Abstract
Purpose
To assess the impact of 3D printed models of renal tumor on patient’s understanding of their conditions. Patient understanding of their medical condition and treatment satisfaction has gained increasing attention in medicine. Novel technologies such as additive manufacturing [also termed three-dimensional (3D) printing] may play a role in patient education.
Methods
A prospective pilot study was conducted, and seven patients with a primary diagnosis of kidney tumor who were being considered for partial nephrectomy were included after informed consent. All patients underwent four-phase multi-detector computerized tomography (MDCT) scanning from which renal volume data were extracted to create life-size patient-specific 3D printed models. Patient knowledge and understanding were evaluated before and after 3D model presentation. Patients’ satisfaction with their specific 3D printed model was also assessed through a visual scale.
Results
After viewing their personal 3D kidney model, patients demonstrated an improvement in understanding of basic kidney physiology by 16.7 % (p = 0.018), kidney anatomy by 50 % (p = 0.026), tumor characteristics by 39.3 % (p = 0.068) and the planned surgical procedure by 44.6 % (p = 0.026).
Conclusion
Presented herein is the initial clinical experience with 3D printing to facilitate patient’s pre-surgical understanding of their kidney tumor and surgery.
Keywords: 3D printing, Renal cancer, Kidney tumors, Partial nephrectomy, Education
Introduction
Tumors affecting the kidney commonly develop asymptomatically [1]. When the diagnosis is made, imaging is the only graphic representation to share with patients so that they can visualize and understand the otherwise non-palpable kidney tumor they are faced with. Ideally speaking, an important aspect of obtaining informed consent from the patient prior to partial nephrectomy surgery is for them to have a basic understanding of kidney physiology and anatomy, tumor location and characteristics and the proposed surgical procedure with its related risks of complications. Patient understanding may be further complicated by the plethora of available contemporary treatment strategies (surveillance, ablation, excision), with their specific risks of complications.
Reported herein is, to our knowledge, the initial experience with 3D printed models in order to improve patients’ education.
Materials and methods
Study methodology
Following kidney tumor diagnosis, seven English-speaking patients who were being considered for partial nephrectomy were enrolled in an IRB-approved single-center prospective pilot study. All patients were referred to a single surgeon (ISG), underwent four-phase MDCT scanning and received similar preoperative information on their disease, tumor characteristics, the planned surgery and its related risk of complications. This information was delivered during a face-to-face consultation with the surgeon using CT scan images.
