Abstract
Background
Physicians’ gaze towards their patients may affect patients’ trust in them. This is especially relevant considering recent developments, including the increasing use of Electronic Health Records, which affect physicians’ gaze behavior. Moreover, socially anxious patients’ trust in particular may be affected by the gaze of the physician.
Objective
We aimed to evaluate if physicians’ gaze towards the face of their patient influenced patient trust and to assess if this relation was stronger for socially anxious patients. We furthermore explored the relation between physicians’ gaze and patients’ perception of physician empathy and patients’ distress.
Design
This was an observational study using eye-tracking glasses and questionnaires.
Participants
One hundred patients and 16 residents, who had not met before, participated at an internal medicine out-patient clinic.
Measures
Physicians wore eye-tracking glasses during medical consultations to assess their gaze towards patients’ faces. Questionnaires were used to assess patient outcomes. Multilevel analyses were conducted to assess the relation between physicians’ relative face gaze time and trust, while correcting for patient background characteristics, and including social anxiety as a moderator. Analyses were then repeated with perceived empathy and distress as outcomes.
Results
More face gaze towards patients was associated with lower trust, after correction for gender, age, education level, presence of caregivers, and social anxiety (β=−0.17, P=0.048). There was no moderation effect of social anxiety nor a relation between face gaze and perceived empathy or distress.
Conclusions
These results challenge the notion that more physician gaze is by definition beneficial for the physician-patient relationship. For example, the extent of conversation about emotional issues might explain our findings, where more emotional talk could be associated with more intense gazing and feelings of discomfort in the patient. To better understand the relation between physician gaze and patient outcomes, future studies should assess bidirectional face gaze during consultations.
KEY WORDS: face gaze, patient trust, physician empathy, eye-tracking, social anxiety
INTRODUCTION
Gaze is a crucial aspect of communication.1, 2 Gaze towards the eyes or face has previously been used as a proxy for “eye contact”.2 It transmits social and attentional information and can direct a conversation.1, 3, 4 Physicians’ gaze is therefore an essential aspect of physician-patient communication. Gaze between physician and patient affects the patient during the consultation.5–7 For instance, during medical consultations, patients follow the physicians’ gaze towards the computer screen.7 Physician gaze has also been related to outcomes after the consultation such as patients’ medication adherence and their physical and cognitive functioning.5, 6, 8, 9
Sub-optimal levels of gaze between physicians and patients may have negative effects on physician-patient relationships,10–12 including reduced trust of patients in their physicians. This is especially relevant considering present-day characteristics of the consultation, such as the increasing use of Electronic Health Records, which may reduce the physicians’ amount of gaze towards the patient.13–16 If increased use of Electronic Health Records leads to reduced gaze towards the patients, this may eventually harm patients’ trust in their physician, whereas trust is crucial for the quality of the patient-physician relationship.17 Ultimately, reduced trust is suggested to lead to harmful long-term effects, such as less medication adherence and lower patient well-being.17–20
The amount of physician gaze towards their patients may not only affect trust, but also patients’ perception of physician empathy21 and their emotional wellbeing, particularly distress.22 Therefore, it is worthwhile to investigate the gaze of the physician and its implications for patients.
Physicians’ gaze may affect patients differently since individual differences, especially social anxiety, influence the perception of gaze towards the eyes.23–25 Individuals who suffer from social anxiety tend to feel unease in social interactions and may therefore experience gaze as unpleasant.26 Social anxiety ranks the third most common mental disorder (after depression and substance abuse) and is associated with greater health care utilization and lower health-related quality of life.27, 28 Due to gaze aversion, these patients may need a different communication approach than others. Whereas higher levels of physician gaze are commonly considered beneficial to the physician-patient relation,11 more gaze could induce distress and negatively affect trust among socially anxious patients. Despite its apparent relevance, we do not yet know whether the negative experience of physician gaze for socially anxious patients can be extrapolated to the medical setting.
We aimed to evaluate whether the level of physician gaze towards their patient predicts patients’ trust. We additionally aimed to explore the relation between physician face gaze and patients’ perception of physician empathy, and their distress. Furthermore, we assessed whether social anxiety moderates the association between physicians’ gaze and patients’ trust, perceived level of empathy, and distress. The results of our study can be used to support physicians in optimizing their nonverbal communication behaviors.
