes in gender and ethnic differences in waitlist registration and LT over time, especially after the implementation of DAAs. We hypothesized that the decrease in chronic HCV due to the use of DAAs and the steadily rising increase in NASH in the U.S. will have led to changes in gender and racial disparities in the LT waitlist registration and indications.
METHODS
Study design and participants
The study cohort included adult patients aged 18 years and older registered for LT in the United Network for Organ Sharing (UNOS)/Organ Procurement and Transplantation Network (OPTN) database between January 1, 2004 and December 31, 2016. Registered patients with a previous LT were excluded along with those registered for another organ other than kidney; patients listed for both liver and kidney were included. Disease diagnosis coding in the UNOS/OPTN registry determined the etiology of chronic liver disease. Based on methods in previous studies, patients with both HCV and ALD disease diagnosis codes were grouped into a separate category to combine HCV/ALD [5]. Of the patients with HCC, the underlying liver disease was determined based on secondary disease diagnosis codes. Similar to previous studies, a modified NASH category was created to include patients with a diagnosis of NASH or those with cryptogenic cirrhosis in the setting of body mass index (BMI)≥30 kg/m2 or diabetes mellitus [5].
Statistical analysis
Multinomial logistic regression modeling was used to test for changes in the rates of waitlist or liver transplant of each diagnostic category over each year of data within each strata. Post-hoc testing across strata was performed with linear hypothesis testing of regression coefficients. Percent change values over time were computed as the difference in observed counts divided by the prior count. The analysis was performed using SAS v9.4 software.
RESULTS
Liver transplant registration between 2004 and 2016
The study included 127,164 adult patients registered for LT. The characteristics of the study population are shown in supplementary Table 1. Overall, the average age was 54.3 ± 10.2 years, 64.5% were male, 70.6% were Caucasians, and the average BMI and MELD score were 28.7 ± 5.8 kg/m2 and 21.1 ± 11.3, respectively. Between 2004 and 2016, ALD rose to become the leading cause of waitlist registration by adults for LT followed by NASH, while HCV with HCC and HCV alone were the 3rd and 4th leading causes (Supp. Figure 1). Since 2004, there was a 68% decrease in the number of waitlist registrants diagnosed with HCV as the primary etiology (p < 0.0001) (Supp. Table 2) and a 97% increase in NASH (p < 0.0001) as etiology for waitlist registrants. Between 2015 and 2016 alone, there was an 11% increase in NASH (p = 0.0385) with a 24% decrease in HCV (p < 0.0001) (Supp. Table 2). Between 2004 and 2016, there was a 1413% increase (p < 0.0001) in the rate of waitlist registrants with HCC and NASH, the largest change observed across all disease categories. During the entire period there was also an overall increase in the rate of waitlist registrations with HCC due to HCV; however, between 2015 and 2016, there was a decrease in this rate of 12% (p = 0.003) (Supp. Table 2), a change that was statistically significant in males but not in females (Table 1).
Table 1.
Change in rates of liver transplant waitlist registration over time by gender
| Etiology | Males 2016 v 2004 | Males 2016 v 2015 | Females 2016 v 2004 | Females 2016 v 2015 | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −67% | <0.0001 | −22% | <0.0001 | −68% | <0.0001 | −27% | <0.0001 |
| ALD | 49% | <0.0001 | 10% | 0.0957 | 87% | <0.0001 | 15% | 0.0564 |
| NASH | 114% | <0.0001 | 12% | 0.0991 | 80% | <0.0001 | 9% | 0.2061 |
| HCC & HCV | 171% | <0.0001 | −12% | 0.0139 | 233% | <0.0001 | −11% | 0.1576 |
| HCV&ALD | −61% | <0.0001 | −12% | 0.0932 | −43% | 0.0103 | −15% | 0.2266 |
| HCC & NASH | 1172% | <0.0001 | 29% | 0.0203 | 2383% | <0.0001 | −11% | 0.3322 |
| HCC & ALD | 273% | <0.0001 | 11% | 0.3195 | n/a | <0.0001 | 5% | 0.8819 |
Percent change computed from observed counts over time and p-values computed from multinomial regression analysis within each sex; n/a indicates percent change not computed due to zero observations in divisor
HCV Hepatitis C virus, ALD Alcoholic liver disease, NASH Non-alcoholic steatohepatitis, HCC Hepatocellular carcinoma
Gender and ethnic differences in liver transplant registration
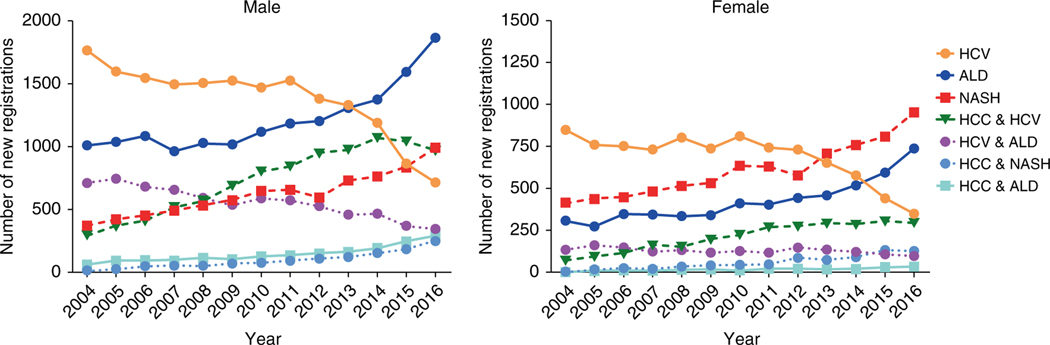
Among both males and females between 2004 and 2016 there was a significant rate increase in waitlist registration due to NASH (114% change in males and 80% change in females, p < 0.0001) (Table 1). There was a 2383% increase in NASH with HCC in the female cohort in this time period among waitlist registrants (p < 0.0001) (Table 1), a change approximately twice the change in males (1172%) over this period. By 2016, NASH had become the leading cause of LT waitlist registration for women while in men the leading cause continued to be ALD (Fig. 1). ALD as the etiology for waitlist registration continued to increase between 2004 and 2016 in both males and females, although the change in females was larger than that in men (87 vs 49%, p = 0.0008) (Table 1).
