Abstract
Purpose:
Sling surgery is the gold standard treatment for stress urinary incontinence in women. While data support the use of sling surgery in younger and middle-aged women, outcomes in older, frail women are largely unknown.
Materials and Methods:
Data were examined for all Medicare beneficiaries ≥65 years who underwent sling surgery with or without concomitant prolapse repair from 2014 to 2016. Beneficiaries were stratified using the Claims-based Frailty Index (CFI) into four categories: not frail (CFI <0.15), pre-frail (0.15≤CFI<0.25), mildly frail (0.25≤CFI< 0.35), and moderately-severely frail (CFI ≥0.35). Outcomes included rates and relative risk of 30-day complications, 1-year mortality, and repeat procedures for persistent incontinence or obstructed voiding at 1 year.
Results:
A total of 54,112 women underwent sling surgery during the study period, 5.2% of whom were mildly to moderately-severely frail. Compared to the not frail group, moderately-severely frail beneficiaries demonstrated an increased adjusted Relative Risk (aRR) of 30-day complications [56.5%, aRR 2.5 (95% CI: 2.2-2.9)] and 1-year mortality [10.5%, aRR 6.7 (95% CI: 4.0-11.2)]. Additionally, there were higher rates of repeat procedures in mildly-severely frail beneficiaries [6.6%, aRR 1.4 (95% CI 1.2-1.6)] compared to beneficiaries who were not frail.
Conclusion:
As frailty increased, there was an increased relative risk of 30-day complications, 1-year mortality, and need for repeat procedures for persistent incontinence or obstructed voiding at 1 year. While there were fewer sling surgeries in performed frail women, the observed increase in complication rates was significant. Frailty should be strongly considered before pursuing sling surgery in older women.
Keywords: stress urinary incontinence, aging, frailty, elderly, sling revision
Introduction
Stress urinary incontinence (SUI) is a common clinical condition that affects up to 53% of women over the age of 60.1 Sling surgery, often considered the gold standard treatment, is the most commonly performed operation to treat SUI the United States.2-4 As the population ages, there will be an increase in older women with SUI seeking surgical treatment who are also frail, meaning that they have additional vulnerabilities and an increased risk for poor health outcomes in response to stressors such as surgery5. While sling surgery is generally regarded as a relatively safe and low-risk procedure, most outcomes data are limited to younger and middle-aged women.
However, very little is known about surgical outcomes in frail older adults undergoing this common procedure. While one study looked at outcomes of sling surgery in Medicare beneficiaries over the age of 65, the impact of frailty on outcomes was not examined.6 There is a growing body of literature indicating that frailty is associated with an increased risk of complications after many types of surgery, including urologic procedures.7-10 Given the paucity of data on outcomes of sling surgery in frail women, it remains unknown whether it is reasonable to perform this type of surgery in this particularly vulnerable population, or if it should be avoided entirely.
In order to address this gap in knowledge, we used a 100% cohort of fee-for-service Medicare claims for female beneficiaries, inclusive of all ages and all levels of frailty, who underwent sling surgery with or without concomitant pelvic organ prolapse (POP) repair from 2014-2016 in the United States. Using the Claims-based Frailty Index (CFI), we examined short-term outcomes including 30-day complications, both overall and for rates of urinary tract infections (UTI) specifically, along with 1-year outcomes including 1-year mortality and need for repeat procedures for either obstructed voiding or persistent incontinence at 1 year following sling surgery. Findings of this study will help better define the risks of sling surgery in all older women of who may be considering surgical correction of SUI.
Materials and Methods
Subjects and Database
We used a 100% cohort of female Medicare beneficiaries undergoing sling surgery from 2014 to 2016. Specifically, we used the Medicare Inpatient, Outpatient, Carrier, and Master Beneficiary Summary files to include all fee-for-service care for female Medicare beneficiaries ages 66 and older who underwent sling placement during this time period. Sling surgery was identified using the Current Procedural Terminology (CPT) code 52788 in the Carrier file. Concomitant POP repair was identified using CPT codes for hysterectomy, anterior/posterior repairs, apical repairs, and colpocleisis surgeries (Supplemental Table 1). Institutional Review Board exemption was obtained for this study (#17-23783).
Outcome measures
Both 30-day and 1-year outcomes were assessed. Thirty-day outcomes included 30-day complications, both overall and for UTI separately, as UTI is a well-known complication of sling surgery.6,11,12 Additionally, since UTI is a more minor complication, it was assessed independent of more serious complications. One-year outcomes included 1-year mortality and the need for repeat procedures (for both urinary incontinence and for outlet obstruction) at 1 year. Thirty-day complications were identified using the International Classification of Diseases, Ninth and Tenth Revisions (ICD-9 and ICD-10) diagnosis codes from the Medicare Files, consistent with the existing literature.9,10,13,14 Complications included infection (including UTI), cardiovascular, renal, pulmonary, nervous system including stroke, deep venous thrombosis or pulmonary embolism, delirium, wound complications, postoperative hemorrhage, postoperative shock, complications secondary to anesthesia, other complications, and reoperation. One-year mortality was determined using the date of death from the Master Beneficiary Summary file.