METHODS
Design and Procedure
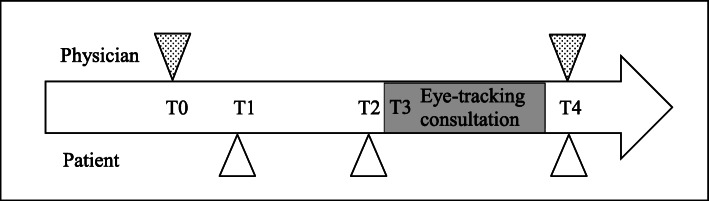
This was an observational study using eye-tracking to assess gaze patterns of physicians and validated questionnaires to assess patient outcomes. The study was conducted at the outpatient clinic of an internal medicine department of a Dutch hospital. It was judged to be exempt from approval by the ethical committee (protocol number W17_107). The study encompassed measurements at 5 time points (T0-T4) (see Fig. 1). At T0, physicians were recruited using snowballing sampling. To limit physicians’ awareness of the purpose of the study, physicians were informed that their use of the Electronic Health Record was the subject of research.
Figure 1.
Graphic representation of the study measurement points. Note: The triangles symbolize the administration of questionnaires. T0 was at an unstructured time point convenient to the physician. T1 occurred around two weeks before the consultation. T2 occurred around 10 minutes before the consultation. T4 was as soon as the patient left the consultation room.
Physicians signed informed consent and completed a baseline questionnaire. Two weeks before visiting for their follow-up consultation, patients—who did not meet the physician before—were telephonically invited to participate. Upon agreement, patients signed informed consent and completed a baseline questionnaire (T1). Just prior to the consultation, patients indicated their current level of distress in a questionnaire (T2). The consultation was video-recorded with a camera positioned in a corner of the consultation room, and the gaze of the physician was tracked using mobile eye-tracking glasses (T3). Immediately after the consultation, physicians and patients responded to questionnaires assessing study outcomes (T4). Patients received a 15 euro gift card for participation. Data were collected between February 2018 and May 2019.
Participants
Participating physicians were residents of internal medicine. Participating patients visited the outpatient clinic for a scheduled follow-up consultation. Patients were eligible who had had no previous consultations with the physician, spoke Dutch fluently, were older than 18 years, and had no mental disabilities or other serious cognitive impairments that could hinder their study participation.
Instruments
Eye-Tracking Glasses
The gaze of the physician towards the patient’s face was tracked using Tobii Pro Glasses 229 (T3). The eye-tracking glasses are equipped with two cameras per eye (measuring pupil movement) and a camera that records the environment. The included accelerometer and gyroscope sensors enable the software to differentiate between head and eye movements, limiting the influence of head movements on eye-tracking data. Calibration was performed for each physician to ensure measurement accuracy, using specific software.29–31 The face of the patient comprised the so-called area-of-interest, which is used to assess the dwell time (the duration of gaze in a specific “area-of-interest”).32
Questionnaires
Questionnaires were provided on paper or electronically (using Qualtrics.com), depending on the participant’s preference.33 Sociodemographic characteristics assessed were age, gender, and nationality of both physicians and patients (T0 and T1).
Patients’ trust in their physician was assessed using the Wake Forest Physician Trust Scale (WFPTS) consisting of 10 items (1= “totally disagree”–5=“totally agree) (T4).34, 35 This scale is used to assess patients’ interpersonal trust in their individual health care provider. Higher scores indicate higher levels of trust. The reliability of the scale in our sample was high (Cronbach’s alpha=.82).
The patient’s perceived level of physician empathy was measured with the Consultation And Relational Empathy (CARE), a 10-item scale (1= “poor”–5=“excellent” and an additional option “does not apply”) (T4).36, 37 This scale measures relational empathy in the clinical context, which is the ability to (1) understand the patient’s situation, perspective, and feelings; (2) communicate that understanding and checking its accuracy; and (3) to act on that understanding in a helpful way. Higher scores indicate higher perceived physician empathy. The reliability of the scale was high (Cronbach’s alpha=.94).
We measured distress before and after the consultation (T2 and T4) using the 6-item state scale Spielberger State-Trait Anxiety Inventory (STAI-6) (1= “not at all”- 4=“very much so”) (T2 and T4).38, 39 This inventory assesses a psychophysiological state following the perception of threat. Reliability was good (Cronbach’s alpha=.77). Change scores in distress were calculated and used in further analyses by subtracting STAI-6 scores before (T2) from STAI-6 scores after the consultation (T4).
Patients’ level of social anxiety was assessed using a commonly used screening tool, the Short Form of Social Interaction Anxiety Scale (SIAS-6) and Social Phobia Scale (SPS-6) (T1). It assesses general social interaction anxiety (e.g., talking to strangers) and fear of being observed (e.g., eating in the presence of others), respectively, and has 12 items (0= “not at all true of me”–5=“extremely true of me”).40, 41 High scores on either of the two scales indicate social anxiety. Reliability was high (Cronbach’s alpha=.84).
