Abstract
Pediatric functional abdominal pain disorders (FAPD) are associated with elevated anxiety in youth and their caregivers, both contributing to an adverse impact on functioning in youth with FAPD. While a CBT approach (i.e., Aim to Decrease Anxiety and Pain Treatment [ADAPT]) is known to improve health outcomes for youth, it is unknown if child-focused treatment improves caregiver anxiety. This secondary analysis of a larger randomized clinical trial examined if child-focused CBT (ADAPT) for pain and anxiety also impacts caregiver anxiety and explored the relation between caregiver anxiety and child symptoms (i.e., pain, disability, anxiety) after treatment. A total of 79 caregiver-child dyads were randomized to ADAPT plus treatment as usual (TAU) or TAU only. Caregiver anxiety and child outcomes (pain, disability, anxiety) were assessed at baseline and approximately eight weeks later. Caregivers of children who completed ADAPT+TAU demonstrated lower anxiety compared to those who only received TAU. Moreover, regardless of treatment assignment, caregivers with greater anxiety had children who reported more pain and anxiety, but not functional disability at post-assessment. Results suggest a brief, child-focused intervention targeting pain and anxiety may also improve caregiver anxiety. As such, suggestions to improve future treatments are offered.
Keywords: pediatric, anxiety, pain, functional abdominal pain, cognitive behavioral therapy, caregiver, parent
Introduction
Functional abdominal pain disorders (FAPD) in youth are highly prevalent and can lead to significant impairments across multiple domains of functioning.10,12,21,35,70 Symptoms of pediatric FAPD can be persistent and, after appropriate medical evaluation, are not attributed to another medical condition.22,37 For a subset of youth, FAPD is associated with persistent pain-related symptoms and development of other psychological problems (e.g., anxiety, depression) that may persist over the long term.56,70
Anxiety-related concerns in youth with FAPD are extremely common and often extend beyond worries directly related to abdominal pain.10,21 Anxiety disorders co-occur in up to two-thirds of youth with chronic pain,36 with high rates of clinical anxiety evidenced in youth with FAPD.10,20,21,23 Further, anxiety disorders predict the maintenance of somatic symptoms over time,49,65 heightened pain sensitivity,67 increased functional impairment,73 and limited response to cognitive-behavioral treatment (CBT) in youth with FAPD.16
Although co-occurring anxiety in FAPD can affect child functioning and treatment response, the literature has recently focused on examining the dynamic association between child pain, psychological function, and the broader family environment and dynamics.4,43,50,54 Specifically, families with children who have chronic pain conditions are likely to have poorer family functioning (e.g., greater family conflict and less family cohesion) compared to families with healthy children.43 Caring for a child with chronic pain can be distressing for a parent, which may evoke pain-promoting caregiver behaviors (e.g., reinforcement of pain through attention, special privileges, etc.) in an effort to ameliorate both child and parent symptoms.55,60 Indeed, caregivers of youth with chronic pain, such as FAPD, demonstrate increased rates of anxiety and general emotional and cognitive distress,11,24,57 which subsequently predicts maladaptive behaviors in response to child pain.9,28,68 These parenting behaviors can then contribute to increased pain perception and child maladjustment.2,8,13,24,58,63,71
Family-focused treatments incorporating parental psychoeducation and family systems therapies are effective in reducing symptoms of pediatric pain in samples of youth with mixed chronic pain conditions,5,25,26,31,41,42,59 though the impact of these treatments on parental mental health is equivocal.25 One examination drawing from a combined inpatient- and day-based child treatment program found that improvements in parental mental health and other broader indices of functioning (i.e., parenting behaviors, social functioning, etc.) predicted improved child functioning and pain reductions in a mixed child chronic pain sample.5 Such intensive treatment approaches can be costly, so it is important to determine if brief outpatient and child-focused treatments can similarly improve caregiver mental health and if these treatments are specifically effective for caregivers of youth with FAPD. Our recent work suggests that youth with FAPD and anxiety benefit from brief treatments that combine in-person and web-based CBT techniques (i.e., Aim to Decrease Anxiety in Pain Treatment [ADAPT]).18,19 Although participating youth displayed improvements in pain-related functioning and anxiety symptoms following ADAPT, it remains unclear if this intervention may also affect caregiver symptoms.
The primary aim of this study is to determine if this brief child-focused intervention for FAPD (ADAPT + medical treatment as usual [TAU]) impacts caregiver anxiety compared to TAU only. A second aim is to examine how caregiver anxiety may relate to child outcomes (e.g., pain, functional disability, and anxiety) at post-treatment assessment.
Methods
Participants
Children and caregivers enrolled in a study evaluating the feasibility of a stepped-care approach and the impact of ADAPT on child outcomes were included in this investigation.18 Eligible child-caregiver dyads were recruited from outpatient pediatric gastroenterology clinics affiliated with a children’s hospital in the Midwestern United States between 2015 and 2018. Children were recruited and deemed eligible if they were between the ages of 9 and 14 years old, diagnosed with FAPD by a gastroenterologist using a checklist based on Rome IV Criteria,37 and evidenced more than a minimal degree of disability (i.e., Functional Disability Inventory [FDI] score ≥ 7; see Measures) as a function of their FAPD. Potential participants were excluded if they were diagnosed with a significant medical condition with an identifiable organic cause, including conditions that may cause abdominal pain (e.g., Celiac Disease, Crohn’s Disease). All procedures were approved by the medical center’s Institutional Review Board and written informed consent and verbal assent was obtained from the child’s caregiver and the child, respectively.
Procedures and Intervention
After obtaining caregiver/patient consent, youth completed a battery of questionnaires reporting on their pain, functional disability, and anxiety. All eligible participants received the first step of care, Enhanced Usual Care (EUC), consisting of basic psychoeducation on pain coping (e.g., gate control theory) and access to several audio-recorded relaxation activities during the clinic visit. Two weeks later, patients were re-screened to re-assess for primary study eligibility (i.e., sustained evidence of more than minimal disability; see Measures). Participants with evidence of more than minimal levels of disability (i.e., FDI score ≥ 7) were then invited to participate in a baseline assessment. During this assessment, children and their caregivers completed a battery of questionnaires (i.e., demographics, caregiver anxiety symptoms). Please refer to the original study18 for additional details.
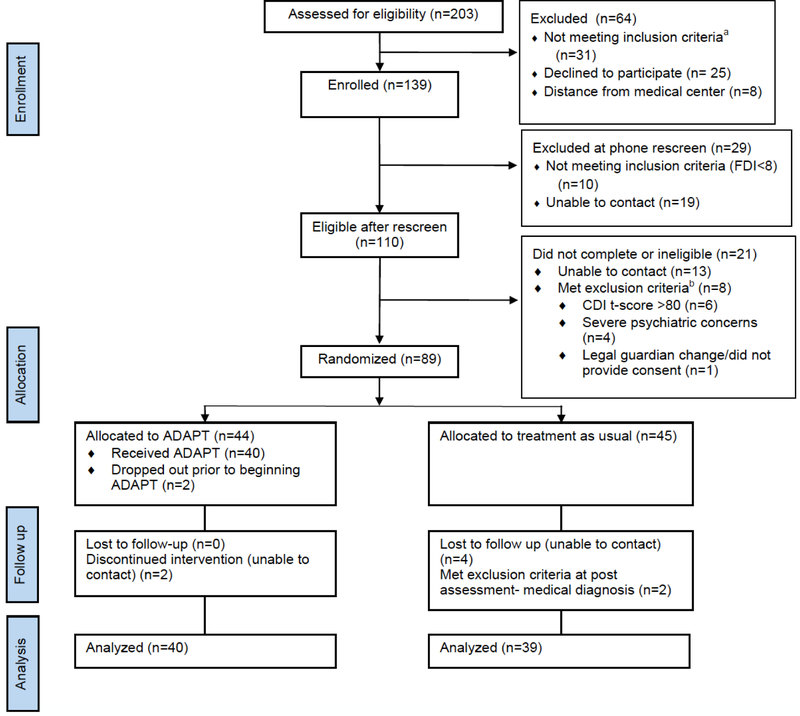
Participants were then randomized from a computer-generated list to receive either ADAPT+TAU or TAU (see Figure 1) using a parallel group, two-arm, superiority trial design with a 1:1 allocation ratio. The study statistician generated the randomization sequence, retained exclusive access to the randomization schedule, and assigned participants to interventions. Study clinicians were trained post-baccalaureate research coordinators who were blinded to treatment allocation. Advanced graduate students in psychology or postdoctoral fellows in psychology served as treatment interventionists with clinical oversight from a licensed psychologist.
