Abstract
Background
The COVID-19 pandemic in 2020 resulted in the older population being asked to remain at home and avoid other people outside their household. This could have implications for both receipt and provision of informal caring.
Objective
To determine if informal care provision by older carers changed during the first wave of the COVID-19 pandemic from pre-pandemic care and if this was associated with a change in mental health and well-being of carers.
Design and setting
Longitudinal nationally representative study of community dwelling adults from The Irish Longitudinal Study on Ageing (TILDA) (Waves 3-COVID-Wave 6).
Methods
We studied a cohort of 3670 adults aged ≥60 in Ireland during the COVID-19 pandemic (July-November 2020) and compared with previous data collections from the same cohort between 2014-2018. Independent variables were caregiving status and caregiving intensity, outcome measures included depressive symptoms (CES-D8), Perceived Stress (PSS4) and Quality of life (CASP12). Mixed models adjusting for socio-demographics and physical health were estimated.
Results
Caregiving increased from 8.2% (2014) to 15.4% (2020). Depression, and stress scores increased while quality of life decreased for all participants. Carers reported poorer mental health, and higher caring hours were associated with increased depression and stress and decreased quality of life scores on average, and increased depression was higher for women.
Conclusions
Informal caregiving increased during the pandemic and family caregivers reported increased adverse mental health and well-being and this continued throughout the early months of the pandemic. The disproportionate burden of depression was highest in women providing higher caring hours.
Keywords: Caring, Ageing, COVID-19, Quality of life, Depressive symptoms, Perceived stress
1. Introduction
The COVID-19 pandemic caused by the virus severe acute respiratory syndrome coronavirus (SARS-Cov-2) emerged across the world since January 2020 and continues in widespread transmission. A pandemic was declared in March 2020 by the World Health Organization and has globally to-date (December 2021) caused 262.9 million cases and 5.2 million deaths, in Ireland there were cumulatively 725.3 thousand cases and 21.6 thousand deaths. (World Health Organization, 2020b) disproportionately affecting the older population (Carr, 2020).
Public health responses have varied between countries as subsequent epidemic waves have passed through countries, including movement restrictions, physical distancing, and limits on home visits in Ireland (Department of the Taoiseach, 2020). These restrictions to reduce transmission will impact on multiple population domains including social, psychological, health and economic, with unequal consequences for people within communities and globally (Carr, 2020; Iob et al., 2020; Marmot, 2020; World Health Organization, 2020a). Over and above the direct effect of COVID-19 infection, the pandemic has led to increased mental health difficulties and decreased well-being through worry (Kivi et al., 2020), vulnerability (Knepple Carney et al., 2020), stress, loneliness, and reduced social contact and engagements (Lebrasseur et al., 2021; Morina et al., 2021). Additionally physical health has been impacted through reduced physical activity, and disruption of normal routines (Morina et al., 2021).
Most carers in Ireland (52.7%) are aged between 40-54, however, older carers have increased between 2011 and 2016, with the largest percentage increase seen among those aged ≥85 years (34.7%) (Central Statistics Office, 2017). Ireland had the highest proportion of persons aged under 15 in the European Union (EU) (32.5%), as a proportion of those aged 15-54, and the second-lowest proportion of persons aged 65 and over (17.9%) (Central Statistics Office, 2014). These differences in the proportion of available adults to provide care, and the increased proportion of younger dependents in Ireland, particularly as the need for informal caregiving increases, with continued pressures on formal state-provided services, suggest that there may also be a differential proportion of informal caregiving to adult children and grandchildren, in addition to older relatives, amongst the older population in Ireland compared to other EU countries. The potential impact of the COVID-19 pandemic on family caregivers has received attention worldwide, cross sectional (Boutoleau-Bretonnière et al., 2020; Budnick et al., 2021; Greaney et al., 2021; Taniguchi et al., 2022), and repeated cross sectional studies of carers have been carried out during the pandemic (Noguchi et al., 2021; Zwar König and Hajek, 2021), however longitudinal quantitative data are sparse. One longitudinal study of adults aged 50 years and over carried out between June and August 2020 across 26 European countries found that parental caregivers who increased caregiving had increased depression and anxiety. Frequency of providing care to parents increased across most European countries, while care for children decreased (Bergmann & Wagner, 2021). Two cross sectional studies of caregivers during 2020 carried out in Ireland found increased psychological distress among caregivers about their own health and the care recipient (The Alzheimer Society of Ireland, 2020a, 2020b), However, no longitudinal study has examined the well-being of carers in Ireland both before and during the COVID-19 pandemic.
Although the phenomenon of the ‘sandwich generation’, caring for older parents with dependent children, is well described prior to the pandemic (McGarrigle et al., 2014), the numbers of older carers reporting caring and the subsequent effects on mental health and well-being are less well understood in Ireland. Formal social care in Ireland is provided on a means-tested basis, funded via the Health Service Executive (HSE) and provided through its network of local health offices, although it is limited by a finite budget. While community care services use in Ireland increases with frailty and disability (O'Halloran et al., 2021), a substantial proportion of caring for older adults is unpaid, informal care by a family member (McGarrigle & Kenny, 2020; McGarrigle et al., 2014, 2018). Caring networks are complex and transitions into and out of the caring role, in addition to sharing tasks with other more specialized caregivers becomes increasingly important, particularly as the care recipient's health decreases (Spillman et al., 2020).
Caring is generally associated with good health when care hours are low. There is strong evidence supporting the health benefits of remaining physically and socially active which lower caring hours may facilitate. Supporting research shows that carers are healthier and demonstrate better mood than non-carers (Beach et al., 2000; Freedman et al., 2014; McGarrigle et al., 2014, 2018). These benefits were mainly seen for women, as were the detrimental effects of high caring hours, for physical health, lower quality of life and higher depressive symptoms (McGarrigle et al., 2014, 2018). Similarly, the impact of care-giving on risk of mortality differs: some prospective studies documenting an increased risk of mortality among caregivers that rises with the amount of self-reported strain experienced (Perkins et al., 2013), others have reported reduced risk of mortality among caregivers (O'Reilly et al., 2008, 2017).
Previous research examining the longitudinal effects of transitioning into family caregiving in general population studies has found that over time, caregiving was associated with worse well-being and increased depression in a general population sample (Haley et al., 2020; Marks et al., 2002). The care recipient was important, and caring for friends was associated with better well-being outcomes for women, while spousal caring was worse for women (Marks et al., 2002), although gender was found not to differ in a more recent study caring for a spouse was associated with worse mental health (Haley et al., 2020).
The theoretical background for this study builds on several bodies of research, reflected in the research about underlying mechanisms that promote health as people age, stress theory and social engagement. Theories underpinning the relationship between social participation and health include Durkheim's work on social integration and suicide, and role accumulation theory. Berkman and colleagues have conceptualized the pathway from social through psychobiological processes with health (Berkman et al., 2000). Activity restriction theory (Williamson & Shaffer, 2000) supports the role of social participation as a mediator between caregiving (and stressors) and health outcomes (Bookwala & Schulz, 2000). Meta-analysis found that activity restriction on caregivers was associated with increased depressive symptoms in support of the activity restriction model of depressed affect (Mausbach et al., 2011). Mausbach and colleagues found increased stress was associated with increased activity restriction and accounted for some of the relationship between stress and depressive symptoms in spouse caregivers of Alzheimer's patients (Mausbach et al., 2012). Furthermore, reduced activity restriction has been found to buffer the relationship between chronic stress and sympathetic nervous system activation in caregivers (Ho et al., 2014).