Data Preparation
The eye-tracking data was analyzed with software to automatically create areas-of-interest around faces, created for this study based on a previously developed algorithm.32 The software was used to create an area-of-interest around the faces of all individuals present in the videos. The output of the software indicated for each video frame (40ms) whether the gaze of the physician was focused on the face of the patient or the caregiver (if present), i.e., within the area-of-interest (coded as “1”) or not (“0”). This output was used to compute the average dwell time of face gaze, which is measured as the mean duration of each gaze instance towards the face. For more details, see Jongerius et al..32
Statistical Analysis
A required sample size of 96 patients was calculated based on multilevel regression analysis (80% power, α=.05, medium effect size=.25), which yields a sample size of N=53.42, 43 To account for the clustering of consultations within physicians, we estimated a design effect of 1.8 (Deff=1+(m-1)ICC), where m is the number of consultations per physician=5 and ICC=.2.44 In total, this yielded a required N of 53×1.8=95.4. Descriptive analyses were done using SPSS 26.45 Because of the nested data, we conducted a multilevel analysis with face gaze (average dwell time) as an independent variable and patients’ reported trust in physicians as a dependent variable. We applied a multilevel Tobit model because trust showed a left-skewed distribution with a ceiling effect.46 In addition to the crude analyses, we adjusted for gender, age, educational level, caregiver presence, and social anxiety because these variables could influence either the level of face gaze or trust.47, 48 To test if social anxiety moderated the effect of face gaze on trust, we examined the interaction between social anxiety and face gaze. We repeated these multilevel models twice, using the exploratory-dependent variables1 perception of physician empathy and2 distress instead. All multilevel analyses were performed with STATA/SE 14.49 All test outcomes were considered significant with an alpha of p<.0.05.
Results
Descriptives
In total, 16 physicians participated, with a median age of 33.5 years (ranged 29 to 38 years). They had a median of 4.5 years in training (ranged from 2 to 6 years). Physicians consulted with between 2 and 14 patients (median=6). In total, 202 patients were approached for participation, of whom 130 telephonically agreed to participate. Reasons for declining to participate were “not interested” or “will cancel appointment for other reasons” or “did not speak Dutch.” We collected 102 measurements of which 100 eye-tracking registrations were complete. Patients were on average 58.1 years old (SD = 14.0). Physical examination was performed in 24 consultations (24%) and a caregiver was present in 17 consultations (17%). Consultations (disregarding physical examinations) had a median duration of 14.1 min (range=3.0–45.1). Table 1 provides an overview of the sample characteristics. Table 2 provides the outcomes of our measures.
Table 1.
Sociodemographic Characteristics of Patients and Physicians
| n (%) | |
|---|---|
| Patients (N=100) | |
| Female gender | 47 (47%) |
| Self-identified nationality | |
| Dutch | 94 (94%) |
| Other European nationalities | 2 (2%) |
| South American | 3 (3%) |
| Middle East | 1 (1%) |
| Education level (n=99) | |
| None/primary school | 29 (29%) |
| Secondary/lower level vocational school | 50 (50%) |
| College/university | 20 (20%) |
| Physicians (N=16) | |
| Female gender | 8 (50%) |
| Self-identified nationality | |
| Dutch | 15 (94%) |
| Arabic | 1 (6%) |
Table 2.
Outcomes of Independent, Dependent, Moderator and Exploratory Variables
| n | Median | Range | |
|---|---|---|---|
| Independent variable | |||
| Face gaze (average dwell time) in seconds | 100 | 1.0 | 0.1–6.8 |
| Dependent variables | |||
| Trust (Wake Forest Physician Trust Scale, range=1–5) | 100 | 4.6 | 2.1–5 |
| Perceived empathy (Consultation And Relational Empathy, range=10–50) | 93 | 43.9 | 27–50 |
| Change in distress (Spielberger State-Trait Anxiety Inventory-S) | 100 | -2.33 | −23.33 to 23.33 |
| Moderating variable | |||
| Social anxiety (Social Phobia Scale-6 and Social Interactional Anxiety Scale-6, range=0–40) | 99 | 1.0 | 0–20 |
Note: For the empathy measure we omitted data of all patients who filled in “does not apply” on at least 3 items (n=6; 6%), which is an acceptable number for this measure.36 One patient did not respond to the social anxiety questionnaire. Therefore, data of this patient were excluded from moderation analyses
Outcomes of the Multilevel Associations
Association between Physician Face Gaze and Patients’ Trust
Face gaze and trust were not significantly associated as indicated by our multilevel regression. The regression coefficient of −0.16 (P=0.098) corresponds with a small to moderate effect size (D=−0.22) (Table 3).44 When adjusting for gender, age, education, caregiver presence, and social anxiety, there was a significant, inverse relation between face gaze and trust. The regression coefficient of −0.17 (P=0.048) corresponds with a small to moderate effect size (D=−0.24). Social anxiety did not moderate the relation between face gaze and trust (P=0.32). The addition of gender, age, education level, and caregiver presence as covariates did not alter test results (P=0.48).