Figure 1.
Consort flow diagram for patients enrolled in ADAPT+TAU versus TAU alone. Reproduced from primary outcome paper.18 This figure was published in The Journal of Pediatrics, Cunningham N, Kalomiris A, Peugh J, Farrell M, Pentiuk S, Mallon D, Le C, Moorman E, Fussner L, Dutta RA, Kashikar-Zuck S, Cognitive Behavior Therapy Tailored to Anxiety Symptoms Improves Pediatric Functional Abdominal Pain Outcomes: A Randomized Clinical Trial, Copyright Elsevier (2020).
Note: aInclusion criteria: 1) Between 9–14 years of age, 2) Diagnosed with FAPD by a gastroenterologist or primary care provider, and 3) More than minimal disability as evidenced by a total score of ≥7 on the FDI.
bParticipants meeting exclusion criteria were deemed ineligible due to mental health concerns if they demonstrated severe depressive symptoms or psychiatric concerns. Three of the 8 participants excluded demonstrated evidence of both of these mental health exclusionary criteria.
ADAPT is a brief, child-focused CBT program with minimal caregiver involvement (see Table 1) designed to help youth manage pain and anxiety associated with FAPD. ADAPT participants took part in 2 in-person sessions and either 2 or 4 web-based sessions with interventionist phone support, depending on presence of child anxiety. In-person sessions were predominantly completed with the child, though caregivers attended a portion of Session 1 to receive psychoeducation on the mind-body connection with regards to the experience of pediatric pain and caregiver guidelines for helping a child to manage chronic pain and anxiety (see Table 1). ADAPT phone support sessions occurred primarily with the child but also consisted of a brief caregiver check-in (5–10 minutes) to receive updates on the child’s progress and to address any questions or concerns. Approximately 8 weeks after baseline, all children and caregivers completed a battery of post-treatment questionnaires, again assessing caregiver anxiety and child symptoms (i.e., pain, functional disability, anxiety).
Table 1.
ADAPT Intervention Components for Youth with FAPD and Their Caregivers
| Intervention Session | Platform | Caregiver Involvement | Session Content and Target Concern |
|---|---|---|---|
| Session 1 | In-person | Direct Participation, 40 minutes | • Program overview a
• Psychoeducation (Pain and Anxiety)a • Parent Guidelines (Pain) a,b • Deep Breathing/Guided Imagery (Pain) |
| Session 2 | In-person | End of Session Review, 10 minutes | • Progressive Muscle Relaxation (Pain) • Calming Statements (Pain) • Activity Pacing (Pain) |
| Session 3 | Web and phone | Brief Check-In, 5 minutes | • Pleasant Activity Scheduling (Pain) • Problem Solving (Pain) |
| Session 4 | Web and phone | Brief Check-In, 5 minutes | • Cognitive Restructuring (Anxiety) |
| Session 5 | Web and phone | Brief Check-In, 5 minutes | • Guided Exposure (Anxiety) • Assertiveness Training (Anxiety) |
| Session 6 | Web and phone | Brief Check-In, 5 minutes | • Maintenance Planning (Pain and Anxiety) |
Note. ADAPT = Aim to Decrease Anxiety and Pain Treatment; FAPD = Functional abdominal pain disorders; All ADAPT sessions were approximately 60 minutes. Web sessions of ADAPT were completed by the child participant independently (30 minutes) followed by phone support (15–30 minutes total) with the interventionist. Phone sessions were conducted primarily between the interventionist and child participant, with a brief portion of time reserved to check-in with caregivers. Caregivers received a review of child skills at the end of in-person sessions and through online videos.
active caregiver participation
content directed towards caregiver, which included how to help child cope with pain/anxiety by encouraging independence, eliminating status checks, giving the child praise for using coping skills, and encouraging normal activity for periods of pain/worry.
Measures
Caregiver anxiety.
Caregivers completed the 21-item short-form of the Depression Anxiety and Stress Scales (DASS) which is designed to measure the core symptoms of anxiety, depression, and stress.44 This instrument has previously demonstrated excellent reliability and internal validity,3,29 and is widely used to assess affective symptoms in both community and clinical samples.3,64 Caregivers were asked to report how much a statement applied to them over the past week using a 0 (did not apply to me at all) to 3 (applied to me very much, or most of the time) scale. Caregivers completed this instrument at the baseline visit and at the end of treatment. A sum of the 7-items comprising the anxiety subscale (e.g., I felt scared without any good reason) was calculated separately for the baseline (α = .85) and post-treatment (α = .85) assessments. The anxiety subscale has cut-off scores for normal (0–3), mild (4–5), moderate (6–7), severe (8–9), and extreme (10+) anxiety symptoms. The anxiety subscale was the focus in this investigation given that the ADAPT intervention is designed to target anxiety specifically, and due to prior literature establishing a link between caregiver anxiety and child pain-related outcomes.57
Functional disability.
Children completed the Functional Disability Inventory (FDI), a 15-item self-report measure of disability in youth with chronic pain.69 This measure assesses a variety of activity limitations in youth as a result of a chronic health condition. It demonstrates strong validity and relates to measures of general somatic symptoms.15 At screening and following treatment, children were asked to report if they had any physical trouble or difficulty completing a variety of activities in the past few days using a 0 (no trouble) to 4 (impossible) scale. The FDI has established total cut-off scores to indicate mild (< 13), moderate (13–29), and severe (30+) disability.32 On average, healthy youth have a total FDI score of 3.5,69 therefore a score ≥ 7 (double the value of healthy youth’s average score) is indicative of more than minimal disability due to pain. This score was used to establish eligibility for participation in the primary outcome study. A total score was calculated from both the screening (α = .85) and post-treatment (α = .89) assessments, with higher scores indicating greater functional disability.
Pain intensity.
Children reported on their average pain levels on a 0 (no pain) to 10 (maximal) scale over the previous two weeks using a Visual Analog Scale (VAS).46 This measure is widely used to assess a variety of chronic and acute pain conditions in children and adults. Higher scores indicate greater pain, with scores ≥ 4 generally indicating moderate amounts of pain. Children were asked to report on their pain at screening and after completing treatment.
Child anxiety.