We assessed procedures to address both persistent SUI and obstructed voiding. Repeat SUI procedures included repeat sling placement (CPT 52788) or urethral bulking (CPT 51715). Procedures to correct obstructed voiding included removal or revision of sling (CPT 57287) and urethrolysis (CPT 53500) procedures.
Covariates
To measure frailty, we used the Claims-based frailty index (CFI) which was developed and validated specifically for use with Medicare data.15-17 This index utilizes a weighted deficit accumulation model that takes into account 93 different variables including 52 ICD-9 codes, 25 CPT-4 codes, and 16 Healthcare Common Procedure Coding System (HCPCS) level II codes. This CFI allows for assessment of risk for adverse health outcomes that are not otherwise quantified using demographic characteristics and traditional comorbidity measures in Medicare data. Using this index, we stratified female beneficiaries into four established categories based on level of frailty: not frail (CFI <0.15), pre-frail (0.15≤CFI<0.25), mildly frail (0.25≤CFI< 0.35), and moderately-severely frail (CFI ≥0.35), consistent with the literature.16
Demographic data including age and race were obtained from the Medicare Carrier files. Information on comorbidities was abstracted from the Medicare Inpatient, Outpatient, and Carrier files in the year preceding sling surgery and was used to calculate the Charlson Comorbidity Index (CCI).18
Statistical analyses
Univariate analysis was performed by standard descriptive statistics. For categorical variables, numbers and percentages were reported and Pearson χ2 tests were performed. For continuous variables, mean ± standard deviation (SD) or median with interquartile range (IQR, 25–75%) were presented and ANOVA performed.
Relative risk was calculated by using Generalized Estimating Equations (GEEs) to explore the association between frailty and the outcome variables of interest (30-day complications, 30-day UTIs, 1-year mortality, and repeat procedures for persistent incontinence or obstructed voiding within 1 year of surgery) adjusting for age, race, CCI, concomitant POP repair and type, and calendar year. Both univariate and multivariate models were created. Due to the small number of repeat procedures at 1 year, beneficiaries in the mild and moderate-severe frailty categories were combined into a single category for these analyses.
For all analyses, p = 0.05 on a 2-sided significance test with a 5% a level was considered statistically significant. Analyses were performed using SAS statistical software, v.9.4
Results
A total of 54,112 women ages 66 years and older underwent sling surgery during the study period. The mean age was 73.6 ± 5.6 years, and 92.3% of women were white. The mean CCI in the cohort was 1.6 ± 1.9. Most female beneficiaries were not frail (46.2%) or pre-frail (48.7%), while only 4.8% and 0.4% were characterized as mildly and moderately-severely frail, respectively. Both age and mean CCI increased with increasing CFI categories, while rates of concomitant POP repair declined with increasing CFI categories. (Table 1).
Table 1.
Characteristics of Baseline Cohort Stratified by Claims-based Frailty Index (CFI)
| Total | Not Frail (CFI<0.15) | Prefrail (0.15≤CFI<0.25) |
Mildly Frail (0.25≤CFI<0.35) |
Moderately to severe frail (CFI≥0.35) |
P value | |