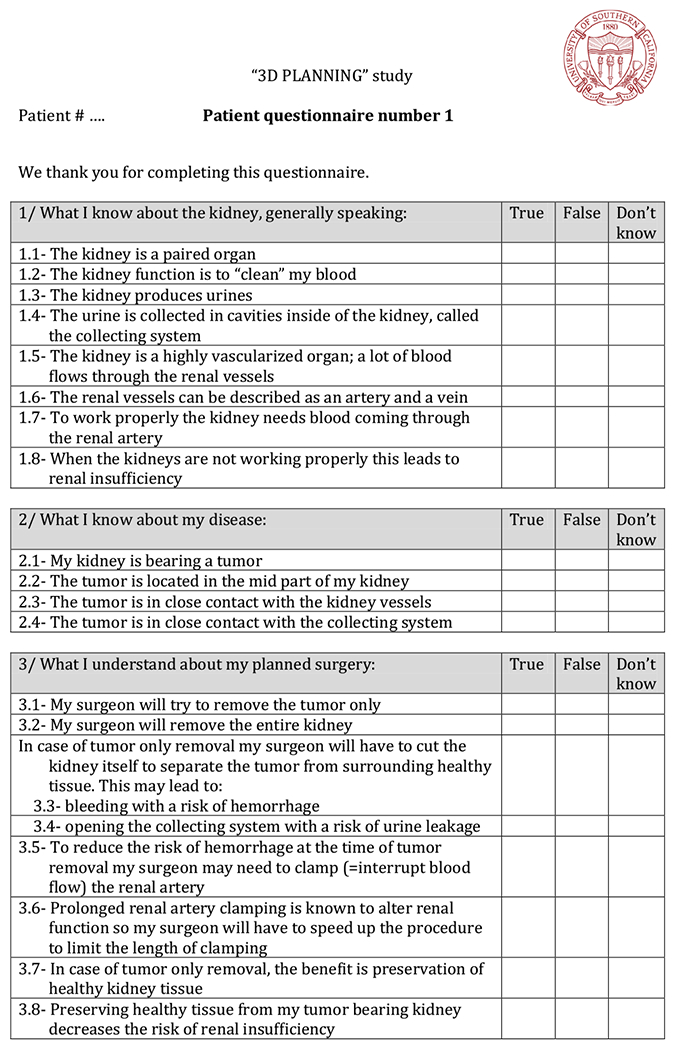
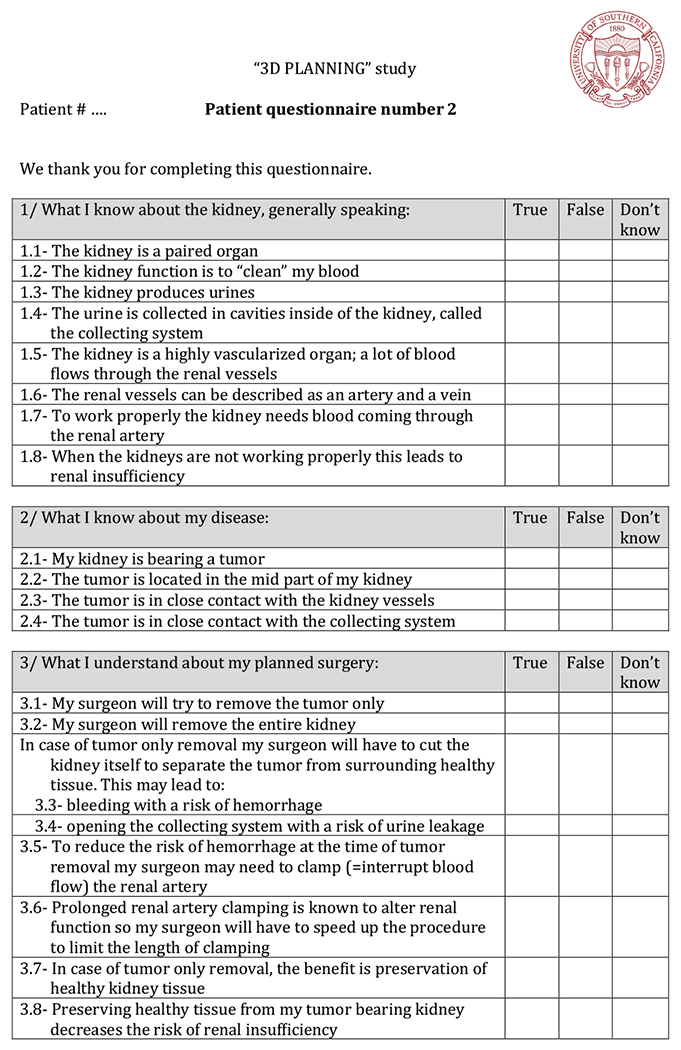
Two questionnaires were created to prospectively evaluate the level of patient’s preoperative knowledge and understanding. This was at first evaluated based on the previously delivered information and CT scan images and secondly using the 3D printed model in order to assess the improvement following the model presentation. Questionnaire #1 consisted of 22 questions to evaluate four components of patient knowledge: (a) basic kidney physiology, (b) basic kidney anatomy, (c) tumor characteristics and (d) planned surgical procedure (“Appendix 1”). Questionnaire #2, in addition to the 22 questions presented in form #1, investigated patient satisfaction using visual analog scales (“Appendix 2”).
The day before surgery, each patient was seen again by an investigator (JCB) and the CT scan images were used again as a teaching aid to deliver information on the organ itself, the disease and the surgery. During this face-to-face visit, patients were free to raise all outstanding issues and then asked to complete questionnaire #1 as baseline reference. Then, that patient’s personal 3D printed model was presented, and after a basic description of the 3D printing process, the patients were again free to ask any question and then completed questionnaire #2.
Statistics
Number of correct responses to the first 22 questions was used as endpoint. Median number of correct responses for each category, before and after 3D printed model presentation, was compared (Wilcoxon test). Statistical analyses were performed using SPSS Statistics version 21.0 (IBM Corporation, Armonk, NY, USA).
3D printed model fabrication
From the DICOM data of patient’s MDCT, kidney structures of interest (tumor, healthy parenchyma, arterial tree, renal vein, collecting system) were extracted using an image recognition algorithm (Synapse 3D, Fujifilm, Tokyo, Japan) and transferred into STL format. Using this STL file, a 3D printed model was created on the OBJET 500 Connex 3 (Stratasys, Eden Prairie, MN, USA) with the assistance of a 3D printing manufacturing company (Fasotec, Makuhari, Chiba, Japan).
The color-segmented 3D model was manufactured by the combination of three different types of photopolymer materials (opaque magenta, opaque yellow and transparent clear material) with 16 μ thickness of each layer under solidification by UV.
As displayed in Figs. 1, 2 and 3, the arterial tree was represented in opaque magenta, the collecting system in opaque yellow and mixing magenta and yellow resulted in opaque orange for tumor display. The renal parenchyma and the renal vein were kept translucent to achieve the best visualization of the relationships between the tumor, the collecting system and the arterial branches.