Children reported on their anxiety symptoms using the 41-item Screen for Child-Anxiety Related Disorders (SCARED).6,7,48 This measure is widely used in pediatric populations to assess a wide array of symptoms of anxiety (i.e., general, separation, social, and somatic symptoms, as well as school avoidance) and demonstrates strong convergent and discriminant validity.6,7 A total sum was calculated across all items, with total scores ≥ 25 suggestive of the presence of clinical level of impairment congruent to a DSM (Diagnostic and Statistical Manual of Mental Disorders) psychological disorder diagnosis.1,17 Children were asked to report how much a statement applied to them over the past three months using a 0 (not true or hardly ever true) to 2 (very true or often true) scale. Children completed this instrument at screening (α = .93) and again at the end of treatment (α = .95), with higher scores indicating more symptoms of anxiety.
Demographics.
Caregivers completed a demographic questionnaire at the baseline visit from which child sex, age, and racial/ethnic background was obtained. In addition, caregivers reported on their own sex, relation to the child participating, parental educational attainment, and parental pain history.
Analytic Plan and Missing Data
A priori power analyses were conducted to determine the required sample size, after which data collection was terminated. Descriptive statistics and bivariate relations among the variables were computed using SPSS version 25 (Table 2). The total score for anxiety could be calculated for a total of 75 caregivers at baseline. Similarly, a total of 75 caregivers reported on their anxiety symptoms at post-treatment. These groups of 75 contained different participants, so a total of 71 (90%) of all caregivers provided complete data at baseline and post-assessment. Caregivers providing complete data at either time point did not generally differ significantly from those who did not provide complete data on demographic or other study variables, with a few exceptions at post-treatment: Caregivers, regardless of their role, were more likely to provide a self-report of their anxiety symptoms if the female caregiver had higher educational attainment (i.e., some college, at minimum; χ2 = 10.50, p = .001). In addition, caregivers whose children reported more pain at post-treatment (t [77] = 2.26, p = .027) were also more likely to report on their anxiety symptoms.
Table 2.
Descriptive Statistics and Pearson Correlations Among the Primary Variables
| M | SD | Range | 2 | 3 | 4 | 5 | 6 | 7 | 8 | |
|---|---|---|---|---|---|---|---|---|---|---|
| 1. DASS (Baseline) | 3.67 | 4.27 | 0.00 – 16.00 | .65*** | .03 | .15 | .15 | .27* | .26* | .28* |
| 2. DASS (Post-treatment) | 3.11 | 3.91 | 0.00 – 15.00 | -- | -.02 | .28* | -.02 | .16 | .29* | .35** |
| 3. VAS (Baseline) | 3.75 | 1.86 | 0.00 – 8.70 | -- | .53*** | .38** | .27* | .08 | .04 | |
| 4. VAS (Post) | 2.73 | 2.22 | 0.00 – 8.60 | -- | .25* | .54*** | .02 | .26* | ||
| 5. FDI (Baseline) | 17.87 | 8.17 | 8.00 – 47.00 | -- | .39*** | .28* | .30** | |||
| 6. FDI (Post) | 11.33 | 9.48 | 0.00 – 41.00 | -- | .24* | .67*** | ||||
| 7. SCARED (Baseline) | 35.12 | 15.68 | 4.00 – 67.00 | -- | .62*** | |||||
| 8. SCARED (Post) | 25.46 | 16.56 | 1.00 – 63.00 | -- |
Note. DASS (Depression Anxiety and Stress Scales) assesses caregiver report of anxiety symptoms. VAS (Visual Analog Scale) assesses child report of severity of pain. FDI (Functional Disability Inventory) assesses child report of functional disability resulting from pain. SCARED (Screen for Child Anxiety Related Disorders) assesses child report of anxiety symptoms. Table contains means and standard deviations for participants used in primary and exploratory analyses.
p < .05
p < .01
p < .001.
Percent reductions were calculated to initially examine decreases in caregiver anxiety between the two treatment groups. Multiple linear regression in Stata version 1566 was used to assess differences in anxiety symptoms for caregivers whose children completed ADAPT+TAU versus TAU alone using maximum likelihood estimation (MLE). Multiple linear regression was used for its ability to control for covariates and greater power as compared to assessing for mean differences. MLE is widely accepted for handling missing data and adjusts the likelihood function so that parameter estimates are only informed by available data. Treatment condition was represented by a binary variable (0 = TAU, 1 = ADAPT+TAU). Analyses controlled for baseline caregiver anxiety symptoms. These analyses also controlled for caregiver sex due to a marginally significant bivariate relation among caregiver sex and caregiver report of anxiety symptoms at post-treatment (r = −.19, p = .098; 0 = female, 1 = male).
A total score was calculated for child participants with missing items on the SCARED (n = 3 [3.80%]), as the number of missing data points (i.e., missing ≤ 2 [<4.88%] items within a questionnaire) was lower than previously established cut-off points (i.e., <10%).61,72 Degree of missing composite-level data was very low for child report of symptoms at baseline (VAS: n = 2 [2.53%], FDI: n = 1 [1.27%]; SCARED: n = 1 [1.27%]) and post-treatment (VAS: n = 0 [0%], FDI: n = 0 [0%]; SCARED: n = 0 [0%]). In order to explore how caregiver anxiety may affect child clinical symptoms (regardless of treatment condition), child post-treatment scores (i.e., VAS, FDI, SCARED) were separately regressed on post-treatment caregiver anxiety. The regression analyses controlled for the child’s respective baseline symptom (i.e., VAS, FDI, SCARED) and caregiver anxiety at baseline. These analyses were again conducted using Stata version 15 using MLE.
Results
Participant Demographics
A total of 203 youth were assessed for eligibility and 139 qualified (see Figure 1). All qualified participants received EUC, and 110 continued to evidence more than minimal disability after the re-screen. Of those, 89 youth remained eligible and were randomized to begin ADAPT+TAU or medical TAU alone. The most common reasons why participants were ineligible include the inability to contact (n = 13), severe psychopathology (n = 7), and study withdrawal (n = 1). Ultimately, 79 youth completed the post assessment, indicating an 88.8% retention rate. Thus, the current sample of treatment completers consisted of 79 child-caregiver dyads (Figure 1; ADAPT+TAU: n = 40, TAU alone: n = 39). Detailed demographic information on this sample is reported in Table 3. The children ranged in age from 9–14 years (M = 11.71, SD = 1.76) and were mostly female (n = 47, 59.49%). The most common diagnoses were FAPD Not Otherwise Specified ([NOS]; n = 45, 56.96%) and Irritable Bowel Syndrome (n = 31, 34.24%). Most children identified as Caucasian and non-Hispanic (n = 71, 89.87%). The participating caregiver was also generally female (n = 69, 87.34%). Most caregivers identified as mothers (n = 64, 81.01%) or fathers (n = 7, 8.86%) of the child participants, though some grandparents (n = 6, 7.59%) and legal guardians such as foster parents (n = 2, 2.53%) participated. Participating caregivers reported that both household caregivers had obtained at least a high school diploma (female caregivers: n = 79, 100%; male caregivers: n = 75, 94.94%). A history of chronic pain was reported in male (17.7%) and female (31.6%) caregivers. Of those caregivers who reported chronic pain, back pain was the most common, followed by headache and abdominal pain.
Table 3.