Fig. 1.
Number of new waitlist registrants by disease category and gender. Left side shows number of new waitlist registrants by disease category in males while the right side shows this number in females. HCV hepatitis C virus, ALD alcoholic liver disease, NASH nonalcoholic steatohepatitis, HCC hepatocellular carcinoma
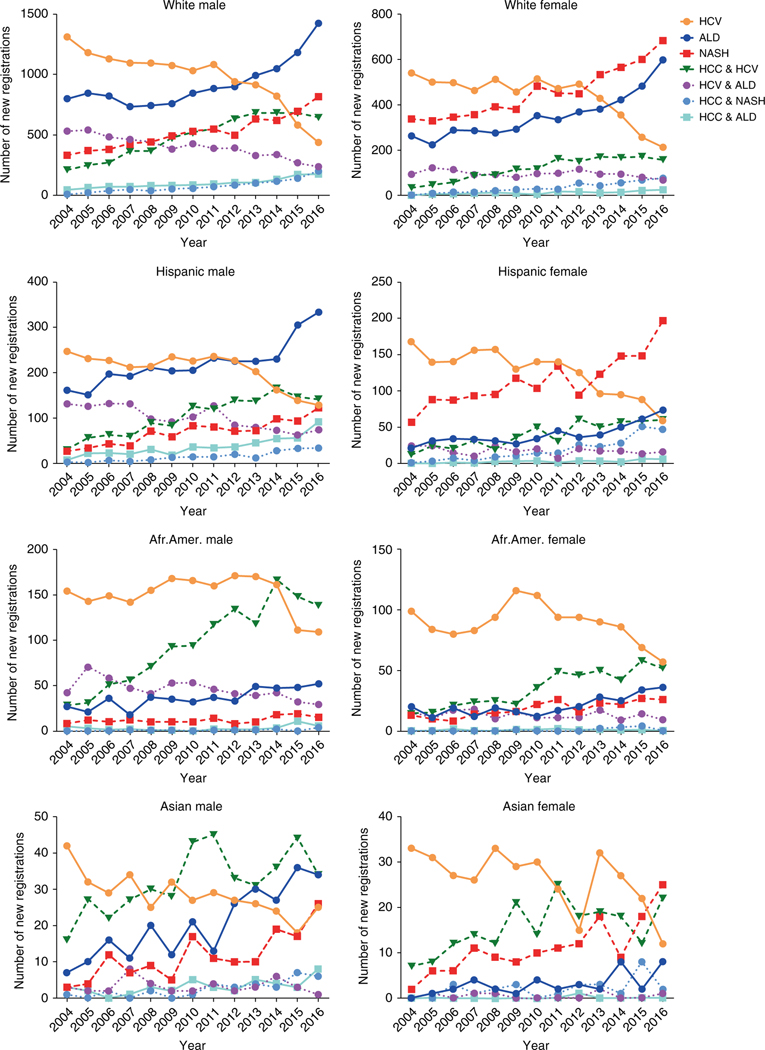
There were also ethnic differences in waitlist registration for LT. Between 2004 and 2016, NASH continued to rise as a cause of waitlist registration across all ethnic groups (Fig. 2). Among Asian, Hispanic, and non-Hispanic white females, NASH was the leading cause of waitlist registration in 2016, whereas HCV remained the leading cause in African American females (Fig. 2). Asian females had an 854% change in NASH waitlist registration while Asian males had a 552% change (Table 2). The African American population had less increase in the rate of waitlist registration for NASH compared to the other ethnic groups. Strikingly, between 2004 and 2016 Hispanic females had a 3010% change in the rate of waitlist registration for NASH with HCC while non-Hispanic white females had a 1992% change (Table 2).
Fig. 2.
Number of new waitlist registrants by disease category and ethnicity by gender over time. Left side shows number of new waitlist registrants by disease category and ethnicity in males while the right side shows new waitlist registrants by disease category and ethnicity in females. HCV hepatitis C virus, ALD alcoholic liver disease, NASH nonalcoholic steatohepatitis, HCC hepatocellular carcinoma
Table 2.
Change in rates of liver transplant waitlist registration over time by ethnicity and gender
| Etiology | White Male 2016 v 2004 | White Male 2016 v 2015 | White Female 2016 v 2004 | White Female 2016 v 2015 | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −71% | < 0.0001 | −29% | < 0.0001 | −68% | < 0.0001 | −25% | 0.0022 |
| ALD | 50% | < 0.0001 | 12% | 0.2546 | 85% | < 0.0001 | 13% | 0.2957 |
| NASH | 106% | < 0.0001 | 9% | 0.5069 | 65% | < 0.0001 | 3% | 0.9557 |
| HCC & HCV | 154% | < 0.0001 | −12% | 0.0147 | 276% | < 0.0001 | −17% | 0.0625 |
| HCV & ALD | −62% | < 0.0001 | −17% | 0.0181 | −39% | 0.1441 | −21% | 0.1177 |
| HCC & NASH | 1645% | < 0.0001 | 36% | 0.0259 | 1992% | < 0.0001 | 3% | 0.9568 |
| HCC & ALD | 223% | < 0.0001 | 0% | 0.6733 | n/a | 0.8713 | −1% | 0.8637 |
| Etiology | Hispanic Male 2016 v 2004 | Hispanic Male 2016 v 2015 | Hispanic Female 2016 v 2004 | Hispanic Female 2016 v 2015 | ||||
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −65% | < 0.0001 | −14% | 0.7761 | −77% | < 0.0001 | −39% | 0.0052 |
| ALD | 41% | 0.0004 | 1% | 0.3817 | 130% | 0.0003 | 9% | 0.8631 |
| NASH | 210% | < 0.0001 | 21% | 0.0869 | 129% | < 0.0001 | 21% | 0.3374 |
| HCC & HCV | 230% | < 0.0001 | −10% | 0.9974 | 231% | < 0.0001 | −8% | 0.5374 |
| HCV & ALD | −62% | < 0.0001 | 8% | 0.3483 | −56% | 0.0415 | 12% | 0.8715 |
| HCC & NASH | 670% | 0.0003 | −5% | 0.8268 | 3010% | 0.0004 | −16% | 0.3132 |
| HCC & ALD | 793% | < 0.0001 | 51% | 0.0088 | n/a | 0.9489 | −9% | 0.8042 |
| Etiology | AA Male 2016 v 2004 | AA Male 2016 v 2015 | AA Female 2016 v 2004 | AA Female 2016 v 2015 | ||||
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −45% | 0.0015 | 5% | 0.5807 | −52% | <0.0001 | −8% | 0.5651 |
| ALD | 48% | 0.0892 | 16% | 0.3948 | 51% | 0.2355 | 18% | 0.6140 |