Fig. 1.
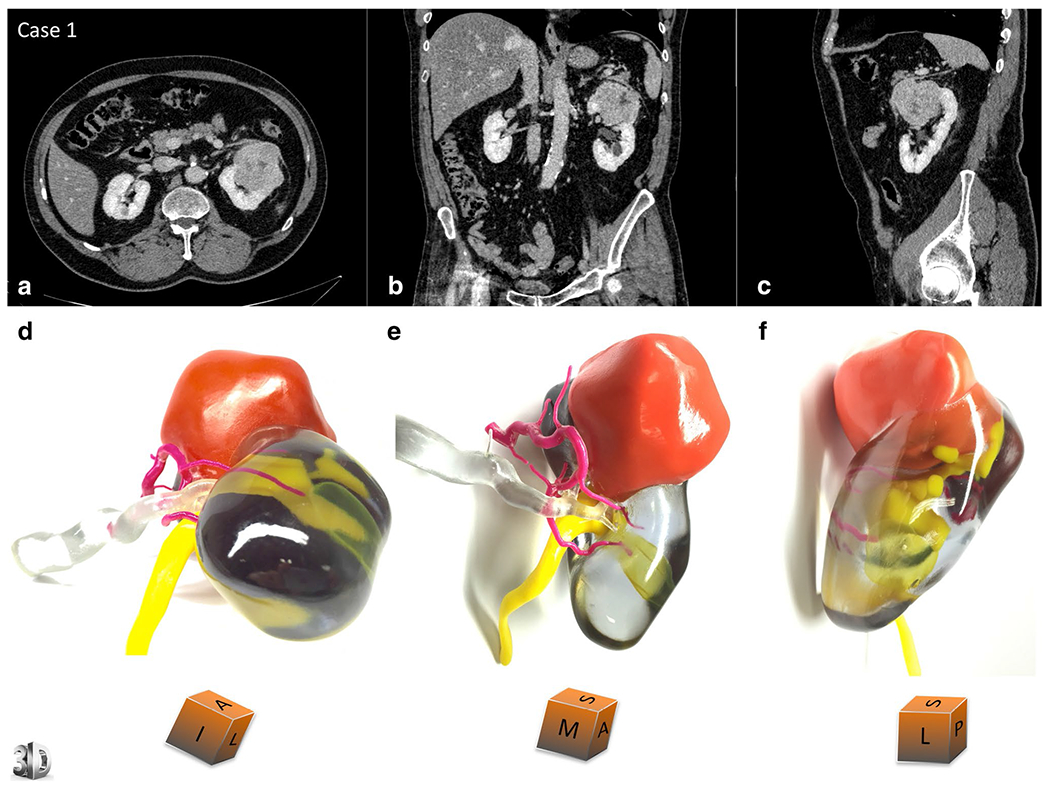
3D printed model for case 1. Comparative views of the CT scan at the nephrographic phase (a axial, b coronal and c sagittal planes) and corresponding views of the physical model (d superior and median view, e median and anterior view, f lateral view). An inferior polar cyst is also displayed on this model (translucent yellow). The cubes show the 3D printed model orientation in space (I = inferior face, A = anterior face, L = lateral side, S = superior face, P = posterior face, M = median side). Case 1 underwent a left radical nephrectomy for a 65 × 56 × 42 mm clear cell renal cell carcinoma, pT1bN0Mx, Fuhrman grade 3
Fig. 2.