|---|---|---|---|---|---|---|
| All Subjects N (%) | 54112 (100.0) | 25012 (46.2) | 26326 (48.7) | 2583 (4.8) | 191 (0.4) | |
| Age N (%): | ||||||
| Mean ± SD | 73.6 ± 5.6 | 72.5 ± 5.0 | 74.4 ± 5.8 | 76.1 ± 6.4 | 77.0 ± 6.5 | <0.001 |
| Median (IQR) | 72.6 (69.0 - 77.1) | 71.50 (68.4 - 75.4) | 73.5 (69.6 - 78.1) | 75.5 (70.8 - 80.4) | 76.4 (72.3 - 81.7) | <0.001 |
| 66-69 | 17468 (32.3) | 9676 (38.7) | 7230 (27.5) | 534 (20.7) | 28 (14.7) | <0.001 |
| 70-74 | 17424 (32.2) | 8478 (33.9) | 8202 (31.2) | 690 (26.7) | 54 (28.3) | |
| 75-79 | 11655 (21.5) | 4689 (18.8) | 6254 (23.8) | 659 (25.5) | 53 (27.8) | |
| 80-85 | 5296 (9.8) | 1653 (6.6) | 3177 (12.1) | 430 (16.7) | 36 (18.9) | |
| ≥85 | 2269 (4.2) | 516 (2.1) | 1463 (5.6) | 270 (10.5) | 20 (10.5) | |
| Race N (%): | ||||||
| White | 49943 (92.3) | 23232 (92.9) | 24128 (91.7) | 2405 (93.1) | 178 (93.2) | <0.001 |
| Black | 1542 (2.9) | 553 (2.2) | 914 (3.5) | 66 (2.6) | 9 (4.7) | |
| Other | 2627 (4.9) | 1227 (4.9) | 1284 (4.9) | 112 (4.3) | 4 (2.1) | |
| Charlson Comorbidity Index N (%): | ||||||
| 0-1 | 33047 (61.1) | 20065 (80.2) | 12613 (47.9) | 364 (14.1) | 5 (2.6) | <0.001 |
| 2-4 | 16614 (30.7) | 4590 (18.4) | 10780 (41.0) | 1189 (46.0) | 55 (28.8) | |
| > 4 | 4451 (8.2) | 357 (1.4) | 2933 (11.1) | 1030 (39.9) | 131 (68.6) | |
| Mean ± SD | 1.6 ± 1.9 | 0.8 ± 1.1 | 2.1 ± 1.9 | 4.1 ± 2.5 | 6.7 ± 2.8 | <0.001 |
| Median (IQR) | 1.0 (0.0 - 2.0) | 0.0 (0.0 - 1.0) | 2.0 (1.0 - 3.0) | 4.0 (2.0 - 6.0) | 6.0 (4.0 - 8.0) | <0.001 |
| Procedure Year N (%): | ||||||
| 2014 | 18949 (35.0) | 8891 (35.6) | 9083 (34.5) | 902 (34.9) | 73 (38.2) | 0.040 |
| 2015 | 17075 (31.6) | 7908 (31.6) | 8265 (31.4) | 844 (32.7) | 58 (30.4) | |
| 2016 | 18088 (33.4) | 8213 (32.8) | 8978 (34.1) | 837 (32.4) | 60 (31.4) | |
| Concomitant POP Repair N (%): | ||||||
| Sling only (no POP repair) | 17170 (31.7) | 6525 (26.1) | 9383 (35.6) | 1150 (44.5) | 112 (58.6) | <0.001 |
| AP repair with sling | 10495 (19.4) | 4423 (17.7) | 5485 (20.8) | 560 (21.7) | 27 (14.1) | |
| Apical repair with sling | 2673 (4.9) | 1389 (5.6) | 1198 (4.6) | 78 (3.0) | 8 (4.2) | |
| AP and apical repair with sling | 9865 (18.3) | 4596 (18.4) | 4831 (18.4) | 414 (16.0) | 24 (12.6) | |
| Hysterectomy and AP repair with sling | 3801 (7.0) | 2204 (8.8) | 1500 (5.7) | 93 (3.6) | 4 (2.1) | |
| Hysterectomy and apical repair with sling | 2564 (4.7) | 1710 (6.8) | 813 (3.1) | 39 (1.5) | 2 (1.1) | |
| Hysterectomy and AP and apical repair with sling | 5912 (10.9) | 3611 (14.4) | 2182 (8.3) | 111 (4.3) | 8 (4.2) | |
| Colpocleisis with sling | 1632 (3.0) | 554 (2.2) | 934 (3.6) | 138 (5.3) | 6 (3.2) |
POP = pelvic organ prolapse; AP = anterior/posterior repair
30-Day Complications
All 30-day complications are shown in Supplemental Table 2. As CFI category increased, rates of all 30-day complications also steadily increased, and moderately-severely frail female beneficiaries demonstrated the highest rate of 30-day complications at 56.5%. UTIs, which were observed in 15.7% of all women within 30 days of sling surgery, represented the most common post-operative complication in this cohort. Similar to all 30-day complications, as CFI categories increased, rates of 30-day UTI increased accordingly, with moderately-severely frail women demonstrating the highest rates of UTI at 37.7% (Figure 1).
Figure 1.