The initial public health response to the COVID-19 pandemic in Ireland recommended that older people aged ≥70 years remain at home, and physically isolate from people outside their household (Department of the Taoiseach, 2020). This may have affected both care receipt and care provision by the older population as maintaining these activities could be challenging with travel restrictions and recommended physical distancing. Additionally, staff redeployment to acute care during this period resulted in an estimated 40% reduction and 30% suspension of state-provided older person services including home help and personal care attendants (Health Service Executive, 2020).
This study aimed to determine if the prevalence of informal caring changed during the COVID-19 pandemic in Ireland and examine longitudinal trends in mental health and well-being, including quality of life, depressive symptoms, and perceived stress, in carers. We considered the following hypotheses:
-
•
COVID-19 and the accompanying restriction measures led to an increase in the frequency of providing informal family caregiving to those who had previously relied on state-provided homecare or other family members.
-
•
COVID-19 and its accompanying restriction measures with reduced social interactions with others led to a worsening of mental health for informal caregivers.
-
•
Caregivers who have increased the hours of caregiving provided have worse trajectories in well-being and mental health than caregivers who have not increased caring hours.
2. Materials and methods
2.1. Overview of TILDA and TILDA-COVID study
We used the Irish Longitudinal Study on Ageing (TILDA), a nationally representative study of adults aged ≥50 years in the Republic of Ireland. Details of the cohort and sampling frame have been described elsewhere (Donoghue et al., 2018). Briefly, at TILDA Wave 1 (2009-2011), 8175 adults aged ≥50 (range 50-105) completed a computer-assisted personal interview (CAPI) in their home. A self-completion questionnaire (SCQ) was also returned by 85% (n=6915). Data were recollected every two years. A TILDA-COVID sub-study was carried out between July-November 2020, during the COVID pandemic, that invited all TILDA participants to complete an SCQ about their experiences during the pandemic. A total of 3,670 participants aged ≥60 years were included (response rate 71%) (Ward et al., 2021).
2.2. Study population
The current study included participants from the COVID-sub-study (COVID-Wave 6) who took part in at least one previous TILDA wave between Wave 3 (2014), when information on caring was first collected and Wave 5, an average follow-up period of 6 years. Overall, 15.4% (n=568) of participants reported caring during the pandemic: caring in previous waves is shown in Table 1 . All participants provided informed written consent. Ethical approval for the TILDA study was granted by the Research Ethics Committee of the Faculty of Health Sciences of Trinity College Dublin and the COVID-19 study from the Irish National Research Ethics Committee COVID-19 (Application number: 20-NREC-COV-030-2).
Table 1.
Characteristics of population sample by wave.
| Wave 3 | Wave 4 | Wave 5 | COVID Wave 6 | |
|---|---|---|---|---|
| N | 3599 | 3544 | 3423 | 3670 |
| Age, mean (sd) | 65.2 (8.6) | 67.4 (8.5) | 69.3 (8.5) | 70.9 (8.5) |
| Sex, n (%) | ||||
| Female | 1630 (52.7) | |||
| Male | 2037 (47.3) | |||
| Educational attainment, n (%) | ||||
| Primary | 683 (36.3) | |||
| Secondary | 1461 (43.2) | |||
| Tertiary | 1518 (20.6) | |||
| Married, n (%) | ||||
| Married | 2625 (69.6) | 2537 (68.3) | 2395 (67.1) | 2566 (67.1) |
| Never married | 295 (8.4) | 296 (8.5) | 288 (8.2) | 297 (8.2) |
| Separated/divorced | 261 (7.8) | 257 (7.7) | 240 (7.4) | 257 (7.4) |
| Widowed | 418 (14.2) | 454 (15.5) | 500 (17.3) | 524 (17.3) |
| Area of residence | ||||
| Dublin | 949 (25.2) | |||
| Other urban | 990 (28.1) | |||
| Rural | 1660 (46.7) | |||
| Informal caringa | ||||
| Caring in last month (overall) | 339 (8.2) | 240 (6.2) | 235 (6.3) | 568 (15.4) |
| Transitions in caring statusb | ||||
| No Caring | 2623 (74.6) | |||
| No Caring – previous carer stopped prior to COVID | 426 (11.0) | |||
| Continued caring | 177 (4.2) | |||
| New Carer | 386 (10.2) | |||
| State-Provided formal care | ||||
| State-provided care attendant | ||||
| No care attendant received | 3783 | 3721 | 3576 | 3044 (92.2) |
| Care received prior to COVID-19 | 4 (0.1) | 9 (0.2) | 24 (0.8) | |
| Continued to receive care attendant | 23 (1.3) | |||
| No longer received care attendant | 178 (6.6) | |||
| State-provided home help prior to COVID-19 | ||||
| No home help received | 3627 (98.5) | 3607 (96.2) | 3600 (95.4) | |
| Any home help received (state or private)c |
136 (3.8) |
149 (4.6) |
||
| State-provided home help State-provided home help during COVID-19 pandemic |
38 (1.4) | 55 (1.8) | 68 (2.5) | |
| No care received | 3009 (91.0) | |||
| Continued to receive home help | 63 (2.0) | |||
| No longer received home help | 181 (6.4) | |||
| Mental health and well-being | ||||
| Quality of life (CASP-12) mean (sd) | 27.1 (5.4) | 27.7 (5.3) | 27.7 (5.1) | 27.5 (5.4) |
| Perceived Stress (PSS4) mean (sd) | 4.0 (3.0) | 4.0 (3.0) | 4.0 (3.0) | 4.7 (2.8) |
| Depressive Symptoms (CES-D8) mean (sd) | 3.2 (3.9) | 3.1 (3.7) | 3.1 (3.6) | 5.3 (4.2) |
Note: All prevalences are weighted to account for survey design clusters and attrition. c: Receipt of private home help was only asked from Wave 4 onwards; a: data missing on informal caring for 7, 6, 13 and 22 participants respectively in Waves 3-6. b: Excludes 5 participants who report caring in Wave 6 but did not take part in Wave3-Wave 5 so no previous caring status known; c: Receipt of private home help was only asked from Wave 4 onwards.
2.3. Study measures
2.3.1. Caregiving measures
Participants were asked if they cared for someone during the COVID-19 pandemic, their relationship to the recipient (spouse, children, grandchild, other relative, friend or neighbor) and care hours/week . We created a caring intensity variable coded 0-3: No caregiving in the last week, low intensity caregiving (1-19 hours caregiving in the last week), moderate caregiving (20-49 hours in the last week), and high intensity caregiving (≥50 hours in the last week). Data from Wave 3 (2014), Wave 4 (2016) and Wave 5 (2018) were used to characterize caring hours in the pre-pandemic period. Transitions in caring status during the pandemic was defined using caring data from the COVID-Wave 6, and each previous wave participant took part in grouped as; No caring; No caring-Stopped since Wave 5; Continued to care; New carer-reported caring during the pandemic-never reported caring previously. This is detailed in Supplementary Fig. 1.
2.3.2. Outcome measures
Quality of life was measured using the Control-Autonomy-Self Realization-Pleasure (CASP-12) 12-item scale (α=0.82) (Sexton et al., 2013). Total scores (range 0-36) were calculated; higher scores indicating better quality of life.
Depressive symptoms were measured using the Centre for Epidemiological Studies Scale for Depression (CES-D8), an 8-item scale (α=0.93) (Radloff, 1977). This scale measured the frequency that participants had experienced a variety of depressive symptoms in the past week. The responses were summed giving a total score (range 0-24); higher scores indicating more depressive symptoms.