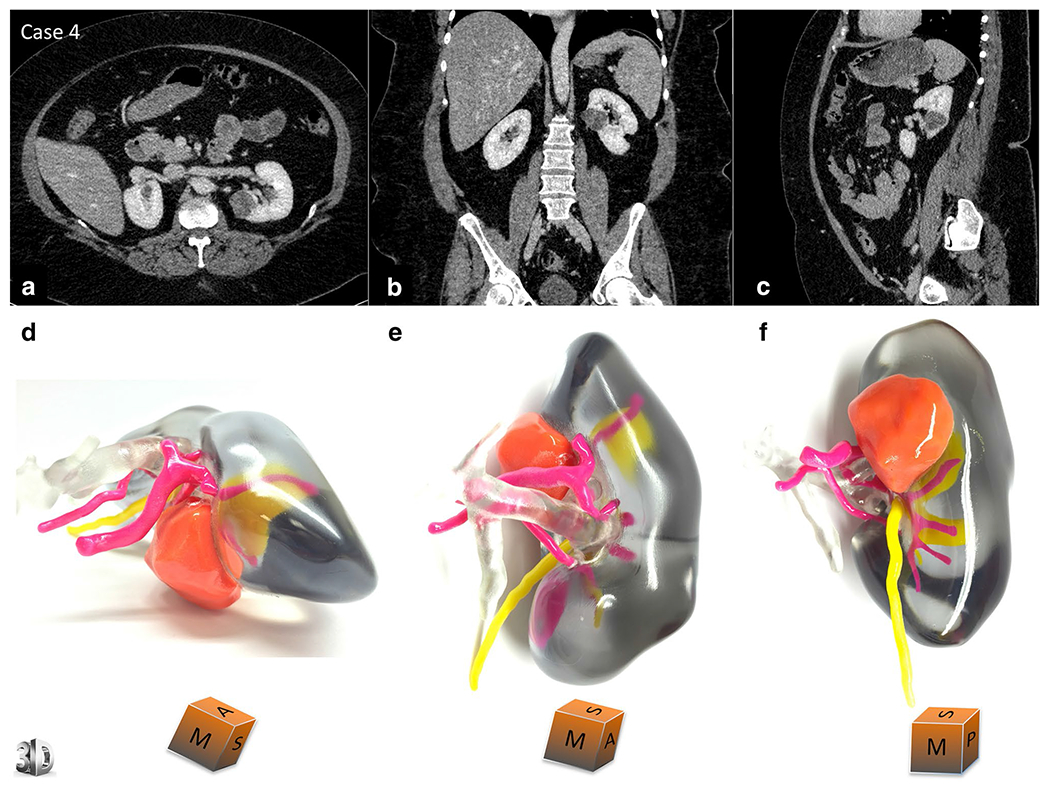
3D printed model for case 4. Comparative views of the CT scan at the nephrographic phase (a axial, b coronal and c sagittal planes) and corresponding views of the physical model (d superior and median view, e median and anterior view, f median and posterior view). The cubes show the 3D printed model orientation in space (I = inferior face, A = anterior face, L = lateral side, S = superior face, P = posterior face, M = median side). Case 7 underwent a left partial nephrectomy for a 36 × 22 × 16 mm clear cell renal cell carcinoma, pT1aNxMx, Fuhrman grade 3
Fig. 3.
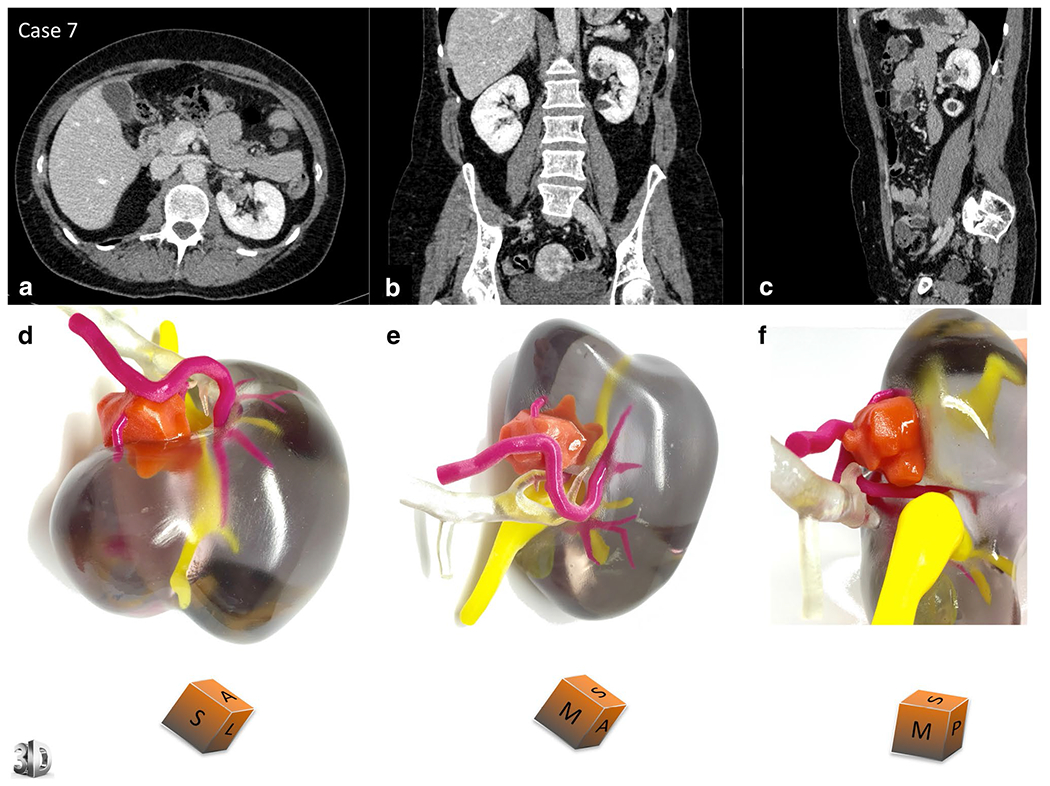
3D printed model for case 7. Comparative views of the CT scan at the nephrographic phase (a axial, b coronal and c sagittal planes) and corresponding views of the physical model (d superior view, e median view, f median view). The cubes show the 3D printed model orientation in space (I = inferior face, A = anterior face, L = lateral side, S = superior face, P = posterior face, M = median side). Case 7 underwent a left partial nephrectomy for a 21 × 15 × 15 mm angiomyolipoma
Results
Table 1 shows patient and tumor demographics.