Sample Characteristics
| ADAPT+TAU (n = 40) |
TAU (n = 39) |
|
|---|---|---|
| Sex | ||
| Female | 20 | 27 |
| Male | 20 | 12 |
| Age M (SD) | 11.67 (1.58) | 11.74 (1.94) |
| Race | ||
| Caucasian | 35 | 38 |
| Asian American | 0 | 0 |
| American Indian | 0 | 1 |
| African American | 3 | 0 |
| Biracial | 1 | 0 |
| Other | 1 | 0 |
| Ethnicity | ||
| Hispanic/Latino | 1 | 1 |
| Pain Diagnosis | ||
| FAPD-NOS | 25 | 20 |
| IBS | 14 | 17 |
| Functional Dyspepsia | 0 | 1 |
| Abdominal Migraine | 1 | 1 |
| Participating Caregiver | ||
| Mother | 33 | 31 |
| Father | 4 | 3 |
| Grandmother | 3 | 2 |
| Grandfather | 0 | 1 |
| Foster Parent | 0 | 2 |
| Caregiver High School Completion | ||
| Mother | 40 | 39 |
| Father | 37 | 38 |
| Caregiver Reported Chronic Pain | ||
| Mother | 9 | 16 |
| Father | 3 | 11 |
| Caregiver Symptoms at Baseline | ||
| DASS M (SD) | 3.54 (4.28) | 3.81 (4.31) |
| Child Symptoms at Baseline | ||
| VAS M (SD) | 3.86 (2.06) | 3.64 (1.64) |
| FDI M (SD) | 19.85 (8.74) | 15.78 (7.05) |
| SCARED M (SD) | 34.00 (18.19) | 35.87 (12.71) |
| Caregiver Symptoms at Post | ||
| DASS M (SD) | 2.49 (3.29) | 3.71 (4.40) |
| VAS M (SD) | 2.50 (2.10) | 3.00 (2.36) |
| FDI M (SD) | 10.20 (8.91) | 12.49 (10.02) |
| SCARED M (SD) | 22.02 (16.39) | 29.00 (16.20) |
Note. Analyses were conducted to determine if demographic or clinical symptom differences were present at baseline between randomization groups. No significant differences in demographics between groups were detected (all χ2s < 3.03, ps > .082, t = 0.17, p = .863), aside from father’s pain history (χ2 = 5.34, p = 0.021). Children assigned to ADAPT+TAU reported higher functional disability at baseline (t = −2.25, p = .027). Groups did not differ on any other clinical symptoms at baseline.
ADAPT = Aim to Decrease Anxiety and Pain Treatment; TAU = Treatment as Usual; FAPD-NOS = Functional Abdominal Pain Disorder-Not Otherwise Specified; IBS = Irritable Bowel Syndrome; DASS = Depression Anxiety and Stress Scales, assesses caregiver report of anxiety symptoms; VAS = Visual Analog Scale; FDI = Functional Disability Inventory; SCARED = Screen for Child Anxiety Related Disorders.
Primary and Exploratory Analyses
Primary analyses were conducted to determine if the ADAPT+TAU resulted in significant reductions in caregiver anxiety compared to TAU only. Caregivers participating in ADAPT+TAU displayed a 29.6% reduction in anxiety (Mpre = 3.54, SDpre = 4.28; Mpost = 2.49, SDpost = 3.29) whereas caregivers undergoing medical TAU only experienced a 2.62% change (Mpre = 3.81, SDpre = 4.31; Mpost = 3.71, SDpost = 4.40). Indeed, regression analyses controlling for caregiver’s sex and baseline anxiety revealed that caregiver anxiety decreased significantly more for those caregivers of children receiving ADAPT+TAU versus TAU only (Table 4; b = −1.42, SE = 0.68, t = −2.10, p = .036, 95% CI = [−2.75, −0.09]).
Table 4.
Post-Treatment Caregiver Anxiety Symptoms Following Treatment
| b | SE | t-value | p | 95% CI | |
|---|---|---|---|---|---|
| Primary Study Aim | |||||
| DV: Caregiver Anxiety (Post-treatment) | |||||
| Intercept | 2.03 | 0.59 | 3.44 | .001 | 0.87 – 3.19 |
| Treatment Condition | −1.42 | 0.68 | −2.10 | .036 | −2.75 – −0.09 |
| Caregiver Sex | −1.89 | 0.98 | −1.93 | .054 | −3.80 – 0.03 |
| Caregiver Anxiety (Baseline) | 0.61 | 0.08 | 7.37 | .000 | 0.45 – 0.77 |
Note. DV = Dependent variable (i.e., outcome variable). Treatment condition represents binary variable with 0 = TAU and 1 = ADAPT+TAU. Caregiver gender was coded such that 0 = female and 1 = male. Caregiver anxiety symptoms were assessed from caregiver report on the DASS (Depression Anxiety and Stress Scales).
Additional analyses were conducted to determine the link between caregiver anxiety and child symptoms (i.e., pain, functional disability, anxiety) after 8 weeks (regardless of treatment assignment). There was a significant link between caregiver anxiety and child pain intensity post-treatment (Table 5; b = 0.21, SE = 0.07, t = 3.24, p = .001, 95% CI = [0.08, 0.34]), such that caregivers with greater reported anxiety following treatment had children who also reported more pain following treatment. The relation between caregiver anxiety and child functional disability following treatment was not significant, though it was in the expected direction (Table 5; b = 0.36, SE = 0.32, t = 1.13, p = .259, 95% CI = [−0.26, 0.98]). Finally, caregivers who reported greater anxiety symptoms following treatment also had children who reported more anxiety symptoms after treatment (Table 5; b = 1.05, SE = 0.49, t = 2.15, p = .032, 95% CI = [0.09, 2.01]). Note that these main effects controlled for baseline levels of caregiver anxiety and respective child symptoms.
Table 5.
Relation Among Caregiver Anxiety and Child Clinical Symptoms Following Treatment
| b | SE | t-value | p | 95% CI | |
|---|---|---|---|---|---|
| Exploratory Study Aims | |||||
| DV: Child VAS (Post-treatment) | |||||
| Intercept | 0.04 | 0.47 | 0.08 | .933 | −0.88 – 0.96 |
| Caregiver Anxiety (Post-treatment) | 0.21 | 0.07 | 3.24 | .001 | 0.08 – 0.34 |
| Child VAS (Baseline) | 0.57 | 0.11 | 5.31 | .000 | 0.36 – 0.78 |
| Caregiver Anxiety (Baseline) | −0.06 | 0.06 | −0.94 | .349 | −0.18 – 0.06 |
| DV: Child FDI (Post-treatment) | |||||
| Intercept | 2.37 | 2.38 | 1.00 | .318 | −2.28 – 7.03 |
| Caregiver Anxiety (Post-treatment) | 0.36 | 0.32 | 1.13 | .259 | −0.26 – 0.98 |
| Child FDI (Baseline) | 0.37 | 0.12 | 3.16 | .002 | 0.14 – 0.60 |
| Caregiver Anxiety (Baseline) | 0.24 | 0.30 | 0.79 | .430 | −0.36 – 0.83 |
| DV: Child SCARED (Post-treatment) | |||||
| Intercept | 2.25 | 3.53 | 0.64 | .524 | −4.67 – 9.17 |
| Caregiver Anxiety (Post-treatment) | 1.05 | 0.49 | 2.15 | .032 | 0.09 – 2.01 |
| Child SCARED (Baseline) | 0.59 | 0.10 | 6.14 | .000 | 0.40 – 0.77 |
| Caregiver Anxiety (Baseline) | −0.16 | 0.46 | −0.35 | .725 | −1.07 – 0.74 |
Note. DV = Dependent variable (i.e., outcome variable). VAS (Visual Analogue Scale) assesses child report of severity of pain. FDI (Functional Disability Inventory) assesses child report of functional disability resulting from pain. SCARED (Screen for Child Anxiety Related Disorders) assesses child report of anxiety symptoms. Caregiver anxiety symptoms were assessed from caregiver report on the DASS (Depression Anxiety and Stress Scales).