Perceived stress was measured using the Perceived Stress Scale (PSS), a 4-item scale (α=0.75) (Cohen et al., 1983). This scale measured frequency that participants appraised situations in their life as stressful in the past month. Responses were summed giving a total score (range 0-16); higher scores indicating more perceived stress.
2.3.2.1. State-provided care
Participants were asked if they continued to receive state-provided personal care attendants (a person employed by the state to assist with bathing/bodily care), or home help (a person employed by the state to help with household chores) since the pandemic outbreak: (Yes continued to receive at the same frequency; Yes, but a reduced frequency; No longer received). This was then assigned to the household in each case. Pre-pandemic state-provided care was characterized as No receipt; Received in the past year.
2.3.2.2. Covariates
We identified potential confounders that affect caring and well-being/mental health outcomes based on existing literature including demographic and socioeconomic characteristics: age, age-squared, highest educational attainment (Primary (8 years), Secondary (12 years), tertiary (>13 years) (English et al., 2019; McGarrigle et al., 2018), marital status (Married, Never Married, Separated/divorced, Widowed) (McGarrigle et al., 2014) and area of residence (Dublin, urban other, rural) (McGarrigle et al., 2014).
2.4. Statistical analyses
Prevalence estimates (95% Confidence Intervals) and means (standard deviation) are presented, weighted using inverse probability weights derived to adjust for attrition and to create estimates that were representative of the general population over time. Caring measures in each wave were compared to Wave 3 using Wald test in Table 2 . Multilevel regression analyses examined longitudinal trends in CESD-8, PSS4 and CASP12 scores by caring status and changing care hours since Wave 3, adjusting for sociodemographic variables to describe the average change in well-being and mental health in a cohort of older adults between 2014-2020 with an unstructured correlation variance to account for the clustering within the participant for estimating change. Interactions between survey wave and sex were incorporated to test the difference in caring over time, and to assess the impact of gender in the caring context. Likelihood ratio tests and the Akaike Information Criterion (AIC) were compared to estimate model fits. All analyses were carried out using Stata/MP 14.0 (StataCorp. 2015).
Table 2.
Caring hours and recipients of care by those who provided care during the COVID-19 pandemic (weighted %).
| Wave 3 | Wave 4 | Wave 5 | COVID-Wave 6 | |
|---|---|---|---|---|
| N (%) | N (%) | N (%) | N (%) | |
| Age of carers (mean, sd) | 64.1 (7.9) | 65.4 (7.3) | 67.5 (7.3)* | 69.9 (7.6)* |
| Caring in last month by age group | ||||
| 54-64a | 179 (9.0) | 115 (7.3) | 87 (7.3) | 146 (15.7)*** |
| 65-74 | 129 (7.9) | 96 (6.6) | 111 (7.2) | 265 (16.4)*** |
| 75+ | 31 (5.9) | 29 (3.3) | 37 (3.8) | 157 (14.0)*** |
| Hours of caring | ||||
| No caring | 3477 (94.9) | 3482 (96.6) | 3340 (95.8) | 3056 (88.7)*** |
| 1-19 | 131 (3.2) | 71 (1.7)*** | 68 (1.9)** | 172 (4.5)* |
| 20-49 | 43 (0.9) | 20 (0.5)* | 42 (1.3) | 109 (3.3)*** |
| 50+ | 52 (0.9) | 44 (1.2) | 46 (1.0) | 131 (3.5)*** |
| Care recipient | ||||
| Spouse | 55 (23.0) | 30 (27.7) | 41 (26.9) | 336 (61.6)*** |
| Child | 24 (13.4) | 18 (14.0) | 21 (12.8) | 52 (9.7) |
| Grandchild | 26 (9.6) | 9 (5.0)* | 24 (20.1) | 46 (9.5) |
| Other relative | 75 (33.1) | 52 (42.8) | 52 (32.0) | 71 (14.0)*** |
| Friend/neighbor | 42 (20.9) | 21 (10.5) | 17 (8.1)** | 31 (5.3)** |
Note: All prevalences are weighted to account for survey design clusters and attrition. Not all who report caring in the last month report hours of care in the last week. a: age 56-64 in Wave 4, 58-64 in Wave 5, 60-64 in Wave 6.
P-values: *<0.05, ***<0.001: reference Wave 3, Wald tests.
3. Results
The sample characteristics from Wave 3 to COVID-Wave 6 are shown in Table 1. Average age of participants during COVID-Wave 6 was 70.9, and 67.1% were married. Both home help and home care attendants receipt reduced during COVID-Wave 6 with 6.6% reporting they no longer received home care attendants and 6.4% no longer received home help. Only 2.0% and 1.3% continued receiving these services during the pandemic respectively (Table 1).
3.1. Prevalence of caring over time
Table 1 shows the changing prevalence of caring by wave. Overall, 15.4% of adults aged ≥60 reported caring for someone during the COVID-19 pandemic, increased from 6.3% in Wave 5. In COVID-Wave 6, 74.6% had never cared, 11.0% had transitioned out of caring, 4.2% continued to care, and 10.2% were new carers. Table 2 shows caring hours also increased: the proportion reporting caring ≥50 hours/week increased from 17.9% in Wave 3 to 30.9% in COVID-Wave 6. The care recipient also changed during the COVID-19 pandemic. The majority reported the main recipient of care was their spouse during this time (62%). Caring for grandchildren, other family members, neighbors and friends decreased, and caring for their spouse increased during the COVID-19 pandemic compared to previous waves (Table 2).
3.2. Well-being and mental health outcomes by caring status and caring hours
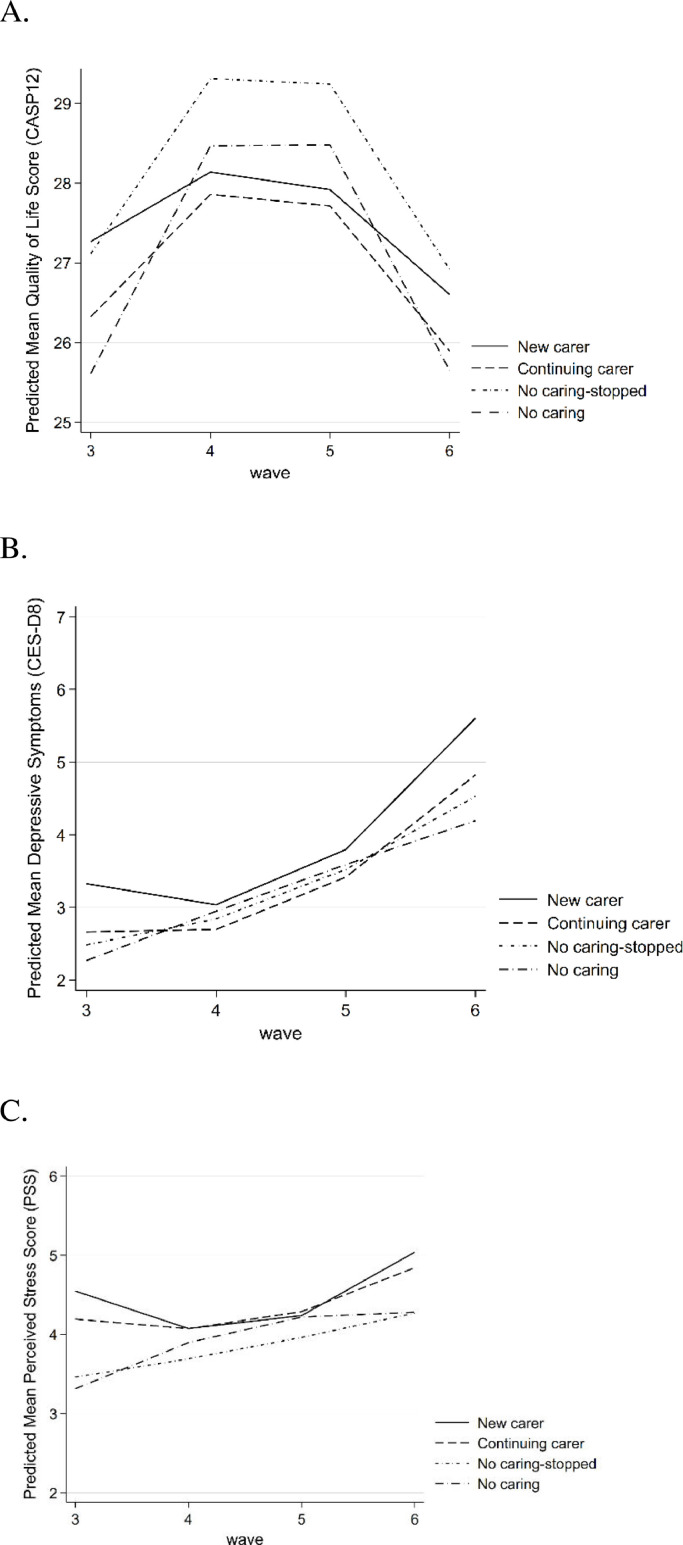
Fig. 1 shows the trajectories in quality of life, depressive symptoms and perceived stress between Wave 3 and COVID-Wave 6, in adults aged ≥60 years by caring status. Well-being trajectories were worse overall in COVID-Wave 6 relative to previous waves regardless of caring status. New carers and those continuing to care, had lower quality of life, and higher depressive symptoms and perceived stress in COVID-Wave 6 relative to non-carers.