| NASH | 44% | 0.3496 | −15% | 0.7361 | 68% | 0.1967 | 7% | 0.9029 |
| HCC & HCV | 280% | <0.0001 | 0% | 0.7838 | 212% | 0.0007 | 0% | 0.8678 |
| HCV & ALD | −47% | 0.0328 | −3% | 0.9548 | −50% | 0.0872 | −29% | 0.4008 |
| HCC & NASH | n/a | 0.9778 | n/a | 0.9742 | n/a | 0.9999 | −100% | 0.9765 |
| HCC & ALD | −23% | 0.7510 | −51% | 0.2206 | n/a | 0.9999 | −100% | 0.9789 |
| Etiology | Asian Male 2016 v 2004 | Asian Male 2016 v 2015 | Asian Female 2016 v 2004 | Asian Female 2016 v 2015 | ||||
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −55% | 0.0179 | 29% | 0.4815 | −72% | 0.0028 | −45% | 0.2076 |
| ALD | 265% | 0.0007 | −13% | 0.5475 | n/a | 0.9781 | 305% | 0.0622 |
| NASH | 552% | 0.0010 | 42% | 0.3213 | 854% | 0.0013 | 41% | 0.1978 |
| HCC & HCV | 60% | 0.0504 | −28% | 0.1535 | 140% | 0.0242 | 86% | 0.0642 |
| HCV&ALD | −75% | 0.2904 | −69% | 0.3014 | n/a | 0.9915 | n/a | 0.9902 |
| HCC & NASH | 351% | 0.1250 | −21% | 0.6541 | n/a | 0.9832 | −75% | 0.1143 |
| HCC & ALD | 101% | 0.2125 | 147% | 0.1979 | n/a | 0.9999 | n/a | 0.9999 |
Percent change computed from observed counts over time and p-values computed from multinomial regression analysis within each ethnicity and sex; n/a indicates percent change not computed due to zero observations in divisor
AA African Americans, HCV Hepatitis C virus, ALD Alcoholic liver disease, NASH Non-alcoholic steatohepatitis, HCC Hepatocellular carcinoma
Liver transplant indications by 2016
By 2016 ALD had become the leading cause of LT overall, increasing by 42% from 2004, while HCV as the cause had decreased by 55% (Supp. Table 3). NASH rose to be the second leading cause of transplant, increasing by 109% between 2004 and 2016 (Supp. Figure 2); (p < 0.001) (Supp. Table 3). Between 2004 and 2016, there was a 940% increase (p < 0.0001) of HCC due to NASH as an indication for LT. Although there was also an overall increased rate of HCC due to HCV during this period, we found that there was a decrease of 27% in the rate of waitlist registrants with HCC due to HCV between 2015 and 2016 (p < 0.0001) (Supp. Table 2). This change was statistically significant in both males and females (Table 1).
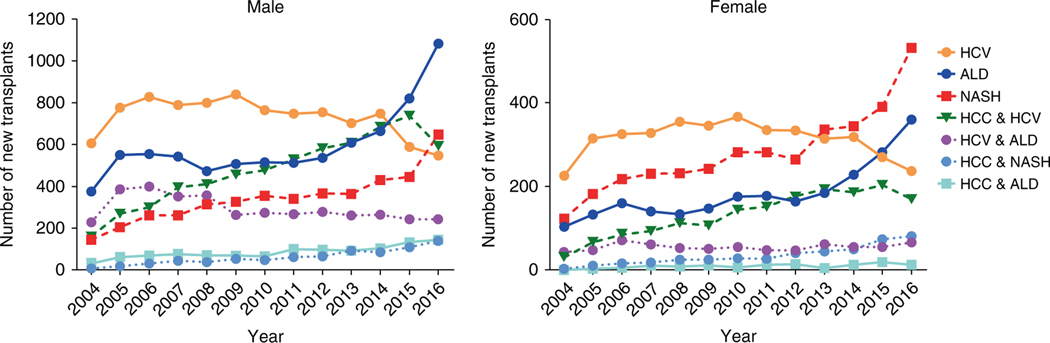
Gender and ethnic differences in liver transplant indications by 2016
By 2016 NASH had become the leading indication for LT in females, followed by ALD and then HCV (Fig. 3). In males, by 2016 ALD had become the leading cause of transplant followed by NASH (Fig. 3). The female population displayed a 91% increase in NASH as the indication for transplant between 2004 and 2016 (p < 0.0001), while males had a 120% increase in the same time period (p < 0.0001) (Table 3). There was a 32% increase in the rate of NASH as the cause of LT in males and a 19% increase in females from 2015 to 2016 (p < 0.0001). There was a decrease in HCV with HCC as a cause for transplant by 27% in both males (p < 0.0001) and females (p = 0.0025) while HCV alone as a cause for transplant decreased by 15% in males (p = 0.0437) and 23% in females between 2015 and 2016 (p = 0.0042) (Table 3).
Fig. 3.
Number of liver transplants by indication and gender. Left side shows number of liver transplants by disease category in males while the right side shows this number in females. HCV hepatitis C virus, ALD alcoholic liver disease, NASH nonalcoholic steatohepatitis, HCC hepatocellular carcinoma
Table 3.