Discussion
Caregivers of children who completed ADAPT+TAU demonstrated lower anxiety compared to those whose children only received TAU. Moreover, regardless of treatment assignment, caregivers with greater anxiety had children who reported more pain and anxiety, but not functional disability at post-assessment. Importantly, caregivers of youth with FAPD and other chronic pain syndromes also experience higher rates of anxiety.11 The role of caregiver mental health requires further investigation given a host of research suggesting that caregiver anxiety is associated with pain-promoting parenting behaviors,60,68 adverse pain and anxiety-related outcomes in children,14,27,60 and even prospectively predicts the onset of future recurrent abdominal pain in children.57 Although novel psychological treatments are emerging that effectively improve pediatric pain- and anxiety-related outcomes,18,19 it is important to examine whether current treatments for child anxiety and pain also impact caregiver anxiety. Caregivers are typically incorporated into child-focused treatments to provide psychoeducation and to promote child adherence. Previously, brief caregiver-focused CBT interventions have shown to be effective in managing parenting behaviors40 and mental health51 as well as child mental51 and physical health outcomes.40 However, is a child-focused approach sufficient to address caregiver anxiety symptoms? At present, the effect of child-focused CBT for pediatric FAPD on caregiver psychological functioning is not well understood. The current investigation specifically examines the role of a brief, child-focused CBT (designed to target pediatric pain and anxiety in FAPD) on caregiver anxiety symptoms.
Our results suggest that a brief outpatient CBT (ADAPT)18,19 for children with FAPD +TAU results in statistically significant reductions in general caregiver anxiety when compared to TAU only. However, it should be noted that caregivers’ anxiety in both conditions remained within the “normal” range of symptoms throughout the research study. Although the link between child and caregiver psychological functioning is well established, only recently have investigations focused on examining how interventions for youth with chronic pain may impact parental psychosocial functioning.5,31 A meta-analysis of 47 randomized clinical trials examining family-based, child-focused therapies for pediatric conditions not specific to chronic pain suggested that parental mental health may not be universally impacted by these interventions.25 With regard to chronic pain, however, no study included in that meta-analysis explicitly examined mental health outcomes in parents. Two more recent investigations of intensive treatment programs for youth with mixed chronic pain conditions examining parental mental health have emerged,5,31 where parents were provided with regular instruction and support, as well as participated in multiple parent-focused sessions. While one of these investigations revealed that parent anxiety levels and general functioning improved significantly following treatment and at a 6-month follow up,5 the other investigation did not find significant differences in parental anxiety symptoms following treatment.31 Results from the current investigation, therefore, uniquely contribute to this evolving literature and reveal that caregivers of youth with FAPD may benefit from a predominantly child-focused CBT.
In comparison to the more intensive programs detailed above, the caregiver component of the ADAPT intervention was brief and consisted of instruction to support the child’s independent coping with pain and/or worries and how to allocate attention appropriately to prevent the inadvertent reinforcement of somatic symptoms. Caregivers were also provided with summaries of skills (e.g., relaxation strategies, problem solving) their child learned to manage their pain symptoms. Therefore, this child-focused intervention is minimally burdensome to the caregiver while still yielding significant reductions in caregiver anxiety. There may be various factors (e.g., anxiety management skills taught as part of the ADAPT intervention, caregiver response to improvements in the child’s symptoms) that may account for the improvement in caregiver anxiety symptoms. Future investigations are warranted to determine if caregiver pain symptoms, which may also be elevated in caregivers of youth with FAPD,11 are similarly reduced from this intervention. Further, additional work is necessary to better understand the dosage of caregiver involvement required to achieve reductions in child and caregiver symptoms. It is possible that the degree of caregiver involvement required may vary based on the severity of child/caregiver symptoms38,39 or the child’s chronic pain diagnosis.25 Interestingly, these preliminary findings suggest ADAPT (a “low dose” treatment for caregivers) is useful for improving caregiver anxiety in families of youth with FAPD.
Exploratory analyses also revealed that caregivers who reported greater anxiety following both ADAPT+TAU and TAU alone treatments also had children who indicated greater pain and anxiety following treatment. This supports existing literature indicating that increased pain and psychological symptoms may cluster in families.11 Interpreted another way, those caregivers who reported fewer anxiety symptoms following treatment also had children who indicated lower levels of pain and anxiety following treatment. These findings suggest that caregiver mental health and child physical and mental health may shift in tandem as a result of ADAPT treatment (or as a result of improvements in child symptoms). Previous work also supports this association and reveals that caregiver emotional health is linked to child pain, functional disability, and anxiety.11,14,16,33,53 While caregiver anxiety was not related to child disability following treatment, it is possible that the rate of change in caregiver anxiety may be slower than the child’s change in function. Prior work has demonstrated a more pronounced reduction in child disability as compared to child pain immediately following treatment,45 though this is not universally found.52 Given this equivocal evidence, future work is needed to determine the temporal relations among changes in these constructs and their link to caregiver anxiety.
Although this investigation suggests ADAPT is effective in reducing caregiver anxiety, understanding the mechanisms leading to this effect remains a crucial next step for future investigations. Exploratory analyses revealing the link between caregiver anxiety and child symptoms at post assessment (regardless of treatment condition) may imply that child anxiety management strategies are effective for caregiver anxiety as well. Perhaps explicitly encouraging caregiver practice and modeling, mentioning how such skills are effective for general anxiety, or non-clinical distress management should be a standard part of pediatric FAPD treatment. The directionality of the relation among caregiver and child symptoms remains unclear, however, so future work should examine caregiver and child symptoms across multiple time points to determine if changes in one member of the dyad’s symptoms precedes or causes changes in the other. It is also possible that caregiver perceptions of increased support from their child’s participation in psychological treatment may alleviate caregiver stress and subsequently improve the caregiver’s psychological well-being.30,31 This may explain why previous treatment examinations revealed that parents of clinically anxious children demonstrate reductions in their own anxiety even without an active parent-training component.62 Further, the effectiveness of family-based treatment for child anxiety disorders may be superior to individual treatment when both parents have anxiety,34 suggesting that anxious parents may benefit from participation in their child’s treatment. Finally, although it was beyond the scope of the current investigation to examine if ADAPT results in observable changes in parenting behaviors,41,42 previous work and theory suggests that caregivers with higher distress regarding their child’s pain may engage in more maladaptive parenting behaviors in response to child pain.4,9,28 It will be interesting for future work to examine how ADAPT may also impact caregiver behaviors in response to child pain symptoms.
It is also worth noting that previous family-based treatment investigations suggest that changes in caregiver mental health and broader functioning predicted improvements in child pain-related functioning and reductions in child pain ratings 6-months following intensive behavioral treatment.5 The current study is limited by its concurrent assessment of caregiver and child symptoms following treatment, but future longitudinal work across multiple time points should examine if similar changes in child symptoms are sustained as a direct result of improvements in caregiver anxiety. Future investigations should also compare treatments that are more child-focused, such as ADAPT, to more comprehensive, family-focused treatments5,25,26,31,41,42,59 that directly target caregiver symptoms on longitudinal child pain- and anxiety-related outcomes.