Table 3.
Multilevel Regression Models between Physician Face Gaze and Patient Trust, Perceived Empathy, and Distress
| Trust Wake Forest Physician Trust Scale |
Perceived empathy Consultation and Relational Empathy |
Distress Spielberger State-Trait Anxiety Inventory-S |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Β (95%CI) | P (n) | D | Β (95%CI) | P (n) | D | Β (95%CI) | P (n) | D | |
| Crude | −0.16 (−0.34, 0.03) | 0.098 (100) | −0.22 | 0.90 (−2.56, 4.37) | 0.609 (93) | 0.08 | 1.37 (0.52, 3.27) | 0.155 (100) | 0.14 |
| Adjusted for patient gender, age, education, social anxiety, and caregiver presence) | −0.17(−0.34, −0.00) | 0.048 (99) | −0.24 | 2.22 (−1.15, 5.60) | 0.197 (93) | 0.21 | 1.34 (−0.58, 3.27) | 0.172 (100) | 0.13 |
Note: all models had physician as a nesting factor. Crude analysis is the multilevel regression between the outcome (trust, perceived empathy, distress) and face gaze. Models are adjusted for patient, gender, age, education, social anxiety, and caregiver presence. All intercepts (B), confidence intervals (CI), values of significance (P), sample size (n), and effect sizes (D), for each model are displayed
Association between Physician Face Gaze and Exploratory Outcome Measures
There was no significant relation between face gaze and perceived empathy as indicated by our multilevel regression. The regression coefficient of 0.90 (P=0.609) corresponds to a small effect size (D=0.08). Adjustment for gender, age, education level, caregiver presence, and social anxiety did not alter test results (P=0.197) and corresponded with a small to moderate effect size (D=0.21). There was no significant relation between face gaze and change in distress as indicated by our multilevel regression. The regression coefficient of 1.37 (P=0.155) corresponds with a small effect size (D=0.14). The addition of gender, age, education level, caregiver presence, and social anxiety as covariates did not change this result.
DISCUSSION
We investigated whether physicians’ face gaze towards their patients predicted patients’ trust. Our results suggest that more face gaze is associated with lower trust, but only when correcting for patient gender, age, education level, and social anxiety, and for the presence of a caregiver. No relation was found between physician face gaze and patient perception of physician empathy or patient distress. Moreover, patients’ social anxiety did not moderate the relation between physician face gaze and patient trust levels.
We hypothesized a positive relation between physicians’ gaze towards the patient and patients’ trust,5, 11 but found the opposite. This contrast may be explained by methodological differences between our study and previous research. We were the first to measure face gaze with eye-tracking in this setting, which enables high observational precision.2 Previous research assessed face gaze using less objective methodologies, such as observer-based coding of video recordings.7–9, 21 Perhaps, researchers are biased to believe that face gaze has positive effects, which may have influenced their assessment and hence the results. It is possible that face gaze has subconscious effects that are yet poorly understood. To the best of our knowledge, only one previous study using more traditional observational methods found a negative relation between physician face gaze and a patient outcomes, specifically distress.22 In the current study, this specific relation was not confirmed. This could be due to differences in patient characteristics: the previous study included patients visiting for genetic breast cancer counseling, whereas our study included internal medicine patients. Patients visiting for genetic breast cancer counseling, often do so to receive emotional support or reduce worries, which differs from follow-up care of the internal medicine patients.22
Another possible explanation for a negative relation between face gaze and trust could lie in the physician’s perception of the quality of communication.50 Trust is a dyadic construct that is created and adjusted in interaction.50 Longer face gaze duration in the current study may occur in more difficult conversations, e.g., involving interactions about emotionally charged issues or in interactions, in which the physician senses a lack of trust in the patient.22 In those circumstances, the physician may unconsciously pay more attention and gaze more extensively to the patient. At the same time, this could feel less comfortable for the patient and may lead to less positive judgements about the physician. Unfortunately, we could not test this assumption because we did not classify the specific content or quality of the communication. Future research should take into account the content of the consultation to explain the relation between face gaze and outcomes.
The negative relation between face gaze and trust could alternatively be explained by the “eye contact effect”,11 meaning that perceived gaze affects neurobehavioral responses and cognitive processing.51, 52 These responses to gaze include, for example, higher bodily self-awareness and a decreased capability to perform cognitive tasks.52–56 In our setting, this would mean that the feeling of being observed could interfere with patients’ trust in their physician. A consultation with a physician can evoke stress in the patient which, in combination with higher levels of physician gaze and associated neurobehavioral and cognitive effects, could lead to decreased trust in the physician because the patient feels overly observed by the physician.57 Previous studies demonstrating the “eye contact effect” were experimental.52–56 To further investigate whether the “eye contact effect” may be relevant to the physician-patient setting, we recommend the integration of such measurements (e.g., assessing autonomic responses) in clinical studies.