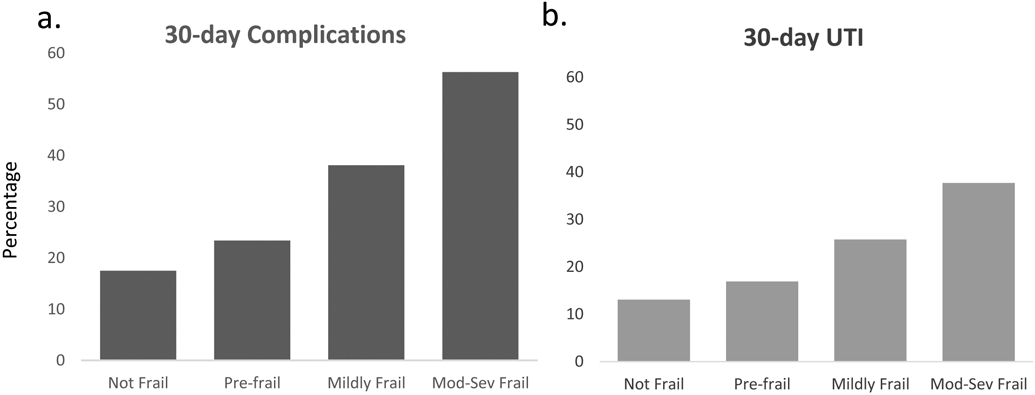
Rates of 30-day complications and 30-day UTI after sling placement stratified by frailty. p<0.001 for both.
After UTI, cardiovascular complications were the next most frequently observed complication in female Medicare beneficiaries. While cardiovascular complications were uncommon in beneficiaries who were not frail (0.5%) they increased to 2.4%, 8.6%, and 19.9% in prefrail, mildly frail, and moderately-severely frail beneficiaries, respectively (p<0.001). Both pulmonary (not frail: 0.8%, prefrail: 1.9%, mildly frail: 5.1%, moderately-severely frail: 9.4%, p<0.001) and renal (not frail: 0.8%, prefrail: 1.7%, mildly frail: 3.6%, moderately-severely frail: 6.3%, p<0.001) complications also increased significantly with increasing CFI category.
Results of multivariate analysis for 30-day complications and 30-day UTIs are shown in Table 2. After adjusting for age, comorbidity, race, concomitant POP repair and type, and calendar year, compared to female beneficiaries who were not frail, those who were pre-frail, mildly frail, moderately-severely frail had an adjusted relative risk (aRR) of any 30-day complication of 1.2 (95% CI: 1.2-1.3; p <0.001), 1.8 (95% CI: 1.7-1.9; p <0.001), and 2.5 (95% CI: 2.2-2.9; p<0.001), respectively. Additionally, moderately-severely frail women also demonstrated the highest relative risk of UTI within 30 days of sling surgery [aRR 2.4, (95% CI 1.9-2.9; p <0.001)], compared to women who were not frail (Table 2).
Table 2.
Relative Risk of 30-day Complications, Urinary Tract Infection, and 1-Year Mortality
| Basic Statistics | Univariate Model RR | Multivariate Model RR | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Observed N (%) |
Event # (%) | P value |
RR & 95% CI | P value | Global p value |
RR & 95% CI | p-value | Global p value |
|
| 30-Day Complications (Including UTI) | |||||||||
| Not Frail (CFI < 0.15) | 25012 (46.2) | 4379 (17.5) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Prefrail (0.15≤CFI<0.25) | 26326 (48.7) | 6138 (23.3) | 1.3 (1.3 - 1.4) | <0.001 | 1.2 (1.2 - 1.3) | <0.001 | |||
| Mildly Frail (0.25≤CFI<0.35) | 2583 (4.8) | 977 (37.8) | 2.2 (2.0 - 2.3) | <0.001 | 1.8 (1.7 - 1.9) | <0.001 | |||
| Moderately-Severely Frail (CFI ≤0.35) | 191 (0.4) | 108 (56.5) | 3.2 (2.8 - 3.7) | <0.001 | 2.5 (2.2 - 2.9) | <0.001 | |||
| 30-Day Urinary Tract Infections | |||||||||
| Not Frail (CFI < 0.15) | 25012 (46.2) | 3281 (13.1) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Prefrail (0.15≤CFI<0.25) | 26326 (48.7) | 4488 (17.0) | 1.3 (1.3 - 1.4) | <0.001 | 1.2 (1.2 - 1.3) | <0.001 | |||
| Mildly Frail (0.25≤CFI<0.35) | 2583 (4.8) | 662 (25.6) | 2.0 (1.8 - 2.1) | <0.001 | 1.7 (1.5 - 1.8) | <0.001 | |||
| Moderately-Severely Frail (CFI ≤0.35) | 191 (0.4) | 72 (37.7) | 2.9 (2.4 - 3.5) | <0.001 | 2.4 (1.9 - 2.9) | <0.001 | |||
| 1-Year Mortality | |||||||||
| Not Frail (CFI < 0.15) | 25012 (46.2) | 85 (0.3) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Prefrail (0.15≤CFI<0.25) | 26326 (48.7) | 298 (1.1) | 3.3 (2.6 - 4.2) | <0.001 | 1.9 (1.5 - 2.5) | <0.001 | |||
| Mildly Frail (0.25≤CFI<0.35) | 2583 (4.8) | 96 (3.7) | 10.9 (8.2 - 14.6) | <0.001 | 3.4 (2.4 - 4.8) | <0.001 | |||
| Moderately-Severely Frail (CFI ≤0.35) | 191 (0.4) | 20 (10.5) | 30.8 (19.3 - 49.1) | <0.001 | 6.7 (4.0 - 11.2) | <0.001 | |||
Models adjusted for age, race, Charlson Comorbidity Index, concomitant POP repair, and calendar year
1-Year Mortality
Overall, 1-year mortality was 0.9% after sling surgery in this cohort of female Medicare beneficiaries. This ranged from 0.3% among non-frail beneficiaries and increased with increasing CFI to 10.5% among moderately-severely frail beneficiaries (p<0.001). On multivariate analysis, compared to female beneficiaries who were not frail, those who were pre-frail, mildly frail, and moderately-severely frail had an aRR of 1-year mortality of 1.9 (95% CI: 1.5-2.5; p<0.001), 3.4 (95% CI: 2.4-4.8; p<0.001), and 6.7 (95% CI: 4.0-11.2; p<0.001), respectively (Table 2).