These results should be interpreted in light of the following limitations: The sample size was relatively small yet offered compelling preliminary evidence of the efficacy of this intervention for reducing caregiver symptoms of anxiety. Additionally, the sample was relatively homogenous among child participants, which is not representative of the larger socio-economic and racial/ethnic composition of the broader nation. Although a variety of caregivers participated, the majority of participating caregivers were women and identified as mothers. Rates of anxiety differ across sexes,47 and although caregiver sex was controlled for in analyses, additional research examining group differences in caregiver anxiety would be beneficial. Unfortunately, caregiver demographics (e.g., age, race, and ethnicity) were not collected in the current investigation. Future work should more comprehensively measure and explore caregiver characteristics. While results showed that caregivers whose children received ADAPT+TAU experienced a reduction in anxiety across eight-weeks (i.e., immediately following treatment), it is unknown how long the effects on caregiver outcomes are sustained. Future investigations should explore if treatment gains are maintained for caregivers, and how this may affect their child’s symptoms. Existing work suggests that parental anxiety may predict the onset of future FAPD,57 though it may also be that FAPD or other chronic pain conditions may result in caregiver stress that can affect both child and caregiver mental health.24 Future work should elucidate the mechanisms leading to changes in caregiver anxiety and child symptoms following ADAPT treatment. In addition, factors contributing to caregivers’ reduction in anxiety, such as improvement in the child’s symptomology or functioning, should be specifically explored to further understand this relationship. Finally, though child pain symptoms were a focus of ADAPT, caregivers’ attitudes (e.g., pain catastrophizing) and parenting behaviors towards their child’s pain were beyond the scope of the investigation. It is important for future studies to examine such caregiver factors in relation to child’s pain functioning after ADAPT.
In conclusion, results of this current randomized clinical trial provide initial evidence that an outpatient CBT intervention designed to target pain and anxiety in pediatric FAPD may also improve caregiver anxiety symptoms. This is particularly important to consider given the established relationship between caregiver anxiety and child symptoms of pain and anxiety, which was further supported in this investigation. Results therefore suggest that a brief and multi-method child-focused intervention may be an effective tool useful for reducing caregiver anxiety in families of youth with FAPD.
Highlights.
Caregivers whose children received treatment for pain and anxiety had lower anxiety
Greater caregiver anxiety was related to greater child anxiety outside of treatment
Greater caregiver anxiety was related to greater child pain regardless of treatment
Caregiver anxiety was not related to child disability regardless of treatment
Perspective.
Caregiver anxiety symptoms diminished after their child with functional abdominal pain completed a course of child-focused CBT targeting pain and anxiety. Further, caregiver anxiety was related to child-reported symptoms (pain and anxiety) after treatment. Therefore, improved caregiver mental health via a child-focused CBT may also improve pediatric outcomes.
Acknowledgements
We would like to thank Christine Le, Erin Moorman, and Dr. Lauren Fussner for their assistance with data collection and management. We would also like to thank Dr. James Peugh for providing his statistical expertise in this study’s design.
Disclosures
All phases of this study were supported by the Sharon S. Keller American Pain Society Grant and the Cincinnati Children’s Hospital Place Outcomes Award (both awarded to the senior author, NRC). In addition, the senior author (NRC) is currently supported by a National Institutes of Health award [K23 AT009458]. The authors have no financial disclosures relevant to this article to report. The authors do not have any conflicts of interest to disclose.
Footnotes
Trial Registration: ClinicalTrials.gov, NCT03134950.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.American Psychiatric Association: Diagnostic and statistical manual of mental disorders, 5th ed. Arlington, VA, American Psychiatric Pub, 2013 [Google Scholar]
- 2.Anthony KK, Bromberg MH, Gil KM, Schanberg LE: Parental perceptions of child vulnerability and parent stress as predictors of pain and adjustment in children with chronic arthritis. Child Health Care 40:53–69, 2011 [Google Scholar]
- 3.Antony MM, Bieling PJ, Cox BJ, Enns MW, Swinson RP: Psychometric properties of the 42-item and 21-item versions of the depression anxiety stress scales in clinical groups and a community sample. Psychol Assess 10:176–181, 1998 [Google Scholar]
- 4.Asmundson GJ, Noel M, Petter M, Parkerson HA: Pediatric fear-avoidance model of chronic pain: foundation, application and future directions. Pain Res Manag 17:397–405, 2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Benore E, Brenner A, Banez GA, Wang L, Worley S: It takes two: parent functioning within the pediatric chronic pain experience and interdisciplinary rehabilitation treatment. Rehabil Psychol 63:205–214, 2018 [DOI] [PubMed] [Google Scholar]
- 6.Birmaher B, Brent DA, Chiappetta L, Bridge J, Monga S, Baugher M: Psychometric properties of the screen for child anxiety related emotional disorders (SCARED): a replication study. J Am Acad Child Adolesc Psychiatry 38:1230–1236, 1999 [DOI] [PubMed] [Google Scholar]
- 7.Birmaher B, Khetarpal S, Brent D, Cully M, Balach L, Kaufman J, Neer SM: The screen for child anxiety related emotional disorders (SCARED): scale construction and psychometric characteristics. J Am Acad Child Adolesc Psychiatry 36:545–553, 1997 [DOI] [PubMed] [Google Scholar]
- 8.Brace MJ, Scott Smith M, McCauley E, Sherry DD: Family reinforcement of illness behavior: a comparison of adolescents with chronic fatigue syndrome, juvenile arthritis, and healthy controls. J Dev Behav Pediatr 21:332–339, 2000 [DOI] [PubMed] [Google Scholar]
- 9.Caes L, Vervoort T, Trost Z, Goubert L: Impact of parental catastrophizing and contextual threat on parents’ emotional and behavioral responses to their child’s pain. Pain 153:687–695, 2012 [DOI] [PubMed] [Google Scholar]
- 10.Campo JV, Bridge J, Ehmann M, Altman S, Lucas A, Birmaher B, Di Lorenzo C, Iyengar S, Brent DA: Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 113:817–824, 2004 [DOI] [PubMed] [Google Scholar]
- 11.Campo JV, Bridge J, Lucas A, Savorelli S, Walker L, Di Lorenzo C, Iyengar S, Brent DA: Physical and emotional health of mothers of youth with functional abdominal pain. Arch Pediatr Adolesc Med 161:131–137, 2007 [DOI] [PubMed] [Google Scholar]
- 12.Campo JV, Comer DM, Jansen-Mcwilliams L, Gardner W, Kelleher KJ: Recurrent pain, emotional distress, and health service use in childhood. J Pediatr 141:76–83, 2002 [DOI] [PubMed] [Google Scholar]
- 13.Chambers CT, Craig KD, Bennett SM: The impact of maternal behavior on children’s pain experiences: an experimental analysis. J Pediatr Psychol 27:293–301, 2002 [DOI] [PubMed] [Google Scholar]