Change in rates of liver transplant indication over time by gender
| Etiology | Males 2016 v 2004 | Males 2016 v 2015 | Females 2016 v 2004 | Females 2016 v 2015 | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −56% | <0.0001 | −15% | 0.0437 | −54% | <0.0001 | −23% | 0.0042 |
| ALD | 41% | <0.0001 | 20% | 0.0017 | 53% | <0.0001 | 11% | 0.3989 |
| NASH | 120% | <0.0001 | 32% | <0.0001 | 91% | <0.0001 | 19% | 0.0896 |
| HCC & HCV | 84% | <0.0001 | −27% | <0.0001 | 129% | <0.0001 | −27% | 0.0025 |
| HCV & ALD | −48% | <0.0001 | −9% | 0.4470 | −32% | 0.5055 | 5% | 0.9280 |
| HCC & NASH | 876% | <0.0001 | 17% | 0.1947 | 1080% | <0.0001 | −6% | 0.6049 |
| HCC & ALD | 118% | <0.0001 | 0% | 0.8961 | n/a | 0.8754 | −45% | 0.0931 |
Percent change computed from observed rates over time and p-values computed from multinomial regression analysis within each sex; n/a indicates percent change not computed due to zero observations in divisor
HCV Hepatitis C virus, ALD Alcoholic liver disease, NASH Non-alcoholic steatohepatitis, HCC Hepatocellular carcinoma
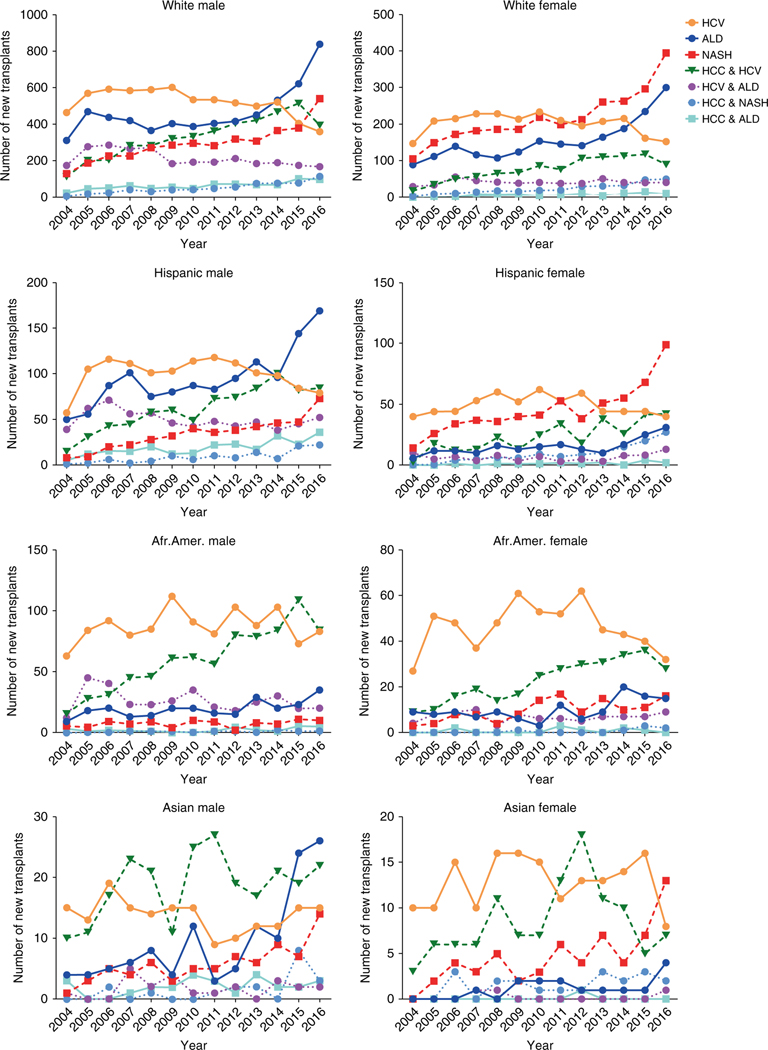
In the analysis of ethnic differences, it was shown that NASH continued to increase as a cause of transplant over time (Fig. 4) between 2004 and 2016. Among non-Hispanic white, Hispanic, and Asian females, NASH was the leading indication for LT in 2016 (Fig. 4, Table 4). Increases in NASH as the cause of transplant were seen in the male ethnic subgroups as well. Most notably this was evident in Asian males with a 597% increase from 2004 to 2016, followed by Hispanic males with a 240% increase and then non-Hispanic white males with a 115% increase (Table 4).
Fig. 4.
Number of liver transplants by indication and ethnicity by gender over time. Left side shows number of liver transplants by disease category and ethnicity in males while the right side shows the number of liver transplants by disease category and ethnicity in females. HCV hepatitis C virus, ALD alcoholic liver disease, NASH nonalcoholic steatohepatitis, HCC hepatocellular carcinoma
Table 4.
