Abstract
Purpose
In a clinical setting, blood oxygen saturation is one of the most important vital sign indicators. A pulse oximeter is a device that measures the blood oxygen saturation and pulse rate of patients with various disorders. However, due to ethical concerns, commercially available pulse oximeters are limited in terms of calibration on critically sick patients, resulting in a significant error rate for measurement in the critical oxygen saturation range. The device’s accessibility in developing countries’ healthcare settings is also limited due to portability, cost implications, and a lack of recognized need. The purpose of this study was to develop a reliable, low-cost, and portable pulse oximeter device with improved accuracy in the critical oxygen saturation range.
Methods
The proposed device measures oxygen saturation and heart rate using the reflectance approach. The rechargeable battery and power supply from the smartphone were taken into account, and the calibration in critical oxygen saturation values was performed using Prosim 8 vital sign simulator, and by comparing with a standard pulse oximeter device over fifteen iterations.
Results
The device’s prototype was successfully developed and tested. Oxygen saturation and heart rate readings were both accurate to 97.74% and 97.37%, respectively, compared with the simulator, and an accuracy of 98.54% for the measurement of blood oxygen saturation was obtained compared with the standard device.
Conclusion
The accuracy of oxygen measurement attained in this study is significant for measuring oxygen saturation for patients in critical care, anesthesia, pre-operative and post-operative surgery, and COVID-19 patients. The advancements made in this research have the potential to increase the accessibility of pulse oximeter in resource limited areas.
Keywords: blood oxygen saturation, pulse oximeter, accuracy, low-cost, portable, critical oxygen saturation range
Introduction
Health risks are on the rise these days, putting millions of people’s lives in danger. Cardiovascular disorders are on the rise, with more than 8 million people dying each year as a result of hypertension. Acute respiratory infections, on the other hand, account for 142 per 1000 live births.1 In these conditions, oxygen therapy is critical for patient care under proper monitoring of blood oxygen saturation.2,3 Patients in emergency situations, those under anesthesia, those in critical care, and those undergoing pre-operative and post-operative surgery all require oxygen saturation monitoring in order to avoid hypoxia.4–6
Pulse oximetry (PO) is a non-invasive technique for measuring peripheral oxygen saturation (SpO2) that is based on the differential absorption of red and infrared light by oxygenated hemoglobin in a small tissue segment.7 In high-income countries’ healthcare settings, PO is commonly used to monitor cardiovascular and respiratory system functionality and it has been designated the “fifth vital sign” in pediatrics.8,9
While pulse oximetry is also a reliable and non-invasive method for identifying children with hypoxemia and monitoring patients during emergency, anesthesia, critical care, pre-operative, and post-operative procedures by measuring non-invasive peripheral oxygen saturation (SpO2),5,6 it is rarely available outside of higher-level facilities in resource-constrained countries due to limited portability, cost implications, and a lack of perceived need among policymakers.7 Pulse oximeters were designed to increase accuracy and performance while focusing on improving accessibility in low-resource settings, resulting in higher referral rates and, ultimately, better health outcomes. This is in part due to a greater emphasis on the necessity of improved access to pulse oximeters and oxygen therapy in Sub-Saharan Africa and Southeast Asia.10–12 According to the feasibility studies conducted recently, health workers in these settings can use these devices effectively,13,14 but usage still remains low.15,16 The current COVID-19 pandemic has posed significant challenges to these settings in terms of access to pulse oximeters because to its influence on lung functionality and the device’s requirement to access blood oxygen saturation in order to administer oxygen therapy.17
Several advanced pulse oximeters have been recently developed. For instance, Huang et al18 developed a ring-type pulse oximeter with a multi-detector and obtained an SPO2 correlation of 98.26% compared with a commercially available pulse oximeter without considering the measurement of oxygen saturation below 80%, the measurement of heart rate, and device accessibility in resource limited areas. In the same manner, Lin et al19 developed a wearable and wireless finger base-type pulse oximeter, focusing only on the measurement of oxygen saturation. Smartphone app pulse oximeters have also been developed with a wide range of accuracy, but the accessibility and reliability of these developments are limited.20 In addition to these, in developing countries, the high initial cost, pulse oximeter probe fragility, and inadequate electricity supply are the main barriers to the access of pulse oximeter.21
In this study, a new prototype of a low-cost portable pulse oximeter device with better accuracy in the critical oxygen saturation region was developed, built, and tested. The device monitors blood oxygen saturation and heart rate via the right index finger and was built with a wide range of calibration compared to previous devices. It has multiple power supply options with increased durability to facilitate device accessibility in resource poor settings.