Table 1.
Patient and tumor characteristics
| Case 1 | Case 2 | Case 3 | Case 4 | Case 5 | Case 6 | Case 7 | |
|---|---|---|---|---|---|---|---|
| Age (years) | 67 | 46 | 54 | 49 | 69 | 33 | 53 |
| Gender | M | M | M | F | M | M | F |
| Education level | 12th g | 12th g | College 2 years | 12th g | 12th g | 12th g | College 2 years |
| Tumor side | Left | Right | Right | Left | Right | Right | Left |
| Tumor size (cm) | 7.2 | 5.6 | 3.8 | 3.5 | 4.1 | 6 | 2.5 |
| Tumor location | Upper pole | Upper pole | Interpolar | Interpolar | Upper pole | Interpolar | Interpolar |
| RENAL Scorea | 9ah | 9ph | 10p | 9ph | 8p | 10ph | 8ph |
| PADUA Scoreb | 10a | 11p | 11p | 11p | 10p | 12p | 7p |
The fabrication cost was $560 per kidney model. For each cognitive component investigated, Fig. 4 reports the level of improvement of patient’s understanding based on an individual analysis.
Fig. 4.
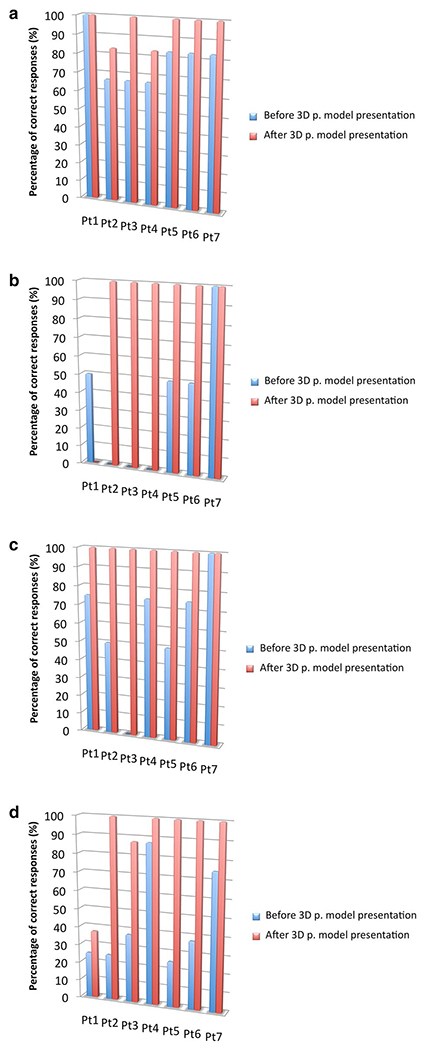
Percentage of correct responses per patient, before and after 3D printed model presentation. Individual analysis of patient’s understanding improvement (percentage of correct responses) on four areas: a basic kidney physiology; b kidney anatomy; c disease and tumor characteristics; d surgical procedure and risk of complications. 3D p. model = 3D printed model. Pt = patient
Table 2 reports a group analysis of the median and percent of correct responses, reflecting the patients’ level of understanding for each component, before and after 3D printed model presentation. Patient’s understanding was significantly improved on basic kidney physiology (p = 0.018), basic kidney anatomy (p = 0.026) and planned surgical procedure (p = 0.026).
Table 2.
Patient’s understanding assessment before and after presentation of the personalized 3D printed model
| Median [range] number and percent of correct responses |
p * | ||
|---|---|---|---|
| Before 3D printed model presentation | After 3D printed model presentation | ||
| Basic kidney physiology | 5 [4–6] | 6 [5–6] | 0.018 |
| 83.3 % [66.7–100] | 100 % [83.3–100] | ||
| Kidney anatomy | 1 [0–2] | 2 [0–2] | 0.026 |
| 50 % [0–100] | 100 % [0–100] | ||
| Disease and tumor characteristics | 3 [0–4] | 4 | 0.068 |
| 75 % [0–100] | 100 % | ||
| Surgical procedure | 3 [2–7] | 8 [3–8] | 0.026 |
| 37.5 % [25–87.5] | 100 % [37.5–100] | ||
For each cognitive component, the number of correct responses among the group of patients reflects the level of understanding
Wilcoxon test
Figure 5 shows the mean improvement rate in patient understanding after viewing their personal 3D kidney model. Patients demonstrated an improvement in their understanding of basic kidney physiology by 16.7 %, kidney anatomy by 50 %, tumor characteristics by 39.3 % and the planned surgical procedure by 44.6 %. Overall improvement was 37.6 %.