Fig. 1.
Conditional multilevel growth model trajectories of (A) quality of life (CASP12), (B) depressive symptoms (CES-D8) and (C) perceived stress (PSS4) by caring status, Wave 3-COVID-Wave 6, the Irish Longitudinal Study on Ageing (TILDA).
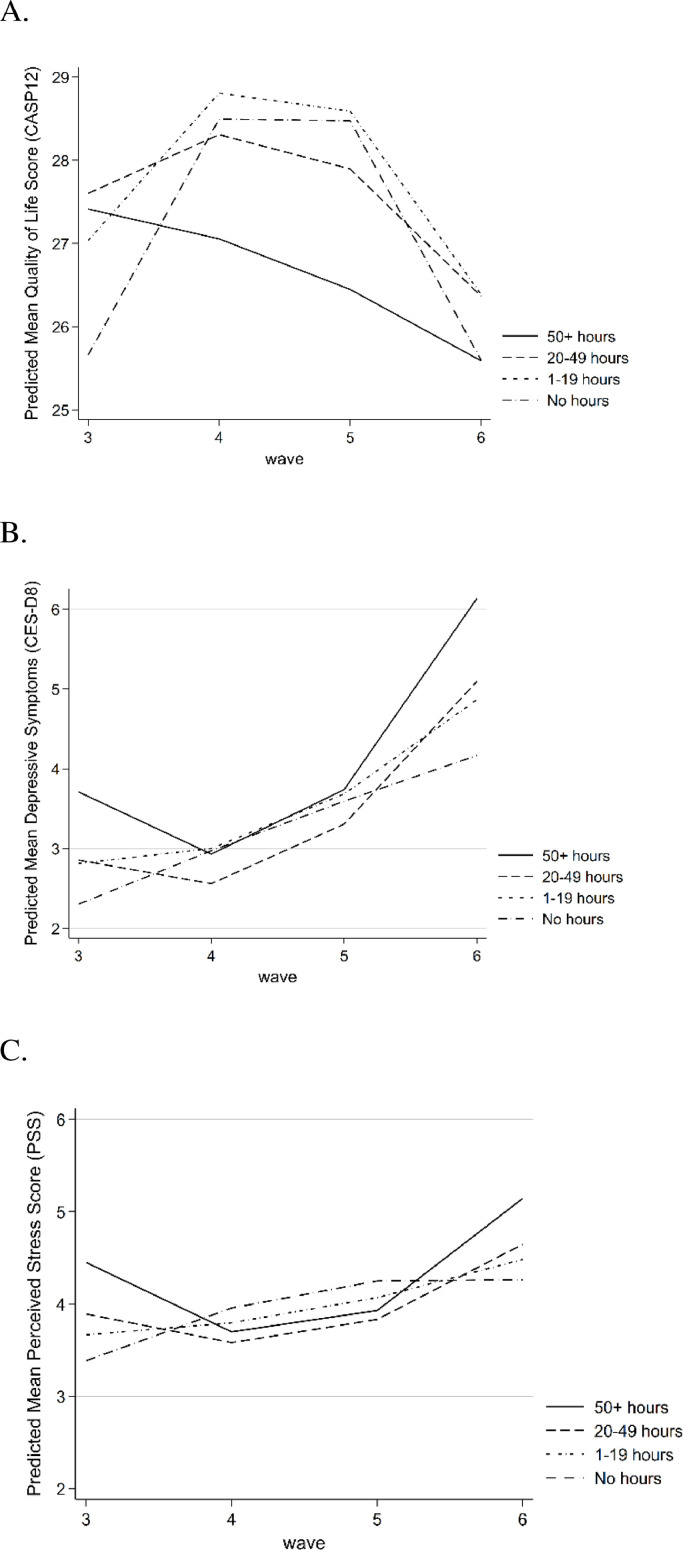
Fig. 2 shows trajectories in well-being and mental health by caring hours between Wave 3 and COVID-Wave 6. Carers providing ≥50 caring hours per week had worse mental health and well-being overall, and this trajectory increased in COVID-Wave 6.
Fig. 2.
Conditional multilevel growth model trajectories of (A) quality of life (CASP12), (B) depressive symptoms (CES-D8) and (C) perceived stress (PSS4) by caring hours, Wave 3-COVID-Wave 6, the Irish Longitudinal Study on Ageing (TILDA).
Table 3 shows results for linear mixed effects models of the relationship of caring status and caring hours, and CASP-12, CES-D8 and PSS4. Model 1 includes caring status, caring hours, and time (wave, wave2). The model showed that, compared to not caring, being a previous carer who did not care during the COVID-19 pandemic was associated with increased CASP-12 scores which were 0.70 points higher on average, and carers who cared ≥50 hours/week had average scores 0.71 points lower. Model 2 was adjusted for covariates including change in state-provided home care and home help received and showed that previous carers who did not care during COVID-19 pandemic maintained significantly higher CASP-12 scores and those caring ≥50 hours/week maintained significantly lower CASP-12 scores. Wave interactions were not significant indicating that these differences did not change over time.
Table 3.