Repeat Procedures at 1 year
Overall, 4.8% of women in the cohort underwent a repeat procedure for persistent incontinence or obstructed voiding at 1 year, with slightly more procedures being done for persistent incontinence (2.9%) than for obstructed voiding (2.1%). As CFI category increased, there was also a corresponding increase in the percentage of these repeat procedures (Figure 2). On multivariate analysis, compared to female beneficiaries who were not frail, beneficiaries who were pre-frail and mildly-severely frail demonstrated an increased aRR of 1.2 (95% CI: 1.1-1.3, p <0.001) and 1.4 (95% CI: 1.2-1.6, p<0.001) for undergoing a repeat procedure at 1 year, respectively (Table 3). Separate multivariate analyses were performed for anti-incontinence and obstructed voiding procedures individually, which indicated similar trends (data not shown).
Figure 2.
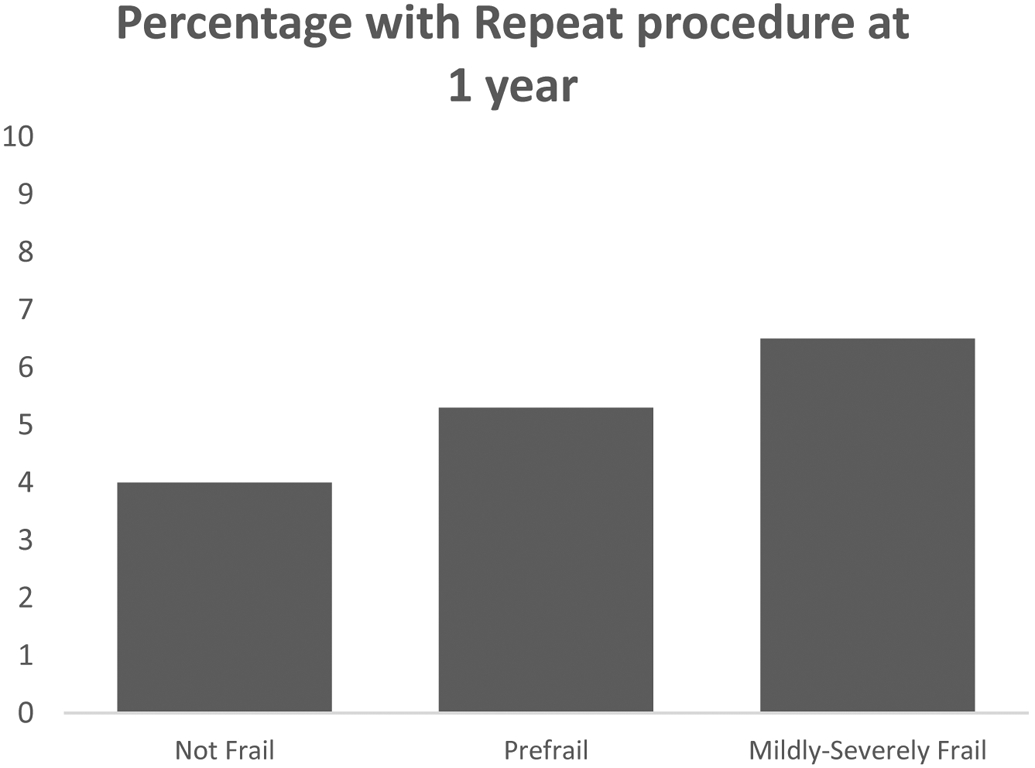
Repeat procedures at 1 year stratified by Claims-based Frailty Index. p<0.001.
Table 3.