Fig. 5.
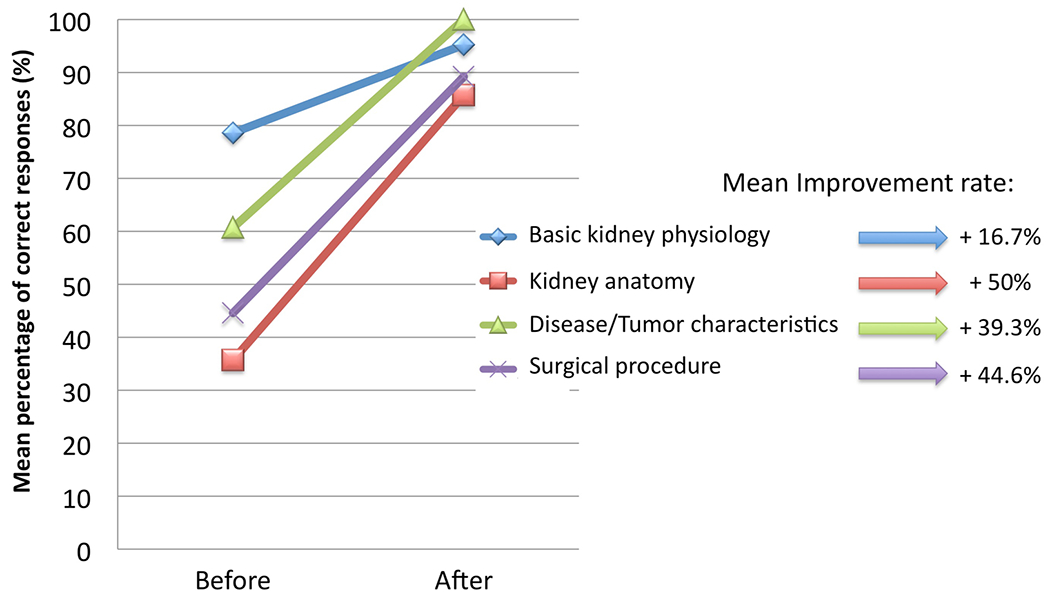
Mean percentage of correct responses per cognitive component, before and after 3D printed model presentation. Group analysis showing the mean improvement rate of patient’s understanding on four cognitive components. After 3D printed model presentation, the mean improvement rate of understanding was 16.7, 50, 39.3 and 44.6 % for basic kidney physiology, kidney anatomy, disease and tumor characteristics and surgical procedure and risk of complications, respectively
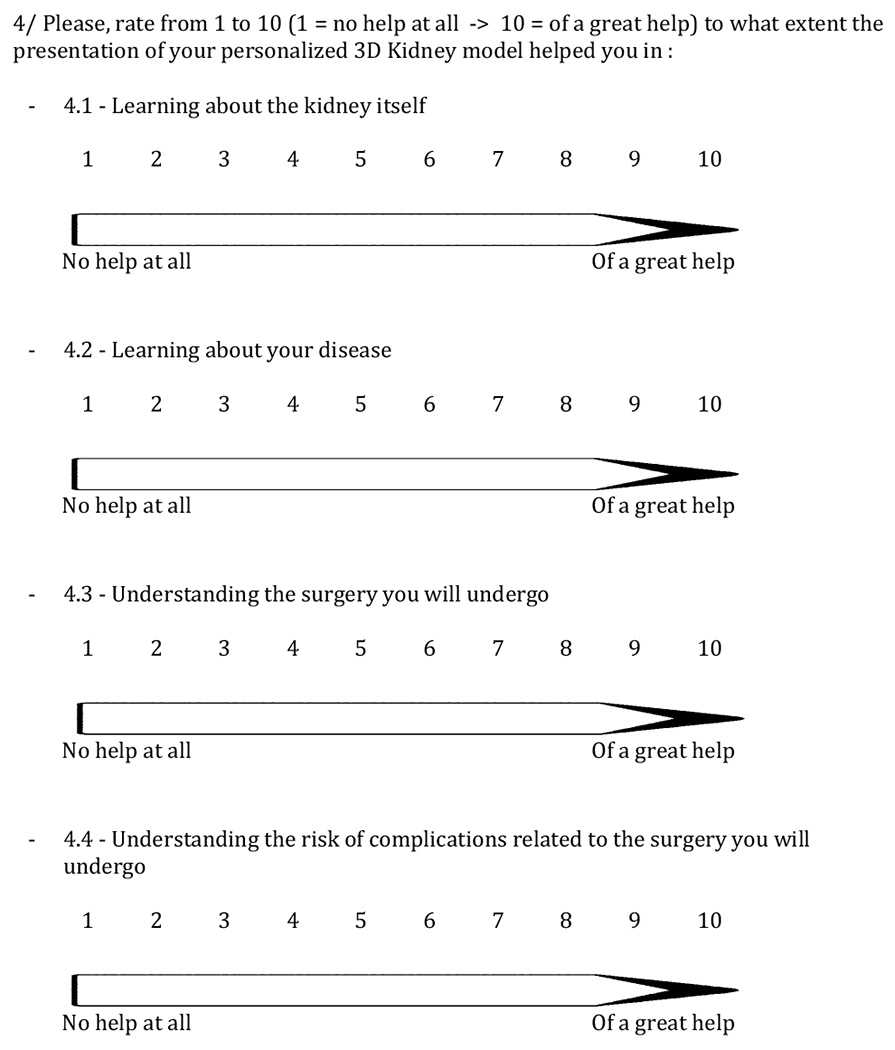
Table 3 reports patients’ satisfaction level in terms of usefulness of the 3D printed model to improve their understanding and knowledge of the kidney organ itself, their disease, the planned surgery and potential complications. The overall mean satisfaction score among the group was 9.4/10, and five patients over 7 rated their experience with their own model at the maximum level.
Table 3.
Patient satisfaction
| The presentation of my personalized 3D kidney model helped me in |
Mean ± SD | ||||
|---|---|---|---|---|---|
| Learning about the kidney itself | Learning about my disease | Understanding the surgery I will undergo | Understanding the risk of complications related to the surgery | ||
| Case 1 | 8 | 6 | 8 | 8 | 7.5 ± 1 |
| Case 2 | 10 | 10 | 10 | 10 | 10 ± 0 |
| Case 3 | 10 | 10 | 10 | 10 | 10 ± 0 |
| Case 4 | 10 | 10 | 10 | 10 | 10 ± 0 |
| Case 5 | 10 | 10 | 10 | 10 | 10 ± 0 |
| Case 6 | 10 | 10 | 10 | 3 | 8.25 ± 3.5 |
| Case 7 | 10 | 10 | 10 | 10 | 10 ± 0 |
| Mean ± SD | 9.7 ± 0.76 | 9.4 ± 1.51 | 9.7 ± 0.76 | 8.7 ± 2.63 | |
The score was given using a visual scale from 1 to 10 with 1 = “no help at all” and 10 = “of a great help” (“Appendix 1”)
Among the entire group, the overall mean satisfaction score was 9.4/10
Discussion
Use of 3D printing in science started more than 20 years ago [2]. Successive improvements in 3D imaging and 3D printing have progressively led various surgical specialties to embrace these innovative technologies, especially in the field of reconstructive surgery [3, 4]. High concordance with patient anatomy, a decrease in production costs of prosthetic materials, expediency of the fabrication process and its potential use for pre-surgical planning or teaching have made 3D printing increasingly popular.