Materials and Methods
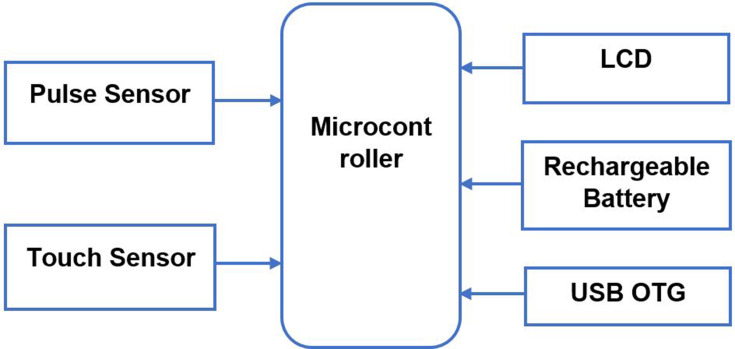
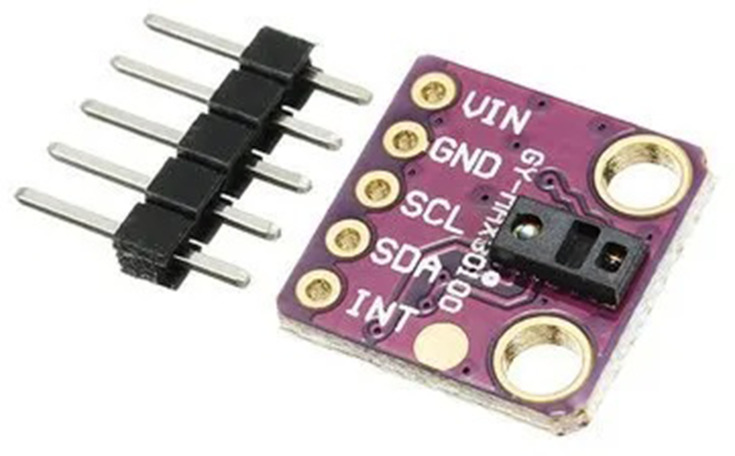
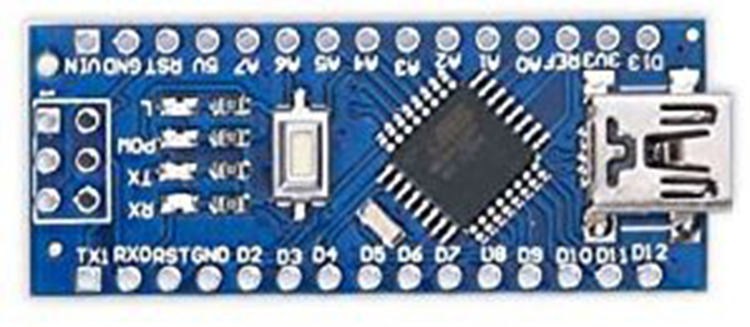
The block diagram of the proposed low-cost portable pulse oximeter device is shown in Figure 1. It is made up of two input sensors, a microcontroller, batteries, and a single output device. MAX30100 is used to monitor the heart rate and the oxygen saturation (SpO2) in the blood. The MAX30100, shown in Figure 2, is an integrated pulse oximetry and heart rate sensor. It employs two light-emitting diodes (LEDs), a photodetector, improved optics, and low-noise signal processing to detect pulse oximetry and heart rate signals.22 Two LEDs in this sensor emit two wavelengths of light (red and infrared). The reflected light is then collected and processed to calculate two biomarkers, the pulse rate and the SpO2. This sensor is connected to an Arduino nano microcontroller (Figure 3), which serves as the system’s brain, through the I2C protocol. I2C is a popular serial communication technology that is used in embedded devices. Finally, a touch sensor is utilized to determine whether the patient has correctly placed his or her finger on the pulse sensor.
Figure 1.
Block diagram of the proposed pulse oximeter device.
Figure 2.
GY-MAX30100 pulse oximeter and heart rate sensor. Image reproduced with permission from Maxim Integrated. 22
Figure 3.