Change in rates of liver transplant indication over time by ethnicity and gender
| Etiology | White Male 2016 v 2004 | White Male 2016 v 2015 | White Female 2016 v 2004 | White Female 2016 v 2015 | ||||
|---|---|---|---|---|---|---|---|---|
|
|
|
|
|
|||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −60% | <0.0001 | −19% | 0.0325 | −51% | 0.0023 | −18% | 0.0754 |
| ALD | 40% | <0.0001 | 23% | 0.0031 | 59% | <0.0001 | 11% | 0.4761 |
| NASH | 115% | <0.0001 | 30% | 0.0011 | 75% | <0.0001 | 15% | 0.2499 |
| HCC & HCV | 76% | <0.0001 | −30% | <0.0001 | 147% | <0.0001 | −34% | 0.0032 |
| HCV & ALD | −50% | <0.0001 | −13% | 0.3364 | −33% | 0.7150 | −11% | 0.5297 |
| HCC& NASH | 877% | <0.0001 | 32% | 0.0594 | 1042% | 0.0001 | −10% | 0.5413 |
| HCC & ALD | 121% | <0.0001 | −12% | 0.4873 | n/a | 0.8867 | −38% | 0.2245 |
| Etiology | Hispanic Male 2016 v 2004 | Hispanic Male 2016 v 2015 | Hispanic Female 2016 v 2004 | Hispanic Female 2016 v 2015 | ||||
|
|
||||||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −48% | 0.1939 | −17% | 0.6369 | −69% | 0.0003 | −26% | 0.9582 |
| ALD | 26% | 0.0099 | 4% | 0.4803 | 62% | 0.1808 | 1% | 0.2915 |
| NASH | 240% | <0.0001 | 37% | 0.0791 | 122% | 0.0041 | 19% | 0.3648 |
| HCC & HCV | 109% | 0.0007 | −9% | 0.9536 | 560% | 0.0060 | −18% | 0.8301 |
| HCV & ALD | −50% | 0.1930 | 2% | 0.6563 | −59% | 0.1017 | 33% | 0.2008 |
| HCC & NASH | 720% | 0.0175 | −7% | 0.9749 | 749% | 0.0264 | 10% | 0.5864 |
| HCC & ALD | 235% | 0.0045 | 38% | 0.1680 | n/a | 0.9834 | −59% | 0.4801 |
| Etiology | AA Male 2016 v 2004 | AA Male 2016 v 2015 | AA Female 2016 v 2004 | AA Female 2016 v 2015 | ||||
|
|
||||||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −36% | 0.1625 | 14% | 0.6539 | −43% | 0.0449 | −26% | 0.0858 |
| ALD | 88% | 0.0594 | 53% | 0.1986 | −20% | 0.5601 | −13% | 0.4280 |
| NASH | −3% | 0.8627 | −9% | 0.7752 | 157% | 0.1622 | 34% | 0.7373 |
| HCC & HCV | 171% | 0.0004 | −23% | 0.1325 | 50% | 0.3749 | −28% | 0.0823 |
| HCV & ALD | −19% | 0.8326 | 0% | 0.9185 | 8% | 0.9484 | 19% | 0.9778 |
| HCC & NASH | n/a | 0.9850 | 0% | 0.9803 | n/a | 0.9906 | −38% | 0.4857 |
| HCC & ALD | −19% | 0.9106 | −16% | 0.7258 | n/a | 0.9999 | −100% | 0.9854 |
| Etiology | Asian Male 2016 v 2004 | Asian Male 2016 v 2015 | Asian Female 2016 v 2004 | Asian Female 2016 v 2015 | ||||
|
|
||||||||
| Change | p-value | Change | p-value | Change | p-value | Change | p-value | |
| HCV | −50% | 0.1456 | −12% | 0.7087 | −55% | 0.3071 | −47% | 0.2713 |
| ALD | 223% | 0.0198 | −5% | 0.8352 | n/a | 0.9924 | 321% | 0.1741 |
| NASH | 597% | 0.0482 | 76% | 0.2544 | n/a | 0.9850 | 96% | 0.1303 |
| HCC & HCV | 9% | 0.5996 | 2% | 0.9961 | 31% | 0.4726 | 47% | 0.4249 |
| HCV & ALD | 0% | 0.9228 | −12% | 0.8857 | n/a | 0.9965 | n/a | 0.9952 |
| HCC & NASH | n/a | 0.9762 | −67% | 0.1025 | n/a | 0.9918 | −30% | 0.7946 |
| HCC & ALD | −50% | 0.4894 | 32% | 0.7776 | n/a | 0.9999 | n/a | 0.9999 |
Percent change computed from observed counts over time and p-values computed from multinomial regression analysis within each ethnicity and gender; n/a indicates percent change not computed due to zero observations in divisor
AA African Americans, HCV Hepatitis C virus, ALD Alcoholic liver disease, NASH Non-alcoholic steatohepatitis, HCC Hepatocellular carcinoma
Cryptogenic cirrhosis vs NASH-only coding for liver transplant registration and indication
In our study, we followed the methods used in multiple recent studies by including cryptogenic cirrhosis with BMI ≥ 30 kg/m2 or diabetes mellitus as an indication for NASH in the UNOS transplant list [4, 5]. This is plausible and well-accepted as NASH has been inferred as the most likely cause of liver disease in patients with a diagnosis of cryptogenic cirrhosis and metabolic syndrome, given the disappearance of NASH-defining histological findings once cirrhosis develops [20, 21]. However, we sought to investigate if our findings would change if we excluded cryptogenic cirrhosis with BMI ≥ 30 kg/m2 or diabetes mellitus as an indication for NASH. Although this might exclude a large population of patients and underrepresent subjects with NASH as the indication for LT, with our analysis we found no change in the general findings. Overall, NASH was still the 2nd leading cause of liver transplant registration and indication following ALD (data not shown). NASH remained the leading cause of liver transplant registration and indication in women. NASH was also the 2nd leading cause of liver transplant indication following ALD in men, and the 3rd leading cause of liver transplant registration with no significant difference from the 2nd leading cause, HCC due to HCV, although the latter is now on the decline.
DISCUSSION
In this study, the etiologies of waitlist registration and LT were evaluated in a population of 127,164 patients from the UNOS database to compare differences in males and females and in ethnic subgroups for the first time since implementation of DAAs for treatment of chronic HCV. We report for the first time that in 2016 NASH was the leading cause of waitlist registration and liver transplant in females. In males, there was also an increased incidence of NASH as the etiology of LT waitlist registration but ALD continued to prevail as the leading etiology. In all ethnic subgroups, the incidence of NASH continued to rise over the 14 years assessed. Most notably, there was a significant rise in NASH in the Hispanic population overall. There was a very substantial increase in waitlist registration and indication for LT for HCC due to NASH in Hispanic females over this 14-year period. We also report for the first time a decrease in LT and waitlist registration for HCC due to HCV between 2015 and 2016.