Maximum likelihood estimates from linear mixed effects models predicting quality of life, depressive symptoms and perceived stress by caring status and hours of caring: fixed and random effects models.
| Quality of life (CASP12) | Depressive symptoms (CES-D8) | Perceived stress (PSS) | |||||
|---|---|---|---|---|---|---|---|
| Model 1 | Model 2 | Model 1 | Model 2 | Model 3 | Model 1 | Model 2 | |
| Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | Coef. (95% CI) | |
| Wave | 2.58 (2.13,3.03) *** | 2.20 (1.73,2.67) *** | -3.83 (-4.23-3.44) *** | -3.67 (-4.07,-3.27) *** | -3.67 (-4.07,-3.27) *** | -1.55 (-1.87,-0.23) *** | -1.35 (-1.67,-1.00) *** |
| Wave2 | -0.30 (-0.35,-0.25) *** | -0.27 (-0.32,-0.22) *** | 0.50 (0.46,0.54) *** | 0.48 (0.44,0.53) *** | 0.48 (0.44, 0.53) *** | 0.20 (0.16, 0.23) *** | 0.18 (0.14,0.22) *** |
| Change in Caring Status | |||||||
| Stopped caring prior to COVID | 0.70 (0.23,1.17)** | 0.50 (0.03,0.97)* | -0.03 (-0.51,0.44) | -0.24 (-0.53,0.06) | -0.24 (-0.54,0.06) | 0.12 (-0.36,0.12) | 0.13 (-0.36,0.11 |
| Continued to care | -0.43 (-1.15,0.27) | -0.54 (-1.27,0.18) | 0.19 (-0.46,0.83) | 0.33 (-0.12,0.79) | 0.34 (-0.11,0.80) | 0.34 (-0.02,0.71) | 0.29 (-0.09,0.66) |
| New carer | -0.45 (-0.94,0.05) | -0.46 (-0.97,0.04) | 0.24 (-0.04,0.52) | 0.18 (-0.13,0.49) |
0.19 (-0.12,0.50) | 0.52 (0.27,0.77) *** | 0.47 (0.22,0.73) *** |
| Hours of caring last month | |||||||
| 1-19 hours | 0.17 (-0.19,0.53) | 0.08 (-0.28,0.447) | 0.07 (-0.24,0.37) | 0.11 (-0.20,0.42) | -0.12 (-0.61,0.37) | -0.14 (-0.39,0.11) | -0.12 (-0.37,0.13) |
| 20-49 hours | -0.03 (-0.47,0.54) | -0.16 (-0.67,0.36) | 0.18 (-0.26,0.61) | 0.23 (-0.21,0.67) | 0.60 (-0.21,1.41) | -0.07 (-0.41,0.28) | -0.04 (-0.39,0.31) |
| 50+ hours | -0.71 (-1.19,-0.24)** | -0.65 (-1.14,-0.17)** | 0.77 (0.37,1.18)*** | 0.90 (0.48,1.32) *** | 0.07 (-0.63,0.76) | 0.36 (0.04,0.68)* | 0.39 (0.06,0.72)* |
| Interaction with sex | |||||||
| women | 0.72 (0.52, 0.91) *** | ||||||
| 1-19#women | 0.37 (-0.25,0.99) | ||||||
| 20-49#women | -0.51 (-1.47,0.45) | ||||||
| 50+#women | 1.28 (0.42,2.14) ** | ||||||
| Constant | 22.55 (21.56,23.53) *** | -11.74 (-18.68,-4.80) *** | 9.96 (9.11,10.81) *** | 19.20 (1409,24.31) *** | 20.00 (14.90, 25.10) *** | 6.69 (5.99,7.39) *** | 24.33. (20.19,28.47) *** |
| Random effects | |||||||
| Var (wave) | 0.68 (0.56,0.82) | 0.59 (0.48,0.73) | 0.47 (0.38,0.58) | 0.48 (0.39, 0.58) | 0.48 (0.39, 0.58) | 0.16 (0.11,0.23) | 0.13 (0.09,0.21) |
| Var (constant) | 33.65 (30.28,37.39) | 30.00 (26.73,33.68) | 12.83 (10.83,15.21) | 12.56 (10.57,14.93) | 12.58 (10.59,14.95) | 9.24 (7.86,10.86) | 8.32 (6.90,9.90) |
| Covar (wave, constant) | -3.18 (-3.80,-2.55) | -2.72 (-3.33,-2.11) | -1.74 (-2.18,-1.30) | -1.79 (-2.23,-1.35) | -1.80 (-2.24,-1.36) | -0.92 (-1.21,-0.64) | -0.79 (-1.07,-0.50) |
| Residual variance | 7.14 (6.87,7.41) | 7.02 (6.75,7.30) | 6.26 (6.05,6.49) | 6.06 (5.85,6.28) | 6.06 (5.84,6.28) | 4.08 (3.93,4.23) | 4.02 (3.87,4.18) |
Model 1: adjusted wave, wave2, random intercept, random slope. Model 2: adjusted model 1 + age, age2, sex, education, area of residence, marital status, State-provided formal care: home help and home carers. Model 3: adjusted model 2 + care hours*sex. *p<0.05, **p<0.01, ***p<0.001.
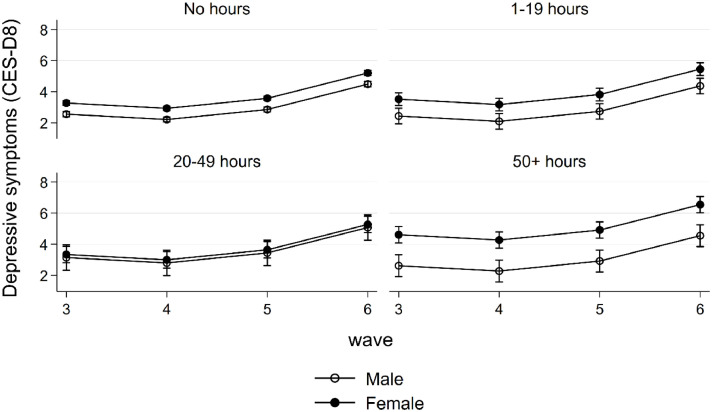
Caring status was not associated with higher CES-D8 scores on average, however carers who cared ≥50 hours/week had CES-D8 scores 0.77 points higher on average in Model 1. These higher scores were maintained in Model 2 when all covariates were included. Wave interactions were not significant. There was an interaction between caring and sex and the increase in depressive symptoms was only in women who cared ≥50 hours/week with CES-D8 scores 1.28 points higher on average (Fig. 3 ).
Fig. 3.
Marginal means of numbers of care hours and the trajectory of depressive symptoms (CES-D8) for men and women, Wave 3-COVID-Wave 6, the Irish Longitudinal Study on Ageing (TILDA).
Overall, perceived stress was relatively low, with an average score of 4.5 for men and 4.9 for women. Becoming a new carer during the COVID-19 pandemic was associated with increased perceived stress and model 1 showed that, compared to not caring, becoming a new carer was associated with PSS4 scores which were 0.52 points higher on average, and those who cared ≥50 hours/week had average scores 0.36 points higher. These significantly higher PSS4 scores remained, in Model 2 when adjusted for covariates. Again, there were no significant time interactions.
4. Discussion
Our study contributes to the caregiving literature by providing compelling evidence of an association between caring, caregiving intensity and adverse mental health and wellbeing among carers aged ≥60 years using nationally representative longitudinal data. Firstly, we hypothesized that caring in the older population would increase due to restrictions on both family visits and state-provided home care. We found that the proportion of adults aged ≥60 providing care doubled during the COVID-19 pandemic. The proportion of carers providing high intensity caring also increased; one third reported caring ≥50 hours/week in 2020. Most were caring for a spouse,- this proportion trebled from 2014. Care for non-household members decreased substantially during the COVID-19 pandemic. Reported state-provided care services receipt halved during the pandemic for those who previously received it which may explain the high proportion of new carers during the pandemic, and the increase in care hours, particularly in those caring for their spouse.