Relative Risk of Repeat Sling Surgery, Urethral Bulking, Sling Revision or Urethrolysis at 1 Year
| Basic Statistics |
Univariate Model RR |
Multivariate Model RR |
|||||||
|---|---|---|---|---|---|---|---|---|---|
| Variable Name | Observed N (%) |
Event # (%) |
P value | RR & 95% CI | P value | Global P value |
RR & 95% CI | P value | Global P value |
| Total N (%) | 54112 (100.0) | 2617 (4.8) | |||||||
| Claims-based Frailty Index: N (%) | |||||||||
| Not frail (CFI < 0.15) | 25012 (46.2) | 1006 (4.0) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Prefrail (0.15 ≤ CFI < 0.25) | 26326 (48.7) | 1428 (5.4) | 1.4 (1.3 - 1.5) | <0.001 | 1.2 (1.1 - 1.3) | <0.001 | |||
| Mildly/Moderately-severely frail (CFI≥0.25) | 2774 (5.1) | 183 (6.6) | 1.6 (1.4 - 1.9) | <0.001 | 1.4 (1.2 - 1.6) | <0.001 | |||
| Age Group: N (%) | |||||||||
| 65-69 | 17468 (32.3) | 746 (4.3) | <0.001 | Ref. | <0.001 | Ref. | 0.009 | ||
| 70-74 | 17424 (32.2) | 848 (4.9) | 1.1 (1.0 - 1.3) | 0.008 | 1.1 (1.0 - 1.2) | 0.020 | |||
| 75-79 | 11655 (21.5) | 623 (5.3) | 1.3 (1.1 - 1.4) | <0.001 | 1.2 (1.1 - 1.3) | 0.001 | |||
| 80-85 | 5296 (9.8) | 279 (5.3) | 1.2 (1.1 - 1.4) | 0.002 | 1.2 (1.0 - 1.3) | 0.028 | |||
| ≥85 | 2269 (4.2) | 121 (5.3) | 1.3 (1.0 - 1.5) | 0.020 | 1.2 (1.0 - 1.4) | 0.116 | |||
| Race: N (%) | |||||||||
| White | 49943 (92.3) | 2472 (4.9) | <0.001 | Ref. | <0.001 | Ref. | <0.001 | ||
| Black | 1542 (2.8) | 58 (3.8) | 0.8 (0.6 - 1.0) | 0.035 | 0.8 (0.6 - 1.0) | 0.026 | |||
| Others | 2627 (4.9) | 87 (3.3) | 0.7 (0.5 - 0.8) | <0.001 | 0.7 (0.6 - 0.9) | 0.001 | |||
| Charlson Comorbidity Index: N (%) | |||||||||
| 0 to 1 | 33047 (61.1) | 1477 (4.5) | <0.001 | Ref. | <0.001 | Ref. | 0.101 | ||
| 2 to 4 | 16614 (30.7) | 868 (5.2) | 1.2 (1.1 - 1.3) | <0.001 | 1.1 (1.0 - 1.2) | 0.188 | |||
| > 4 | 4451 (8.2) | 272 (6.1) | 1.4 (1.2 - 1.6) | <0.001 | 1.2 (1.0 - 1.3) | 0.037 | |||
Model adjusted for concomitant POP repair and calendar year
Discussion
In this study, increasing CFI category was associated with an increased relative risk of 30-day complications, 30-day UTIs, and 1-year mortality following sling surgery. Importantly, CFI was independently associated with these increased risks even after adjusting for age, CCI, and concomitant POP repair demonstrating the value of assessing frailty independently. To date, this is the first study that has utilized the CFI with a 100% cohort of Medicare beneficiaries undergoing sling surgery with or without concomitant POP repair to assess surgical outcomes. Our findings underscore the importance of considering and measuring frailty in the preoperative setting, as an emerging body of evidence demonstrates the negative association that frailty has on the risk of postoperative complications.7-10.
In general, reported rates of serious complications following sling surgery are low. In the Trial of Mid-Urethral Slings (TOMUS), which compared transobturator to retropubic sling placement in 597 women, there were no reported cardiovascular complications, pulmonary complications, or death within 1 year of surgery.19 This differs significantly from the findings in our study in which cardiovascular complications, pulmonary complications, and 1-year mortality were observed. These complication rates increased significantly with increasing frailty in moderately-severely frail women who experienced high rates of cardiovascular complications (19.9%), pulmonary complications (9.4%), and 1-year mortality (10.5%). Notably, the study population in the TOMUS trial had an average age of 53 years, which differs significantly from the average age of 74 years in our study. This is not unique to the TOMUS trial; most data regarding outcomes of sling surgery do not account for the heterogeneity of older women with SUI, as they are generally not included in these types of trials. Our study uses real-world data examine surgical outcomes in older women to allow for more appropriate risk stratification and patient counselling prior to surgical intervention.