Arduino nano microcontroller. Image reproduced with permission from Arduino .45
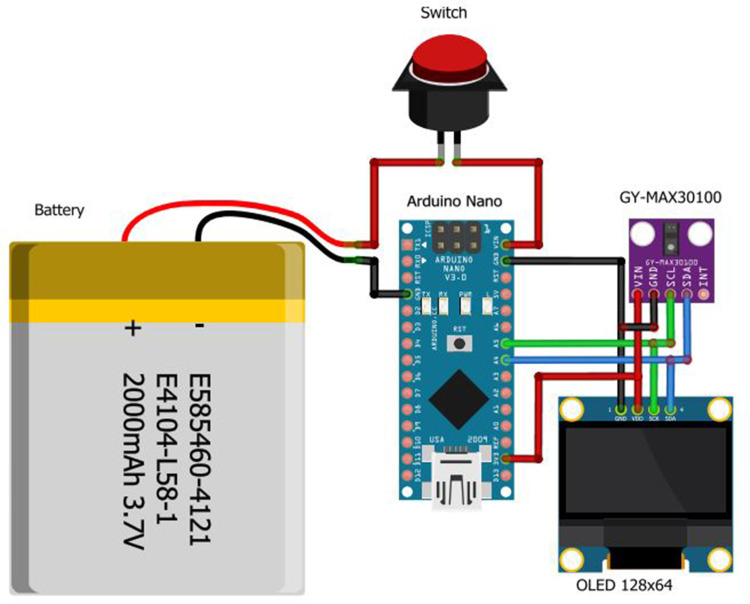
The measurement results will be shown on an OLED 124×64 display. It has a 1.8-inch screen. The pulse oximeter is powered by 3.7 V lithium-ion batteries with a capacity of 2000 mAh and also from a smartphone using USB OTG (on-the-Go). The energy in the batteries is sufficient to run the device continuously for approximately 13 hours, and they can be charged through the charger port. The power supply from the smartphone is used when the battery runs out and charging is not feasible. Figure 4 shows the wiring diagram for the low-cost portable pulse oximeter.
Figure 4.
The wiring diagram of the proposed pulse oximeter device.
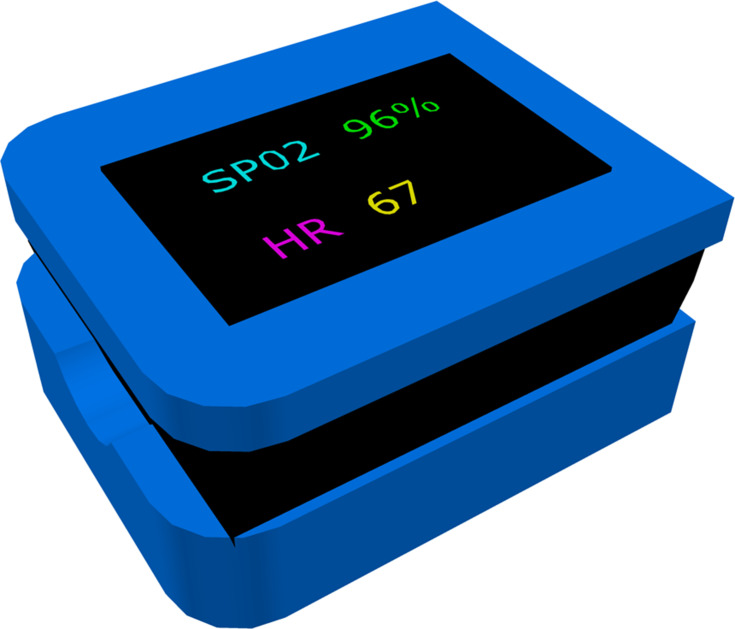
The device’s 3D design was developed using Automated Computer Aided Design (AutoCAD) software, as illustrated in Figure 5, and the actual device body was produced using a 3D printer. The program code was written in C using an open-source Arduino sketch.
Figure 5.
3D design of the proposed pulse oximeter device designed on AutoCAD software.