Social anxiety did not moderate the relation between physicians’ face gaze and patient trust. Previous studies found such associations in student samples (i.e., including young and highly educated people) and used different questionnaires to assess social anxiety.23, 24 In contrast, our sample included more variation in age and education levels. Furthermore, social anxiety levels were low in our sample, with little variation, which could explain the lack of a moderation effect. We recommend that future research further entangles the relation between face gaze and trust, especially for samples of socially anxious individuals. This could be relevant to understand and adapt to the communication needs of such socially more vulnerable individuals.
A limitation of this study is that we did not distinguish between face gaze towards the patient versus towards the caregiver. Therefore, the measured gaze towards the patient could be an overestimation in the minority of consultations including a caregiver. Secondly, the effects of face gaze of the physician towards the patient on trust were only present when adjusted for confounding variables, i.e., gender, age, educational level, the presence of a caregiver, and social anxiety. Third, we cannot exclude the possibility of a Hawthorne effect, meaning that results may have been biased because physicians were aware of being observed.58 Finally, we did not take into account the face gaze of the patient towards the physician, because we did not want to overly burden patients. Earlier studies show that the level of face gaze in a conversation depends on both individuals.59 Face gaze is a bidirectional, interactional phenomenon, in which individuals adjust their level of face gaze towards each other. Future studies should therefore additionally take into account patients’ face gaze towards the physician. Furthermore, our sample was largely homogeneous. Future research could take into account cultural context, such as ethnicity, of patients and physicians.60
Study strengths include being the first to utilize mobile eye-tracking glasses, which allow for more objective and precise measurement of physician face gaze compared to other modalities (e.g., observer-based coding of video recordings).2 Second, we have included a much larger sample compared to earlier mobile eye-tracking studies.24, 61–63
Concluding, we unexpectedly found physician face gaze to be negatively associated with patients’ trust in their physician. Therefore, our results challenge the current view that physician gaze is by definition beneficial to patients and their trust, encouraging continued and more in-depth research on this topic. The results give strength to the nuance of communication skills, in that good communication skills are not simply a discrete set of behaviors, but rather, a set of behaviors that must be appropriate for certain contexts and situations. Ultimately, these findings may lead to enhancement of physician-patient communication, improving their relation and thereby the quality of care. We found no relation between face gaze and other outcomes, i.e., patients’ perception of physician empathy and patient distress. Future studies should be performed to better understand the relation between nonverbal communication and outcomes. These should involve the bidirectional study of face gaze in physician-patient consultations and account for the level of emotional talk in the consultation.
Acknowledgements
The authors thank all patients, caregivers, and physicians, who participated in this study.
Declarations
Conflict of Interest
The authors declare that they do not have a conflict of interest.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Kleinke CL. Gaze and eye contact: a research review. Psychological bulletin. 1986;100(1):78. doi: 10.1037/0033-2909.100.1.78. [DOI] [PubMed] [Google Scholar]
- 2.Jongerius C, Hessels RS, Romijn JA, Smets E, Hillen MA. The Measurement of Eye Contact in Human Interactions: A Scoping Review. JOURNAL OF NONVERBAL BEHAVIOR. 2020.
- 3.Freeth M, Foulsham T, Kingstone A. What affects social attention? Social presence, eye contact and autistic traits. PloS one. 2013;8(1):e53286. doi: 10.1371/journal.pone.0053286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Jokinen K, Harada K, Nishida M, Yamamoto S, editors. Turn-alignment using eye-gaze and speech in conversational interaction. Eleventh Annual Conference of the International Speech Communication Association; 2010.