The increasing prevalence of NASH has been attributed to rising obesity, diabetes mellitus type 2, and dyslipidemia [22, 23]. Wong et al reported that in 2013 NASH became the second leading etiology of liver disease among new adult LT waitlist registrants [5]; Goldberg et al. reported that NASH was the 3rd leading cause of LT waitlist registration in adults in 2015 [4]. Using the most recent UNOS/OPTN data our study shows that NASH is now the second leading cause of LT waitlist registration overall, but demonstrates for the first time that NASH is the primary cause in females. Several prior studies have noted that men are more predisposed to NAFLD than females taking into account visceral adiposity based on waist-to-hip circumference ratio [24–29]. However, a study by the NASH Clinical Research Network found that females have more severe stages of NAFLD [30] and our finding may be in part attributable to this [30]. In addition, it is possible that our finding results from a difference in women’s behavior in seeking medical care [30]. In addition, it has been consistently shown that men regularly consume more alcohol than women and are more likely to drink excessively [31], and that the likelihood of developing ALD is based on both the duration and amount of heavy drinking [32] which may have been an important factor in keeping ALD in the higher position as a cause of LT in men.
The fact that a high prevalence of NASH in the Hispanic population has led to increasing rates of LT waitlist registration is not surprising but poses a substantial healthcare challenge given that between 2000 and 2010 Hispanics accounted for approximately 50% of U.S. population growth [33]. Prior studies have reported an increased prevalence of NAFLD in the Hispanic population and noted some gender differences as well [18, 34, 35]. NAFLD is more common in Hispanics than in other ethnic groups, probably due to the high prevalence of the associated metabolic abnormalities in this population, as well as possible genetic differences such as PNPLA3 [36, 37]. While metabolic syndrome is often higher in the African American population, our study highlighted a lower frequency of NASH as an indication for transplant when compared to other ethnic groups. The paradoxical lower frequency of NASH in the African American population despite rates of obesity and insulin resistance similar to or greater than those in Hispanic patients has been noted in prior studies, with this ethnic difference attributed to genetic or environmental factors [18, 35, 37, 38]. However, NASH is increasing as a cause of waitlist registration and LT in African American females. This is not surprising since our recent epidemiological study showed that although African Americans have a lower overall risk of NAFLD compared to other ethnic groups, it is a significant cause of chronic liver disease and cirrhosis in this ethnic group [34].
The increase in HCC due to NASH has been previously reported [39, 40], supporting our finding that this is significantly on the rise as a cause for waitlist registration for LT. Previous reports projected that HCC due to HCV would not peak until 2025 to 2030 [41, 42]. One of these studies took into consideration the implementation of the DAAs [41]. Recent UNOS data showed that HCC due to HCV as a cause of LT had not decreased in the post-DAA era as of 2015 [3]. In contradiction, we report for the first time a decline in HCC due to HCV as a cause for waitlist registration and LT indication from 2015 to 2016. This could be due to the fact that DAAs decreased the incidence of HCC [43]. It is also plausible that DAAs reduced the rate of hepatic decompensation allowing HCC due to HCV to be managed through other treatments such as resection. Further studies are needed to explore this important finding.
Our study highlights the burden of ALD, NASH and HCV as etiologies of LT. This is not surprising as these etiologies are of significance in the general U.S. population. The Centers for Disease Control and Prevention (CDC) estimates chronic hepatitis C to affect 2.7–3.9 million people in the U.S. In 2015, the CDC estimated that there were 21,028 alcoholic liver disease deaths, accounting for a rate of 6.5 per 100,000 population [44]. It is estimated that 10–15% of alcoholics will develop cirrhosis. Based on a recent meta-analysis by Younossi and colleagues, the prevalence of NAFLD in North America is estimated as 24.13%. We have shown that NAFLD is the most common cause of cirrhosis in the multiethnic cohort from California and Hawaii [7, 45].
There are several limitations to our study. First, given that the data was obtained from the UNOS registry, errors in miscoding or entering diagnoses may have occurred since the classification of NASH or any other etiology as the indication for waitlist registration/transplant does not require confirmation [5]. The observed increase in frequency of NASH as an indication for LT was possibly influenced by ascertainment bias in the setting of increased awareness of NASH as well as the ability to accurately document NASH in the UNOS database starting in 2001 [5, 46, 47]. Although our inclusion of cryptogenic cirrhosis patients with a BMI > 30 kg/m2 in the NASH category is consistent with previously published studies, a potential limitation of our analysis is that several of these patients likely had ascites in the setting of chronic liver disease and their dry weight after paracentesis or diuresis was not accounted for [5, 46, 47]. However, our overall findings did not change when we performed a separate analysis excluding cryptogenic cirrhosis patients with a BMI ≥ 30 kg/m2 from the NASH category. Another limitation is that fatty liver may occur concomitantly with other liver diseases such as HCV in those with obesity and/or metabolic syndrome [48]. Since NAFLD/NASH are currently diagnoses of exclusion, neither the UNOS database nor our current study account for this important phenomenon. Despite these limitations, our study highlights key trends that reflect the dynamic epidemiology of waitlisted and transplanted patients in the U.S. Awareness of the gender and ethnic differences could allow us to tailor diagnostic and interventional measures that target specific populations susceptible to particular liver diseases. Our study is the most recent to assess these differences and the most detailed analysis since DAAs for treatment of chronic hepatitis C were implemented. Most importantly, this is the first study to show that NASH is the leading cause of LT in women. It also shows the significant risk of HCC due to NASH, especially in women, and the decline in HCC due to HCV.
CONCLUSION
In summary, with the advent of DAAs, the burden of chronic HCV has decreased [3, 4], while over the course of the last decade, NASH has risen to be the second leading etiology of chronic liver disease among new LT registrants in the U.S [4–7]. This combination of events has resulted in substantial changes in the etiologies underlying LT waitlisting and transplant. Importantly, we report here that HCC due to HCV decreased as an etiology for LT for the first time between 2015 and 2016. NASH is currently the second leading indication overall and, in females, the leading indication for waitlist registration/liver transplantation in the U.S. Hispanic, white and Asian females are more likely to have NASH as the leading indication of waitlist registration and LT. Current studies have displayed that NASH patients are less likely to receive LT compared to other disease indications [5]. Based on our study, given the rate of increase in NASH as the primary indication for LT, NASH will likely rise to become the leading indication for LT in males as well. Further studies are needed to develop new therapeutic approaches for the prevention and treatment of NASH as it continues to rise across all subpopulations.