Results
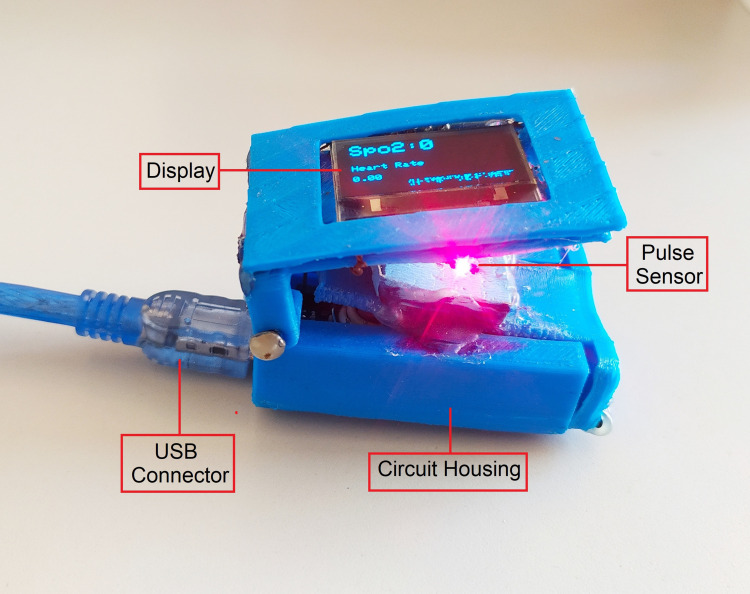
The block diagram, electronic components, the wiring diagram, and the 3D design of the proposed low-cost portable pulse oximeter (ie, Figures 1– 5) were successfully assembled, and the prototype is constructed as shown in Figure 6. The online resource 1 shows a demonstration of the low-cost portable pulse oximeter’s operation. The prototype was tested using a ProSim 8 vital signs simulator from Fluke Biomedical and by comparing it with a standard pulse oximeter device to check its accuracy by taking fifteen iterations as shown in Table 1. Pulse rate, and SpO2 at different levels were given using the simulator through the artificial finger placed on the prototype, and the measurement by the developed device was compared against the given parameters. The percentage errors for the measurement of SPO2 and HR were computed using Equation 1–3.23
 |
(1) |
 |
(2) |
 |
(3) |
Figure 6.
Final prototype of the proposed pulse oximeter device.
Table 1.
Evaluation of Our Device with Vital Sign Simulator and Standard Pulse Oximeter Device
| Iteration Number | Test on Prosim 8 Vital Sign Simulator | Comparison with Standard Device | |||||||
|---|---|---|---|---|---|---|---|---|---|
| SPO2 Test | Heart Rate Test | SPO2 Test | |||||||
| Values from the Simulator | Measurement by Our Prototype | % Error | Values from the Simulator | Measurement by Our Prototype | % Error | Measurement by Standard Pulse Oximeter | Measurement by Our Prototype | % Error | |
| 1 | 70 | 67 | 4.29 | 120 | 123 | 2.50 | 68 | 67 | 1.47 |
| 2 | 72 | 69 | 4.17 | 115 | 117 | 1.74 | 70 | 69 | 1.43 |
| 3 | 74 | 71 | 4.07 | 110 | 113 | 2.73 | 73 | 71 | 2.74 |
| 4 | 76 | 74 | 2.63 | 105 | 107 | 1.90 | 75 | 74 | 1.33 |
| 5 | 78 | 76 | 2.56 | 100 | 103 | 3.00 | 77 | 76 | 1.30 |
| 6 | 80 | 78 | 2.5 | 95 | 98 | 3.16 | 79 | 78 | 1.27 |
| 7 | 81 | 79 | 2.47 | 90 | 92 | 2.22 | 80 | 79 | 1.25 |
| 8 | 83 | 81 | 2.41 | 85 | 86 | 1.18 | 83 | 81 | 2.41 |
| 9 | 85 | 83 | 2.35 | 80 | 80 | 0.00 | 84 | 83 | 1.19 |
| 10 | 88 | 86 | 2.27 | 75 | 76 | 1.33 | 88 | 86 | 2.27 |
| 11 | 90 | 89 | 1.11 | 70 | 71 | 1.43 | 90 | 89 | 1.11 |
| 12 | 93 | 92 | 1.08 | 65 | 66 | 1.54 | 93 | 92 | 1.08 |
| 13 | 95 | 96 | 1.05 | 60 | 62 | 3.33 | 96 | 96 | 0.00 |
| 14 | 97 | 97 | 0 | 55 | 52 | 5.45 | 98 | 97 | 1.02 |
| 15 | 99 | 98 | 1.01 | 50 | 46 | 8.00 | 100 | 98 | 2.00 |
| Average % Error | 2.26 | 2.63 | 1.46 | ||||||
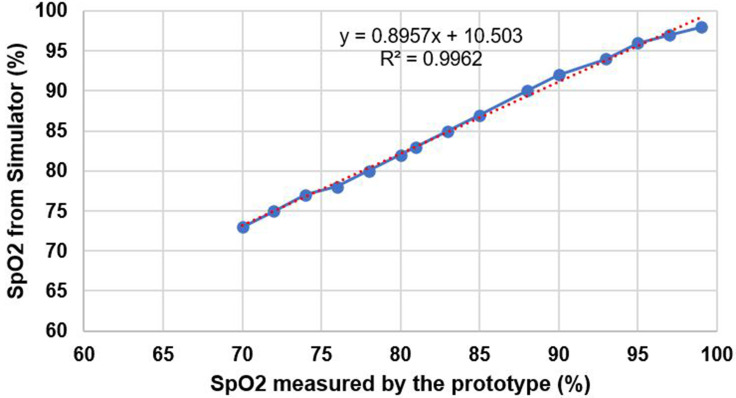
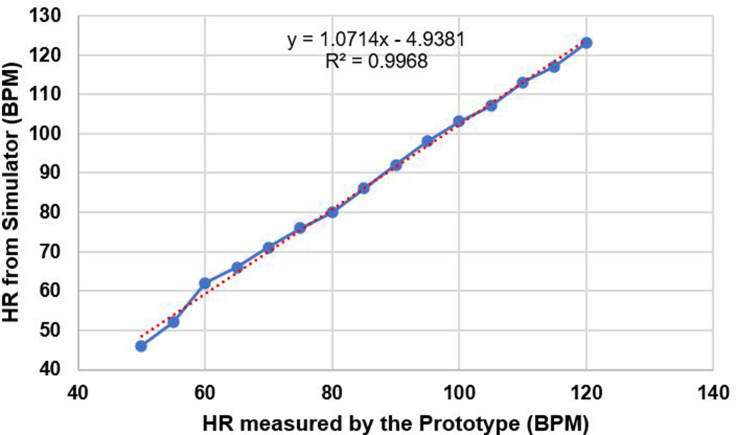