Care hour increases during the pandemic are reported in other studies (Budnick et al., 2021; Cohen et al., 2021a), with higher care hours in rural areas (Cohen et al., 2021b) and a study of caring outside of the home also found an increased frequency of providing care to parents during the pandemic across most European countries, while care to children decreased (Bergmann & Wagner, 2021). In contrast a study in Germany found that the overall prevalence of informal caregivers remained unchanged during the second wave of the pandemic, compared to before the epidemic, however prevalence of informal caring was high at 14% (Zwar et al., 2021). It was hypothesized that informal caregivers have already been responsible for the majority of care recipients in Germany before the pandemic, however the study did find similar to our findings, that long-term carers reported both more care hours and higher caring intensity during the pandemic (Zwar et al., 2021).
Secondly, we hypothesized that COVID-19 and its accompanying restriction measures with reduced social interactions with others led to a worsening of mental health for informal caregivers. During the COVID-19 pandemic we found that quality of life decreased, and depressive symptoms and perceived stress increased in adults aged ≥60 in Ireland. Finally, our third hypothesis that carers who had increased the hours of caregiving provided would have worse trajectories in well-being and mental health than caregivers who have not increased caring hours was also confirmed. Mixed effects models showed that higher care hours during the pandemic were associated with lower quality of life scores, higher depressive symptoms, and perceived stress than in non-carers and this remained following adjustment for covariates. There were no interactions between caring measures and wave suggesting any negative associations between caring and well-being measures were already established at Wave 3 of TILDA and were sustained through the pandemic. Becoming a new carer during the pandemic was also associated with increased perceived stress.
This concurs with other research which found that carers experienced increased psychosocial burdens during the pandemic with more concerns and loss of support (Budnick et al., 2021) including carers of people with dementia (Canevelli et al., 2020). Repeated cross-sectional studies in Japan between March-October 2020 found that the prevalence of depressive symptoms increased among caregivers during the pandemic regardless of the caregiving role and severity of care recipients’ needs (Noguchi et al., 2021). Furthermore our finding of increased depression only in women carers concurs with a study in Japan which also found deterioration in mental health during the pandemic in women only (Taniguchi et al., 2022). This increased depression in women may indicate the greater vulnerability of women to the reduction in other social interactions during the pandemic. Social meetings with friends and family are known to be protective for both sexes, however there is some suggestion that caring for grandchildren and participation in social interactions outside the home are more beneficial for women (Carayanni et al., 2012). Alternatively, research has found that women have a greater tendency to ruminate when distressed (focusing on one's symptoms of distress) than men, which can lead to increased depression (Nolen-Hoeksema et al., 1999). These gender differences were not seen for perceived stress or quality of life. Other measures of poor mental health have been found including increased loneliness (Taniguchi et al., 2022), carer burden (Cohen et al., 2021a) and self-reported deterioration in mental health including increased suicidal ideation (Taniguchi et al., 2022). Caregiving burden increased with increasing caregiving intensity (Cohen et al., 2021a).
The challenges of caring are well established, and research suggests that adverse effects on health and well-being can be successfully offset with appropriate additional social interaction, supportive family and social circles, including religious and volunteering groups (McGarrigle et al., 2018; Orr et al., 2022, 2019; Ward et al., 2019). All these social supports were effectively removed from the older population during the COVID-19 pandemic through remain-at-home advice and this study also shows a parallel increase in poorer well-being for non-carers. However, this study demonstrates that this effect was accentuated for the already higher stressed and depressed population of carers. Many former and new family carers assumed additional responsibilities within a short period of time, with limited access to other sources of support and this will have contributed to the increased stress and lower well-being seen in this and other studies (Irani et al., 2021). There is some evidence that other sources of formal and informal support filled the caring void vacated by the State. For example, one study in Germany found that while caring intensity increased, help from friends with shopping and the use of privately employed carers and other ambulatory support services increased during the pandemic (Zwar et al., 2021). Furthermore, as the older population already had a high prevalence of informal caring provision, this may indicate possible solutions that the carers implemented to protect their care recipients while still obtaining support (Zwar et al., 2021). Given the demonstrated importance of combining informal care with state-provided care and social support, future public health policies should ensure the maintenance and provision of increased additional supports from outside the household to support family carers.
There are some limitations to our study. We surveyed the population over a relatively short period early during the pandemic, when there were no vaccines, comparatively low cases and deaths and strict restrictions. Therefore, this study reflects the initial pandemic response of both policy and personal behaviors. Future data collection waves will examine if caring, and mental health and well-being have returned to pre-COVID-19 levels or if the legacy is longer lasting. We asked about formal care services receipt however these only account for carers caring within their own household and if the household member is also in the study. This represented at least 63% of spouse carers, but state-provided services received for non-household care recipients may be under-counted.
Public health interventions should consider the potential negative effects of remain-at-home orders for the older population in future COVID-19 waves. Both care receipt and care provision are crucial for maintaining health and preventing care home admissions. More alternative population protection strategies should be considered that allow the older population to maintain social contacts and state-provided care. A European-wide study found that unmet need was significantly more likely to be reported by care recipients during the first COVID-19 wave in countries with longer stay-at home orders (Bergmann & Wagner, 2021). The pandemic also affected intergenerational caring which constitutes an important contribution by the older population in Ireland and has been a valued social support structure for adult children, grandparents, and grandchildren (McGarrigle et al., 2014, 2018). This contribution included grandparents facilitating working parents by helping with childcare (McGarrigle et al., 2018), and adult children supporting ageing parents with essential tasks like household help and bathing, washing and dressing (McGarrigle et al., 2014).
While the COVID-19 pandemic stay-at-home orders and media coverage rhetoric has doubtlessly led to an exacerbation of ageism, which itself may be associated with declining physical and cognitive health (McGarrigle, Ward, & Kenny, 2022), physical deconditioning (Lebrasseur et al., 2021) and an increase or worsening of adverse mental health outcomes in older populations has also occurred. Older adults reported a greater loneliness due to pandemic-related social isolation (Lebrasseur et al., 2021). However, these impacts may have been worse for informal carers with already poorer mental health and wellbeing. Carers had increased worries about the person they cared for, in addition to worries about their own health, which often led to reducing other formal care services received and increasing their own carer hours while simultaneously losing social support.
5. Conclusions
This study demonstrated that while the availability of both state-provided and informal care for older people was reduced during the COVID-19 pandemic, there was a concomitant increase in caring by older household members. This was associated with lower well-being and mental health in an already struggling group. This study provides further evidence of the detrimental indirect effects of the COVID-19 pandemic on older people and emphasizes for policymakers the importance of prioritizing state-provided and informal care arrangements for the older population and ensuring that support services remain available to support family carers even during public health crises.
Funding
Financial support for TILDA was provided by the Government of Ireland, The Atlantic Philanthropies and Irish Life Plc. Financial support for the TILDA COVID-19 study was provided by the Health Research Board under the COVID-19 Pandemic Rapid Response Funding Call (Grant no. COV19-2020-070).
CRediT authorship contribution statement
C.A. McGarrigle: Conceptualization, Methodology, Formal analysis, Writing – original draft, Funding acquisition. M. Ward: Writing – review & editing, Funding acquisition. C. De Looze: Writing – review & editing, Funding acquisition. A. O'Halloran: Writing – review & editing, Funding acquisition. R.A. Kenny: Writing – review & editing, Funding acquisition, Supervision.
Declaration of Competing Interest
The authors have no conflict of interest.
Footnotes
Supplementary material associated with this article can be found, in the online version, at doi:10.1016/j.archger.2022.104719.