Supplementary Material
Study Highlights.
WHAT IS CURRENT KNOWLEDGE
Nonalcoholic steatohepatitis followed hepatitis C and alcoholic liver disease as liver transplant causes in 2015.
With the use of direct-acting antivirals hepatitis C has decreased as a liver transplant indication.
Hepatocellular carcinoma due to HCV had not decreased as a liver transplant cause by 2015.
WHAT IS NEW HERE
NASH is now the leading cause of liver transplant in women across various ethnic groups.
Hepatocellular carcinoma due to NASH has increased dramatically, especially in Hispanic women.
Hepatocellular carcinoma due to HCV decreased as a liver transplant indication between 2015 and 2016.
Acknowledgments
CONFLICT OF INTERESTS
Guarantor of the article: Mazen Noureddin, MD.
Potential competing interests: MN: Scientific advisory board for OWL Metabolomics, Abbott, Gilead, Intercept and Echosens, and speaker for Abbott’s and Echosens. Research support: Gilead, Galmed, Galectin, Genfit, Tobira, Conatus, Zydus and Shire. Minor shareholder of Anaetos. VS: speaker’s bureau: Gilead, AbbVie, Intercept, Salix, Advisory board: Gilead, AbbVie.
Footnotes
SUPPLEMENTARY MATERIAL accompanies this paper at https://doi.org/10.1038/s41395-018-0088-6
REFERENCES
- 1.Kim WR, Lake JR, Smith JM, et al. OPTN/SRTR 2015 annual data report: liver. Am J Transplant. 2017;17(Suppl 1):174–251. [DOI] [PubMed] [Google Scholar]
- 2.Yang JD, Larson JJ, Watt KD, et al. Hepatocellular carcinoma is the most common indication for liver transplantation and placement on the waitlist in the United States. Clin Gastroenterol Hepatol. 2017;15:767–75 e3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Flemming JA, Kim WR, Brosgart CL, et al. Reduction in liver transplant wait-listing in the era of direct-acting antiviral therapy. Hepatology. 2017;65:804–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Goldberg D, Ditah IC, Saeian K, et al. Changes in the prevalence of hepatitis C virus infection, nonalcoholic steatohepatitis, and alcoholic liver disease among patients with cirrhosis or liver failure on the waitlist for liver transplantation. Gastroenterology. 2017;152:1090–9 e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wong RJ, Aguilar M, Cheung R, et al. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015;148:547–55. [DOI] [PubMed] [Google Scholar]
- 6.Doycheva I, Issa D, Watt KD, et al. Nonalcoholic steatohepatitis is the most rapidly increasing indication for liver transplantation in young adults in the United States. J Clin Gastroenterol. 2017;52:339–46. [DOI] [PubMed] [Google Scholar]
- 7.Setiawan VW, Stram DO, Porcel J, et al. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: the Multiethnic Cohort. Hepatology. 2016;64:1969–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Charlton M. Nonalcoholic fatty liver disease: a review of current understanding and future impact. Clin Gastroenterol Hepatol. 2004;2:1048–58. [DOI] [PubMed] [Google Scholar]
- 9.Myers RP, Shaheen AA, Aspinall AI, et al. Gender, renal function, and outcomes on the liver transplant waiting list: assessment of revised MELD including estimated glomerular filtration rate. J Hepatol. 2011;54:462–70. [DOI] [PubMed] [Google Scholar]
- 10.Mindikoglu AL, Regev A, Seliger SL, et al. Gender disparity in liver transplant waiting-list mortality: the importance of kidney function. Liver Transpl. 2010;16:1147–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Asrani SK, Kim WR, Kamath PS. Race and receipt of liver transplantation: location matters. Liver Transpl. 2010;16:1009–12. [DOI] [PubMed] [Google Scholar]
- 12.Mathur AK, Schaubel DE, Gong Q, et al. Racial and ethnic disparities in access to liver transplantation. Liver Transpl. 2010;16:1033–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Alter MJ, Kruszon-Moran D, Nainan OV, et al. The prevalence of hepatitis C virus infection in the United States, 1988 through 1994. N Engl J Med. 1999;341:556–62. [DOI] [PubMed] [Google Scholar]
- 14.Ge J, Roberts JP, Lai JC. Race/ethnicity is associated with ABO-nonidentical liver transplantation in the United States. Clin Transp. 2017;31 10.1111/ctr.13011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kemmer N, Zacharias V, Kaiser TE, et al. Access to liver transplantation in the MELD era: role of ethnicity and insurance. Dig Dis Sci. 2009;54:1794–7. [DOI] [PubMed] [Google Scholar]
- 16.Moylan CA, Brady CW, Johnson JL, et al. Disparities in liver transplantation before and after introduction of the MELD score. JAMA. 2008;300:2371–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Reid AE, Resnick M, Chang Y, et al. Disparity in use of orthotopic liver transplantation among blacks and whites. Liver Transpl. 2004;10:834–41. [DOI] [PubMed] [Google Scholar]
- 18.Weston SR, Leyden W, Murphy R, et al. Racial and ethnic distribution of nonalcoholic fatty liver in persons with newly diagnosed chronic liver disease. Hepatology. 2005;41:372–9. [DOI] [PubMed] [Google Scholar]
- 19.Setiawan VW, Wei PC, Hernandez BY, et al. Disparity in liver cancer incidence and chronic liver disease mortality by nativity in Hispanics: the Multiethnic Cohort. Cancer. 2016;122:1444–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Caldwell SH, Oelsner DH, Iezzoni JC, et al. Cryptogenic cirrhosis: clinical characterization and risk factors for underlying disease. Hepatology. 1999;29:664–9. [DOI] [PubMed] [Google Scholar]
- 21.Clark JM, Diehl AM. Nonalcoholic fatty liver disease: an underrecognized cause of cryptogenic cirrhosis. JAMA. 2003;289:3000–4. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM, Carroll MD, Kit BK, et al. Prevalence of obesity and trends in the distribution of body mass index among US adults, 1999–2010. JAMA. 2012;307:491–7. [DOI] [PubMed] [Google Scholar]