In addition, patients can benefit from the introduction of personalized physical 3D models with the intent of facilitating mutual understanding between patient and physician. Silberstein at al. recently reported 3D printed models of five renal units with malignancy [5]. The authors stated that patients and families verbally expressed improved understanding of their condition and treatment options. However, no objective assessment of the level of improvement was reported. To our knowledge, our study is the first of its kind, specifically designed to evaluate the concept of 3D printing to assist patient education in the field of urology.
We have shown that use of such patient-specific 3D physical models is valuable for patient understanding, with an overall 37.6 % increase in correct responses. It is noteworthy that although every single patient was provided with extensive verbal and written preoperative information as well as a detailed explanation of their CT scan images, their initial reference level of understanding was low. This was especially true regarding basic kidney anatomy but more surprisingly also regarding the planned surgical procedure and its associated risk of complications. This reflects how difficult it can be for patients to understand CT images and also how difficult it can be for the physician to adjust his/her message to an individual patient’s understanding ability [6]. Since in our study, the 3D printed models were used as an aid for mutual exchange, we witnessed how they helped patients raise and ask their own questions, enhancing their understanding. Three-dimensional printed model appeared to be most appropriate in helping the patient understand basic kidney anatomy. As a consequence, it is a helpful tool to deliver comprehensible and personalized messages about partial nephrectomy and its specific risks of complications.