Appendix. Supplementary materials
References
- Beach S.R., Schulz R., Yee J.L., Jackson S. Negative and positive health effects of caring for a disabled spouse: Longitudinal findings from the caregiver health effects study. Psychology and Aging. 2000;15:259–271. doi: 10.1037//0882-7974.15.2.259. [DOI] [PubMed] [Google Scholar]
- Bergmann M., Wagner M. The impact of COVID-19 on informal caregiving and care receiving across Europe during the first phase of the pandemic. Frontiers in Public Health. 2021;9:673874. doi: 10.3389/fpubh.2021.673874. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berkman L.F., Glass T., Brissette I., Seeman T.E. From social integration to health: Durkheim in the new millennium. Social Science & Medicine. 2000;51:843–855. doi: 10.1016/s0277-9536(00)00065-4. 1982. [DOI] [PubMed] [Google Scholar]
- Bookwala J., Schulz R. A comparison of primary stressors, secondary stressors, and depressive symptoms between elderly caregiving husbands and wives: The Caregiver Health Effects Study. Psychology and Aging. 2000;15:607–616. doi: 10.1037//0882-7974.15.4.607. [DOI] [PubMed] [Google Scholar]
- Boutoleau-Bretonnière C., Pouclet-Courtemanche H., Gillet A., Bernard A., Deruet A.L., Gouraud I., Mazoue A., Lamy E., Rocher L., Kapogiannis D., El Haj M. The effects of confinement on neuropsychiatric symptoms in Alzheimer's disease during the COVID-19 crisis. Journal of Alzheimer's Disease. 2020;76:41–47. doi: 10.3233/JAD-200604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Budnick A., Hering C., Eggert S., Teubner C., Suhr R., Kuhlmey A., Gellert P. Informal caregivers during the COVID-19 pandemic perceive additional burden: Findings from an ad-hoc survey in Germany. BMC Health Services Research. 2021;21(1):353. doi: 10.1186/s12913-021-06359-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canevelli M., Valletta M., Toccaceli Blasi M., Remoli G., Sarti G., Nuti F., Sciancalepore F., Ruberti E., Cesari M., Bruno G. Facing dementia during the COVID-19 outbreak. Journal of the American Geriatrics Society. 2020;68:1673–1676. doi: 10.1111/jgs.16644. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carayanni V., Stylianopoulou C., Koulierakis G., Babatsikou F., Koutis C. Sex differences in depression among older adults: Are older women more vulnerable than men in social risk factors? The case of open care centers for older people in Greece. European Journal of Ageing. 2012;9:177–186. doi: 10.1007/s10433-012-0216-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carr D. COVID-19: Trends, disparities, and consequences for older adults. The Journals of Gerontology: Series B. 2020;76:e65–e67. doi: 10.1093/geronb/gbaa211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Central Statistics Office . Central Statistics Office; 2014. Measuring Ireland’s progress 2012.https://www.cso.ie/en/releasesandpublications/ep/p-mip/measuringirelandsprogress2012/ [Google Scholar]
- Central Statistics Office . Central Statistics Office; 2017. Census of population 2016 – Profile 9 health, disability and carers.https://www.cso.ie/en/releasesandpublications/ep/p-cp9hdc/p8hdc/p9cd/ [Google Scholar]
- Cohen S., Kamarck T., Mermelstein R. A global measure of perceived stress. Journal of Health and Social Behavior. 1983;24:385–396. [PubMed] [Google Scholar]
- Cohen S.A., Kunicki Z.J., Drohan M.M., Greaney M.L. Exploring changes in caregiver burden and caregiving intensity due to COVID-19. Gerontology and Geriatric Medicine. 2021;7 doi: 10.1177/2333721421999279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen S.A., Kunicki Z.J., Nash C.C., Drohan M.M., Greaney M.L. Rural-urban differences in caregiver burden due to the COVID-19 pandemic among a national sample of informal caregivers. Gerontology and Geriatric Medicine. 2021;7 doi: 10.1177/23337214211025124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Department of the Taoiseach, 2020. Speech of the Taoiseach Leo Varadkar TD, Government buildings, 27 March 2020. www.gov.ie, Dublin.
- Donoghue O.A., McGarrigle C.A., Foley M., Fagan A., Meaney J., Kenny R.A. Cohort profile update: The Irish longitudinal study on ageing (TILDA) International Journal of Epidemiology. 2018;47:1398. doi: 10.1093/ije/dyy163. -1398l. [DOI] [PubMed] [Google Scholar]
- English A.N., Bellingtier J.A., Neupert S.D. It's "the Joneses": The influence of objective and subjective socioeconomic status on subjective perceptions of aging. European Journal of Ageing. 2019;16:121–128. doi: 10.1007/s10433-018-0475-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman V.A., Cornman J.C., Carr D. Is spousal caregiving associated with enhanced well-being? New evidence from the panel study of income dynamics. Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2014;69:861–869. doi: 10.1093/geronb/gbu004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- StataCorp . StataCorp LP; TX: 2015. Stata statistical software: Release 14. College Station. [Google Scholar]
- Greaney M.L., Kunicki Z.J., Drohan M.M., Ward-Ritacco C.L., Riebe D., Cohen S.A. Self-reported changes in physical activity, sedentary behavior, and screen time among informal caregivers during the COVID-19 pandemic. BMC Public Health [Electronic Resource] 2021;21:1292. doi: 10.1186/s12889-021-11294-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Haley W.E., Roth D.L., Sheehan O.C., Rhodes J.D., Huang J., Blinka M.D., Howard V.J. Effects of transitions to family caregiving on well-being: A longitudinal population-based study. Journal of the American Geriatrics Society. 2020;68:2839–2846. doi: 10.1111/jgs.16778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Service Executive . A strategic framework for delivery. Health Service Executive (HSE); 2020. Service continuity in a COVID environment.http://hdl.handle.net/10147/627846 [Google Scholar]
- Ho J.S., Bordon J., Wang V., Ceglowski J., Kim D.H., Chattillion E.A., Patterson T.L., Grant I., Ziegler M.G., Mills P.J., Mausbach B.T. Reduced activity restriction buffers the relations between chronic stress and sympathetic nervous system activation. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2014;69:408–416. doi: 10.1093/geronb/gbt028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iob E., Frank P., Steptoe A., Fancourt D. Levels of severity of depressive symptoms among at-risk groups in the UK during the COVID-19 pandemic. JAMA Network Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.26064. -e2026064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Irani E., Niyomyart A., Hickman R.L. Family caregivers’ experiences and changes in caregiving tasks during the COVID-19 pandemic. Clinical Nursing Research. 2021;30:1088–1097. doi: 10.1177/10547738211014211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kivi M., Hansson I., Bjälkebring P. Up and about: Older adults’ well-being during the COVID-19 pandemic in a Swedish longitudinal study. The Journals of Gerontology: Series B. 2020;76:e4–e9. doi: 10.1093/geronb/gbaa084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Knepple Carney A., Graf A.S., Hudson G., Wilson E. Age moderates perceived COVID-19 disruption on well-being. The Gerontologist. 2020;61:30–35. doi: 10.1093/geront/gnaa106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lebrasseur A., Fortin-Bédard N., Lettre J., Raymond E., Bussières E.-L., Lapierre N., Faieta J., Vincent C., Duchesne L., Ouellet M.-C., Gagnon E., Tourigny A., Lamontagne M.-È., Routhier F. Impact of the COVID-19 pandemic on older adults: Rapid review. JMIR Aging. 2021;4:e26474. doi: 10.2196/26474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks N.F., Lambert J.D., Choi H. Transitions to caregiving, gender, and psychological well-being: A prospective U.S. national study. Journal of Marriage and Family. 2002;64:657–667. [Google Scholar]
- Marmot M. Society and the slow burn of inequality. Lancet. 2020;395:1413–1414. doi: 10.1016/S0140-6736(20)30940-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach B.T., Chattillion E.A., Moore R.C., Roepke S.K., Depp C.A., Roesch S. Activity restriction and depression in medical patients and their caregivers: A meta-analysis. Clinical Psychology Review. 2011;31:900–908. doi: 10.1016/j.cpr.2011.04.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mausbach B.T., Roepke S.K., Chattillion E.A., Harmell A.L., Moore R., Romero-Moreno R., Bowie C.R., Grant I. Multiple mediators of the relations between caregiving stress and depressive symptoms. Aging & Mental Health. 2012;16:27–38. doi: 10.1080/13607863.2011.615738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarrigle, C., Kenny, R.A., 2020. Receipt of care and caring in community-dwelling adults aged 50 and over in Ireland. The Irish Longitudinal Study on Ageing (TILDA), Dublin.