Based on the percentage error calculation, the average accuracy for measuring SPO2 and heart rate was 97.74% and 97.37%, respectively, on the simulator, while an average accuracy of 98.54% was obtained for SPO2 measurement when compared with the standard pulse oximeter device. Figure 7 depicts the calibration curve for SPO2 measurement using the simulator, whereas Figure 8 depicts the calibration curve for heart rate measurement. In addition to the accuracy test, the device’s cost effectiveness was assessed by estimating the cost of materials used to construct the prototype, which came to $13.24.
Figure 7.
Calibration curve of SPO2 measurement.
Figure 8.
Calibration curve of heart rate measurement.
Discussion
The measurement of blood oxygen saturation is becoming a standard screening tool in clinical settings in order to determine the respiratory system’s performance.24,25 The pulse oximeter is essential in emergency medicine, critical care, anesthetic delivery, and pre-operative and post-operative surgery to appropriately monitor the status of patients for remedial action to reduce mortality and morbidity.4,5,26,27 The use of pulse oximeters is especially critical at all levels of health care facilities for monitoring COVID-19 patients since it produces silent hypoxia without shortness of breath28 which results in lung injury, additional problems, and death.29,30 Detection of this silent hypoxia in COVID-19 patients at an early stage is therefore of significant importance to prevent morbidity and mortality in these patients.31,32
The development of pulse oximeters for enhanced accessibility and accuracy should take into account their practical constraints such as calibration of measurement accuracy in the critical oxygen saturation range, portability, power requirement, and cost.33–36 Measurement inaccuracy is expected with commercially available pulse oximeters for critically ill patients due to ethical issues about calibrating the device on ill patients, resulting in substantial deviations in measurement,37 despite the significance of accurately monitoring the blood oxygen saturation of critically ill patients receiving oxygen therapy.26,38–40
In this study, a low-cost portable pulse oximeter with improved accuracy and accessibility was developed. In comparison to recently developed pulse oximeters such as the ring type wearable pulse oximeter, which has an SPO2 measurement accuracy of 98.26%18 and the deluxe hand-held pulse oximeter, which has an SPO2 average measurement accuracy of 97.67%,41 our device has a better SPO2 measurement accuracy of 98.54%. Taking the power issue into account, the deluxe handheld pulse oximeter uses non-rechargeable AA batteries,41 which are not affordable in resource poor settings. But in our device, we have used a rechargeable battery and an option to power the device from a smartphone.