- 5.Hillen MA, de Haes HC, van Tienhoven G, Bijker N, van Laarhoven HW, Vermeulen DM, et al. All eyes on the patient: the influence of oncologists’ nonverbal communication on breast cancer patients’ trust. Breast cancer research and treatment. 2015;153(1):161–71. doi: 10.1007/s10549-015-3486-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mikesell L. Medicinal relationships: caring conversation. Medical education. 2013;47(5):443–52. doi: 10.1111/medu.12104. [DOI] [PubMed] [Google Scholar]
- 7.Montague E, Asan O. Dynamic modeling of patient and physician eye gaze to understand the effects of electronic health records on doctor–patient communication and attention. International journal of medical informatics. 2014;83(3):225–34. doi: 10.1016/j.ijmedinf.2013.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gorawara-Bhat R, Dethmers DL, Cook MA. Physician eye contact and elder patient perceptions of understanding and adherence. Patient education and counseling. 2013;92(3):375–80. doi: 10.1016/j.pec.2013.03.002. [DOI] [PubMed] [Google Scholar]
- 9.Ambady N, Koo J, Rosenthal R, Winograd CH. Physical therapists’ nonverbal communication predicts geriatric patients’ health outcomes. Psychology and aging. 2002;17(3):443. doi: 10.1037/0882-7974.17.3.443. [DOI] [PubMed] [Google Scholar]
- 10.Mast MS. On the importance of nonverbal communication in the physician–patient interaction. Patient education and counseling. 2007;67(3):315–8. doi: 10.1016/j.pec.2007.03.005. [DOI] [PubMed] [Google Scholar]
- 11.MacDonald K. Patient-clinician eye contact: social neuroscience and art of clinical engagement. Postgraduate medicine. 2009;121(4):136–44. doi: 10.3810/pgm.2009.07.2039. [DOI] [PubMed] [Google Scholar]
- 12.Bayliss AP, Tipper SP. Predictive gaze cues and personality judgments: Should eye trust you? Psychological Science. 2006;17(6):514–20. doi: 10.1111/j.1467-9280.2006.01737.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Asan O. D. Smith P, Montague E. More screen time, less face time–implications for EHR design. Journal of evaluation in clinical practice. 2014;20(6):896–901. doi: 10.1111/jep.12182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Asan O, Young HN, Chewning B, Montague E. How physician electronic health record screen sharing affects patient and doctor non-verbal communication in primary care. Patient education and counseling. 2015;98(3):310–6. doi: 10.1016/j.pec.2014.11.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Margalit RS, Roter D, Dunevant MA, Larson S, Reis S. Electronic medical record use and physician–patient communication: an observational study of Israeli primary care encounters. Patient education and counseling. 2006;61(1):134–41. doi: 10.1016/j.pec.2005.03.004. [DOI] [PubMed] [Google Scholar]
- 16.Bohannon LS, Herbert AM, Pelz JB, Rantanen EM. Eye contact and video-mediated communication: A review. Displays. 2013;34(2):177–85. doi: 10.1016/j.displa.2012.10.009. [DOI] [Google Scholar]
- 17.Ward P. Trust and communication in a doctor-patient relationship: a literature review. Arch Med. 2018;3(3):36. [Google Scholar]
- 18.Thom DH. Physician behaviors that predict patient trust. Journal of Family Practice. 2001;50(4):323-. [PubMed]
- 19.Polinski J, Kesselheim A, Frolkis J, Wescott P, Allen-Coleman C, Fischer M. A matter of trust: patient barriers to primary medication adherence. Health Education Research. 2014;29(5):755–63. doi: 10.1093/her/cyu023. [DOI] [PubMed] [Google Scholar]
- 20.Ernstmann N, Wirtz M, Nitzsche A, Gross SE, Ansmann L, Gloede TD, et al. Patients’ trust in physician, patient enablement, and health-related quality of life during colon cancer treatment. Journal of Cancer Education. 2017;32(3):571–9. doi: 10.1007/s13187-017-1166-y. [DOI] [PubMed] [Google Scholar]
- 21.Montague E, Chen P-y, Xu J, Chewning B, Barrett B. Nonverbal interpersonal interactions in clinical encounters and patient perceptions of empathy. J Participat Med. 2013;5:e33.
- 22.Pieterse AH, Van Dulmen AM, Beemer FA, Bensing JM, Ausems MG. Cancer genetic counseling: communication and counselees’ post-visit satisfaction, cognitions, anxiety, and needs fulfillment. Journal of Genetic Counseling. 2007;16(1):85–96. doi: 10.1007/s10897-006-9048-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hessels RS, Holleman GA, Cornelissen TH, Hooge IT, Kemner C. Eye contact takes two–autistic and social anxiety traits predict gaze behavior in dyadic interaction. Journal of Experimental Psychopathology. 2018;9(2):jep. 062917.
- 24.Honma M. Hyper-volume of eye-contact perception and social anxiety traits. Consciousness and cognition. 2013;22(1):167–73. doi: 10.1016/j.concog.2012.12.002. [DOI] [PubMed] [Google Scholar]
- 25.Schulze L, Renneberg B, Lobmaier JS. Gaze perception in social anxiety and social anxiety disorder. Frontiers in human neuroscience. 2013;7:872. doi: 10.3389/fnhum.2013.00872. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Teachman BA, Allen JP. Development of social anxiety: Social interaction predictors of implicit and explicit fear of negative evaluation. Journal of Abnormal Child Psychology. 2007;35(1):63. doi: 10.1007/s10802-006-9084-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Russell G, Shaw S. A study to investigate the prevalence of social anxiety in a sample of higher education students in the United Kingdom. Journal of Mental Health. 2009;18(3):198–206. doi: 10.1080/09638230802522494. [DOI] [Google Scholar]
- 28.Katzelnick DJ, Kobak KA, DeLeire T, Henk HJ, Greist JH, Davidson JR, et al. Impact of generalized social anxiety disorder in managed care. American Journal of Psychiatry. 2001;158(12):1999–2007. doi: 10.1176/appi.ajp.158.12.1999. [DOI] [PubMed] [Google Scholar]
- 29.Tobii Pro. Tobii Pro Glasses 2 2019 [July 10, 2019]. Available from: https://www.tobiipro.com/product-listing/tobii-pro-glasses-2/.