- 14.Chow ET, Otis JD, Simons LE: The longitudinal impact of parent distress and behavior on functional outcomes among youth with chronic pain. J Pain 17:729–738, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Claar RL, Walker LS: Functional assessment of pediatric pain patients: psychometric properties of the functional disability inventory. Pain 121:77–84, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Cohen LL, Vowles KE, Eccleston C: The impact of adolescent chronic pain on functioning: disentangling the complex role of anxiety. J Pain 11:1039–1046, 2010 [DOI] [PubMed] [Google Scholar]
- 17.Cunningham NR, Jagpal A, Peugh J, Farrell MK, Cohen MB, Mezoff AG, Lynch-Jordan A, Kashikar-Zuck S: Risk categorization predicts disability in pain-associated functional gastrointestinal disorders after 6 months. J Pediatr Gastroenterol Nutr 64:685–690, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Cunningham NR, Kalomiris A, Peugh J, Farrell M, Pentiuk S, Mallon D, Le C, Moorman E, Fussner L, Dutta RA, Kashikar-Zuck S: Cognitive behavior therapy tailored to anxiety symptoms improves pediatric functional abdominal pain outcomes: a randomized clinical trial. J Pediatr 230:62–70.e63, 2021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Cunningham NR, Nelson S, Jagpal A, Moorman E, Farrell M, Pentiuk S, Kashikar-Zuck S: Development of the aim to decrease anxiety and pain treatment for pediatric functional abdominal pain disorders. J Pediatr Gastroenterol Nutr 66:16–20, 2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Di Lorenzo C, Colletti RB, Lehmann HP, Boyle JT, Gerson WT, Hyams JS, Squires RHJ, Walker LS, Kanda PT: Chronic abdominal pain in children: a clinical report of the American Academy of Pediatrics and the North American Society For Pediatric Gastroenterology, Hepatology And Nutrition: American Academy of Pediatrics Subcommittee on Chronic Abdominal Pain and Naspghan Committee on Abdominal Pain. J Pediatr Gastroenterol Nutr 40:245–248, 2005 [DOI] [PubMed] [Google Scholar]
- 21.Dorn LD, Campo JC, Thato S, Dahl RE, Lewin D, Chandra R, Di Lorenzo C: Psychological comorbidity and stress reactivity in children and adolescents with recurrent abdominal pain and anxiety disorders. J Am Acad Child Adolesc Psychiatry 42:66–75, 2003 [DOI] [PubMed] [Google Scholar]
- 22.Drossman DA: Functional gastrointestinal disorders: history, pathophysiology, clinical features and Rome IV. Gastroenterology 150:1262–1279.e2, 2016 [DOI] [PubMed] [Google Scholar]
- 23.Dufton LM, Dunn MJ, Compas BE: Anxiety and somatic complaints in children with recurrent abdominal pain and anxiety disorders. J Pediatr Psychol 34:176–186, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Eccleston C, Crombez G, Scotford A, Clinch J, Connell H: Adolescent chronic pain: patterns and predictors of emotional distress in adolescents with chronic pain and their parents. Pain 108:221–229, 2004 [DOI] [PubMed] [Google Scholar]
- 25.Eccleston C, Fisher E, Law E, Bartlett J, Palermo TM: Psychological interventions for parents of children and adolescents with chronic illness. Cochrane Database Syst Rev 4:Cd009660, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Eccleston C, Palermo TM, Williams AC, Lewandowski Holley A, Morley S, Fisher E, Law E: Psychological therapies for the management of chronic and recurrent pain in children and adolescents. Cochrane Database Syst Rev 2014:Cd003968, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Evans S, Meldrum M, Tsao JC, Fraynt R, Zeltzer LK: Associations between parent and child pain and functioning in a pediatric chronic pain sample: a mixed methods approach. Int J Disabil Hum Dev 9:11–21, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Hechler T, Vervoort T, Hamann M, Tietze AL, Vocks S, Goubert L, Hermann C, Wager J, Blankenburg M, Schroeder S, Zernikow B: Parental catastrophizing about their child’s chronic pain: are mothers and fathers different? Eur J Pain 15:515.e511–519, 2011 [DOI] [PubMed] [Google Scholar]
- 29.Henry JD, Crawford JR: The short-form version of the depression anxiety stress scales (DASS-21): construct validity and normative data in a large non-clinical sample. Br J Clin Psychol 44:227–239, 2005 [DOI] [PubMed] [Google Scholar]
- 30.Homer CJ, Klatka K, Romm D, Kuhlthau K, Bloom S, Newacheck P, Van Cleave J, Perrin JM: A review of the evidence for the medical home for children with special health care needs. Pediatrics 122:e922–937, 2008 [DOI] [PubMed] [Google Scholar]
- 31.Kanstrup M, Wicksell RK, Kemani M, Wiwe Lipsker C, Lekander M, Holmström L: A clinical pilot study of individual and group treatment for adolescents with chronic pain and their parents: effects of acceptance and commitment therapy on functioning. Children (Basel) 3, 2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kashikar-Zuck S, Flowers SR, Claar RL, Guite JW, Logan DE, Lynch-Jordan AM, Palermo TM, Wilson AC: Clinical utility and validity of the functional disability inventory among a multicenter sample of youth with chronic pain. Pain 152:1600–1607, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Kashikar-Zuck S, Parkins IS, Graham TB, Lynch AM, Passo M, Johnston M, Schikler KN, Hashkes PJ, Banez G, Richards MM: Anxiety, mood, and behavioral disorders among pediatric patients with juvenile fibromyalgia syndrome. Clin J Pain 24:620–626, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Kendall PC, Hudson JL, Gosch E, Flannery-Schroeder E, Suveg C: Cognitive-behavioral therapy for anxiety disordered youth: a randomized clinical trial evaluating child and family modalities. J Consult Clin Psychol 76:282–297, 2008 [DOI] [PubMed] [Google Scholar]
- 35.King S, Chambers CT, Huguet A, MacNevin RC, McGrath PJ, Parker L, MacDonald AJ: The epidemiology of chronic pain in children and adolescents revisited: a systematic review. Pain 152:2729–2738, 2011 [DOI] [PubMed] [Google Scholar]
- 36.Knook LME, Konijnenberg AY, van der Hoeven J, Kimpen JLL, Buitelaar JK, van Engeland H, de Graeff-Meeder ER: Psychiatric disorders in children and adolescents presenting with unexplained chronic pain: what is the prevalence and clinical relevancy? Eur Child Adolesc Psychiatry 20:39–48, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Koppen IJ, Nurko S, Saps M, Di Lorenzo C, Benninga MA: The pediatric Rome IV criteria: What’s new? Expert Rev Gastroenterol Hepatol 11:193–201, 2017 [DOI] [PubMed] [Google Scholar]
- 38.Langer SL, Romano JM, Levy RL, Walker LS, Whitehead WE: Catastrophizing and parental response to child symptom complaints. Child Health Care 38:169–184, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Langer SL, Walker LS, Romano JM, Whitehead WE, Feld L, Levy RL: Predictors of maternal responses to child abdominal pain. Child Health Care 36:63–81, 2007 [Google Scholar]