Apart from the inclusion of multiple power supply options, the developed prototype has the advantage of low power consumption and good results in low peripheral perfusion situations, which is comparable to existing reflective type pulse oximeters.42,43 The device is inexpensive ($13.24) when compared to commercially available finger pulse oximeters, which cost $20 - $50 without import and taxation costs,21 and handheld pulse oximeters, which can cost up to $266.41 The obtained average accuracy of oxygen saturation measurement and heart rate measurements are in the recommended accuracy range for finger pulse oximeters, such as ±3% for oxygen saturation and ±3 bpm for heart rate,44 and this could be further improved by proper attenuation of the ambient light.
Conclusion
The accuracy of oxygen measurement achieved in this study is significant for measuring oxygen saturation of patients in critical care, under anesthesia, pre-operative and post-operative surgery, and patients with COVID-19 due to the requirement for measurement accuracy for these patients. The device’s accuracy, durability, portability, and low cost will make it more accessible to patients, thereby improving their lives by lowering mortality and morbidity. The developed pilot prototype is intended to be a trustworthy tool for patient monitoring in a clinical setting with enhanced finger attachment and ambient light prevention during measurement.
Acknowledgments
We would like to thank Jimma University, Jimma Institute of Technology, and School of Biomedical Engineering.
Funding Statement
This work was supported by Jimma University through COVID-19 research projects with grant number CBE/CS/JiT/16/13. Author H.D. has received research support from Jimma University.
Abbreviations
AutoCAD, automated computer aided design; BPM, breaths per minute; 3D, three dimensional; HR, heart rate; LED, light emitting diodes; LCD, liquid crystal display; OLED, organic light emitting diode; OTG, On-The-Go; PO, pulse oximeter; SPO2, spot oxygen saturation; USB, universal serial bus.
Ethical Approval
This study does not involve human subjects. No ethical approval is required.
Author Contributions
All authors made a significant contribution to the work reported, whether that is in the conception, study design, execution, acquisition of data, analysis and interpretation, or in all these areas; took part in drafting, revising or critically reviewing the article; gave final approval of the version to be published; have agreed on the journal to which the article has been submitted; and agree to be accountable for all aspects of the work.
Disclosure
The authors have no relevant financial or non-financial interests to disclose in this work.
References
- 1.Kumar A, Chattree G, Periyasamy S. Smart healthcare monitoring system. Wirel Pers Commun. 2018;101(1):453–463. doi: 10.1007/S11277-018-5699-0 [DOI] [Google Scholar]
- 2.Heffner JE. The story of oxygen. Respir Care. 2013;58(1):18–30. doi: 10.4187/RESPCARE.01831 [DOI] [PubMed] [Google Scholar]
- 3.Marciniuk DD, Schraufnagel DE, Ferkol T, et al. Forum of international respiratory societies. Global Impact Respir Dis. 2017;4:54. [Google Scholar]
- 4.Jubran A. Pulse oximetry. Crit Care. 2015;19(1):1–7. doi: 10.1186/s13054-015-0984-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pedersen T, Nicholson A, Hovhannisyan K, Møller AM, Smith AF, Lewis SR. Pulse oximetry for perioperative monitoring. Cochrane Database Syst Rev. 2014;2014(3). doi: 10.1002/14651858.CD002013.PUB3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Suzuki S. Oxygen administration for postoperative surgical patients: a narrative review. J Intensive Care. 2020;8(1):1–6. doi: 10.1186/S40560-020-00498-5/TABLES/1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Duke T, Subhi R, Peel D, Frey B. Pulse oximetry: technology to reduce child mortality in developing countries. Ann Trop Paediatr. 2009;29(3):165–175. doi: 10.1179/027249309X12467994190011 [DOI] [PubMed] [Google Scholar]
- 8.Salyer JW. Neonatal and pediatric pulse oximetry. Respir Care. 2003;48(4):386–388. [PubMed] [Google Scholar]