- 30.Tobii Pro. Tobii Pro Lab 2019 [July 10, 2019]. Available from: https://www.tobiipro.com/product-listing/tobii-pro-lab/.
- 31.Nyström M, Andersson R, Holmqvist K, Van De Weijer J. The influence of calibration method and eye physiology on eyetracking data quality. Behavior research methods. 2013;45(1):272–88. doi: 10.3758/s13428-012-0247-4. [DOI] [PubMed] [Google Scholar]
- 32.Jongerius C, Callemein T, Goedemé T, Van Beeck K, Romijn JA, Smets E, et al. Eye-tracking glasses in face-to-face interactions: manual versus automated assessment of Areas-of-Interest. 2021;In press. [DOI] [PMC free article] [PubMed]
- 33.Qualtrics. Provo, UT, USA2020.
- 34.Bachinger SM, Kolk AM, Smets EM. Patients’ trust in their physician—Psychometric properties of the Dutch version of the “Wake Forest Physician Trust Scale”. Patient Education and Counseling. 2009;76(1):126–31. doi: 10.1016/j.pec.2008.11.020. [DOI] [PubMed] [Google Scholar]
- 35.Hall MA, Camacho F, Lawlor JS, DePuy V, Sugarman J, Weinfurt K. Measuring trust in medical researchers. Medical care. 2006:1048-53. [DOI] [PubMed]
- 36.van Dijk I. Scholten Meilink Lenferink N, Lucassen PL, Mercer SW, van Weel C, Speckens AE. Reliability and validity of the Dutch version of the Consultation and Relational Empathy Measure in primary care. Family Practice. 2017;34(1):119–24. doi: 10.1093/fampra/cmw116. [DOI] [PubMed] [Google Scholar]
- 37.Mercer SW, Maxwell M, Heaney D, Watt G. The consultation and relational empathy (CARE) measure: development and preliminary validation and reliability of an empathy-based consultation process measure. Family practice. 2004;21(6):699–705. doi: 10.1093/fampra/cmh621. [DOI] [PubMed] [Google Scholar]
- 38.Marteau TM, Bekker H. The development of a six-item short-form of the state scale of the Spielberger State—Trait Anxiety Inventory (STAI) British journal of clinical Psychology. 1992;31(3):301–6. doi: 10.1111/j.2044-8260.1992.tb00997.x. [DOI] [PubMed] [Google Scholar]
- 39.van der Bij AK, de Weerd S, Cikot RJ, Steegers EA, Braspenning JC. Validation of the dutch short form of the state scale of the Spielberger State-Trait Anxiety Inventory: considerations for usage in screening outcomes. Public Health Genomics. 2003;6(2):84–7. doi: 10.1159/000073003. [DOI] [PubMed] [Google Scholar]
- 40.Peters L, Sunderland M, Andrews G, Rapee RM, Mattick RP. Development of a short form Social Interaction Anxiety (SIAS) and Social Phobia Scale (SPS) using nonparametric item response theory: The SIAS-6 and the SPS-6. Psychological assessment. 2012;24(1):66. doi: 10.1037/a0024544. [DOI] [PubMed] [Google Scholar]
- 41.de Beurs E, Tielen D, Wollmann L. The Dutch social interaction anxiety scale and the social phobia scale: reliability, validity, and clinical utility. Psychiatry journal. 2014;2014. [DOI] [PMC free article] [PubMed]
- 42.Faul F, Erdfelder E. GPOWER: A priori, post-hoc, and compromise power analyses for MS-DOS [Computer program] Bonn, FRG: Bonn University, Department of Psychology; 1992. [Google Scholar]
- 43.Faul F, Erdfelder E, Buchner A, Lang A-G. Statistical power analyses using G* Power 3.1: Tests for correlation and regression analyses. Behavior research methods. 2009;41(4):1149–60. doi: 10.3758/BRM.41.4.1149. [DOI] [PubMed] [Google Scholar]
- 44.Cohen J. Statistical power analysis for the behavioral sciences. 2. Hillsdale, NJ, USA: Á/L. Erbaum Press; 1988. [Google Scholar]
- 45.SPSS Inc. 26 ed. Chicago, IL, USA2020.