Another recent study compared outcomes of sling surgery in women with and without frailty. This study found that frail women were more likely to have increased LOS after sling surgery, but overall rates of serious complications after surgery were low in both groups.20 Importantly, the population in this study was significantly younger than the population in our study with a mean age of 56.4 versus 73.6 years. Additionally, our study stratified women into 4 categories of frailty and included more complete data of all fee-for-service Medicare beneficiaries. These two studies taken together emphasize the importance of assessing frailty in all women but demonstrate that accounting for frailty is particularly important in more elderly populations.
The rate of repeat procedures after sling surgery seen in our study is slightly lower that what has been previously reported where 8% of women required a procedure to relieve obstruction.6 This may due to the fact that the authors of that study accounted for additional CPT codes, such as placement of urethral catheter and urethral dilation. However, these codes, particularly urethral catheterization, are known to be unreliable so may explain the lower number of repeat procedures seen in our study.21 Regardless, the rates of repeat procedures seen our study were not ubiquitous in women over 66, and also increased with increasing CFI category. The most notable finding is that frailty was independently associated with this difference in observed rates. One possibility is that frailty represents additional vulnerability towards poor post-operative outcomes, including surgical failures. Another possibility is that frail older adults have more issues with underactive bladders22, leading to an increased risk of retention with sling placement. Looking only at age treats older adults as a homogenous group while using frailty helps to account for differences on an individual level.
In the clinical setting, a practical assessment of frailty is the use of the Timed Up and Go Test (TUGT). The TUGT is performed by asking patients to stand from a seated position in a chair, walk at their normal pace 10 feet to a mark on the floor, turn around, return to the chair, and sit back down. A time of ≤10 seconds, 11-15 seconds, and ≥15 seconds corresponds to not frail, pre-frail, and frail categories. The TUGT has been used in urologic practice to help stratify patients into categories of frailty. 23
A major strength of this study is the use of a large national 100% sample of female Medicare beneficiaries undergoing sling surgery, however, it does not capture pre-operative clinical information such as the type or severity of incontinence, results of urodynamic testing (if performed), or post-void residual volumes. Additionally, we were unable to assess outcomes such as patient satisfaction or improvements in quality of life after surgery or determine the reason for the patient’s repeat procedure at 1-year. Despite these limitations, the data used in this study are ideal for assessing real world outcomes of sling surgery in women ages 65 and older, as they capture data on all women with all levels of frailty, the majority of whom may not have met criteria for clinical trials. Another limitation is that procedure code 57288 captures all sling types including synthetic (retropubic, transobturator, and single incision) and autologous fascia pubovaginal slings which carry different risk benefit profiles. However, it’s reasonable to assume that the breakdown of sling type would not be different amongst groups.
Conclusion
In this study, we found that increasing frailty, as determined by the CFI, was associated with an increased relative risk of 30-day complications including UTIs, 1-year mortality, and the need for repeat procedures for persistent incontinence and obstructed voiding at 1 year. While there were far fewer sling procedures performed in mildly and moderately-severely frail women, the increase in observed complication rates among this frail older cohort were significant and clinically important. These data highlight the notion that frailty should be strongly considered when making decisions regarding sling surgery in older women.
Supplementary Material
Source of Funding:
NIH-NIA R01AG058616
References
- 1.Abufaraj M, Xu T, Cao C, et al. Prevalence and Trends in Urinary Incontinence Among Women in the United States 2005-2018. Am J Obstet Gynecol. Published online March 13, 2021. doi: 10.1016/j.ajog.2021.03.016 [DOI] [PubMed] [Google Scholar]
- 2.Anger JT, Weinberg AE, Albo ME, et al. Trends in Surgical Management of Stress Urinary Incontinence Among Female Medicare Beneficiaries. Urology. 2009;74(2):283–287. doi: 10.1016/j.urology.2009.02.011 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Suskind AM, Kaufman SR, Dunn RL, et al. Population-based trends in ambulatory surgery for urinary incontinence. Int Urogynecology J. 2013;24(2):207–211. doi: 10.1007/s00192-012-1823-y [DOI] [PubMed] [Google Scholar]