- 9.Mower WR, Sachs C, Nicklin EL, Baraff LJ. Pulse oximetry as a fifth pediatric vital sign. Pediatrics. 1997;99(5):681–686. doi: 10.1542/PEDS.99.5.681 [DOI] [PubMed] [Google Scholar]
- 10.Floyd J, Wu L, Hay Burgess D, Izadnegahdar R, Mukanga D, Ghani AC. Evaluating the impact of pulse oximetry on childhood pneumonia mortality in resource-poor settings. Nature. 2015;528(7580):S53–S59. doi: 10.1038/NATURE16043 [DOI] [PubMed] [Google Scholar]
- 11.Herbert LJ, Wilson IH. Pulse oximetry in low-resource settings. Breathe. 2014;9(2):90–97. doi: 10.1183/20734735.038612 [DOI] [Google Scholar]
- 12.Hamid MA, Chandna A, Siddiqui S, Fayyaz J. Pulse oximetry: a reliable and cost effective screening tool in children with pneumonia for developing countries. J Pak Med Assoc. 2016;66(8):1015–1018. [PubMed] [Google Scholar]
- 13.McCollum ED, King C, Deula R, et al. Pulse oximetry for children with pneumonia treated as outpatients in rural Malawi. Bull World Health Organ. 2016;94(12):893–902. doi: 10.2471/BLT.16.173401 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Emdin CA, Mir F, Sultana S, et al. Utility and feasibility of integrating pulse oximetry into the routine assessment of young infants at primary care clinics in Karachi, Pakistan: a cross-sectional study. BMC Pediatr. 2015;15(1):1–11. doi: 10.1186/S12887-015-0463-Z/TABLES/4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Graham HR, Ayede AI, Bakare AA, et al. Oxygen for children and newborns in non-tertiary hospitals in South-west Nigeria: a needs assessment. Afr J Med Med Sci. 2016;45(1):31–49. [PubMed] [Google Scholar]
- 16.Graham H, Tosif S, Gray A, et al. Providing oxygen to children in hospitals: a realist review. Bull World Health Organ. 2017;95(4):288. doi: 10.2471/BLT.16.186676 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.World Health Organization. Clinical management of Severe Acute Respiratory Infection (SARI) when COVID-19 disease is suspected: interim guidance. World Health Organization; 2020. [Google Scholar]
- 18.Huang CY, Chan MC, Chen CY, Lin BS. Novel wearable and wireless ring-type pulse oximeter with multi-detectors. Sensors. 2014;14(9):17586–17599. doi: 10.3390/S140917586 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lin BS, Huang CY, Chen CY, Lin JH. Design of a finger base-type pulse oximeter. Rev Sci Instrum. 2016;87(1):013108. doi: 10.1063/1.4940237 [DOI] [PubMed] [Google Scholar]
- 20.Jordan TB, Meyers CL, Schrading WA, Donnelly JP. The utility of iPhone oximetry apps: a comparison with standard pulse oximetry measurement in the emergency department. Am J Emerg Med. 2020;38(5):925. doi: 10.1016/J.AJEM.2019.07.020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Herbert LJ, Wilson IH. Pulse oximetry in low-resource settings. Breathe. 2012;9(2):90–98. doi: 10.1183/20734735.038612 [DOI] [Google Scholar]
- 22.MAX30100 pulse oximeter and heart-rate sensor IC for wearable health | Maxim Integrated. Available from: https://www.maximintegrated.com/en/products/sensors/MAX30100.html?__cf_chl_managed_tk__=.DurUSpxq8Vq0QOFjc0AA129N2Kxy3R.CCTTVZNbDIo-1642763294-0-gaNycGzNCFE#tech-docs. Accessed January 21, 2022.
- 23.Dese K, Ayana G, Lamesgin Simegn G. Low cost, non-invasive, and continuous vital signs monitoring device for pregnant women in low resource settings (Lvital device). HardwareX. 2022;11:e00276. doi: 10.1016/J.OHX.2022.E00276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Walton RAL, Hansen BD. Venous oxygen saturation in critical illness. J Vet Emerg Crit Care. 2018;28(5):387–397. doi: 10.1111/VEC.12749 [DOI] [PubMed] [Google Scholar]
- 25.Hartog C, Bloos F. Venous oxygen saturation. Best Pract Res Clin Anaesthesiol. 2014;28(4):419–428. doi: 10.1016/J.BPA.2014.09.006 [DOI] [PubMed] [Google Scholar]
- 26.Martin DS, Grocott MPW. Oxygen therapy in critical illness: precise control of arterial oxygenation and permissive hypoxemia. Crit Care Med. 2013;41(2):423–432. doi: 10.1097/CCM.0B013E31826A44F6 [DOI] [PubMed] [Google Scholar]
- 27.Sun Z, Sessler DI, Dalton JE, et al. Postoperative hypoxemia is common and persistent: a prospective blinded observational study. Anesth Analg. 2015;121(3):709. doi: 10.1213/ANE.0000000000000836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Harun MAA, Hossain MM, Bari MA, et al. Pulse oximetry is essential in home management of elderly COVID-19 patients. Bangladesh J Otorhinolaryngol. 2020;26(1):55–67. doi: 10.3329/BJO.V26I1.47954 [DOI] [Google Scholar]