In addition to objective performance, we assessed overall patient satisfaction through four specific questions. The overall feedback was highly favorable with a mean rating of 9.4/10. Patient satisfaction with healthcare experience has now become a priority. Indeed, it is more and more taken into account not only by patient associations, but it has also recently been linked to Medicare reimbursement in the USA. Moreover, Kennedy et al. [7] recently demonstrated that patient perceptions of their care were influenced by factors over and above surgical outcome. Improving patient education by the use of personalized 3D printed models appears to be a promising way to efficiently enhance the quality of personal exchange between a patient and his surgeon and influence overall patient satisfaction.
However, financial costs of patient-specific 3D printed models represent a limitation that merits discussion. Indeed, our models had a unit cost of $560 that was related to their multi-material and multi-color characteristics. This resulted in high quality and detailed models whose fabrication was only made possible by a professional 3D printer. Nevertheless, a balance between quality, user-friendliness and cost efficiency could easily be defined resulting in the production of monocolor, monomaterial more simple models as reported by Watson [8]. In short order and with further development, additive manufacturing will achieve lower production and equipment costs. Consider that, in 2009, The Economist announced the future launch of a less than $5000 3D printer; four years later, the same source was reporting on how competition and expiry of early patents brought the price of 3D printers below $1000 [9, 10].
Moreover, using this kind of models not only for patient counseling but also for students, residents and fellows surgical teaching could help achieve better cost-effectiveness. Indeed, such models, in making easier 3D anatomical understanding, may certainly be useful tools to enhance surgical strategy discussion and improve preoperative planning.
Conclusion
As our results suggest, additive manufacturing is certainly of major interest for patient education in surgery. Increasing spread of the technology and multi-purpose use of the models for treatment planning, trainee teaching and patient education may help achieve cost efficiency. Larger sample size and assessment in other pathologies are needed to confirm these preliminary findings.
Acknowledgments
Fondation ARC pour la Recherche sur leCancer (SAE20131200704) : Dr Jean-Christophe Bernhard; Association Française d’Urologie (AFU)(AFU-2013) : Dr Jean-Christophe Bernhard; The Glenn & Wendy Miller/Inderbir GillKidney Cancer Program : Inderbir S Gill.
Appendix 1
Appendix 2
Footnotes
Conflict of interest The authors declare that they have no competing interests.
Ethical standard The study was IRB approved. All patients received oral information about the objectives and methodology of the study, and informed written consent was obtained from all participants before inclusion. All CT images were anonymized before use for 3D modeling.
References
- 1.Jayson M, Sanders H (1998) Increased incidence of serendipitously discovered renal cell carcinoma. Urology 51(2):203–205 [DOI] [PubMed] [Google Scholar]
- 2.Jones N (2012) Science in three dimensions: the print revolution. Nature 487:22–23 [DOI] [PubMed] [Google Scholar]
- 3.Cohen A, Laviv A, Berman P, Nashef R, Abu-Tair J (2009) Mandibular reconstruction using stereolithographic 3-dimensional printing modeling technology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 108:661–666 [DOI] [PubMed] [Google Scholar]
- 4.Duncan JM, Daurka J, Akhtar K (2014) Use of 3D printing in orthopaedic surgery. BMJ 348:g2963 [Google Scholar]
- 5.Silberstein JL, Maddox MM, Dorsey P, Feibus A, Thomas R, Lee BR (2014) Physical models of renal malignancies using standard cross-sectional imaging and 3-dimensional printers: a pilot study. Urology 84:268–272 [DOI] [PubMed] [Google Scholar]
- 6.Eltorai AE, Sharma P, Wang J, Daniels AH (2015) Most American Academy of Orthopaedic Surgeons’ online patient education material exceeds average patient reading level. Clin Orthop Relat Res 473(4):1181–1186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kennedy GD, Tevis SE, Kent KC (2014) Is there a relationship between patient satisfaction and favorable outcomes? Ann Surg 260:592–598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Watson RA (2014) A low-cost surgical application of additive fabrication. J Surg Educ 17:14–17 [DOI] [PubMed] [Google Scholar]
- 9.A factory on your desk. Manufacturing: producing solid objects, even quite complex ones, with 3D printers is gradually becoming easier and cheaper. The Economist 3, September 2009. Accessed 15 Mar 2015
- 10.3D printing scales up. The Economist 3, September 2013. Accessed 15 Mar 2015
- 11.Kutikov A, Uzzo RG (2009) The RENAL nephrometry score: a comprehensive standardized system for quantitating renal tumor size, location and depth. J Urol 182:844–853 [DOI] [PubMed] [Google Scholar]
- 12.Ficarra V, Novara G, Secco S et al. (2009) Preoperative aspects and dimensions used for an anatomical (PADUA) classification of renal tumours in patients who are candidates for nephron-sparing surgery. Eur Urol 56:786–793 [DOI] [PubMed] [Google Scholar]