- 4.Jonsson Funk M, Levin PJ, Wu JM. Trends in the Surgical Management of Stress Urinary Incontinence. Obstet Gynecol. 2012;119(4):845–851. doi: 10.1097/AOG.0b013e31824b2e3e [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Xue QL. The Frailty Syndrome: Definition and Natural History. Clin Geriatr Med. 2011;27(1):1–15. doi: 10.1016/j.cger.2010.08.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Anger JT, Litwin MS, Wang Q, et al. Complications of Sling Surgery Among Female Medicare Beneficiaries. Obstet Gynecol. 2007;109(3):707–714. doi: 10.1097/01.AOG.0000255975.24668.f2 [DOI] [PubMed] [Google Scholar]
- 7.Suskind AM, Walter LC, Jin C, et al. The impact of Frailty on complications in patients undergoing common urologic procedures; a study from the American College of Surgeons National Surgical Quality Improvement Database. BJU Int. 2016;117(5):836–842. doi: 10.1111/bju.13399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Medendorp AR, Anger JT, Jin C, et al. The impact of frailty on artificial urinary sphincter placement and removal procedures. Urology. 2019;129:210–216. doi: 10.1016/j.urology.2019.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Suskind AM, Zhao S, Boscardin WJ, et al. Comparative outcomes for pelvic organ prolapse surgery among nursing home residents and matched community-dwelling older adults. J Urol. 2021;205(1):199–205. doi: 10.1097/JU.0000000000001331 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Suskind AM, Zhao S, Nik-Ahd F, et al. Comparative outcomes for older adults undergoing surgery for bladder and bowel dysfunction. J Am Geriatr Soc. Published online April 5, 2021. doi: 10.1111/jgs.17118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Berger AA, Tan-Kim J, Menefee SA. The impact of midurethral sling surgery on the development of urinary tract infections. Int Urogynecology J. Published online April 2, 2021. doi: 10.1007/s00192-021-04779-x [DOI] [PubMed] [Google Scholar]
- 12.Nygaard I, Brubaker L, Chai TC, et al. Risk factors for urinary tract infection following incontinence surgery. Int Urogynecology J. 2011;22(10):1255–1265. doi: 10.1007/s00192-011-1429-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Massarweh NN, Legner VJ, Symons RG, et al. Impact of advancing age on abdominal surgical outcomes. Arch Surg Chic Ill 1960. 2009;144(12):1108–1114. doi: 10.1001/archsurg.2009.204 [DOI] [PubMed] [Google Scholar]
- 14.Hendren S, Birkmeyer JD, Yin H, et al. Surgical complications are associated with omission of chemotherapy for stage III colorectal cancer. Dis Colon Rectum. 2010;53(12):1587–1593. doi: 10.1007/DCR.0b013e3181f2f202 [DOI] [PubMed] [Google Scholar]
- 15.Kim DH, Schneeweiss S, Glynn RJ, et al. Measuring Frailty in Medicare Data: Development and Validation of a Claims-Based Frailty Index. J Gerontol A Biol Sci Med Sci. 2018;73(7):980–987. doi: 10.1093/gerona/glx229 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kim DH, Glynn RJ, Avorn J, et al. Validation of a Claims-Based Frailty Index Against Physical Performance and Adverse Health Outcomes in the Health and Retirement Study. J Gerontol A Biol Sci Med Sci. 2019;74(8):1271–1276. doi: 10.1093/gerona/gly197 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Kim DH, Patorno E, Pawar A, et al. Measuring Frailty in Administrative Claims Data: Comparative Performance of Four Claims-Based Frailty Measures in the U.S. Medicare Data. J Gerontol A Biol Sci Med Sci. 2020;75(6):1120–1125. doi: 10.1093/gerona/glz224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. doi: 10.1016/0895-4356(92)90133-8 [DOI] [PubMed] [Google Scholar]
- 19.Richter HE, Albo ME, Zyczynski HM, et al. Retropubic versus transobturator midurethral slings for stress incontinence. N Engl J Med. 2010;362(22):2066–2076. doi: 10.1056/NEJMoa0912658 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Medendorp AR, Liu H, Kwan L, et al. The Impact of Frailty on Outcomes of Sling Surgery with and without Prolapse Repair. J Urol. 2021;206(2):382–389. doi: 10.1097/JU.0000000000001769 [DOI] [PubMed] [Google Scholar]
- 21.Meddings J, Reichert H, Dueweke E, et al. Issues Regarding Identification of Urinary Catheter Use From Medical Records. Agency for Healthcare Research and Quality (AHRQ). Published August 2018. Accessed October 13, 2021. http://www.ahrq.gov/hai/patient-safety-resources/advances-in-hai/hai-article18.html [Google Scholar]
- 22.Chuang YC, Plata M, Lamb LE, et al. Underactive Bladder in Older Adults. Clin Geriatr Med. 2015;31(4):523–533. doi: 10.1016/j.cger.2015.06.002 [DOI] [PubMed] [Google Scholar]
- 23.Pangilinan J, Quanstrom K, Bridge M, et al. The Timed Up and Go Test as a Measure of Frailty in Urologic Practice. Urology. 2017;106:32–38. doi: 10.1016/j.urology.2017.03.054 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