- 29.Jouffroy R, Jost D, Prunet B. Prehospital pulse oximetry: a red flag for early detection of silent hypoxemia in COVID-19 patients. Crit Care. 2020;24(1). doi: 10.1186/S13054-020-03036-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Luks AM, Swenson ER. Pulse oximetry for monitoring patients with COVID-19 at home. potential pitfalls and practical guidance. Ann Am Thorac Soc. 2020;17(9):1040–1046. doi: 10.1513/ANNALSATS.202005-418FR [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Wilkerson RG, Adler JD, Shah NG, Brown R. Silent hypoxia: a harbinger of clinical deterioration in patients with COVID-19. Am J Emerg Med. 2020;38(10):2243.e5. doi: 10.1016/J.AJEM.2020.05.044 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Teo J. Early detection of silent hypoxia in Covid-19 Pneumonia using smartphone pulse oximetry. J Med Syst. 2020;44(8). doi: 10.1007/S10916-020-01587-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Seifi S, Khatony A, Moradi G, Abdi A, Najafi F. Accuracy of pulse oximetry in detection of oxygen saturation in patients admitted to the intensive care unit of heart surgery: comparison of finger, toe, forehead and earlobe probes. BMC Nurs. 2018;17(1). doi: 10.1186/S12912-018-0283-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Gürün Kaya A, Öz M, Akdemir Kalkan İ, et al. Is pulse oximeter a reliable tool for non-critically ill patients with COVID-19? Int J Clin Pract. 2021;75(12). doi: 10.1111/IJCP.14983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Nitzan M, Romem A, Koppel R. Pulse oximetry: fundamentals and technology update. Med Dev. 2014;7(1):231. doi: 10.2147/MDER.S47319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hess DR. Pulse oximetry: beyond SpO2. Respir Care. 2016;61(12):1671–1680. doi: 10.4187/RESPCARE.05208 [DOI] [PubMed] [Google Scholar]
- 37.Durbin CG, Rostow SK. More reliable oximetry reduces the frequency of arterial blood gas analyses and hastens oxygen weaning after cardiac surgery: a prospective, randomized trial of the clinical impact of a new technology. Crit Care Med. 2002;30(8):1735–1740. doi: 10.1097/00003246-200208000-00010 [DOI] [PubMed] [Google Scholar]
- 38.Batchelder PB, Raley DM. Maximizing the laboratory setting for testing devices and understanding statistical output in pulse oximetry. Anesth Analg. 2007;105(6Suppl):S85–S94. doi: 10.1213/01.ANE.0000268495.35207.AB [DOI] [PubMed] [Google Scholar]
- 39.Perkins GD, McAuley DF, Giles S, Routledge H, Gao F. Do changes in pulse oximeter oxygen saturation predict equivalent changes in arterial oxygen saturation? Crit Care. 2003;7(4):R67. doi: 10.1186/CC2339 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Wilson BJ, Cowan HJ, Lord JA, Zuege DJ, Zygun DA. The accuracy of pulse oximetry in emergency department patients with severe sepsis and septic shock: a retrospective cohort study. BMC Emerg Med. 2010;10. doi: 10.1186/1471-227X-10-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Deluxe Handheld Pulse Oximeter. SpO2 monitor for adults & children. Available from: https://www.concordhealthsupply.com/Deluxe-Handheld-Pulse-Oximeter-p/cci-300m.htm?fbclid=IwAR3JXUIjTJv6T9aWoeQwiBROTTU0ErD_Fqh429f0f_8FxXUr_AaZdQHsv0A. Accessed February 16, 2022.
- 42.Agashe GS, Coakley J, Mannheimer PD. Forehead pulse oximetry: headband use helps alleviate false low readings likely related to venous pulsation artifact. Anesthesiology. 2006;105(6):1111–1116. doi: 10.1097/00000542-200612000-00010 [DOI] [PubMed] [Google Scholar]
- 43.Mendelson Y, Ochs BD. Noninvasive pulse oximetry utilizing skin reflectance photoplethysmography. IEEE Trans Biomed Eng. 1988;35(10):798–805. doi: 10.1109/10.7286 [DOI] [PubMed] [Google Scholar]
- 44.Pan American Health Organization.Technical and regulatory aspects of the use of pulse oximeters in monitoring COVID-19 patients. 2020;(August): 1–18.
- 45.Arduino. Arduino board nano. Available from: https://www.arduino.cc/en/pmwiki.php?n=Main/ArduinoBoardNano. Accessed February 17, 2022.