- 46.McBee M. Modeling outcomes with floor or ceiling effects: An introduction to the Tobit model. Gifted Child Quarterly. 2010;54(4):314–20. doi: 10.1177/0016986210379095. [DOI] [Google Scholar]
- 47.Hillen M, Koning C, Wilmink J, Klinkenbijl J, Eddes E, Kallimanis-King B, et al. Assessing cancer patients’ trust in their oncologist: development and validation of the Trust in Oncologist Scale (TiOS) Supportive Care in Cancer. 2012;20(8):1787–95. doi: 10.1007/s00520-011-1276-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Halepian L, Saleh MB, Hallit S, Khabbaz LR. Adherence to insulin, emotional distress, and trust in physician among patients with diabetes: a cross-sectional study. Diabetes Therapy. 2018;9(2):713–26. doi: 10.1007/s13300-018-0389-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.StataCorp. In: 14, editor. College Station, Texas, USA2020.
- 50.Petrocchi S, Iannello P, Lecciso F, Levante A, Antonietti A, Schulz P. Interpersonal trust in doctor-patient relation: Evidence from dyadic analysis and association with quality of dyadic communication. Social science & medicine. 2019;235:112391. doi: 10.1016/j.socscimed.2019.112391. [DOI] [PubMed] [Google Scholar]
- 51.Senju A, Johnson MH. The eye contact effect: mechanisms and development. Trends in cognitive sciences. 2009;13(3):127–34. doi: 10.1016/j.tics.2008.11.009. [DOI] [PubMed] [Google Scholar]
- 52.Conty L, Russo M, Loehr V, Hugueville L, Barbu S, Huguet P, et al. The mere perception of eye contact increases arousal during a word-spelling task. Social neuroscience. 2010;5(2):171–86. doi: 10.1080/17470910903227507. [DOI] [PubMed] [Google Scholar]
- 53.Baltazar M, Hazem N, Vilarem E, Beaucousin V, Picq J-L, Conty L. Eye contact elicits bodily self-awareness in human adults. Cognition. 2014;133(1):120–7. doi: 10.1016/j.cognition.2014.06.009. [DOI] [PubMed] [Google Scholar]
- 54.Pönkänen LM, Peltola MJ, Hietanen JK. The observer observed: Frontal EEG asymmetry and autonomic responses differentiate between another person's direct and averted gaze when the face is seen live. International Journal of Psychophysiology. 2011;82(2):180–7. doi: 10.1016/j.ijpsycho.2011.08.006. [DOI] [PubMed] [Google Scholar]
- 55.Conty L, George N, Hietanen JK. Watching Eyes effects: When others meet the self. Consciousness and cognition. 2016;45:184–97. doi: 10.1016/j.concog.2016.08.016. [DOI] [PubMed] [Google Scholar]
- 56.Conty L, Gimmig D, Belletier C, George N, Huguet P. The cost of being watched: Stroop interference increases under concomitant eye contact. Cognition. 2010;115(1):133–9. doi: 10.1016/j.cognition.2009.12.005. [DOI] [PubMed] [Google Scholar]
- 57.De Haes H, Bensing J. Endpoints in medical communication research, proposing a framework of functions and outcomes. Patient education and counseling. 2009;74(3):287–94. doi: 10.1016/j.pec.2008.12.006. [DOI] [PubMed] [Google Scholar]
- 58.Franke RH, Kaul JD. The Hawthorne experiments: First statistical interpretation. American sociological review. 1978:623-43.
- 59.Broz F, Lehmann H, Nehaniv CL, Dautenhahn K, editors. Mutual gaze, personality, and familiarity: Dual eye-tracking during conversation. 2012 IEEE RO-MAN: The 21st IEEE International Symposium on Robot and Human Interactive Communication; 2012: IEEE.
- 60.Cooper LA, Powe NR. Disparities in patient experiences, health care processes, and outcomes: The role of patient–provider racial, ethnic, and language concordance: Commonwealth Fund New York, NY. 2004. [Google Scholar]
- 61.Franchak JM, Kretch KS, Adolph KE. See and be seen: Infant–caregiver social looking during locomotor free play. Developmental science. 2018;21(4):e12626. doi: 10.1111/desc.12626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.King M, Hu F, McHugh J, Murphy E, Newman E, Irving K, et al., editors. Visibility of wearable sensors as measured using eye tracking glasses. International Joint Conference on Ambient Intelligence; 2013: Springer.
- 63.Ye Z, Li Y, Fathi A, Han Y, Rozga A, Abowd GD, et al., editors. Detecting eye contact using wearable eye-tracking glasses. Proceedings of the 2012 ACM conference on ubiquitous computing; 2012: ACM.