- 23.Must A, Spadano J, Coakley EH, et al. The disease burden associated with overweight and obesity. JAMA. 1999;282:1523–9. [DOI] [PubMed] [Google Scholar]
- 24.Fan JG, Zhu J, Li XJ, et al. Prevalence of and risk factors for fatty liver in a general population of Shanghai, China. J Hepatol 2005;43:508–14. [DOI] [PubMed] [Google Scholar]
- 25.Papatheodoridis GV, Goulis J, Christodoulou D, et al. High prevalence of elevated liver enzymes in blood donors: associations with male gender and central adiposity. Eur J Gastroenterol Hepatol. 2007;19:281–7. [DOI] [PubMed] [Google Scholar]
- 26.Vernon G, Baranova A, Younossi ZM. Systematic review: the epidemiology and natural history of non-alcoholic fatty liver disease and non-alcoholic steatohepatitis in adults. Aliment Pharmacol Ther. 2011;34:274–85. [DOI] [PubMed] [Google Scholar]
- 27.Zelber-Sagi S, Nitzan-Kaluski D, Halpern Z, et al. Prevalence of primary non-alcoholic fatty liver disease in a population-based study and its association with biochemical and anthropometric measures. Liver Int. 2006;26:856–63. [DOI] [PubMed] [Google Scholar]
- 28.Park KS, Lee YS, Park HW, et al. Factors associated or related to with pathological severity of nonalcoholic fatty liver disease. Korean J Intern Med. 2004;19:19–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chalasani N, Younossi Z, Lavine JE, et al. The diagnosis and management of nonalcoholic fatty liver disease: practice guidance from the American Association for the Study of Liver Diseases. Hepatology. 2017;67:328–57. [DOI] [PubMed] [Google Scholar]
- 30.Neuschwander-Tetri BA, Clark JM, Bass NM, et al. Clinical, laboratory and histological associations in adults with nonalcoholic fatty liver disease. Hepatology. 2010;52:913–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention. Excessive alcohol use and risks to men’s health. 2017. [cited 2017 October 31]. https://www.cdc.gov/alcohol/fact-sheets/mens-health.htm
- 32.Mann RE, Smart RG, Govoni R. The epidemiology of alcoholic liver disease. (Bethesda: Maryland; 2004). [PMC free article] [PubMed] [Google Scholar]
- 33.Ennis SR, Rios-Vargas M, Albert NG. The Hispanic Population: 2010. Washington, D. C.: United States Census Bureau; 2011. [Google Scholar]
- 34.Setiawan VW, Stram DO, Porcel J, et al. Prevalence of chronic liver disease and cirrhosis by underlying cause in understudied ethnic groups: The multiethnic cohort. Hepatology. 2016;64:1969–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. [DOI] [PubMed] [Google Scholar]
- 36.Romeo S, Kozlitina J, Xing C, et al. Genetic variation in PNPLA3 confers susceptibility to nonalcoholic fatty liver disease. Nat Genet. 2008;40:1461–5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Sookoian S, Pirola CJ. Meta-analysis of the influence of I148M variant of patatin-like phospholipase domain containing 3 gene (PNPLA3) on the susceptibility and histological severity of nonalcoholic fatty liver disease. Hepatology. 2011;53:1883–94. [DOI] [PubMed] [Google Scholar]
- 38.Wagenknecht LE, Scherzinger AL, Stamm ER, et al. Correlates and heritability of nonalcoholic fatty liver disease in a minority cohort. Obesity. 2009;17:1240–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Estes C, Razavi H, Loomba R, et al. Modeling the epidemic of nonalcoholic fatty liver disease demonstrates an exponential increase in burden of disease. Hepatology. 2017;67:123–33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wong RJ, Cheung R, Ahmed A. Nonalcoholic steatohepatitis is the most rapidly growing indication for liver transplantation in patients with hepatocellular carcinoma in the U.S. Hepatology. 2014;59:2188–95. [DOI] [PubMed] [Google Scholar]
- 41.Petrick JL, Kelly SP, Altekruse SF, et al. Future of hepatocellular carcinoma incidence in the United States forecast through 2030. J Clin Oncol. 2016;34:1787–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Davis GL, Alter MJ, El-Serag H, et al. Aging of hepatitis C virus (HCV)-infected persons in the United States: a multiple cohort model of HCV prevalence and disease progression. Gastroenterology. 2010;138:513–21. 521 e1–6 [DOI] [PubMed] [Google Scholar]
- 43.Kanwal F, Kramer J, Asch SM, et al. Risk of hepatocellular cancer in HCV patients treated with direct-acting antiviral agents. Gastroenterology. 2017;153:996–1005 e1. [DOI] [PubMed] [Google Scholar]
- 44.Murphy SL, Xu JQ, Kochanek KD, et al. Final data for 2015. Hyattsville, MD: National Center for Health Statistics; 2017. [PubMed] [Google Scholar]
- 45.Younossi ZM, Koenig AB, Abdelatif D, et al. Global epidemiology of nonalcoholic fatty liver disease-Meta-analytic assessment of prevalence, incidence, and outcomes. Hepatology. 2016;64:73–84. [DOI] [PubMed] [Google Scholar]
- 46.Charlton MR, Burns JM, Pedersen RA, et al. Frequency and outcomes of liver transplantation for nonalcoholic steatohepatitis in the United States. Gastroenterology. 2011;141:1249–53. [DOI] [PubMed] [Google Scholar]
- 47.Kwok R, Tse YK, Wong GL, et al. Systematic review with meta-analysis: non-invasive assessment of non-alcoholic fatty liver disease–the role of transient elastography and plasma cytokeratin-18 fragments. Aliment Pharmacol Ther. 2014;39:254–69. [DOI] [PubMed] [Google Scholar]
- 48.Noureddin M, Wong MM, Todo T, et al. Fatty liver in hepatitis C patients post-sustained virological response with direct-acting antivirals. World J Gastroenterol. 2018;24:1269–77. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.