- 40.Levy RL, Langer SL, van Tilburg MAL, Romano JM, Murphy TB, Walker LS, Mancl LA, Claar RL, DuPen MM, Whitehead WE, Abdullah B, Swanson KS, Baker MD, Stoner SA, Christie DL, Feld AD: Brief telephone-delivered cognitive behavioral therapy targeted to parents of children with functional abdominal pain: a randomized controlled trial. Pain 158:618–628, 2017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, DuPen MM, Ballard SA, Labus J, Welsh E, Feld LD, Whitehead WE: Twelve-month follow-up of cognitive behavioral therapy for children with functional abdominal pain. JAMA Pediatr 167:178–184, 2013 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Levy RL, Langer SL, Walker LS, Romano JM, Christie DL, Youssef N, DuPen MM, Feld AD, Ballard SA, Welsh EM, Jeffery RW, Young M, Coffey MJ, Whitehead WE: Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am J Gastroenterol 105:946–956, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lewandowski AS, Palermo TM, Stinson J, Handley S, Chambers CT: Systematic review of family functioning in families of children and adolescents with chronic pain. J Pain 11:1027–1038, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Lovibond PF, Lovibond SH: The structure of negative emotional states: comparison of the depression anxiety stress scales (DASS) with the Beck depression and anxiety inventories. Behav Res Ther 33:335–343, 1995 [DOI] [PubMed] [Google Scholar]
- 45.Lynch-Jordan AM, Sil S, Peugh J, Cunningham N, Kashikar-Zuck S, Goldschneider KR: Differential changes in functional disability and pain intensity over the course of psychological treatment for children with chronic pain. Pain 155:1955–1961, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.McGrath PJ, Walco GA, Turk DC, Dworkin RH, Brown MT, Davidson K, Eccleston C, Finley GA, Goldschneider K, Haverkos L, Hertz SH, Ljungman G, Palermo T, Rappaport BA, Rhodes T, Schechter N, Scott J, Sethna N, Svensson OK, Stinson J, von Baeyer CL, Walker L, Weisman S, White RE, Zajicek A, Zeltzer L: Core outcome domains and measures for pediatric acute and chronic/recurrent pain clinical trials: PedIMMPACT recommendations. J Pain 9:771–783, 2008 [DOI] [PubMed] [Google Scholar]
- 47.McLean CP, Asnaani A, Litz BT, Hofmann SG: Gender differences in anxiety disorders: prevalence, course of illness, comorbidity and burden of illness. J Psychiatr Res 45:1027–1035, 2011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Monga S, Birmaher B, Chiappetta L, Brent D, Kaufman J, Bridge J, Cully M: Screen for child anxiety-related emotional disorders (SCARED): convergent and divergent validity. Depress Anxiety 12:85–91, 2000 [DOI] [PubMed] [Google Scholar]
- 49.Mulvaney S, Lambert EW, Garber J, Walker LS: Trajectories of symptoms and impairment for pediatric patients with functional abdominal pain: a 5-year longitudinal study. J Am Acad Child Adolesc Psychiatry 45:737–744, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Palermo TM, Chambers CT: Parent and family factors in pediatric chronic pain and disability: an integrative approach. Pain 119:1–4, 2005 [DOI] [PubMed] [Google Scholar]
- 51.Palermo TM, Law EF, Bromberg M, Fales J, Eccleston C, Wilson AC: Problem-solving skills training for parents of children with chronic pain: a pilot randomized controlled trial. Pain 157:1213–1223, 2016 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Palermo TM, Law EF, Zhou C, Holley AL, Logan D, Tai G: Trajectories of change during a randomized controlled trial of internet-delivered psychological treatment for adolescent chronic pain: how does change in pain and function relate? Pain 156:626–634, 2015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Palermo TM, Putnam J, Armstrong G, Daily S: Adolescent autonomy and family functioning are associated with headache-related disability. Clin J Pain 23:458–465, 2007 [DOI] [PubMed] [Google Scholar]
- 54.Palermo TM, Valrie CR, Karlson CW: Family and parent influences on pediatric chronic pain: a developmental perspective. Am Psychol 69:142–152, 2014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Peterson CC, Palermo TM: Parental reinforcement of recurrent pain: The moderating impact of child depression and anxiety on functional disability. J Pediatr Psychol 29:331–341, 2004 [DOI] [PubMed] [Google Scholar]
- 56.Ramchandani PG, Fazel M, Stein A, Wiles N, Hotopf M: The impact of recurrent abdominal pain: predictors of outcome in a large population cohort. Acta Paediatr 96:697–701, 2007 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Ramchandani PG, Stein A, Hotopf M, Wiles NJ: Early parental and child predictors of recurrent abdominal pain at school age: results of a large population-based study. J Am Acad Child Adolesc Psychiatry 45:729–736, 2006 [DOI] [PubMed] [Google Scholar]
- 58.Reid GJ, McGrath PJ, Lang BA: Parent-child interactions among children with juvenile fibromyalgia, arthritis, and healthy controls. Pain 113:201–210, 2005 [DOI] [PubMed] [Google Scholar]
- 59.Sanders MR, Shepherd RW, Cleghorn G, Woolford H: The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J Consult Clin Psychol 62:306–314, 1994 [DOI] [PubMed] [Google Scholar]
- 60.Sieberg CB, Williams S, Simons LE: Do parent protective responses mediate the relation between parent distress and child functional disability among children with chronic pain? J Pediatr Psychol 36:1043–1051, 2011 [DOI] [PubMed] [Google Scholar]
- 61.Simon E, Bögels SM: Screening for anxiety disorders in children. Eur Child Adolesc Psychiatry 18:625–634, 2009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Simon E, Bögels SM, Voncken JM: Efficacy of child-focused and parent-focused interventions in a child anxiety prevention study. J Clin Child Adolesc Psychol 40:204–219, 2011 [DOI] [PubMed] [Google Scholar]
- 63.Simons LE, Claar RL, Logan DL: Chronic pain in adolescence: parental responses, adolescent coping, and their impact on adolescent’s pain behaviors. J Pediatr Psychol 33:894–904, 2008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Sinclair SJ, Siefert CJ, Slavin-Mulford JM, Stein MB, Renna M, Blais MA: Psychometric evaluation and normative data for the depression, anxiety, and stress scales-21 (DASS-21) in a nonclinical sample of U.S. adults. Eval Health Prof 35:259–279, 2012 [DOI] [PubMed] [Google Scholar]
- 65.Stanford EA, Chambers CT, Biesanz JC, Chen E: The frequency, trajectories and predictors of adolescent recurrent pain: a population-based approach. Pain 138:11–21, 2008 [DOI] [PubMed] [Google Scholar]
- 66.StataCorp L: Stata statistical software: Release 15 (2017). College Station, TX: StataCorp LP, 2017 [Google Scholar]
- 67.Tsao JC, Lu Q, Kim SC, Zeltzer LK: Relationships among anxious symptomatology, anxiety sensitivity and laboratory pain responsivity in children. Cogn Behav Ther 35:207–215, 2006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Vervoort T, Trost Z, Sütterlin S, Caes L, Moors A: Emotion regulatory function of parent attention to child pain and associated implications for parental pain control behaviour. Pain 155:1453–1463, 2014 [DOI] [PubMed] [Google Scholar]
- 69.Walker LS, Greene JW: The functional disability inventory: measuring a neglected dimension of child health status. J Pediatr Psychol 16:39–58, 1991 [DOI] [PubMed] [Google Scholar]
- 70.Walker LS, Guite JW, Duke M, Barnard JA, Greene JW: Recurrent abdominal pain: a potential precursor of irritable bowel syndrome in adolescents and young adults. J Pediatr 132:1010–1015, 1998 [DOI] [PubMed] [Google Scholar]
- 71.Walker LS, Zeman JL: Parental response to child illness behavior. J Pediatr Psychol 17:49–71, 1992 [DOI] [PubMed] [Google Scholar]
- 72.Weitkamp K, Romer G, Rosenthal S, Wiegand-Grefe S, Daniels J: German screen for child anxiety related emotional disorders (SCARED): reliability, validity, and cross-informant agreement in a clinical sample. Child Adolesc Psychiatry Ment Health 4:19, 2010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Wendland M, Jackson Y, Stokes LD: Functional disability in paediatric patients with recurrent abdominal pain. Child Care Health Dev 36:516–523, 2010 [DOI] [PubMed] [Google Scholar]