- McGarrigle C.A., Cronin H., Kenny R.A. The impact of being the intermediate caring generation and intergenerational transfers on self-reported health of women in Ireland. International Journal of Public Health. 2014;59:301–308. doi: 10.1007/s00038-013-0521-y. [DOI] [PubMed] [Google Scholar]
- McGarrigle C.A., Timonen V., Layte R. Choice and constraint in the negotiation of the grandparent role: A mixed-methods study. Gerontology and Geriatric Medicine. 2018;4 doi: 10.1177/2333721417750944. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McGarrigle C.A., Ward M., Kenny R.A. Negative aging perceptions and cognitive and functional decline: Are you as old as you feel? Journal of the American Geriatrics Society. 2022;70(3):777–788. doi: 10.1111/jgs.17561. [DOI] [PubMed] [Google Scholar]
- Morina N., Kip A., Hoppen T.H., Priebe S., Meyer T. Potential impact of physical distancing on physical and mental health: A rapid narrative umbrella review of meta-analyses on the link between social connection and health. BMJ Open. 2021;11 doi: 10.1136/bmjopen-2020-042335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noguchi T., Hayashi T., Kubo Y., Tomiyama N., Ochi A., Hayashi H. Association between family caregivers and depressive symptoms among community-dwelling older adults in Japan: A cross-sectional study during the COVID-19 pandemic. Archives of Gerontology and Geriatrics. 2021;96 doi: 10.1016/j.archger.2021.104468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nolen-Hoeksema S., Larson J., Grayson C. Explaining the gender difference in depressive symptoms. Journal of Personality and Social Psychology. 1999;77:1061–1072. doi: 10.1037//0022-3514.77.5.1061. [DOI] [PubMed] [Google Scholar]
- O’Halloran A., Hartley P., Moloney D., McGarrigle C., Kenny R., Romero-Ortuno R. Informing patterns of health and social care utilisation in Irish older people according to the Clinical Frailty Scale [version 1; peer review: 2 approved] HRB Open Research. 2021;4:54. doi: 10.12688/hrbopenres.13301.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- O'Reilly D., Connolly S., Rosato M., Patterson C. Is caring associated with an increased risk of mortality? A longitudinal study. Social Science & Medicine. 2008;67:1282–1290. doi: 10.1016/j.socscimed.2008.06.025. 1982. [DOI] [PubMed] [Google Scholar]
- O'Reilly D., Rosato M., Ferry F., Moriarty J., Leavy G. Caregiving, volunteering or both? Comparing effects on health and mortality using census-based records from almost 250,000 people aged 65 and over. Age and Ageing. 2017;46:821–826. doi: 10.1093/ageing/afx017. [DOI] [PubMed] [Google Scholar]
- Orr J., Kenny R.A., McGarrigle C.A. Religiosity and quality of life in older christian women in Ireland: A mixed methods analysis. Journal of Religion and Health. 2022 doi: 10.1007/s10943-022-01519-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orr J., Tobin K., Carey D., Kenny R.A., McGarrigle C. Religious attendance, religious importance, and the pathways to depressive symptoms in men and women aged 50 and over living in Ireland. Research on Aging. 2019;41:891–911. doi: 10.1177/0164027519860270. [DOI] [PubMed] [Google Scholar]
- Perkins M., Howard V.J., Wadley V.G., Crowe M., Safford M.M., Haley W.E., Howard G., Roth D.L. Caregiving strain and all-cause mortality: Evidence from the REGARDS study. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2013;68:504–512. doi: 10.1093/geronb/gbs084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff L.S. The CES-D scale: A self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Sexton E., King-Kallimanis B.L., Conroy R.M., Hickey A. Psychometric evaluation of the CASP-19 quality of life scale in an older Irish cohort. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2013;22:2549–2559. doi: 10.1007/s11136-013-0388-7. [DOI] [PubMed] [Google Scholar]
- Spillman B.C., Freedman V.A., Kasper J.D., Wolff J.L. Change over time in caregiving networks for older adults with and without dementia. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2020;75:1563–1572. doi: 10.1093/geronb/gbz065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Taniguchi Y., Miyawaki A., Tsugawa Y., Murayama H., Tamiya N., Tabuchi T. Family caregiving and changes in mental health status in Japan during the COVID-19 pandemic. Archives of Gerontology and Geriatrics. 2022;98:104531. doi: 10.1016/j.archger.2021.104531. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The Alzheimer Society of Ireland . 2020. COVID-19: Impact & need for people living with dementia and family carers Dublin, Ireland. [Google Scholar]
- The Alzheimer Society of Ireland . 2020. Caring and coping with dementia during COVID-19. Dublin, Ireland. [Google Scholar]
- Ward M., Clarke N., Wang M., McGarrigle C.A., De Looze C., O’Halloran A.M., Kenny R.A. Study protocol for TILDA COVID-19 survey. Altered lives in a time of crisis: preparing for recovery from the impact of the COVID-19 pandemic on the lives of older adults [version 1; peer review: 1 Approved] HRB Open Research. 2021;4:51. doi: 10.12688/hrbopenres.13248.1. [DOI] [Google Scholar]
- Ward M., McGarrigle C.A., Kenny R.A. More than health: Quality of life trajectories among older adults-findings from the Irish longitudinal study of ageing (TILDA) Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2019;28:429–439. doi: 10.1007/s11136-018-1997-y. [DOI] [PubMed] [Google Scholar]
- Williamson G.M., Shaffer D.R. In: Physical illness and depression in older adults: A handbook of theory, research, and practice. Williamson G.M., Shaffer D.R., Parmelee P.A., editors. Kluwer Academic/Plenum; New York: 2000. The activity restriction model of depressed affect: Antecedents and consequences of restricted normal activities; pp. 173–200. [Google Scholar]
- World Health Organization . 2020. Health inequity and the effects of COVID-19. Assessing, responding to and mitigating the socioeconomic impact on health to build a better future. Copenhagen. [Google Scholar]
- World Health Organization, 2020b. WHO coronovirus (COVID-19) Dashboard. World Health Organization, Geneva. https://covid19.who.int/.
- Zwar L., König H.-H., Hajek A. Informal caregiving during the COVID-19 pandemic: Findings from a representative, population-based study during the second wave of the pandemic in Germany. Aging & Mental Health. 2021:1–9. doi: 10.1080/13607863.2021.1989377. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.